Documente Academic
Documente Profesional
Documente Cultură
Nursing Care Plan For Pleural Effusion
Încărcat de
Joseph Angelo Fortuna CarmonaDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Nursing Care Plan For Pleural Effusion
Încărcat de
Joseph Angelo Fortuna CarmonaDrepturi de autor:
Formate disponibile
Nursing Care Plan for Pleural Effusion
NCP for Pleural Effusion
Pleural Effusion A pleural effusion is an excess accumulation of fluid in the pleural space around the lungs. Medical ImageThe pleura are thin membranes that enclose the lungs and line the inside of the chest cavity. The 'pleural space' describes the small space between the inner and outer layers of pleura, which normally contains a small volume of lubricating pleural fluid to allow the lungs to expand without friction. This fluid is constantly being formed through leakage of fluid from nearby capillaries and then re-absorbed by the body's lymphatic system. With a pleural effusion, some imbalance between production and reabsorption of pleural fluid leads to excess fluid building up in the pleural space. There are two major types of pleural effusion : Transudative effusions, where the excess pleural fluid is low in protein; and Exudative effusions, where the excess pleural fluid is high in protein. Causes Anything that causes an imbalance between production and reabsorption of pleural fluid can lead to development of a pleural effusion. Medical Image Transudative pleural effusions (those low in protein) usually form as a result of excess capillary fluid leakage into the pleural space. Common causes of transudative effusions include : Congestive heart failure; Nephrotic syndrome; Cirrhosis of the liver; Pulmonary embolism; and Hypothyroidism. Exudative effusions, which are high in protein, are often more serious than transudative effusions. They are formed as a result of inflammation of the pleura, which might happen for example in lung disease. Common causes of exudative effusions include : Pneumonia; Lung cancer, or other cancers; Connective tissue diseases, including rheumatoid arthritis and systemic lupus erythematosus; Pulmonary embolism; Asbestosis; Tuberculosis; and Radiotherapy. Source : virtualmedicalcentre.com
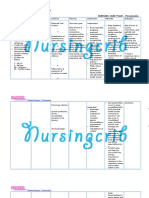
Nursing Care Plan for Pleural Effusion Nursing Assessment
1. 2. 3. 4. 5.
6.
Activity / rest Symptoms: dyspnea with activity or rest Circulation Signs: Tachycardia, dysrhythmias, heart rhythm Gallop, hypertension / hypotension Ego integrity Signs: fear, anxiety Food / fluid The existence of the installation of central venous IV / infusion Pain / comfort Symptoms depend on the size / area involved: Pain is aggravated by breathing in, the possibility of spread to the neck, shoulders, abdomen Signs: Be careful on the area of pain, behavioral distraction Respiratory Symptoms: Difficulty breathing, cough, history of chest surgery / trauma, Signs: Tachypnoea, use of accessory respiratory muscles in the chest, intercostal retraction, decreased breath sounds and decreased fremitus (on the side involved), Chest percussion: hyper resonant in the area filled with air and noise deaf in fluid-filled area Observation and palpation of the chest: chest movement is not the same (paradoksik) when trauma. Skin: pale, cyanosis, sweating.
Nursing Care Plan for Pleural Effusion
Definition A pleural effusion is an accumulation of fluid between the layers of tissue that line the lungs and chest cavity. Causes Your body produces pleural fluid in small amounts to lubricate the surfaces of the pleura, the thin tissue that lines the chest cavity and surrounds the lungs. A pleural effusion is an abnormal, excessive collection of this fluid. Two different types of effusions can develop : Transudative pleural effusions are caused by fluid leaking into the pleural space. This is caused by elevated pressure in, or low protein content in, the blood vessels. Congestive heart failure is the most common cause.
Exudative effusions usually result from leaky blood vessels caused by inflammation (irritation and swelling) of the pleura. This is often caused by lung disease. Examples include lung cancer, lung infections such as tuberculosis and pneumonia, drug reactions, and asbestosis.
Symptoms Chest pain, usually a sharp pain that is worse with cough or deep breaths Cough Fever Hiccups Rapid breathing Shortness of breath Source : http://www.nlm.nih.gov/medlineplus Assessment 1. Patient identity At this stage the nurse needs to know about the name, age, gender, home address, religion or belief, ethnicity, languages spoken, education and employment status of patients. 2. Main complaint The main complaint is the main factor that encourages patients to seek help or treatment to the hospital. Usually in patients with acquired pleural effusi complaint form shortness of breath, feeling the weight on the chest, pain due to irritation of the pleura Pleuritic that is sharp and localized, especially when coughing and breathing as well as non-productive cough. Disease History Now Patients with pleural effusi will usually preceded by signs such as cough, shortness of breath, pain Pleuritic, heavy feeling in chest, weight loss and so on. There should also be asked from any complaints that arise. What action has been taken to reduce or eliminate these complaints. Formerly Disease History To ask whether the patient had suffered from lung diseases such as tuberculosis, pneumoni, heart failure, trauma, ascites, and so on. This is needed to determine possible predisposing factors. Family Disease History To ask whether any family members who suffer from diseases that was allegedly the cause of pleural effusi like Ca lung, asthma, pulmonary tuberculosis and others. Psychosocial History Include feelings of illness of patients, how to handle it and how the patient's behavior toward action taken against him.
3.
4.
5.
6.
Nursing Diagnosis Ineffective breathing pattern related to decreased lung expansion secondary to accumulation of fluid in the pleural cavity Nursing Plan Objectives : Patients able to maintain normal lung function Criterion Results : Rhythm, frequency and depth of breathing in the normal range, the chest X-ray examinations did not find any accumulation of fluid, audible breath sounds. Plan of action : Identify the causative factor. Rational: By identifying the causes, we can determine which type of pleural effusi can take appropriate action.
Examine the quality, frequency and depth of breathing, report any changes that occur. Rational: By reviewing the quality, frequency and depth of breathing, we can determine how far the patient's condition changes. Lay the patient in a comfortable position, in a sitting position, with the head of the bed elevated 60 to 90 degrees. Rational: Decrease the diaphragm to expand the chest so the lungs can expand the maximum. Observation of vital signs (temperature, pulse, blood pressure, RR and response of patients). Rational: Improved tachcardi RR and an indication of decline in lung function. Perform auscultation of breath sounds every 2-4 hours. Rational: to determine abnormalities Auscultation of breath sounds in the lungs. Help and teach the patient to cough and breath in effective. Rational: Pressing the painful area when coughing or breathing deeply. Emphasis pectoral muscle and abdominal makes cough more effective. Collaboration with other medical teams to deliver O2 and medicines as well as thorax images. Rational: Giving oxygen may reduce the load and prevent the occurrence of respiratory cyanosis due hiponia. With the thorax images can be monitored the progress of the reduction in fluid and the return of flower power lung.
Nursing Care Plan for Diabetes Mellitus
NCP - Nursing Care Plan for Diabetes Mellitus
Diabetes Mellitus Diabetes mellitus, often simply referred to as diabetesis a group of metabolic diseases in which a person has high blood sugar, either because the body does not produce enough insulin, or because cells do not respond to the insulin that is produced. This high blood sugar produces the classical symptoms of polyuria (frequent urination), polydipsia (increased thirst) and polyphagia (increased hunger). There are three main types of diabetes : Type 1 diabetes: results from the body's failure to produce insulin, and presently requires the person to inject insulin. (Also referred to as insulin-dependent diabetes mellitus, IDDM for short, and juvenile diabetes.) Type 2 diabetes: results from insulin resistance, a condition in which cells fail to use insulin properly, sometimes combined with an absolute insulin deficiency. Gestational diabetes: is when pregnant women, who have never had diabetes before, have a high blood glucose level during pregnancy. It may precede development of type 2 DM. Other forms of diabetes mellitus include congenital diabetes, which is due to genetic defects of insulin secretion, cystic fibrosis-related diabetes, steroid diabetes induced by high doses of glucocorticoids, and several forms of monogenic diabetes. All forms of diabetes have been treatable since insulin became available in 1921, and type 2 diabetes may be controlled with medications. Both type 1 and 2 are chronic conditions that usually cannot be cured. Pancreas transplants have been tried with limited success in type 1 DM; gastric bypass surgery has been successful in many with morbid obesity and type 2 DM. Gestational diabetes usually resolves after delivery. Diabetes without proper treatments can cause many complications. Acute complications include hypoglycemia, diabetic ketoacidosis, or nonketotic hyperosmolar coma. Serious long-term complications include cardiovascular disease, chronic renal failure, retinal damage. Adequate treatment of diabetes is thus important, as well as blood pressure control and lifestyle factors such as smoking cessation and maintaining a healthy body weight.en.wikipedia.org
Causes The cause of diabetes depends on the type. Type 2 diabetes is due primarily to lifestyle factors and genetics. Type 1 diabetes is also partly inherited and then triggered by certain infections, with some evidence pointing at Coxsackie B4 virus. There is a genetic element in individual susceptibility to some of these triggers which has been traced to particular HLA genotypes (i.e., the genetic "self" identifiers relied upon by the immune system). However, even in those who have inherited the susceptibility, type 1 diabetes mellitus seems to require an environmental trigger. Signs and Symptoms The classical symptoms of diabetes are polyuria (frequent urination), polydipsia (increased thirst) and polyphagia (increased hunger). Symptoms may develop rapidly (weeks or months) in type 1 diabetes while in type 2 diabetes they usually develop much more slowly and may be subtle or absent. Prolonged high blood glucose causes glucose absorption, which leads to changes in the shape of the lenses of the eyes, resulting in vision changes; sustained sensible glucose control usually returns the lens to its original shape. Blurred vision is a common complaint leading to a diabetes diagnosis; type 1 should always be suspected in cases of rapid vision change, whereas with type 2 change is generally more gradual, but should still be suspected. People (usually with type 1 diabetes) may also present with diabetic ketoacidosis, a state of metabolic dysregulation characterized by the smell of acetone; a rapid, deep breathing known as Kussmaul breathing; nausea; vomiting and abdominal pain; and an altered states of consciousness. A rarer but equally severe possibility is hyperosmolar nonketotic state, which is more common in type 2 diabetes and is mainly the result of dehydration. Often, the patient has been drinking extreme amounts of sugar-containing drinks, leading to a vicious circle in regard to the water loss. A number of skin rashes can occur in diabetes that are collectively known as diabetic dermadromes.
Nursing Care Plan for Diabetes Mellitus Assessment Family Health History Are there families who suffer from illnesses such as client ? Patient Health History and Previous Treatment How long suffered from DM client, how to handle, get what kind of insulin therapy, how to take the medicine whether regular or not, what is done to cope with illness clients. Activity / Rest: Tired, weak, hard Moves / walking, muscle cramps, decreased muscle tone. Circulation Is there a history of hypertension, AMI, claudication, numbness, tingling in the extremities, ulcers on the feet long healing time, tachycardia, changes in blood pressure Ego Integrity Stress, anxiety Elimination Changes in the pattern of urination (polyuria, nocturia, anuria), diarrhea Food / Fluids Anorexia, nausea, vomiting, do not follow the diet, weight loss, thirst, the use of diuretics. Neurosensori Dizziness, headache, numbness, muscle weakness numbness, paraesthesia, visual disturbances. Pain / Leisure Abdominal strain, pain (is / weight) Respiratory Cough with or without purulent sputum
Security Dry skin, itching, skin ulcer.
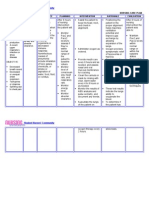
Nursing Diagnosis and Nursing Intervention Fluid volume deficient related to osmotic diuresis from hyperglycemia Planning After 8 hours of nursing interventions, the patient will demonstrate adequate hydration. Intervention Monitor orthostatic blood pressure changes. Rational : Hypovolemia may be manifested by hypotension and tachycardia. Assess peripheral pulses, capillary refill, skin turgor, and mucous membrane. Rational : Indicators of level of dehydration, adequacy of circulating volume. Monitor respiratory pattern like Kussmauls respirations and acetone breath. Rational : Lungs remove carbonic acid through respirations, producing a compensatory respiratory alkalosis for ketoacidosis. Monitor input and output. Note urine specific gravity. Rational : Provides ongoing estimate of volume replacement needs, kidney function, and effectiveness of therapy. Promote comfortable environment. Cover patient with light sheets. Rational : Avoids overheating, which could promote further fluid loss. Monitor temperature, skin color and moisture. Rational : Fever, chills, and diaphoresis are common with infectious process; fever with flushed, dry skin may reflect dehydration.
1. Deficient Fluid Volume
Glucose appears in the urine (glycosuria) because the kidney excretes the excess glucose to make the blood glucose level normal. Glucose excreted in the urine acts as osmotic diuretic and causes excretion of increased amount of water, resulting in fluid volume deficit or polyuria.
Assessment Nursing Planning Diagnosi s Nursing Rationale Evaluation Interventio ns
Subjective: (none)
Objective:
elevated temperatur e of 38.4C/axill a increased urine output. sweating of the skin thirst exhaustion weight loss dry skin or mucous membrane
Deficient Short Establish Friendly Short Fluid Term:After 3 rapportTake relationship Term:After 3 Volume of NI, patient and record with patient of NI, patient r/t shall have vital and to be will have intracellu verbalized signsMonitor able to each verbalized lar DHN understanding the others understanding 2 the of causative temperature concernTo of causative DM II factors and obtain factors and purpose of baseline purpose of Assess skin turgor and individual dataTo individual mucous therapeutic monitor therapeutic membranes for changes in interventions interventions signs of and temperatur and dehydration e medications.Lo medications.L ng Term:After ong Encourage the 2 days of NI, Dry skin and Term:After 2 patient to mucous the patient days of NI, the increase fluid membranes patient will shall have intake are signs of have maintained dehydration maintained fluid volume at Administer a functional fluid volume at IVF as ordered To replace level as a functional by the Doctor fluid loss and level as evidenced by prevent individual good Administer evidenced by dehydration skin turgor, individual anti-pyretic as moist mucous prescribed by To replace good skin the Doctor. membrane and electrolytes turgor, moist stable vital and fluid loss mucous signs. membrane To decrease and stable vital signs body
temperature
and will have less occurrence of dehydration.
S-ar putea să vă placă și
- Nursing Care PlanDocument13 paginiNursing Care PlanCris Solis33% (3)
- 6 Pleural Effusion Nursing Care PlansDocument7 pagini6 Pleural Effusion Nursing Care PlansShaina Fe RabaneraÎncă nu există evaluări
- 1 Ineffective Breathing PatternDocument8 pagini1 Ineffective Breathing PatternNoel MontemayorÎncă nu există evaluări
- Nursing Care Plans For UTIDocument2 paginiNursing Care Plans For UTIHannah Pin67% (3)
- Impaired Gas ExchangeDocument3 paginiImpaired Gas ExchangeBenedicto RosalÎncă nu există evaluări
- Chronic Obstructive Bronchitis Is An Inflammation of The BronchiDocument9 paginiChronic Obstructive Bronchitis Is An Inflammation of The Bronchiinamaliit100% (1)
- A Renal Failure (NCP)Document2 paginiA Renal Failure (NCP)Julie Aranda Hapin100% (1)
- Case Study Pleural EffusionDocument4 paginiCase Study Pleural EffusionKhristine Anne FabayÎncă nu există evaluări
- ANOLIN, Marc Edriann T. Nursing Care Plan Assessmen T Diagnosis Rationale Planning Interventio N Rationale EvaluationDocument2 paginiANOLIN, Marc Edriann T. Nursing Care Plan Assessmen T Diagnosis Rationale Planning Interventio N Rationale EvaluationEdrianne Tui100% (2)
- HYPERVOLEMIA CAREDocument2 paginiHYPERVOLEMIA CAREAlroi Abrantes50% (2)
- NCP For StokeDocument5 paginiNCP For StokeMemedÎncă nu există evaluări
- Risk For Decreased Cardiac OutputDocument3 paginiRisk For Decreased Cardiac OutputSid Artemis FriasÎncă nu există evaluări
- Student Nurses' Community: Nursing Care Plan Assessment Diagnosis Inference Planning Intervention Rationale EvaluationDocument3 paginiStudent Nurses' Community: Nursing Care Plan Assessment Diagnosis Inference Planning Intervention Rationale Evaluationgreyciee은Încă nu există evaluări
- Pleural Effusion NCPsDocument7 paginiPleural Effusion NCPsJaja Nagallo100% (2)
- NCP PTBDocument2 paginiNCP PTBKath TalubanÎncă nu există evaluări
- Heart Failure NCPDocument9 paginiHeart Failure NCPMiriam EstradaÎncă nu există evaluări
- Nursing ManagementDocument16 paginiNursing ManagementNica Marie LumbaÎncă nu există evaluări
- Nursing Care PlansDocument5 paginiNursing Care PlansMa Liezel M Camba100% (1)
- Nursing Care PlanDocument10 paginiNursing Care PlanMalou SanÎncă nu există evaluări
- Ineffective Breathing PatternDocument185 paginiIneffective Breathing PatternSusi LambiyantiÎncă nu există evaluări
- Pleural EffusionDocument5 paginiPleural EffusionTerizla MobileÎncă nu există evaluări
- Nursing Care Plan for PneumoniaDocument3 paginiNursing Care Plan for PneumoniaFARAH MAE MEDINAÎncă nu există evaluări
- Chronic Obstructive Pulmonary Disease (COPD)Document1 paginăChronic Obstructive Pulmonary Disease (COPD)Bheru LalÎncă nu există evaluări
- NCP PTBDocument2 paginiNCP PTBMack Jhed AnarconÎncă nu există evaluări
- Assessment Nursing Diagnosis Inference Objectives Nursing Intervention Rationale EvaluationDocument10 paginiAssessment Nursing Diagnosis Inference Objectives Nursing Intervention Rationale EvaluationJobelle AcenaÎncă nu există evaluări
- Far Eastern University Nursing Care Plan Nursing Diagnosis Analysis Goals and Objectives Intervention Rationale EvaluationDocument1 paginăFar Eastern University Nursing Care Plan Nursing Diagnosis Analysis Goals and Objectives Intervention Rationale EvaluationSarah CarreteroÎncă nu există evaluări
- NCP BMDocument1 paginăNCP BMSourabh MehraÎncă nu există evaluări
- Nursing Care PlanDocument3 paginiNursing Care Planjnx_anonymousÎncă nu există evaluări
- Causes and Nursing Care of Pleural EffusionDocument4 paginiCauses and Nursing Care of Pleural EffusionHania Polangi100% (1)
- Ineffective Airway Clearance-Nursing Care Plan For COPDDocument2 paginiIneffective Airway Clearance-Nursing Care Plan For COPDRnspeakcom100% (1)
- Nursing Care for Pleuritic Chest PainDocument1 paginăNursing Care for Pleuritic Chest PainAira AlaroÎncă nu există evaluări
- Nursing Care Plan 7 Knowledge DeficitDocument8 paginiNursing Care Plan 7 Knowledge Deficitdbryant0101100% (8)
- Ineffective Airway ClearanceDocument2 paginiIneffective Airway ClearanceHanya Bint PotawanÎncă nu există evaluări
- Ineffective Airway Clearance CareplanDocument6 paginiIneffective Airway Clearance CareplanderreshaÎncă nu există evaluări
- Asthma Nanda Diagnoses Goals InterventionsDocument4 paginiAsthma Nanda Diagnoses Goals InterventionsZinya RobinsonÎncă nu există evaluări
- Nursing Care Plan 6 Impaired Gas ExchangeDocument9 paginiNursing Care Plan 6 Impaired Gas Exchangedbryant0101100% (12)
- Managing Impaired Gas Exchange in an Elderly COPD PatientDocument23 paginiManaging Impaired Gas Exchange in an Elderly COPD PatientKaren Joyce Costales Magtanong100% (3)
- Nursing Care PlanDocument4 paginiNursing Care Planapi-309251523Încă nu există evaluări
- NCP Baby DDocument3 paginiNCP Baby DYna LafuenteÎncă nu există evaluări
- Nursing Care Plan FinalDocument16 paginiNursing Care Plan FinalErickson OcialÎncă nu există evaluări
- Nursing Care Plan 2Document6 paginiNursing Care Plan 2ayanori_boyÎncă nu există evaluări
- NCP PneumoniaDocument2 paginiNCP PneumoniaChristian Apelo Serquillos100% (2)
- Nursing Care Plan HF FinalDocument10 paginiNursing Care Plan HF FinalCristina L. JaysonÎncă nu există evaluări
- NCPDocument15 paginiNCPCamille PinedaÎncă nu există evaluări
- Asthma Nursing Care Plan NCP Ineffective Airway Clearance CompressDocument2 paginiAsthma Nursing Care Plan NCP Ineffective Airway Clearance CompressMargarette GeresÎncă nu există evaluări
- Heart Perfusion Nursing CareDocument12 paginiHeart Perfusion Nursing CareSesinando Niez Quilao Jr.100% (1)
- Nursing Care Plan For Heart Failure ChronicDocument26 paginiNursing Care Plan For Heart Failure ChronicbrantÎncă nu există evaluări
- Content: Outline Form Only Make A Separate Sheet For The Content. The Health Teaching Plan Should Focus On Home Care For Patients With Mood DisorderDocument4 paginiContent: Outline Form Only Make A Separate Sheet For The Content. The Health Teaching Plan Should Focus On Home Care For Patients With Mood DisorderRaffy Sebastian Seballos100% (1)
- NCP BronchopneumoniaDocument8 paginiNCP BronchopneumoniaCrisantaCasliÎncă nu există evaluări
- Novilyn C. Pataray BSN - Ii Cystic Fibrosis: St. Paul College of Ilocos SurDocument1 paginăNovilyn C. Pataray BSN - Ii Cystic Fibrosis: St. Paul College of Ilocos SurCharina AubreyÎncă nu există evaluări
- NCP Acitivity IntoleranceDocument3 paginiNCP Acitivity IntolerancegizelleÎncă nu există evaluări
- Sample CHN Teaching Learning GuideDocument3 paginiSample CHN Teaching Learning GuideSUREEN MAY ANG REGULARÎncă nu există evaluări
- Nursing Care Plan - Pulmonary EmbolismDocument3 paginiNursing Care Plan - Pulmonary EmbolismPui_Yee_Siow_6303100% (10)
- Risk For InjuryDocument2 paginiRisk For InjuryRo-anne AkuÎncă nu există evaluări
- Pleural Effusion: Presented By:-Gayathri Gopakumar BSC - Nursing 2 YearDocument30 paginiPleural Effusion: Presented By:-Gayathri Gopakumar BSC - Nursing 2 YearGAYATHRI GOPAKUMARÎncă nu există evaluări
- NCP PleuralDocument5 paginiNCP Pleuraljanine_valdezÎncă nu există evaluări
- Kelvin RHDDocument33 paginiKelvin RHDWizy KayzÎncă nu există evaluări
- Pleural Effusion: PathophysiologyDocument6 paginiPleural Effusion: PathophysiologyNyamburaÎncă nu există evaluări
- Pneumonia Symptoms ExplainedDocument13 paginiPneumonia Symptoms Explainedshenecajean carajay100% (1)
- Women's Pneumonia ReportDocument9 paginiWomen's Pneumonia ReportNohaira SADANGÎncă nu există evaluări
- Demi-Human Headgear SetDocument5 paginiDemi-Human Headgear SetJoseph Angelo Fortuna CarmonaÎncă nu există evaluări
- D (Data) A (Action) R (Response)Document1 paginăD (Data) A (Action) R (Response)Joseph Angelo Fortuna CarmonaÎncă nu există evaluări
- Congestive Heart FailureDocument8 paginiCongestive Heart Failureiancel_038893% (27)
- Reaction ChloeDocument1 paginăReaction ChloeErick CarmonaÎncă nu există evaluări
- Drug StudyDocument7 paginiDrug StudyJoseph Angelo Fortuna CarmonaÎncă nu există evaluări
- Pepper WhereDocument1 paginăPepper WhereJoseph Angelo Fortuna CarmonaÎncă nu există evaluări
- D (Data) A (Action) R (Response)Document1 paginăD (Data) A (Action) R (Response)Joseph Angelo Fortuna CarmonaÎncă nu există evaluări
- Pathophysiology of Dengue Hemorrhagic FeverDocument1 paginăPathophysiology of Dengue Hemorrhagic FeverJoseph Angelo Fortuna CarmonaÎncă nu există evaluări
- Skeleton of ChickenDocument8 paginiSkeleton of ChickenShoulder HackerÎncă nu există evaluări
- The Lung Meridian Acu-PointsDocument1 paginăThe Lung Meridian Acu-PointsVicaas VSÎncă nu există evaluări
- Case 1-Clinical Case StudyDocument4 paginiCase 1-Clinical Case StudyRachel VillanuevaÎncă nu există evaluări
- CTT NSG CareDocument11 paginiCTT NSG CareLigriv Ssor AllirevaÎncă nu există evaluări
- Respiratory EmergencyDocument14 paginiRespiratory EmergencyThomas SentanuÎncă nu există evaluări
- Exercises and Yoga For Cervical Spondylosis: Neck PainDocument5 paginiExercises and Yoga For Cervical Spondylosis: Neck PainKaran Aggarwal100% (2)
- MODULE 4-Do's and Don'Ts in Physical Activities and Exercise Proper Breathing and Warm-Up - StretchingDocument65 paginiMODULE 4-Do's and Don'Ts in Physical Activities and Exercise Proper Breathing and Warm-Up - StretchingAljeya EvanchezÎncă nu există evaluări
- Simulation Scenarios PDFDocument59 paginiSimulation Scenarios PDFryan24Încă nu există evaluări
- Physical Assessment TemplateDocument9 paginiPhysical Assessment TemplateArky VessaliuzÎncă nu există evaluări
- New Microsoft Word DocumentDocument18 paginiNew Microsoft Word Documentapi-427712934Încă nu există evaluări
- 3.3 The Intercostal Spaces and MuscleDocument8 pagini3.3 The Intercostal Spaces and MuscleCearlene GalleonÎncă nu există evaluări
- Kinesiotaping For Isolated Rib Fractures in Emergency DepartmentDocument10 paginiKinesiotaping For Isolated Rib Fractures in Emergency DepartmentDaniel GuevaraÎncă nu există evaluări
- Full Body Reflexology Chart Template Free PDF Format PDFDocument37 paginiFull Body Reflexology Chart Template Free PDF Format PDFShadrina Al Shafama100% (3)
- This Study Resource Was Shared Via: Assessment Nursing Diagnosis Inference Goal Nursing Intervention Rationale EvaluationDocument3 paginiThis Study Resource Was Shared Via: Assessment Nursing Diagnosis Inference Goal Nursing Intervention Rationale EvaluationJanine Dela CruzÎncă nu există evaluări
- Bronchoscopy: DR Supriya Kokane-PatilDocument18 paginiBronchoscopy: DR Supriya Kokane-PatilPARAG PATIL100% (1)
- DR Nury Jumat Nury - RevDocument46 paginiDR Nury Jumat Nury - RevJerry Kurnia WahyudiÎncă nu există evaluări
- 9 People Vs Pagador G.R. Nos. 140006-10Document18 pagini9 People Vs Pagador G.R. Nos. 140006-10Cheza ComiaÎncă nu există evaluări
- Life Saving Pocket - GuideDocument10 paginiLife Saving Pocket - GuideNur FarhanaÎncă nu există evaluări
- A Patient With Fever and CoughDocument3 paginiA Patient With Fever and CoughJefferson MorenoÎncă nu există evaluări
- Chest Pain Types and Causes ExplainedDocument2 paginiChest Pain Types and Causes ExplainedGerryNickÎncă nu există evaluări
- Essentials of Physiotherapy After Thoracic Surgery - What Physiotherapists Need To Know. A Narrative ReviewDocument15 paginiEssentials of Physiotherapy After Thoracic Surgery - What Physiotherapists Need To Know. A Narrative ReviewMariana MadridÎncă nu există evaluări
- Pathophysiology of pneumothorax and hemothoraxDocument3 paginiPathophysiology of pneumothorax and hemothoraxAllana RayosÎncă nu există evaluări
- Reinterpreting Ba Duan Jing From The Theories of The Eight Extra MeridiansDocument20 paginiReinterpreting Ba Duan Jing From The Theories of The Eight Extra MeridiansAdrian Stan100% (1)
- RIB FractureDocument46 paginiRIB Fracturebanjar1982Încă nu există evaluări
- Chest Tube Nursing CareDocument1 paginăChest Tube Nursing CareVanessa LadraÎncă nu există evaluări
- Attending SkillsDocument31 paginiAttending SkillsAllysa Marie CotandaÎncă nu există evaluări
- IV. Physical Assessment Norms Actual Findings Interpretation and Analysis General Appearance Posture / GaitDocument9 paginiIV. Physical Assessment Norms Actual Findings Interpretation and Analysis General Appearance Posture / GaitMarianne_Miraflo_154Încă nu există evaluări
- Allied Health Science: B.Sc. Dialysis TechnologyDocument26 paginiAllied Health Science: B.Sc. Dialysis TechnologyNk Tower0% (1)
- Surprising Causes of Chest PainDocument4 paginiSurprising Causes of Chest PainRaprnaÎncă nu există evaluări