Documente Academic
Documente Profesional
Documente Cultură
Nursing Management of Upper GI Bleeding
Încărcat de
Via Katherine PanganibanDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Nursing Management of Upper GI Bleeding
Încărcat de
Via Katherine PanganibanDrepturi de autor:
Formate disponibile
OUR LADY OF FATIMA UNIVERSITY COLLEGE OF NURSING
Nursing Management of Patient with Upper Gastrointestinal Bleeding
Submitted by: Fatima Mae D.L. Panganiban BSN 3Y3 -8D
Submitted to: Mrs. Eden Salazar, RN
Nursing Management of Patient with Upper Gastrointestinal Bleeding CLR, an 84 year old female with a medical history of nonerosive gastritis last July 2011, was diagnosed with upper gastrointestinal bleeding probably secondary to BPUB:
Cardiovascular infarct, left MCA distribution. The patient had therapeutic procedure that is colonoscopy with SNARE
polypectomy in November 16, 2011. Patient was admitted in November 6, 2011 at 3:18pm. Patients chief complaint was generalized body weaknesses and it is the reason for the patient to be admitted in AFPMC for the 4th time. The patient was a previous smoker 3 years ago.
Pathophysiology Acute gastrointestinal (GI) bleeding is a potentially lifethreatening abdominal emergency that remains a common cause of hospitalization. Upper gastrointestinal bleeding (UGIB) is defined as bleeding derived from a source proximal to the ligament of Treitz. The incidence of UGIB is approximately 100 cases per 100,000 populations per year. Bleeding from the upper GI tract is approximately 4 times as common as bleeding from the lower GI
tract and is a major cause of morbidity and mortality. Mortality rates from UGIB are 6-10% overall. The diagnosis of and therapy for nonvariceal upper gastrointestinal bleeding (UGIB) has evolved since the late 20th century from with passive medical diagnostic therapy until
esophagogastroduodenoscopy
surgical intervention was needed to active intervention with endoscopic techniques followed by angiographic and surgical approaches if endoscopic therapy fails. Variceal hemorrhage is not discussed in this article because the underlying mechanisms of bleeding are different and require different therapies. The underlying mechanisms of nonvariceal bleeding
involve either arterial hemorrhage, such as in ulcer disease and mucosal deep tears, or low-pressure venous hemorrhage, as in telangiectasias and angioectasias. In variceal hemorrhage, the underlying pathophysiology is due to elevated portal pressure transmitted to esophageal and gastric varices and resulting in portal gastropathy.
History Patients has a known case of non-erosive gastritis last July 2011 but was also admitted to the institution last April 2011 with a case of UGIB to BPUD and was then maintained on Esomeprazole 40mg/tab 1tab BID in 6 weeks and Refamide 100mg/tab 1tab TID. On her readmission last October 2011, patient went home against medical advice and was prescribed with Pantoprazole 40mg/tab 1tab ODBB for 4weeks. After the patients discharged, her meloma did not restore. No follow-up consult was done. 4days after discharge, she complained of generalized body weakness associated with loss of appetite. 4days prior to admission, patient had 4episodes of loss bowel movement, blackish in color amounting to 2 cup. Other associated signs and symptoms include occasional burning, epigastric pain and dizziness. No vomiting noted. Persistence of symptoms prompted consult hence admission.
Nursing Physical Assessment CLR was alert, conscious, oriented and coherent to person, place and time. She is not in cardio respiratory distress or in any alarming event. Her first vital signs upon admission were that her temperature was 36.7C, her pulse rate was 90bpm, her respiratory rate was 20cpm and her blood pressure was 110/70. Patients HEENT results had antistatic schlera, pink palpated conjunctivae, no neck vein engorgement. Chest exam results were symmetrical chest expansion, no retraction and with clean breath sound. In cardiovascular system has dynamic permission, has normal rate with regular rhythm and with no murmurs. In abdomen exam, the results were flabby, soft, no-tenders and no palpable mass. Extremities are full and with equal pulse, no edema. Rectal exam has positive dark stool upon examining with finger, has good sphincter with no mass. Active problem is melena. In her system review, she has no cough, chest pain, cold or difficulty in breathing. She is positive with hypertension but had maintained on Telmisartan. Also, she had no Diabetes Mellitus or allergy in medicines. Ionized calcium is higher than normal that is 1.15mmo/L upon receiving her laboratory test in November 19, 2011. Creatinine is normal. There is a decrease of
Hematocrit and Hemoglobin and increase in WBC. CK-total is higher than normal and sodium level is low. Related Treatment The patient had her radiologic test on November 6, 2011 and in her results, there are 3 defined opacities seen in the left upper lung. Her heart is not enlarged. Aorta is calcified. Her right hemidiaphragm is elevated while the left hemidiaphragm and sulci are intact. There are degenerative changes seen on the visualized osseous structures. The impression is that she has PTB. Atheromators aorta and elevated right hemidiaphragm considerations are: liver pathology, phrenic nerve paralysis, eventration and degenerative osteoarthritis. On her CT-scan of the whole abdomen shows that she has multiple contrast-enhanced axial images reveal a normal-sized liver with a well defined non-contrast enhancing oyst in segment 5 measuring 2 x 1.3 cm and without intrinsic mass or calcifications. The hepatic surface is smooth. There is segmental gaseous dilatation of the small intestine and colon due to a dyanamic ileus. The pancreas, spleen, adrenal, kidneys, ureters, urinary bladder and stomach as well as the lymph nodes and peritoneum are unremarkable save for few benign left renal cortical cysts. No lytic bone lesion is seen. Impressions are
hepatic cyst, dynamic ileus and no intra-abdominal mass or enlarged lymph nodes. Medicines that are prescribed are given at the exact time of medication. Cefepime 1g/IV q12 anti-infective/cepholosporin Erythropoietin B5000 (once a week with BP precaution) immunomodulators/ biological response modifiers Esomeprazole 40mg/tab 1tab ODBB antiulcer drug Rebamepide 100mg/tab 1tab TID antacid drug Simvastatin 40mg/tab 1tab ODHS antilipemic drug Trifusal 300mg/cap 1cap TID antiplatelet agent drug
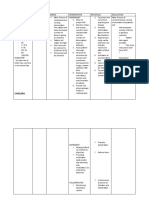
Nursing Care Plan CLRs nursing diagnosis is intolerance related to generalize weakness as manifested by discomfort, fatigue and dizziness. Patient feels discomfort, fatigue, dizziness. She has a
temperature of 36.7C, pulse rate of 90bpm, respiratory of 20cpm, and a blood pressure of 110/70. Patient verbalized that she her body weakens. The nursing goal to the patient is that in short term: after 30 to 60 minutes of nursing intervention, the patient will be able to: Participate in necessary physical activity with appropriate increases in blood pressure and monitor patterns with in normal
limits. Identify activities or anxiety. To producing situations that may contribute to activity intolerance. While on long term: after 2 to 4hours of nursing intervention, the patient will be able to: Balances activity and rest. Perform home maintenance
management with some help. Verbalize understanding of need for medications that may increase tolerance for activities. The nursing interventions to the patient in independent are, note client reports of weakness, difficulty in accomplishing task. The rationale behind this is symptoms may be result or contribute to intolerance of activity. Assess nutritional status. The rationale behind this is adequate energy reserves are requirements for activity. Provide positive atmosphere, while acknowledging difficulty of the situation for the client. The rationale behind this is it helps to minimize frustration and rechannel energy. In dependent interventions are Adjust activities to prevent overexertion. The rationale behind this is to reduce intensity level or discontinues activity that causes undesired physiological changes. Monitor response to supplemental
medication and changes in regimen. The rationale behind this is to monitor the effect of the medications that were given. Note treatment-related factors, such as side effects/interaction
of medication. The rationale behind this is to monitor the effect of the medications that were given. Provide referrals to other
disciplines such as exercise physiologist, recreational/leisure specialist, as indicated. The rationale behind this is to develop individually appropriate therapeutic regimens. On short term intervention, after 30to 60 minutes of nursing intervention, the patient was able to: Participate in necessary physical activity with appropriate increases in blood pressure and monitor patters with in normal limits. Identify activities or anxiety-producing situations that may contribute to activity intolerance. While on long term intervention, after 2 to 4hours of nursing intervention, the patient was able: Balances activity and rest. Perform home maintenance management with some help Verbalize understanding of need for medications that may increase tolerance for activities.
Recommendation The patient should follow up with her physician regarding to her condition, medications and therapy. The patient should also follow up her nutritionist about her dietary needs. Her diet must include low-cholesterol, low-fat diet. Also, she must maintain her prevention to smoking. She must also live a healthier lifestyle, have lesser stress activities and thing that can exhaust the patient rapidly. The patient must also take her
maintenance and supplemental medicines to lessen the risk of being ill again. The nurse must orient the patient about her condition and the risk factors that she may encounter once outside the hospital ground. Advice and teach her the importance of weekly check-up to her physician. The nurse must also orient the relatives about the condition of the patient and help the patient to feel better upon leaving the hospital care.
Reference
http://emedicine.medscape.com/article/187857-overview http://www.scribd.com/
S-ar putea să vă placă și
- Managing Upper GI Bleeding in a Male PatientDocument19 paginiManaging Upper GI Bleeding in a Male PatientMary Ann Garcia100% (1)
- Case No 45: of Intermittent Abdominal Pain Abdominal Bloating and Nausea and Vomiting (NVDocument17 paginiCase No 45: of Intermittent Abdominal Pain Abdominal Bloating and Nausea and Vomiting (NVPremiums of the RoseÎncă nu există evaluări
- Diverticular DiseaseDocument8 paginiDiverticular Diseasenurse_enzo100% (1)
- Risk For Bleeding - Cirrhosis NCPDocument2 paginiRisk For Bleeding - Cirrhosis NCPPaula AbadÎncă nu există evaluări
- Assess For Signs of HyperglycemiaDocument9 paginiAssess For Signs of HyperglycemiaSheril Sularte CasanesÎncă nu există evaluări
- NCP2 - DengueDocument4 paginiNCP2 - DengueSummer SuarezÎncă nu există evaluări
- NCP FVDDocument1 paginăNCP FVDsisjing88510Încă nu există evaluări
- NCP CKDDocument3 paginiNCP CKDRiel TumandaÎncă nu există evaluări
- Scribd 020922 Case Study-Oncology A&kDocument2 paginiScribd 020922 Case Study-Oncology A&kKellie DÎncă nu există evaluări
- Case Study Ugib Lower MBDocument65 paginiCase Study Ugib Lower MBQuolette Constante100% (1)
- Betahistine Drug InfoDocument3 paginiBetahistine Drug InfoAshish KarnÎncă nu există evaluări
- NCP PainDocument2 paginiNCP PainApril_Ivy_Raga_3835Încă nu există evaluări
- NCP Fluid Volume DeficitDocument3 paginiNCP Fluid Volume DeficitNecheal BaayÎncă nu există evaluări
- DP Discharge Plan@@@@@@@@Document6 paginiDP Discharge Plan@@@@@@@@Maemae SumalinogÎncă nu există evaluări
- NCPDocument3 paginiNCPJoevelyn LaynoÎncă nu există evaluări
- Drug StudyDocument20 paginiDrug StudydjanindÎncă nu există evaluări
- NCPDocument10 paginiNCPNefre Dayap DarrocaÎncă nu există evaluări
- Nursing Care Plan: Fluid Volume DeficitDocument2 paginiNursing Care Plan: Fluid Volume DeficitGenEsis CarandangÎncă nu există evaluări
- Assessment Diagnosis Planning Intervention Rationale EvaluationDocument4 paginiAssessment Diagnosis Planning Intervention Rationale EvaluationJhoizel VenusÎncă nu există evaluări
- Subjective Cues:: Nursing Care ProcessDocument8 paginiSubjective Cues:: Nursing Care ProcessBianca Marithè RejanoÎncă nu există evaluări
- Imbalanced NutritionDocument2 paginiImbalanced NutritionRizza 이 동해 Ocampo100% (1)
- Physical Assessment Appendix FinalDocument6 paginiPhysical Assessment Appendix FinalLucelle ArellanoÎncă nu există evaluări
- Penicillin GDocument2 paginiPenicillin Gapi-295691235Încă nu există evaluări
- NCPDocument15 paginiNCPCamille PinedaÎncă nu există evaluări
- Assessment/ Cues Nursing Diagnosis Background Knowledge Goal and Objectives Nursing Interventions and Rationale EvaluationDocument6 paginiAssessment/ Cues Nursing Diagnosis Background Knowledge Goal and Objectives Nursing Interventions and Rationale EvaluationimnasÎncă nu există evaluări
- NURSING CARE PLAN FOR POSTPARTUM HEMORRHAGEDocument3 paginiNURSING CARE PLAN FOR POSTPARTUM HEMORRHAGEKrizzy Chen100% (1)
- Nursing Care Plan EportfolioDocument14 paginiNursing Care Plan Eportfolioapi-279212367Încă nu există evaluări
- Nursing Care Plan for Diabetic Patient with DehydrationDocument2 paginiNursing Care Plan for Diabetic Patient with DehydrationRodolfo Bong SemaneroÎncă nu există evaluări
- DRUG STUDY Brokenshire College Study on BevacizumabDocument2 paginiDRUG STUDY Brokenshire College Study on BevacizumabJai GoÎncă nu există evaluări
- Which It Is A Process Whereby Pancreatic Enzymes Destroy Its Own Tissue Leading ToDocument8 paginiWhich It Is A Process Whereby Pancreatic Enzymes Destroy Its Own Tissue Leading ToAriane-Gay Cristobal DuranÎncă nu există evaluări
- NCP and Case Study on Fluid Volume Deficient PatientDocument4 paginiNCP and Case Study on Fluid Volume Deficient PatientErnest Brian FernandezÎncă nu există evaluări
- NCP Risk InfectionDocument1 paginăNCP Risk InfectionEni RahmawatiÎncă nu există evaluări
- Incomplete Spinal Cord Injury Nursing CareDocument6 paginiIncomplete Spinal Cord Injury Nursing CareTherese MargaretÎncă nu există evaluări
- Gastritis Types, Causes, Symptoms and TreatmentDocument17 paginiGastritis Types, Causes, Symptoms and TreatmentSri Wahyuni HarliÎncă nu există evaluări
- Benign Prostatic Hyperplasia NCPDocument3 paginiBenign Prostatic Hyperplasia NCPsimonjosanÎncă nu există evaluări
- Activity IntoleranceDocument2 paginiActivity Intolerancepooper123Încă nu există evaluări
- PO preparations of oral vitamin B12 may be mixed with fruit juicesDocument2 paginiPO preparations of oral vitamin B12 may be mixed with fruit juicesShannon0% (1)
- Fluid VolumeDocument2 paginiFluid Volumecoldfire28Încă nu există evaluări
- Renal Failure NCPDocument3 paginiRenal Failure NCPjsksÎncă nu există evaluări
- Cs AGNDocument177 paginiCs AGNMa Rafaela Rosales PalomponÎncă nu există evaluări
- Nursing Care Plan: Assessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Risk For ConstipationDocument4 paginiNursing Care Plan: Assessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Risk For Constipationkenneth_bambaÎncă nu există evaluări
- Case Presentation Hypokalemic ManDocument61 paginiCase Presentation Hypokalemic ManHussain AzharÎncă nu există evaluări
- Liver Cirrhosis Care PlanDocument3 paginiLiver Cirrhosis Care PlanWendy EscalanteÎncă nu există evaluări
- Case For NCPDocument5 paginiCase For NCPSarah Jane MaganteÎncă nu există evaluări
- Ugib Case StudyDocument36 paginiUgib Case StudyRJ MarquezÎncă nu există evaluări
- Acute Pain Assessment and Nursing InterventionsDocument1 paginăAcute Pain Assessment and Nursing InterventionsAi RouÎncă nu există evaluări
- NCP MeningitisDocument2 paginiNCP MeningitisARISÎncă nu există evaluări
- Rufino, Leslie Kriztel S. BSN 3-2 Group 1Document6 paginiRufino, Leslie Kriztel S. BSN 3-2 Group 1Deinielle Magdangal RomeroÎncă nu există evaluări
- MorphineDocument3 paginiMorphineAizat KamalÎncă nu există evaluări
- Ca6 NCP Pain - NinaDocument6 paginiCa6 NCP Pain - NinaNinaÎncă nu există evaluări
- HNBBDocument3 paginiHNBBManelle SingzonÎncă nu există evaluări
- NCP BronchopneumoniaDocument8 paginiNCP BronchopneumoniaCrisantaCasliÎncă nu există evaluări
- Generic NameDocument2 paginiGeneric NamePerdie Branden ReizÎncă nu există evaluări
- Nursing Care Plan for Impaired Bowel EliminationDocument4 paginiNursing Care Plan for Impaired Bowel EliminationMara Jon Ocden CasibenÎncă nu există evaluări
- Urea Cycle Disorders - Management - UpToDateDocument21 paginiUrea Cycle Disorders - Management - UpToDatePIERINAÎncă nu există evaluări
- Ranitidine, ParacetamolDocument3 paginiRanitidine, ParacetamoltaekadoÎncă nu există evaluări
- TAHBSO ReportDocument4 paginiTAHBSO ReportsachiiMeÎncă nu există evaluări
- Hepatic FailureDocument37 paginiHepatic FailureWinston Dela FuenteÎncă nu există evaluări
- Clinical Document 1Document7 paginiClinical Document 1api-253709303Încă nu există evaluări
- Development and Validation of Stability Indicating RP-HPLC Method For Simultaneous Estimation of Sofosbuvir and Ledipasvir in Tablet Dosage FormDocument4 paginiDevelopment and Validation of Stability Indicating RP-HPLC Method For Simultaneous Estimation of Sofosbuvir and Ledipasvir in Tablet Dosage FormBaru Chandrasekhar RaoÎncă nu există evaluări
- Knowing God: Prayer and Fasting 2013Document40 paginiKnowing God: Prayer and Fasting 2013ccforgph100% (4)
- An Interview - ExercisesDocument3 paginiAn Interview - ExercisesCarmen GloriaÎncă nu există evaluări
- Saloni Shah - LLM DissertationDocument156 paginiSaloni Shah - LLM DissertationNilesh BatraÎncă nu există evaluări
- 0 BOSH FrameworkDocument18 pagini0 BOSH Frameworkharold fontiveros100% (1)
- Personnel management: Hiring & developing employeesDocument5 paginiPersonnel management: Hiring & developing employeesАлина УсялитеÎncă nu există evaluări
- Final ESIA On Construction Materials - Tamiru BultoDocument110 paginiFinal ESIA On Construction Materials - Tamiru BultoKayo Shankulie100% (1)
- The Payment of Bonus Act 1965 PDFDocument30 paginiThe Payment of Bonus Act 1965 PDFappu kunda100% (1)
- Catalogue of DDSY23S Energy Meter: Smart Metering and System Solution ProviderDocument2 paginiCatalogue of DDSY23S Energy Meter: Smart Metering and System Solution ProviderNadine MichaelsÎncă nu există evaluări
- Report On Baby Food Industry in BangladeshDocument5 paginiReport On Baby Food Industry in BangladeshIffatur RahmanÎncă nu există evaluări
- Airtel's Africa Growth: Surviving CompetitionDocument9 paginiAirtel's Africa Growth: Surviving CompetitionSagar RiazÎncă nu există evaluări
- Pros and Cons of Vegan DietsDocument3 paginiPros and Cons of Vegan DietsCristian AsmazaÎncă nu există evaluări
- Plateau Pressure Ventilation MeasurementDocument1 paginăPlateau Pressure Ventilation MeasurementImtiaz AliÎncă nu există evaluări
- Plant Nematology: A Briefly IntroductionDocument463 paginiPlant Nematology: A Briefly IntroductionRodrigo CarralÎncă nu există evaluări
- LAOKEN Comparison With J&JDocument3 paginiLAOKEN Comparison With J&JMario Alfonso MartinezÎncă nu există evaluări
- Lembar Latihan - P1 - PD MitraDocument123 paginiLembar Latihan - P1 - PD MitratiengcityÎncă nu există evaluări
- CEP Lesson Plan Form: Colorado State University College of Health and Human Sciences Page 1Document13 paginiCEP Lesson Plan Form: Colorado State University College of Health and Human Sciences Page 1Apple AterradoÎncă nu există evaluări
- HPAD 201 Sat Days 2 and 3Document11 paginiHPAD 201 Sat Days 2 and 3Arianne A ZamoraÎncă nu există evaluări
- Causes & Prevention of Coronary Artery DiseaseDocument41 paginiCauses & Prevention of Coronary Artery DiseaseeenagpurcongÎncă nu există evaluări
- Changes in Demand and Supply of Face Masks Under CovidDocument3 paginiChanges in Demand and Supply of Face Masks Under CovidHanh HoangÎncă nu există evaluări
- Edan Sonotrax ManualDocument47 paginiEdan Sonotrax ManualDaniel GalindoÎncă nu există evaluări
- Spiegel Et Al 1999 Psycho OncologyDocument12 paginiSpiegel Et Al 1999 Psycho Oncologyfatimaramos31Încă nu există evaluări
- Nescafe Alegria Nutritional Facts PDFDocument3 paginiNescafe Alegria Nutritional Facts PDFOmarÎncă nu există evaluări
- Observations of Children's Interactions With Teachers, PeersDocument25 paginiObservations of Children's Interactions With Teachers, PeersMazlinaÎncă nu există evaluări
- A.686 (17) Cod AlarmeDocument39 paginiA.686 (17) Cod Alarmeciocioi iancuÎncă nu există evaluări
- The DrunktionaryDocument239 paginiThe DrunktionaryRed Rex 2015Încă nu există evaluări
- Ascha_ASJ19_Nonsurgical Management of Facial Masculinization and FeminizationDocument15 paginiAscha_ASJ19_Nonsurgical Management of Facial Masculinization and Feminizationallen.515Încă nu există evaluări
- G450 G500 6x4 SpecificationsDocument4 paginiG450 G500 6x4 SpecificationsSupervisor MecánicoÎncă nu există evaluări
- Rhodes-Solutions Ch2 PDFDocument16 paginiRhodes-Solutions Ch2 PDFOscar GarzónÎncă nu există evaluări
- Post Harvest Value Chainof Carrot AReviewDocument12 paginiPost Harvest Value Chainof Carrot AReviewDave RoneÎncă nu există evaluări