Documente Academic
Documente Profesional
Documente Cultură
Balance Skeletal Traction. BST Procedure
Încărcat de
hannjazzDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Balance Skeletal Traction. BST Procedure
Încărcat de
hannjazzDrepturi de autor:
Formate disponibile
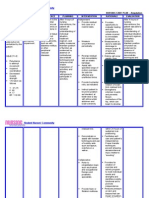
BALANCE SKELETAL TRACTION APPLICATION
Traction : is the act of pulling or drawing which is associated with counter traction. The pulling force is applied to a part of the body
while a counter traction pulls in the opposite direction. In straight or running traction coutertraction is supplied by the patient’s
body with the bed in one of the following positions;
1. Flat
2. Tilted away from the traction pull
3. Altered by elevating the head and / or knee gatch
THE PROCEDURE
I. Purpose and identification of traction
a. Purpose: used in the treatment or fractured extremities;
1. To lessen muscle spasm
2. To reduce fracture
3. To provide immobilization
4. To maintain alignment
5. To correct or prevent deformities in the case of arthritis patient with flexion contraction
6. To help lessen the curvature of the spine before correction surgery
b. Basic types of traction;
1. Skin traction
2. Skeletal traction
3. Manual traction
2. Check for Doctor’s Order
3. Identification of parts
a. Orthopedic bed/ Balkan frame
- 2 horizontal bars
- diagonal bar
- 4 vertical bars
- 3 pulleys
- Clamps
- Overhead trapeze
- Cross bar
- Firm mattress
- Fracture board
- Shock blocks / lock
b. BST equipments
- Thomas splint
- Pearson attachment
- Rest splint
- Cord/Sash
- Foot rest
- Safety pins/ paper clips
- Thigh rope(shortest)
- Suspension rope(longest)
- Traction rope(longer)
- Traction weight
- Suspension weight
4. Traction set-up
Prepared by: James M. Alo, R.N, MAN, MAPsycho, PhD, Page 1
a.
Thomas splint and pearson splint
1. Attach the rest splint to the Thomas splint with Pearson attachment
2. Upper part is the Thomas splint which will support the thigh and lower part is the Pearson attachment
that will support the leg.
3. Tie the short rope to the medial upright of the Thomas splint with slip-knot to ensure privacy to the
patient.
b. Application of slings to the Thomas splint and Pearson attachment.
1. Start from the large and wide slings (at least 2 pcs) to the Thomas splint and 3 slings smaller and
narrower to the Pearson attachment.
c. Principles of sling application
1. Smooth side should be touching the patient skin for comfort
2. At least 1 inch apart in between slings for ventilation
3. Not to tight not too loose to support the normal structure of the leg
4. Provide space at the popliteal and heel area to provide ventilation and prevent irritation.
5. Insertion of apparatus
a. Patient’s instructions
1. Instruct the patient to flex the unaffected leg and hold on the overhead trapeze bar
b. 3 manpower team
1. Apply manual traction (1st nurse) of the affected leg
2. In the count of 1,2, & 3 with the coordination in movement, simultaneously, 2nd nurse lifting the
affected leg and
3. 3rd nurse removing the Braun Bohler while inserting the assembled apparatus (Thomas splint, Pearson
attachment & rest splint).
6. Application of traction weight
a. Application of traction weight (10% of the body weight)
1. There should be continuous traction, so don’t remove the manual traction until kthe longer rope has
been tied to the steinman pin holder (club hitch knot/ eight knot), then insert the other end of the rope
to the third pulley to the traction weight(club hitch knot) and securely tied.
2. Check the groin part of the thigh if resting on the half ring to promote comfort.
b. Application of suspension weight (50% of the traction weight)
1. Tie first the other end of the short rope on the lateral aspect of the Thomas splint.
2. Tie the longest rope to the middle of the short rope with slip knot.
3. Insert the other end of the rope to the first pulley, passing through the hanged suspension weight, to
the 2nd pulley
4. Prior in tying the rope make it sure the rope is inside thetraction rope for support and prevent the
affected leg from swaying sideways. Then tie to the Thomas splint using clove hitch knot then to the
Pearson attachment.
5. Release the suspension weight
c. Removal of the rest splint
d. Applying of foot support
1. You may start applying ribbon knot at the lateral and medial side of the Thomas splint, then to Pearson
attachment.
7. Checking efficiency of traction
a. Principles of Skeletal Traction
1. Have an opposite pull or counter traction.
2. The application of shock block or lock and weight of the patient serve as the counter traction .
3. Line of pull should be in line with the deformity. The 1st pulley should be in line with the groin. The 2nd
pulley should be in line with the knee, and traction line should be straight with the deformity.
4. Traction should be continuous and weights should be hanging freely.
Prepared by: James M. Alo, R.N, MAN, MAPsycho, PhD, Page 2
5.
The position of the patient should be in dorsal recumbent or supine position .
6.
It should be free from friction;
- Weights should be hanging freely.
- Observe for signs of wear and tear on the ropes and bags.
- Ropes should run freely along the grove of the pulley.
- Knots should be away from the pulley.
8. Transport/removal of traction ( what is being 1st assembled should be the last to remove);
a. Attach the rest splint,
b. Anchor the suspension weight,
c. Remove the suspension rope,
d. Apply manual traction,
e. Remove traction weight, then tie the rope to the rest splint, Thomas and Pearson using the clove hitch knot
f. Patient is ready for transfer to the stretcher, and
g. Instruct the patient to flex his unaffected leg while holding on the trapeze bar and simultaneously helping the
patient transfer to the stretcher.
9. Nursing care to patient in traction
a. Should be free from any of the following;
1. Impaired circulation of the extremeties,
2. Respiratory distress,
3. Emphasize good condition of the skin particularly at ischial, sacral, poplitieal, dorsum of foot, and heel
part,
4. Contracture of joint like footdrop
5. Signs of infection;
- Assess skin integrity
- Traction pin site dressing regularly
- Monitor for temperature, color, odor of the affected part.
b. Should have bone alignment and position of extremity in which the purpose of traction should be accomplished.
c. Provide patient’s comfort such as;
1. Traction should never be a source of undue discomforrt,
2. Care of the skin, mouth, hair, nails, toes, and genitals should be included in the plan of daily care.
d. Provide exercises such as;
1. ROM exercise of all the unaffected joints
2. Static quadriceps exercises,
3. Flexion and extension of the toes and fingers in traction.
e. Provide supportive therapy
f. Monitor the nutritional status of the patient
g. Complaint of the patient should be assess
h. Check the traction set-up if;
1. The apparatus is accomplishing each purpose of traction,
2. The equiments are safe as possible,
3. Sash, cords and pulleys is unobstructed,
4. Knots, clamps, and weighs are secured, and
5. Weights are free from any friction,
10. What are the complications to patient with traction?
a. Fat embolism
1. Patient with long bone fracture is prone like; tibia, fibula, radius, ulna, femur, and humerus. Fatty
globules from the bone goes to the lungs and usually occurs within 48 hours.
2. Signs/symptoms: restlessness, altered LOC, tachycardia, tachypnea, BP, petichial rash over the upper
chest/neck.
Prepared by: James M. Alo, R.N, MAN, MAPsycho, PhD, Page 3
3. Nursing consideration: inform the doctor.
b.
Compartment syndrome
1. Increase pressure within one or more compartment causing massive compromise circulation, leading to
tissue perfusion anoxia. This is w/n 4-6 hrs pc the onset neurovascular damage F irriversible.
2. Sx/Sy: pain & swelling, pain unrelieved by analgesic, distal pulse, & loss of sensation.
3. Nsg consideration: Assess VS, & notify the doctor.
c. Infection/ osteomyelitis
1. Is an acute/chronic inflammatory process of the bone and its structures secondary to infection with
pyogenic organisms.
2. Sx/Sy: fever, pain, edema, warmth, tender, reduction in the use of extremity, WBC & pulse.
3. Nsg consideration: Assess, notify the doctor.
d. Avascular necrosis
1. Interruption of the blood supply to the bone tissue bone death.
2. Sx/Sy: pain & sensation
3. Nsg consideration: assess & notify doctor
11. What are the possible nursing diagnosis?
a. Pain
b. Highrisk for infection
c. Impaired physical mobility
d. High risk for skin integrity
e. High risk for injury
f. High risk for altered tissue perfusion
g. High risk for self-esteem disturbance
Prepared by: James M. Alo, R.N, MAN, MAPsycho, PhD, Page 4
S-ar putea să vă placă și
- Pathophysiology of OsteosarcomaDocument5 paginiPathophysiology of Osteosarcomafanvicfay100% (9)
- Cast and TractionsDocument6 paginiCast and Tractionsmiss RN100% (12)
- Pathophysiology OsteosarcomaDocument4 paginiPathophysiology OsteosarcomaGladys Barcelona0% (1)
- Gray Cook & Brett Jones - Kettlebells From The Center Dynami - Manual (2010)Document104 paginiGray Cook & Brett Jones - Kettlebells From The Center Dynami - Manual (2010)ilya neviditsin100% (2)
- BST Traction TechniqueDocument5 paginiBST Traction Techniquebimbong120% (1)
- BST Skeletal Traction Procedure and Nursing CareDocument4 paginiBST Skeletal Traction Procedure and Nursing CareIris BalinoÎncă nu există evaluări
- Balanced Suspension Skeletal TractionDocument4 paginiBalanced Suspension Skeletal Tractionfegerilene100% (1)
- Traction TechniquesDocument12 paginiTraction TechniquesJolo Q. Bilaos67% (3)
- Setting up a Balance Skeletal TractionDocument6 paginiSetting up a Balance Skeletal Tractionandrea villanuevaÎncă nu există evaluări
- Spinal Cord Injury NCPDocument2 paginiSpinal Cord Injury NCPEmmanuelRodriguez100% (1)
- NCP OrthoDocument5 paginiNCP OrthoMyluck Elaine Wailan100% (4)
- Orthopedic NursingDocument9 paginiOrthopedic Nursingsilimaanghang100% (2)
- Herniated Nucleus PulposusDocument41 paginiHerniated Nucleus PulposusMichael John F. Natividad100% (1)
- Cast Care GuideDocument12 paginiCast Care GuidesuperduperfriendshipÎncă nu există evaluări
- Nursing Care Plan: West Visayas State University College of NursingDocument4 paginiNursing Care Plan: West Visayas State University College of NursingLizaEllaga100% (1)
- POC NotesDocument3 paginiPOC NotesJosef SuenoÎncă nu există evaluări
- BST ChecklistDocument3 paginiBST ChecklistBailey100% (1)
- TRX Quick Start ManualDocument15 paginiTRX Quick Start ManuallancillottoÎncă nu există evaluări
- Clinical Focus SampleDocument2 paginiClinical Focus Samplehannjazz100% (5)
- 7 - 10 Minutes Yoga Nidra ScriptDocument3 pagini7 - 10 Minutes Yoga Nidra ScriptJeyashankar RamakrishnanÎncă nu există evaluări
- Iyengar YogaDocument38 paginiIyengar YogaYoga Avec Nathalie100% (1)
- 2.balance Skeletal TractionDocument18 pagini2.balance Skeletal TractionKatrina Ponce75% (4)
- Khaye:: Traction: Is The Act of Pulling or Drawing Which Is Associated With Counter TractionDocument4 paginiKhaye:: Traction: Is The Act of Pulling or Drawing Which Is Associated With Counter TractionChloe MorningstarÎncă nu există evaluări
- Balanced Skeletal TractionDocument4 paginiBalanced Skeletal TractionOshin Tibangwa Wagayen100% (2)
- Balance Skeletal TractionDocument7 paginiBalance Skeletal TractionNina Ann LiwanagÎncă nu există evaluări
- Ortho GadgetsDocument18 paginiOrtho Gadgetsmckulit_joey100% (3)
- Balanced Suspension Skeletal TractionDocument4 paginiBalanced Suspension Skeletal TractionPrince Rener Velasco Pera100% (1)
- Orthopedic Nursing LectureDocument34 paginiOrthopedic Nursing Lecturesjardio100% (2)
- Orthopedic Nursing. Lecture Notes at Philipine Orthopedic CenterDocument7 paginiOrthopedic Nursing. Lecture Notes at Philipine Orthopedic Centerhannjazz100% (5)
- Types of Traction for Bone and Spine InjuriesDocument3 paginiTypes of Traction for Bone and Spine Injuriessophia yemaneÎncă nu există evaluări
- CAST TYPES AND INDICATIONSDocument4 paginiCAST TYPES AND INDICATIONSCharisse CamantigueÎncă nu există evaluări
- NCP - OsteosarcomaDocument5 paginiNCP - OsteosarcomaNelson Lacsamana100% (1)
- NCP: FracturesDocument21 paginiNCP: FracturesJavie100% (1)
- Pathophysiology Bone Fracture (Tibia)Document1 paginăPathophysiology Bone Fracture (Tibia)Brainan Aquino0% (2)
- Braces Ortho..Document16 paginiBraces Ortho..karendelarosa062770% (1)
- Poc Pott's DiseaseDocument8 paginiPoc Pott's Diseasealsbeth50% (4)
- NCP BkaDocument4 paginiNCP BkaKeeshia CesnerosÎncă nu există evaluări
- Cast and TractionsDocument3 paginiCast and TractionsMacaRonie PepeRownie del RioÎncă nu există evaluări
- Casts. Braces. TractionDocument3 paginiCasts. Braces. TractionClancy Anne Garcia Naval100% (1)
- Nursing Care Plan Orthopedic Philipine CenterDocument4 paginiNursing Care Plan Orthopedic Philipine CenterAnonymous NZTQVgjaÎncă nu există evaluări
- Orthopedic EquipmentsDocument64 paginiOrthopedic EquipmentsJasmin Jacob100% (8)
- NCP Impaired Physical MobilityDocument2 paginiNCP Impaired Physical MobilityJohn Michael FernandezÎncă nu există evaluări
- AmputationDocument2 paginiAmputationFabian Ugalino Pino Jr.100% (3)
- Orthopedic Nursing Orthopedic Gadget-A Piece of Special Device Designed To Correct Deformoities or To PreserveDocument5 paginiOrthopedic Nursing Orthopedic Gadget-A Piece of Special Device Designed To Correct Deformoities or To PreserveSophia Kaye AguinaldoÎncă nu există evaluări
- Orthopedic HardwareDocument27 paginiOrthopedic HardwareJasmin Jacob100% (3)
- POC - Review NotesDocument9 paginiPOC - Review NotesSTEFFI GABRIELLE GOLEZÎncă nu există evaluări
- Philippine Orthopedic Center Lecture NotesDocument7 paginiPhilippine Orthopedic Center Lecture Notesxteovisio100% (2)
- Orthopedic HardwareDocument36 paginiOrthopedic HardwareMarivic Diano100% (1)
- Scolio NCPDocument3 paginiScolio NCPkevinluisa1850% (4)
- Orthopedic Nursing: TractionDocument2 paginiOrthopedic Nursing: TractionGhee EvangelistaÎncă nu există evaluări
- Balance Skeletal TractionDocument5 paginiBalance Skeletal TractionRachel Ann JimenezÎncă nu există evaluări
- Return Demo FormatDocument4 paginiReturn Demo Formatfamy15Încă nu există evaluări
- BST Skeletal Traction SetupDocument6 paginiBST Skeletal Traction SetupAia JavierÎncă nu există evaluări
- Orthopedic NursingDocument2 paginiOrthopedic NursingMichelle TamorÎncă nu există evaluări
- Procedure for applying balanced skeletal tractionDocument3 paginiProcedure for applying balanced skeletal tractionJuliene Hannah FloresÎncă nu există evaluări
- The Balanced Skeletal TractionDocument1 paginăThe Balanced Skeletal TractionGemarie Adarlo CastilloÎncă nu există evaluări
- BST ChecklistDocument3 paginiBST ChecklistAlthea TuguinayÎncă nu există evaluări
- Lower Extremity Traction TechniquesDocument22 paginiLower Extremity Traction TechniquesJo-Anne Karen SerdeñaÎncă nu există evaluări
- Ortho LecDocument7 paginiOrtho LecKemmy GarciaÎncă nu există evaluări
- Taping Reference Sheet-3815621Document3 paginiTaping Reference Sheet-3815621api-383568582Încă nu există evaluări
- Application Balanced Skeletal TractionDocument6 paginiApplication Balanced Skeletal TractionLorenz ChristopherÎncă nu există evaluări
- TractionDocument19 paginiTractionNikko Melencion0% (1)
- TractionDocument11 paginiTractionDenalyn Ann TormoÎncă nu există evaluări
- Assistive Devices For Walking, Casts, and Traction CareDocument7 paginiAssistive Devices For Walking, Casts, and Traction Careアンナドミニク100% (1)
- This Will Be A Good Resource For Psychiatric Nursing ReviewerDocument1 paginăThis Will Be A Good Resource For Psychiatric Nursing ReviewerhannjazzÎncă nu există evaluări
- NSG Theories & ResearchDocument5 paginiNSG Theories & ResearchhannjazzÎncă nu există evaluări
- Psychiatric NSGDocument186 paginiPsychiatric NSGhannjazzÎncă nu există evaluări
- Psychiatric NSGDocument186 paginiPsychiatric NSGhannjazzÎncă nu există evaluări
- Clinical Evaluation of The Psychiatric PatientDocument4 paginiClinical Evaluation of The Psychiatric Patienthannjazz100% (1)
- Orthopedic Nursing. Lecture Notes at Philipine Orthopedic CenterDocument7 paginiOrthopedic Nursing. Lecture Notes at Philipine Orthopedic Centerhannjazz100% (5)
- Exercise Booklet for Ankle and Leg StrengtheningDocument19 paginiExercise Booklet for Ankle and Leg StrengtheningMiss M.Încă nu există evaluări
- Infant Tub BathDocument47 paginiInfant Tub BathMay Chelle ErazoÎncă nu există evaluări
- Neurological AssessmentDocument7 paginiNeurological AssessmentSharon LawrenceÎncă nu există evaluări
- Understanding Body Parts Through Physical ActivityDocument11 paginiUnderstanding Body Parts Through Physical ActivityMD BadillaÎncă nu există evaluări
- Physical Education and Health 4: Deped Physical Fitness TestDocument17 paginiPhysical Education and Health 4: Deped Physical Fitness TestPrances PelobelloÎncă nu există evaluări
- Correct Mark 1.00 Out of 1.00: LocomotorDocument7 paginiCorrect Mark 1.00 Out of 1.00: Locomotorspinel sunÎncă nu există evaluări
- Conditioning and Warm Up ProgramDocument23 paginiConditioning and Warm Up ProgramJeneyse Ajap BalcenaÎncă nu există evaluări
- FitSimplifyResistanceTubeBandEbook PDFDocument35 paginiFitSimplifyResistanceTubeBandEbook PDFAnthony DinicolantonioÎncă nu există evaluări
- Limb Length DiscrepancyDocument75 paginiLimb Length DiscrepancyDavidBeatonComuladaÎncă nu există evaluări
- Athletes Foot - PresentationDocument6 paginiAthletes Foot - PresentationCitha HoffÎncă nu există evaluări
- Foot Reflexology: We Recommend That You Allocate at Least 30 Minutes To This WorksheetDocument5 paginiFoot Reflexology: We Recommend That You Allocate at Least 30 Minutes To This WorksheetAstro TriinityÎncă nu există evaluări
- 4.3 - Educating Patients, Family, and Health Care Professionals About Foot CareDocument1 pagină4.3 - Educating Patients, Family, and Health Care Professionals About Foot CareEva Cica SusantiÎncă nu există evaluări
- Core Flexibility-Static and Dynamic Stretches For The CoreDocument3 paginiCore Flexibility-Static and Dynamic Stretches For The CoreMagno FilhoÎncă nu există evaluări
- HHMDDocument7 paginiHHMDSrikanth KrishnamurthyÎncă nu există evaluări
- Reformer Mat3Document66 paginiReformer Mat3Suat Barut100% (1)
- Idiopathic Toe Walking A Kinematic and Kinetic ProfileDocument8 paginiIdiopathic Toe Walking A Kinematic and Kinetic Profileyarimar hoyosÎncă nu există evaluări
- Neurologic Objective Structured Clinical EvaluationDocument4 paginiNeurologic Objective Structured Clinical EvaluationKendall Marie BuenavistaÎncă nu există evaluări
- Lower Limb Trauma: Cast Application For Common FracturesDocument58 paginiLower Limb Trauma: Cast Application For Common FracturesdrusmanjamilhcmdÎncă nu există evaluări
- Tone Up Real Fast With These 22 Yoga PosesDocument16 paginiTone Up Real Fast With These 22 Yoga PosesMukesh VÎncă nu există evaluări
- Dark Blue and Orange Fitness Gym Trifold BrochureDocument4 paginiDark Blue and Orange Fitness Gym Trifold BrochureKavya PandyaÎncă nu există evaluări
- Keiser PerformanceDocument22 paginiKeiser PerformanceВиталий БартулёвÎncă nu există evaluări
- PresjurDocument18 paginiPresjurIhsanÎncă nu există evaluări
- Scaffold Inspection Form: General Rules For All Scaffolds YES NO N/ADocument1 paginăScaffold Inspection Form: General Rules For All Scaffolds YES NO N/Areja fahleza100% (1)
- Blast Fat With 12-Minute HIIT WorkoutsDocument17 paginiBlast Fat With 12-Minute HIIT WorkoutsdeluxÎncă nu există evaluări
- Rodgers Mfa 2018Document1 paginăRodgers Mfa 2018SharmilaÎncă nu există evaluări
- Neck ExercisesDocument2 paginiNeck Exercisesdong fuxiongÎncă nu există evaluări
- Pe-8 Q4 W8 V4Document8 paginiPe-8 Q4 W8 V4Ericzon SantosÎncă nu există evaluări