Documente Academic
Documente Profesional
Documente Cultură
Nursing Diagnosis
Încărcat de
Si Bunga JonquilleDescriere originală:
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Nursing Diagnosis
Încărcat de
Si Bunga JonquilleDrepturi de autor:
Formate disponibile
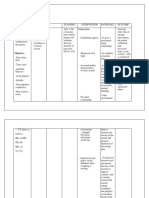
Nursing Diagnosis Impaired Gas Exchange r/t altered oxygen supply
Long Term Goal Patient will maintain optimal gas exchange
Short Term Goals / Outcomes: Patient will maintain normal arterial blood gas (ABGs). Patient will be awake and alert. Patient will demonstrate a normal depth, rate and pattern of respirations. Interventions Assess respirations: quality, rate, pattern, depth and breathing effort. Rationale Rapid, shallow breathing and hypoventilation affect gas exchange by affecting CO2 levels. Flaring of the nostrils, dyspnea, use of accessory muscles, tachypnea and /or apnea are all signs of severe distress that require immediate intervention. Absence of ventilation, asymmetric breath sounds, dyspnea with accessory muscle use, dullness on chest percussion and gross chest wall instability (i.e. flail chest or sucking chest wound) all require immediate attention. Evaluation Patient is free of signs of distress. ABGs show PaCO2 between 3545 Pts respirations are of a normal rate and depth. Patient exhibits spontaneous breathing, no dyspnea, use of accessory muscles, resonance on percussion and no chest wall abnormalities.
Assess for lifethreatening problems. (i.e. resp arrest, flail chest, sucking chest wound).
Auscultate lung Absence of lung sounds, JVD and / or tracheal Patients lungs sounds are clear sounds. Also assess deviation could signify a Pneumothorax or to auscultate throughout all lobes. for the presence of Hemothorax. jugular vein distention (JVD) or tracheal deviation. Assess for signs of hypoxemia. Tachycardia, restlessness, diaphoresis, Patient is free of signs of headache, lethargy and confusion are all signs hypoxia. of hypoxemia.
Monitor vital signs. Initially with hypoxia and hypercapnia blood Patient is normotensive with pressure (BP), heart rate and respiratory rate heart rate 60 100 bpm and all increase. As the condition becomes more respiratory rate 10-20. severe BP may drop, heart rate continues to be rapid with arrhythmias and respiratory failure may ensue. Assess for changes in orientation and behavior. Monitor ABGs. Restlessness is an early sign of hypoxia. Patient is awake, alert and Mentation gets worse as hypoxia increases due oriented X3. to lack of blood supply to the brain. Increasing PaCO2 and decreasing PaO2 are signs of respiratory failure. ABGs show PaCO2 between 3545 and PaO2 between 80 100.
Place the patient on Pulse oximetry is useful in detecting changes continuous pulse in oxygenation. Oxygen saturation should be oximetry. maintained at 90% or greater. Assess skin color for development of cyanosis, especially circumoral cyanosis. Provide supplemental oxygen, via 100% O2 non-rebreather mask. Prepare the patient for intubation. Lack of oxygen delivery to the tissues will result in cyanosis. Cyanosis needs treated immediately as it is a late development in hypoxia. Early supplemental oxygen is essential in all trauma patients since early mortality is associated with inadequate delivery of oxygenated blood to the brain and vital organs. Early intubation and mechanical ventilation are necessary to maintain adequate oxygenation and ventilation, prior to full decompensation of the patient.
SaO2 via pulse oximetry remains at 90 100%. Patient is free of cyanosis.
Patient is receiving 100% oxygen. SaO2 via pulse oximetry is 90 100%.
Artificial airway is placed and maintained without complications. Appropriate injury specific treatment has been started.
Treat the underlying Treatment needs to focus on the underlying injuries with problem that leads to the respiratory failure. appropriate interventions. If rib fractures exist: 1. Assess for paradoxical chest movements. 2. Provide adequate pain 3. relief. Assess breath sounds. If Pneumothorax or Hemothorax exist: 1. obtain chest x-ray 2. prepare for insertion of a chest tube A chest x-ray confirms the presence of a Pneumothorax and / or Hemothorax. A chest tube decreases the thoracic pressure and re-inflates the lung tissue. A three sided dressing gives the accumulated air a way to escape, thereby decreasing Paradoxical movements accompanied by dyspnea and pain in the chest wall indicate flail chest. Flail chest is a life-threatening complication of rib fractures that requires mechanical ventilation and aggressive pulmonary care. Pain relief is essential to enhance coughing and deep breathing. Absence of bilateral breath sounds in the presence of a flail chest, indicates a pneumo/hemo thorax.
No paradoxical movements are noted. Patient reports pain as <3 on 0-10 scale. Bilateral breath sounds present in all lobes.
Chest tube is placed and connected to 20cm wall suction with good tidaling and no air leak or SQ emphysema noted.
If open thoracic pressure and preventing a tension Pneumothorax Pneumothorax. A chest tube must then be exists place a inserted. dressing that is taped on three sides for temporary management.
Three-sided dressing maintained. No further cardiopulmonary decompensation noted in patient.
Position patient with Promotes better lung expansion and improved Patients rate and pattern are of head of bed 45 gas exchange. normal depth and rate at 45 degrees (if degree angle. tolerated). Assist patient with coughing and deep breathing techniques (positioning, incentive spirometry, frequent position changes, splinting of the chest). Suction patient as needed. Promotes alveolar expansion and prevents alveolar collapse. Splinting helps reduce pain and optimizes deep breathing and coughing efforts. Patient is able to cough and deep breathe effectively.
Suctioning aides to remove secretions from the airway and optimizes gas exchange.
Patient suctioned for moderate amount of thin yellow secretion. Lung sounds clear after suctioning. Patients SaO2 remained >90% during suctioning.
Hyperoxygenate patient with 100% before and after suctioning. Keep suctioning to 10-15 seconds.
Prevents alteration in oxygenation during suctioning.
Pace activities and Even simple activities, such as bathing, can provide rest periods increase oxygen consumption and cause to prevent fatigue. fatigue.
No changes to cardiopulmonary status noted during activity. Patients SaO2 remains >90% during activities.
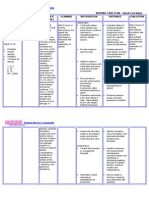
Medical Diagnoses: Impaired Physical Mobility, Musculoskeletal impairment secondary to stroke
Nursing Client Nursing DX/Clinical Goals/Desired Interventions/Actions/Or Problem Outcomes/Objecti ders and Rationale ves Subjective Problem: Long Term: * Apply any ordered brace before mobilizing Pts Impaired Pt will be able to the client. daughter Physical ambulate around states that Mobility the nurses station Rationale: her 2X by discharge. Brace support and mother stablilize a body part, was allowing increased experienci mobility. (Ackley & ng Ladwig, 2008, p 552). progressiv e right *Increase independence sided in ADLs weakness over 2 Rationale: days prior Providing unnecessary to assistance with transfers admission and activities may . promote dependence and a loss of mobility. Objective (Ackley & Ladwig, 2008, p 552). Diagnosis of stroke *Obtain any assistive devices needed for Pt activity. demonstr ates right Rationale: sided Assistive devices can paralysis help increase mobility. (Ackley & Ladwig, 2008, Pt p 552). demonstr R/T: Short Term: ates *Assess the pts pain by decreased Musculoskel Pt will perform using the 10 point pain grips and etal passive range of rating scale q4 hrs or reflexes impairment motion exercises PRN. on the left secondary by the end of this side to stroke shift, by 1900. Rationale: Single- item ratings of Assessme nt *I Evaluation Goa Intervention ls s
pain intensity are valid and reliable as measures of pain intensity. AEB Pt demonstrate s right sided paralysis Pt demonstrate s difficulty with mobility and activity. Pt demonstrate s decreased grips and reflexes on left side Diagnosis of stroke The clients report of pain is the single most reliable indicator of pain. (Ackley & Ladwig, 2008, p. 604-605). *Before activity, treat pain. Rationale: Pain limits mobility and is often exacerbated by movement. (Ackley & Ladwig, 2008, p 552).
Nursing Care Plan for Low Self-Esteem
Nursing Care Plan for Low Self-Esteem Low self-esteem is a person rejects as something precious and is not responsible for their own lives. If the individual often fails it tends to lower self-esteem. Low self-esteem if it loses the love and appreciation of others. Self-esteem derived from self and others, the main aspect is to be accepted and received awards from other people. Low self-esteem disturbance described as negative feelings about themselves, including the loss of confidence and self esteem, sense of failure to reach the desire, self-criticism, reduced productivity, which is directed destructive to others, feelings of inadequacy, irritable and withdrawn socially. Nursing Care Plan for Low Self-Esteem Nursing Assessment for Low Self - Esteem
1. Subjective Data: Clients say: I can not afford, can not, do not know anything, stupid, self-
criticism, expressing feelings of shame about themselves.
2. Objective Data:
Clients looked more like himself, confused when asked to choose an alternative action, want to injure himself / want to end life. Nursing Diagnosis for Low Self - Esteem
1. Risk for Social Isolation : withdrawing associated with low self-esteem. 2. Self-Concept Disturbance : low self-esteem associated with dysfunctional grieving.
Nursing Intervention for Low Self - Esteem Goal
1. Clients can build a trusting relationship with nurses.
Action:
o
Construct a trusting relationship: Greetings therapeutic, self introduction, Explain the purpose, Create a peaceful environment, definition of contract (time, place and subject.)
o o o
Give clients the opportunity to express his feelings. Take time to listen to the client. Tell the client that he is someone who is valuable and responsible and able to help themselves.
2. Clients can identify the skills and positive aspects that are owned.
Action:
o o o
Discuss the capabilities and the positive aspects of client owned. Avoid giving negative assessments of each meet clients, give praise a realistic priority. Clients can assess the ability and positive aspect owned.
3. Clients can assess the capabilities that can be used.
Action:
o o
Discuss with the client's abilities can still be used. Discuss also the ability to continue after returning home.
4. Clients can define / plan activities appropriate capabilities.
Action:
o o o
Plan your activities with a client that can be done every day according to ability. Increase activities in accordance with client's tolerance condition. Give examples of how implementation of activities that clients should do.
5. Clients can perform activities according to the conditions and capabilities.
Action:
o o o
Give a chance to try activities that have been planned. Give praise for success Discuss the possibility of implementation at home.
6. Clients can utilize the existing support system.
Action:
o o o o
Give health education to families about how to care for clients. Helps families provide support for client care. Help prepare the family environment at home. Give positive reinforcement for family involvement.
NURSING DIAGNOSIS: Ineffective breathing pattern
related to: A. decreased rate and depth of respirations associated with the depressant effect of some medications (e.g. narcotic [opioid] analgesics, sedatives, centrally acting muscle relaxants) that may be given for treatment of current diagnosis; B. diminished lung/chest wall expansion associated with: 1. recumbent positioning (in this position, full expansion of the lungs is restricted by the bed surface and by the abdominal contents pushing up against the diaphragm) 2. weakness. Desired Outcome The client will maintain an effective breathing pattern as evidenced by normal rate and depth of respirations. Nursing Actions and Selected Purposes/Rationales A. Assess for signs and symptoms of an ineffective breathing pattern (e.g. shallow or slow respirations). B. Implement measures to improve breathing pattern: 1. place client in a semi- to high Fowler's position unless contraindicated; position client with pillows to prevent slumping 2. if client must remain flat in bed, assist with position change at least every 2 hours unless contraindicated 3. instruct client to deep breathe or use incentive spirometer every 1 - 2 hours 4. perform actions to reduce chest or abdominal pain if present (e.g. splint chest/abdomen with a pillow when positioning, coughing, and deep breathing; administer prescribed analgesics) in order to increase the client's willingness to move and breathe more deeply 5. perform actions to decrease fear and anxiety (see Diagnosis 13, action b) in order to prevent the shallow and/or rapid breathing that can occur with fear and anxiety 6. assist with positive airway pressure techniques (e.g. IPPB, continuous positive airway pressure [CPAP], bilevel positive airway pressure [BiPAP], expiratory positive airway pressure [EPAP]) if ordered 7. instruct client to avoid intake of gas-forming foods (e.g. beans, cauliflower, cabbage, onions), carbonated beverages, and large meals in order to prevent gastric distention and additional pressure on the diaphragm 8. increase activity as allowed 9. administer central nervous system depressants judiciously; hold medication and consult physician if respiratory rate is less than 12/minute.
C. Consult appropriate health care provider (e.g. physician, respiratory therapist) if: 1. ineffective breathing pattern continues 2. signs and symptoms of impaired gas exchange (e.g. restlessness, irritability, confusion, significant decrease in oximetry results, decreased PaO2 and increased PaCO2 levels) are present.
NURSING DIAGNOSIS: Altered urinary elimination: incontinence
related to: A. increased reflex activity of the bladder and loss of voluntary control of urinary elimination associated with upper motor neuron involvement if it has occurred; B. decreased ability to control urination associated with decreased level of consciousness or inability to recognize sensation of bladder fullness; C. inability to get to bedside commode or bathroom in a timely manner associated with: 1. delay in obtaining assistance resulting from inability to communicate the urge to urinate 2. impaired physical mobility. Desired Outcome The client will experience urinary continence. Nursing Actions and Selected Purposes/Rationales A. Assess client's pattern of fluid intake and urination (e.g. times and amounts of fluid intake, types of fluids consumed, times and amounts of voluntary and involuntary voiding, reports of sensation of need to void, activities preceding incontinence). B. Implement measures to reduce the risk of urinary incontinence: 1. offer bedpan or urinal or assist client to bedside commode or bathroom every 2-4 hours if indicated 2. allow client to assume a normal position for voiding unless contraindicated in order to promote complete bladder emptying 3. perform actions to reduce delays in toileting (e.g. have call signal within client's reach and respond promptly to requests for assistance; have bedpan, urinal, or bedside commode readily available to client; provide client with easy-to-remove clothing such as pajamas with Velcro closures or an elastic waistband) 4. if client is aphasic, establish an effective method for him/her to communicate the urge to urinate
5. instruct client to space fluids evenly throughout the day rather than drinking a large quantity at one time (rapid filling of bladder can result in incontinence if client has decreased urinary sphincter control) 6. limit oral fluid intake in the evening to decrease possibility of nighttime incontinence 7. instruct client to avoid drinking alcohol and beverages containing caffeine (alcohol and caffeine have a mild diuretic effect and act as irritants to the bladder; these factors may make urinary control more difficult). C. If urinary incontinence persists, consult physician about intermittent catheterization, insertion of indwelling catheter, or use of external catheter.
Nursing Diagnosis: Constipation Nursing care plans For Diagnosis Constipation NANDA Definition: A decrease in a person's normal frequency of defecation, accompanied by difficult or incomplete passage of stool and/or passage of excessively hard, dry stool
Suggested NOC Labels Bowel Elimination Hydration Client Outcomes Maintains passage of soft, formed stool every 1 to 3 days without straining States relief from discomfort of constipation Identifies measures that prevent or treat constipation NIC Interventions (Nursing Interventions Classification) Suggested NIC Labels Constipation/Impaction Management Nursing Interventions and Rationales
Observe usual pattern of defecation including time of day, amount and frequency of stool, consistency of stool, history of bowel habits or laxative use; diet including fluid intake; exercise patterns; personal remedies for constipation; obstetrical/gynecological history; surgeries; alterations in perianal sensation; present bowel regimen. There often are multiple reasons for constipation; the first step is assessment of usual patterns of bowel elimination. Have the client or family keep a diary of bowel habits including time of day; usual stimulus; consistency, amount, and frequency of stool; fluid consumption; and use of any aids to defecation. A diary of bowel habits is valuable in treatment of constipation. Review client's current medications. Many medications affect normal bowel function, including opiates, antidepressants, antihypertensives, anticholinergics, diuretics, anticonvulsants, antacids containing aluminum, iron supplements, and muscle relaxants.
Palpate for abdominal distention, percuss for dullness, and auscultate bowel sounds. In clients with constipation the abdomen is often distended with a palpable colon. Check for impaction; perform digital removal per physician's order. If impaction is present, use cleansing regimen until you obtain a very soft stool. If using an enema, the client must be able to bodily retain the fluid. If the client has poor sphincter tone, use a cone tip irrigating bag to assist the client in retaining the fluids. This also decreases the amount of fluid necessary for cleansing. Provide privacy for defecation. Assist the client to the bathroom and close the door if possible. Bowel elimination is a very private act, and a lack of privacy can contribute to constipation. Encourage fiber intake of 25 g/day for adults. Emphasize foods such as fresh fruits, beans, vegetables, and bran cereals. Add fiber to diet gradually. Fiber helps prevent constipation by giving stool bulk. Add fiber to diet gradually because a sudden increase can cause bloating, gas, and diarrhea. A daily fiber intake of 25 g can increase frequency of stools in clients with constipation. Dietary supplements of fiber in the form of bran or wheat fiber are helpful for women experiencing constipation with pregnancy. Encourage a fluid intake of 1.5 to 2 L/day (6 to 8 glasses of liquids per day). If oral intake is low, gradually increase fluid intake. Fluid intake must be within the cardiac and renal reserve. Adequate fluid intake is necessary to prevent hard, dry stools. Increasing fluid intake to 1.5 to 2 L/day along with fiber intake of 25 g can significantly increase frequency of stools in clients with constipation. Encourage client to be out of bed as soon as possible, and to own activities of daily living (ADLs) as able. Encourage exercises such as turning and changing positions in bed, lifting their hips off the bed, doing range of motion exercises, alternating lifting each knee to the chest, doing wheelchair lifts, doing waist twists, stretching arms away from body, and pulling in the abdomen while taking deep breaths. Activity, even minimal, increases peristalsis, which is necessary to prevent constipation. At each meal, sprinkle bran over client's food as allowed by client and prescribed diet. Ensure that client receives adequate fluid (1500 ml/day) along with bran. The number of bowel movements is increased and the use of laxatives is decreased in a client who eats wheat bran. A study done on institutionalized elderly male clients with chronic constipation demonstrated that with bran use, clients were able to discontinue use of oral laxatives. Initiate a regular schedule for defecation, using the client's normal evacuation time whenever possible. Offer hot coffee, hot lemon water, or prune juice before breakfast, or while sitting on the toilet if necessary. An optimal time for many individuals is 30 minutes after breakfast because of the gastrocolic reflex. A schedule gives the client a sense of control, but more importantly it promotes evacuation before drying of stool and constipation occur. Hot liquids can stimulate peristasis and result in defecation. Emphasize to the client the necessary ingredients for a normal bowel regimen (e.g., fluid, fiber, activity, and regular schedule for defecation). Help client onto bedside commode or toilet with client's hips flexed and feet flat. Have client deep breathe through mouth to encourage relaxation of the pelvic floor muscle and use the abdominal muscles to help evacuation. Provide laxatives, suppositories, and enemas as needed and as ordered only; establish a client goal of eliminating their use. Avoid soapsuds enemas, or use a low concentration of
castile soap only. Use of laxatives should be avoided. Soapsuds enemas can cause damage to the colonic mucosa. The use of a soapsuds enema was shown to increase stool output as compared with tap water enemas in preoperative liver transplant patients; amount of mucosal irritation was unknown. For the stable neurological client, consider use of a bowel routine of Therevac enema or suppositories every other day, or performing digital stimulation with physician's permission. For persistent constipation, refer to physician for evaluation. Use of the Therevac SB mini-enema was found to cut time needed for bowel care by as much as one hour or more as compared with use of suppositories.
Nursing Diagnosis: Bowel incontinence
Nursing Care Plans For Bowel incontinence
NANDA Definition: Change in normal bowel habits characterized by involuntary passage of stool NOC Outcomes (Nursing Outcomes Classification) Suggested NOC Labels Bowel Continence Bowel Elimination Client Outcomes Regular, complete evacuation of fecal contents from the rectal vault Defecates soft-formed stool Decreased or absence of bowel incontinence incidences Intact skin in the perianal/perineal area Demonstrates the ability to isolate, contract, and relax pelvic muscles , Increases pelvic muscle strength . NIC Interventions (Nursing Interventions Classification) Suggested NIC Labels Bowel Incontinence Care Bowel Training Bowel Incontinence Care: Encopresis Nursing Interventions and Rationales
In a reasonably private setting, directly question any client at risk about the presence of fecal incontinence. If the client reports altered bowel elimination patterns, problems with bowel control or "uncontrollable diarrhea," complete a focused nursing history including
previous and present bowel elimination routines, dietary history, frequency and volume of uncontrolled stool loss, and aggravating and alleviating factors. Unless questioned directly, patients are unlikely to report the presence of fecal incontinence. The nursing history determines the patterns of stool elimination to characterize involuntary stool loss and the likely etiology of the incontinence . Complete a focused physical assessment including inspection of perineal skin, pelvic muscle strength assessment, digital examination of the rectum for presence of impaction and anal sphincter strength, and evaluation of functional status (mobility, dexterity, visual acuity). A focused physical examination helps determine the severity of fecal leakage and its likely etiology. A functional assessment provides information concerning the impact of functional status on stool elimination patterns and incontinence. Complete an assessment of cognitive function. Dementia, acute confusion, and mental retardation are risk factors for fecal incontinence. Document patterns of stool elimination and incontinent episodes via a bowel record, including frequency of bowel movements, stool consistency, frequency and severity of incontinent episodes, precipitating factors, and dietary and fluid intake. This document is used to confirm the verbal history and to assist in determining the likely etiology of stool incontinence. It also serves as a baseline to evaluate treatment efficacy. Identify the probable causes of fecal incontinence. Fecal incontinence is frequently multifactorial; therefore identification of the probable etiology of fecal incontinence is necessary to select a treatment plan likely to control or eliminate the condition. Improve access to toileting:
o Identify usual toileting patterns among persons in the acute care or long term care facility and plan opportunities for toileting accordingly. o Provide assistance with toileting for patients with limited access or impaired functional status. o Institute a prompted toileting program for persons with impaired cognitive status. o Provide adequate privacy for toileting. o Respond promptly to requests for assistance with toileting. For the client with intermittent episodes of fecal incontinence related to acute changes in stool consistency, begin a bowel reeducation program consisting of: o Cleansing the bowel of impacted stool if indicated. o Normalizing stool consistency by adequate intake of fluids and dietary or supplemental fiber. o Establishing a regular routine of fecal elimination based on established patterns of bowel elimination
Begin a prompted defecation program for the adult with dementia, mental retardation, or related learning disabilities. Prompted urine and fecal elimination programs have been shown to reduce or eliminate incontinence in the long term care facility and community settings. Begin a scheduled stimulation defecation program, including the following steps, for persons with neurological conditions causing fecal incontinence:
o Before beginning the program, cleanse the bowel of impacted fecal material. o Implement strategies to normalize stool consistency, including adequate intake of fluid and fiber and avoidance of foods associated with diarrhea. o Whenever feasible, determine a regular schedule for bowel elimination based on previous patterns of bowel elimination. o Provide a stimulus before assisting the patient to a position on the toilet. Digital stimulation, stimulating suppository, "mini-enema," or pulsed evacuation enema may be used. The scheduled, stimulated defecation program relies on consistency of stool and a mechanical or chemical stimulus to produce a bolus contraction of the rectum with evacuation of fecal material.
Begin a pelvic floor reeducation or muscle exercise program for persons with sphincter incompetence or pseudodyssynergia of the pelvic muscles, or refer persons with fecal incontinence related to sphincter dysfunction to a nurse specialist or other therapist with clinical expertise in these techniques of care. Pelvic muscle reeducation, including biofeedback, pelvic muscle exercise, and/or pelvic muscle relaxation techniques, is a safe and effective treatment for selected persons with fecal incontinence related to sphincter or pelvic floor muscle dysfunction. Begin a pelvic muscle biofeedback program among patients with urgency to defecate and fecal incontinence related to recurrent diarrhea. Pelvic muscle reeducation, including biofeedback, can reduce uncontrolled loss of stool among persons who experience urgency and diarrhea as provacative factors for fecal incontinence. Reducing the incidence of diarrhea can help to reduce bowel incontinence. Cleanse the perineal and perianal skin following each episode of fecal incontinence. When incontinence is frequent, use an incontinence cleansing product specifically designed for this purpose. Frequent cleaning with soap and water may compromise perianal skin integrity and enhance the irritation produced by fecal leakage. Apply mineral oil or a petroleum based ointment to the perianal skin when frequent episodes of fecal incontinence occur. These products form a moisture and chemical barrier to the perianal skin that may prevent or reduce the severity of compromised skin integrity with severe fecal incontinence. Assist the patient to select and apply a containment device for occasional episodes of fecal incontinence. A fecal containment device will prevent soiling of clothing and reduce odors in the patient with uncontrolled stool loss. Teach the caregivers of the patient with frequent episodes of fecal incontinence and limited mobility to regularly monitor the sacrum and perineal area for pressure ulcerations. Limited mobility, particularly when combined with fecal incontinence, increases the risk of pressure ulceration. Routine cleansing, pressure reduction techniques, and management of fecal and urinary incontinence reduces this risk. Consult the physician concerning the use of an anal continence plug for the patient with frequent stool loss. The anal continence plug is a device that can reduce or eliminate persistent liquid or solid stool incontinence in selected patients. Apply a fecal pouch to the patient with frequent stool loss, particularly when fecal incontinence produces altered perianal skin integrity. Fecal pouches contain stool loss, reduce odor, and protect the perianal skin from chemical irritation resulting from contact with stool.
Consult the physician concerning the use of a rectal tube for the patient with severe fecal incontinence. A large-sized French indwelling catheter has been used for fecal containment when incontinence is severe and perianal skin integrity significantly compromised. The safety of this technique remains unknown.
S-ar putea să vă placă și
- Implant Failure and ManagementDocument59 paginiImplant Failure and ManagementDrIbrahimShaikh0% (1)
- 23 ENT DiordersDocument114 pagini23 ENT Diordersmohamed shamsÎncă nu există evaluări
- Healthcare StatisticsDocument20 paginiHealthcare StatisticsAnonymous ibmeej9Încă nu există evaluări
- Hematology - Oncology - PREP 2021Document46 paginiHematology - Oncology - PREP 2021drthanalla100% (1)
- Medicine English Fun Activities Games Grammar Drills Grammar Guides 17199Document20 paginiMedicine English Fun Activities Games Grammar Drills Grammar Guides 17199LisleÎncă nu există evaluări
- Procedures in Obstetrics and Gynaecology TextbookDocument272 paginiProcedures in Obstetrics and Gynaecology TextbookPriyaÎncă nu există evaluări
- Nursing Diagnosis For Coronary Artery Disease - Acute PainDocument2 paginiNursing Diagnosis For Coronary Artery Disease - Acute PainAngie Mandeoya100% (1)
- Valdez Reflective-Questions PDFDocument3 paginiValdez Reflective-Questions PDFDexel Lorren ValdezÎncă nu există evaluări
- Nursing Care PlanDocument26 paginiNursing Care PlanDinda MaretaÎncă nu există evaluări
- NCP Alzheimers DiseaseDocument2 paginiNCP Alzheimers DiseaseShawn TejanoÎncă nu există evaluări
- 1-Equine Digestion PowerPointDocument15 pagini1-Equine Digestion PowerPointMazhar FaridÎncă nu există evaluări
- SP CSDocument4 paginiSP CSKhan HansÎncă nu există evaluări
- Fistula NCPDocument1 paginăFistula NCPHasna LisnaÎncă nu există evaluări
- 1 Ineffective Airway ClearanceDocument8 pagini1 Ineffective Airway ClearanceEsel Mae DinamlingÎncă nu există evaluări
- 2014 Fundamentals of Skeletal Radiology, 4eDocument239 pagini2014 Fundamentals of Skeletal Radiology, 4eLuís RobertoÎncă nu există evaluări
- APOLONIO, JC - Natural Theory - Thomas AquinasDocument3 paginiAPOLONIO, JC - Natural Theory - Thomas AquinasJustin ApolonioÎncă nu există evaluări
- Guaifenesin Drug CardDocument1 paginăGuaifenesin Drug CardJessie JenningsÎncă nu există evaluări
- NCPDocument10 paginiNCPNefre Dayap DarrocaÎncă nu există evaluări
- NCP Self Care DeficitDocument3 paginiNCP Self Care DeficitLeizel ApolonioÎncă nu există evaluări
- Healthcare - Nursing Care Plan - Excess Fluid VolumeDocument4 paginiHealthcare - Nursing Care Plan - Excess Fluid VolumeBenjamin CañalitaÎncă nu există evaluări
- Novilyn C. Pataray BSN - Ii: Assessment Diagnosi S Pathophysiolog Y Planning Interevention Rationale EvaluationDocument1 paginăNovilyn C. Pataray BSN - Ii: Assessment Diagnosi S Pathophysiolog Y Planning Interevention Rationale EvaluationCharina AubreyÎncă nu există evaluări
- Narratives Case NotesDocument4 paginiNarratives Case NotesKnigh RiderÎncă nu există evaluări
- Burns - Skin Integrity, ImpairedDocument2 paginiBurns - Skin Integrity, Impairedmakyofrancis20Încă nu există evaluări
- MicrocephalyDocument4 paginiMicrocephalykurei_bluflamedÎncă nu există evaluări
- Assessmen T Diagnosis Planning Intervention Rationale EvaluationDocument3 paginiAssessmen T Diagnosis Planning Intervention Rationale EvaluationJoric MagusaraÎncă nu există evaluări
- Nursing Care Plans For Activity IntoleranceDocument4 paginiNursing Care Plans For Activity IntolerancethebigtwirpÎncă nu există evaluări
- NCP Alcoholic NeuropathyDocument5 paginiNCP Alcoholic NeuropathyPeachy Marie Anca100% (1)
- TAHBSO ReportDocument4 paginiTAHBSO ReportsachiiMeÎncă nu există evaluări
- NCP Blood Glucose Imbalance 4thDocument2 paginiNCP Blood Glucose Imbalance 4thRainier IbarretaÎncă nu există evaluări
- Case StudyDocument11 paginiCase StudyRadenroro Atih Utari RizkyÎncă nu există evaluări
- Nursing Care Plan ForDocument7 paginiNursing Care Plan ForVanessaMUellerÎncă nu există evaluări
- Content: Outline Form Only Make A Separate Sheet For The Content. The Health Teaching Plan Should Focus On Home Care For Patients With Mood DisorderDocument4 paginiContent: Outline Form Only Make A Separate Sheet For The Content. The Health Teaching Plan Should Focus On Home Care For Patients With Mood DisorderRaffy Sebastian Seballos100% (1)
- Activity IntoleranceDocument2 paginiActivity IntoleranceDiane AbanillaÎncă nu există evaluări
- Nursing Diagnosis, Planning, Implementation and EvaluationDocument1 paginăNursing Diagnosis, Planning, Implementation and EvaluationErjohn Vincent Lim100% (1)
- Nursing Interventions CHFDocument3 paginiNursing Interventions CHFbanyenye25100% (1)
- LCPDDocument7 paginiLCPDakoismeÎncă nu există evaluări
- NCPDocument2 paginiNCPAnne De VeraÎncă nu există evaluări
- MastitisDocument13 paginiMastitisapi-232713902Încă nu există evaluări
- FractureDocument1 paginăFractureReechie TeasoonÎncă nu există evaluări
- Managing Fatigue Through Activity Pacing and RestDocument2 paginiManaging Fatigue Through Activity Pacing and ResthaniehaehaeÎncă nu există evaluări
- Nursing Care Plan: Risk For Disuse SyndromeDocument2 paginiNursing Care Plan: Risk For Disuse SyndromeRozsy FakhrurÎncă nu există evaluări
- NCPDocument9 paginiNCPHendy Hency YunusÎncă nu există evaluări
- How to treat and prevent breast engorgementDocument1 paginăHow to treat and prevent breast engorgementkurniaÎncă nu există evaluări
- Assessment Diagnosis Planning Intervention Rationale EvaluationDocument4 paginiAssessment Diagnosis Planning Intervention Rationale EvaluationJhoizel VenusÎncă nu există evaluări
- Cord Prolapse March 23Document2 paginiCord Prolapse March 23Kathleen Vargas100% (1)
- Learning Derived (Lysha)Document1 paginăLearning Derived (Lysha)Choy DavidÎncă nu există evaluări
- 5ncp AnemiaDocument8 pagini5ncp Anemiabeverly_domingoÎncă nu există evaluări
- Retinopathy of PrematurityDocument15 paginiRetinopathy of Prematuritymarissa ulkhairÎncă nu există evaluări
- NCPDocument6 paginiNCPNik Rose ElÎncă nu există evaluări
- Nursing Care PlanDocument3 paginiNursing Care PlanJASMINE JOY BADUAÎncă nu există evaluări
- Lonzaga Assessment PDFDocument7 paginiLonzaga Assessment PDFNiño Naryana Luke PanchoÎncă nu există evaluări
- Cues Nursing Diagnosis Scientific Reason Objective Nursing Intervention Rationale EvaluationDocument4 paginiCues Nursing Diagnosis Scientific Reason Objective Nursing Intervention Rationale Evaluationjomsportg0% (1)
- Subjective:: Assessment Diagnosis Planning Implementation Rationale EvaluationDocument2 paginiSubjective:: Assessment Diagnosis Planning Implementation Rationale EvaluationAyra PunzalanÎncă nu există evaluări
- Cues Nursing Diagnosis Rationale Goals and Objectives Nursing Intervention Rationale Evaluation SubjectiveDocument4 paginiCues Nursing Diagnosis Rationale Goals and Objectives Nursing Intervention Rationale Evaluation SubjectiveFaye Dianne Damian-BuenafeÎncă nu există evaluări
- Case Study RespiDocument3 paginiCase Study RespiMark Jheran AlvarezÎncă nu există evaluări
- Nursing Care Plan EportfolioDocument14 paginiNursing Care Plan Eportfolioapi-279212367Încă nu există evaluări
- Propranolol, Prophylactic Warfarin, Low Molecular Weight Heparin (LMWH), Furosemide, AntibioticsDocument8 paginiPropranolol, Prophylactic Warfarin, Low Molecular Weight Heparin (LMWH), Furosemide, AntibioticsArlyn MarcelinoÎncă nu există evaluări
- NCP MRMDocument2 paginiNCP MRMKhloe Cristel Llanes Torres100% (1)
- Nursing Care Plan for GastroenteritisDocument7 paginiNursing Care Plan for GastroenteritisChris Denver BancaleÎncă nu există evaluări
- Case Study 2Document7 paginiCase Study 2desdav100% (1)
- Impaired Tissue PerfusionDocument2 paginiImpaired Tissue PerfusionLyka Mae Imbat - PacnisÎncă nu există evaluări
- LortabDocument1 paginăLortabSheri490Încă nu există evaluări
- Viii. Nursing Care Plan: Asessment Diagnosis Planning Intervention Rationale EvaluationDocument3 paginiViii. Nursing Care Plan: Asessment Diagnosis Planning Intervention Rationale Evaluationhehehe29Încă nu există evaluări
- Nursing Care Plan for Spinal Cord InjuryDocument3 paginiNursing Care Plan for Spinal Cord InjuryDan Leo UnicoÎncă nu există evaluări
- NCP FinalDocument7 paginiNCP FinalRuss RussÎncă nu există evaluări
- Nursing Care Plan for Pre-operative AnxietyDocument1 paginăNursing Care Plan for Pre-operative AnxietyVoid LessÎncă nu există evaluări
- Improve Patient Satisfaction ScoresDocument5 paginiImprove Patient Satisfaction ScoresAce TabioloÎncă nu există evaluări
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideDe la EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideÎncă nu există evaluări
- SENCHS Joins The Philippine Dengue AwarenessDocument3 paginiSENCHS Joins The Philippine Dengue AwarenessFhikery ArdienteÎncă nu există evaluări
- Winkler - Chapter 8. Khalid AlshareefDocument4 paginiWinkler - Chapter 8. Khalid AlshareefKhalid Bin FaisalÎncă nu există evaluări
- Assesment Diagnosis Planning Intervention Rationale EvaluationDocument2 paginiAssesment Diagnosis Planning Intervention Rationale EvaluationSienaÎncă nu există evaluări
- A Prospective Study On Acute Limb Ischemia - Presentation, Management, Outcome - Our Institutional ExperienceDocument6 paginiA Prospective Study On Acute Limb Ischemia - Presentation, Management, Outcome - Our Institutional ExperienceIJAR JOURNALÎncă nu există evaluări
- Pharmacology and The Older AdultDocument26 paginiPharmacology and The Older AdultJether Joy Hyacinth VelardeÎncă nu există evaluări
- NCP KoDocument1 paginăNCP Kojiellianemae100% (1)
- Analysis of The Concept of Successful Breastfeeding PDFDocument11 paginiAnalysis of The Concept of Successful Breastfeeding PDFAyu WulandariÎncă nu există evaluări
- All Mycoses SGDDocument140 paginiAll Mycoses SGDkashan100% (1)
- Heritage Health - Pre Auth FormDocument6 paginiHeritage Health - Pre Auth FormBOOKREADER_NOWÎncă nu există evaluări
- Malaria effects and causesDocument17 paginiMalaria effects and causesAnonymous XByxyTÎncă nu există evaluări
- ImmunosuppressionDocument1 paginăImmunosuppressionabc007200Încă nu există evaluări
- Presented by DR Rahul D AgrawalDocument64 paginiPresented by DR Rahul D AgrawalRahul AgrawalÎncă nu există evaluări
- Brain injury patterns in hypoxiaDocument7 paginiBrain injury patterns in hypoxiaDr.Deepak S MD,MRCPCHÎncă nu există evaluări
- Back Pain Differential DiagnosisDocument9 paginiBack Pain Differential DiagnosisSachin KpÎncă nu există evaluări
- J Paediatrics Child Health - 2017 - Halliday - The Fascinating Story of SurfactantDocument6 paginiJ Paediatrics Child Health - 2017 - Halliday - The Fascinating Story of SurfactantTin TomašićÎncă nu există evaluări
- Biosure RGDocument2 paginiBiosure RGJuan Martinez Del AngelÎncă nu există evaluări
- SRJI 4-3-2015 Historical Roots of Acupressure Pillows PatentsDocument4 paginiSRJI 4-3-2015 Historical Roots of Acupressure Pillows PatentsDr. Krishna N. SharmaÎncă nu există evaluări
- Temu Ilmiah Reumatologi (TIR) 2023 - Perhimpunan Reumatologi IndonesiaDocument1 paginăTemu Ilmiah Reumatologi (TIR) 2023 - Perhimpunan Reumatologi IndonesiabelanjayukdiÎncă nu există evaluări
- Primary Chest Wall Hydatid Cyst - A Rare Case Report: - PresenterDocument8 paginiPrimary Chest Wall Hydatid Cyst - A Rare Case Report: - PresenterEdison Varghese VadakkencheryÎncă nu există evaluări
- FNDRC Vol 2 AppendicesDocument43 paginiFNDRC Vol 2 AppendicesJohn Michael Macabenta100% (1)
- 2013 Pankaj R BodadeDocument8 pagini2013 Pankaj R BodadeGeorge StoicaÎncă nu există evaluări
- He367t R1 RCDocument2 paginiHe367t R1 RCSedighe VafaieÎncă nu există evaluări