Documente Academic
Documente Profesional
Documente Cultură
PEDIATRICS
Încărcat de
RizMarieDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
PEDIATRICS
Încărcat de
RizMarieDrepturi de autor:
Formate disponibile
XVII. PEDIATRICS A. ASSESSMENT: 1. OBSERVATION: Always begin with observation. a.
Behavior: Are they happy, friendly, scared, sad, or withdrawn? b. Appearance: Are they well cared for? (hair clean and cut, hygiene, dressed appropriately for weather) c. Nutritional status: Are they skinny or obese? d. Affect: Is it RIGHT for the situation? e. Consolability: Is the child CONTENT and relaxed? A normal HEALTHY baby should be consolable. f. Position: Are they guarding in pain, do they assume a position that helps them breathe? 2. Distraction Techniques: a. This is done to make sure we get the most accurate PHYSICAL assessment and vital signs. b. Dont forget to talk to PARENTS even before you talk to the child. 3. Vital Signs: LEAST invasive first Observe before TOUCHINGor even talking to them. a. Order of obtaining vital signs: 1) Respirations 2) Heart Rate 3) Blood Pressure 4) Temperature b. Always count RR and HR for one full minute because of IRREGULARITIES. c. If vital signs cannot be taken without disturbing the child, then record the BEHAVIOR with the measurements. d. Temperature: 1) Rectal: Do not use in children over 3 MONTHS months. Most reliable measurement of CORE temperature. 2) Axillary: All ages may be done when an ORAL route is not possible. 3) Oral: Start at age 3. 4) Tympanic: All ages. e. Oxygen saturation: Used to obtain a picture of blood oxygen level through the skin.
1) Check perfusion, skin temp, and edema to determine the best location for sensor probe. 2) Common sites are ORAL and AXILLARY. 3) Record what is going on at the time the pulse ox is measured. Will activity level affect the oxygen level? YES 4) The pulse wave form/intensity display on the oximeter machine should correlate with the childs RADIAL pulse. 4. Nutritional Assessment: a. General growth within ________ to__________ percent for height, weight and head circumference is desired. 1) The fiftieth percentile is the LEAST growth. 2) What happens to the growth rate between 6 and 12 years of age? SLOWS DOWN 3) How much earlier do girls experience the onset of adolescence?___________ b. Lab Values: 1) Hemoglobin/Hematocrit 2) __________________ 3) Creatinine 4) Nitrogen Hint: Always document where temperature was taken, do not add a degree. 5. Physical Assessment: a. Hair 1) Want hair to be _______________ and soft to touch. 2) Poorly nourished it will be _________ and course. b. Fingernails 1) Tell you about hygiene 2) Emotional status c. Skin If skin is pale, it could be a sign of anemia. d. Eyes If eyes are sunken, could be a sign of DEHYDRATION. e. Mouth Assess mucosa color and moisture. f. Teeth Assess hygiene and check their gums. 6. Pain Assessment a. The name of the pain scale is CRIES, its an acronym for: Crying (0-2) Requires increased oxygen (0-2) Increased vital signs (0-2)
Expression (0-2) Sleepless (0-2) The __________________ the score the __________ pain in all the scales. b. FLACC Face, Legs, Activity, ______________, Consolability. 0-10 scale: 0 no pain, 10 worst pain Hurst Review Services 233 c. Wong-Baker rating scale is used on children at what age? Any age but usually 3 years and older. Make sure child has cognitive development and is not developmentally delayed. Scale is 0-5. d. Numerical scale is used at age 5 and older. B. Respiratory System: 1. General Assessment: a. Accessory muscle use. b. Flaring __________ c. Pallor d. Sternal ________________ e. Consolability crying, restlessness and agitation may mean hypoxia. f. Capillary refill greater than________ seconds. 2. Upper Respiratory Disease: a. Laryngotracheobronchitis: Most ________________ type of Croup experienced by children admitted to the hospital and primarily affects children under 5. 1) Causes: Parainfluenza, adenovirus, and RSV 2) S/S: Slight to severe diarrhea ________________ or brassy cough. Increased temperature. 234 Hurst Review Services 3) Tx: Mild croup can be treated at home with steam (hot showers), cool mist humidifiers, car rides with windows down. If symptoms worsen or do not improve, hospitalization is required with corticosteroid therapy. b. Epiglottitis: 1) Causes: H. influenza 2) S/S: Absence of cough Drooling Agitation with the rapid progression to severe respiratory distress.
3) Tx: This is an emergency May require intubation or trach IV antibiotics and corticosteroids c. Tonsillitis: 1) S/S: Difficulty swallowing and breathing so child is a _____________ breather and they have bad breath. Impaired taste and smell, voice has nasal/muffled quality. Persistent couch Swollen tonsils can block drainage of the ear canal and cause otitis media. 2) Tx: Tonsillectomy How should a client be positioned after a tonsillectomy? Place on side with elevated head of bed or __________. Why are brown and red fluids not given post op? We do not want anything to be confused with ___________. What would indicate that hemorrhaging is occurring? ______________ swallowing How many days post op is the client at risk for hemorrhage? Hint: Children with Epiglottitis usually look worse than they sound, and the kid with LTB sounds worse then they look. Hurst Review Services 235 Complaint post op? Sore throat and slight _______ pain Low grade temp Bad breath d. Otitis Media: 1) Patho: What part of the ear is affected? __________ ear The Eustachian tubes are blocked. It usually follows an upper respiratory infection. 2) S/S: What does the tympanic membrane look like with otitis? Bulging and bright ______ 3) Tx: Do heating pads help with the pain? _________ Avoid ________________. And provide soft foods. Lie on the ___________________ side. May not hear you. Avoid smoke. May require PE tubes to keep the middle ear ________________.
The ear tube (grommet) stays in about 6 months and then falls out. 4) Prevention: While tubes are in wear ear plugs when bathing or swimming. Have baby _______________________ for feedings. No bottle propping. AVOID nose blowing. Avoid smoke. 3. Lower Respiratory Tract Disease a. RSV Respiratory Syncytial Virus: 1) Causes: An acute viral infection that affects the bronchioles and includes RSV bronchiolitis or RSV pneumonia. Leading cause of Lower Respiratory Tract Illness in children less than ________ years. 236 Hurst Review Services 2) Risk Factors: Prematurity Congenital disorders Smoke Focus is on _________________ (high risk will get RSV vaccine) 3) S/S: URI Nasal ____________________ Mild fever Dyspnea Nonproductive ________ Tachypnea with flaring nares Retraction and _________________ It is important to know the onset of s/s because the disease will become worse on days _________________. 4) Dx: Nasal ________________. 5) Tx: Transmission _________________ precautions. Teach good hand washing Mild Treat symptoms (supportive care: antipyretics) Severe Oxygen: may need mechanical ventilation IV fluids Suction Antipyretics Antiviral (Ribavirin) Hint: Sign and symptoms can range from mild to severe; can go from cough, runny nose with copious amounts of mucus, to severe respiratory distress!
b. Pneumonia: 1) Causes: Viral (RSV, adenovirus or parainfluenza) Bacterial (Culprit is ____________ pneumonia) children <4 yrs Mycotic (walking pneumonia) primarily in adolescents. Aspiration pneumonia (something other than air gets in the lung) 2) S/S: Fine ____________ or rhonchi with a cough that is productive or nonproductive. Abdominal distention Back pain Fever that is usually high. Chest pain from coughing 3) Tx: Oxygen Fluids Antibiotics Antipyretics Nebulizer Cough suppressant c. Asthma: (see 5th day material) d. Down Syndrome: 1) What type of infection are Down Syndrome children prone to developing? _______________________ Why? Because they have a poor _________________ system 2) The most common type of defect associated with Down Syndrome is ___________ ______________. 3) The primary aim in genetic counseling is to inform the parents of their _____________. e. Cystic Fibrosis: 1) Causes: ____________ trait, and must get trait from _______ parents. 2) S/S: ___________, _________________ secretions. Characterized by ____________ gland dysfunction. (These secrete mucus) Thick, sticky secretions are found in the _____________ and GI tract. 238 Hurst Review Services 3) Dx: Diagnostic test for cystic fibrosis? Positive __________ chloride test At risk for ___________________. The earliest sign in the newborn is the meconium, called _____________. They will have steatorrhea stools, which means ________ and _________.
4) Tx: Enzymes that help improve digestion are the ______________ enzymes. Take _______ minutes prior to eating, do not crush or chew. Need a well balanced, low fat, high calorie, ________ protein diet. Require _______% of the recommended daily allowance. They need to take ________ soluble vitamins including A, D, E, and K. C. Cardiac: 1. Heart Failure: a. Causes: Usually due to congenital defects. b. S/S: 1) Lips turn blue when taking a ______________. 2) Increase pulse at rest, or with slight _______________. 3) Increased respiratory rate 4) Scalp sweating 5) Fatigue 6) Sudden weight _______ c. Tx: 1) Ongoing assessment 2) Control room temperature 3) Sit them up 4) Rest 5) __________ stimuli 6) Cool, humidified oxygen 7) Uninterrupted sleep Fluid retention think heart problems first! Hurst Review Services 239 2. Cardiac Medications for pediatric clients: a. Digoxin: 1) Infants rarely get more than _______cc. 2) Give ______ hour before and _____ hours after feedings. 3) DO NOT mix with medicine, ___________ or fluid. 4) Always check the dose with another nurse. 5) Check the apical pulse for __________________. b. Ace Inhibitors: enalapril (Vasotec), captopril (Capoten) 1) Side effects: ____________ blood pressure Kidney problems ________ cough 2) Action: They block __________________. c. Lasix: To decrease the volume. 3. Nutrition in HF Pediatric Client: a. Well rested prior to eating. 1) Feed them when they wake up or show signs of hunger.
2) ______________ crying. b. Small frequent feedings every __________, no longer than ________________. c. High calories. d. We want to use a ________nipple with a __________ opening so the baby wont have to work so hard to get the formula out. e. May require gavage feedings. f. Usually dont require sodium and water restrictions because of decreased intake. 240 Hurst Review Services 4. Acquired Cardiac Disease: a. Rheumatic Fever is an inflammatory disease that occurs after an infection with ___________ beta hemolytic streptococcus. 1) Major cardiac clinical manifestation is _____________. 2) Therapeutic management is ________________, if they are allergic then erythromycin is the drug of choice. b. Kawasaki Disease is characterized by wide spread ______________ of the small and medium sized blood vessels. Coronary arteries are most susceptible. Treatment: High dose IV immune-globulin _______________ therapy _____________ environment. D. GI System: 1. Cleft Palate/Cleft Lip: a. What is the top nursing diagnosis? Alternation in __________________ 1) Feed with an ______________ nipple or medicine dropper down the side of the mouth. 2) Burp frequently so they will not swallow a lot of _____________. b. Cleft Lip Repair: 1) Position on back or side lying to protect the ___________________. 2) Do not place them ________________. 3) Clean the suture line with ______________ post op. c. Cleft Palate Repair: 1) Place them prone to promote drainage. 2) Avoid putting things in their mouth (thermometers, straws). 3) Soft diet until well healed 4) Are speech defects common? _______
5) When is the best time to do this? Before ___________ development. 6) What type of restraints would be used? ____________ Hurst Review Services 241 2. GER, GERD: GER becomes GERD when complications such as failure to thrive, bleeding, or difficulty swallowing (dysphagia) occurs. a. Positioning: 1) ____________ position with feedings and at night. 2) 30 degree elevated prone position to _________ reflux and improve stomach ____________. b. Feedings: 1) Small frequent feedings of ____________ formula. 2) Breast feeding continues with more frequent feedings or expressing the milk for thickening with rice cereal. c. Medication: H2 blockers, Proton pump inhibitors 3. Esophageal Atresia/T-E Fistula: a. Causes: The saliva cannot make it to the stomach because the esophagus ends in a blind ____________. b. S/S: 1) Why do babies with esophageal atresia not have meconium? Because they never swallowed _____________ fluid. 2) How are they feed? _____________ tube 3) T E Fistula watch for C_____________ Chocking especially while drinking Cyanosis The first feeding needs to be ____________. The top nursing diagnosis is potential for ________________. c. Tx: 1) They will do corrective surgery and the infant is placed on their back with _________ and ________________ elevated. 2) It is not uncommon to see polyhydramnios in pregnancy when the infant has GI problems. The infant does not swallow any amniotic fluid so it just builds up. 242 Hurst Review Services 4. Pyloric Stenosis
a. S/S: 1) Projectile VOMITTING usually after eating. 2) Very hungry 3) OLIVE shaped mass in epigastric region. 4) Peristalsis is obvious. b. Dx: Pyloric ultrasound c. Tx: 1) Hydration 2) Intake and OUTPUT 3) Daily WEIGHT 4) Monitor urine specific gravity 5) _________________ 5. Intussusception: (When a piece of bowel goes backwards inside itself forming an obstruction) a. S/S: 1) Sudden ______________ 2) Cramping 3) Abdominal _____________ 4) Inconsolability 5) Drawing up _____________ 6) Currant ____________ stools (monitor stools) b. Dx/Tx: The definitive diagnosis is through a _________ __________ and this will sometimes fix the problem. Teach sign and symptoms of reoccurrence. 6. Hirschsprungs Disease: a congenital anomaly also known as aganglionic megacolon that results in a mechanical obstruction along the bowel (sigmoid). a. S/S: 1) The presenting symptom is _______________________. 2) Abdominal distention. 3) ____________- like stools that have a foul smell. Hurst Review Services 243 b. Tx: 1) Remove the portion of the bowel that is diseased. 2) May require two surgeries to give the intestines time to heal. 7. Imperforate Anus: There is no __________________ opening, therefore the baby will not pass the _______________. They will do surgery, so they may come back with a ________________ colostomy. 8. Celiac Disease: a. Causes: A genetic malabsorption disorder where there is a permanent intestinal
intolerance to ______________. b. Tx: 1) No food with ___________________. (Vegetable proteins) 2) They cannot have BROW. B____________ R____________ O____________ W___________ 3) They can have RCS. R____________ C____________ S____________ 9. Genitourinary: a. UTI-Urinary Tract Infection: 1) S/S: In newborns and children <2, the s/s may be nonspecific- might even seem to be a GI problem. Failure to thrive _________ problems Vomiting and __________ If left untreated kidney becomes small, tissue may be destroyed and scarring occurs and then the kidney could lead to ______________. Urine smells fishy Predisposing factors (renal anomalies, constipation, bubble baths, poor hygiene, pin worms, sexual abuse) 244 Hurst Review Services Classic symptoms in children >2: Frequency Dysuria Fever ___________ pain Hematuria 2) Dx: Properly collected urine specimen Most accurate method is _______________. 3) Tx: Antibiotic therapy: PO or IV b. Testicular torsion: surgical emergency Painful condition caused by the sudden twisting of the spermatic cord which results in the loss of blood flow to the ___________. Occurs in 1 out of every 40,000 males with a peak onset of _______ years of age. Most common cause of __________ loss in adolescent males. If not diagnosed in a timely manner, they can ________ the affected testicle.
1) S/S: Unilateral pain to affected testicles Edema May experience __________ and vomiting _______________ of the testicles 2) Tx: Surgery E. Hematology: 1. General Information: When caring for a client with a hematologic disorder, always include ______________ isolation as part of their plan of care. High risk for _________________ Encourage __________ __________ Always use sterile technique. 2. Sickle Cell Disease (SCD) This is a hereditary disorder in which the ___________________ is partly or completely replaced with sickleshaped hemoglobin. Sickle shaped hemoglobin or Hgbs cannot carry _________ like normal Hgb. a. S/S: 1) __________ in the areas of involvement. 2) Anorexia. 3) Exercise _____________________. b. Tx: 1) _________ __________ 2) HYDRATION 3) Analgesics 4) Antibiotics 5) ___________ transfusions and 6) Oxygen F. Childhood Cancer: 1. Leukemia: a. This is cancer of the blood forming tissue and proliferation of _____________ white cells. b. When thinking of leukemia always remember immunosuppression, thrombocytopenia, ________________. c. Two types ALL (acute lymphoid leukemia) and AML (acute myelogenous) d. S/S: Fever Pallor Anorexia Petechiae Vague abdominal pain Easily acquired infections
2. Now, Wilms tumor or nephroblastoma are found where? _________________ a. Most common presenting sign is ___________________ or non-tender mass on one side of the abdomen. b. Dont palpate the ______________. c. ____________ _____________ while bathing or moving the client. 246 Hurst Review Services G. Neurology: 1. Hydrocephalus: A disturbance of the ventricular circulation of the cerebral spinal fluid in the __________________. Increase of cranial pressure. a. S/S: 1) Bulging of the _____________ fontanel 2) Dilated scalp veins 3) Depressed ________ 4) Irritability and changes in the __________ 5) High-pitched cry b. Tx: Insertion of a VP (ventriculoperitoneal shunt) 1) Measure the __________ occipital circumference 2) Fontanel and cranial_______________ line assessment 3) Monitor the temperature 4) ___________ position 2. Seizure Disorders: Should consider as a symptom of an underlying disorder rather than a disease. May have a short term memory lapses. School work deteriorates which may be ___________ indicator of a problem. a. Classification: 1) Partial: Limited to a particular location of the brain. An ___________ may be the only manifestation. Simple partial means without loss of consciousness with various sensations: Numbness, tingling, prickling, or pain. Complex partial means they have ______________ consciousness and may be confused and unable to respond. 2) Generalized: Loss of ________________. Types:
Tonic-clonic (formally known as grand mal) Myoclonic (sudden, brief contractures of a muscle or group of muscles; may look like a startle reflex) Absence (formally called petit mal and characterized by a brief loss of consciousness) Hurst Review Services 247 b. Tx: Diagnostic testing: EEG, Ultrasound, CT/X-ray Anticonvulsants Airway, Breathing and Circulation DO NOT put anything in the childs _______________. H. Musculoskeletal System 1. Scoliosis is a lateral curvature and ___________ of the spine. Seldom apparent before age 10, and can be genetic. a. Contributing factors: Heavy __________________ (suitcases, grocery, etc.) Carrying children on hips b. Tx: The 3 Os Observation Orthosis (supports and braces) O ______________ which usually is spinal fusion with rod. I. Early Childhood Conditions: 1. Pin Worms: How are they spread? __________________________ How are they diagnosed? _________________________ a. S/S: Intense rectal _________________ General irritability Restlessness Poor sleep Bed wetting Distractibility Short attention span b. Tx: Mebendazole (Vermox) Hand ______________ Keep fingernails ______________ 248 Hurst Review Services 2. Chicken Pox: Prevent ___________ in the lesions. Home remedies that alleviate itching are ___________ bath, __________ ___________ paste. Is it contagious? ________ If they have an increased risk for severe varicella, Acyclovir is prescribed. J. Middle Childhood Conditions: Head Lice:
Common symptom: _________________ How are lice spread? _________________ contact K. Adolescent Conditions: Mononucleosis: What is the name of the virus that causes infectious mononucleosis? _____________ How is it spread? ____________ intimate contact Tx: Rest, analgesics and fluid The spleen will be enlarged so you dont want them to participate in contact sports.
S-ar putea să vă placă și
- RESPIRATORYDocument3 paginiRESPIRATORYRizMarie67% (3)
- NATIONAL COUNCIL LICENSURE EXAMINATION FOR REGISTERED NURSES (NCLEX-RN): Passbooks Study GuideDe la EverandNATIONAL COUNCIL LICENSURE EXAMINATION FOR REGISTERED NURSES (NCLEX-RN): Passbooks Study GuideÎncă nu există evaluări
- BURNSDocument4 paginiBURNSRizMarie100% (2)
- ONCOLOGYDocument6 paginiONCOLOGYRizMarie100% (2)
- ORTHODocument2 paginiORTHORizMarie50% (2)
- FINALTHOUGHTSDocument5 paginiFINALTHOUGHTSRizMarieÎncă nu există evaluări
- NEUROLOGICALDocument3 paginiNEUROLOGICALRizMarie100% (4)
- Psychiatric NursingDocument5 paginiPsychiatric NursingRizMarie100% (4)
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideDe la EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideÎncă nu există evaluări
- MANAGEMENTDocument3 paginiMANAGEMENTRizMarie50% (4)
- ENDOCRINEDocument5 paginiENDOCRINERizMarie100% (3)
- Exam Facts NCLEX PN Nursing Study GuideDe la EverandExam Facts NCLEX PN Nursing Study GuideEvaluare: 3.5 din 5 stele3.5/5 (6)
- ACIDDocument2 paginiACIDRizMarie100% (2)
- Hurst - Content Review - Cardio (Edit)Document8 paginiHurst - Content Review - Cardio (Edit)Elaine NorbergÎncă nu există evaluări
- Fluids and ElectrolytesDocument6 paginiFluids and ElectrolytesRizMarie100% (1)
- NCLEX Helpful HintsDocument2 paginiNCLEX Helpful HintsJamie Antonini GrantÎncă nu există evaluări
- Hurst BurnsDocument4 paginiHurst BurnsKristin Jones100% (5)
- Ati 2Document10 paginiAti 2KitesaMedeksa100% (6)
- ATI Comprehensive Predictor: Study Online atDocument9 paginiATI Comprehensive Predictor: Study Online atVanessaMUellerÎncă nu există evaluări
- NCLEX Test Taking TipsDocument3 paginiNCLEX Test Taking TipsjrilleraÎncă nu există evaluări
- Testing Strategies: Hurst Review Services 240Document3 paginiTesting Strategies: Hurst Review Services 240reynold100% (1)
- Sata ListDocument11 paginiSata ListNaidin Catherine De Guzman-AlcalaÎncă nu există evaluări
- NCSBN Test Questions: Review: Michelle Hall June 2009Document7 paginiNCSBN Test Questions: Review: Michelle Hall June 2009Michelle Sammons-Hall100% (4)
- Review NotesDocument82 paginiReview Notesjames100% (2)
- Chronic Arterial Vs Chronic Venous PDFDocument1 paginăChronic Arterial Vs Chronic Venous PDFRizMarieÎncă nu există evaluări
- Select All That Apply SATADocument58 paginiSelect All That Apply SATANicholas TagleÎncă nu există evaluări
- Key Concepts For An NCLEX-RN Cram SheetDocument3 paginiKey Concepts For An NCLEX-RN Cram Sheetema100% (2)
- CNS Stimulants and Depressants PDFDocument5 paginiCNS Stimulants and Depressants PDFRizMarie100% (1)
- NCLEX Study GuideDocument7 paginiNCLEX Study Guidemmgoodall22100% (3)
- Nclex PointersDocument2 paginiNclex PointersKira95% (19)
- My Nclex Study GuideDocument4 paginiMy Nclex Study GuideLogin Nurse100% (1)
- How To PassDocument9 paginiHow To PassPatrick Tera ReyesÎncă nu există evaluări
- Archer Incorrect Questions For NclexDocument19 paginiArcher Incorrect Questions For NclexSpoon100% (1)
- NCLEX RN Practice Questions 17Document29 paginiNCLEX RN Practice Questions 17clarheena89% (9)
- CARDIODocument7 paginiCARDIORizMarie100% (7)
- Nclex NotesDocument18 paginiNclex Notesmaane1005Încă nu există evaluări
- Nclex ReviewDocument27 paginiNclex ReviewNicole Chadwick100% (4)
- Hesi GemsDocument27 paginiHesi Gemssugarplum22Încă nu există evaluări
- 2pdfnclex ReviewDocument187 pagini2pdfnclex Reviewgarvita100% (1)
- RemarDocument4 paginiRemarChelle RocoÎncă nu există evaluări
- Common Lab Values With Normals and Critical Values PDFDocument2 paginiCommon Lab Values With Normals and Critical Values PDFRizMarie100% (7)
- RN Intense Remedial Packet AnswersDocument53 paginiRN Intense Remedial Packet AnswersAli Resendiz50% (4)
- Breaking Down The NCLEX QuestionsDocument2 paginiBreaking Down The NCLEX QuestionsKaloy KamaoÎncă nu există evaluări
- Nclex Sata 1 5Document14 paginiNclex Sata 1 5Elizabella Henrietta TanaquilÎncă nu există evaluări
- Obstetric Questions: Please State Whether The Following Statements Are TRUE or FALSEDocument8 paginiObstetric Questions: Please State Whether The Following Statements Are TRUE or FALSEjulialeo90% (10)
- Hesi v4 Sample 2015Document2 paginiHesi v4 Sample 2015james67% (3)
- Nclex StudyDocument14 paginiNclex StudyKNQGÎncă nu există evaluări
- Testing StrategiesDocument1 paginăTesting StrategiesRizMarie100% (2)
- LP K EnglishDocument3 paginiLP K Englishivander sudarnotoÎncă nu există evaluări
- Newborn AssessmentDocument8 paginiNewborn Assessmentapi-259796113Încă nu există evaluări
- Reading Final Qs 1 1 PDFDocument64 paginiReading Final Qs 1 1 PDFMuntaserAlawiÎncă nu există evaluări
- Lesson 13. Pediatric UnitDocument21 paginiLesson 13. Pediatric UnitPaola ChaconÎncă nu există evaluări
- English For Professional Nurse 2Document7 paginiEnglish For Professional Nurse 2Anonymous HWsv9pBUhÎncă nu există evaluări
- Asthma 05 2011 Ta PDFDocument3 paginiAsthma 05 2011 Ta PDFRizMarie100% (1)
- RenalDocument3 paginiRenalStefanie HenryÎncă nu există evaluări
- Fluids and ElectrolytesDocument6 paginiFluids and ElectrolytesRizMarie100% (1)
- Common Lab Values With Normals and Critical Values PDFDocument2 paginiCommon Lab Values With Normals and Critical Values PDFRizMarie100% (7)
- CNS Stimulants and Depressants PDFDocument5 paginiCNS Stimulants and Depressants PDFRizMarie100% (1)
- Testing StrategiesDocument1 paginăTesting StrategiesRizMarie100% (2)
- Psychiatric NursingDocument5 paginiPsychiatric NursingRizMarie100% (4)
- MATERNITYDocument6 paginiMATERNITYRizMarie100% (3)
- Chronic Arterial Vs Chronic Venous PDFDocument1 paginăChronic Arterial Vs Chronic Venous PDFRizMarieÎncă nu există evaluări
- NEUROLOGICALDocument3 paginiNEUROLOGICALRizMarie100% (4)
- ENDOCRINEDocument5 paginiENDOCRINERizMarie100% (3)
- TestDocument6 paginiTestRizMarieÎncă nu există evaluări
- FINALTHOUGHTSDocument5 paginiFINALTHOUGHTSRizMarieÎncă nu există evaluări
- MANAGEMENTDocument3 paginiMANAGEMENTRizMarie50% (4)
- GASTROINTESTINALDocument5 paginiGASTROINTESTINALRizMarie100% (3)
- NELEC2Document2 paginiNELEC2RizMarieÎncă nu există evaluări
- CARDIODocument7 paginiCARDIORizMarie100% (7)
- NP Test - 350 Items Key AnswerDocument56 paginiNP Test - 350 Items Key AnswerRizMarie100% (1)
- ACIDDocument2 paginiACIDRizMarie100% (2)
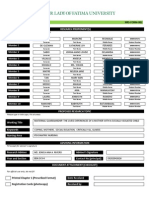
- Pathophysiology: Our Lady of Fatima UniversityDocument2 paginiPathophysiology: Our Lady of Fatima UniversityRizMarieÎncă nu există evaluări
- Chronic Osteomyelitis (M&R)Document8 paginiChronic Osteomyelitis (M&R)RizMarieÎncă nu există evaluări
- C CCC CCCCCC C C C (C C+ CCC CC) Cãc CCCCC CC CC, CCCC C (C C) CC CC CCCC CC C CC C C (CC) CDocument5 paginiC CCC CCCCCC C C C (C C+ CCC CC) Cãc CCCCC CC CC, CCCC C (C C) CC CC CCCC CC C CC C C (CC) CRizMarieÎncă nu există evaluări
- RizalDocument7 paginiRizalRizMarieÎncă nu există evaluări
- NRes FormDocument1 paginăNRes FormRizMarieÎncă nu există evaluări
- Asian CivDocument4 paginiAsian CivRizMarieÎncă nu există evaluări
- Gastroesophageal Reflux DiseaseDocument3 paginiGastroesophageal Reflux DiseaseTANYAÎncă nu există evaluări
- Towards Better Patient Care Drugs To Avoid in 2023Document11 paginiTowards Better Patient Care Drugs To Avoid in 2023Santiago ChávezÎncă nu există evaluări
- Globus PharyngusDocument10 paginiGlobus PharyngusamalÎncă nu există evaluări
- Reflux Symptom Index ValidationDocument4 paginiReflux Symptom Index ValidationSebastian Castro TigheÎncă nu există evaluări
- Veterinary Medical Terminology: Dr.H.HoseinzadehDocument27 paginiVeterinary Medical Terminology: Dr.H.HoseinzadehJuk CondeÎncă nu există evaluări
- Prevalence of Gastroesophageal Reflux Disease (GERD) in Dyspepsia Patients in Primary Referral HospitalDocument6 paginiPrevalence of Gastroesophageal Reflux Disease (GERD) in Dyspepsia Patients in Primary Referral HospitalAbrar TaraÎncă nu există evaluări
- W L S A: Laparoscopic Sleeve Gastrectomy (LSG)Document32 paginiW L S A: Laparoscopic Sleeve Gastrectomy (LSG)lucyÎncă nu există evaluări
- SulodexideDocument7 paginiSulodexideZera Cortez100% (1)
- How-Do-I-Treat-My-Cough-At-Night-Parkinson PatientDocument1 paginăHow-Do-I-Treat-My-Cough-At-Night-Parkinson PatientMuhammad BabarÎncă nu există evaluări
- Chapter 017Document17 paginiChapter 017MuhTaswinTachir100% (1)
- 13 Inflammatory Disorders of LarynxDocument83 pagini13 Inflammatory Disorders of LarynxAbhishek ShahÎncă nu există evaluări
- GERD Diagnosis and Management 2013Document21 paginiGERD Diagnosis and Management 2013vhinrichÎncă nu există evaluări
- MS Lec Gi and Icp Reviewer - Limon, Adine Jeminah DDocument8 paginiMS Lec Gi and Icp Reviewer - Limon, Adine Jeminah DShawn TejanoÎncă nu există evaluări
- Term 3 Rationale Pharmacology and MCNDocument35 paginiTerm 3 Rationale Pharmacology and MCNKing KongÎncă nu există evaluări
- OesophagusDocument15 paginiOesophagusIBRAHEM JUMAHÎncă nu există evaluări
- Dyspepsia & GERDDocument18 paginiDyspepsia & GERDKiani LarasÎncă nu există evaluări
- 42-0139!00!02-EXP, Antacid Analysis and TitrationDocument18 pagini42-0139!00!02-EXP, Antacid Analysis and TitrationYogita Tonger0% (1)
- Just One Voice - High Res Ebook PDFDocument92 paginiJust One Voice - High Res Ebook PDFmwi66399Încă nu există evaluări
- Yukot, ChungDocument18 paginiYukot, ChungCath DetoperezÎncă nu există evaluări
- Gastrointestinal Imaging - The Requisites (4e) (2014) (Unitedvrg)Document435 paginiGastrointestinal Imaging - The Requisites (4e) (2014) (Unitedvrg)crazyballerman80890% (10)
- SIBODocument146 paginiSIBOMundhir Al-Khusaibi78% (9)
- Approach To Uninvestigated DyspepsiaDocument18 paginiApproach To Uninvestigated DyspepsiaAshish SatyalÎncă nu există evaluări
- Shely Dinda Fatma Anggraeni - P17321205020 - Group e - K5 - Resume Journal - Alih Kredit 2021Document8 paginiShely Dinda Fatma Anggraeni - P17321205020 - Group e - K5 - Resume Journal - Alih Kredit 2021shelydindafatmaanggraeniÎncă nu există evaluări
- Assessment of Feeding and MealtimeDocument11 paginiAssessment of Feeding and Mealtimeabdurrakhman saparÎncă nu există evaluări
- Swasthya Kalyan Institute of Naturopathy and Yogic Sciences Sitapura, JaipurDocument26 paginiSwasthya Kalyan Institute of Naturopathy and Yogic Sciences Sitapura, JaipurCyber MagicÎncă nu există evaluări
- Chinese Herb ChartDocument32 paginiChinese Herb ChartXronia PollaÎncă nu există evaluări
- Holistic Health Solutions PDFDocument667 paginiHolistic Health Solutions PDFBhargavaÎncă nu există evaluări
- Gerd - Peptic Ulcer - GastritisDocument87 paginiGerd - Peptic Ulcer - GastritisErickson V. LibutÎncă nu există evaluări
- Gastroenterology MCQDocument2 paginiGastroenterology MCQsanthyakunjumon100% (7)
- Block 3Document63 paginiBlock 3M Kaisar PahlawanÎncă nu există evaluări
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDe la EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedEvaluare: 5 din 5 stele5/5 (81)
- The Obesity Code: Unlocking the Secrets of Weight LossDe la EverandThe Obesity Code: Unlocking the Secrets of Weight LossEvaluare: 4 din 5 stele4/5 (6)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDDe la EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDEvaluare: 5 din 5 stele5/5 (1)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDe la EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeEvaluare: 2 din 5 stele2/5 (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityDe la EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityEvaluare: 4 din 5 stele4/5 (27)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionDe la EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionEvaluare: 4 din 5 stele4/5 (404)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisDe la EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisEvaluare: 4.5 din 5 stele4.5/5 (42)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsDe la EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsEvaluare: 5 din 5 stele5/5 (1)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaDe la EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaEvaluare: 4.5 din 5 stele4.5/5 (266)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisDe la EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisEvaluare: 4 din 5 stele4/5 (1)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsDe la EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsÎncă nu există evaluări
- Why We Die: The New Science of Aging and the Quest for ImmortalityDe la EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityEvaluare: 4 din 5 stele4/5 (3)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryDe la EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryEvaluare: 4 din 5 stele4/5 (44)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.De la EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Evaluare: 4.5 din 5 stele4.5/5 (110)
- Gut: the new and revised Sunday Times bestsellerDe la EverandGut: the new and revised Sunday Times bestsellerEvaluare: 4 din 5 stele4/5 (392)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisDe la EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisEvaluare: 3.5 din 5 stele3.5/5 (2)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsDe la EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsEvaluare: 3.5 din 5 stele3.5/5 (3)
- The Marshmallow Test: Mastering Self-ControlDe la EverandThe Marshmallow Test: Mastering Self-ControlEvaluare: 4.5 din 5 stele4.5/5 (58)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingDe la EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingEvaluare: 4 din 5 stele4/5 (1138)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningDe la EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningEvaluare: 4 din 5 stele4/5 (3)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsDe la EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsEvaluare: 4.5 din 5 stele4.5/5 (170)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessDe la EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessEvaluare: 4.5 din 5 stele4.5/5 (328)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)De la EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Încă nu există evaluări