Documente Academic
Documente Profesional
Documente Cultură
Nursing Care Plan For Peritonitis NCP
Încărcat de
dericTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Nursing Care Plan For Peritonitis NCP
Încărcat de
dericDrepturi de autor:
Formate disponibile
Student Nurses Community
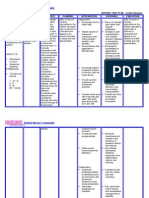
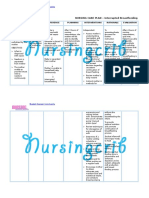
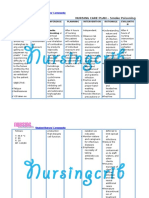
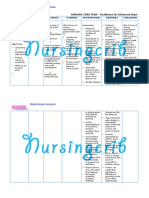
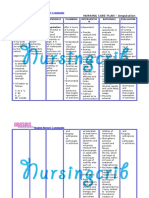
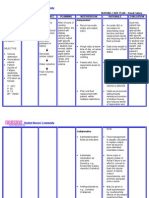
NURSING CARE PLAN Peritonitis
ASSESSMENT
SUBJECTIVE:
Sumasakit ang
tiyan ko at
nasusuko ako
(I've been
experiencing
abdominal pain and
I feel nauseous)
as verbalized by
the patient.
OBJECTIVE:
Dry mucous
membranes
Poor skin
turgor
Weak
peripheral
pulses
V/S taken as
follows
T: 36.5C
P: 49
R: 14
BP: 110/ 80
DIAGNOSIS
INFERENCE
PLANNING
INTERVENTION
Deficient
(mixed) fluid
volume may be
related to fluid
shifts from
extracellular,
intravascular,
and interstitial
compartments
into intestines
and/or
peritoneal
space;
vomiting;
medically
restricted
intake;
nasogastric or
intestinal
aspiration;
fever;
hypermetabolic
state.
Peritonitis is an
acute
inflammation of
the
visceral/parietal
peritoneum and
endothelial lining
of the abdominal
cavity, or
peritoneum.
Peritonitis can be
classified as
primary or
secondary,
localized or
generalized.
When the
peritoneal cavity
is contaminated
by bacteria, the
body initially
produces an
inflammatory
reaction that
walls off a
localized area to
fight the
infection. If this
walling off
process fails, the
inflammation
spreads and
contamination
becomes
massive,
resulting in
After 8 hours of
nursing
interventions, the
Patient will
demonstrate
improved fluid
balance as
evidenced by
adequate urinary
output with
normal specific
gravity, stable
vital signs, moist
mucous
membranes,
good skin turgor,
prompt capillary
refill, and weight
within acceptable
range.
Independent
Monitor vital signs,
noting presence of
hypotension
(including postural
changes),
tachycardia, and
fever. Measure
central venous
pressure (CVP) if
available.
Maintain accurate
intake and output
and correlate with
daily weights.
Include measured
and estimated
losses, such as
with gastric suction,
drains, dressing,
hemovacs,
diaphoresis, and
abdominal girth for
third spacing fluid.
Measure urine
specific gravity.
Observe skin and
RATIONALE
Aids in
evaluating
degree of fluid
deficit,
effectiveness of
fluid
replacement
therapy, and
response to
medications.
Reflects over all
hydration status.
Reflects
hydration status
and changes in
renal function,
which may warn
of developing
acute renal
failure in
response to
EVALUATION
After 8 hours of
nursing
interventions, the
Patient was able
to demonstrate
improved fluid
balance as
evidenced by
adequate urinary
output with
normal specific
gravity, stable
vital signs, moist
mucous
membranes,
good skin turgor,
prompt capillary
refill, and weight
within acceptable
range.
Student Nurses Community
diffuse peritonitis.
mucous membrane
dryness and turgor.
Eliminate noxious
sights or smells
from environment.
Change position
frequently, provide
frequent skin care,
and maintain, dry
wrinkle-free
bedding.
Collaborative
Monitor laboratory
studies.
Maintain NPO
status with NG or
intestinal aspiration.
hypovolemia
and effect of
toxins.
Hypovolemia,
fluid shifts, and
nutritional
deficits
contribute to
skin turgor and
taut edematous
tissues.
Reduces gastric
stimulation and
vomiting
response.
Edematous
tissue with
compromised
circulation is
prone to
breakdown.
Provides
information
about hydration
and organ
function.
Reduces
vomiting caused
by hyperactivity
of bowel;
manages
stomach and
intestinal fluids.
S-ar putea să vă placă și
- Topnotch Radiology For Moonlighters - Sept 2019Document72 paginiTopnotch Radiology For Moonlighters - Sept 2019Cara Marrero IguidÎncă nu există evaluări
- Nursing Care Plan For Risk For Aspiration NCPDocument5 paginiNursing Care Plan For Risk For Aspiration NCPderic100% (8)
- Nursing Care Plan For Liver CirrhosisDocument14 paginiNursing Care Plan For Liver Cirrhosisken93% (75)
- Crohn's DiseaseDocument2 paginiCrohn's Diseasederic100% (11)
- Mental and Emotional Health Powerpoint - Fall2015Document45 paginiMental and Emotional Health Powerpoint - Fall2015api-312719755Încă nu există evaluări
- NCP Cardiogenic ShockDocument3 paginiNCP Cardiogenic ShockTrixia Camporedondo100% (1)
- PeritonitisDocument9 paginiPeritonitismardsz100% (4)
- Nursing Care Plan Hemorrhagic StrokeDocument8 paginiNursing Care Plan Hemorrhagic StrokeJeffrey Dela Cruz50% (4)
- Nursing Care Plan For Liver Cirrhosis NCPDocument14 paginiNursing Care Plan For Liver Cirrhosis NCPderic92% (12)
- Uterine CancerDocument20 paginiUterine Cancerzyrine jhen100% (4)
- Tachycardia NCPDocument2 paginiTachycardia NCPRemita Hutagalung50% (4)
- Nursing Care Plan For Overflow Urinary Incontinence NCPDocument2 paginiNursing Care Plan For Overflow Urinary Incontinence NCPderic71% (7)
- NCP CroupDocument3 paginiNCP Croupaurezea100% (3)
- Nursing Care Plan For Risk For Compromised Human Dignity NCPDocument3 paginiNursing Care Plan For Risk For Compromised Human Dignity NCPderic100% (2)
- NCP Crohn'sDocument2 paginiNCP Crohn'sJanice Marco100% (1)
- Iii. Nursing Care PlansDocument13 paginiIii. Nursing Care PlansLharra Cagulada-Postrano100% (1)
- Assessment Nursing Diagnosis Planning Intervention Evaluation S: Patient Was SeenDocument3 paginiAssessment Nursing Diagnosis Planning Intervention Evaluation S: Patient Was Seenkaren kate ablesÎncă nu există evaluări
- Nursing Care Plan For Interrupted Breastfeeding NCPDocument3 paginiNursing Care Plan For Interrupted Breastfeeding NCPderic88% (8)
- Nursing Care Plan For Multiple Sclerosis NCPDocument2 paginiNursing Care Plan For Multiple Sclerosis NCPderic88% (17)
- Nursing Care Plan For Seizure NCPDocument2 paginiNursing Care Plan For Seizure NCPderic88% (40)
- Monthly Wellness Tip Heat StressDocument1 paginăMonthly Wellness Tip Heat StressbharathaninÎncă nu există evaluări
- Nursing Care Plan For Smoke Poisoning NCPDocument2 paginiNursing Care Plan For Smoke Poisoning NCPderic100% (3)
- Nursing Care Plan For "Glaucoma"Document7 paginiNursing Care Plan For "Glaucoma"jhonroks100% (7)
- Nursing Care Plan For Pneumonia NCPDocument3 paginiNursing Care Plan For Pneumonia NCPderic79% (133)
- Nursing Care Plan (Septick Shock)Document6 paginiNursing Care Plan (Septick Shock)REMILYN ROSE ASUNCION67% (9)
- Nursing Care Plan For Readiness For Enhanced Spiritual Well Being NCPDocument4 paginiNursing Care Plan For Readiness For Enhanced Spiritual Well Being NCPderic83% (6)
- Thyroidectomy NCPDocument3 paginiThyroidectomy NCPKim Enrico Jumarang100% (2)
- Nursing Care Plan For Readiness For Enhanced Sleep NCPDocument4 paginiNursing Care Plan For Readiness For Enhanced Sleep NCPderic100% (2)
- Liver NCPDocument5 paginiLiver NCPMerrill HansÎncă nu există evaluări
- Nursing Care Plan For Peptic Ulcer NCPDocument2 paginiNursing Care Plan For Peptic Ulcer NCPderic85% (46)
- Nursing Care Plan For GlaucomaDocument3 paginiNursing Care Plan For Glaucomaderic79% (28)
- Nursing Care Plan Ineffective Breathing Pattern Hepatic MassDocument2 paginiNursing Care Plan Ineffective Breathing Pattern Hepatic MassRheegell Ellar-Fuertes100% (3)
- Management of Septic Peritonitis Related To Mortality in IBDDocument2 paginiManagement of Septic Peritonitis Related To Mortality in IBDRafif Abdurrahman WijisaksonoÎncă nu există evaluări
- Nursing Care Plan For Neonatal Sepsis NCPDocument3 paginiNursing Care Plan For Neonatal Sepsis NCPderic67% (9)
- Nursing Care PlanDocument3 paginiNursing Care PlanBhie DizonÎncă nu există evaluări
- Nursing Care Plan For HemodialysisDocument2 paginiNursing Care Plan For Hemodialysisderic80% (20)
- Nursing Care Plan For Upper Gastrointestinal Bleeding NCPDocument3 paginiNursing Care Plan For Upper Gastrointestinal Bleeding NCPderic79% (14)
- Liver Cirrhosis NCP 1Document6 paginiLiver Cirrhosis NCP 1Paolo Rafael D EsguerraÎncă nu există evaluări
- NCP Peptic Ulcer DsDocument4 paginiNCP Peptic Ulcer Dsplug0650% (10)
- Assessment Diagnosis Planning Implimentation Rationale ResponseDocument4 paginiAssessment Diagnosis Planning Implimentation Rationale Responsekhate fonteÎncă nu există evaluări
- Nursing Care Plan For Readiness For Enhanced Hope NCPDocument4 paginiNursing Care Plan For Readiness For Enhanced Hope NCPderic100% (6)
- Nursing Care Plan For Ineffective Infant Feeding Pattern NCPDocument3 paginiNursing Care Plan For Ineffective Infant Feeding Pattern NCPderic71% (14)
- Nursing Care Plan For AIDS/HIVDocument3 paginiNursing Care Plan For AIDS/HIVderic81% (16)
- Nursing Care Plan For Rabies NCPDocument3 paginiNursing Care Plan For Rabies NCPderic100% (9)
- NCP StressDocument2 paginiNCP StressWaqas Javed100% (7)
- Preoperative and Post Liver Transplant Nursing Care PlanDocument5 paginiPreoperative and Post Liver Transplant Nursing Care PlanOctoober67% (6)
- Nursing Care Plan For Insufficient Breastmilk NCPDocument2 paginiNursing Care Plan For Insufficient Breastmilk NCPderic100% (17)
- Case: Liver Cirrhosis Assessment:: Nursing InferenceDocument7 paginiCase: Liver Cirrhosis Assessment:: Nursing InferenceLovelyn GanirÎncă nu există evaluări
- Penerapan PMKP RS Arjaty Daud 2022 UPDATEDocument15 paginiPenerapan PMKP RS Arjaty Daud 2022 UPDATERUNI DARYANTI100% (1)
- Nursing Care Plan For AmputationDocument3 paginiNursing Care Plan For Amputationderic80% (25)
- Nursing Care Plan For Disturbed Sleep Pattern NCPDocument3 paginiNursing Care Plan For Disturbed Sleep Pattern NCPderic67% (3)
- Nursing Care Plan For Insomnia NCPDocument2 paginiNursing Care Plan For Insomnia NCPderic83% (23)
- Nursing Care Plan For Myocardial Infarction NCPDocument8 paginiNursing Care Plan For Myocardial Infarction NCPderic87% (15)
- NCP Heart BlockDocument3 paginiNCP Heart BlockEköw Santiago Javier33% (3)
- CP Intestinal Obstruction Nursing Care PlanDocument7 paginiCP Intestinal Obstruction Nursing Care PlanKatherine 'Chingboo' Leonico Laud95% (21)
- Irrigating Cystoclysis Final OutputDocument6 paginiIrrigating Cystoclysis Final OutputNissie Degulacion100% (3)
- Nursing Care Plan For Rape Trauma Syndrome NCPDocument5 paginiNursing Care Plan For Rape Trauma Syndrome NCPderic100% (4)
- NCP GunshotDocument13 paginiNCP GunshotMichael John F. Natividad0% (1)
- Nursing Care Plan For Carbon Monoxide PoisoningDocument3 paginiNursing Care Plan For Carbon Monoxide Poisoningderic73% (11)
- NCP PancreatitisDocument2 paginiNCP PancreatitisJeanelle Generoso100% (1)
- ThesisDocument30 paginiThesisSimran JosanÎncă nu există evaluări
- Prostate Cancer NCPDocument1 paginăProstate Cancer NCPKathleen Dimacali0% (1)
- Myocarditis NCP 2Document8 paginiMyocarditis NCP 2astro_aaron117375% (4)
- OT Relevance RMTDocument12 paginiOT Relevance RMTFredy RamoneÎncă nu există evaluări
- Nursing Students Peritonitis Care PlanDocument2 paginiNursing Students Peritonitis Care PlanJide Manuel100% (1)
- A Case Study On Choledocholithiasis - CompressDocument81 paginiA Case Study On Choledocholithiasis - Compressandreea ndreÎncă nu există evaluări
- 5 Altered Nutrition Less Than Body Requirements Chronic Renal Failure Nursing Care PlansDocument3 pagini5 Altered Nutrition Less Than Body Requirements Chronic Renal Failure Nursing Care Plansjustin_sane40% (5)
- Nursing Care Plan For Post Trauma NCPDocument5 paginiNursing Care Plan For Post Trauma NCPderic82% (11)
- NCP-Esophageal Varices Pleural EffusionDocument6 paginiNCP-Esophageal Varices Pleural Effusiontinatin98933% (3)
- Nursing Care Plan Renal FailureDocument2 paginiNursing Care Plan Renal FailureMark Jason Rabadan100% (1)
- Anatomy and Physiology-Liver CirrhosisDocument2 paginiAnatomy and Physiology-Liver CirrhosisHilmi Ramos100% (3)
- Burns - Fluid Volume, Risk For DeficientDocument3 paginiBurns - Fluid Volume, Risk For Deficientmakyofrancis20Încă nu există evaluări
- NCP (Deficient Fluid VolumeDocument3 paginiNCP (Deficient Fluid VolumeNica RespondoÎncă nu există evaluări
- Preoperative TeachingDocument11 paginiPreoperative TeachingDani ThomasÎncă nu există evaluări
- Nursing Care PlanDocument5 paginiNursing Care PlanAnju Luchmun100% (2)
- Lung Cancer N C P BY BHERU LALDocument2 paginiLung Cancer N C P BY BHERU LALBheru Lal100% (1)
- NCP Leptospirosis - NewDocument5 paginiNCP Leptospirosis - Newglaiza_requintoÎncă nu există evaluări
- Acute Pain NCPDocument2 paginiAcute Pain NCPBobby Valencerina100% (1)
- NCP For RS-HF (Cor PulmonaleDocument5 paginiNCP For RS-HF (Cor PulmonaleMika Saldaña100% (1)
- NCP For FrostbiteDocument2 paginiNCP For FrostbiteRommar RomeroÎncă nu există evaluări
- Abdominal PainDocument2 paginiAbdominal Paindelan7dust78% (18)
- NCP pAlPITATIONSDocument3 paginiNCP pAlPITATIONSHazel PalomaresÎncă nu există evaluări
- Nursing Care Plan For RabiesDocument1 paginăNursing Care Plan For RabiesAngel VillamorÎncă nu există evaluări
- NCP - Patient With Endotracheal TubeDocument1 paginăNCP - Patient With Endotracheal TubeSelwynVillamorPatenteÎncă nu există evaluări
- Ineffective Airway Clearance Related To SinusitisDocument3 paginiIneffective Airway Clearance Related To SinusitisBarbara Detaro71% (7)
- NCP Near DrowningDocument1 paginăNCP Near Drowningchristine louise bernardoÎncă nu există evaluări
- PeritonitisDocument6 paginiPeritonitisDiane ArgoteÎncă nu există evaluări
- Appendicitis: Differential Diagnoses & Workup Treatment & Medication Follow-UpDocument12 paginiAppendicitis: Differential Diagnoses & Workup Treatment & Medication Follow-UpnetonetinÎncă nu există evaluări
- PeritonitissDocument46 paginiPeritonitissNinaÎncă nu există evaluări
- Acute AppendicitisDocument5 paginiAcute AppendicitisPrasetya Ismail PermadiÎncă nu există evaluări
- لقطة شاشة 2022-04-21 في 11.10.40 صDocument55 paginiلقطة شاشة 2022-04-21 في 11.10.40 صEngi KazangyÎncă nu există evaluări
- Pa Tho Physiology of Typhoid Fever and Acute GastroenteritisDocument4 paginiPa Tho Physiology of Typhoid Fever and Acute GastroenteritisJade Fatima D. CaymoÎncă nu există evaluări
- Intra-Abdominal and Pelvic EmergenciesDocument21 paginiIntra-Abdominal and Pelvic Emergenciesqhrn48psvwÎncă nu există evaluări
- Acute Suppurative PeritonitisDocument47 paginiAcute Suppurative PeritonitissanjivdasÎncă nu există evaluări
- Case Report Vella NurfatimahDocument4 paginiCase Report Vella NurfatimahVella NurfatimahÎncă nu există evaluări
- 3 Common Pediatric Surgery ContinuedDocument5 pagini3 Common Pediatric Surgery ContinuedMohamed Al-zichrawyÎncă nu există evaluări
- Nursing Care Plan For Pedia TB Meningitis NCPDocument2 paginiNursing Care Plan For Pedia TB Meningitis NCPderic100% (1)
- Notes: Generally, What Are They?Document10 paginiNotes: Generally, What Are They?Yusril MarhaenÎncă nu există evaluări
- Laws Governing Gerontological Nursing PracticeDocument18 paginiLaws Governing Gerontological Nursing PracticeGlizzle MacaraegÎncă nu există evaluări
- 2010 Bandelow ExtendedDocument16 pagini2010 Bandelow ExtendedRian YupitaÎncă nu există evaluări
- Effects of Cuscuta Chinensis Lam. Versus Fluoxetine For Treatment of Major Depression: A Double-Blind, Randomized Controlled TrialDocument10 paginiEffects of Cuscuta Chinensis Lam. Versus Fluoxetine For Treatment of Major Depression: A Double-Blind, Randomized Controlled TrialBaru Chandrasekhar RaoÎncă nu există evaluări
- 1 s2.0 S1526054219300235 MainDocument4 pagini1 s2.0 S1526054219300235 MainBruno SantosÎncă nu există evaluări
- Approach To Floppy InfantDocument44 paginiApproach To Floppy InfantNavya Hegde100% (2)
- Drugs Used in The Treatment of Congestive Heart FailureDocument18 paginiDrugs Used in The Treatment of Congestive Heart Failurekarina azlia amandaÎncă nu există evaluări
- Categorical and Hypothetical ImperativesDocument4 paginiCategorical and Hypothetical ImperativesKathe KiunisalaÎncă nu există evaluări
- AERGDocument12 paginiAERGsupaidi97Încă nu există evaluări
- WHO Drug Information: Herbal Medicines Regulatory ActionDocument91 paginiWHO Drug Information: Herbal Medicines Regulatory ActionLia PuspitasariÎncă nu există evaluări
- Miron Zhang i-PRF Drug DeliveryDocument17 paginiMiron Zhang i-PRF Drug Deliverygary manningÎncă nu există evaluări
- SOCT Copernicus: OPTOPOL Technology S.ADocument4 paginiSOCT Copernicus: OPTOPOL Technology S.AakhterÎncă nu există evaluări
- Regulation of RespirationDocument21 paginiRegulation of RespirationSheeraz ShahzadÎncă nu există evaluări
- Types: There Is A Range Of, IncludingDocument15 paginiTypes: There Is A Range Of, IncludingBhossneil Betonio LacadenÎncă nu există evaluări
- Assesment and Summary of FindingsDocument3 paginiAssesment and Summary of Findingscami bihagÎncă nu există evaluări
- Bulacan State University College of Nursing City of Malolos, BulacanDocument2 paginiBulacan State University College of Nursing City of Malolos, BulacanVIRGINIA M. SANTOSÎncă nu există evaluări
- Clotting Concept Analysis Diagram and ExplanationDocument2 paginiClotting Concept Analysis Diagram and ExplanationJulius Haynes100% (1)
- 19Document5 pagini19Ira TryÎncă nu există evaluări
- 2021 06 Reference Texts Textes de ReferenceDocument14 pagini2021 06 Reference Texts Textes de Referenceaishwarya desaiÎncă nu există evaluări
- Daftar Isi FormulariumDocument9 paginiDaftar Isi FormulariumNilam atika sariÎncă nu există evaluări
- Cipla - Sheet1Document14 paginiCipla - Sheet1Conflict YTÎncă nu există evaluări
- Donating Corneas: Emma Hart and Alyssa NovelliDocument12 paginiDonating Corneas: Emma Hart and Alyssa NovellisueiannacciÎncă nu există evaluări