Documente Academic
Documente Profesional
Documente Cultură
Chapter 6 - Immune Diseases (Part I) (Robbins and Cotran Pathologic Basis of Disease)
Încărcat de
Ernie G. Bautista II, RN, MDDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Chapter 6 - Immune Diseases (Part I) (Robbins and Cotran Pathologic Basis of Disease)
Încărcat de
Ernie G. Bautista II, RN, MDDrepturi de autor:
Formate disponibile
Immunity
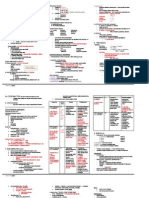
General Features of Immune System Deficiency infections, tumor Hyperactive fatal disease Autoimmunity - immune reaction against own tissues & cells Two Mechanisms of Immunity 1. Innate immunity 2. Adaptive immunity Innate Immunity natural, native immunity defense mechanism that are present even before infection first line of defense Skin/epithelial barriers, phagocytic cells, natural killer cells, plasma proteins 2 most imp cellular rxn Inflammation Phagocytic cells Antiviral defense Dentritic & NK cells Adaptive Immunity acquired, specific immunity mechanisms that are stimulated by microbes and capable of recognizing non microbial substances (Ags) develop later after exposure to microbes more powerful immune response Consists of lymphocytes and their (ex. Antibodies) Can be: cellular or humoral immunity 1. Cell Mediated or Cellular Immunity against intracellular and extracellular microbes, parasites and ab normal cells mediated by T lymphocytes 2. Humoral Immunity against extracellular microbes & toxins mediated by B lymphocytes (Immunoglobulin) Cells of immune system Lymphocytes CD4 + T4 & C8 + T8 Nave lymphocytes immunologically inexperienced Effector cells eliminates microbes Memory cells With Previous exposure With Heightened awareness
Cells and Tissues of the Immune System T lymphocytes B lymphocytes Macrophages Dendritic cells Natural killer cells T lymphocytes From BM stem cells Maturation in thymus Found 60-70% in blood and T cell zones (paracortical/ parafollicular area) Recognize by peptides presented by MHC of Antigen presenting cells express receptors for chemokines recognizes spec. cell bound Ag by TCR cannot be activated by soluble Ags presentation of Ag is required B lymphocytes From BM precursors Found 10-20% in blood recognizes Ag thru B-cell Ag receptor complex IgM & IgD -Ag binding component form plasma cells that secrete Igs requires help of CD4+ Tcells Stimulated by Ags and other signals Plasma cells Immunoglobulin production Monodimer IgD, E, G Dimer IgA Pentamer IgM (biggest & has more binding site) Macrophages Function as APCs in T cell activation Key effector cell -- in Cell med. immunity Involved in effector phase -- in humoral immunity role in induction of cell mediated immunity role as effector cells in cell mediated immunity eg. delayed hypersensitivity role in effector phase of immunity Dendritic cells Aka: Interdigitating DC Most important APC Located under epithelia and interstitial Langerhans cells (note langhans a macrophage) An immature dendritic cells Found in skin Follicular dendritic cells Found in germinal centers of lymphoid tissues
Has Fc receptors for IgG & receptors for C3b
Natural killer cells AKA: large granular lymphocytes 10-15% of blood lymphos w/ abundant azurophilic granules innate ability to kill w/o previous sensitization to Ags tumor cells, virally infected cells, some normal cells part of innate immune system CD 16 & CD 56 (+) Ab dependent cell mediated cytotoxicity Fxn balanced by activating/inhibiting receptors Secrete Cytokine ex: IFN-gamma Tissues of the Immunes System Generative lymphoid organs Thymus (Primary) and BM Peripheral lymphoid organs LN, spleen, mucosal & cutaneous lymphoid tissues, mucosal associated lymphoid tissue (MALT) Lymphocyte recirculation More on T cells B cells stay; antibody circulates T cells T cell zone (LN) Ag from APC activation circulation Target microbes/ tissues
Structure and Function of Histocompatibility Complex (MHC) molecules Important in the antigen recognition by Tcells Associated with many autoimmune disease (ex. In the case of allografts) Products of genes that evoke rejection of transplanted organs bind peptide fragments of foreign CHONs for presentation to Ag specific receptors chromosome 6 major histocompatibility complex (MHC) or human leukocyte antigen (HLA) occur in 2 forms: class I class II MHC locus has genes that encodes: Complement components TNF Lymphotoxin Class I MHC Imp in Ag recognition by T cells Display peptide fragments of CHON to recognized by Ag Spec T cells Expressed on all nucleated cells & platelets Composed of polymorphic heavy chain glycoprotein encoded in the following: HLA-A, HLA-B, HLA-C Bind peptides derived from endogenous CHONs Ex. Viral antigen in the cytoplasm & present to and recognized by CD8+ cytotoxic T cells Class II MHC Confined to APCs, including: Dendritic cells Macrophage B-cells Activated T-cells Noncovalently associated with alpha- & beta- chains coded in HLA-D with 3 defined subloci DP, DQ, DR Bind peptides derived from exogenous CHONs & present to CD4+ helper T lymphocytes
Cytokines Messenger molecules of immune system A short acting soluble mediators Example: Interleukins Secreted in bursts similar to mediators Regulate lymphocyte growth Activate inflammatory cells Mediate innate immunity IL-1, IL-12, TNF, type I interferons, chemokines, IFN gamma Adaptive responses IL-2,4,5,17. IFN-gamma Stimulate hematopoiesis CSFs colony stimulating factors
Prepared by: EGBII; 8-13-11
HLA and Disease association 1. Inflammatory diseases HLA-B27 associated eg. Ankylosing spondylitis 2. Inherited errors of metabolism HLA-BW47 - 21 hydroxylase disease HLA-A - hereditary hemochromatosis 3. Autoimmune diseases DR locus- AA endocrinopathies
Maybe in state of shock w/in mins (anaphylactic shock)
B. Local Exemplified by atopic allergies 1. Immediate or initial phase 5-30 mins after exposure Primary mast cell mediators resp. for initial phase Includes o Biogenic amines (histamine) o Chemotactic mediators (eosinophil & neutrophil) o Enzymes (chymase & tryptase) Late phase 2-24 hours after initial allergen exposure Driven by lipid mediators & cytokines o Produces by mast cells Lipid mediators include o LT-B4,C4,D4,E4 o Prostaglandin D2 o PAF Cytokines include o TNF-a o Interleukines o GM-CSF o Chemokines
Basophils similar to mast cells found in the circulation can be recruited to inflammatory sites TH2 cells Initiation & propagation IL-4 B cells switch to IgE & TH2 production (autocrine) Promotes inflammation Eosinophils Important in late phase Recruited by chemokines IL-5 most potent eosinophil activating cytokine Liberate: o Proteolytic enzymes o Major basic proteins o Eosinophilic cationic protein IMMEDIATE HYPERSENSITIVITY Susceptibility is genetically determined Basis not clear/ hereditary predisposition in o CHROMOSOME 5q31 & 6p Where genes for TH2 are located ATOPY predisposition to develop localized immediate hypersensitivity NON-ATOPIC ALLERGY o Triggered by extreme temperature & exercise o NO TH2 cells nor IgE involved
LOCAL IMMEDIATE HYPERSENSITIVITY Allergic reactions Atopic allergy Diseases: o Bronchial asthma o Angioedema o Allergic rhinitis o Urticarial/ pruritus o Inhaled or ingested Preformed mediators/ Primary mediators: Found in initial response 1. Biogenic amines (eg. Histamine) 2. Enzymes (eg. Neutral proteases, acid hydrolases) 3. Proteoglycans (eg. Heparin, chondroitin sulfate) Lipid mediators/ Secondary mediators: 1. Lipids mediators 1. Syn in mast cell membrane 2. Activates phospholipase A2 3. Leukotrienes 4. Prostoglandin D2 P 5. Platelet activating factor Leukotrienes o C4 & D4 most potent (than histamine) vasoactive & spasmogenic agents o B4 chemotatic for neutrophils, eosinophils and monocytes Prostaglandin D2 o most abundant mediator from cyclooxygenase pathway o intense bronchospasm o increased mucus secretion Platelet Activating Factor o platelet aggregation o histamine release o bronchospasm o increased vascular permeability o vasodilation o Chemotactic for neutrophils and eosinophils 2. Cytokines Many are from mast cells o TNF, IL-1,4, chemokines
Hypersensitivity
MECHANISM OF HYPERSENSITIVITY REACTIONS Altered reaction nd 2 exposure Exogenous and endogenous antigens may be triggered hypersensitivity rxns Often associated w/inheritance of susceptibility genes Imbalance between effector mechnisms of immune responses and control mechanisms TYPES 1. Immediate hypersensitivity (type I) 2. Antibody-mediated (type II) 3. Immune complex mediated (type III) 4. Cell mediated (type IV) Immediate Hypersensitivity (Type I) rapid immunologic reaction (w/in mins.) after combination of Ag with Ab bound to mast cells of previous sensitized individuals most mediated by IgE antibodies release of vasogenic, spasmogenic subst., cytokines (recruitment of inflam. cells) Usually, Allergy Most mediated by TH2m IgE ab, & mast cells Release of mediators & pro inflammatory cytokines Synthesis of IgE requires induction of CD4+ helper T cells of TH2 type (w/c produce multiple cytokines) IL-4 produced by TH2 cells is essential for IgE synthesus IL-3, 5, GM-CSF promotes production & survival of eosinophils
2.
Primary mediators/ degranulation contents .Histamine .Protease .Chemotactic factors; ECF &NCF
Secondary mediators/ membrane phospholipids .Leukotrienes B,C,D4 .Prostaglandin-D2 .PAF
A. Systemic Usually follows injection of Ag (parenteral or oral administration) skin testing done to lower occurance
Masts cells BM derived near b.v., nerves, subepithelium have cytoplasmic membrane bound basophilic granules containing mediatiors IgE Fc receptors where the allergen normally bound
SYSTEMIC ANAPHYLAXIS Vascular shock, edema, difficulty of breathing May go into shock Ex: penicillin, food allergies, insect IV or oral
Different types of hypersensitivity Disease Ag involved Manifestations SLE PGN Nuclear Ag Strep. Cell wall Ag Nephritis, skin lesion, arthritis Nephritis
Prepared by: EGBII; 8-13-11
PAN (polyarthritis nodosa) Reactive arthritis Arthur reaction
Hep.B virus antigen in some Bacterial Ag
Systemic vasculitis Arthritis, vaasculitis, nephritis Cutaneous vasculitis
Various foreign proteins
Antibody Mediated Hypersensitivity (Type II) Mediated by Abs directed toward Antigens on cell surfaces or extracellular matrix (3) mechanisms o Opsonization & Phagocytosis o Complement and Fc mediated Inflammation o Antibody-Mediated Cellular Dysfunction Cells opsonized by IgG Ab are recognized by phagocyte Fc receptors Phagocytosis and destruction of opsonzied cell follows Activation of complement also occurs Formation of membrane attack complex (MAC) C5b-C9 cell lysis Classical, alternative, lectin pathways 1.OPSONIZATION & PHAGOCYTOSIS Transfusion reaction (type A patient transfused with type B blood) Erythroblastosis fetalis(HDN) o Rh Ag of baby + anti-Rh of mother autoimmune hemolytic anemia agranulocytosis thrombocytopenia drug reactions Ab Dependent cellular w/o phagocytosis can occur by nonsensitized cells bearing Fc receptors called ADCC or by natural killer cells Ex. NK cells, IgG or IgE 2.COMPLEMENT & Fc RECEPTOR MEDIATED INFLAMMATION Abs deposit into fixed tissues, injuries is due to inflammation Complement is activated (C3a, C5a) Fc receptor involvement Ex. o Glomerulonephritis o Vascular rejection
3.ANTIBODY MEDIATED CELLULAR DYSFUNCTION Impairment/ dysregulate function NO cell injury, NO inflammation o Compared to ADCC & opsonization NO tissue damage Only activate or block normal cellular or hormonal function Example: o Myasthenia gravis o Pemphigus vulgaris o Graves disease *memorize each examples Immune Complex Mediated Hypersensitivity (Type III) Mediated by Ag-Ab complexes immune complexes Forming either in the circulation or at site of Ag deposition Enhanced by increased vascular permeability resulting from inflammation Cell activation by immune complex binding to Fc/ C3b receptors tissue damage by inflammation at the site of deposition of the immune complex (IC) Ag-Ab w/in circulation (circulating immune complex) deposited in vessel walls o Releases vasoactive mediators + cytokines Some at extravascular sites (in situ IC) 2 types of Ag: o exogenous o endogenous 2 types of type 3: o Generalized/ Systemic o Localized
IC & complement can be visualized by: IMMUNOFLUORECENCE microscopy o Granular fluorescence exogenous o Linear fluorescence endogenous Ie. Glomerular basement membrane Immune Complex Mediated Hypersensitivity (Type IV) Initiated specifically by sensitized Tlymphocytes Initiated by antigen activated Tlymphocytes o DELAYED type CD4+ T cells with few CD8+ Only stimulate inflammation & activate phagocytosis o DIRECT cell toxicity CD8+ T cells Directly kill tissue cell DELAYED type (CD4+) principal pattern to: *Granulomatous diseases o *myocobacterium, fungi o TB skin test sensitivity o Transplant rejection/ allograft rejection o Contact dermatitis Causing granuloma: o Macrophage activation o Inflammation o Tissue injury CYTOTOXIC T-LYMPHOCYTE (CTL) mediated (CD8+) involved in: Neoplastic cell lysis Transplant rejection/ allograft Virus infected cells (hepatitis) Type 1 DM CTL mediated by perforin-granzyme & Fas-FasL pathways including apoptosis
Autoimmune Diseases
Immune reactions against self-Ags 3 requirements: 1. presence of autoimmune reaction 2. reaction is not secondary to tissue damage 3. Absence of another well defined cause of dse. From tissue injury caused by T cells or Abs reacting to self-Ags types: >organ specific >generalized or systemic TOLERANCE lack of reaction to self antigens AUTOIMMUNE DSE. loss of self tolerance IMMUNOLOGICAL TOLERANCE o Phenomenon of unresponsiveness to an antigen as a result to exposure of lymphocytes to that antigen SELF TOLERANCE unresponsiveness to an individuals own antigen and can be: o CENTRA tolerance o PERIPHERAL tolerance
SYSTEMIC/ GENERALIZED Circulating IC that are systemically deposited Ex: GN Vasculitis Serum sickness o Results from recruitment or prolonged antigen exposure & ongoing IC deposition = there is thickening of intimal layer LOCALIZED Arthus reaction o Characterized by localized tissue vasculitis with necrosis
*Transplant rejection can be both delayed & direct
CENTRAL TOLERANCE death of self reactive T & B lymphocyte clones during their maturation in lymphoid organs (in thymus & BM) THYMUS o Immature T cells w/TCRs encounters by Ag and die by apoptosis by: o Negative selection or deletion AIRE (autoimmune regulator) o Required for the development of T cell tolerance o Stimulates expression of some peripheral tissue restricted antigen o Is critical for deletion of immature T cells specific for the antigens o Mutation in this gene leads to autoimmune polyendocrinopathy BONE MARROW o B cells receptor editing renders B cell NOT to be specific for self antigen o Apoptosis happens if receptor editing does not occur Many self reactive T/B cell escape this.
Prepared by: EGBII; 8-13-11
PERIPHERAL TOLERANCE Autoreactive T cells that escape thymic deletion can be inactivated in the periphery via the following mechanisms: o Anergy o Suppression by regulatory T cells o Deletion by activation induced cell death o Antigen sequestration ANERGY o Prolong or irreversible inactivation of lymphocytes o Occur when they recognize selfantigen in the absence of necessary costimulatory signals from normal parenchymal cells SUPPRESSION BY REGULATORY TCELLS o Develop in thymus or induced in periphery o Can be identified by expression of: CD4 Alpha-chain of IL-2 (CD25) Transcription factor (Foxp3) o May inhibit lymphocyte activation by secreting cytokines (IL-10 & TGF-beta) o Mutation in Foxp3 causes severe autoimmunity: Immune dysregulation Polyendocrinopathy Enteropathy X-linked (IPEX) DELETION BY ACTIVATION-INDUCED CELL DEATH o CD4 + T cells o Undergo apoptosis ANTIGEN SEQUESTRATION o Immune privileged sites (brain, eye, testis) sequesters tissue antigens across a relatively impermeable blood tissue barrier o Because some antigens are hidden from the immune system MECHANISMS OF AUTOIMMUNE DISEASES Helper T cells control both cellular & humoral immunity Helper T cells tolerance critical for prevention of autoimmune diseases Multiple pathways allow tolerance to be bypassed involving some combination of: o Susceptibility genes and
Environmental triggers
Inheritance of susceptibility genes Contributes to the breakdown of self tolerance Most autoimmune disease are complex multigenic disorders HLA genes are highly associated (not the cause) with autoimmune diseases Enviromental triggers Associated with infections Also promote activation of self-reactive lymphocytes Mechanisms: o Up-regulate co-stimulators on APC & overcome peripheral tolerance o Infections might break tolerance by Molecular mimicry self Ags (rheumatic heart disease) o Infectious agents share epitopes with self-antigens GENERAL FEATURES Progressive & persistent o Manifest by epitope sharing* because immune response spreads to determinants that were not initially recognized Manifestations are determined by nature of underlying response Different autoimmune dses show overlaps (clinical, pathologic, serologic) AUTOIMUNE DISEASES Single organ 2-3 organs RA Sjogren Hashimotos
1% of world population suffers from RA Women are 3x affected than men Peak prevalence: 20s 30s There is familial association & link with HLA-DR4 or DR1 PATHOGENESIS:
Initiation of arthritogenic antigen (microbial agent) Loss of self-tolerance CD4+ T cell activation Releasing Cytokines & Inflammatory mediators (esp.IL-1 & TNF-a) Pannus formation or exuberant synovium Joint destruction
Dry eyes (corneal inflammation, erosion, ulceration) Dry & crusted nose, nasal septum perforation Dry mouth (oral mucosa atrophy with fissures & ulcers) *Mikulicz syndrome: o Lacrimal & salivary gland enlargement from any cause o Ex; sarcoidosis, leukemia, lymphoma, & other tumors Biopsy of the lip essential for diagnosis to examine minor salivary glands
SYSTEMIC LUPUS ERYTHEMATOSUS
Prototype of multisystem disease of autoimmune origin acute or insidious onset chronic, remitting, relapsing, febrile illness Characterized by injury to skin, joints, kidney, serosal membranes (polyserositis) Predominantly females F:M = 9:1 Age incidence: 20-30s Unknown etiology Failure of mechanisms that maintains selftolerance (+) numerous autoantibodies, esp. ANA (hallmark*) ANA (anti-nuclear antibodies) reveals: o 1. Abs to DNA o 2. Abs to histones o 3. Abs to non-histones bound to RNA o 4. Abs to nucleolar Ags *these are detected in indirect immunofluorescence Four basic patterns of nuclear fluorescence: o 1. Homogenous/diffuse o 2. Rim/peripheral o 3. Speckled o 4. Nucleolar HOMOGENOUS/ DIFFUSE o Abs to: Chromatin Double stranded DNA Histones RIM/ PERIPHERAL o Anti double stranded DNA SPECKLED o Most common ANTI: SM SS-A SS-B Ribonucleoprotein
SJOGREN SYNDROME
Chronic disease characterized by: o 1. Dry eyes (keratoconjunctivitis) o 2. Dry mouth (xerostomia) Immunologic destruction of lacrimal & salivary glands 2 forms: o 1. Primary/ Sicca syndrome 40% o 2. Secondary associated with another autoimmune disease (ex. RA) 60%
Multi-systemic SLE Scleroderma Mixed CT dse.
Autoimmune Diseases Rheumatoid arthritis Sjogren syndrome Systemic Lupus Erythematosus Systemic sclerosis/ Scleroderma Inflammatory myopathies Mixed CT disease Polyarteritis nodosa
RHEUMATOID ARTHRITIS
A chronic inflammatory disease affecting primarily the JOINTS o Formation of pannus Other tissues involved: skin, blood vessels, lungs, heart
SICCA SYNDROME Lymphocytic infiltration & fibrosis of lacrimal & salivary glands (+) CD4+ helper T cells, some B cells 75% - RA factor + 50-80% - ANA + 90% anti SS-A (Ro) & anti SS-B (La) Triggered by inflammation (EBV, Hepa C, HTLV1) o Initiating trigger w/c causes Local cell death Release of tissue self antigen (a-fodrin) MORPHOLOGY Lymphoid follicles seen Ductal lining epithelial hyperplasia Acini atrophy, fibrinosis, hyalinization Parenchymal fatty replacement CLINICAL COURSE High risk for B cell lymphomas Women: 50-60 y/o
Prepared by: EGBII; 8-13-11
NUCLEOLAR o Anti RNA most often in systemic sclerosis Immunofluorescence for ANAs is sensitive but non-specific because other autoimmune dses are frequently positive Positivity increase with age All patients are (+) for ANA Anti double stranded DNA and anti-SMITH antigen o *are diagnostic of SLE Antiphospholipid Abs in 40-50% o Directed against epitopes of plasma CHONs Prothrombin Annexin V B2 glycoprotein Protein S and C o False + syphilis test because of phospholipid B2 glycoprotein complex binds with cardiolipin antigen Some Ab interfere w/in vitro clotting tests o lupus anticoagulant However, pts have complication assocd w/hypercoagulable state 0 o 2 antiphospholipid antibody syndrome
Procainamide
MECHANISM OF TISSUE INJURY Most visceral lesions are type 3 hypersensitivity In tissues o nuclei of damaged cells react with ANA In vitro o Phagocytic cell engulfes denatured nucleus of injured cell LE cell MORPHOLOGY In KIDNEYS, there are 5 patterns of LUPUS NEPHRITIS: o Class I: Minimal mesangial o Class II: mesangial proliferative o Class III: Focal proliferative several prolif; deposition of complex in glomerulous (some) o Class IV: Diffuse proliferative several prolif; deposition of complex in glomerulous (most) o Class V: Membranous Thickening of Bowmans BLOOD VESSELS o Acute necrotizing vasculitis JOINTS o Non erosive synovitis CNS o Non inflammatory occlusion of small vessels o Impaired neuronal function CVS o Libman-Sacks endocarditis nonbacterial o Pericarditis > myocarditis SPLEEN o Capsular thickening o Follicular hyperplasia LUNGS o Pleuritis, effusions o Interstitial pneumonitis SKIN o Malar erythema, including bridge of nose (butterfly rash) o Sunlight exacerbates the lesions o VACUOLAR degeneration of epidermal basal laye o Edema, perivascular inflammation dermis CRITERIA FOR CLINICAL DIAGNOSIS (4 or more) 1. Malar rash 2. Sicord rash
3. 4. 5. 6. 7. 8. 9. 10.
Photosensitivity Oral ulcers Arthritis Serositis Renal Neurologic ANA, Ab titers Hematologic a. Anemia b. Thrombocytopenia
(+) inappropriate activation of humoral immunity produces autoantibodies
CLINICAL COURSE Variable, unpredictable Flare ups and remissions 90% 5-yr survival rate, 80% @ 10-yr Most common COD Renal failure Intercurrent infection OTHER SYNDROMES Chronic discoid LE Skin manifestation mimics SLE, rare sytemic involvement Face and scalp, skin plaques ANA test 35% Subacute cutaneous LE Skin rash widespread, superficial, non-scarring Anti SS-A, HLA-DR3 genotype Drug induced LE Hydralazine, procainamide, INH, d-penicillamine ANA+ UNCOMMON renal and CNS involvement
ANTIBODIES Anti DNA topoisomerase 1 (anti Scl 70) o In 10-20% of patients o Patients have pulmonary fibrosis & peripheral vascular resistance o Highly specific for diffuse scleroderma Anti centromere antibody o In 20-30% of patients o Patients with CREST or limited cutaneous systemic sclerosis Vascular damage Microvascular disease present in EARLY course May be the initial lesion Cause in not known Widespread narrowing of microvasculature leads to ischemic injury & scarring Fibrosis
FACTORS Genetic Immunological Environmental Genetic predisposition st 1 degree 20% Monozygotic twins >20% HLA DQ (ds Ab, anti SM, anti PL) Inherited deficiency C2, C4, or C1q Immunological factors: Defective elimination of self reactive B cells in BM CD4 helper T cells escape tolerance Nuclear DNA & RNA activate B lymphocytes (TLR) Environmental factors: UV light Sex hormone Female in repro years Pregnancy Drugs Hydralazine
Primary abnormality in collagen production Culmination of multiple abnormalities Example: o Fibrogenic cytokines o Hyperresponsiveness of fibroblasts o Scarring
SYSTEMIC SCLEROSIS/ SCLERODERMA
Unknown Autoimmune responses, vascular damage, & collage deposition contribute to tissue injury CD4+ T cells associated Excessive systemic fibrosis skin Female 3:1 Abnormal immune responses o CD4+ T cells responds to an antigen o Accumulate in skin & release cytokines that activates inflammatory cells & fibroblasts
CHRONIC DISEASE Characterized by: 1. Chronic inflammation 2. Widespread damage to small BV 3. Progressive interstitial & perivascular fibrosis in skin & other organs TWO MAJOR CATEGORIES 1. DIFFUSE a. Widespread skin involvement b. w/ rapid progression & early visceral involvement c. DNA tropoisomerase I 2. LIMITED a. Skin involvement is confined to: i. Fingers ii. Forearms iii. Face iv. Some with CREST syndrome CREST Syndrome 1. Calcinosis in skin 2. Raynaud phenomenon (sensi. to cold)
Prepared by: EGBII; 8-13-11
3. Esophageal dismotility 4. Sclerodactyly 5. Telengiectasia MORPHOLOGY Skin o o GIT o
Diffuse sclerotic atrophy Begins in fingers & distal regions of upper extremities
Preogressive atrophy & collagenous fibrosis replacement of muscularie o Esophagus (rubber hose) o Results to GERD Musculoskeletal o Synovial hyperplasia o Hypertrophy o Fibrosis similar to RA but NO joint destruction o Inflammatory myositis Kidneys o 2/3 patients o Vascular lesions o Hypertension in 30% of patients o Renal failure 50% death Lungs o 50% of patients o Vasospasms, fibrosis (pulmonary hypertension) Heart o Pericarditis o Effusion o Myocardial fibrosis o Right ventricular hypertrophy CLINICAL F:M = 3:1 Peak: 50-60 y/o Malignant hypertension with subsequent renal failure Right sided heart failure - *major cause of death
Prepared by: EGBII; 8-13-11
S-ar putea să vă placă și
- Chapter 6 - Immune Diseases (Part II) (Robbins and Cotran Pathologic Basis of Disease)Document3 paginiChapter 6 - Immune Diseases (Part II) (Robbins and Cotran Pathologic Basis of Disease)Ernie G. Bautista II, RN, MD100% (5)
- Chapter 7 Neoplasia 1 2 Robbins and Cotran Pathologic Basis of DiseaseDocument9 paginiChapter 7 Neoplasia 1 2 Robbins and Cotran Pathologic Basis of DiseaseArun Nayak100% (11)
- Chapter 1 - Cellular Injury, Cell Adaptation & Cell Death (Robbins and Cotran Pathologic Basis of Disease)Document3 paginiChapter 1 - Cellular Injury, Cell Adaptation & Cell Death (Robbins and Cotran Pathologic Basis of Disease)Ernie G. Bautista II, RN, MD91% (34)
- Robbins Pathology - Chapter 6 TransDocument31 paginiRobbins Pathology - Chapter 6 Transnath nathÎncă nu există evaluări
- Robbins Pathology Chapter 13 - White Blood CellsDocument7 paginiRobbins Pathology Chapter 13 - White Blood Cellsscorpiosphinx7980% (5)
- Robbins Pathology - Chapter 5 TransDocument20 paginiRobbins Pathology - Chapter 5 Transnath nath100% (1)
- Robbins Pathology - Chapter 1 TransDocument11 paginiRobbins Pathology - Chapter 1 Transnath nathÎncă nu există evaluări
- Chapter 8 Infectious Diseases Robbins and Cotran Pathologic Basis of DiseaseDocument12 paginiChapter 8 Infectious Diseases Robbins and Cotran Pathologic Basis of DiseaseArun Nayak86% (7)
- Robbins Pathology - Chapter 3 TransDocument18 paginiRobbins Pathology - Chapter 3 Transnath nath100% (6)
- Robbins Pathology - Chapter 2 TransDocument19 paginiRobbins Pathology - Chapter 2 Transnath nath100% (3)
- Robbins Pathology - Chapter 4 TransDocument9 paginiRobbins Pathology - Chapter 4 Transnath nathÎncă nu există evaluări
- Robbins and Cotran's Pathologic Basis of Disease Chapter 1Document14 paginiRobbins and Cotran's Pathologic Basis of Disease Chapter 1Mon Dominguez100% (2)
- Robbin's SummariesDocument98 paginiRobbin's SummariesnopedontsuemepleaseÎncă nu există evaluări
- Liver - RobbinsDocument25 paginiLiver - Robbinssarguss14100% (2)
- Pathology A - The Cell As A Unit of Health and DiseaseDocument13 paginiPathology A - The Cell As A Unit of Health and DiseaseYui VainÎncă nu există evaluări
- GASTROINSTINAL TRACT Robbins 8th EditionDocument4 paginiGASTROINSTINAL TRACT Robbins 8th EditionLim EricÎncă nu există evaluări
- Robbins Pathology Chapter 14 - RBCsDocument7 paginiRobbins Pathology Chapter 14 - RBCsscorpiosphinx79100% (10)
- Acute Inflammation - Robbins Basic Pathology - Inflammation & RepairDocument24 paginiAcute Inflammation - Robbins Basic Pathology - Inflammation & RepairLuis Adrian De Jesús100% (9)
- Robbins Questions Chp1-10Document28 paginiRobbins Questions Chp1-10verbatimmt100% (1)
- Chapter 2 (Questions 2008-2009 Compiled)Document89 paginiChapter 2 (Questions 2008-2009 Compiled)vetpathforum100% (1)
- Robbins Pathology NotesDocument48 paginiRobbins Pathology NotesRajesh Kumar Asunala91% (93)
- Chapter 4 (Questions 2008-2009 Compiled)Document44 paginiChapter 4 (Questions 2008-2009 Compiled)vetpathforum100% (1)
- Patho - Inflammation SummaryDocument28 paginiPatho - Inflammation SummaryTep Gonzales71% (7)
- General PATHOLOGYDocument72 paginiGeneral PATHOLOGYlimpek100% (2)
- Chapter 1 (Questions 2008-2009 Compiled)Document65 paginiChapter 1 (Questions 2008-2009 Compiled)vetpathforum100% (2)
- Ch.1 Baby Robbins OutlineDocument11 paginiCh.1 Baby Robbins OutlinePA2014100% (3)
- Chapter 6 (Questions 2008-2009 Compiled)Document52 paginiChapter 6 (Questions 2008-2009 Compiled)vetpathforumÎncă nu există evaluări
- Chapter 1 Compiled General Pathology QuestionsDocument14 paginiChapter 1 Compiled General Pathology Questionsvetpathforum90% (10)
- General Pathology MCQsDocument32 paginiGeneral Pathology MCQsedcrfvtgb12345684% (37)
- Pathoma Notes CH 1-3Document11 paginiPathoma Notes CH 1-3imdaking12392% (25)
- Cellular responses to stress and toxic insultsDocument29 paginiCellular responses to stress and toxic insultsMK100% (1)
- Hemodynamic Disorders, Thromboembolic Disease and ShockDocument13 paginiHemodynamic Disorders, Thromboembolic Disease and Shockpjcanero100% (5)
- Cell Injury Mcqs ExplainedDocument5 paginiCell Injury Mcqs ExplainedDocAxi Maximo Jr Axibal88% (8)
- TOPNOTCH MEDICAL BOARD PREP PATHO SUPERTABLEDocument47 paginiTOPNOTCH MEDICAL BOARD PREP PATHO SUPERTABLEDianne GalangÎncă nu există evaluări
- Robbins Basic Pathology 9th Edition QBankDocument4 paginiRobbins Basic Pathology 9th Edition QBankVarshini Tamil SelvanÎncă nu există evaluări
- Pathology, Lecture 10, NeoplasiaDocument190 paginiPathology, Lecture 10, NeoplasiaAli Al-Qudsi97% (35)
- Quiz PathologyDocument28 paginiQuiz PathologyMedShare86% (35)
- Top 100 Pathology Secrets List W/ NotesDocument6 paginiTop 100 Pathology Secrets List W/ NotesPA2014100% (4)
- MCQs in Cell Injury and HistochemistryDocument5 paginiMCQs in Cell Injury and Histochemistryashour_abdelsalam632692% (12)
- Cellular Adaptations and Responses to StressDocument19 paginiCellular Adaptations and Responses to StressFu Xiao ShanÎncă nu există evaluări
- CNS Path ChartDocument10 paginiCNS Path Chartjamesomoore100% (1)
- RObbinsDocument37 paginiRObbinsapi-374646950% (4)
- Pathology Question PapersDocument26 paginiPathology Question PapersShane Rodriguez100% (2)
- General Pathology MCQDocument3 paginiGeneral Pathology MCQSooPl33% (3)
- Chapter 7 (Questions 2008-2009 Compiled)Document27 paginiChapter 7 (Questions 2008-2009 Compiled)vetpathforum100% (1)
- Chapter 11 Blood Vessels 8th Ed NotesDocument7 paginiChapter 11 Blood Vessels 8th Ed NotesKyle Christopher SiaÎncă nu există evaluări
- Chapter 14 Red Blood CellsDocument37 paginiChapter 14 Red Blood CellsCatherine LiuÎncă nu există evaluări
- Neoplasia Pathogenesis and ClassificationDocument10 paginiNeoplasia Pathogenesis and ClassificationCharlene Fernández100% (4)
- Lung Head and NeckDocument26 paginiLung Head and Neckzeroun24100% (2)
- Lecture 19, Ch. 43Document21 paginiLecture 19, Ch. 43S. SpencerÎncă nu există evaluări
- Unit II Cells & Organs of ImmuneDocument69 paginiUnit II Cells & Organs of ImmuneSAMUELÎncă nu există evaluări
- Immunity 2022Document53 paginiImmunity 2022Craft Hachz By dhiyaÎncă nu există evaluări
- 21 Immunology Principles 2010-2Document46 pagini21 Immunology Principles 2010-2Ashoog AlkhaldiÎncă nu există evaluări
- Diseases of The Immune System (I)Document55 paginiDiseases of The Immune System (I)Visca ZerlindaÎncă nu există evaluări
- Immunophysiology OverviewDocument40 paginiImmunophysiology OverviewSafa TaweelÎncă nu există evaluări
- IS3 - Antigens and the Major Histocompatibility ComplexDocument30 paginiIS3 - Antigens and the Major Histocompatibility ComplexnasarcedaÎncă nu există evaluări
- The Immune System and Lymphoid OrgansDocument68 paginiThe Immune System and Lymphoid OrgansAbraham Dawson machachaÎncă nu există evaluări
- It 4 - Sel Dan Jaringan Sistim ImunDocument90 paginiIt 4 - Sel Dan Jaringan Sistim Imunezra soÎncă nu există evaluări
- ENI Immunity To Bacteria-Fungi InfectionDocument28 paginiENI Immunity To Bacteria-Fungi InfectionEnny WulandariÎncă nu există evaluări
- Immunopathology: Normal Immune ResponseDocument13 paginiImmunopathology: Normal Immune ResponseChinedu H. DuruÎncă nu există evaluări
- Acne VulgarisDocument49 paginiAcne VulgarisErnie G. Bautista II, RN, MD100% (1)
- AstrocytomaDocument11 paginiAstrocytomaErnie G. Bautista II, RN, MDÎncă nu există evaluări
- KCR 2020 Guideline For Scientific ExhibitionDocument2 paginiKCR 2020 Guideline For Scientific ExhibitionErnie G. Bautista II, RN, MDÎncă nu există evaluări
- UrolithiasisDocument79 paginiUrolithiasisErnie G. Bautista II, RN, MDÎncă nu există evaluări
- Parvo BacteriaDocument2 paginiParvo BacteriaErnie G. Bautista II, RN, MDÎncă nu există evaluări
- Herpes, Pox, Rhabdo, Arena VIRUSDocument7 paginiHerpes, Pox, Rhabdo, Arena VIRUSErnie G. Bautista II, RN, MDÎncă nu există evaluări
- Guide in Reporting Complete Physical Examination (2013) - Source: Bates' Guide To Physical Examination.Document8 paginiGuide in Reporting Complete Physical Examination (2013) - Source: Bates' Guide To Physical Examination.Ernie G. Bautista II, RN, MD100% (6)
- Subcutaneous Systemic Opportunistic MycosesDocument5 paginiSubcutaneous Systemic Opportunistic MycosesErnie G. Bautista II, RN, MD100% (2)
- MISC Bacteria (Legionella, Listeria, Gardnerella, Actinobacillus, Bartonella, Calymato-Bacterium, Flavobacterium, Streptobacillus)Document6 paginiMISC Bacteria (Legionella, Listeria, Gardnerella, Actinobacillus, Bartonella, Calymato-Bacterium, Flavobacterium, Streptobacillus)Ernie G. Bautista II, RN, MDÎncă nu există evaluări
- Antivirals, Rubella, Peecorna VIRUSDocument3 paginiAntivirals, Rubella, Peecorna VIRUSErnie G. Bautista II, RN, MDÎncă nu există evaluări
- Eye and Ear HistologyDocument96 paginiEye and Ear HistologyErnie G. Bautista II, RN, MD100% (1)
- Sporeforming & Non-Spore Forming BacteriaDocument9 paginiSporeforming & Non-Spore Forming BacteriaErnie G. Bautista II, RN, MD100% (1)
- Ricketsiae BacteriaDocument2 paginiRicketsiae BacteriaErnie G. Bautista II, RN, MDÎncă nu există evaluări
- EnterobacteriaceaeDocument3 paginiEnterobacteriaceaeErnie G. Bautista II, RN, MDÎncă nu există evaluări
- Antimicrobial AgentsDocument3 paginiAntimicrobial AgentsErnie G. Bautista II, RN, MD100% (2)
- Histology of Female Reproductive SystemDocument2 paginiHistology of Female Reproductive SystemErnie G. Bautista II, RN, MDÎncă nu există evaluări
- Introduction To Nervous SystemDocument4 paginiIntroduction To Nervous SystemErnie G. Bautista II, RN, MD100% (1)
- Histology of Male Reproductive SystemDocument2 paginiHistology of Male Reproductive SystemErnie G. Bautista II, RN, MDÎncă nu există evaluări
- Histology of Endocrine SystemDocument1 paginăHistology of Endocrine SystemErnie G. Bautista II, RN, MD100% (1)
- Histology of Sensory & Motor Nerve EndingsDocument2 paginiHistology of Sensory & Motor Nerve EndingsErnie G. Bautista II, RN, MD100% (1)
- General Sensory PathwaysDocument1 paginăGeneral Sensory PathwaysErnie G. Bautista II, RN, MDÎncă nu există evaluări
- DiencephalonDocument4 paginiDiencephalonErnie G. Bautista II, RN, MD100% (3)
- Development of Reproductive SystemDocument2 paginiDevelopment of Reproductive SystemErnie G. Bautista II, RN, MDÎncă nu există evaluări
- Development of Endocrine SystemDocument1 paginăDevelopment of Endocrine SystemErnie G. Bautista II, RN, MDÎncă nu există evaluări
- Cranial Nerves (Association & Motor Neurons)Document2 paginiCranial Nerves (Association & Motor Neurons)Ernie G. Bautista II, RN, MD100% (3)
- Lower Limb: Front and Medial Aspect of ThighDocument8 paginiLower Limb: Front and Medial Aspect of ThighErnie G. Bautista II, RN, MDÎncă nu există evaluări
- Brainstem & LesionsDocument4 paginiBrainstem & LesionsErnie G. Bautista II, RN, MDÎncă nu există evaluări
- Coping With RosaceaDocument17 paginiCoping With RosaceaDiana TanaseÎncă nu există evaluări
- Understanding Toxic Goiter and Its Nursing CareDocument22 paginiUnderstanding Toxic Goiter and Its Nursing CareJohn Matley Caampued100% (2)
- Nursing Assessment: Gastrointestinal System (Chapter 39) : Structures and FunctionsDocument4 paginiNursing Assessment: Gastrointestinal System (Chapter 39) : Structures and FunctionsPrince K. TaileyÎncă nu există evaluări
- Activating A Stroke Alert - A Neurological Emergency - CE591Document7 paginiActivating A Stroke Alert - A Neurological Emergency - CE591Czar Julius Malasaga100% (1)
- Futility CasesDocument2 paginiFutility CasesBindashboy0Încă nu există evaluări
- Cases to Examine- EuthanasiaDocument1 paginăCases to Examine- EuthanasiadamianmackytÎncă nu există evaluări
- IMCI Learning FeedbackDocument1 paginăIMCI Learning Feedbackinah krizia lagueÎncă nu există evaluări
- Traumatic InjuriesDocument45 paginiTraumatic Injuriesibrahim bataÎncă nu există evaluări
- Hydrocephalus AND Neural Tube DefectDocument7 paginiHydrocephalus AND Neural Tube DefectTherese ArellanoÎncă nu există evaluări
- Gabix Caps Leaflet PakistanDocument2 paginiGabix Caps Leaflet Pakistandalalala7662Încă nu există evaluări
- Nasogastric & Gavage - NsoDocument5 paginiNasogastric & Gavage - NsojamesÎncă nu există evaluări
- Post TestDocument11 paginiPost Testoomculun100% (6)
- Bilateral Variation in The Branching Pattern of The Axillary Artery - A Case ReportDocument5 paginiBilateral Variation in The Branching Pattern of The Axillary Artery - A Case ReportIJAR JOURNALÎncă nu există evaluări
- HPNDocument32 paginiHPNkaren GoÎncă nu există evaluări
- MH Guideline For Web v2Document1 paginăMH Guideline For Web v2FilbertaÎncă nu există evaluări
- Circumcision in HemophiliaDocument11 paginiCircumcision in HemophiliaRicho WijayaÎncă nu există evaluări
- Pex 09 03Document4 paginiPex 09 03Illich Ramirez TantaÎncă nu există evaluări
- LVS Chronic Pain WsDocument49 paginiLVS Chronic Pain WsdtncorreoÎncă nu există evaluări
- Malaria in Children: Department of Paediatrics and Child Health, Mbarara UniversityDocument13 paginiMalaria in Children: Department of Paediatrics and Child Health, Mbarara UniversityMwanja MosesÎncă nu există evaluări
- Factors Affecting Inter Individual Variations in Drug ResponseDocument10 paginiFactors Affecting Inter Individual Variations in Drug Responsehumera50% (4)
- Gowning: Bagasbas, Krizzamer P. Balagso, Jezzica RDocument13 paginiGowning: Bagasbas, Krizzamer P. Balagso, Jezzica RNdor BariboloÎncă nu există evaluări
- 5 White Blood Cells Types and Their FunctionsDocument3 pagini5 White Blood Cells Types and Their FunctionsSN Wijesinhe100% (1)
- Dissociation Affect Dysregulation Somatization BVDKDocument22 paginiDissociation Affect Dysregulation Somatization BVDKkanuÎncă nu există evaluări
- 3 Main Food Group: Reporter: Mercy Grace Yongco - MPA IDocument11 pagini3 Main Food Group: Reporter: Mercy Grace Yongco - MPA ICHOSEN TABANASÎncă nu există evaluări
- A Review On The Diseases and Treatments That Affect The Bone Physiology and StrengthDocument17 paginiA Review On The Diseases and Treatments That Affect The Bone Physiology and StrengthErnest Gabriel Cruz AdvinculaÎncă nu există evaluări
- Pharmacovigilance 1Document28 paginiPharmacovigilance 1Gideon AdurojaÎncă nu există evaluări
- Nutrition Care ProcessDocument22 paginiNutrition Care ProcessIrhamna Fauziah100% (1)
- Red Cross Medical CertificateDocument2 paginiRed Cross Medical CertificateScribdTranslationsÎncă nu există evaluări
- COX-2 Inhibitors: Mechanisms and ExamplesDocument16 paginiCOX-2 Inhibitors: Mechanisms and ExamplesYousab MKÎncă nu există evaluări
- Clinical Abstract: Bañag, Daraga, Albay Contact Nos.: (Globe) 09271684061 (Smart) 09475160066Document1 paginăClinical Abstract: Bañag, Daraga, Albay Contact Nos.: (Globe) 09271684061 (Smart) 09475160066kolintang1Încă nu există evaluări