Documente Academic
Documente Profesional
Documente Cultură
CCRN Cardiac
Încărcat de
MikeDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
CCRN Cardiac
Încărcat de
MikeDrepturi de autor:
Formate disponibile
4/6/2013
Cardiac Blood Flow
Beth Torres, PhD, RN, CCRN
CJW Medical Center
Events during Diastole
Events during Systole
Remember:
The cardiac muscle gets its perfusion during diastole.
Perfusion is determined by coronary perfusion pressure
Coronary Perfusion Pressure = Diastolic BP PCWP
3
Normal: 60 -80 mmHg
During systole the cardiac muscle has to overcome
the pressures ahead of each chamber:
The right ventricle meets low to no pressure in the lungs.
The left ventricle must overcome the diastolic pressure in the
4
aorta.
Compensation for Decreased Cardiac Output
Hemodynamics
Cardiac Output = HR x Stroke Volume (SV)
cardiac output heart rate.
Heart rate is controlled by stimulation of
both the sympathetic and
parasympathetic nervous system
Heart Rate
Normal Cardiac Output:
4-8liters / minute
Preload
Afterload
Cardiac Output
Stroke Volume
Contractility
Muscle Synchrony
5
4/6/2013
Stroke Volume (SV)
Preload
The force on the ventricle during relaxation (diastole)
Primary determinant is the volume of blood filling the
ventricle
Right Ventricle = RVEDP (Right heart preload):
Right Atrial Pressure (RAP); CVP
Normal values: 2-6mmHg
Stroke Volume- the amount of volume ejected
by the ventricle with each systolic contraction
OR, amount of blood ejected by the heart with
each beat
Normal: 60-130ml
SV = (CO/HR) x 1000
Left Ventricle = LVEDP (Left heart preload):
PCWP, PAWP, or PAOP
Pulmonary Artery Diastolic (PAD)
Left Atrial Pressure (LAP)
Normal values: 8-12mmHg
Contractility
Afterload
Defined as the squeezing force generated by the
ventricles.
Afterloadthe ventricular force or pressure
required to overcome impedance to ejection.
As impedance , ejection velocity and SV ,
while ventricular workload & O2 consumption
Refers to both the pressures of this ejection and the
amount of blood ejected.
Manipulate with inotropic drugs
Systemic vascular resistance (SVR): Left
Normal SVR: 900-1400 dynes /sec/cm-5
Best global measure is CO
Pulmonary vascular resistance (PVR): Right
Normal PVR: 50-250 dynes /sec/cm-5
Normal ejection fraction is 50 70 %
9
Cardiac Index
10
Supply
Cardiac Indexa more precise expression of CO,
which takes into account the patients size
Normal CI = 2.5-4.2 L/min
CI < 2.0 is considered cardiogenic shock
1.8-2.2 is low perfusion
Calculate:
CI =
&
Demand
Coronary artery patency
Diastolic filling time
Diastolic pressure
Hemoglobin
Arterial oxygen saturation
Oxygen extraction by the
tissue
Heart rate
Preload
Afterload
Contractility
Oxygen Demand
Oxygen Supply
CO
BSA
11
Heart
12
4/6/2013
Factors of SvO2 & ScvO2
SVO2
SVO2 amount of oxygen in the mixed
venous blood in the pulmonary artery
Normal SVO2: 70-75% (range 60-80%)
An estimate of the amount of oxygen
returning to the cardiopulmonary circulation
Reflects the patients ability to balance O2
supply and demand at the tissue level
SaO2
O2 Tissue
Consumption
CO
Hgb
13
Oxygen Delivery
Question
SvO2 = 75%
SaO2 = 100%
Venous
Return
Oxygen
Consumption
14
25%
Arterial
Oxygen
Delivery
Which of the following is a normal
compensatory response to a decrease in
cardiac output?
a. Increased oxygen delivery
b. Decreased oxygen consumption
c. Increased oxygen extraction
d. Decreased serum lactate
The Cell
15
Cardiac Assessment
16
Arterial Waveform
Hemodynamic Monitoring
Systolic Ejection (A)
Peak of waveform
Normal 90-140
ECG Interpretation
Diastole (C)
Lowest portion of waveform
Normal 60-90
Dicrotic Notch (B)
Closure of Aortic valve
Heart Sounds
17
A
B
C
18
4/6/2013
Review: Right Atrial Waveform
Peripheral Arterial Waveform
The PA catheter is threaded manually to the
right atrium. A continuous pressure reading
will demonstrate a CVP /RA waveform
Normal RA:
2-6 mmHG
19
Preload
What Decreases:
Hypovolemia
Position Change
Vasodilation
Right Heart Damage
Atrial Arrhythmias
Pericardial Effusion
20
CVP waveform
Pressure measurement is taken from
What Increases:
the a waveform (mean) at endexpiration
Normal RA/CVP: 2-6 mmHg
Vasoconstriction
fluid volume
ventricular filling
time
Bradycardia
PEEP
Tension
Pneumothorax
21
22
Pulmonary Artery Waveform
Right Ventricular Waveform
As the PA catheter floats through the pulmonic valve and
The RV is very irritable and ectopy is a potential
complication during PA catheter insertion
Watch the monitor closely for Ventricular
Tachycardia
into pulmonary circulation, the pulmonary systolic pressure
remains similar to RV systolic pressure
The catheter should stay here during continuous
monitoring.
Normal PA:
Sys: 20-30 mmHg
Dia: 5-10
Mean: 10-20
Normal RV:
Sys: 15-30
Dia: 2-6 mmHG
23
24
4/6/2013
Phlebostatic axis
Pulmonary Capillary Wedge Pressure
Advance until it becomes lodged in a
pulmonary artery slightly smaller at
than the inflated balloon.
No blood flows distal to the catheter
tip.
This pressure, the pulmonary artery
occlusion pressure (POAP), reflects
LV pressure when the mitral valve
is open.
Resembles CVP waveform. The a
wave falls later in the T-P cycle.
Head of the bed can range from flat to 60 degrees
PA pressures may be significantly different in patients
Normal PCWP:
4 12 mmHG
in a lateral position.
Allow 5 minutes for stabilization after changing the
patients position
The PCWP should be 1-4 mmHG
lower than the PAD.
IT SHOULD NEVER BE HIGHER!
25
26
Technical Factor:
Mechanical Ventilation
Technical Factors:
Effect of Patient Respirations
If the patient is on a mechanical ventilator, the
positive pressure pushes up the PA tracing.
Ventilator Valleys
A PEEP > 10 will artificially elevate PA pressures
If patient is breathing spontaneously, the negative
pressure pulls down the PA tracing. Spontaneous
sky
The most accurate reading is obtained at respiratory
end expiration.
27
Technical Factor:
Spontaneous Respirations
28
Afterload
Normal SVR = 900-1400 dynes/sec/cm3
SVR = MAP-CVP x 80
CO
MAP = systolic BP + (2) diastolic BP
3
Example:
29
BP = 120/80 (93)
CVP = 5
CO = 5
SVR = [(93 5) / 5] x 80 = 1406
30
4/6/2013
ECG Monitoring
Pulmonary Vascular Resistance (PVR)
Pulmonary Vascular Resistance (PVR)
Treatment of Significant Arrhythmias
reflects blood flow through the pulmonary
circulation
The resistance is influenced by the
pulmonary capillaries & arteries
Normal PVR = 50-250 dynes/sec/cm
PVR = MPAP-PCWP x 80
CO
31
Conduction System
32
Refractory Period
33
Premature Ventricular Contractions
KEY CONCEPT: An electrical stimulus landing on
the T wave, may cause disorganized ventricular
contractions OR VENTRICULAR FIBRILLATION34
Question
The cardiac monitor shows the rhythm below
for your patient. Which of the following
medications might the physician order?
The complexes have a QRS > .12 seconds.
Significance:
PVCs can occur in healthy persons with normal hearts and no
apparent cause.
Patients can be asymptomatic or feel racing heart / skipped
beats.
Frequent PVCs increase risk of fatal arrhythmias x 5.
Treat: More than 6/min, multi-focal, R on T configuration
35
a. Atropine
b. Adenocard
c. Cardizem
d. Amiodarone
36
4/6/2013
Amiodarone
A patient with which of the following is at
greatest risk for torsades de pointes?
Dosage:
Non-VT/V.fib: 150 mg IV over 10 min.
Pulseless VT/V.fib: 300mg IV bolus
a. Depressed ST segment
b. Tall, tented T waves
Adverse effects:
Hypotension and bradycardia are common
during initial bolus.
May be prevented by slowing the rate of
infusion.
c.
Prolonged QT interval
d. u-wave
37
Second Line Drug: Lidocaine
38
Too Fast
Administration:
Bolus: 1.0-1.5 mg/kg IVP; may repeat in 5-10
minutes to max of 3mg/kg
Infusion: 1-4 mg/min
Does not prolong QT
Adverse effects:
Confusion (most common), seizures,
tremors.
39
Sinus Tachycardia
40
Supraventricular Tachycardia
Rate: 100-150 bpm
Significance:
If very fast, the heart cannot refill & results
in CO
This tachycardia originates above the ventricles, but
below the SA node.
Characteristics:
Rate: Rapid! Usually 160-250. May start / stop abruptly.
QRS is normal looking.
No bizarre, early, or late beats.
TREAT THE CAUSE!
Too fast to see a P wave.
Significance:
Must treat if prolonged
41
42
4/6/2013
Atrial Flutter
SVT Treatment
Significance:
Consider this a hazardous rhythm because it can
suddenly change to a rapid ventricular response.
Try VAGAL maneuvers.
If not effective, administer:
ADENOSINE
Indicated for stable SVT
unresponsive to vagal maneuvers.
Dose: 6 mg IV PUSH
12 mg IV PUSH
12 mg IV PUSH
If patient is stable, no initial treatment.
If ventricular rate is rapid, treatment is required.
Adenosine depresses sinus & AV node activity.
HALF LIFE: 10 seconds
Not effective in ventricular rhythms.
43
44
Atrial Fibrillation
Question
R-R interval is always irregular
Significance:
If stable or chronic may be tolerated.
If patient has symptoms, treatment will be
required.
Consider hazardous because ventricular rate
can suddenly .
Also lose atrial kick, which is 20% of the CO
A 69-year-old patient presents to the ED with
complaints of palpitations and irregular heart
beats for the last three of days. The cardiac
monitor shows atrial fibrillation, a heart rate of
136 beats/min. His blood pressure is 124/76 mm
Hg. Which of the following medications would
the physician likely order?
a.
b.
c.
d.
Lidocaine
Cardizem
Corvert
Adenocard
45
46
To Control Rate,
Use Selective - Blockers
Irregular Narrow Complex
Tachycardia: Control of Rate
Non-Selective:
Propranolol (Inderal)
Nadolol (Corgard)
Rate can be controlled by:
Selective agents:
Beta Blockers
Calcium Channel Blockers
Amiodarone *
Atenolol (Tenormin)
Betaxolol (Zebeta)
Metoprolol (Lopressor)
Vasodilatory, Non-selective
Labetalol (Normodyne)
*Not considered a first line
agent for narrow complex
tachycardias
Carvedilol (Coreg)
Shortest half-life:
Esmolol
47
48
4/6/2013
Ventricular Tachycardia
To Control Rate:
Use Calcium Channel Blockers
Wide & bizarre QRS (> .12 sec)
Significance:
Slows AV node conduction & prolongs AV
nodal refractoriness
Treatment is REQUIRED
Pulse or NO Pulse?
Pulse & STABLE? Use AMIODARONE
Pulse & UNSTABLE
ELECTRICAL CARDIOVERSION
Example: Diltiazem
Do not use in:
Drug-induced tachycardia
Heart blocks
Concurrent use of Beta blockers.
49
Question
50
Electrical Cardioversion
The nurse should perform which of the
following interventions for a patient
with chest pain, hypotension, and
tachycardia at a rate of 180 beats/min?
a. Administer amiodarone 150mg IV over 10
min
b. Administer adenosine 6 mg rapid IVP
c. Perform synchronized cardioversion
d. Defibrillate with 300 joules
Immediate electrical cardioversion is indicated
for a patient with serious signs & symptoms
related to tachycardia.
51
Synchronized Cardioversion:
Energy Selection
52
Synchronized Cardioversion:
Energy Selection
If the rhythm does not change, recharge to 200 joules
& repeat
Start with 100 joules.
Repeat with 300 joules & 360 joules, if needed.
Complications include:
Deterioration into ventricular fibrillation
Embolization of a thrombus
Push the Synch button!
53
54
4/6/2013
Synchronized Cardioversion:
Pre-Medication
Too Slow
For awake, alert patients who are hemodynamically
stable, pre-medicate with both a sedative and a
analgesic
Sedatives
Diazepam
Midazolam
Etomidate
Analgesics
Fentanyl
Morphine
Merperidine
Watch for apnea &
hypoventilation after
sedation.
Frequent vital signs are
required before
& after cardioversion
55
3Heart Block
Sinus Bradycardia
Characteristics:
HR > 60
All intervals within
normal limits
except rate
56
Significance:
PREPARE TO PACE!
May be normal in
New guidelines:
chronotropic drips
healthy, young
patient.
Treat symptomatic
bradycardias!
57
58
Temporary Pacemakers
Symptomatic Bradycardia
Treat Bradycardia with BRADE
Use an external generator. 3 types:
Atropine: 0.5 mg IV push
Transcutaneous
Repeat every 3 5 min to total of 0.04 mg/kg (3 mg)
Dopamine: 2 to 10 mcg/kg/min
Transvenous
Epinephrine gtt: Start at 1 mcg/ min and titrate
to patient response.
Epicardial
59
60
10
4/6/2013
Transcutaneous Pacemaker
Transvenous Pacemaker
Epicardial Pacemaker
Temporary
Generator
Epicardial Pacemaker
Lead Placement
Transvenous Pacemaker
Lead Placement
61
62
The NASPE/BPEG Generic (NBG) Code
External Pacing
Position
Category Chamber(s)
Paced
Pacing producers an electrical artifact on
the strip called a spike.
QRS appears wide & bizarre (like a PVC)
II
III
IV
Chamber(s)
Sensed
Response to
Sensing
Programmability
Rate Modulation
Antitachyarrhythmia
Function(s)
O = None
O = None
O = None
O = None
O = None
A = Atrium
A = Atrium
T = Triggered
P = Simple Programmable
P = Pacing
V = Ventricle
V = Ventricle
I = Inhibited
M = Multiprogrammable
S = Shock
D = Dual (A+V)
D = Dual (A+V)
D = Dual (T+I)
C = Communicating
D = Dual (P+S)
R = Rate Modulation
Manufacturers
Designation
Only
63
S = Single
(A or V)
S = Single
(A or V)
Note: Positions I through III are used
exclusively for antibradyarrhythmia
function
64
Sensitivity
Pacing Codes
VVI
the number,
sensitivity(more sensitive)
Pacing in Ventricle only
Sensing in Ventricle only
Response will be inhibited if it senses activity
in the Ventricle
65
5.0v
2.8v
1.4v
66
11
4/6/2013
Loss of Capture
Troubleshooting
Electrical stimuli delivered by
the pacemaker does not initiate depolarization of
the atria or ventricle
Failure to capture
Improper Sensing
Loss of Output
Atrial
No capture
Ventricular
No capture
Fusion
67
68
Undersensing
Failure to Capture
Failure of the pacemaker to sense
intrinsic R-waves or intrinsic P-waves
Leads to OVER PACING
69
Undersensing: Causes
70
Undersensing
Battery depletion
Decreased QRS voltage
Fusion beat
Dislodged/fractured lead
Inappropriate sensitivity setting
What to do:
Increase the sensitivity by
lowering the number
(lower the fence)
71
72
12
4/6/2013
Oversensing
Oversensing
Inhibition of the pacemaker by events the
pacemaker should ignore
What to do:
Eliminate interference
Adjust sensitivity: Make less sensitive by
increasing the number (raise the fence)
Leads to UNDER PACING
73
No Output
74
OH, NO!
Pacemaker fails to emit stimuli at the
programmed intervals
Battery depletion/pacemaker off
Faulty cable connection
Oversensing
Dislodged/fractured lead
75
Ventricular Fibrillation
76
Defibrillation
Energy Requirements for adults:
If using a biphasic defibrillator:
150- 200 joules initially
For second and subsequent shocks, use
the same energy or higher
If using a monophasic defibrilators:
Select a dose of 360 joules for all shocks
Significance:
Requires immediate defibrillation & CPR!
77
78
13
4/6/2013
Epinephrine:
Epinephrine
Special considerations / Cautions
Administer 1 mg (10 ml of 1:10,000)
every 3 5 minutes
May be given via ETT
Instill 2 to 2.5 mg into ETT
Stimulation of alpha adrenergic receptors:
peripheral vasoconstriction & coronary
& cerebral blood flow
If given IV, be sure to flush with 20 ml of
fluid or elevated arm
High doses have not been shown to
improve survival
Makes ventricular fibrillation more
responsive to defibrillation
79
80
Pulseless Electrical Activity
Vasopressin
Any organized rhythm that DOES NOT PRODUCE
Can be substituted for the first or second dose of
epinephrine
A PULSE.
Characteristics: Variable
Give 40 units IV bolus.
Significance:
Immediate CPR is required.
Look for possible reversible causes.
Effects:
Coronary perfusion pressure
Vital organ blood flow
Cerebral oxygen delivery
81
Asystole
82
PULSELESS ARREST / ASYSOLE
Treat PEA with P-E-A:
Possible Causes
Epinephrine
Atropine (old)
Continue CPR and administer:
Epinephrine 1 mg IV, every 3 5 minutes
Atropine 1 mg IV, every 3 5 minutes
83
(up to 3 doses) (OLD guideline)
84
14
4/6/2013
PULSELESS ARREST / ASYSOLE
Therapeutic Hypothermia
No electrical therapy is indicated.
Move quickly to identify reversible causes:
Hs:
Hypothermia,
Hypoxemia,
Hypoglycemia,
Hypovolemia,
Hydrogen ions
(acidosis),
Hypo-hyperkalemia
Recommended for
witnessed pulseless VT &
VF arrests
Ts:
Toxins,
Tamponade,
Tension pneumothorax,
Thrombosis (cardiac and
pulmonary),
Trauma
Tablet (overdose)
May be beneficial in
PEA/Asystole arrests
Potential complications
Infection
Bradycardia
Electrolyte imbalances
Cool to 32-34C for 12-24
hours
Prevent shivering
Potassium
Calcium
Phosphorus
Magnesium
Hyperglycemia
85
Heart Sounds
S3: ventricular gallop
Normal in children
Adults: LVEDP
(preload); LV failure
Summation gallop
S4, S1,S2, S3
CHF, anemia,
ischemic hearts
86
Systolic murmurs
Aortic stenosis
Pulmonic stenosis
Mitral insufficiency
Tricuspid
insufficiency
Diastolic murmurs
Aortic insufficiency
Pulmonic
insufficiency
Mitral stenosis
Tricuspid stenosis
87
88
Risk Factors
Acute Coronary Syndromes (ACS)
The common
pathophysiology is ruptured
or eroded plaque.
Cigarette smoking
Hypertension
Obesity
Diabetes Mellitus
SBP > 160 mm Hg
Gender/Age
DBP > 95 mm Hg
Sedentary lifestyle
Hyperlipidemia
Total chol >240
mg/dL
Family history
HDL <35 mg/dL
89
90
15
4/6/2013
Classification of Infarct
Coronary Arteries
Right coronary (RCA)
Left coronary (LCA)
STEMI- ST segment elevation
Non-STEMI- Non-ST segment elevation infarct
The goal is to open the artery to restore blood
flow.
TIME IS MUSCLE
Want to treat within 12 hours
Late restoration of patent artery still increases
survival
Left anterior
descending (LAD)
Circumflex (CF)
91
Supplies blood to:
SA node-55% hearts
AV node-90% hearts
Right Coronary
Artery
RA & RV muscle
92
Left Anterior Descending
Coronary Artery
Supplies blood to:
Anterior/lateral surface LV
Bundle of His
Anterior 2/3
Inferiorposterior wall of LV
intraventricular septum
1/3 septum, posterior
R bundle branch
fascicle of left bundle
branch
Inferior surface RV
Anterior L bundle branch
LV papillary muscle
93
94
Ischemia: T wave Changes
Left Circumflex
The normal T wave has the following
characteristics:
Supplies blood to:
AV node 10% hearts
SA node in 45% hearts
Lateral posterior surface of LV
Portion of posterior wall
Asymmetry
The T wave is normally positive in leads I, II, V3 to V6
The T wave is less than 2/3 the height of the preceding
R wave.
95
96
16
4/6/2013
Abnormal T Waves: Ischemia
Abnormal T Waves: Potassium
If a T wave is flipped and symmetrical, it suggests ischemia
T waves that are tall and peaked suggest elevated potassium levels
97
The ST segment
Abnormal ST Segments: Ischemia
The key thing to identify with the ST segment is
its relationship to the baseline.
ST depression suggests ischemia in the
The normal ST segment is isoelectric or level with the
area viewed by that lead
ST depression is considered significant if:
baseline
Normal ST
Segment
Elevated ST
Segment
98
Depressed
ST Segment
Depression >1 mm below the baseline
Depression is seen in 2 or more leads
facing the same area of the heart
ST depression occurs in < 20 minutes of ischemia.
99
ST Depression
100
ST Segment Elevation: Injury
ST elevation is considered
significant if:
Elevation is > 1 mm in the
limb leads or > 2 mm in the
precordial leads
Elevation occurs in two or
more leads facing the same
area of the heart
101
ST elevation occurs within
20-40 minutes after injury
occurs.
102
17
4/6/2013
ST Elevation
Q Waves: Infarction
Pathological Q wave represents an area of dead
tissue or infarction.
The Q wave is > 0.04 seconds wide
The Q wave is >1/4 of the height of the R wave
that follows.
Q waves usually take up 24 hours to develop.
They do not reveal when the infarction
occurred.
Early development of Q waves predicts a
large infarction.
103
Pathologic Q Waves
104
Cardiac Markers
CPK 3 isoenzymes
CPK-MB is more specific to myocardium. Normal values:
CK (Total) - Males < 180, Females <130
CK MB Mass - < 8.0
CK Relative Index - < 4.0
Can be falsely elevated in renal failure, skeletal muscle injury,
marathon runners
Elevations do not occur for up to 6 hours after injury.
Troponin I
Elevations start within 3 hours after ischemic event.
Normal value: < 0.6
Remains elevated longer than CPK -MB
Highly sensitive markers for cardiac injury
105
Case Study
106
Risk Stratification
45 y.o. Male w/ history of CRD, HTN, and
pancreatitis. Onset of abd pain in am. Felt like
severe gas. Not like previous pancreatitis pain.
Initial Interventions
(within 10 minutes)
Targeted history
Biomarker
1230
1900
0445
<0.04
245.4
258.35
3792
3487
493.8
330.5
Oxygen, Monitor, IV (Oh, MY!)
12 lead ECG
Troponin I
CK
CK-MB
2.8
Vital signs
Serum Markers
Goal:
Door to Drug: 30 minutes
Door to Balloon: 90 minutes
MONA
107
108
18
4/6/2013
The 12 Lead ECG:
Four Column Layout
12 Lead ECG machines layout the various
leads in 4 standard columns:
109
110
12 Lead ECG Layout
Using the 12 Lead ECG:
Localization of Problems
High Lateral
High Lateral
Inferior
Lateral
AVR None
V1 Septal
V4 Anterior
II Inferior
AVL Lateral
V2 Septal
V5 Lateral
III Inferior
AVF Inferior
V3 Anterior
V6 Lateral
Septal
Anterior
Low Lateral
Note: This one has 2 leads of rhythm strips
111
Localizing Injury
Affected
Part
Vessel(s)
Involved
Leads
Anterior
LAD
V3, V4
Inferior
RCA
II, III, avF
Lateral
Septal
Circumflex
LAD
V5, V6, I, avL
V1, V2
Posterior
Circumflex; Reciprocal
RCA
changes, V1, V2
Right
RCA
Ventricular
112
TREATMENT
Electrical Complications
PVC, SVT, 2 AV Mobitz II,
CHB, BBB, Hemiblocks
PVC, SB, ST, JR, PAC, Atrial
Fib, 2 AV Mobitz II
(Wenckeback)
PVC, SB, ST, PAC, A. Fib
Same as Anterior
Same as Inferior
V4R
113
114
19
4/6/2013
MONA Greets Them at the Door
Treatment
STEMI
Non-STEMI
NO
Time from onset <12 hr ?
Admit to monitored bed
YES
Reperfusion:
Door to needle: < 30 min
Door to balloon: < 90 min
NTG
Beta Blockers
ACE Inhibitors
Statin Therapy
Heparin
Clopidogrel
Non-Diagnostic
NTG
Beta Blockers
ACE Inhibitors
Statin Therapy
Heparin
Glycoprotein
IIB/IIIA Inhibitor
Clopidogrel
Follow serial markers
Repeat ECG
Consider stress test
Early Invasive Therapy within 48 hr of AMI
Oxygen:
Continue for at least
initial 6 hours, then
DC if oxygen
saturation is >90%.
Nitroglycerin: Dilates
Aspirin: Inhibits
platelet aggregation.
Give 162- 325 mg as
soon as patient
arrives in ED.
CHEW.
If NTG does not relieve pain:
coronary arteries to increase
blood flow to heart.
preload by venous
dilation. Give:
Give Morphine 2-4 mg IV
every 5- 15 minutes until
pain free.
Morphine relieves anxiety /
pain & acts as vasodilator.
115
Question
Re-Perfusion Strategy: Fibrinolytics
Breaks up the fibrin network that binds clots
together
Indications:
ST elevation in 2 or more leads
Onset of symptoms < 12 hours
MAY CAUSE DEATH FROM BRAIN
HEMORRHAGE
Agents available : alteplase (tPA, Activase),
retaplase (Retavase), streptokinase (Streptase),
tenecteplase (TNKase)
116
Which of the following lab results should be
reported to the cardiologist for a patient
with ACS who is scheduled to go for cardiac
catherization & possible PCI?
a. aPTT 65 sec
b. Troponin 0.2ng/ml
c. Serum K+ 4.9 mEq/L
d. Serum creatinine 2.3 mg/dL
117
118
Adjunctive Medications
If a Blockage is found:
Multiple options are available
Balloon angioplasty
Coronary atherectomy
Stent placement
Laser
receptor blocking agents
Clopidogrel (Plavix);
Prasugrel (Effient)
Heparin, Lovenox
ACE Inhibitors & ARBs
Statins
119
120
20
4/6/2013
Blockers
Blockers
Mechanism of action:
Blocks catecholamines
from binding to adrenergic receptors.
heart rate, blood
pressure, and myocardial
contractility
AV nodal conduction
incidence of primary
ventricular fibrillation
Absolute
Contraindications
Severe CHF
SBP < 100 mm HG
Acute asthma
2nd or 3rd degree heart block
Cautions
Mild / moderate CHF
Heart rate <60
History of asthma
Insulin dependent
diabetes
Severe Peripheral
Vascular Disease
121
Heparin vs. Enoxaparin (Lovenox)
Unfractionated heparin
Given as a continuous infusion
Keep PTT within target range of 50 to 70 (1.5 to 2x
baseline)
Reversal agent: Protamine sulfate
Low molecular weight- Enoxaparin
Given as an injection every 12 hours
122
Medications to Prevent Platelet Aggregation
CAUTION: Use of these agents have resulted in bleeding
complications such as retroperitoneal bleeds at PCI site &
intracranial hemorrhage.
Glycoprotein IIB/IIIC
Clopidogrel (Plavix):
Inhibitors
Irreversible inhibition of
(Reopro, Aggrastat, Integrelin)
platelet aggregates
Inhibit platelet aggregation
Start 300 mg dose at the
Shown to decrease mortality &
time of reperfusion,
continue 75 mg daily
dose for 8 days.
May need to withhold
for 5 7 days prior to
CABG
124
should be used in all patients
with non-STEMI as soon as
possible in conjunction with
aspirin, heparin, clopidogrel,
and early PCI
DO NOT administer either within 6 hours of nonspecific fibrinolytic
123
ACE Inhibitors
RAS & ACE Inhibitors
Decreased renal
blood flow
Mechanism of action
JG cells
stimulated
Renin
released
Reaction with
angiotensinogen
Reduces BP by inhibiting angiotensin-
converting enzyme
Alters left ventricular remodeling that occurs
Increased
blood vol.
post MI by inhibiting tissue ACE
Lowers peripheral vascular resistance by
vasodilation
Reduces mortality and CHF after an acute MI
Improved renal
blood flow
125
Na+, H2O
retention
Aldosterone
secretion
Increased arterial
blood pressure
Angiotensin I then
II production
Vasoconstriction
126
21
4/6/2013
MI Complications
Statins
complications such as reinfarction, recurrent
angina, and arrhythmias
Dysrhythmias most
occurs with inferior /
common complication
of the deaths occur within
both total cholesterol and LDL.
1st hour of symptoms -usually due to v. fib
Stabilize platelets, improve endothelial
function, & inhibit inflammatory response.
Heart failure Can range
Should be started within 24 hours
from mild dysfunction to CHF
to cardiogenic shock.
127
Question
Your MI patient suddenly develops LOC, a weak, thready
pulse, and bilateral posterior crackles in the lower lung fields.
VS: 78/46; HR 139; RR 25
u/o < 30 ml for the last hour
O2 sat 89% on 4L NC
You suspect
RV infarction:
posterior MI. Incidence
around 40%
Patients with RV infarct
need VOLUME & are
very sensitive to NTG
Emboli:
Thrombi form on inner
wall at site of MI. Most
common with large
anterior MI.
Papillary muscle
rupture
128
Assistance to the Failing Ventricle:
Intra Aortic Balloon Counterpulsation
a. Stroke
b. ARDS
c.
Pulmonary embolus
d. Cardiogenic shock
129
IABP Placement
130
IABP- How does it work?
Inflation during diastole
When the IABP balloon is properly
placed, it is just distal to the left
subclavian artery.
If the IABP balloon is displaced
proximally, it can occlude the takeoff of the left subclavian artery
If the IABP balloon is displaced
Aortic root pressure
Aortic diastolic pressure
Coronary perfusion pressure
CPP = Aortic diastolic pressure
myocardial wall tension
Oxygen supply
Stroke volume = Heart rate
distally, it can occlude the take-off
of the renal arteries
131
132
22
4/6/2013
Primary Effect of IABP Therapy
IABP- How does it work?
Supply
Deflation immediately
prior to systole
Aortic end-diastolic
Demand
pressure
Impedance to ejection
Afterload
Oxygen demand
Supply Balloon Inflation
Demand Balloon Deflation
133
Indications
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
134
Contraindications
Cardiogenic shock
Refractory ventricular failure
Unstable refractory angina / impending infarction
Mechanical complications due to acute myocardial
infarction
Ischemia related to intractable ventricular
arrhythmias
Cardiac support for high risk general surgical and
coronary angiography / angioplasty patients
Septic shock
Weaning from cardiopulmonary bypass
Intra-operative pulsatile flow generation
Support for failed angioplasty and valvuloplasty
Severe aortic insufficiency
Abdominal or aortic aneurysm
Severe calcific aorta-iliac disease or
peripheral vascular disease
135
Congestive Heart Failure: Definition
Question
Systolic failure: cardiac contractility
An IABP is used to manage cardiogenic shock in
order to increase
a.
Diastolic failure: impaired cardiac relaxation
and abnormal ventricular filling.
Coronary perfusion during systole
The heart is unable to generate a cardiac output
sufficient to meet the demands of the body.
Manifested by:
Poor tissue perfusion and congestion of the
vascular beds
Symptoms of inadequate tissue perfusion
b. Myocardial oxygen supply
c.
136
LV filling volume
d. LV systolic pressure
137
138
23
4/6/2013
Pathophysiology:
Systolic Dysfunction
Impaired LV contractility results in
reduced ejection fraction (EF < 40%)
Ventricle is dilated, thin walled
Dilated Heart
(Systolic Failure)
Etiology:
Acute Myocardial Infarction
Coronary Artery Disease,
Hypertension
Valvular Heart Disease
Toxins
Endocrine
Congenital
Chronic Heart Failure:
Pathophysiology
Myocardial Toxicity
Morbidity
Mortality
Hypertrophic Heart
(Diastolic Failure)
Sarcoidosis
Amyloidosis
140
Forward Failure
BNP
ANP
Peripheral vasoconstriction
Hemodynamic alterations
Remodeling and
progressive
worsening LV function
Left Ventricular Failure
Fall in LV Performance
Activation of RAAS, SNS
Normal systolic function with the impaired
ability of the ventricle to relax (lusitropy) and
fill with blood
filling pressures result due to stiff ventricles
Ventricle is thickened and concentrically
hypertrophied
Etiology
Hypertension, coronary artery disease
Cardiomyopathy
Aortic Stenosis
Infiltrative diseases
139
Myocardial
Injury
Pathophysiology:
Diastolic Dysfunction
Heart Failure Symptoms
Signs of Decreased CO
Fatigue, poor exercise
tolerance
Tachycardia
Narrow pulse pressure
Cool, pale, diaphoretic
Altered mental status
Decreased urine output
Backward Failure
Signs of Elevated
Pulmonary Pressure
Dyspnea, tachypnea
Orthopnea
Cough, wheeze
Hypoxia
Respiratory Alkalosis
Crackles, rhonchi
S3,S4
141
142
Right Ventricular Failure
Dependent edema
What kind of
heart failure
does this man
have
Right or Left ?
RAP/CVP
Fluid vol. Backs into portal system
GI s/s
Ascites
Nocturia
Weakness, fatigue
Murmur of TR
143
144
24
4/6/2013
Classification of Heart Disease
ACC/AHA Heart Failure Stage
A
B
Structural heart disease,
but no symptoms of heart
failure
With cardiac disease, but
asymptomatic and without
limitations of physical activity
Structural heart disease
with prior or current
symptoms of heart failure
II
Symptoms with moderate
exertion resulting in slight
limitation of physical activity
III
Symptomatic with minimal
exertion resulting in marked
limitations of physical activity
IV
Symptomatic at rest. Inability
to carry on any physical
activity without discomfort
Refractory heart failure
requiring specialized
interventions
Compensatory Mechanisms
NYHA Functional Class
At high risk for heart failure,
but no symptoms or
structural heart disease
None
In the short term, compensatory mechanisms
maintain cardiac output.
In the long term, all of these factors trigger a
process of pathologic growth and remodeling.
Include:
Stimulation of SNS
Activation of Renin-Angiotensin-Aldosterone System
Hypertrophy
145
146
VENTRICULAR REMODELING
Myocardial Hypertrophy
Decrease contractilitydecreased stroke
volumeActivation of SNS & RAAS
Increased ventricular volumes
Late compensatory mechanism
Larger cells less contractile & require more oxygen
Increased ventricular pressures
Ischemia leads to fibrosis and necrosis
Increased ventricular wall tension
Thinning of ventricle wall & chamber dilation
Decrease contractility
Fibrous tissue deposits
HEART FAILURE
147
148
Pharmacologic
Pillars of Treatment:
Systolic Treatment
Drug Therapy using the A-B-C-Ds
Loop diuretics
Spironolactone
Diastolic Treatment
ACE inhibitors: Block RAAS
Beta Blockers
Diuretics
Beta blockers: Block SNS
ACE inhibitors
Beta Blockers
Contractility: Digitalis
Digoxin
ACE inhibitors
Calcium Channel
Diuretics, VasoDILATORS:
Blockers
Preload & Afterload
149
150
25
4/6/2013
Angiotensin II Receptor Antagonists: ARBs
Beta Blocker Selection
Beta blockers recommended for heart failure include:
Indicated for patients who cannot
tolerate ACE Inhibitors.
Act directly on angiotensin receptors.
Increased selectivity & specificity by
directly blocking angiotensin
receptors
Example: Losartan
both preload and afterload
Fewer side effects
Carvedilol (a non-selective agent)
Metoprolol: Long acting
Bisoprolol
Doses may need to be titrated gradually over a period of
several weeks.
Selective agents incidence
of:
Bronchospasm
Cold extremities
Other peripheral side effects
151
Preload: Diuretics
GOAL: To restore fluid balance
Beneficial effects
Excrete sodium and water
Decrease CVP
Symptom relief
Decrease shortness of
breath & edema
152
Preload / Afterload: Vasodilators
Vasodilators that target
Preload:
Nitroglycerin
Morphine
Detrimental effects
Electrolyte imbalances
Decrease renal
function
Activates RAAS
Hypotension
Vasodilators that target
Afterload:
Nipride
NTG at > 50mcg/min
Use Daily Weight
For diuresis monitoring
153
Contractility
Nitrates not as
Effective as ACE
Inhibitors
154
BNP: Brain Natriuretic Peptide
Natriuretic peptides are a family of naturally
Digoxin: Used for inotropic support
occurring molecules.
Actions:
Dobutamine: Used short term
cardiac preload by causing vasodilatation &
vascular capacitance.
sympathetic tone.
Induce natriuesis (sodium excretion) by actions
on renal vasculature and tubules.
Milrinone: Used for patients who develop
tolerance to dobutamine
155
156
26
4/6/2013
BNP Measurement
Natrecor (Nesiritide)
Measurement of BNP can differentiate patients with
heart failure from patients without heart failure.
BNP level >100 is indicative of HF
May also be elevated in right sided failure due to
pulmonary disease and end stage renal disease.
May see false negative in patients with flash
pulmonary edema and heart failure due to mitral
regurgitation.
Synthetic natriuretic peptide (BNP)
Approved for IV use in acute decompensated heart
failure
pulmonary pressures
Improves dyspnea
Contraindicated with systolic BP < 90
Monitor closely for hypotension and
arrhythmias
157
158
Adjunct Therapies
Left Ventricular Assist Device
All AT RISK patients should be on:
Beta blockers
ACE
Statins Believed to decrease inflammatory response
May also require:
Anticoagulants If patient develops atrial fibrillation
Antiarrhythmics
Physical conditioning
Consider:
Biventricular Pacing / Cardiac Re-synchronization
IABP
Assist Devices
Transplant
159
160
Question
Heart Transplant
A patient status-post heart transplant develops
second degree heart block, Type II. VS: 86/40; HR
44; RR 24. The patient c/o chest pain. Skin is
warm and dry. Breath sounds clear. You should
a. Prepare for transcutaneously pacing
b. Draw labs to determine if patient is rejecting the heart
c. Administer 0.5 mg atropine
d. Reassure the patient that what he is experiencing is
normal after a heart transplant
161
162
27
4/6/2013
Acute Inflammatory Diseases
Question
Myocarditis
Acute rejection in cardiac transplantation is
diagnosed by:
a. ECG
b. Chest x-ray
c. Echocardiography
d. Endomycardial biopsy
Endocarditis
Pericarditis
163
Myocarditis
164
Question
Inflammation of the myocardium
Etiology: viral, bacterial, parasitic, fungal,
radiation to chest
Acute or chronic
S/S: chest soreness, burning: with inspiration;
syncope; fever; S3, S4;
Dx: WBC; CK-MB; Cardiomegaly; diffuse ST
& T wave abnormalities; SVT or ventricular
dysrhythmias
Which of the following medication
regimens would be most appropriate to
relieve chest pain in a patient with
diagnosis of myocarditis?
a.
NTG 1/150 grains sublingual
b. Furosemide 40 mg IV
c.
Ibuprofen 800 mg PO
d. Morphine sulphate 2 mg IV
165
Infective Endocarditis
166
Question
Definition: Inflammation of the
endocardium, usually occurring in the
membranous lining of the heart valves
The valve most often effected by infective
endocarditis is:
a. Mitral
b. Aortic
c. Tricuspid
d. Pulmonary
Etiology:
Congenital or acquired heart disease
Invasive monitoring (PA catheters,
temporary pacing wires, etc)
Cardiac surgery
IV catheters / dialysis access devices
GI / GU tubes (Foley cath)
Dental procedures / poor oral hygeineg use
167
168
28
4/6/2013
Infective Endocarditis:
Presentation
Janeway
lesions
Infectious symptoms (fever, chills, malaise)
Fatigue, night sweats, anorexia, weight loss
Symptoms of heart failure
Infectious Endocarditis
Diagnosis: Blood cultures; TEE
Management
Prevention:
Patients with valve disease should receive antibiotics prior to any
invasive procedure
Good hygiene
No street drugs
Decrease myocardial oxygen demand
Control and treat infection
Antibiotics for 6 8 weeks
Monitor for complications
Systemic emboli
Valve surgery may be required
New murmur (aortic insufficiency most common)
Vascular signs:
Splinter hemorrhages
Petechiae on chest, oral mucosa, abdomen
Janeway lesions: Flat, erythematous lesion on
palm, soles of feet
Roths spots: Round white lesions on retina
Oslers nodes: Painful nodules on fingers,
toes
Oslers
Nodes
169
Pericarditis
Pericarditis
Etiology:
Presentation:
Sharp, stabbing pain that radiates to the left
shoulder
Aggravated by inspiration, supine position
Relieved by sitting up or leaning forward
Dyspnea, tachypnea
Tachycardia
Murmur / rub
Fever
Diagnostic:
Idiopathic
Post MI May be acute
170
(within 7 days) or
Dresslers syndrome
(occurs 2 wks or more
later)
Trauma
Infection
Radiation
Drugs
Troponin elevated, WBC
Definition:
Inflammatory process involving the
visceral or parietal pericardium
Diffuse ST elevation in all leads
171
Pericarditis - Management
Cardiac Tamponade
Management
Non-steroidal anti-inflammatory drugs
Treat cause
Monitor for complications:
172
If fluid accumulates in the pericardial sac, there is
potential for development of cardiac tamponade.
Tamponade has a constrictive effect on the heart.
Must be treated urgently!
TAMPONADE
Dysrhythmias
Anticipate pericardiocentesis or pericardial
window
173
174
29
4/6/2013
Hypertension Definitions
Question
Hypertension: Elevation in BP above 140 /90 on at least 3 separate
occasions
Hypertensive Urgency: Develops over days to weeks. Characterized
by diastolic BP, but are usually not associated with end organ
damage.
Hypertensive Crisis: Elevation severe enough to cause the threat of
immediate vascular necrosis and end organ damage. Usually > 180 / 120
or MAP over 150.
The classic triad (Becks triad) of symptoms of
cardiac tamponade are:
a. Rales, muffled heart sounds, bradycardia
b. Widened pulse pressure, atrial dysrhythmias
c. Tachycardia, hypotension, narrow pulse
pressure
d. Hypertension, flushing, pulse paradoxus
Accelerated: DBP >120
Malignant: DBP > 140
Hypertensive Emergency: Develops over hours to days. BP must be
lowered within minutes to an hour to reduce potential complications or
new / progressive end organ damage.
Hypertensive Encephalopathy: BP > 250/ 150
175
176
Hypertensive Crisis
Principles of Treatment
Goal: Reduce cardiac & renal mortality and morbidity
BP = CO x PVR
Usually require ICU admission
BP= Cardiac Output x Peripheral Vascular Resistance
Reduce BP gradually to maintain cerebral perfusion.
In hypertensive emergency:
All antihypertensives must act by:
cardiac output
peripheral vascular resistance.
Decrease MAP 25% within first hour
Decrease to 160/ 100 within next 2- 6 hours, then gradual reduction over
next 24 hours
Agents:
Sodium nitroprusside, fenoldopam, hydralazine
Hydralazine good in eclampsia
177
Question
178
Cardiomyopathy
When admitting a patient with hypertensive
crisis, the nurses immediate concern is
to prevent which of the following
complications?
a. Stroke
b. End organ failure
c. Seizures
d. Left ventricular hypertrophy
Dilated
Hypertrophic (Idiopahtic
hypertrophic subaortic stenosis
[IHSS])
Restrictive
179
180
30
4/6/2013
Cardiomyopathy: Dilated
Cardiomyopathy: Hypertrophic
mass & thickening of myocardium
Myocardial fibers degenerate & fibrotic changes
occur
Fibrosis occurs
Systolic and diastolic dysfunction
Mitral Insufficiency
LV chamber in size
Ventricles rigid & stiff
LA dilates
May develop outflow obstruction
Ventricular rhythms common cause of death
181
182
Your patient, admitted with cardiomyopathy, c/o
dyspnea, & palpitations. CM: SR, no ectopy.
You anticipate management to include
Cardiomyopathy: Restrictive
Restricted filling of ventricles
Etiology: Idiopathic; Amyloidosis
a.Insertion of a left ventricular assist device
compliance; LV stiff & can not dilate or
contract well in systole
b.Preparing the patient for a cadiomyoplasty
c. Administration of enalopril (Captopril)
LVEDP ; contractility ; CO HF
Death
d.Loading the patient with digoxin
183
Cardiomyopathy: Rx
ACE inhibitors
B-blockers
Antidysrhythmic
agents
Antibiotics (at risk for
infectious
endocarditis)
184
Coronary Artery Bypass Grafting
The internal mammary artery
is frequently used because of its
long-term patency.
Other conduits include:
DCM: + inotropes;
diuretics
HOCM: Avoid agents
that preload; avoid +
inotropes (can worsen
obstruction)
Saphenous veins
Radial artery
Gastroepiploic artery
Inferior epigastric artery
185
CABG remains the treatment of choice for patients with three
vessel coronary artery disease, complex lesions, or more than
75% occlusion of the left main.
186
31
4/6/2013
Question
Question
Upon arrival to the ICU
post-CABG, the patient
has the following:
BP 180/110;
HR 70, 100% paced;
RAP 6; PAD 10
CO 3.5
U/O 60 ml
Upon turning the postoperative CABG
patient, the nurse observes 200 ml of
bloody drainage in the CT drainage
system. The nurse should perform which
of the following?
a.
Autotransfuse the patient
b. Aggressively strip the CT tubing
What should the nurse do
first?
Obtain lab for coagulation studies
d. Continue to monitor the patients CT drainage
c.
a. Bolus with 250ml to
RAP & PAD
b. NTG gtt by 6.6
mcg/min to BP
c. pacer to 75 to
improve CO
d. Administer
propranolol 1 mg IV
to BP
187
After a mitral valve replacement, the patient
is most likely to have which of the following as
part of the patients plan of care?
188
Valve Surgery
The primary cause for valve disease is
rheumatic fever.
Most commonly affected the aortic and
a. Ace-inhibitor
b. Beta-blocker
mitral valves
If allowed to persist, congestive heart
failure can occur.
Positive inotropic agent
d. Anticoagulant
c.
Surgical repair can include replacement
of the defective valve with either a
mechanical or tissue valve.
Patients with mechanical valves will
require lifetime anticoagulation
189
Cardiac Trauma
190
Question
Cardiac contusion is the most common blunt
injury to the heart.
Following a motor-vehicle accident, pericardial
tamponade is suspected. Which of the
following findings is consistent with traumatic
tamponade?
a. Muffled heart sounds
b. Pericardiocentesis of 50ml of blood
c. ST-segment depression in the limb leads
d. Rales on auscultation
Rarely fatal, but should be suspected if the patient
has anterior chest wall trauma and fractures of the
sternum and ribs.
Signs are similar to MI with ST changes and elevation
of enzymes
ECG changes: RBBB; ST; ventricular dysrhythmias
Right ventricle is most often affected
Aortic rupture is the result of a blunt trauma
deceleration injury
191
192
32
4/6/2013
Aortic Aneurysms
Which of the following findings is most
indicative of a leaking abdominal aortic
aneurysm?
Thoracic or Abdominal.
Abdominal are more common (65%)
Two patterns:
a. Back pain
b. Bounding peripheral pulses
Weakness and bulging of the entire vessel
wall
Weakness and bulging within the vessel
wall
Patients with an aneurysm may be
c. Intermittent claudication
asymptomatic
Rupture of the aneurysm causes acute
pain that radiates to the back,
unrelieved by changes in position.
Mortality from rupture is 90%. The
only chance for survival is emergent
repair.
d. Nausea and vomiting
193
Aortic Dissection
194
Question
Tear in the intimal layer of the aorta
allows blood to flow into the medial layer,
creating a false channel.
It is usually accompanied by
hypertension that is not well
controlled.
Most common is ascending aorta
dissection, with many occurring only
centimeters from the aortic valve.
High risk of death from acute aortic
regurgitation and pericardial
tamponade.
Symptoms: Severe tearing or
ripping chest pain, moves to the back
as dissection progresses
Post-endovascular AAA repair, a patient has the
following findings: BP 124/76; HR 92; RR 18. Distal
pulses 2+, cap refill 2 sec. Groin without s/s of
hematoma. U/O is 20ml/hr for 2 hours. The most
likely cause of the decreased u/o is:
a. Renal toxic effects of contrast agents
b. Occlusion of the renal artery by the endograft
c. Hypovolemia due to operative blood loss
d. Hypovolemia due to retroperitoneal bleeding
195
196
Your patient has a history of hypertension and CAD.
Assessment reveals skin temperature of legs &
feet, pulses & pallor when the legs are elevated &
reddish-blue discoloration of the legs. Patient c/o
leg pain. You suspect
a. Peripheral arterial disease
b. Chronic venous insufficiency
c. Acute arterial occlusion
d. Deep vein thrombosis
Question
On PO day 2 after an AAA, your patient develops
hypotension, tachycardia, abdominal
distention, and WBC. These findings
indicate
a. Post-op graft infection
b. Ischemic colitis
c. Aortic-enteric fistula
d. Abdominal compartment syndrome
197
198
33
4/6/2013
Acute Peripheral Vascular Insufficiency
Acute Arterial Occlusion
Peripheral Stents
Medications: Antiplatelet; Thrombolytics
Carotid Stenosis
Endartarectomy
Question
After aorto-femoral
bypass surgery for
acute arterial
occlusion, your
patient has
CPK, K+ 5.9 mE/L
PaO2 90
PaCO2 24
HCO3 19
This patient is at risk for
developing
a.
b.
c.
d.
Dysrhythmias
Graft occlusion
Pulmonary embolus
Heart Failure
199
Question
Question
A patient is receiving thrombolytics via
continuous infusion for acute limb
ischemia suddenly complains of pain in
the affected extremity. The most
appropriate nursing action includes:
After femoral-popliteal bypass surgery, patient
c/o pain unrelieved by narcotics. Dressing D
& I. Skin warm, pale, & dry. Cap refill 2 sec.
Distal pulses 2+. Motor strength slightly .
Gastrocnemius muscle slightly swollen & is
doughy to palpation. These findings are
consistent with
a.
b.
c.
d.
200
a. Administer narcotic pain medication to relieve the
pain
b. Elevate the affected extremity above the level of
the heart
Compartment syndrome
Graft occlusion
Development of false aneurysm
Heparin induced thrombocytopenia (HIT)
c. Notify the MD that the patient may have
compartment syndrome
d. Discontinue the thrombolytic infusion and notify
the MD
201
202
Structural Heart Defects:
Atrial septal defects
Structural Heart Defects
Left-to-right shunt
resulting in right
chamber overload
Atrial septal defects
Ventricular septal defects
RA, RV dilate
Valvular disease
Leads to pulmonary
hypertension
Dysrhythmias: Afib,
A.Flutter, PR
prolongation,
Incomplete RBBB. LAD
203
Treatment:
Antibiotics to prevent
endocarditis
Manage heart failure s/s
Surgical repair
204
34
4/6/2013
Structural Heart Defects:
Ventricular Septal Defects
Valvular Disease
Left-to-right shunt
Mitral Regurgitation
Pulmonary HTN
S/S
Tachypnea
Sweating
Hemoptysis
Heart Failure
Holosystolic murmur
Mitral Stenosis
Treatment
Antibiotics
Manage HF s/s
Surgical repair
Aortic Regurgitation
Aortic Stenosis
205
206
Other Structural Defects
Coarctation of Aorta
Patent Ductus Artiosus
workload LA & LV
Left-sided HF
Narrowing of lumen &
flow
Tx
Tx
Ab
Ab
Tx HF
Antihypertensives
Surgical Closure
Surgery (1-5 yo)
Lets Test Ourselves Some More!
207
Which of the following vasopressors is
indicated for low CO syndrome when the
desired effect is vasoconstriction without
tachycardia?
a. Norepinephrine (Levophed)
b. Phenylephrine (Neosynephrine)
c. Dopamine
d. Epinephrine
208
Your patient c/o chest pain. The ECG shows ST
elevation in Leads II, III, & aVF. You
administer NTG 1/150 grains SL. The
patients BP drops from 136/84 to 82/50
mmHg. The most likely cause of the
decrease in BP is:
a. Right ventricular MI
b. Papillary muscle rupture
c. Hypersensitivity to NTG
d. Rupture of a ventricular free wall
209
210
35
4/6/2013
Two hrs post-CABG, patient
has these findings:
BP 80/62 (68)
CVP 15
These findings are
consistent with:
PAD 14
a. Normal post-op
CO 3
course
CT output 50ml/hr
b. Myocardial stunning
for 2 hrs.
c. Cardiac tamponade
d. Perioperative MI
Your post-op patient has a HR 132, BP
80/66, PCWP 5, Hgb 8.
Which medication would help?
a.
b.
c.
d.
Vasopressin 20 unit IVP
Administer 1 unit of PRBC
Administer 250ml NS bolus
Start dopamine at 10mcg/kg/min
211
Which of the following medications will
worsen the symptoms of hypertropic
cardiomyopathy?
a. Calcium channel blockers
b. Amiodarone
c. Beta Blockers
d. Nitrates
212
Patient admitted to the ICU status postcardiac arrest. Immediate
management of this patient includes:
a. Monitoring for hyperkalemia
b. Maintaining a blood glucose 120-
150mg/dL
c. Initiating clinically induced hypothermia
d. Monitoring labs for WBC & Plt counts
213
Chest pain that is NOT relieved by rest
& NTG is called:
Coronary artery perfusion is
dependent upon:
a.
b.
c.
d.
214
Diastolic pressure
Systolic pressure
Afterload
SVR
a.
b.
c.
d.
215
Variant angina
Stable angina
Unstable angina
Prinzmetals angina
216
36
4/6/2013
A patient admitted with CHF has the
following: BP 94/60, HR 125, RR 24,
u/o 50 ml for 2 hours. Cool clammy &
LOC. Which of the following would
be included in the patients plan of
care?
The primary function of drug
therapy with beta-blockers in
heart failure is to:
a. Increase blood pressure
b. Block compensatory mechanisms
c. Increase urine output
d. Decrease dysrhythmias
Positive inotropes, diuretics, vasodilators
a.
b. ACE-inhibitors, adenosine, beta-blockers
Beta-blockers, diuretics, calcium-channel blockers
c.
d. Negative inotropes, digoxin, antidysrhythmics
217
218
A direct effect of sodium nitroprusside
(Nipride) is to:
Which of the following medications best
improves LV function?
a. Decrease stroke volume
a. Dopamine (Intropin)
b. Increase venous return
b. Captopril (Capoten)
c. Decrease afterload
c. Digoxin (Lanoxin)
d. Increase pulmonary vascular resistance
d. Procainamide (Pronestyl)
219
Which of the following pulmonary artery
catheter findings would be anticipated
in a patient with chronic emphysema?
Which of the following findings is most
consistent with high left ventricular
filling pressure?
a.
b.
c.
d.
220
a.
Sinus bradycardia
Diastolic murmur
Peripheral edema
Bibasilar crackles
b.
c.
d.
221
Increased RAP
Decreased RAP
Increased PCWP
Decreased PCWP
222
37
4/6/2013
Two hours after a permanent DDD pacemaker is
inserted for SSS, the patient goes into atrial
fibrillation. Which of the following pacing
modes is indicated for this patient?
Which of the following is a
contraindication to the use of an
IABP?
a.
a. Aortic valve insufficiency
b.
b. Mitral valve insufficiency
c.
d.
c. Ventricular aneurysm
DVI
DDD
VAT
VVI
d. Ventricular septal defect
223
In patients with angina, CCB are effective
because they:
224
Your patient c/o chest pain that is sharp,
constant, & worse when lying down. The
pain lessens when sitting up & leaning
forward. These symptoms are consistent
with
a. Pulmonary embolism
b. Abdominal aortic aneurysm
c. Pericarditis
d. Myocardial infarction
a. Inhibit vasodilation
b. Increase myocardial contractility
c. Increase venous return
d. Reduce myocardial oxygen consumption
225
*New PCCN Cardiac Content
226
Thanks
Starting 06-26-2013, content includes:
Genetic Cardiac Disease
Long QT syndrome,
Special thanks to
Carol Boswell, RN, MSN, CCRN
for the use of many of her slides in this
presentation.
Brugada syndrome
Minimally-invasive cardiac surgery (i.e., nonsternal
approach)
Vascular disease: minimally-invasive interventions
(e.g., stents, endografts)
Cardiomyopathies: stress-induced (e.g., Takotsubo)
227
228
38
4/6/2013
Questions?
Beth Torres, PhD, RN, CCRN
CJW Medical Center,
Chippenham Campus
Beth.Torres@hcahealthcare.com
804-327-4186
229
39
S-ar putea să vă placă și
- The 12-Lead Electrocardiogram for Nurses and Allied ProfessionalsDe la EverandThe 12-Lead Electrocardiogram for Nurses and Allied ProfessionalsÎncă nu există evaluări
- EKG and ECG Interpretation: Learn EKG Interpretation, Rhythms, and Arrhythmia Fast!De la EverandEKG and ECG Interpretation: Learn EKG Interpretation, Rhythms, and Arrhythmia Fast!Încă nu există evaluări
- ECG & EKG Interpretation: How to interpret ECG & EKG, including rhythms, arrhythmias, and more!De la EverandECG & EKG Interpretation: How to interpret ECG & EKG, including rhythms, arrhythmias, and more!Încă nu există evaluări
- Arterial Blood Gas Analysis - making it easyDe la EverandArterial Blood Gas Analysis - making it easyEvaluare: 4.5 din 5 stele4.5/5 (4)
- EKG | ECG: An Ultimate Step-By-Step Guide to 12-Lead EKG | ECG Interpretation, Rhythms & Arrhythmias Including Basic Cardiac DysrhythmiasDe la EverandEKG | ECG: An Ultimate Step-By-Step Guide to 12-Lead EKG | ECG Interpretation, Rhythms & Arrhythmias Including Basic Cardiac DysrhythmiasEvaluare: 3 din 5 stele3/5 (5)
- ECG/EKG Interpretation: An Easy Approach to Read a 12-Lead ECG and How to Diagnose and Treat ArrhythmiasDe la EverandECG/EKG Interpretation: An Easy Approach to Read a 12-Lead ECG and How to Diagnose and Treat ArrhythmiasEvaluare: 5 din 5 stele5/5 (2)
- CCRN-PCCN-CMC Review Cardiac Part 3Document18 paginiCCRN-PCCN-CMC Review Cardiac Part 3Giovanni MictilÎncă nu există evaluări
- Nursing: Lab Values: a QuickStudy Laminated 6-Page Reference GuideDe la EverandNursing: Lab Values: a QuickStudy Laminated 6-Page Reference GuideÎncă nu există evaluări
- EKG | ECG Interpretation. Everything You Need to Know about 12-Lead ECG/EKG InterpretationDe la EverandEKG | ECG Interpretation. Everything You Need to Know about 12-Lead ECG/EKG InterpretationEvaluare: 3 din 5 stele3/5 (1)
- Invasive Hemodynamic MonitoringDocument24 paginiInvasive Hemodynamic Monitoringheyyymeee100% (3)
- Ccrn Certification Examination Practice Questions and Answers with Rationale: First EditionDe la EverandCcrn Certification Examination Practice Questions and Answers with Rationale: First EditionEvaluare: 5 din 5 stele5/5 (1)
- Adult CCRN Exam Flashcards, Second Edition: Up-to-Date Review and PracticeDe la EverandAdult CCRN Exam Flashcards, Second Edition: Up-to-Date Review and PracticeEvaluare: 5 din 5 stele5/5 (1)
- Adult CCRN Exam Premium: Study Guide for the Latest Exam Blueprint, Includes 3 Practice Tests, Comprehensive Review, and Online Study PrepDe la EverandAdult CCRN Exam Premium: Study Guide for the Latest Exam Blueprint, Includes 3 Practice Tests, Comprehensive Review, and Online Study PrepÎncă nu există evaluări
- Haemodynamic Monitoring & Manipulation: an easy learning guideDe la EverandHaemodynamic Monitoring & Manipulation: an easy learning guideÎncă nu există evaluări
- Surviving the ICU: A Toolkit for the Critical Care NurseDe la EverandSurviving the ICU: A Toolkit for the Critical Care NurseÎncă nu există evaluări
- CCRN PulmonaryDocument107 paginiCCRN PulmonaryCzarina Charmaine Diwa100% (4)
- CCRN QuestionsDocument19 paginiCCRN QuestionsMelissaDavis67% (6)
- CRITICAL CARE NURSE: Passbooks Study GuideDe la EverandCRITICAL CARE NURSE: Passbooks Study GuideÎncă nu există evaluări
- CCRN ReviewDocument22 paginiCCRN ReviewMelissaDavis71% (7)
- CCRN Sample QuestionsDocument5 paginiCCRN Sample Questionsgwapdose50% (2)
- Schaum's Outline of Critical Care Nursing: 250 Review QuestionsDe la EverandSchaum's Outline of Critical Care Nursing: 250 Review QuestionsEvaluare: 5 din 5 stele5/5 (1)
- CCRN AACN PremiumQs PDF PDFDocument70 paginiCCRN AACN PremiumQs PDF PDFTracy Pope100% (2)
- CCRN-PCCN-CMC Review Cardiac Part 2Document21 paginiCCRN-PCCN-CMC Review Cardiac Part 2Giovanni Mictil100% (1)
- Cardiovascular Nursing: Scope and Standards of PracticeDe la EverandCardiovascular Nursing: Scope and Standards of PracticeEvaluare: 5 din 5 stele5/5 (2)
- CCRN Synergy and Exam StartegiesDocument12 paginiCCRN Synergy and Exam StartegiesMarcus, RN100% (2)
- CCRN Exam CramDocument2 paginiCCRN Exam CramJan Marcus0% (3)
- CCRNDocument17 paginiCCRNNílo Stárn100% (1)
- The Art of the Iv Start: Common Techniques and Tricks of the Trade for Establishing Successful Peripheral Intravenous LinesDe la EverandThe Art of the Iv Start: Common Techniques and Tricks of the Trade for Establishing Successful Peripheral Intravenous LinesÎncă nu există evaluări
- Vascular Nursing: Scope and Standards of PracticeDe la EverandVascular Nursing: Scope and Standards of PracticeÎncă nu există evaluări
- Critical Care Nursing Certification: Springhouse Review ForDocument384 paginiCritical Care Nursing Certification: Springhouse Review ForNrhildaÎncă nu există evaluări
- Critical Care Manual of Clinical Procedures and CompetenciesDe la EverandCritical Care Manual of Clinical Procedures and CompetenciesÎncă nu există evaluări
- CCRN Review Part 1: "Never Let What You Cannot Do Interfere With What You Can Do"Document160 paginiCCRN Review Part 1: "Never Let What You Cannot Do Interfere With What You Can Do"Paolo VegaÎncă nu există evaluări
- Advance Cardiac Life Support: Short, Sweet and to the PointDe la EverandAdvance Cardiac Life Support: Short, Sweet and to the PointEvaluare: 3 din 5 stele3/5 (2)
- Mastering ICU Nursing: A Quick Reference Guide, Interview Q&A, and TerminologyDe la EverandMastering ICU Nursing: A Quick Reference Guide, Interview Q&A, and TerminologyÎncă nu există evaluări
- Cardiac Arrhythmia Recognition: an easy learning guideDe la EverandCardiac Arrhythmia Recognition: an easy learning guideÎncă nu există evaluări
- 2023 Certified Emergency Nurse (CEN) No-Fluff Study Guide:De la Everand2023 Certified Emergency Nurse (CEN) No-Fluff Study Guide:Evaluare: 2 din 5 stele2/5 (1)
- CCRNPart 2Document164 paginiCCRNPart 2Paolo Vega100% (5)
- 8 Week CCRN Study PlanDocument6 pagini8 Week CCRN Study PlanJoshua Atienza100% (2)
- CCRN-PCCN-CMC Review Cardiac Part 1 PDFDocument14 paginiCCRN-PCCN-CMC Review Cardiac Part 1 PDFGiovanni Mictil100% (1)
- CCRN Review Course 2015Document81 paginiCCRN Review Course 2015Michelle LindsayÎncă nu există evaluări
- Advanced Practice in Critical Care: A Case Study ApproachDe la EverandAdvanced Practice in Critical Care: A Case Study ApproachSarah McGloinÎncă nu există evaluări
- Bonehead Electrocardiography: The Easiest and Best Way to Learn How to Read Electrocardiograms—No Bones About It!De la EverandBonehead Electrocardiography: The Easiest and Best Way to Learn How to Read Electrocardiograms—No Bones About It!Evaluare: 5 din 5 stele5/5 (2)
- EKG/ECG Interpretation Made Easy: A Practical Approach to Passing the ECG/EKG Portion of NCLEXDe la EverandEKG/ECG Interpretation Made Easy: A Practical Approach to Passing the ECG/EKG Portion of NCLEXEvaluare: 5 din 5 stele5/5 (2)
- Ward-based Critical Care: a guide for health professionalsDe la EverandWard-based Critical Care: a guide for health professionalsEvaluare: 4 din 5 stele4/5 (5)
- Schaum's Outline of Emergency Nursing: 242 Review QuestionsDe la EverandSchaum's Outline of Emergency Nursing: 242 Review QuestionsEvaluare: 4.5 din 5 stele4.5/5 (3)
- Emergency Department Resuscitation of the Critically Ill, 2nd Edition: A Crash Course in Critical CareDe la EverandEmergency Department Resuscitation of the Critically Ill, 2nd Edition: A Crash Course in Critical CareÎncă nu există evaluări
- CCRN EexamhandbookDocument30 paginiCCRN EexamhandbookBahaa Ahmad Assoud100% (2)
- 209 Pope, B. CCRN-PCCN-CMC Review Cardiac Part 1Document14 pagini209 Pope, B. CCRN-PCCN-CMC Review Cardiac Part 1peanant100% (1)
- Acid-Base WorksheetDocument2 paginiAcid-Base WorksheetMayer Rosenberg100% (18)
- Lesson 3 - Substance Use, Addictions, Mental Health, Stigma and Discrimination and in The WorkplaceDocument8 paginiLesson 3 - Substance Use, Addictions, Mental Health, Stigma and Discrimination and in The WorkplaceCala WritesÎncă nu există evaluări
- OS Pharmacy L III - IVDocument125 paginiOS Pharmacy L III - IVashagrie67% (3)
- NCP JourrnallldsdDocument17 paginiNCP JourrnallldsdCHRISTINE JOY. MOLINAÎncă nu există evaluări
- Hospital Outpatient Prospective Payment System 2019 Updates - Shared1Document112 paginiHospital Outpatient Prospective Payment System 2019 Updates - Shared1Nunya BiznesÎncă nu există evaluări
- Daftar Jurnal Kedokteran Internasional GratisDocument3 paginiDaftar Jurnal Kedokteran Internasional GratisdoktermutiaÎncă nu există evaluări
- Reflection Paper Pediatric Community-Acquired Pneumonia in The United StatesDocument2 paginiReflection Paper Pediatric Community-Acquired Pneumonia in The United StatesLecery Sophia WongÎncă nu există evaluări
- Family Laboratory For Medical Analysis: Test & SpecimenDocument1 paginăFamily Laboratory For Medical Analysis: Test & SpecimenMohamad BadranÎncă nu există evaluări
- ANMDocument13 paginiANMhiiihhhhhhhhÎncă nu există evaluări
- PhobiaDocument4 paginiPhobiaZeba QuadiriÎncă nu există evaluări
- An Approach To A Floppy InfantDocument33 paginiAn Approach To A Floppy InfantayunisallehÎncă nu există evaluări
- Patient Wellbeing Assessment and Recovery Plan - Children and AdolescentsDocument12 paginiPatient Wellbeing Assessment and Recovery Plan - Children and AdolescentsSyedaÎncă nu există evaluări
- On and Off Male Birth Control MethodsDocument2 paginiOn and Off Male Birth Control MethodsLeón L.PÎncă nu există evaluări
- Chorea 9Document35 paginiChorea 9sanjay kamineniÎncă nu există evaluări
- Wards and Departments in The Hospital NamingDocument4 paginiWards and Departments in The Hospital NamingSlebeww PetewÎncă nu există evaluări
- Icd9 Icd10 Reference SheetDocument1 paginăIcd9 Icd10 Reference Sheetapi-272182068Încă nu există evaluări
- Myofascial Pain Dysfunction Syndrome - A RevisitDocument9 paginiMyofascial Pain Dysfunction Syndrome - A RevisitRhea RejiÎncă nu există evaluări
- Pe 11 Quarter 3 Lesson 1Document17 paginiPe 11 Quarter 3 Lesson 1Donah Kate AlbaÎncă nu există evaluări
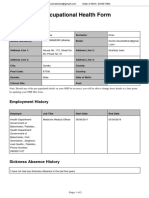
- Occupational Health Form: General DetailsDocument2 paginiOccupational Health Form: General DetailsKhushal khanÎncă nu există evaluări
- P1 RleDocument34 paginiP1 RleMary Jean GicaÎncă nu există evaluări
- Meningococcal Infection in ChildrenDocument6 paginiMeningococcal Infection in ChildrenAdrian KhomanÎncă nu există evaluări
- Data 14-12-2021 Formulir TB TerbaruDocument1 paginăData 14-12-2021 Formulir TB TerbaruAksaÎncă nu există evaluări
- Grand Case Presentation InformationDocument7 paginiGrand Case Presentation InformationCristina L. JaysonÎncă nu există evaluări
- Acadia PharmaceuticalsDocument3 paginiAcadia PharmaceuticalsAman DecoraterÎncă nu există evaluări
- Rachel Bray - ResumeDocument2 paginiRachel Bray - Resumeapi-625221885Încă nu există evaluări
- Improving VO2 Max Through ExerciseDocument1 paginăImproving VO2 Max Through ExercisecathyÎncă nu există evaluări
- Worksheet 4, Ubaidillah, 3BDocument6 paginiWorksheet 4, Ubaidillah, 3BUbay SegaÎncă nu există evaluări
- John Leung, MD: Have You Brought With You The Following?Document3 paginiJohn Leung, MD: Have You Brought With You The Following?Andres AÎncă nu există evaluări
- Bilateral OsteoarthritisDocument58 paginiBilateral OsteoarthritisMaya VilÎncă nu există evaluări
- Diabetes Jigsaw ActivitiesDocument11 paginiDiabetes Jigsaw ActivitiesJacqueline CullieÎncă nu există evaluări