Documente Academic
Documente Profesional
Documente Cultură
A Practical Classification of Childhood Hypopigmentation Disorders
Încărcat de
Kerin ArdyDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
A Practical Classification of Childhood Hypopigmentation Disorders
Încărcat de
Kerin ArdyDrepturi de autor:
Formate disponibile
Acta Derm Venereol 2010; 90: 611
MINI-REVIEW
A Practical Classification of Childhood Hypopigmentation Disorders
Hong Liang Tey
National Skin Centre, 1, Mandalay Road, Singapore, Singapore
Hypopigmentation disorders in children can be due to a
wide variety of congenital and acquired diseases. A clinical approach to hypopigmentation disorders based on
the typical age of onset and the extent of lesions is proposed. The disorders are categorized into onset in early and
later childhood, and in each category they are subdivided into localized and generalized pigmentary disorders.
Clinical findings, comprising the sites of involvement,
degree of pigment loss, and associated morphological findings, are used to distinguish the disorders further. This
classification provides a systematic approach to a clinical
condition in which the causes are heterogeneous and histological examination of the skin is rarely diagnostic. Key
words: approach; childhood; pediatric; hypopigmentation;
hypopigmented.
(Accepted October 26, 2009.)
Acta Derm Venereol 2010; 90: 611.
Hong Liang Tey, National Skin Centre, 1, Mandalay Road,
Singapore 308205, Singapore. E-mail: teyhongliang111@
yahoo.com
The colour of the skin is mainly due to melanin and blood
but can be altered in non-physiological conditions such as
carotenemia, drug intake, jaundice and chronic renal failure. Hypopigmentation refers to any form of decreased
pigmentation, whereas hypomelanosis refers specifically
to a decrease in melanin content. Depigmentation, in
contrast to hypopigmentation, describes the almost total
loss of pigmentation, resulting in a whitish appearance
that comes from the underlying dermis.
Hypopigmentation disorders can generally be categorized based on their aetiologies, age of onset, and
extent of involvement. In early childhood, many of
these disorders have a genetic origin and present with
generalized pigmentary dilution. In later childhood,
many of these diseases are acquired and cause localized
hypopigmentation. Other clinical features can aid in
the further differentiation of these disorders, such as
the sites of involvement, degree of pigment loss, and
associated morphological signs. In the clinical approach
to be presented here, the disorders are categorized primarily according to the typical age of onset into early
andlater childhood.
Acta Derm Venereol 90
Onset in early childhood
In this article, disorders that present in early childhood
describe those disorders that occur up to the first 2
years of life. Most of these disorders present at birth
or during infancy and have a genetic basis. Clinically,
these disorders can be divided into those characterized
by generalized hypopigmentation and those causing
localized disease.
Generalized hypopigmentary disorders
Disorders with generalized diffuse pigmentary dilution
are usually due to mutations of genes responsible for
the production of melanin or the processing of melano
somes, and hypopigmentation of the skin and hair is
present. During embryogenesis, progenitor melanoblasts migrate between mesodermal and ectodermal layers to reach their final destinations in the epidermis and
hair follicular bulbs, as well as the inner ear cochlea,
choroids, ciliary body, and iris (1). Therefore, the eyes,
in addition to the skin and hair, can exhibit pigmentary
dilution. In a group of generalized hypopigmentary disorders, hypopigmentation involves the eyes in addition
to the skin and hair, and this group has been typified as
oculocutaneous albinism (Fig. 1).
Oculocutaneous albinism (OCA) is the most common
type of pigmentary dilutional disorder, of which type 2
comprises the majority of the cases. In OCA type 1A, in
which there is complete absence of tyrosinase activity,
there is permanent and complete absence of pigment from
birth. In OCA types 1B, 2, 3, and 4, however, pigment
production may increase over time. In these latter types
of OCA and including HermanskyPudlak and Chediak
Higashi syndromes, the pigmentary dilution may be
subtle, and comparison with family members will be
helpful. This is especially so in fair-skinned races.
Common to all types of OCA, there is reduced visual
acuity and ocular nystagmus (2) and these distinguish
OCA from other forms of congenital hypopigmentation.
The ocular abnormalities are due to misrouting of the
optic nerve and this may result from deficiency of tyrosinase. Tyrosine hydroxylase, in particular, is important
in the proper routing of retinal projections at the optic
chiasm during development (3). Infants who are unable
to fixate or have nystagmus should be sent for a thorough
ocular examination as early intervention is crucial for
2010 The Authors. doi: 10.2340/00015555-0794
Journal Compilation 2010 Acta Dermato-Venereologica. ISSN 0001-5555
Childhood hypopigmentation
melanolysosomal disease, is characterized
by silvery hair, mild hypopigmentation,
and severe central nervous system dysfunEyes, skin
Skin and hair
and hair
ction (6). Its molecular basis is currently
not known.
Oculocutaneous
Inborn errors
Nutritional
Genodermatoses
Menkes syndrome is an X-linked realbinism
of metabolism
deficiencies
cessive multi-systemic disorder due to
Defects in
Defects in
Unknown
Phenylketonuria
Neurologic
inappropriate intracellular copper storage.
Copper
melanin
packaging of
mechanism
defects
production
melanosomes
It is typified by hair shaft abnormalities,
Homocysteinuria
Griscelli and
HermanskyCross
Elejalde
of which pili torti is the most common.
OCA 1-4
Pudlak
syndrome
Selenium
syndromes
syndrome
Histidinaemia
Pigmentary abnormalities consist of
Menkes
lightly pigmented hair and generalized
Prader-Willi &
syndrome
Chediak-Higashi
Angelman
syndrome
or localized hypopigmentation. Progressyndromes
Skeletal
defects
sive central nervous system deterioration
occurs and results in death by 3 years of
EEC
age (7).
syndrome
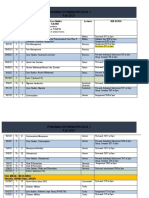
Pigmentary dilution and skeletal deFig. 1. Generalized hypopigmentation with early onset.
fects occur in Ectrodactyly-Ectodermal
dysplasia-Cleft lip/palate (EEC) synvisual development. In addition, hypopigmented babies
drome. The lobster-claw deformities of the hands
should undergo a systemic evaluation to exclude other
and feet and cleft lip and palate enable the syndrome
rarer disorders. For example, the presence of mental retarto be recognized easily. The cutaneous features consist
dation suggests Angelman and PraderWilli syndromes,
of diffuse hypopigmentation and dryness of the skin
an obese baby may have PraderWilli syndrome, bleeding
and hair (8).
diatheses may be a sign of HermanskyPudlak syndrome,
Loss of hair and skin pigmentation due to selenium
immune deficiency points to ChediakHigashi syndrome,
deficiency has been described in children receiving
and structural ocular and neurological abnormalities suglong-term total parenteral nutrition, and repigmentation
gest Cross syndrome.
occurred after selenium supplementation (9). HypopigImpairment of melanin synthesis occurs in certain
mentation of the skin and hair has also been described
diseases of inborn errors of metabolism, such as phenylin severely malnourished infants, and this was attributed
ketonuria, homocystinuria and histidinaemia, which are
to copper deficiency because tyrosinase is a copperdue to the absence or defect in phenylalanine hydroxydependent enzyme. However, as multiple nutritional
lase, cystathionine synthetase, and histidase, respectideficiencies tend to co-exist, the pathogenesis was difvely. These three disorders are transmitted in an autoficult to confirm (10).
somal recessive manner and are associated with mental
In all of the disorders outlined in Fig. 1, the epidermis
retardation and other systemic dysfunction.
generally contains normal numbers of melanocytes and
Some genetic disorders result in pigmentary dilution
histology of the skin is not helpful in differentiating
of the skin and hair, but spare the eyes. The patients
these conditions. The pathophysiological defect of
should be screened for systemic abnormalities and if
hypopigmentation lies either in melanin biosynthesis
neurological defects are present, the differential dior melanosome formation and trafficking. Disorder of
agnoses will include Griscelli, Elejalde and Menkes
melanin biosynthesis can be due to tyrosinase defects
syndromes. Griscelli and Elejalde syndromes are rare,
(occurring in OCA types 1 and 3 and copper deficiency)
autosomal recessive disorders with abnormalities in the
or melanosomal dysfunction (occurring in OCA types
transport of lysosome-related organelles, which include
2 to 4). Abnormalities in the formation, transport, and
melanosomes, platelet-dense bodies and lymphocyte
transfer of melanosomes occur in HermanskyPudlak,
lytic granules (4). Besides cutaneous pigmentatory diluChediakHigashi, and Griscelli syndromes.
tion, the consequence of disrupted melanosome transfer
is silver discoloration of the hair, which can be seen to
Localized hypopigmentary disorders
contain multiple clumps of melanin under light micro
Localized hypopigmentation presenting in early childscopy. In fact, Griscelli, Elejalde and ChediakHigashi
hood can be due to genetic or acquired causes. These
syndromes have been termed silvery hair syndromes
disorders can clinically be categorized based on whether
(5). Apart from pigmentary dilution and neurological
the lesions are depigmented or hypopigmented (Fig. 2).
abnormalities, Griscelli syndrome is also characterized
Piebaldism and vitiligo are both characterized by
by immunological impairment. There are three types of
an absence of epidermal melanocytes and the clinical
the disease known currently, and Elejalde syndrome has
presentation of depigmentation. Unlike vitiligo, lesions
the same clinical features as Griscelli syndrome type
in piebaldism are present at birth and almost always re1. Elejalde syndrome, also known as neuroectodermal
Onset in early childhood
Generalised hypopigmentation
Acta Derm Venereol 90
H. L. Tey
Onset in early childhood
Localised hypopigmentation
Depigmented
Vitiligo
Piebaldism
Waardenburg
syndrome
Tietz syndrome
Hypopigmented
Congenital
Acquired
Naevus
anaemicus
Post-inflammatory
hypopigmentation
Ash-leaf macule
in tuberous
sclerosis
Naevus depigmentosus
& hypomelanosis of Ito
(pigmentary mosaicism)
Fig. 2. Localized hypopigmentation with early onset.
main stable throughout life. There are usually normally
pigmented to hyperpigmented skin as islands within the
depigmented patches and at the lesional borders in piebaldism. The lesions are classically distributed over the
mid-forehead, anterior trunk and mid-extremities, and
they are hardly ever found near the midline on the back
this is due to the embryonic pattern of dorso-ventral migration of melanocytes. The c-KIT and SLUG genes have
been found to be mutated in piebaldism. Dysfunction of
the protein product, a tyrosine kinase transmembrane
receptor on melanocytes, leads to aborted migration and
survival of melanocytes in the skin (11).
In patients presenting with signs of piebaldism, it is
important to check for features of Waardenburg syndrome (WS), which include heterochromia irides and a
broad nasal root. In WS type 1, dystopia canthorum is
present in addition to these features (12). In WS type 2,
unlike the other types of WS, sensorineural deafness is
common. WS type 3 consists of limb defects in addition
to features of type 1 disease and WS type 4 consists of
Hirschsprung disease in addition to features of type 1
disease. It is therefore important to screen for hearing
and musculoskeletal defects and chronic constipation in
an infant with dysmorphic features of WS. In WS, there
is a failure of melanocytes to migrate and survive in the
epidermis, hair follicles, irides and inner ear. Certain
genes are involved in neural crest development and
mutations of these genes in WS type 4 lead to defects
of both melanocyte development in the various organs
and neuronal development in the distal colon (leading to
Hirschsprung disease or congenital aganglionosis). In WS
type 2, the microphthalmia-associated transcription factor
(MITF) gene is mutated and mutation of the same gene
can also lead to Tietz syndrome. Tietz syndrome is clinically distinguishable from WS type 2 in that the former
is characterized by a more severe phenotype, presenting
Acta Derm Venereol 90
with generalized, instead of patchy hypopigmentation and
complete, instead of variable hearing loss (13).
In an infant who presents with a single hypopigmented
macule or patch, the main differential diagnoses are nevus
depigmentosus, an ash leaf macule of tuberous sclerosis, and nevus anemicus. Nevus anemicus is a localized
vascular anomaly in which the vessels are hypersensitive
to catecholamines and it can be distinguished from the
hypomelanotic disorders in a few ways. Using diascopy,
nevus anemicus can be made to blend into the surrounding blanched skin. Nevus anemicus is not accentuated
by Woods lamp, in contrast to lesions which contain less
melanin. The reflex vasodilatory response is also absent
upon application of pressure and heat; scratching a line
across nevus anemicus will not induce erythema in the
lesion and the contrast can be seen in the surrounding
normal skin.
The most common causes of a single hypomelanotic
patch are nevus depigmentosus and an ash-leaf macule of tuberous sclerosis. The diagnosis of tuberous
sclerosis becomes more likely if there are multiple
hypomelanotic macules (only about 10% of patients
with tuberous sclerosis present with a single hypomelanotic lesion) (14) or if the lesion is lance ovate-shape
like ash leaves (rounded at one end and pointed at the
other). Ash-leaf macules are usually the first manifestation of tuberous sclerosis and the other cutaneous features, such asfacial angiofibromas, only start appearing
after the age of 5 years (15). The diagnosis of tuberous
sclerosis may therefore only be apparent when the child
is older. Histologically, the primary finding in both
nevus depigmentosus and ash-leaf spot is a decrease in
epidermal melanin content. Ultrastructural differences
have been described, consisting of a decrease in the
transfer of melanosomes in nevus depigmentosus and a
decreased number of melanosomes in tuberous sclerosis
(16). The differentiation between nevus depigmentosus
andtuberous sclerosis remains clinical.
Hypomelanosis of Ito is a descriptive term for streaks
of hypopigmentation that presents in infancy. It is not a
specific diagnosis and it may occur as a consequence of
several different chromosomal abnormalities that perturb
various genes relevant to skin pigmentation. Although
the characteristic configurations are whorled and linear,
the lesions can be patchy as well. On the other hand,
there is a variant of nevus depigmentosus that consists
of segmental or linear hypopigmentation and this overlap
with hypomelanosis of Ito clinically. Some clinicians
have use the term naevoid linear hypopigmentation to
encompass both conditions (17). Upon the diagnosis of
hypomelanosis of Ito, it is essential to exclude associated
systemic abnormalities, which occurs in about one-third
of children (18), affecting the central nervous and musculoskeletal systems and the heart particularly.
The lesions in hypomelanosis of Ito tend to follow the lines of Blaschko, which are believed to be
Childhood hypopigmentation
pathways of migration and proliferation of epidermal
cells during embryogenesis. The bands of abnormally
pigmented skin represent clones of cells carrying a
mutation in a gene expressed in the skin. Apart from
somatic mutations, mosaicism following the lines
of Blaschko is also seen in chromosomal mosaicism
and functional mosaicism (random X-chromosome
inactivation through lyonization). Clinically, these
disorders present with linear pigmentary changes as
one of their features. The linear or segmental variant
of nevus depigmentosus, hypomelanosis of Ito, and
linear and whorled hyperpigmentation are probably a
phenotypic spectrum of such genetic mosaicism and
have recently been classified under the term pigmentary mosaicism.
The important genodermatoses presenting with
pigmentary dilution and hypopigmented lesions in the
infancy period are listed in Table I. The disorders have
been classified according to their pathogenetic defects
in melanogenesis.
Onset in later childhood
Disorders which typically presents after the first one to
two years of life are included here. Most of these are
acquired in origin. Similar to those presenting in early
childhood, these diseases can be clinically divided into
those characterized by generalized hypopigmentation
and those causing localized disease.
Generalized hypopigmentary disorders
Generalized hypopigmentation presenting in an older
child is uncommon. The causes include vitiligo universalis (presenting with depigmentation), inborn errors
of metabolism (homocysteinuria and histidinaemia),
malnutrition (in particular copper and selenium deficiency), and a delay in the diagnosis of an infancy-
Onset in later childhood
Generalised hypopigmentation
Depigmented
Vitiligo
universalis
Hypopigmented
Inborn errors
of metabolism
Malnutrition
Homocysteinuria
Copper
deficiency
Histidinaemia
Selenium
deficiency
Fig. 3. Generalized hypopigmentation with late onset.
onset pigmentary dilutional disorder. The causes and
approach are presented in Fig. 3.
Homocysteinuria and histidinaemia (also known as histidinuria) usually present during early childhood. Central
nervous system disorders are features of both diseases
and musculoskeletal and cardiovascular abnormalities
are also present in homocysteinuria.
Localized hypopigmentary disorders
Hypopigmentary disorders presenting in later childhood are usually localized. The common causes are
presented in Fig. 4.
Vitiligo is characterized clinically by depigmented
macules and patches that correspond histologically to
a decrease or absence of melanocytes in the epidermis
and, less often, the hair follicles. Its most common age
of onset is 1030 years of age, with a mean age of 20
years. In general, vitiligo can be categorized based on
the distribution into localized, generalized, and universal forms. Localized forms can be segmental, focal, or
Table I. Underlying defects in genodermatoses with pigmentary dilution or hypopigmented lesions (from ref. 19)
Defect
Disease
Proliferation and migration of melanocytes Piebaldism
Waardenburg syndrome (WS)
Production of melanin
Packaging of melanosomes
Transfer of melanosomes
Gene
c-kit
WS1 and WS3: PAX3
WS2A: MITF
WS4: SOX10, EDN3, EDNRB
Tietz syndrome
MITF
Oculocutaneous albinism (OLA)
OCA1: TYR
OCA2: OCA2
OCA3: TYRP1
OCA4: MATP
Prader-Willi and Angelman syndrome OCA2 (gene causing hypopigmentation)
Menkes syndrome
ATP7A
ChediakHigashi syndrome
LYST
HermanskyPudlak syndrome
Type 1: HPS1
Tuberous sclerosis
TSC1, TSC2
Griscelli syndrome
Type 1: MYO5A
Type 2: RAB27A
Type 3: MLPH (or MYO5A F-exon del)
Incontinentia pigmenti
NEMO
Locus
4q12
2q35
3p14.1p12.3
22q13, 20q13.213.3, 13q22
3p14.1p12.3
11q14q21
15q11.2q12
9p23
5p13.3
15q21
Xq13.213.3
1q42.1q42.2
10q23.1
9q33q34, 16p13.3
15q21.1
15q21.1
2q37
Xq28
Acta Derm Venereol 90
10
H. L. Tey
Onset in later childhood
Localised hypopigmentation
Depigmented
Vitiligo
Hypopigmented
Post-inflammatory
hypopigmentation
Lichen sclerosus
and Morphea
Mycosis fungoides
Eczema and
Pityriasis alba
Pityriasis
lichenoides chronica
Lichen striatus
Post infection
Trauma
Fig. 4. Localized hypopigmentation with late onset.
mucosal and generalized forms can be acrofacial or the
vulgaris type. Established generalized and segmental
forms are usually easily recognized as depigmented
patches in their typical distribution and configuration,
respectively. However, focal and mucosal types of vitiligo can be difficult to recognize, especially for early
lesions that are not yet depigmented. The following, if
present, can help support the diagnosis of vitiligo in
ambiguous cases: leucotrichia, Koebner phenomenon,
halo naevi, and associated autoimmune diseases, such
as thyroid abnormalities and alopecia areata.
A common cause of post-inflammatory hypopigmentation in older children is pityriasis alba and this
is typically limited to the face. Post-inflammatory hypopigmentation is also commonly seen in association
with atopic dermatitis as well as with other forms of
eczema. The decrease in pigmentation can be the result
of a disruption in the transfer of melanin to keratinocytes secondary to the inflammatory process or the
application of potent topical corticosteroids. In addition,
post-inflammatory hypopigmentation in children can
also be due to pityriasis lichenoides chronica and lichen
striatus. When an older child presents with widespread
36mm macular hypopigmentation, pityriasis lichenoides chronica should be considered. In lichen striatus,
the hypopigmentation is typically linear following the
lines of Blaschko and multiple small, flat-topped papules may be seen. Post-infectious hypopigmentation can
result from superficial cutaneous infections as well as
childhood viral exanthems and varicella. Post-traumatic
hypopigmentation is also not uncommon in children due
to the frequent superficial injuries they sustain.
If the hypopigmented lesions are associated with an
atrophic epidermal surface, lichen sclerosus, morphea
and the hypopigmented variant of mycosis fungoides are
to be considered. Lichen sclerosus is a pruritic chronic
inflammatory dermatosis that results in hypopigmented
to depigmented porcelain white plaques, which are asActa Derm Venereol 90
sociated with epidermal atrophy and dermal induration.
Up to 15% of cases occur in children, and the lesions
in the majority of these cases occur at the vulva with
absence of extragenital manifestations. Possible pathogenetic mechanisms in the development of this leukoderma include decreased melanin production, blocked
transfer of melanosomes to keratinocytes, and loss of
melanocytes (20). Lichen sclerosus and morphea have
been considered to be closely related by many authors,
but this remains controversial.
Hypopigmentation is not uncommonly seen in lesions
of localized scleroderma (morphea) and systemic sclerosis. The lesions may mimic vitiligo and the clues to
the diagnosis of scleroderma include the presence of
perifollicular hyperpigmentation (forming a salt and
pepper dyschromatosis) and induration of the dermis.
The epidermal melanocytes in the interfollicular regions
disappear, but those in the near vicinity of hair follicles
are retained. This is in contrast to vitiligo in which melanocytes in both regions are affected. In re-pigmenting
vitiligo, re-pigmentation typically starts in the perifollicular region, and differentiating it from scleroderma
can sometimes be difficult.
The hypopigmented variant of mycosis fungoides (MF)
is a rare condition in childhood or adolescence (21), but
this variant seems to be more frequent in children compared to other types of MF (22). This condition should be
considered if there are scattered irregular hypopigmented
patches on non-sun exposed areas of the body and one
should search for typical patch, plaque and tumour lesions
of MF, which may be present concurrently. Histologically,
epidermotropism of atypical lymphocytes may be seen
together with a decrease or absence of epidermal melanin
and pigmentary incontinence.
Investigations
Investigations are dependent on the diagnoses suspected. In congenital hypopigmentary disorders, karyotyping and molecular genetic analysis of the skin and
blood may be considered, especially when the child
has associated developmental delay or structural abnormalities. In conditions which exhibit mosaicism, skin
biopsy plays a more important role in the diagnosis and
blood tests are of limited use. However, the advanced
molecular techniques required for diagnosis of these
congenital disorders are not widely available. Biopsy
of hypopigmented lesions for histology in general is
rarely diagnostic, but this is important in acquired
disorders where inflammatory disorders or mycosis
fungoides is suspected.
Management
In general, treatment for many hypopigmented disorders is limited, especially those which are congenital
Childhood hypopigmentation
in origin. Hypopigmented diseases with an associated
inflammatory component may be treated with topical
corticosteroids and calcineurin inhibitors when lesions
are limited and with phototherapy when lesions are
widespread and the child is older. Autologous grafting
of cultured and non-cultured melanocytes has been
used successfully to treat stable vitiligo and piebaldism (23).
The importance of sun protection, including the use of
a broad-spectrum sunscreen on hypopigmented lesions,
should be emphasized to patients and parents. Hypopigmented lesions are more susceptible to sun damage and
the lesions will be more obvious with the differential
tanning response compared with the surrounding normal
skin. In addition, Koebner phenomenon may arise in
lesions of vitiligo.
Cosmetic cover-ups for camouflage may be the only
option in some hypopigmented disorders. Topical stains
and tanning products may be used on the lesions to
decrease the colour disparity with the normal skin, and
most of these products contain dihydroxyacetone as the
active ingredient.
The psychosocial aspect of the patient is an important
integral part of management. This is particularly so in
schoolchildren, when the hypopigmentary disorder can
be the source of significant embarrassment and psychological trauma to the developing child. Co-operation
and regular communication between the physician,
parents and school is essential, and enrolling the help of
counsellors and child psychiatrists should be instituted
early when appropriate.
Conclusion
Hypopigmentation disorders in children can be due to
a wide variety of congenital and acquired diseases. A
clinical approach to hypopigmentation disorders based
on the typical age of onset of disease and the extent of
the lesions is presented here. Further distinction of the
disorders is dependent on the clinical findings, comprising the sites of involvement, degree of pigment loss
and associated morphological findings. A systematic
approach will be useful for this clinical condition, the
causes of which causes are heterogeneous, and histological examination of the skin is often non-diagnostic.
The author declares no conflict of interest.
References
1. Holbrook KA, Underwood RA, Vogel AM, Gown AM,
Kimball H. The appearance, density and distribution of
melanocytes in human embryonic and fetal skin revealed
by the anti-melanoma monoclonal antibody, HMB-45. Anat
Embryol (Berl)1989; 180: 443.
2. Hornyak TJ. Albinism and other genetic disorders of pig-
11
mentation. In: Wolff K, Goldsmith LA, Katz SI, Gilchrest
BA, Paller AS, Leffell DJ, editors. Fitzpatricks dermatology in general medicine, 7th edn. New York: McGraw-Hill;
2008, p. 609.
3. Lavado A, Jeffrey G, Tovar V, de la Villa P, Montoliu L.
Ectopic expression of tyrosine hydroxylase in the pigmented epithelium rescues the retinal abnormalities and visual
function common in albinos in the absence of melanin. J
Neurochem 2006; 96: 12011211.
4. DellAngelica EC, Mullins C, Caplan S, Bonifacino JS.
Lysosome-related organelles. FASEB J2000:14: 1265.
5. Van Den Bossche K, Naeyaert JM, Lambert J. The quest for
the mechanism of melanin transfer. Traffic2006; 7: 769.
6. Cahali JB, Fernandez SA, Oliveira ZN, Machado MC,
Valente NS, Sotto MN. Elejalde syndrome: report of a
case and review of the literature. Pediatr Dermatol2004;
21: 479.
7. Kaler SG, Holmes CS, Goldstein DS, Tang J, Godwin SC,
Donsante A, et al. Neonatal diagnosis and treatment of
Menkes disease. N Engl J Med 2008; 358: 605614.
8. Buss PW, Hughes HE, Clarke A. Twenty-four cases of the
EEC syndrome: clinical presentation and management. J
Med Genet 1995; 32: 716723.
9. Vinton NE, Dahlstrom KA, Strobel CT, Ament ME. Macro
cytosis and pseudoalbinism: Manifestations of selenium
deficiency. J Pediatr1987; 111: 711717.
10. Olivares M, Uauy R. Copper as an essential nutrient. Am J
Clin Nutr1996; 63: 791S.
11. Spritz RA. The molecular basis of human piebaldism. Pigment Cell Res 1992; 5: 340343.
12. Read AP, Newton VE. Waardenburg syndrome. J Med Genet
1997; 34: 656665.
13. Tietz W. A syndrome of deaf-mutism associated with albinism showing dominant autosomal inheritance. Am J Hum
Genet 1963: 15: 259264.
14. Ortonne JP, Mosher DB, Fitzpatrick TB. Vitiligo and
other hypomelanoses of hair and skin. New York: Plenum
Medical; 1983.
15. Bolognia JL. A clinical approach to leukoderma. Int J Dermatol 1999; 38: 568572.
16. Bolognia JL, Pawelek JM. Biology of hypopigmentation.
J Am Acad Dermatol 1988; 19: 217225.
17. Ortonne JP. Vitiligo and other disorders of hypopigmentation. In: Bolognia JL, Jorizzo JL, Rapini RP, editors.
Dermatology, 2nd edn. Philadelphia: Mosby Elsevier;
2008, p. 928.
18. Nehal KS, PeBenito R, Orlow SJ. Analysis of 54 cases of
hypopigmentation and hyperpigmentation along the lines
of Blaschko. Arch Dermatol 1996; 132: 11671170.
19. Online Mendelian Inheritance in Man. Available at: http://
www.ncbi.nlm.nih.gov/sites/entrez. Assecces Dec 9, 2009.
20. Lapeere H, Boone B, Schepper SD. Hypomelanoses and
hypermelanoses. In: Wolff K, Goldsmith LA, Katz SI,
Gilchrest BA, Paller AS, Leffell DJ, editors. Fitzpatricks
dermatology in general medicine, 7th edn. New York:
McGraw-Hill; 2008, p. 629.
21. Neuhaus IM, Ramos-Caro FA, Hassanein AM. Hypopigmented mycosis fungoides in childhood and adolescence.
Pediatr Dermatol 2000; 17: 403406.
22. Ardig M, Borroni G, Muscardin L, Kerl H, Cerroni L.
Hypopigmented mycosis fungoides in Caucasian patients:
a clinicopathologic study of 7 cases. J Am Acad Dermatol
2003; 49: 264270.
23. Bondanza S, Bellini M, Roversi G. Piebald trait: implication of kit mutation on in vitro melanocyte survival and on
the clinical application of cultured epidermal autografts. J
Invest Dermatol 2007; 127: 676686.
Acta Derm Venereol 90
S-ar putea să vă placă și
- Comparison of Angiotensin Converting Enzyme (Ace) Inhibitors Drug Approximate Dose Equivalence Maximum Daily Dose (Mg/day) Once Daily DosingDocument1 paginăComparison of Angiotensin Converting Enzyme (Ace) Inhibitors Drug Approximate Dose Equivalence Maximum Daily Dose (Mg/day) Once Daily DosingKerin ArdyÎncă nu există evaluări
- 10Document7 pagini10Kerin ArdyÎncă nu există evaluări
- HB in Cardio PDFDocument5 paginiHB in Cardio PDFKerin ArdyÎncă nu există evaluări
- Trombocytosis Essential PDFDocument5 paginiTrombocytosis Essential PDFKerin ArdyÎncă nu există evaluări
- Ferritin TrendsDocument4 paginiFerritin TrendsKerin ArdyÎncă nu există evaluări
- Management and Outcomes For Patients With TTP: Analysis of 100 Cases at A Single InstitutionDocument6 paginiManagement and Outcomes For Patients With TTP: Analysis of 100 Cases at A Single InstitutionBilly Shan LastKagerooboroÎncă nu există evaluări
- Trombocytosis Essential PDFDocument5 paginiTrombocytosis Essential PDFKerin ArdyÎncă nu există evaluări
- Essential Trombocytosis EssentialDocument4 paginiEssential Trombocytosis EssentialKerin ArdyÎncă nu există evaluări
- Pregnancy Outcomes in Women with ThalassemiaDocument3 paginiPregnancy Outcomes in Women with ThalassemiaKerin ArdyÎncă nu există evaluări
- 631927Document8 pagini631927Kerin ArdyÎncă nu există evaluări
- Pregnancy Outcomes in Women with ThalassemiaDocument3 paginiPregnancy Outcomes in Women with ThalassemiaKerin ArdyÎncă nu există evaluări
- Vitiligo in ChildrenDocument4 paginiVitiligo in ChildrenKerin ArdyÎncă nu există evaluări
- Ferritin TrendsDocument4 paginiFerritin TrendsKerin ArdyÎncă nu există evaluări
- HB in Cardio PDFDocument5 paginiHB in Cardio PDFKerin ArdyÎncă nu există evaluări
- 8261 23271 1 PBDocument8 pagini8261 23271 1 PBKerin ArdyÎncă nu există evaluări
- Superoxide Dismutase Activity Colorimetric Assay Kit Ab65354Document3 paginiSuperoxide Dismutase Activity Colorimetric Assay Kit Ab65354Kerin ArdyÎncă nu există evaluări
- 10.1016@S0190 9622 (81) 80205 8Document6 pagini10.1016@S0190 9622 (81) 80205 8Kerin ArdyÎncă nu există evaluări
- Essential Trombocytosis EssentialDocument4 paginiEssential Trombocytosis EssentialKerin ArdyÎncă nu există evaluări
- 28 14Document10 pagini28 14Kerin ArdyÎncă nu există evaluări
- Ni Hms 600206Document13 paginiNi Hms 600206Kerin ArdyÎncă nu există evaluări
- HLA-C Expression Pattern Differences Between Psoriasis and EczemaDocument7 paginiHLA-C Expression Pattern Differences Between Psoriasis and EczemaKerin ArdyÎncă nu există evaluări
- Ni Hms 600206Document13 paginiNi Hms 600206Kerin ArdyÎncă nu există evaluări
- HLA-Cw6 and The Genetic Predisposition To Psoriasis: A Meta-Analysis of Published Serologic StudiesDocument3 paginiHLA-Cw6 and The Genetic Predisposition To Psoriasis: A Meta-Analysis of Published Serologic StudiesKerin ArdyÎncă nu există evaluări
- Human Papillomavirus-Associated Cancers in Patients With Human Immunodeficiency Virus Infection and Acquired Immunodeficiency SyndromeDocument11 paginiHuman Papillomavirus-Associated Cancers in Patients With Human Immunodeficiency Virus Infection and Acquired Immunodeficiency SyndromeKerin ArdyÎncă nu există evaluări
- Hum. Mol. Genet. 2000 Asumalahti 1533 42Document10 paginiHum. Mol. Genet. 2000 Asumalahti 1533 42Kerin ArdyÎncă nu există evaluări
- 1089 FullDocument2 pagini1089 FullKerin ArdyÎncă nu există evaluări
- The Epidemiology of HPVDocument9 paginiThe Epidemiology of HPVMG's Fhya Part IIÎncă nu există evaluări
- Molecular Dissection of Psoriasis: Integrating Genetics and BiologyDocument14 paginiMolecular Dissection of Psoriasis: Integrating Genetics and BiologyKerin ArdyÎncă nu există evaluări
- EScholarship UC Item 8r48b2j2Document3 paginiEScholarship UC Item 8r48b2j2Kerin ArdyÎncă nu există evaluări
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (119)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Inflammatory Bowel DiseaseDocument25 paginiInflammatory Bowel DiseaseAndrew WdsmithÎncă nu există evaluări
- Aloe JuiceDocument12 paginiAloe JuiceAloe JuiceÎncă nu există evaluări
- Tobler - MWO Raum Und Zeit Final - English - FinalDocument6 paginiTobler - MWO Raum Und Zeit Final - English - Finalheinz_toblerÎncă nu există evaluări
- Basic Dharmafect ProtocolDocument4 paginiBasic Dharmafect ProtocolXimenaBandaÎncă nu există evaluări
- Sign Symptoms Deficiency QuestionnaireDocument17 paginiSign Symptoms Deficiency Questionnairepizes6884Încă nu există evaluări
- Course Work EssayDocument12 paginiCourse Work EssayKanza NajamÎncă nu există evaluări
- SMK Kesehatan Ciamis Ujian Kenaikan Kelas SoalDocument5 paginiSMK Kesehatan Ciamis Ujian Kenaikan Kelas Soalsmk kesehatan ciamisÎncă nu există evaluări
- Word HNPDocument14 paginiWord HNPALan ButukÎncă nu există evaluări
- 07 PtosisDocument25 pagini07 Ptosisbc22yÎncă nu există evaluări
- CT BR SureSubtraction CT DSADocument11 paginiCT BR SureSubtraction CT DSAWALVRadiologyÎncă nu există evaluări
- Genetic Attribution For Schizophrenia, Depression, and Skin Cancer: Impact On Social DistanceDocument7 paginiGenetic Attribution For Schizophrenia, Depression, and Skin Cancer: Impact On Social DistancenigoÎncă nu există evaluări
- A Brief History of TobaccoDocument10 paginiA Brief History of Tobaccoapi-263857514Încă nu există evaluări
- S807 Mini Review v4Document37 paginiS807 Mini Review v4Daen de LeonÎncă nu există evaluări
- Annexure - A Incident Assessment Risk MatrixDocument4 paginiAnnexure - A Incident Assessment Risk MatrixDilshad aliÎncă nu există evaluări
- Clinical Summary Guide 05Document2 paginiClinical Summary Guide 05Diarti_PMIKÎncă nu există evaluări
- Buter t1 Case Studies CalendarDocument4 paginiButer t1 Case Studies Calendarapi-602288180Încă nu există evaluări
- All You Need Know About Mouth CancerDocument7 paginiAll You Need Know About Mouth CancerKaknika KapoorÎncă nu există evaluări
- Kuretase Case Report 2Document3 paginiKuretase Case Report 2Lydia AmaliaÎncă nu există evaluări
- CeramFab Inc. & WYG Refractories SuitDocument27 paginiCeramFab Inc. & WYG Refractories SuitBenjamin DuerÎncă nu există evaluări
- 1 Repeat Breeding in BovineDocument20 pagini1 Repeat Breeding in BovineYousef HussienÎncă nu există evaluări
- Makalah Analytical ExpotitionDocument12 paginiMakalah Analytical Expotitionsendal jepit100% (2)
- Imaging Acute Abdomen DR - Rivani Kurniawan FixDocument86 paginiImaging Acute Abdomen DR - Rivani Kurniawan FixRivani KurniawanÎncă nu există evaluări
- DR - Sreedhar Tirunagari BAMS, MD, MBA, PHD, Diploma in Public Health AYUSH ProfileDocument11 paginiDR - Sreedhar Tirunagari BAMS, MD, MBA, PHD, Diploma in Public Health AYUSH ProfileDr Sreedhar TirunagariÎncă nu există evaluări
- Nails As Indicators of Health StatusDocument21 paginiNails As Indicators of Health Statusnur wahidÎncă nu există evaluări
- Kerala Uiversity Bhms PapersDocument31 paginiKerala Uiversity Bhms PapersKarthikÎncă nu există evaluări
- Health Assessment: 2 Data Collected During Assessment (Cues)Document24 paginiHealth Assessment: 2 Data Collected During Assessment (Cues)Mabes50% (2)
- Pathophysiology of Myoma and EndometriosisDocument15 paginiPathophysiology of Myoma and EndometriosisEarle Jimenez Niervo RNÎncă nu există evaluări
- Gestational Trophoblastic DiseaseDocument40 paginiGestational Trophoblastic DiseaseAayupta Mohanty100% (2)
- Pdhpe Assessment Task Term 1 Drug Use in AdolescentsDocument10 paginiPdhpe Assessment Task Term 1 Drug Use in Adolescentsapi-463236687100% (2)
- Cleaning and Sanitizing Methods PDFDocument21 paginiCleaning and Sanitizing Methods PDFLinnuha UlinÎncă nu există evaluări