Documente Academic
Documente Profesional
Documente Cultură
Nursing Care Plan For Myocardial Infarction
Încărcat de
mariejo95%(125)95% au considerat acest document util (125 voturi)
211K vizualizări7 paginiThe client reports of chest pain radiating to the left arm and neck and back. Assisting the client in quantifying pain may help to differentiate preexisting and current pain patterns as well as identify complications. Assessing characteristics of chest pain, including location, duration, quality, intensity, presence of radiation, precipitating and alleviating factors.
Descriere originală:
Titlu original
Nursing Care Plan for myocardial infarction
Drepturi de autor
© Attribution Non-Commercial (BY-NC)
Formate disponibile
DOC sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentThe client reports of chest pain radiating to the left arm and neck and back. Assisting the client in quantifying pain may help to differentiate preexisting and current pain patterns as well as identify complications. Assessing characteristics of chest pain, including location, duration, quality, intensity, presence of radiation, precipitating and alleviating factors.
Drepturi de autor:
Attribution Non-Commercial (BY-NC)
Formate disponibile
Descărcați ca DOC sau citiți online pe Scribd
95%(125)95% au considerat acest document util (125 voturi)
211K vizualizări7 paginiNursing Care Plan For Myocardial Infarction
Încărcat de
mariejoThe client reports of chest pain radiating to the left arm and neck and back. Assisting the client in quantifying pain may help to differentiate preexisting and current pain patterns as well as identify complications. Assessing characteristics of chest pain, including location, duration, quality, intensity, presence of radiation, precipitating and alleviating factors.
Drepturi de autor:
Attribution Non-Commercial (BY-NC)
Formate disponibile
Descărcați ca DOC sau citiți online pe Scribd
Sunteți pe pagina 1din 7
XI.
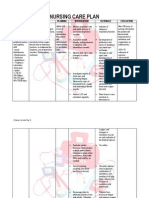
NURSING CARE PLAN
ASSESSMENT DIAGNOSIS PLANNING INTERVENTION RATIONALE EVALUATION
Subjective: Acute (Chest) STG: INDEPENDENT: STG:
Within 1 hour 1. assess 1. pain is indication of Within 1 hour of
The client Pain r/t
of nursing characteristics of MI. assisting the client nursing intervention,
reports of chest myocardial chest pain, including
interventions, in quantifying pain the client had
pain radiating toischemia resulting location, duration,
the client will may differentiate pre- improved comfort in
the left arm and from coronary have improved quality, intensity, existing and current chest, as evidenced
neck and back. artery occlusion comfort in chest, presence of radiation, pain patterns as well by:
with as evidenced by: precipitating and as identify • States a
loss/restriction of • States a alleviating factors, and complications. decrease in the
blood flow to an decrease in as associated rating of the
Objective: the rating symptoms, have client chest pain.
area of the rate pain on a scale of
• Restlessness myocardium and of the • Is able to rest,
chest pain. 1-10 and document
• Facial necrosis of the displays
• Is able to findings in nurse’s reduced
grimacing myocardium. notes.
rest, tension, and
• Fatigue displays 2. obtain history of 2. this provides sleeps
• Peripheral reduced previous cardiac pain information that may comfortably.
tension, and familial history of help to differentiate • Requires
cyanosis cardiac problems.
and sleeps current pain from decrease
• Weak pulse previous problems and
comfortabl analgesia or
• Cold and y. complications. nitroglycerin.
clammy skin • Requires Goal was met.
3. assess respirations, 3. respirations may be
• Palpitations decrease
BP and heart rate with
analgesia increased as a result LTG:
• Shortness of each episodes of chest of pain and associate
or The client had an
breath nitroglyceri
pain. anxiety. improved feeling of
• Elevated 4. maintain bedrest 4. to reduce oxygen
n. control as evidenced
during pain, with consumption and
temperature position of comfort,
by verbalizing a
LTG: demand, to reduce sense of control over
• Pain scale of maintain relaxing competing stimuli and
The client will present situation
8/10 have an
environment to reduces anxiety. and future outcomes
promote calmness.
improved feeling within 2 days of
of control as nursing intervention.
evidenced by Goal was met.
5. prepare for the 5.pain control is a
verbalizing a
administration of priority, as it indicates
sense of control
medications, and ischemia.
over present
monitor response to
situation and
drug therapy. Notify
future outcomes
physician if pain does
within 2 days of
not abate.
nursing
interventions.
6.istruct patient in 6. to decrease
nitroglycerin SL myocardial oxygen
administration after demand and workload
hospitalization. on the heart.
Instruct patient in
activity alterations and
limitations.
7. to promote
7. instruct knowledge and
patient/family in compliance with
medication effects, therapeutic regimen
side-effects, and to alleviate fear of
contraindications and unknown.
symptoms to report.
DEPENDENT: 1. serial ECG and stat
1. obtain a 12-lead ECGs record changes
ECG on admission, that can give evidence
then each time chest of further cardiac
pain recurs for damage and location
evidence of further of MI.
infarction as
prescribed.
2. Morphine is the
2. administer drug of choice to
analgesics as ordered, control MI pain, but
such as morphine other analgesics may
sulfate, meferidine of be used to reduce
Dilaudid N. pain and reduce the
workload on the heart.
3. administer beta- 3. to block
blockers as ordered. sympathetic
stimulation, reduce
heart rate and lowers
myocardial demand.
4. administer calcium- 4. to increase
channel blockers as coronary blood flow
ordered. and collateral
circulation which can
decrease pain due to
ischemia.
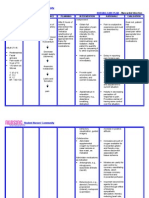
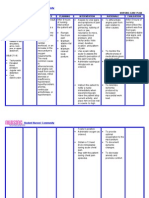
ASSESSMENT DIAGNOSIS PLANNING INTERVENTION RATIONALE EVALUATION
INDEPENDENT:
Subjective: Activity STG: 1. monitor heart rate, 1.changes in VS assist STG:
rhythm, respirations with monitoring
The client Intolerance Within 3 days and blood pressure for physiologic responses to
Within 3 days of
reports of r/t cardiac of nursing abnormalities. Notify increase in activity. nursing
increased dysfunction, interventions, physician of significant interventions,
work of changes in the client will be changes in VS. the client tolerated
breathing oxygen able to tolerate 2. Alleviation of factors activity without
2. Identify causative that are known to create
associated supply and activity without factors leading to intolerance can assist with
excessive dyspnea
with feelings consumption excessive intolerance of activity. development of an and had been able
of weakness as dyspnea and will activity level program. to utilize breathing
and tiredness. evidenced be able to utilize 3. encourage patient to 3. to help give the patient techniques and
by shortness breathing assist with planning a feeling of self-worth and energy
activities, with rest well-being.
Objective: of breath. techniques and periods as necessary. conservation
• Increased energy 4. instruct patient in 4. to decrease energy techniques
heart rate conservation energy conservation expenditure and fatigue. effectively.
• Increased techniques techniques. Goal was met.
effectively. 5. assist with active or 5.to maintain joint
blood passive ROM exercises mobility and muscle tone.
pressure at least QID. LTG:
• Dyspnea LTG: 6.to improve respiratory Within 5 days of
with Within 5 days 6. turn patient at least function and prevent skin nursing
of nursing every 2 hours, and prn. breakdown. interventions, the
exertion
• Pallor interventions, client increased
7. instruct patient in 7. to improve breathing
• Fatigue the client will be isometric and breathing and to increase activity and achieved
and able to increase exercises. level. desired activity
weakness and achieve level,
desired activity 8. provide 8. to promote self-worth progressively, with
• Decreased patient/family with and involves patient and
level, no intolerance
oxygen exercise regimen, with his family with self-care.
progressively, symptoms noted,
saturation written instructions.
with no such as respiratory
• Ischemic
intolerance DEPENDENT: compromise.
ECG 1.Assisst patient with 1. to gradually increase
symptoms Goal was met.
changes ambulation, as ordered, the body to compensate
noted, such as
with progressive for the increase in
respiratory increases as patient’s overload.
compromise. tolerance permits.
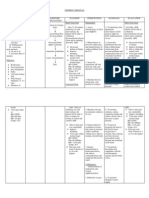
ASSESSMENT DIAGNOSIS PLANNING INTERVENTION RATIONALE EVALUATION
INDEPENDENT:
Subjective: Deficient STG: 1. monitor patient’s 1. to promote optimal STG:
readiness to learn and learning environment
The client Knowledge r/t The client will determine best methods
The client
when patient show
verbalizes new diagnosis be able to to use for teaching. willingness to learn.
verbalized and
questions and lack of verbalize and 2. provide time for 2. to establish trust. demonstrated
regarding understanding demonstrate individual interaction with understanding of
problems and of medical understanding patient. information given
3. instruct patient on 3. to provide information regarding condition,
misconceptions condition. of information procedures that may be to manage medication
about his given regarding performed. regimen and to ensure
medications, and
condition. condition, Instruct patient on compliance. treatment regimen
medications, medications, dose, within 3 days of
Objective: and treatment effects, side effects, nursing
contraindications, and
• Lack of regimen within signs/symptoms to report interventions.
4. client may need to
improvemen 3 days of to physician. increase dietary Goal was met.
t of nursing 4. instruct in dietary potassium if placed on
previous interventions. needs and restrictions, diuretics; sodium should LTG:
such as limiting sodium be limited because of The client had
regimen
or increasing potassium. the potential for fluid
• Inadequate LTG: been able to
retention.
follow-up on The client will 5. provide printed 5. to provide reference correctly perform all
instructions able to correctly materials when possible for the patient and tasks prior to
given. perform all for patient/family to family to refer. discharge.
tasks prior to reviews. Goal was met.
• Anxiety 6. have patient
discharge. 6. to frovide information
• Lack of demonstrate all skills that that patient has gained
understan- will be necessary for a full understanding of
ding. postdischarge. instruction.
7. instruct exercises to be 7. these are helpful in
performed, and to avoid improving cardiac
overtaxing activities. function.
DEPENDENT:
1. refer patient to cardiac 1. to provide further
rehabilitation as ordered improvement and
rehabilitation
postdischarge.
.
S-ar putea să vă placă și
- How To Make Your Girl Squirt EffortlesslyDocument80 paginiHow To Make Your Girl Squirt EffortlesslyKimberly63% (8)
- Psych Nursing Complete Edited Royal PentagonDocument32 paginiPsych Nursing Complete Edited Royal PentagonRichard Ines Valino100% (68)
- Coronary Artery Disease - Case StudyDocument19 paginiCoronary Artery Disease - Case StudyJulieteeySarania100% (3)
- Acute Myocardial InfarctionDocument35 paginiAcute Myocardial Infarctionvirnzrobz80% (10)
- Nursing Care Plan For Liver CirrhosisDocument14 paginiNursing Care Plan For Liver Cirrhosisken93% (75)
- NCP Heart FailureDocument11 paginiNCP Heart FailureaZhermAine100% (1)
- Nursing Care Plan: Assessment Diagnosis Planning Intervention Rationale EvaluationDocument3 paginiNursing Care Plan: Assessment Diagnosis Planning Intervention Rationale Evaluationandronicoc100% (5)
- NCPDocument9 paginiNCPTracy Camille EscobarÎncă nu există evaluări
- Case Study Acute Myocardial InfarctionDocument11 paginiCase Study Acute Myocardial InfarctionChristine Elaine Batusin Ilagan91% (23)
- Nursing Care Plan For Coronary Artery DiseaseDocument3 paginiNursing Care Plan For Coronary Artery DiseaseLorraineAnneSantiagoCandelario91% (22)
- Decreased Cardiac OutputDocument3 paginiDecreased Cardiac OutputTiffany Mathis100% (1)
- Myocardial InfarctionDocument21 paginiMyocardial InfarctionasdnofalÎncă nu există evaluări
- Nursing Care Plan Age: 60 Years OldDocument4 paginiNursing Care Plan Age: 60 Years OldLouise GudmalinÎncă nu există evaluări
- Assessment Diagnoses: Planning Intervention Rationale EvaluationDocument13 paginiAssessment Diagnoses: Planning Intervention Rationale EvaluationdaleaimeeÎncă nu există evaluări
- Decreased Cardiac Output NCPDocument2 paginiDecreased Cardiac Output NCPbaba69baba100% (1)
- Nursing Care Plan - Myocardial InfarctionDocument3 paginiNursing Care Plan - Myocardial Infarctionderic80% (10)
- Acute Myocardial Infarction - CSDocument49 paginiAcute Myocardial Infarction - CSMASII94% (17)
- NURSING CARE PLAN For Myocardial InfarctionDocument16 paginiNURSING CARE PLAN For Myocardial InfarctionFreisanChenMandumotan100% (1)
- Astrovega EZINE March 2023Document51 paginiAstrovega EZINE March 2023VARA PRASADÎncă nu există evaluări
- NURSING CARE PLAN For Myocardial InfarctionDocument13 paginiNURSING CARE PLAN For Myocardial Infarctionbanyenye2593% (14)
- NCP Myocardial InfarctionDocument1 paginăNCP Myocardial InfarctionjamieboyRN88% (8)
- Assessment Inferen CE Plannin G Interve Ntion Rationa LE Evalua TionDocument4 paginiAssessment Inferen CE Plannin G Interve Ntion Rationa LE Evalua TionBg Celo33% (3)
- Nursing Care PlanDocument37 paginiNursing Care Planpia lestrange100% (6)
- NCP #1 Acute PainDocument3 paginiNCP #1 Acute PainJheanAlphonsineT.MeansÎncă nu există evaluări
- NCP AnginaDocument3 paginiNCP AnginaShie LA100% (1)
- Nursing Care PlanDocument7 paginiNursing Care Planmcd7r883% (6)
- Nursing Care Plan For HypertensionDocument5 paginiNursing Care Plan For Hypertensionmariejo89% (84)
- NURSING CARE PLAN Decreased Cardiac Output FnaDocument2 paginiNURSING CARE PLAN Decreased Cardiac Output FnaAce Dioso Tubasco100% (1)
- Ineffective Tissue PerfusionDocument1 paginăIneffective Tissue PerfusionRhae RaynogÎncă nu există evaluări
- Case Study Myocardial InfarctionDocument23 paginiCase Study Myocardial InfarctionJester GalayÎncă nu există evaluări
- Assessment Nursing Diagnosis Planning Interventions Rationale EvaluationsDocument3 paginiAssessment Nursing Diagnosis Planning Interventions Rationale EvaluationsAjay SupanÎncă nu există evaluări
- Nursing Care Plan For Upper Resrpiratory Tract InfectionDocument2 paginiNursing Care Plan For Upper Resrpiratory Tract Infectionmariejo90% (30)
- NCP For Acute Coronary SyndromeDocument3 paginiNCP For Acute Coronary Syndromesarahtot75% (4)
- Myocardial InfarctionDocument5 paginiMyocardial InfarctionDharline Abbygale Garvida AgullanaÎncă nu există evaluări
- NCPDocument4 paginiNCPfairwoods90% (10)
- Nursing Care Plan For Myocardial InfarctionDocument7 paginiNursing Care Plan For Myocardial InfarctionjamieboyRN88% (8)
- NCP For Pain OBDocument2 paginiNCP For Pain OBMao100% (18)
- NCP For Mi PainDocument2 paginiNCP For Mi PainKahMallariÎncă nu există evaluări
- Nursing Care PlanDocument4 paginiNursing Care Planmanu_gutierrez0891% (11)
- Front Page of Our ThesisDocument13 paginiFront Page of Our Thesismariejo100% (4)
- Nursing Diagnosis Diabetic KetoacidosisDocument11 paginiNursing Diagnosis Diabetic Ketoacidosismonisha50% (4)
- Nursing Care Plan For Myocardial Infarction NCPDocument8 paginiNursing Care Plan For Myocardial Infarction NCPderic87% (15)
- NCP - Acute Pain Related Myocardial IschemiaDocument2 paginiNCP - Acute Pain Related Myocardial IschemiaKian HerreraÎncă nu există evaluări
- NCP Heart BlockDocument3 paginiNCP Heart BlockEköw Santiago Javier33% (3)
- Care Plan Unstable AnginaDocument4 paginiCare Plan Unstable Anginaالغزال الذهبي50% (6)
- Research On Curriculum DevelopmentDocument16 paginiResearch On Curriculum Developmentmariejo100% (8)
- Research On Curriculum DevelopmentDocument16 paginiResearch On Curriculum Developmentmariejo100% (8)
- Myocarditis NCP 2Document8 paginiMyocarditis NCP 2astro_aaron117375% (4)
- Nursing Care Plan For HypocalcemiaDocument1 paginăNursing Care Plan For Hypocalcemiamariejo78% (18)
- NURSING CARE PLAN - Myocardial Infarction Assessment Diagnosis Inference Planning Intervention Rationale EvaluationDocument4 paginiNURSING CARE PLAN - Myocardial Infarction Assessment Diagnosis Inference Planning Intervention Rationale Evaluationsweethoney220% (1)
- Soal News ItemDocument11 paginiSoal News ItemYehezkiel Rivaldo Widjaya100% (1)
- ACUTE PAIN BSN III KOLCABA NCP 8th ROTATIONDocument4 paginiACUTE PAIN BSN III KOLCABA NCP 8th ROTATIONKrisheille Amano MirandaÎncă nu există evaluări
- Myocardial Infarction NCPDocument3 paginiMyocardial Infarction NCPlapistolero33% (3)
- NCP - Difficulty of BreathingDocument2 paginiNCP - Difficulty of BreathingTarquin Tomada33% (3)
- Nursing Care PlanDocument13 paginiNursing Care PlanCris Solis33% (3)
- Nursing Care Plan For Myocardial InfarctionDocument7 paginiNursing Care Plan For Myocardial InfarctionRocelyn CristobalÎncă nu există evaluări
- Assessment Diagnosis Planning Intervention Rationale EvaluationDocument6 paginiAssessment Diagnosis Planning Intervention Rationale EvaluationBalloonsRus PHÎncă nu există evaluări
- Diagnostic TestsDocument5 paginiDiagnostic TestsKathleen DimacaliÎncă nu există evaluări
- Nursing Care Plan For Myocardial Infarction NCPDocument8 paginiNursing Care Plan For Myocardial Infarction NCPRhomyrose CampanaÎncă nu există evaluări
- Cues and Objectives Explanation of The Problem Goals and Objectives Interventions Rationale EvaluationDocument4 paginiCues and Objectives Explanation of The Problem Goals and Objectives Interventions Rationale EvaluationShaina Fe RabaneraÎncă nu există evaluări
- N U R S I N G Care Plan For AterosclerosiDocument2 paginiN U R S I N G Care Plan For AterosclerosiRoxy TofyÎncă nu există evaluări
- NCPDocument2 paginiNCPDarien AquinoÎncă nu există evaluări
- Nursing Care Plan: Defining The Assessment Diagnosis Scientific Explanation Objectives Interventions Rationale EvaluationDocument2 paginiNursing Care Plan: Defining The Assessment Diagnosis Scientific Explanation Objectives Interventions Rationale EvaluationLovella Gonzales LimÎncă nu există evaluări
- Acute Pain!!!!!!!!!!!!!!!Document3 paginiAcute Pain!!!!!!!!!!!!!!!ahz_kerian2Încă nu există evaluări
- Angina PectorisDocument22 paginiAngina Pectorismacoy08Încă nu există evaluări
- NCP 3 in ER Module (Bernales, JLE)Document3 paginiNCP 3 in ER Module (Bernales, JLE)Jan Lianne BernalesÎncă nu există evaluări
- NCP - BSN12F - Pumbaya (Module 4)Document3 paginiNCP - BSN12F - Pumbaya (Module 4)Ellah PumbayaÎncă nu există evaluări
- Final Zollinger-Ellison SyndromeDocument9 paginiFinal Zollinger-Ellison SyndromeGLYDEL CORDEROÎncă nu există evaluări
- NCP 2Document2 paginiNCP 2Loreily ShyreenÎncă nu există evaluări
- Nursing Care Plans: Vasovagal Response, Decreasing BP and Heart RateDocument3 paginiNursing Care Plans: Vasovagal Response, Decreasing BP and Heart RateRachelle Ann DomingoÎncă nu există evaluări
- Republic Act 7305Document28 paginiRepublic Act 7305mariejoÎncă nu există evaluări
- ParaphiliasDocument4 paginiParaphiliasmariejoÎncă nu există evaluări
- Calcium ImbalanceDocument12 paginiCalcium ImbalancemariejoÎncă nu există evaluări
- Dyestone Green MX SDS SA-0172-01Document5 paginiDyestone Green MX SDS SA-0172-01gede aris prayoga mahardikaÎncă nu există evaluări
- Cainta Catholic College Cainta, Rizal Senior High SchoolDocument54 paginiCainta Catholic College Cainta, Rizal Senior High SchoolandyÎncă nu există evaluări
- Redacted Letter To Winn Correctional Center, June 10, 2021Document5 paginiRedacted Letter To Winn Correctional Center, June 10, 2021Katie CrolleyÎncă nu există evaluări
- CHN2 Module 5Document2 paginiCHN2 Module 5Nopdy JaronÎncă nu există evaluări
- Allergic Rhinitis and School PerformanceDocument8 paginiAllergic Rhinitis and School PerformanceMahmoud AbdallahÎncă nu există evaluări
- Pemilihan Kerjaya Menurut Teori HollandDocument2 paginiPemilihan Kerjaya Menurut Teori HollandKHAIRUNISAÎncă nu există evaluări
- Cervical Spine ICF ClassificationDocument2 paginiCervical Spine ICF ClassificationKyle DavisÎncă nu există evaluări
- TETRINDocument2 paginiTETRINDr.2020Încă nu există evaluări
- V6 - Health CS VC Collectors 22.08.2023Document92 paginiV6 - Health CS VC Collectors 22.08.2023MdnowfalÎncă nu există evaluări
- Jadbinder Seehra Periodontal Outcomes Associated With Impacted Maxillary Central Incisor and Canine Teeth Following Surgical Exposure and Orthodontic AlignmentDocument15 paginiJadbinder Seehra Periodontal Outcomes Associated With Impacted Maxillary Central Incisor and Canine Teeth Following Surgical Exposure and Orthodontic Alignmentcruzjulio480Încă nu există evaluări
- Lakewood Police Department Return To Work Decision MatrixDocument1 paginăLakewood Police Department Return To Work Decision MatrixMichael_Roberts2019Încă nu există evaluări
- Implant-Supported Fixed Dental Prosthesis With A MicrolockingDocument31 paginiImplant-Supported Fixed Dental Prosthesis With A MicrolockingbalwantÎncă nu există evaluări
- Ieltsfever Academic Reading Practcie Test 50 PDFDocument11 paginiIeltsfever Academic Reading Practcie Test 50 PDFLOÎncă nu există evaluări
- Risk Assessment ExampleDocument3 paginiRisk Assessment Examplecotin006Încă nu există evaluări
- University of Lucknow: AssignmentDocument17 paginiUniversity of Lucknow: AssignmentArpit SrivastavaÎncă nu există evaluări
- October JournalDocument36 paginiOctober Journalrammvr05Încă nu există evaluări
- EpidimologyDocument78 paginiEpidimologyWeji ShÎncă nu există evaluări
- SeminarDocument6 paginiSeminarDoktere WongndesoÎncă nu există evaluări
- Nursing SeatmatrixDocument8 paginiNursing SeatmatrixKanza KaleemÎncă nu există evaluări
- Fourth Quarter Reviewer in Mapeh 7 GENERAL INSTRUCTIONS: Review The Following Questions. The Answer Keys Are Indicated in The LastDocument5 paginiFourth Quarter Reviewer in Mapeh 7 GENERAL INSTRUCTIONS: Review The Following Questions. The Answer Keys Are Indicated in The LastUnibelle Joy LachicaÎncă nu există evaluări
- Causes and Consequences of Occupational Fatigue: Meta-Analysis and Systems ModelDocument13 paginiCauses and Consequences of Occupational Fatigue: Meta-Analysis and Systems ModelLinna SriwaningsiÎncă nu există evaluări
- Nitobond EP : Constructive SolutionsDocument4 paginiNitobond EP : Constructive SolutionsChidi OkoloÎncă nu există evaluări
- Izombie Rules (D20 Modern Variant Rule) : Zombie StatsDocument7 paginiIzombie Rules (D20 Modern Variant Rule) : Zombie StatsJames LewisÎncă nu există evaluări
- Toolkit Part 11Document48 paginiToolkit Part 11tinydaisyÎncă nu există evaluări
- DIR-FLoortime Interested Providers 020311Document2 paginiDIR-FLoortime Interested Providers 020311circlestretchÎncă nu există evaluări
- Turtura ResumeDocument1 paginăTurtura ResumeaturturaÎncă nu există evaluări
- Tired 2. Motivated 3. Excited 4. Scared 5. Angry 6. Happy 7. Disappointed 8. Bored 9. Delighted 10.sadDocument11 paginiTired 2. Motivated 3. Excited 4. Scared 5. Angry 6. Happy 7. Disappointed 8. Bored 9. Delighted 10.sadAnita Zarza BandaÎncă nu există evaluări