Documente Academic
Documente Profesional
Documente Cultură
A& P Notes
Încărcat de
JSeasharkTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
A& P Notes
Încărcat de
JSeasharkDrepturi de autor:
Formate disponibile
Anatomy & Physiology
Outlines of Selected Book Chapters
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
1. AN INTRODUCTION TO THE HUMAN BODY
I. ANATOMY AND PHYSIOLOGY DEFINED A. Through a study of anatomy and its subdivisions, the body may be examined at different levels of structural organization. 1. Anatomy may be defined as the study of structure and the relationships among structures. 2. Subdivisions of anatomy include surface anatomy, gross anatomy, systemic anatomy, regional anatomy, radiographic anatomy, developmental anatomy, embryology, cytology, and pathological anatomy. B. A study of physiology deals with how body parts function: the structure of a part determines its function. 1. 2. Physiology is the study of how body structures function. Subdivisions of physiology include cell physiology, systems physiology, pathophysiology, exercise physiology, neurophysiology, endocrinology, cardiovascular physiology, immunophysiology, respiratory physiology, renal physiology, and reproductive physiology. C. Three noninvasive techniques of palpation, auscultation, and percussion are used to assess certain aspects of body structure and function. 1. In palpation the examiner feels body surfaces with the hands; an example would be pulse and heart rate determination. 2. In auscultation, the examiner listens to body sounds to evaluate the functioning of certain organs, as in listening to the lungs or heart. 3. In percussion, the examiner taps on the body surface with the fingertips and listens to the resulting echo.
II.
LEVELS OF ORGANIZATION A. The human body consists of several levels of structural organization. 1. The chemical level includes atoms, the smallest units of matter that participate in chemical reactions, and molecules, two or more atoms joined together. 2. 3. Cells are the basic structural and functional units of an organism. Tissues consist of groups of similarly specialized cells and the substances surrounding them that usually arise from a common ancestor and perform certain special functions. 4. Organs are structures of definite form that are composed of two or more different tissues and have specific functions. 5. 6. Systems consist of related organs that have a common function. The human organism is a collection of structurally and functionally integrated systems; any living individual.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
B.
The systems of the human body are the integumentary, skeletal, muscular, nervous, endocrine, cardiovascular, lymphatic, respiratory, urinary, and reproductive.
III.
CHARACTERISTICS of the LIVING HUMAN ORGANISM A. Basic Life Processes
1. All living things have certain characteristics that distinguish them from nonliving things. 2. Among the life processes in humans are metabolism, responsiveness, movement,
growth, differentiation, and reproduction. a. Metabolism is the sum of all chemical processes that occur in the body, including catabolism and anabolism. b. Responsiveness is the ability to detect and respond to changes in the external or internal environment. c. Movement includes motion of the whole body, individual organs, single cells, or even organelles inside cells. d. Growth refers to an increase in size and complexity, due to an increase in the number of cells, size of cells, or both. e. Differentiation is the change in a cell from an unspecialized state to a specialized state. f. Reproduction refers either to the formation of new cells for growth, repair, or replacement, or the production of a new individual. 3. An autopsy (as discussed in a clinical application) is a postmortem examination of the body and dissection of its internal organs to confirm or determine the cause of death. B. Homeostasis is a condition of equilibrium in the body s internal environment produced by the ceaseless interplay of all the body s regulatory processes. C. Body Fluids
1. For the body s cells to survive, the composition of the surrounding fluids must be
precisely maintained at all times.
a. Fluid inside body cells is called intracellular fluid. b. Fluid outside body cells is called extracellular fluid (ECF) and is found in two
principal places.
1) ECF filling the narrow spaces between cells of tissues is called
interstitial fluid, intercellular fluid, or tissue fluid.
2) ECF in blood vessels is termed plasma. 2. Since ECF is in constant motion throughout the body and also surrounds all body cells, it
is often called the body s internal environment.
IV.
CONTROL OF HOMEOSTASIS A. Homeostatic imbalances occur because of disruptions from the external or internal environments.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
B.
Homeostasis is regulated by the nervous system and endocrine system, acting together or independently.
1. The nervous system detects changes and sends nerve impulses to counteract the
disruption.
2. The endocrine system regulates homeostasis by secreting hormones. 3. Whereas nerve impulses cause rapid changes, hormones usually work more slowly.
C. Feedback Systems
1. General Principles
a. A feedback system is a cycle of events in which information about the status of a condition is continually monitored and fed back (reported) to a central control region (Figure 1.2). b. c. Any disruption that changes a controlled condition is called a stimulus. A feedback system consists of three basic components. 1) A receptor monitors changes in a controlled condition and sends input in the form of nerve impulses or chemical signals to a control center. 2) The control center sets the range of values within which a controlled condition should be maintained, evaluates the input it receives from the receptors, and generates output commands when they are needed. 3) An effector is a body structure that receives output from the control center and produces a response or effect that changes the controlled condition. d. If a response reverses the original stimulus, the system is a negative feedback system. e. If a response enhances the original stimulus, the system is a positive feedback system. D. Negative Feedback Systems
1. A negative feedback system reverses a change in a controlled condition. 2. Homeostasis of Blood Pressure (BP): Negative Feedback (Figure 1.3) a. If a stimulus (stress) causes blood pressure (controlled condition) to rise,
pressure-sensitive cells (baroreceptors) in certain arteries send impulses (input) to the brain (control center). The brain sends impulses (output) to the heart (effector), causing the heart rate to decrease (response) and return of blood pressure to normal (restoration of homeostasis).
b. The activity of the effector produces a result, a drop in blood pressure, that
opposes the stimulus, an increase in blood pressure.
E. Positive Feedback System
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
1. A positive feedback system tends to strengthen or reinforce a change in one of the
body s controlled conditions.
2. Normal childbirth provides a good example of a positive feedback system. a. When labor begins, the uterus is stretched (stimulus) and stretch-sensitive
nerve cells in the cervix of the uterus (receptors) send impulses (input) to the hypothalamus (control center). The hypothalamus causes the release of oxytocin (output) which stimulates the uterus (effector) to contract more forcefully (response). Movement of the baby s head down the birth canal causes further stretching, the release of more oxytocin, and even more forceful contractions. The cycle is broken with the birth of the baby.
b. The positive feedback system reinforces a change in a controlled condition. F. Homeostatic Imbalances 1. Disruption of homeostasis can lead to disease and death. 2. Disorder is a general term for any derangement of abnormality of function. 3. Disease is a more specific term for an illness characterized by a recognizable set of signs
and symptoms.
a. A local disease is one that affects one part or a limited region of the body. b. A systemic disease affects either the entire body or several parts. c. Symptoms are subjective changes in body functions that are not apparent to an
observer; e.g., headache or nausea.
d. Signs are objective changes that a clinician can observe and measure; e.g., fever
or rash.
4. Diagnosis is the art of distinguishing one disease from another or determining the nature
of a disease; a diagnosis is generally arrived at after the taking of a medical history and the administration of a physical examination (Clinical Application).
G. Aging and Homeostasis
1. Aging is characterized by a progressive decline in the body s responses to restore
homeostasis
2. These changes such as crinkled skin, gray hair and loss of bone mass are apparent in all
body systems.
V. BASIC ANATOMICAL TERMINOLOGY
A. Body Positions 1. Anatomical Position a. The anatomical position is a standardized method of observing or imaging the
body that allows precise and consistent anatomical references.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
b. When in the anatomical position, the subject stands erect facing the observer,
the upper extremities are placed at the sides, the palms of the hands are turned forward, and the feet are flat on the floor.
2. Reclining Position a. If the body is lying face down, it is in the prone position. b. If the body is lying face up, it is in the supine position.
B. Regional Names
1. Regional names are names given to specific regions of the body for reference. 2. Examples of regional names include cranial (skull), thoracic (chest), brachial (arm),
patellar (knee), cephalic (head), and gluteal (buttock). C. Directional Terms
1. Directional terms are used to precisely locate one part of the body relative to another
and to reduce length of explanations.
2. Commonly used directional terms, such as dorsal, superior, medial, and distal.
D. Planes and Sections
1. Planes are imaginary flat surfaces that are used to divide the body or organs into definite
areas. Principal planes include: midsagittal (medial) and parasagittal, frontal (coronal), transverse (cross-sectional or horizontal) and oblique.
2. Sections are flat surfaces resulting from cuts through body structures. They are named
according to the plane on which the cut is made and include transverse, frontal, and midsagittal sections. E. Body Cavities
1. Body cavities are spaces within the body that help protect, separate, and support
internal organs.
2. Dorsal Body Cavity a. The dorsal body cavity is located near the dorsal surface of the body and has
two subdivisions, the cranial cavity and the vertebral canal.
1) The cranial cavity is formed by the cranial bones and contains the
brain.
2) The vertebral (spinal) canal is formed by the bones of the vertebral
column and contains the spinal cord.
b. Three layers of protective tissue, called meninges, line the dorsal body cavity. 3. Ventral Body Cavity b. The ventral body cavity is subdivided by the diaphragm into an upper thoracic
cavity and a lower abdominopelvic cavity.
c. The thoracic cavity contains two pleural cavities, and the mediastinum, which
includes the pericardial cavity.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
1) The pleural cavities enclose the lungs, while the pericardial cavity
surrounds the heart.
2) The mediastinum is a broad, median partition between the lungs that
extends from the sternum to the vertebral column, it contains all contents of the thoracic cavity except the lungs.
c. The abdominopelvic cavity is divided into a superior abdominal and an inferior
pelvic cavity. 1) Viscera of the abdominal cavity include the stomach, spleen, pancreas, liver, gallbladder, small intestine, and most of the large intestine.
2) Viscera of the pelvic cavity include the urinary bladder, portions of the
large intestine and internal female and male reproductive structures.
4. Thoracic and Abdominal Cavity Membranes a. A thin, slippery serous membrane covers the viscera within the thoracic and
abdominal cavities and also lines the walls of the thorax and abdomen.
b. Parts of the serous membrane are the parietal layer which lines the walls of the
cavities and the visceral layer which covers and adheres to the viscera within the cavities.
c. Serous fluid between the two layers reduces friction and allows the viscera to
slide somewhat during movements.
d. The serous membranes include the pleura, pericardium and peritoneum. 1) The pleural membrane surrounds the lungs, with the visceral pleura
clinging to the surface of the lungs and the parietal pleura lining the chest wall.
2) The serous membrane of the pericardial cavity is the pericardium, with
visceral pericardium covering the surface of the heart and the parietal pericardium lining the chest wall.
3) The peritoneum is the serous membrane of the abdominal cavity, with
the visceral peritoneum covering the abdominal viscera and the parietal peritoneum lining the abdominal wall.
5. Abdominopelvic Regions and Quadrants a. To describe the location of organs easily, the abdominopelvic cavity may be
divided into nine regions by drawing four imaginary lines.
b. To locate the site of an abdominopelvic abnormality in clinical studies, the
abdominopelvic cavity may be divided into quadrants by passing imaginary horizontal and vertical lines through the umbilicus.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
6. Clinical Application: Autopsy a. An autopsy is a postmortem examination of the body and dissection of its
internal organs to confirm or determine the cause of death.
b. An autopsy supplies much information relating to the deceased individual.
VII. MEDICAL IMAGING A very specialized branch of anatomy and physiology that is essential for the diagnosis of many disorders is medical imaging, one division of which is radiography, which includes the use of x-rays.
B. Medical imaging techniques allow physicians to peer inside the body to provide clues to
abnormal anatomy and deviations from normal physiology in order to help diagnose disease.
Critical Thinking Questions
1. A 67-year old man is found dead after being involved in an unwitnessed automobile accident. His family
reports that he had a history of heart disease and diabetes mellitus. An autopsy is ordered to determine the cause of death. Describe the procedures used in an autopsy and what the pathologist would examine in this specific case to make a determination.
2. A 37-year old woman is admitted to the hospital after complaining of chest pains. She admits to having
had severe headaches for several days prior to seeking medical help. She is also taking medications for high blood pressure and is four months pregnant. Which medical imaging procedures would be the best choice of a physician attempting to determine her condition? (Assume all equipment is available and there are unlimited funds to cover costs incurred.)
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
2. THE INTEGUMENTARY SYSTEM
I. INTRODUCTION A. The skin and its accessory structures make up the integumentary system. B. The integumentary system functions to guard the body s physical and biochemical integrity, maintain a constant body temperature, and provide sensory information about the surrounding environment. II. STRUCTURE OF THE SKIN A. The skin consists of different tissues that are joined together to perform specific functions and is the largest organ of the body. 1. Dermatology is the medical specialty that deals with diagnosing and treating skin disorders. a. b. Structurally the skin consists of two parts The superficial portion of the skin is the epidermis and is composed of epitehlial tissue. c. The deeper layer of the skin is the dermis and is primarily composed of connective tissue. d. Deep to the dermis is the subcutaneous layer or hypodermis. 1) It is not a part of the skin. 2) It consists of areolar and adipose tissue. 3) It serves as a fat storage area, an area for blood vessel passage, and an area of pressure nerve endings. B. Epidermis 1. The epidermis is composed of stratified squamous epithelium and contains four principal types of cells: keratinocytes, melanocytes, Langerhans cells, and Merkel cells a. Keratinocytes produce the protein keratin, which helps protect the skin and underlying tissue from heat, microbes, and chemicals, and lamellar granules, which release a waterproof sealant b. Melanocytes produce the pigment melanin which contributes to skin color and absorbs damaging ultraviolet (UV) light c. d. Langerhans cells participate in immune responses Merkel cells contact a sensory structure called a tactile (Merkel) disc and function in the sensation of touch 2. There are four or five layers of the epidermis, depending upon the degree of friction and mechanical pressure applied to the skin. From deepest to most superficial the layers of the epidermis are stratum basale (stratum germinativum), stratum spinosum, stratum granulosum, stratum lucidum (only in palms and soles), and stratum corneum
a. The stratum basale is the deepest layer of the epidermis and contains some
stem cells capable of undergoing cell division to form new cells.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
1) Keratinocytes with a cytoskeleton of tonofilaments are found in this layer. 2) This layer is sometimes called the stratum germinativum to indicate its role in the formation of new cells. 3) When the germinal portion of the epidermis is destroyed, new skin cannot regenerate with a skin graft. b. c. The stratum spinosum provides strength and flexibility to the skin. The stratum granulosum marks the transition between the deeper, metabolically active strata and the dead cells of the more superficial strata. This layer also shows the formation of a water repellent sealant between the cells. 1) This layer consists of keratinocytes that are undergoing apoptosis. 2) This layer is characterized by the presence of keratohyalin which converts tonofilaments into keratin. d. e. The stratum lucidum is present only in the fingers, palms, and soles. The stratum corneum is the most superficial layer and consists of dead cells. 1) Lamellar granules in this layer make it water-repellent. 2) Constant exposure to friction will cause this layer to increase in depth with the formation of a callus, an abnormal thickening of the epidermis. 3. Keratinization and Growth of the Epidermis
a. Keratinization, replacement of cell contents with the protein keratin, occurs as
cells move to the skin surface over 2-4 weeks.
b. Epidermal growth factor and other hormone-like proteins play a role in
epidermal growth. 4. Psoriasis is a chronic skin disorder characterized by a more rapid division and movement of keratinocytes through the epidermal strata (Clinical Application). C. Dermis 1. The dermis is composed of connective tissue containing collagen and elastic fibers and has two regions a. The papillary layer is areolar connective tissue containing fine elastic fibers, dermal papillae, corpuscles of touch (Meissner s corpuscles), and free nerve endings for sensations of heat, cold, pain, tickle, and itch. b. The deeper part of the dermis is the reticular region consisting of dense,
irregular connective tissue containing bundles of collagen fibers and some elastic fibers. 1) Spaces between the fibers may contain adipose cells, hair follicles, sebaceous glands, and sudoriferous glands.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
2) The collagen and elastic fibers provide strength, extensibility (ability to stretch), and elasticity (ability to return to original shape after stretching) to skin. 2. Epidermal ridges increase friction for better grasping ability and provide the basis for fingerprints and footprints. The ridges typically reflect contours of the underlying dermis.
3. Overexposure to the sun can lead to photodamage of the skin and photosensitivity in
individuals who are taking certain medications. D. The Structural Basis of Skin Color 1. The wide variety of colors in skin is due to three pigments - melanin, carotene, and hemoglobin (in blood in capillaries) - in the dermis. 2. Albinism is the inherited inability of an individual to produce melanin. Vitiligo is the complete or partial loss of melanocytes from patches of the skin resulting in irregular white spots. 3. The color of skin and mucous membranes can provide clues for diagnosing certain problems, such as cyanosis, jaundice, and erythema (Clinical Application). E. Types of skin 1. Thin skin covers all parts of the body except for the palms, palmar surfaces of the digits, and soles. a. b. 2. Thin skin lacks epidermal ridges. It has a sparser distribution of sensory receptors than thick skin.
Thick skin covers the palms, palmer surfaces of the digitis, and soles. a. b. It features a stratum lucidum and thick epidermal ridges. It lacks hair follicles, arrector pili muscles, and sebaceous glands, and has more sweat glands than thin skin.
III. ACCESSORY STRUCTURES OF THE SKIN A. Accessory structures of the skin develop from the embryonic epidermis and include hair, glands, and nails. B. Hairs, or pili, are present on most skin surfaces except the palms, palmar surfaces of the digits, soles, and plantar surfaces of the digits. 1. Anatomy of Hair a. Hair consists of a shaft above the surface a root that penetrates the dermis and subcutaneous layer, the cuticle, and a hair follicle b. c. New hairs develop from cell division of the matrix in the bulb. Associated with hairs are sebaceous (oil) glands, arrectores pilorum muscles, and root plexuses 2. Hair removal
a. Depilatories dissolve the protein in the hair shaft
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
b. Electrolysis uses an electric current to destroy the hair matrix.
3. Hair Growth
a. The hair growth cycle consists of a growing stage and a resting stage. b. Both rate of growth and the replacement cycle can be altered by illness, diet,
high fever, surgery, blood loss, severe emotional stress, and gender. 4. Types of hair
a. Lanugo is a fine, nonpigmented hair that covers the fetus. b. Vellus hair is a short, fine hair that replaces lanugo c. Course pigmented hair appears in response to androgens d. Hair that appears in response to androgens and hair of the head, eyelashes and
eyebrows is known as terminal hair. 5. Hair Color
a. Hair color is due primarily to the amount and type of melanin. b. Graying of hair occurs because of a progressive decline in tyrosinase.
6. 7. C. Functions of hair include protection, decrease in heat loss, and sensing light tough. Hormones influence the growth and loss of hair (Clinical applications).
Skin Glands a. Sebaceous (oil) glands are usually connected to hair follicles; they are absent in the palms and soles b. Sebaceous glands produce sebum, which moistens hairs, waterproofs and softens the skin, and inhibits bacterial growth. c. 2. Acne results when sebaceous glands become inflamed (Clinical Application).
Sudoriferous (sweat) glands are divided into apocrine and eccrine types. a. Eccrine sweat glands have an extensive distribution; their ducts terminate at pores at the surface of the epidermis. 1) The main function of eccrine sweat glands is to help regulate body temperature through evaporation. 2) They also help eliminate wastes such as urea. b. Apocrine sweat glands are limited in distribution to the skin of the axilla, pubis, and areolae; their duct open into hair follicles.
3.
Ceruminous glands are modified sudoriferous glands that produce a waxy substance called cerumen. a. b. These glands are found in the external auditory meatus. An abnormal amount of cerumen in the external auditory meatus or canal can result in impaction and prevent sound waves from reaching the ear drum (Clinical Application). c.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
D. Nails 1. Nails are hard, kertainized epidermal cells over the dorsal surfaces of the terminal portions of the fingers and toes. 2. The principal parts of a nail are the body, free edge, root, lunula, eponychium, and matrix 3. 4. Cell division of the matrix cells produces new nails. Functionally, nails help in grasping and manipulating small objects in various ways and provide protection against trauma to the ends of the digits. FUNCTIONS OF SKIN A. Thermoregulation, the homeostatic control of body temperature, is due to the skin liberating sweat at its surface and by adjusting the flow of blood in the dermis. B. C. The skin provides protection through physical, chemical and biological barriers. Cutaneous sensations, including touch, pressure, vibration, tickle, heat, cold, and pain arise in the skin. D. The skin plays minor roles in excretion, the elimination of wastes from the body, and absorption, the passage of material from the external environment into body cells. E. Synthesis of Vitamin D requires activation of a precursor molecule in the skin by UV light, with enzymes in the liver and kidneys modifying the activated molecule to produce calcitriol, the most active form of vitamin D. F. Transdermal drug administration is a method of drug passage across the epidermis and into the blood vessels of the dermis (Clinical Application). V. MAINTAINING HOMEOSTASIS: SKIN WOUND HEALING A. Epidermal Wound Healing 1. In an epidermal wound (e.g., an abrasion or a first-degree or second-degree burn), the central portion of the wound usually extends deep down to the dermis, whereas the wound edges usually involve only superficial damage to the epidermal cells. 2. Epidermal wounds are repaired by enlargement and migration of basal cells, contact inhibition, and division of migrating and stationary basal cells. 3. Epidermal growth factor stimulates basal cells to divide and replace the ones that have moved into the wound. B. Deep Wound Healing 1. When an injury extends to tissues deep to the epidermis, the repair process is more complex than epidermal healing, and scar formation results. 2. Phases of Deep Wound Healing a. During the inflammatory phase, a blood clot unites the wound edges, epithelial cells migrate across the wound, vasodilatation and increased permeability of blood vessels deliver phagocytes, and fibroblasts form.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
b.
During the migratory phase, epithelial cells beneath the scab bridge the wound, fibroblasts begin scar tissue, and damaged blood vessels begin to grow. During this phase, tissue filling the wound is called granulation tissue.
c. d.
During the proliferative phase, the events of the migratory phase intensify. During the maturation phase, the scab sloughs off, the epidermis is restored to normal thickness, collagen fibers become more organized, fibroblasts begin to disappear, and blood vessels are restored to normal.
3. VI.
Scar tissue formation (fibrosis) can occur in deep wound healing.
DEVELOPMENT OF THE INTEGUMENTARY SYSTEM A. The epidermis is derived from ectoderm. Hair, nails, and skin glands are epidermal derivatives. B. C. The dermis is derived from wandering mesenchymal cells. The connective tissue and blood vessels associated with the gland develop from mesoderm.
VII. AGING AND THE INTEGUMENTARY SYSTEM A. Vernix caseosa, a fatty secretion from sebaceous glands, covers and protects the skin of the fetus, beginning at about the sixth month of fetal development, and aids in the birth of the fetus. B. C. With puberty, some adolescents develop acne. Most effects of aging of the skin do not occur until an individual reaches the late forties.
D. Among the effects of aging on the integument are wrinkling, slower growth of hair and nails, dryness and cracking due to sebaceous gland atrophy, decrease in number of melanocytes (gray hair, blotching) and Langerhans cells (decreased immune responsiveness), and loss of subcutaneous fat (thinner skin). E. VIII. Chronic ultraviolet exposure causes photodamage of the skin (Clinical Application).
DISORDERS: HOMEOSTATIC IMBALANCES A. Skin cancer can be caused by excessive exposure to sunlight. 1. The three most common forms are basal cell carcinoma, squamous cell carcinoma, and malignant melanoma. 2. Among the risk factors for skin cancer are skin type, sun exposure, family history, age, and immunologic status. B. Burns 1. Tissue damage from excessive heat, electricity, radioactivity, or corrosive chemicals that destroys (denatures) proteins in the exposed cells is called a burn. 2. Generally, the systemic effects of a burn are a greater threat to life than are the local effects. 3. Depending on the depth of damage, skin burns are classified as first-degree and seconddegree (partial-thickness) and third-degree (full-thickness). 4. The seriousness of a burn is determined by its depth, extent, and area involved, as well as the person s age and general health. When the burn area exceeds 70%, over half of the victims die.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
5.
Two methods for determining the extent of a burn are the rule of nines and the LundBowder method.
C.
Pressure sores, also known as decubitus ulcers, are caused by a constant deficiency of blood to tissues overlying a bony projection that has been subjected to prolonged pressure against an object such as a bed, cast, or splint; the deficiency results in tissue ulceration.
Critical Thinking Questions 1. A victim of a fire is admitted to the emergency room. You observe considerable damage to the epidermis and dermis of both arms and the front and back portions of the trunk. You also note patches of charred skin and insensitivity to touch. What type of burn is indicated by these characteristics? Using the LundBrowder method as a guide, estimate how much of the person s body is burned. What is the probability of scarring? Explain your answer. 2. Explain why a person who lived in a dark cave might have weaker bones and teeth than someone who lived outdoors, even if their diets were the same. (Hint: Calcium and phosphorus are important to bone and tooth structures.) 3. A 70 year old man was diagnosed by his dermatologist with the three forms of skin cancer. Describe the types of skin cancer the patient has, the possible treatment for each type, and the prognosis.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
3. THE SKELETAL SYSTEM: BONE TISSUE
I. INTRODUCTION A. Bone is made up of several different tissues working together: bone, cartilage, dense connective tissue, epithelium, various blood forming tissues, adipose tissue, and nervous tissue. B. Each individual bone is an organ; the bones, along with their cartilages, make up the skeletal system. II. FUNCTIONS OF THE SKELETAL SYSTEM A. Bones support the soft tissues and provide attachment sites for muscles, thereby serving as the structural framework for the body. B. C. Many of the body s internal organs are protected by bony coverings. Bones assist skeletal muscles to produce movement.
D. Bones store and release several minerals, especially calcium and phosphorus, to help maintain mineral homeostasis. E. F. Hemopoiesis, blood cell formation, occurs in the red marrow of bones. Yellow marrow of adult bones serves as a site of triglyceride storage.
III. STRUCTURE OF BONE A. The structure of bone can be analyzed by studying a long bone (Figure 6.1). B. A typical long bone consists of numerous parts. 1. 2. 3. The diaphysis is the shaft of the long bone. The epiphyses are the ends of the bone The metaphyses are the areas between the epiphysis and diaphysis and include the epiphyseal plate in growing bones. 4. Hyaline cartilage (articular cartilage) at the ends of the bones reduces friction and absorbs shock at freely moveable joints. 5. The periosteum is a connective tissue covering of the surface of the bone which contains osteogenic cells, protects bone, assists in fracture repair, helps nourish bone tissue, and serves as an attachment point for ligaments and tendons. 6. 7. The space within the diaphysis is the marrow cavity. The endosteum is the lining of the medullary cavity.
IV. HISTOLOGY OF BONE TISSUE A. Bone (osseous) tissue consists of widely separated cells surrounded by large amounts of matrix. B. There are four principal types of bone cells. 1. 2. 3. 4. C. Osteogenic cells undergo cell division and develop into osteoblasts. Osteoblasts are bone-building cells. Osteocytes are mature bone cells and the principal cells of bone tissue. Osteoclasts are derived from monocytes and serve to break down bone tissue.
The matrix of bone contains inorganic salts, primarily hydroxyapatite and some calcium carbonate, and collagen fibers.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
1.
These and a few other salts are deposited in a framework of collagen fibers, a process called calcification or mineralization.
2.
Mineral salts confer hardness on bone while collagen fibers give bone its great tensile strength.
3.
The process of calcification occurs only in the presence of collagen fibers.
D. Depending on the size and distribution of the spaces between the hard components of bone, the regions of a bone may be categorized as compact or spongy 1. Compact Bone a. b. Compact bone is arranged in units called osteons or Haversian systems. Osteons contain blood vessels, lymphatic vessels, nerves, and osteocytes along with the calcified matrix. c. Osteons are aligned in the same direction along lines of stress. These lines can change as the stresses on the bone changes. 2. Spongy Bone a. Spongy (cancellous) bone does not contain osteons. It consists of trabeculae surrounding many red marrow filled spaces. b. It forms most of the structure of short, flat, and irregular bones, and the epiphyses of long bones. c. 3. Spongy bone tissue is light and supports and protects the red bone marrow.
A bone scan is a diagnostic procedure that can detect certain bone abnormalities or disorders (Clinical Application).
V. BLOOD AND NERVE SUPPLY OF BONE A. Bone is richly supplied with blood. B. The arterial supply to bone involves several vessels. 1. The periosteal arteries pass through Volkmans canals to a multitude of vessels that supply the outer compact bone region. 2. The nutrient artery passes through the nutrient canal and sends branches into the central Haversian canals to provide for osteocytes. 3. The artery continues into the medullae to supply blood for the marrow and osteocells via the epiphyseal artery. C. Veins that carry blood away from long bones are evident in three places. 1. 2. One or two nutrient veins follow the nutrient artery in the diaphysis. Epiphyseal and metaphyseal veins accompany epiphyseal and metaphyseal arteries in the epiphysis. 3. Periosteal veins exit with their periosteal arteries in the periosteum.
D. Nerves follow vessels into bone tissue and the periosteum where they sense damage and transmit pain messages.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
VI. BONE FORMATION
A. Bone formation is termed osteogenesis or ossification and begins when mesenchymal cells
provide the template for subsequent ossification. Two types of ossification occur. 1. Intramembranous ossification is the formation of bone directly from or within fibrous connective tissue membranes. 2. B. Endochondrial ossification is the formation of bone from hyaline cartilage models.
Intramembranous ossification forms the flat bones of the skull and the mandible. 1. An ossification forms from mesenchymal cells as they convert to osteoblasts and lay down osteoid matrix. 2. 3. The matrix surrounds the cell and then calcifies as the osteoblast becomes an osteocyte. The calcifying matrix centers join to form bridges of trabeculae that constitute spongy bone with red marrow between. 4. The periosteum first forms a collar of spongy bone that is then replaced by compact bone.
C.
Endochondrial ossification involves replacement of cartilage by bone and forms most of the bones of the body. 1. 2. 3. 4. 5. The first step in endochondrial ossification is the development of the cartilage model. Step two is the growth of the cartilage model. In step three, the primary ossification center develops in the diaphysis. Step four involves the development of secondary ossification centers in the epiphysis. The final process is the formation of articular cartilage and the epiphyseal plate.
VII. BONE GROWTH A. Growth in Length 1. To understand how a bone grows in length, one needs to know details of the epiphyseal or growth plate. 2. The epiphyseal plate consists of four zones: the zone of resting cartilage, zone of proliferation cartilage, zone of hypertrophic cartilage, and zone of calcified cartilage. 3. The activity of the epiphyseal plate is the only means by which the diaphysis can increase in length. 4. When the epiphyseal plate closes, is replaced by bone, the epiphyseal line appears and indicates the bone has completed its growth in length. B. Growth in Thickness 1. 2. Bone can grow in thickness or diameter only by appositional growth. Bone grows in diameter as a result of interstitial and appositional addition of new bone tissue by osteoblasts around the outer surface of the bone and to a lesser extent internal bone dissolution by osteoclasts in the bone cavity. C. Factors Affecting Bone Growth
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
1.
Adequate dietary intake of minerals and vitamins is necessary for growth and maintenance of bone. a. Calcium and phosphorus are needed for bone growth in large concentrations, with other minerals needed in smaller amounts. b. Vitamins C, K, B12, and A are needed for bone growth.
2.
The most important hormones for stimulation of bone growth during childhood are the insulinlike growth factors (IGFs), which are stimulated by human growth hormone (hGH).
3. 4.
Thyroid hormones and insulin are also necessary hormones for bone growth. At puberty the sex hormones, estrogen and testosterone, stimulate sudden growth and modifications of the skeleton to create the male and female forms.
5.
Hormonal abnormalities can affect growth in height (Clinical Application).
VII. BONES AND HOMEOSTASIS A. Bone Remodeling 1. 2. Remodeling is the ongoing replacement of old bone tissue by new bone tissue. Old bone is constantly destroyed by osteoclasts, whereas new bone is constructed by osteoblasts. B. Fracture and Repair of Bone 1. 2. A fracture is any break in a bone. Common fractures include open (compound) fracture, closed (simple) fracture, comminuted fracture, greenstick fracture, impacted fracture, Pott s fracture, and Colles s fracture. 3. A stress fracture is a series of microscopic fissures in bone that forms without any evidence of injury to other tissues. 4. Fracture repair involves formation of a clot called a fracture hematoma, organization of the fracture hematoma into granulation tissue called a procallus (subsequently transformed into a fibrocartilaginous [soft] callus), conversion of the fibrocartilaginous callus into the spongy bone of a bony (hard) callus, and, finally, remodeling of the callus to nearly original form. 5. Treatments for fractures include the anatomic realignment of the bone fragments, immobilization to maintain realignment, and restoration of function (Clinical Application). C. Bone s Role in Calcium Homeostasis 1. Bone is the major reservoir for calcium ions (Ca ) in the body; the blood level calcium ions (Ca ) are very closely regulated due to calcium s importance in cardiac, nerve, enzyme, and blood physiology. 2. An important hormone regulating Ca2+ exchange between bone and blood is parathyroid hormone (PTH), secreted by the parathyroid gland. It increases blood calcium ion levels.
2+ 2+
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
3.
Another hormone that contributes to the homeostasis of blood Ca is calcitonin (CT). It is secreted by the thyroid gland and decreases blood Ca levels.
2+
2+
IX. EXERCISE AND BONE TISSUE A. Within limits, bone has the ability to alter its strength in response to mechanical stress by increasing deposition of mineral salts and production of collagen fibers. B. Removal of mechanical stress weakens bone through demineralization (loss of bone minerals) and collagen reduction. C. Weight-bearing activities, such as walking or moderate weightlifting, help build and retain bone mass. X. DEVELOPMENTAL ANATOMY OF THE SKELETAL SYSTEM A. Bone forms from mesoderm by intramembranous or endochondrial ossification. B. Around the fifth week of embryonic life, extremities develop from limb buds, which consist of mesoderm and ectoderm. C. By the sixth week, a constriction around the middle portion of the limb buds produces hand plates and foot plates, which will become hands and feet. D. By the seventh week, the arm, forearm and hand are evident in the upper linb bud and the thigh, leg, and foot appear in the lower limb bud. E. F. By the eighth week the limb buds have developed into limbs. The notochord is a flexible rod of tissue that lies in a position where the future vertebral column will develop.
XI. AGING AND BONE TISSUE A. Of two principal effects of aging on bone, the first is the loss of calcium and other minerals from bone matrix (demineralization), which may result in osteoporosis. B. The second principal effect of aging on the skeletal system is a decreased rate of protein synthesis, resulting in decreased production of matrix components (mostly collagen) and making bones more susceptible to fracture. XII. DISORDERS: HOMEOSTATIC IMBALANCES A. Osteoporosis is a decrease in the amount and strength of bone tissue owing to decreases in hormone output. In osteoporosis, bone resorption outpaces bone formation. B. Rickets and osteomalacia are disorders in which bones fail to calcify.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
Critical Thinking Questions 1. A 17-year-old male is admitted to the emergency room with a possible fracture of the tibia. Roentgenograms (x-rays of his leg are taken), and he explains to you that the accident occurred while he was playing basketball. He also tells you that he expects to play basketball when he enters college in the fall and asks you if you think he will grow any more. Examining the roetgenograms, you observe that the epiphyseal cartilage of his shin bone appears undamaged by the injury. Based on this observation, how would you answer his question about his future growth? 2. A 55-year-old woman is told by her physician that she has osteoporosis. He explains to her that her condition is related to change of life. What are three ways by which she might have prevented or forestalled this situation and what might the physician suggest to improve the present condition? 3. The ski patrol were called to two skiing accidents. The first accident involved a 16 year old male who sustained a fracture to his tibia and fibula. The second accident involved a 35 year old female who damaged the articular cartilage in her knee. Which of the two accident victims will heal faster? Be able to explain why.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
4. THE SKELETAL SYSTEM: THE AXIAL SKELETON
I. INTRODUCTION
A. Familiarity with the names, shapes, and positions of individual bones helps to locate other organs and to understand how muscles produce different movements due to attachment on individual bones and the use of leverage with joints. B. The bones, muscles, and joints together form the musculoskeletal system.
II. DIVISIONS OF THE SKELETAL SYSTEM A. The axial skeleton consists of bones arranged along the longitudinal axis of the body. The parts of
the axial skeleton, composed of 80 bones, are the skull, hyoid bone, vertebral column, sternum, and ribs.
B. The appendicular skeleton comprises one of the two major divisions of the skeletal system. 1. It consists of 126 bones in the upper and lower extremities (limbs or appendages) and
the pectoral (shoulder) and pelvic (hip) girdles, which attach them to the rest of the skeleton. III. TYPES OF BONES A. Almost all of the bones of the body can be classified on the basis of shape: long, short, flat, irregular, and sesamoid. B. Sutural bones are classified on the basis of location.
IV. BONE SURFACE MARKINGS A. Bones show characteristic surface markings which are structural features adapted for specific
functions.
B. There are two major types of surface markings. 1. Depressions and openings participate in joints or allow the passage of soft tissue. 2. Processes are projections or outgrowths that either help form joints or serve as
attachment points for connective tissue.
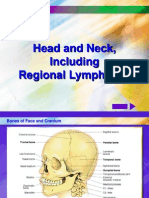
V. SKULL A. The skull, composed of 22 bones, consists of the cranial bones (cranium) and the facial bones
(face) (Figures.
B. General Features 1. The skull forms the large cranial cavity and smaller cavities, including the nasal cavity
and orbits (eye sockets).
2. Certain skull bones contain mucous membrane lined cavities called paranasal sinuses. 3. The only moveable bone of the skull, other than the ear ossicles within the temporal
bones, is the mandible.
4. Immovable joints called sutures hold the skull bones together. 5. The cranial bones have many functions.
a. They protect the brain.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
b. Their inner surfaces attach to membranes that stabilize the positions of the
brain, blood vessels, and nerves.
c. The outer surfaces of cranial bones provide large areas of attachment for
muscles that move the various parts of the head.
d. Facial bones form the framework of the face and protect and provide support
for the nerves and blood vessels in that area.
e. Cranial and facial bones together protect and support the special sense organs. C. Cranial Bones 1. Frontal Bones a. The frontal bones form the forehead, the roofs of the orbits, and most of the
anterior part of the cranial floor.
b. A black eye results from accumulation of fluid and blood in the upper eyelid
following a blow to the relatively sharp supraorbital margin (brow line). (Clinical Application)
2. Parietal bones form the greater portion of the sides and roof of the cranial cavity. 3. Temporal bones form the inferior lateral aspects of the cranium and part of the cranial
floor.
4. The occipital bone forms the posterior part and most of the base of the cranium. 5. The sphenoid bone is called the keystone of the cranial floor because it articulates with
all the other cranial bones, holding them together.
6. The ethmoid bone forms part of the anterior portion of the cranial floor, the medial wall
of the orbits, the superior portion of the nasal septum, and most of the superior side walls of the nasal cavity. It is a major superior supporting structure of the nasal cavity.
D. Facial Bones 1. Nasal bones form part of the bridge of the nose. 2. The maxillae unite to form the upper jawbone and articulate directly with every bone of
the face except for the mandible.
a. They form part of the floors of the orbits, part of the lateral walls and floor of
the nasal cavity, and most of the hard palate.
b. Cleft palate and cleft lip result from a lack of fusion of portions of the palatine
and maxillary bones during fetal development. (Clinical Application)
3. The zygomatic bones (cheekbones) form the prominences of the cheeks and part of the
lateral wall and floor of each orbit.
4. The lacrimal bones form a part of the medial wall of each orbit and are the smallest
bones of the face
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
5. Palatine bones form the posterior portion of the hard palate, part of the floor and lateral
wall of the nasal cavity, and a small portion of the floors of the orbits
6. The inferior nasal conchae (turbinates) form a part of the inferior lateral wall of the nasal
cavity.
7. The vomer, found on the floor of the nasal cavity, is one of the components of the nasal
septum.
8. The mandible (jawbone) is the largest, strongest facial bone and the only moveable skull
bone (other than the ear ossicles).
a. The mandible articulates with the temporal bone to form the
temporomandibular joint.
b. Temporomandibular joint (TMJ) syndrome is dysfunction to varying degrees of
the temporomandibular joint. Causes appear to be numerous and the treatment is similarly variable. (Clinical Application)
E. Nasal Septum 1. The nasal septum is a vertical partition that divides the nasal cavity into right and left
sides .
2. A deviated nasal septum is a lateral deflection of the septum from the midline, usually
resulting from improper fusion of septal bones and cartilage. (Clinical Application)
F. The orbits (eye sockets) 1. The orbits contain the eyeballs and associated structures and are formed by seven bones
of the skull.
2. Five important foramina are associated with each orbit G. Unique Features of the Skull 1. Sutures a. Sutures are immovable joints found only between skull bones and hold skull
bones together.
b. Sutures include the coronal, sagittal, lamboidal,and squamous sutures, among
others
2. Paranasal Sinuses a. Paranasal sinuses are cavities in bones of the skull that communicate with the
nasal cavity.
b. They are lined by mucous membranes and also serve to lighten the skull and
serve as resonating chambers for speech.
c. Cranial bones containing the sinuses are the frontal, sphenoid, ethmoid, and
maxillae.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
d. Sinusitis occurs when membranes of the paranasal sinuses become inflamed
due to infection or allergy. (Clinical Application)
3. Fontanels a. Fontanels are dense connective tissue membrane-filled spaces between the
cranial bones of fetuses and infants. They remain unossified at birth but close early in a child s life.
b. The major fontanels are the anterior, posterior, anterolaterals, and
posterolaterals .
c. Fontanels have two major functions. 1) They enable the fetal skull to modify its size and shape as it passes
through the birth canal.
2) They permit rapid growth of the brain during infancy.
HYOID BONE
A. The hyuoid bone is a unique component of the axial skeleton because it does not articulate with
any other bones.
B. The hyoid bone consists of a horizontal body and paired projections, the lesser and greater horns.
VERTEBRAL COLUMN 1. 2. The vertebral column, along with the sternum and ribs, makes up the trunk of the skeleton. The 26 bones of the vertebral column are arranged into five regions: cervical, thoracic, lumbar, sacral, and coccygeal. 3. Normal Curves of the Vertebral Column
2. The four normal vertebral curves are the cervical and lumbar (anteriorly convex curves)
and thoracic and sacral (anteriorly concave curves).
3. In the fetus, there is only a single anteriorly concave curve. a. The cervical curve develops as the child begins to hold his head erect. b. The lumbar curve develops as the child begins to walk. c. All curves are fully developed by age 10.
4. Between adjacent vertebrae, from the first cervical (atlas) to the sacrum, are intervertebral discs that form strong joints, permit various movements of the vertebral column, and absorb vertical shock.
E. Parts of a typical vertebra include a body, a vertebral arch, and several processes. F. Regions of the Vertebral Column
1. Cervical Region
a. There are 7 cervical vertebrae. b. The first cervical vertebra is the atlas and supports the skull.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
c. The second cervical vertebra is the axis, which permits side-to-side rotation of
the head.
d. The third to sixth correspond to the structural patterns of the typical cervical
vertebrae.
e. The seventh called the vertebra prominens is somewhat different 2. Thoracic Region a. There are 12 thoracic vertebrae. b. These vertebrae articulate with the ribs. 3. Lumbar Region a. There are 5 lumbar vertebrae. b. They are the largest and strongest vertebrae in the column. 4. Sacrum a. The sacrum is formed by the union of 5 sacral vertebrae and serves as a strong
foundation for the pelvic girdle.
6. Coccyx a. The coccyx is formed by the fusion of 4 coccygeal vertebrae. b. Caudal anesthesia (epidural block), frequently used during labor (in childbirth),
causes numbness in the regions innervated by the sacral and coccygeal nerves (approximately from the waist to the knees). (Clinical Application) VIII. THORAX A. The term thorax refers to the entire chest. 1. The skeletal part of the thorax (a bony cage) consists of the sternum, costal cartilages, ribs, and the bodies of the thoracic vertebrae. 2. The thoracic cage encloses and protects the organs in the thoracic and superior abdominal cavities. It also provides support for the bones of the shoulder girdle and upper limbs. B. Sternum 1. 2. C. Ribs 1. 2. The 12 pairs of ribs give structural support to the sides of the thoracic cavity. The first 7 pairs of ribs are called true ribs; the remaining five pairs, false ribs (with the last two false ribs called floating ribs). 3. Rib fractures are the most common types of chest injuries. (Clinical Application) The sternum is located on the anterior midline of the thoracic wall. It consists of three parts: manubrium, body, and xiphoid process
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
IX.
DISORDERS: HOMEOSTATIC IMBALANCES A. Protrusion of the nucleus pulposus into an adjacent vertebral body is called a herniated (slipped) disc. This movement exerts pressure on spinal nerves, causing considerable pain. B. Spina bifida is a congenital defect caused by failure of the vertebral laminae to unite at the midline. This may involve only one or several vertebrae; nervous tissue may or may not protrude through the skin.
Critical Thinking Questions
1. A six-year-old child is diagnosed with severe scoliosis. Considering what you know about abnormal spinal
curvatures and about the thoracic cavity, what risks would you expect a physician to outline for the parents of this child?
2. As you were driving down the highway, you observed a one car wreck. When you stopped to render aid,
the driver of the car complained of chest pain in the area of the ribs and pain upon breathing after impacting the steering wheel of his car. What might be the cause of the pain and the possible consequences?
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
THE SKELETAL SYSTEM: THE APPENDICULAR SKELETON
I.
INTRODUCTION
A. The appendicular skeleton includes the bones of the upper and lower extremities and the
shoulder and hip girdles.
B. The appendicular skeleton functions primarily to facilitate movement. II. PECTORAL (SHOULDER) GIRDLE A. The pectoral or shoulder girdle attaches the bones of the upper limbs to the axial skeleton. B. Clavicle 1. The clavicle or collar bone lies horizontally in the superior and anterior part of thorax
superior to the first rib and articulates with the sternum and the clavicle.
2. The clavicle, one of the most frequently broken bones in the body, transmits mechanical
force from the upper limb to the trunk. (Clinical Application)
C. Scapula 1. The scapula or shoulder blade articulates with the clavicle and the humerus. 2. The scapulae articulate with other bones anteriorly, but are held in place posteriorly
only by complex shoulder and back musculature. III. UPPER LIMB (EXTREMITY)
A. Each upper limb consists of 30 bones including the humerus, ulna, radius, carpals, metacarpals,
and phalanges.
B. Humerus 1. The humerus is the longest and largest bone of the upper limb. 2. It articulates proximally with the scapula and distally at the elbow with both the radius
and ulna.
C. Ulna and Radius 1. The ulna is located on the medial aspect of the forearm. 2. The radius is located on the lateral aspect (thumb side) of the forearm 3. The radius and ulna articulate with the humerus at the elbow joint, with each other, and
with three carpal bones.
D. Carpals, Metacarpal, and Phalanges 1. The eight carpal bones, bound together by ligaments, comprise the wrist. 2. Five metacarpal bones are contained in the palm of each hand 3. Each hand contains 14 phalanges, three in each finger and two in each thumb.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
IV. PELVIC (HIP) GIRDLE A. The pelvic (hip) girdle consists of two hipbones (coxal bones) and provides a strong and stable support for the lower extremities, on which the weight of the body is carried.
1. Each hipbone (coxal bone) is composed of three separate bones at birth: the ilium, pubis,
and ischium.
2. These bones eventually fuse at a depression called the acetabulum, which forms the
socket for the hip joint. B. The ilium is the larger of the three components of the hip bone and articulates (fuses) with the ischium and pubis. C. The ischium is the inferior, posterior portion of the hip bone.
D. The pubis is the anterior and inferior part of the hip bone. E. True and False Pelves
1. Together with the sacrum and coccyx, the two hipbones (coxal bones) form the pelvis. 2. The greater (false) and lesser (true) pelvis are anatomical subdivisions of this basin-like
structure. V. COMPARISON OF FEMALE AND MALE PELVES
A. Male bones are generally larger and heavier than those of the female; the male s joint surfaces
also tend to be larger.
B. Muscle attachment points are more well-defined in the bones of a male than of a female due to
the larger size of the muscles in males.
C. A number of anatomical differences exist between the pelvic girdles of females and those of
males, primarily related to the need for a larger pelvic outlet in females to facilitate childbirth. VI. COMPARISON OF PECTORAL AND PELVIC GIRDLES
A. The pectoral girdle does not directly articulate with the vertebral column; the pelvic girdle does. B. The pectoral girdle sockets are shallow and maximize movement; those of the pelvic girdle are
deeper and allow less movement.
C. The structure of the pectoral girdle offers more movement than strength; the pelvic girdle, more
strength than movement. VII. LOWER LIMB (EXTREMITY)
A. Each lower extremity is composed of 30 bones, including the femur, tibia, fibula, tarsals,
metatarsals, and phalanges.
B. Femur 1. The femur or thighbone is the largest, heaviest, and strongest bone of the body. 2. It articulates with the hip bone and the tibia. C. Patella
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
1. The patella or kneecap is a sesamoid bone located anterior to the knee joint. 2. It functions to increase the leverage of the tendon of the quadriceps femoris muscle, to
maintain the position of the tendon when the knee is bent, and to protect the knee joint.
3. Patellofemoral stress syndrome is a common knee problem in runners. (Clinical
Application)
D. Tibia and Fibula 1. The tibia or shinbone is the larger, medial, weight-bearing bone of the leg. 2. The fibula is parallel and lateral to the tibia. E. Tarsals, Metatarsals, and Phalanges 1. Seven tarsal bones constitute the ankle and share the weight associated with walking. 2. Five metatarsal bones are contained in the foot. 3. The arrangement of phalanges in the toes is the same as that described for the fingers
and thumb above - fourteen bones in each foot.
F. Arches of the Foot 1. The bones of the foot are arranged in two nonrigid arches that enable the foot to
support the weight of the body; provide an ideal distribution of body weight over the hard and soft tissues, and provide leverage while walking.
2. Flatfoot, clawfoot, and clubfoot are caused by decline, elevation, or rotation of the
medial longitudinal arches. (Clinical Application)
VIII. DISORDERS: HOMEOSTATIC IMBALANCE A. The term hip fracture most commonly applies to a break in the bones associated with the hip
joint.
B. Hip fractures often require surgical treatment.
Critical Thinking Questions 1. A 25-year-old obstetrical patient confides that she is quite concerned about the very large size of the baby she is carrying relative to her small frame and possible problems she might have at the time of delivery. Explain the various adaptations of the female skeleton that will help her during delivery. Also explain to her the diagnostic techniques that can be utilized to help rule out a true problem with delivery.
2. You have been a runner all of your life. Yesterday, you ran down a street undergoing construction and
today your right leg and knee hurt. Explain what possible problem might be occurring with your knee joint.
3. Explain why the pectoral girdle is less stable than the pelvic girdle.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
JOINTS I. INTRODUCTION A. A joint (articulation or arthrosis) is a point of contact between two or more bones, between
cartilage and bones, or between teeth and bones.
B. The scientific study of joints is called arthrology.
II. JOINT CLASSIFICATION
A. Structural classification is based on the presence or absence of a synovial (joint) cavity and type
of connecting tissue. Structurally, joints are classified as fibrous, cartilaginous, or synovial.
B. Functional classification of joints is based on the degree of movement permitted. Joints may be
synarthroses (immovable), amphiarthroses (partially movable), or diarthroses (freely movable). III. FIBROUS JOINTS
A. Fibrous joints lack a synovial cavity, have the articulating bones held together by fibrous
connective tissue, and permit little or no movement.
B. Types of fibrous joints include sutures, syndesmoses, and gomphoses. 1. A suture is a fibrous joint composed of a thin layer of dense fibrous connective tissue
that unites skull bones.
a. A synostosis is a suture joint that has ossified. An example of a synostosis is the
frontal suture between the left and right sides of the frontal bone.
b. A synostosis is functionally classified as a synarthrosis. 2. A syndesmosis is a fibrous joint in which there is more fibrous connective tissue than in a
suture.
3. A gomphosis is a fibrous joint in which a cone-shaped peg fits into a socket. An example
is the root of a tooth in its socket. IV. CARTILAGINOUS JOINTS
A. A cartilaginous joint lacks a synovial cavity, has the articulating bones connected by either
fibrocartilage or hyaline cartilage, and allows little or no movement.
B. The two types of cartilaginous joints are synchondroses and symphyses. 1. A synchrondosis is a cartilaginous joint in which the connecting material is hyaline
cartilage.
2. A symphysis is a cartilaginous joint in which the connecting material is a disc of
fibrocartilage. Examples are the interverterbral discs and the pubic symphysis. V. SYNOVIAL JOINTS
A. Synovial joints have a synovial (joint) cavity between the articulating bone and are freely movable
(diarthrotic).
B. Structure of Synovial Joints 1. Articular cartilage
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
a. The articular cartilage covers the bones at synovial joints. b. The articular cartilage reduces friction at the joint with movement and helps
absorb shock
2. Articular Capsule a. The articular capsule surrounds a diarthrosis, encloses the synovial cavity, and
unites the articulating bones.
b. The articular capsule is composed of two layers - the outer fibrous capsule
(which may contain ligaments) and the inner synovial membrane (which secretes a lubricating and joint-nourishing synovial fluid)
c. The flexibility of the fibrous capsule permits considerable movement at a joint,
whereas its great tensile strength helps prevent bones from dislocating.
d. Other capsule features include ligaments and articular fat pads. 3. Synovial fluid, secreted by the synovial membrane, lubricates and reduces friction in the
joint and supplies nutrients to and removes metabolic wastes from the joint.
4. Accessory Ligaments and Articular Discs a. Many diarthroses also contain accessory ligaments and articular discs (menisci) b. Ligaments help hold bone to bone. c. Articular discs modify the shape of the joint surfaces of the articulating bones,
help maintain the stability of the joint, and direct the flow of synovial fluid to areas of greatest friction.
5. Torn cartilage, occurring frequently in the knees of athletes, is damage to the articular
discs that lie between the ends of some bones. Removal, to prevent erosion and arthritis, is usually accomplished by arthroscopy.
C. Nerve and Blood Supply 1. Nerves that supply a joint are the same as those that supply the skeletal muscles that
move the joint.
2. Numerous arteries and veins supply the joints and surrounding structures. D. Sprain and Strain (Clinical Application) 1. A sprain is the forcible wrenching or twisting of a joint that stretches or tears its
ligaments but does not dislocate the bone.
2. A strain is a stretched or partially torn muscle. E. Bursae and Tendon Sheaths 1. Bursae are synovial fluid filled saclike structures that cushion the movement of one body
part over another. They are found where one part of the body moves over another.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
2. Tendon sheaths are tubelike bursae that wrap around tendons where there is
considerable friction, such as the tendon of the biceps brachii at the shoulder joint.
3. Bursitis is a chronic inflammation of a burse. F. Types of Synovial Joints 1. Plantar joints permit mainly side-to-side and back-and-forth gliding movements. These
joints are nonaxial and include the intercarpal, intertarsal, sternoclavicular, acromioclavicular, sternocostal, and vertebrocostal joints.
2. A hinge joint contains the convex surface of one bone fitting into a concave surface of
another bone. Movement is primarily flexion or extension in a single plane. Examples include the elbow, knee, ankle, and interphalangeal joints.
3. In a pivot joint, a round or pointed surface of one bone fits into a ring formed by another
bone and a ligament. Movement is rotational and monaxial. An example is the atlas rotating about the axis.
4. In an condyloid joint, an oval-shaped condyle of one bone fits into an elliptical cavity of
another bone. Movements are flexion-extension, abduction-adduction, and circumduction; an example is the joint between the carpals and the radius.
5. A saddle joint contains one bone whose articular surface is saddle-shaped and another
bone whose articular surface is shaped like a rider sitting in the saddle. Movements are flexion-extension, abduction-adduction, and circumduction.
6. In a ball-and-socket joint, the ball-shaped surface of one bone fits into the cuplike
depression of another. Movements are flexion-extension, abduction-adduction, rotation, and circumduction; the only examples are the shoulder joint and hip joint.
VI. TYPES OF MOVEMENT AT SYNOVIAL JOINTS A. Gliding movements occur when relatively flat bone surfaces move back and forth and from side
to side with respect to one another.
1. In gliding joints there is no significant alteration of the angle between the bones. 2. Gliding movements occur at plantar joints. B. Angular Movements 1. In angular movements there is an increase or a decrease in the angle between
articulating bones.
2. The principal angular movements are flexion, extension and hyperextension. a. Flexion results in a decrease in the angle between articulating bones. b. Extension results in an increase in the angle between articulating bones. c. Lateral flexion involves the movement of the trunk sideways to the right or left
at the waist. The movement occurs in the frontal plane and involves the intervertebral joints.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
d. Hyperextension is a continuation of extension beyond the anatomical position
and is usually prevented by the arrangement of ligaments and the anatomical alignment of bones.
3. Abduction, Adduction, and Circumduction a. Abduction refers to the movement of a bone away from the midline b. Adduction refers to the movement of a bone toward the midline c. Circumduction refers to movement of the distal end of a part of the body in a
circle
1) Circumduction occurs as a result of a continuous sequence of flexion,
abduction, extension, and adduction.
2) Condyloid, saddle, and ball-and-socket joints allow circumduction. C. In rotation, a bone revolves around its own longitudinal axis 1. Pivot and ball-and-socket joints permit rotation. 2. If the anterior surface of a bone of the limb is turned toward the midline, medial
rotation occurs. If the anterior surface of a bone of the limb is turned away from the midline, lateral rotation occurs
D. Special Movements 1. Elevation is an upward movement of a part of the body 2. Depression is a downward movement of a part of the body 3. Protraction is a movement of a part of the body anteriorly in the transverse plane. 4. Retraction is a movement of a protracted part back to the anatomical position. 5. Inversion is movement of the soles medially at the intertarsal joints so that they face
away from each other.
6. Eversion is a movement of the soles laterally at the intertarsal joints so that they face
away from each other.
7. Dorsiflexion refers to bending of the foot at the ankle in the direction of the superior
surface.
8. Plantar flexion involves bending of the foot at the ankle joint in the direction of the
plantar surface.
9. Supination is a movement of the forearm at the proximal and distal radioulnar joints in
which the palm is turned anteriorly or superiorly.
10. Pronation is a movement of the forearm at the proximal and distal radioulnar joints in
which the distal end of the radius crosses over the distal end of the ulna and the palm is turned posteriorly or inferiorly.
11. Opposition is the movement of the thumb at the carpometacarpal joint in which the
thumb moves across the palm to touch the tips of the finger on the same hand.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
E. A dislocation or luxation is a displacement of a bone from a joint. VII.
SELECTED JOINTS OF THE BODY
A. Shoulder Joint 1. This is a ball-and-socket joint formed by the head of the humerus and the glenoid cavity
of the scapula.
2. Movements at the joint include flexion, extension, abduction, adduction, medial and
lateral rotation, and circumduction of the arm.
3. This joint shows extreme freedom of movement at the expense of stability. B. Elbow Joint 1. This is a hinge joint formed by the trochlea of the humerus, the trochlear notch of the
ulna, and the head of the radius.
2. Movements at this joint are flexion and extension of the forearm. C. Hip Joint 1. This ball-and-socket joint is formed by the head of the femur and the acetabulum of the
hipbone.
2. Movements at this joint include flexion, extension, abduction, adduction,
circumduction, and medial and lateral rotation of the thigh.
3. This is an extremely stable joint due to the bones making up the joint and the accessory
ligaments and muscles.
D. Knee Joints 1. This is the largest and most complex joint of the body and consists of three joints within
a single synovial cavity.
2. Movements at this joint include flexion, extension, slight medial rotation, and lateral
rotation of the leg in a flexed position.
VIII. FACTORS AFFECTING CONTACT AND RANGE OF MOTION AT SYNOVIAL JOINTS A. Structure and shape of the articulating bone B. Strength and tautness of the joint ligaments C. Arrangement and tension of the muscles D. Apposition of soft parts E. Hormones F. Disuse IX. AGING AND JOINTS A. Various aging effects on joints include decreased production of synovial fluid, a thinning of the
articular cartilage, and loss of ligament length and flexibility.
B. The effects of aging on joints are due to genetic factors as well as wear and tear on joints.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
X. DISORDERS: HOMEOSTATIC IMBALANCES A. Common injuries to joints include: rotator cuff injuries, separated shoulder, tennis elbow,
dislocation of the radial head and knee injuries.
B. Rheumatism and Arthritis 1. Rheumatism refers to any painful state of the supporting structures of the body - bones,
ligaments, joints, tendons, or muscles.
2. Arthritis is a form of rheumatism in which the joints become inflamed. B. Rheumatoid arthritis is an autoimmune disease in which the body s immune system attacks its
own cartilage and joint linings resulting in loss of joint function (Figure 9.15).
C. Osteoarthritis is a degenerative joint disease commonly known as wear-and-tear arthritis. It is
characterized by deterioration of articular cartilage and bone spur formation. It is noninflammatory and primarily affects weight-bearing joints.
D. Gouty arthritis is a condition in which sodium urate crystals are deposited in soft tissues of joints,
causing inflammation, swelling, and pain. If not treated, bones at affected joints will eventually fuse, rendering the joints immobile.
Critical Thinking Questions
1. A patient is diagnosed as having the following clinical symptoms: swollen joints, pain and tenderness in
the joints, and some joint immobility. What is the probable disorder? Since no bone spurs have formed, what disorder could be ruled out? What condition is suspected if the patient has an excessive buildup of uric acid in the blood?
2. An exercise instructor and an anatomy instructor got together and decided to test their students together.
The test question required the students to describe exercise activities that include each of the different synovial joint movements. What exercises would demonstrate or include each of the synovial joint movements?
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
THE MUSCULAR SYSTEM
I. INTRODUCTION A. The muscular system specifically concerns skeletal muscles and associated connective tissue that
make individual muscle organs.
B. This chapter discusses how skeletal muscles produce movement and describes the principal
skeletal muscles.
II. HOW SKELETAL MUSCLES PRODUCE MOVEMENT A. Muscle Attachment Sites: Origin and Insertion 1. Skeletal muscles produce movements by exerting force on tendons, which in turn pull on
bones or other structures, such as skin.
2. Most muscles cross at least one joint and are attached to the articulating bones that
form the joint.
3. When such a muscle contracts, it draws one articulating bone toward the other. a. The attachment to the stationary bone is the origin. b. The attachment to the movable bone is the insertion. 4. Tenosynovitis is an inflammation of the tendons, tendon sheaths, and synovial
membranes surrounding certain joints (Clinical Application).
B. Lever Systems and Leverage 1. Bones serve as levers and joints serve as fulcrums. 2. The lever is acted on by two different forces: resistance (load) and effort. 3. Levers are categorized into three types first-class (ERF), second-class (FRE), and thirdclass (FER) according to the position of the fulcrum, effort, and resistance on the lever.
4. Leverage, the mechanical advantage gained by a lever, is largely responsible for a
muscle s strength and range of motion (ROM), i.e., the maximum ability to move the bones of a joint through an arc.
C. Effects of Fascicle Arrangement 1. Skeletal muscle fibers (cells) are arranged within the muscle in bundles called fasciculi. 2. The muscle fibers are arranged in a parallel fashion within each bundle, but the
arrangement of the fasciculi with respect to the tendons may take one of four characteristic patterns: parallel, fusiform, pennate, and circular.
3. Fascicular arrangement is correlated with the power of a muscle and the range of
motion.
D. Coordination Within Muscle Groups
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
1. Most movements are coordinated by several skeletal muscles acting in groups rather
than individually, and most skeletal muscles are arranged in opposing (antagonistic) pairs at joints.
2. A muscle that causes a desired action is referred to as the prime mover (agonist); the
antagonist produces an opposite action.
3. Most movements also involve muscles called synergists, which serve to steady a
movement, thus preventing unwanted movements and helping the prime mover function more efficiently.
4. Some synergist muscles in a group also act as fixators, which stabilize the origin of the
prime mover so that it can act more efficiently.
5. Under different conditions and depending on the movement and which point is fixed,
many muscles act, at various times, as prime movers, antagonists, synergists, or fixators.
6. Some of the benefits of stretching (Clinical Application) include: improved physical
performance, decreased risk of injury, reduced muscle soreness, improved posture, increased synovial fluid, and increased neuromuscular co-ordination.
III. HOW SKELETAL MUSCLES ARE NAMED A. The names of most of the nearly 700 skeletal muscles are based on several types of
characteristics.
B. These characteristics may be reflected in the name of the muscle. C. The most important characteristics include the direction in which the muscle fibers run, the size,
shape, action, numbers of origins, and location of the muscle, and the sites of origin and insertion of the muscle.
V. DISORDERS: HOMEOSTATIC IMBALANCES A. Running Injuries 1. Most running injuries involve the knee. Other commonly injured sites are the calcaneal
(Achilles) tendon, medial aspect of the tibia, hip area, groin area, foot and ankle, and back.
2. Running injuries are frequently related to faulty training techniques. 3. Running injuries can be treated initially (first 2-3 days) with rest, ice, compression, and
elevation (RICE therapy). Alternating moist heat and ice massage may be used as a follow-up treatment. Sometimes, nonsteroidal anti-inflammatory drugs (NSAIDS) or local injections of corticosteroids are needed; an alternate fitness program is necessary to keep active during the recovery period followed by careful rehabilitative exercise.
B. Compartment Syndrome 1. Skeletal muscles in the limbs are organized in units called compartments.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
2. In compartment syndrome, some external or internal pressure constricts the structures
within a compartment, resulting in damaged blood vessels and subsequent reduction of the blood supply to the structures within the compartment.
3. Without intervention, nerves suffer damage, and muscle develop scar tissue that results
in permanent shortening of the muscles, a condition called contracture.
Critical Thinking Questions
1. Your next door neighbor has been diagnosed with Bell s palsy. Your neighbor wants you to explain what
Bell s palsy is and what tissues are affected. What will you tell your neighbor?
2. The pitcher of your son s little league baseball team has a rotator cuff injury. What is this injury and what
might cause it?
3. A local athlete pulled his groin during a game. What is a pulled groin and what muscles are affected?
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
THE SPINAL CORD AND SPINAL NERVES
I. INTRODUCTION
A. The spinal cord and spinal nerves mediate reactions to environmental changes. B. The spinal cord has several functions. 1. It processes reflexes. 2. It is the site for integration of EPSPs and IPSPs that arise locally or are triggered by nerve
impulses from the periphery and brain.
3. It is a conduction pathway for sensory and motor nerve impulses.
II. SPINAL CORD ANATOMY
A. The spinal cord is protected by two connective tissue coverings, the meninges and vertebra, and a
cushion of cerebrospinal fluid.
1. The vertebral column provides a bony covering of the spinal cord (Figure 13.1b). 2. Meninges a. The meninges are three coverings that run continuously around the spinal cord
and brain.
1) The outermost layer is the dura mater. 2) The middle layer is the arachnoid. 3) The innermost meninx is the pia mater, a thin, transparent connective
tissue layer that adheres to the surface of the spinal cord and brain.
4) Inflammation of the meninges is known as meningitis. 5) Denticulate ligaments are thickenings of the pia mater that suspend
the spinal cord in the middle of its dural sheath.
B. External Anatomy of the Spinal Cord 1. The spinal cord begins as a continuation of the medulla oblongata and terminates at
about the second lumbar vertebra in an adult.
2. It contains cervical and lumbar enlargements that serve as points of origin for nerves to
the extremities.
3. The tapered portion of the spinal cord is the conus medullaris, from which arise the filum
terminale and cauda equina.
4. Spinal nerves a. The 31 pairs of spinal nerves are named and numbered according to the region
and level of the spinal cord from which they emerge.
b. There are 8 pairs of cervical nerves, 12 pairs of thoracic nerves, 5 pairs of
lumbar nerves, 5 pairs of sacral nerves, and 1 pair of coccygeal nerves.
c. Spinal nerves are the paths of communication between the spinal cord and
most of the body.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
d. Roots are the two points of attachment that connect each spinal nerve to a
segment of the spinal cord.
1) The posterior or dorsal (sensory) root contains sensory nerve fibers and
conducts nerve impulses from the periphery into the spinal cord; the posterior root ganglion contains the cell bodies of the sensory neurons from the periphery.
2) The anterior or ventral (motor) root contains motor neuron axons and
conducts impulses from the spinal cord to the periphery; the cell bodies of motor neurons are located in the gray matter of the cord.
5. Removal of cerebrospinal fluid from the subarachnoid space is called a spinal tap
(lumbar puncture). This procedure is used to diagnose pathologies and to introduce antibiotics, contrast media, anesthetics, and chemotherapeutic drugs. (Clinical Application)
C. Internal Anatomy of the Spinal Cord 1. The anterior median fissure and the posterior median sulcus penetrate the white matter
of the spinal cord and divide it into right and left sides.
2. The gray matter of the spinal cord is shaped like the letter H or a butterfly and is
surround by white matter.
a. The gray matter consists primarily of cell bodies of neurons and neuroglia and
unmyelinated axons and dendrites of association and motor neurons.
b. The white matter consists of bundles of myelinated axons of motor and sensory
neurons.
3. The gray commissure forms the cross bar of the H-shaped gray matter. 4. In the center of the gray commissure is the central canal, which runs the length of the
spinal cord and contains cerebrospinal fluid.
5. Anterior to the gray commissure is the anterior white commissure, which connects the
white matter of the right and left sides of the spinal cord.
6. The gray matter is divided into horns, which contain cell bodies of neurons. 7. The white matter is divided into columns. a. Each column contains distinct bundles of nerve axons that have a common
origin or destination and carry similar information.
b. These bundles are called tracts.
1) Sensory (ascending) tracts conduct nerve impulses toward the brain. 2) Motor (descending) tracts conduct impulses down the cord.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
III. SPINAL CORD PHYSIOLOGY A. The spinal cord has two principal functions. 1. The white matter tracts are highways for nerve impulse conduction to and from the brain. 2. B. The gray matter receives and integrates incoming and outgoing information.
Sensory and Motor Tracts 1. Sensory information from receptors travels up the spinal cord to the brain along two main routes on each side of the cord: the spinothalamic tracts and the posterior column tract. 2. Motor information travels from the brain down the spinal cord to effectors (muscles and glands) along two types of descending tracts: direct pathways and indirect pathways. 3. The axons of various nerves and CNS tracts develop myelin sheaths at different times which explains the poor sensory and motor development of newborns. (Clinical Application)
C.
Reflexes and Reflex Arcs 1. The spinal cord serves as an integrating center for spinal reflexes. This occurs in the gray matter. 2. A reflex is a fast, predictable, automatic response to changes in the environment that helps to maintain homeostasis. 3. Reflexes may be spinal, cranial, somatic, or autonomic.
D. Reflex Arc 1. A reflex arc is the simplest type of pathway; pathways are specific neuronal circuits and thus include at least one synapse. 2. The five functional components of a reflex arc are the receptor, sensory neuron, motor neuron, integrating center neuron, and effector. 3. Reflexes help to maintain homeostasis by permitting the body to make exceedingly rapid adjustments to homeostatic imbalances. 4. Somatic spinal reflexes include the stretch reflex, tendon reflex, flexor (withdrawal) reflex, and crossed extensor reflex; all exhibit reciprocal innervation. a. Stretch Reflex 1) The stretch reflex is ipsilateral and is important in maintaining muscle tone and muscle coordination during exercise. 2) A two-neuron or monosynaptic reflex arc contains one sensory neuron and one motor neuron. A stretch reflex, such as the patellar reflex, is an example. 3) It operates as a feedback mechanism to control muscle length by causing muscle contraction. b. Tendon Reflex
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
1) The tendon reflex is ipsilateral and prevents damage to muscles and tendons as a result of stretching. 2) It operates as a feedback mechanism to control muscle tension by causing muscle relaxation when muscle force becomes too extreme.
c. Flexor and Crossed Extensor Reflexes
1) Flexor or Withdrawal Reflex a) The flexor (withdrawal) reflex is ipsilateral and is a protective withdrawal reflex that moves a limb to avoid pain. b) This reflex results in contraction of flexor muscles to move a limb to avoid injury or pain. c) It works with the crossed extensor reflex to maintain balance. 2) Crossed Extensor Reflex a) This is a balance-maintaining reflex that causes a synchronized extension of the joints of one limb and flexion of the joints in the opposite limb. b) The crossed extensor reflex, which is contralateral, helps to maintain balance during the flexor reflex. 5. Reflexes are often used for diagnosing disorders of the nervous system and locating injured tissue. (Clinical Application) a. If a reflex is absent, or abnormal, the damage may be somewhere along a particular conduction pathway. b. Among the clinically important reflexes are the plantar flexion and Babinski reflexes. IV. SPINAL NERVES A. Spinal nerves connect the CNS to sensory receptors, muscles, and glands and are part of the peripheral nervous system. 1. The 31 pairs of spinal nerves are named and numbered according to the region and level of the spinal cord from which they emerge. 2. Roots of the lower lumbar, sacral, and coccygeal nerves are not in line with their corresponding vertebrae and thus form the cauda equina. 3. Spinal nerves connect to the cord via an anterior and a posterior root. Since the posterior root contains sensory axons and the anterior root contains motor axons, a spinal nerve is a mixed nerve, at least at its origin. B. Connective Tissue Covering of Spinal Nerves 1. Spinal nerve axons are grouped within connective tissue sheathes.
a. A fiber is a single axon within an endoneurium. b. A fascicle is a bundle of fibers within a perineurium.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
c. A nerve is a bundle of fascicles within an epineurium.
2. C. Numerous blood vessels are within the coverings. Distribution of Spinal Nerves 1. Shortly after passing through its intervertebral foramen, a spinal nerve divides into several branches; these branches are known as rami. 2. Branches of a spinal nerve include the dorsal ramus, ventral ramus, meningeal branch, and rami communicantes. 3. The anterior rami of spinal nerves T2-T12 do not enter into the formation of plexuses and are known as intercostal or thoracic nerves. a. b. These nerves directly innervate structures they supply in the intercostal spaces. Their posterior rami supply the deep back muscles and skin of the posterior aspect of the thorax. 4. The ventral rami of spinal nerves, except for T2-T12, form networks of nerves called plexuses. a. Emerging from the plexuses are nerves bearing names that are often descriptive of the general regions they supply or the course they take. b. The cervical plexus supplies the skin and muscles of the head, neck, and upper part of the shoulders; connects with some cranial nerves; and supplies the diaphragm. 1) Damage to the spinal cord above the origin of the phrenic nerves (C3C5) causes respiratory arrest. 2) Breathing stops because the phrenic nerves no longer send impulses to the diaphragm. c. The brachial plexus constitutes the nerve supply for the upper extremities and a number of neck and shoulder muscles. 1) A number of nerve disorders may result from injury to the brachial plexus. 2) Among these injuries are Erb-Duchene palsy or waiter s tip palsy, Klumphe s palsy, wrist drop, carpal tunnel syndrome, claw hand, and winged scapula. d. The lumbar plexus supplies the anterolateral abdominal wall, external genitals, and part of the lower extremities. 1) The largest nerve arising from the lumbar plexus is the femoral nerve. 2) Injury to the femoral nerve is indicated by an inability to extend the leg and by loss of sensation in the skin over the anteromedial aspect of the thigh.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
3) Obturator nerve injury is a common complication of childbirth and results in paralysis of the adductor muscles of the leg and loss of sensation over the medial aspect of the thigh. e. The sacral plexus supplies the buttocks, perineum, and part of the lower extremities. 1) The largest nerve arising from the sacral plexus (and the largest nerve in the body) is the sciatic nerve. 2) Injury to the sciatic nerve (common peroneal portion) and its branches results in sciatica, pain that extends from the buttock down the back of the leg. 3) Sciatic nerve injury can occur due to a herniated (slipped) disc, dislocated hip, osteoarthritis of the lumbosacral spine, pressure from the uterus during pregnancy, or an improperly administered gluteal injection. D. Dermatomes 1. The skin over the entire body is supplies by spinal nerves that carry somatic sensory nerves impulses into the spinal cord. 2. All spinal nerves except C1 innervate specific, constant segments of the skin; the skin segments are called dermatomes. 3. Knowledge of dermatomes helps a physician to determine which segment of the spinal cord or which spinal nerve is malfunctioning. E. An injury that entirely severs the spinal cord is said to cause a complete transection. (Clinical Application) 1. After the injury, there will be a permanent loss of sensations in dermatomes below the injury. 2. Voluntary muscle contractions will also be lost below the transection.
V. DISORDERS; HOMEOSTATIC IMBALANCES A. Shingles is an acute infection of the peripheral nerves by the herpes zoster virus; the virus migrates down peripheral nerves, causing pain, skin discoloration, and a characteristic line of skin blisters. B. Poliomyelitis (infantile paralysis or polio) is a viral infection characterized by fever, headache, stiff neck and back, deep pain and weakness, and loss of certain somatic reflexes. Paralysis is produced when the virus destroys motor neuron cell bodies.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
Critical Thinking Questions 1. After touching a very hot barbecue grill, you immediately withdraw your hand. What kind of reflex arc is involved? Where are the receptors located? What is the function of the receptors? Where is the center in this reflex arc? What is the role of the effector? 2. A patient with a suspected neurological disorder is examined and found to have an exaggerated patellar reflex and no abdominal reflex. Describe a normal patellar reflex and a normal abdominal reflex. In view of the findings, where is the probable site of injury or disease in the central nervous system? If your diagnosis is correct, what body activities are most likely to be affected? 3. Explain why spinal segment #25 does not lie under vertebra #25 (lumbar vertebra #5, or L5). Why is this knowledge useful in performing a spinal tap (lumbar puncture)?
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
THE BRAIN AND CRANIAL NERVES
I. INTRODUCTION A. The brain is the center for registering sensations, correlating them with one another and with stored information, making decisions, and taking action. 1. 2. B. It is also the center for intellect, emotions, behavior, and memory. It also directs our behavior towards others.
In this chapter we will consider the principal parts of the brain, how the brain is protected and nourished, and how it is related to the spinal cord and to the 12 pairs of cranial nerves.
II. OVERVIEW OF BRAIN ORGANIZATION AND BLOOD SUPPLY A. The major parts of the brain are the brain stem, diencephalon, cerebrum, and cerebellum. B. Blood Flow and the Blood-Brain Barrier 1. Blood flows to the brain mainly via blood vessels that branch from the cerebral arterial circle (circle of Willis) at the base of the brain; the veins that return blood from the head to the heart. 2. Although the brain comprises only about 2% of the total body weight, it utilizes about 20% of the oxygen used by the entire body. The brain is one of the most metabolically active organs of the body, and the amount of oxygen it uses varies with the degree of mental activity. 3. Any interruption of the oxygen supply to the brain can result in weakening, permanent damage, or death of brain cells. Interruption of the mother s blood supply to a child during childbirth before it can breathe may result in paralysis, mental retardation, epilepsy, or death. 4. Because carbohydrate storage in the brain is limited, the supply of glucose to the brain must be continuous. Glucose deficiency may produce mental confusion, dizziness, convulsions, and unconsciousness. 5. A blood-brain barrier (BBB) protects brain cells from harmful substances and pathogens by serving as a selective barrier to prevent passage of many substances from the blood to the brain. 6. An injury to the brain due to trauma, inflammation, or toxins causes a breakdown of the BBB, permitting the passage of normally restricted substances into brain tissue. The BBB may also prevent entry of drugs that could be used as therapy for brain cancer or other CNS disorders, so research is exploring ways to transport drugs past the BBB. C. Protective Covering of the Brain 1. 2. The brain is protected by the cranial bones and the cranial meninges. The cranial meninges are continuous with the spinal meninges and are named dura mater, arachnoid, and pia mater. 3. Three extensions of the dura mater separate parts of the brain: the falx cerebri, falx cerebelli, and the tentorium cerebelli.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
III. CEREBROSPINAL FLUID A. Cerebrospinal fluid (CSF) is a clear, colorless liquid that protects the brain and spinal cord against chemical and physical injuries and carries oxygen, glucose, and other needed chemicals from the blood to neurons and neuroglia. B. C. There are four CSF filled cavities within the brain called ventricles. CSF contributes to hemostasis by providing mechanical protection, chemical protection, and circulation. D. CSF is formed by filtration from networks of capillaries called choroid plexuses (found in the ventricles) and circulates through the subarachnoid space, ventricles, and central canal. E. Materials entering CSF from the choroid capillaries cannot leak between the surrounding ependymal cells; these constitute the blood-cerebrospinal fluid barrier, which permits certain substances to enter the fluid but excludes others and protects the brain and spinal cord from harmful elements. F. Most of the fluid is absorbed by the arachnoid villi of the superior sagittal blood sinus; this absorption normally occurs at the same rate at which CSF is produced in the choroid plexuses, thereby maintaining a relatively constant CSF volume and pressure. G. If CSF cannot circulate or drain properly due to some obstruction in the ventricles or subarachnoid space, a condition called hydrocephalus develops. The fluid buildup that occurs causes increased pressure on the brain, either internally or externally, depending on where the blockage is present. Surgically draining the ventricles and diverting the flow of CSF by an implanted shunt can positively and dramatically affect the individual s prognosis. (Clinical Application)
IV. THE BRAIN STEM A. Medulla Oblongata 1. The medulla oblongata, or just medulla, is continuous with the upper part of the spinal cord and contains portions of both motor and sensory tracts. 2. It also contains the nuclei of origin for cranial nerves VIII (cochlear and vestibular branches) through XII. 3. Structural regions of the medulla include the pyramids and the inferior olivary nucleus.
a. Decussation of pyramids results in neurons in the left cerebral cortex
controlling skeletal muscles on the right side of the body and neurons in the right cerebral cortex controlling skeletal muscles on the left side.
b. Inferior olivary neurons relay impulses from proprioceptors to the cerebellum.
4. Functional regions include nuclei that are reflex centers for regulation of heart rate, respiratory rate, vasoconstriction, swallowing, coughing, vomiting, sneezing, and hiccuping; the first three are considered vital reflexes. 5. Injury to the medulla can be fatal or lead to serious problems. (Clinical Application)
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
B.
Pons 1. The pons is located superior to the medulla. It connects the spinal cord with the brain and links parts of the brain with one another by way of tracts. 2. It relays nerve impulses related to voluntary skeletal movements from the cerebral cortex to the cerebellum. 3. The pons also contains the pneumotaxic and apneustic areas, which help control respiration along with the respiratory center in the medulla. 4. It contains nuclei for cranial nerves V through VII and the vestibular branch of VIII.
C.
Midbrain 1. The midbrain connects the pons and diencephalon. It conveys motor impulses from the cerebrum to the cerebellum and spinal cord, sends sensory impulses from the spinal cord to the thalamus, and regulates auditory and visual reflexes. 2. Structures within the midbrain include the cerebral peduncles, the corpora quadrigemina, the left and right substantia nigra, the left and right red nucleus, and the medial lemniscus. 3. 4. It also contains nuclei of origin for cranial nerves III and IV. A large portion of the brain stem is called the reticular formation. a. It consists of small areas of gray matter interspersed among fibers of white matter and has both sensory and motor functions. b. It helps regulate muscle tone, alerts the cortex to incoming sensory signals (reticular activating system, or RAS) and is responsible for maintaining consciousness and awakening from sleep.
V. THE CEREBELLUM A. The cerebellum occupies the inferior and posterior aspects of the cranial cavity and consists of two hemispheres and a central, constricted vermis. B. C. It is attached to the brain stem by three pairs of cerebellar peduncles. The cerebellum functions in the coordination of skeletal muscle contractions and in the maintenance of normal muscle tone, posture, and balance. VI. THE DIENCEPHALON A. Thalamus 1. The thalamus is located superior to the midbrain and contains nuclei that serve as relay stations for all sensory impulses, except smell, to the cerebral cortex. 2. 3. There are seven major groups of thalamic nuclei on each side. It also registers conscious recognition of pain and temperature and some awareness of light touch and pressure. 4. It plays an essential role in awareness and the acquisition of knowledge, which is termed cognition.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
B.
Hypothalamus 1. The hypothalamus is found inferior to the thalamus, has four major regions (mammillary, tuberal, supraoptic, and preoptic), controls many body activities, and is one of the major regulators of homeostasis. 2. The hypothalamus has a great number of functions. a. b. It functions in regulation of emotional and behavioral patterns. It regulates eating and drinking through the feeding center, satiety center, and thirst center. c. d. It aids in controlling body temperature. It regulates circadian rhythms and states of consciousness.
C.
Epithalamus 1. The epithalamus lies superior and posterior to the thalamus and contains the pineal gland and the habenular nuclei. 2. The pineal gland secretes melatonin to influence diurnal cycles in conjunction with the hypothalamus. 3. The habenular nuclei are involved in olfaction, especially emotional responses to odors.
D. Subthalamus 1. The subthalamus lies immediately inferior to the thalamus and includes tracts and the paired subthalamic nuclei, which connect to motor areas of the cerebrum. 2. The subthalamic nuclei and red nucleus and substantia nigra of the midbrain work together with the basal ganglia, cerebellum, and cerebrum in control of body movements. E. Circumventricular Organs 1. Parts of the diencephalon, called circumventricular organs (CVOs), can monitor chemical changes in the blood because they lack a blood-brain barrier. 2. CVOs include part of the hypothalamus, the pineal gland, the pituitary gland, and a few other nearby structures. 3. They function to coordinate homeostatic activities of the endocrine and nervous systems. 4. VII. THE CEREBRUM A. The cerebrum is the largest part of the brain. 1. The surface layer, the cerebral cortex, is 2-4 mm thick and is composed of gray matter. The cortex contains billions of neurons. 2. 3. The cortex contains gyri (convolutions), deep grooves called fissures, and shallower sulci. Beneath the cortex lies the cerebral white matter, tracts that connect parts of the brain with itself and other parts of the nervous system. They are also thought to be the site of entry into the brain of HIV.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
B.
The cerebrum is nearly separated into right and left halves, called hemispheres, by the longitudinal fissure. Internally it remains connected by the corpus callosum, a bundle of transverse white fibers.
C. Lobes 1. 2. 3. Each cerebral hemisphere is further subdivided into four lobes by sulci or fissures. The cerebral lobes are named the frontal, parietal, temporal, and occipital. A fifth part of the cerebrum, the insula, lies deep to the parietal, frontal, and temporal lobes and cannot be seen in an external view of the brain. D. White Matter 1. The white matter is under the cortex and consists of myelinated axons running in three principal directions. 2. Association fibers connect and transmit nerve impulses between gyri in the same hemisphere. 3. Commissural fibers connect gyri in one cerebral hemisphere to the corresponding gyri in the opposite hemisphere. 4. Projection fibers form ascending and descending tracts that transmit impulses from the cerebrum to other parts of the brain and spinal cord. E. Basal Ganglia 1. 2. F. The basal ganglia are paired masses of gray matter in each cerebral hemisphere. They are responsible for helping to control muscular movements.
Limbic System 1. 2. The limbic system is found in the cerebral hemispheres and diencephalon. It functions in emotional aspects of behavior and memory, and is associated with pleasure and pain.
G. Brain Injuries 1. Lapse in memory is one of many effects resulting from brain injuries; brain injuries are commonly associated with head injuries and result, in part, from displacement and distortion of neuronal tissue at the moment of impact and in part from the release of disruptive chemicals from injured brain cells. 2. Various degrees of brain injury are described by the terms concussion, contusion, and laceration. CEREBRAL CORTEX AREAS AND FUNCTIONS A. Specific types of sensory, motor, and integrative signals are processed in certain cerebral regions. 1. Sensory Areas a. The sensory areas of the cerebral cortex are concerned with the reception and interpretation of sensory impulses. b. Some important sensory areas include the primary somatosensory area, primary visual area, primary auditory area, and primary gustatory area.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
2.
Motor Areas a. b. The motor areas are the regions that govern muscular movement. Two important motor areas are the primary motor area and Broca s speech area.
3.
Association Areas a. The association areas are concerned with complex integrative functions such as memory, emotions, reasoning, will, judgment, personality traits, and intelligence. b. Association areas include the somatosensory association area, visceral association area, auditory association area, Wernicke s (posterior language) area, common integrative area, premotor area, frontal eye field area, and language areas.
4.
Injury to the association or motor speech areas results in aphasia, an inability to use or comprehend words. (Clinical Application)
B.
Hemispheric Lateralization 1. The two hemispheres of the cerebrum are not bilaterally symmetrical, either anatomically or functionally, with the functional asymmetry called hemispheric lateralization. 2. The left hemisphere is more important for right-handed control, spoken and written language, and numerical and scientific skills. 3. The right hemisphere is more important for left-handed control, musical and artistic awareness, space and pattern perception, insight, imagination, and generating mental images of sight, sound, touch, taste, and smell.
C.
Brain Waves 1. 2. Electrical potentials generated by brain cells are called brain waves. Brain waves generated by the cerebral cortex are recorded as an electroencephalogram (EEG). 3. An EEG may be used to diagnose epilepsy and other seizure disorders, infectious diseases, tumors, trauma, hematomas, metabolic abnormalities, degenerative diseases, and periods of unconsciousness and confusion; it may also provide useful information regarding sleep and wakefulness. 4. An EEG may also be one criterion in confirming brain death (complete absence of brain waves in two EEGs taken 24 hours apart).
IX. CRANIAL NERVES A. Twelve pairs of cranial nerves originate from the brain B. The pairs are named primarily on the basis of distribution and numbered by order of attachment to the brain.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
C.
Some cranial nerves (I, II, and VIII) contain only sensory fibers and are called sensory nerves. The rest are mixed nerves because they contain both sensory and motor fibers.
X. DEVELOPMENTAL ANATOMY OF THE NERVOUS SYSTEM A. The development of the nervous system begins with a thickening of the ectoderm called the neural plate. B. The parts of the brain develop from primary and secondary vesicles.
XI. AGING AND THE NERVOUS SYSTEM A. Age-related effects involve loss of neurons and decreased capacity for sending nerve impulses to and from the brain; processing of information also diminishes. B. Other effects include decreased conduction velocity, slowing of voluntary motor movements, and increased reflex time. C. Degenerative changes and disease states involving the sense organs can alter vision, hearing, taste, smell, and touch. XII. DISORDERS: HOMEOSTATIC IMBALANCES A. The most common brain disorder is a cerebrovascular accident (CVA or stroke). 1. CVAs are classified into two principal types: ischemic (the most common type), due to a decreased blood supply, or hemorrhagic, due to a blood vessel in the brain that bursts. 2. 3. Common causes of CVAs are intracerebral hemorrhage, emboli, and atherosclerosis. CVAs are characterized by abrupt onset of persisting neurological symptoms that arise from destruction of brain tissue (infarction). B. A transient ischemic attack (TIA) is an episode of temporary cerebral dysfunction caused by impaired blood flow to the brain. 1. Symptoms include dizziness, weakness, numbness, or paralysis in a limb or in half of the body; drooping of one side of the face; headache; slurred speech or difficulty understanding speech; or a partial loss of vision or double vision. 2. Onset is sudden and a TIA usually persists for only a few minutes, rarely lasting as long as 24 hours. 3. Causes of the impaired blood flow include blood clots, atherosclerosis, and certain blood disorders; TIAs commonly are forerunners of future CVAs. C. Alzheimer s disease (AD) is a disabling neurological disorder that afflicts about 11% of the population over age 65. 1. Its causes are unknown, its effects are irreversible and devastating, and it has no cure at the present time. 2. It involves widespread intellectual impairment, personality changes, sometimes delirium, and culminates in dementia, the loss of reason and ability to care for oneself. 3. A person with AD usually dies of some complication that affects bedridden patients, such as pneumonia. 4. Brains of AD victims show three distinct structural abnormalities:
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
a. Great loss of neurons in specific regions (e.g., hippocampus and cerebral
cortex).
b. Plaques of abnormal proteins deposited outside neurons (amyloid plaques). c. Tangled protein filaments within neurons (neurofibrillary tangles).
Critical Thinking Questions 1. A 35-year-old male exhibits the following symptoms: tremors of the arms and hands, rigidity of the facial muscles, wide-eyed unblinking stare, and saliva drooling from the corners of the mouth. What is the probable disorder? How may the condition be treated? 2. An 18-year-old male was involved in a car wreck where he suffered a whiplash injury. Based on your knowledge of the brain stem, what problems might he be facing depending on the extent of his injuries?
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
THE SPECIAL SENSES
I. INTRODUCTION A. Receptors for the special senses - smell, taste, vision, hearing, and equilibrium - are housed in complex sensory organs. B. C. Ophthalmology is the science that deals with the eye and its disorders. Otolaryngology is the science that deals with the other special senses.
II. OLFACTION: SENSE OF SMELL A. Both smell and taste are chemical senses. B. Anatomy of olfactory receptors
1. The receptors for olfaction, which are bipolar neurons, are in the nasal epithelium in the
superior portion of the nasal cavity.
2. They are first-order neurons of the olfactory pathway. 3. Supporting cells are epithelial cells of the mucous membrane lining the nose. 4. Basal stem cells produce new olfactory receptors.
C. Physiology of Olfaction
1. Genetic evidence suggests there are hundreds of primary scents. 2. In olfactory reception, a generator potential develops and triggers one or more nerve
impulses. D. Adaptation to odors occurs quickly, and the threshold of smell is low: only a few molecules of certain substances need be present in air to be smelled. E. Olfactory receptors convey nerve impulses to olfactory nerves, olfactory bulbs, olfactory tracts, and the cerebral cortex and limbic system. F. Hyposmia, a reduced ability to smell, affects half of those over age 65 and 75% of those over 80. It can be caused by neurological changes, drugs, or the effects of smoking (Clinical Application).
III. GUSTATORY: SENSE OF SMELL A. Taste is a chemical sense. 1. 2. 3. B. To be detected, molecules must be dissolved. Taste stimuli classes include sour, sweet, bitter, and salty. Other tastes are a combination of the four taste sensations plus olfaction.
Anatomy of Taste Buds and Papillae 1. 2. 3. The receptors for gustation, the gustatory receptor cells, are located in taste buds. Taste buds consist of supporting cells, gustatory receptor cells, and basal cells. Taste buds are found in papillae. a. b. The papillae include circumvallate, fungiform, and filiform papillae. They appear as elevations on the tongue.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
C.
Physiology of Gustation 1. When a tastant is dissolved in saliva it can make contact with the plasma membrane of gustatory receptor cells. 2. Receptor potentials developed in gustatory hairs cause the release of neurotransmitter that gives rise to nerve impulses. 3. Individual gustatory receptors in certain regions of the tongue are more sensitive than others to the primary taste sensations. 4. Figure 16.3 shows the responses of three groups of taste neurons to sweet, salty, and sour chemicals.
D. Taste Thresholds and Adaptation
1. Taste thresholds vary for each of the primary tastes with the threshold for bitter being
the lowest, then sour, and finally salty and sweet.
2. Adaptation to taste occurs quickly.
E. Gustatory receptor cells convey nerve impulses to cranial nerves V, VII, IX, and S, the medulla, the thalamus, and the parietal lobe of the cerebral cortex. F. Taste aversion causes individuals to avoid foods which upset their digestive system. Because cancer treatments cause nausea, cancer patients may lose their appetites because they develop taste aversion for most food (Clinical Application).
IV. VISION A. Introduction 1. More than half the sensory receptors in the human body are located in the eyes. 2. A large part of the cerebral cortex is devoted to processing visual information. B. Accessory Structures of the Eyes 1. Eyelids a. The eyelids shade the eyes during sleep, protect the eyes from excessive light
and foreign objects, and spread lubricating secretions over the eyeballs.
b. From superficial to deep, each eyelid consists of epidermis, dermis,
subcutaneous tissue, fibers of the orbicularis oculi muscle, a tarsal plate, tarsal glands, and conjunctiva.
1) The tarsal plate gives form and support to the eyelids. 2) The tarsal glands secrete a fluid to keep the eye lids from adhering to
each other.
3) The conjunctiva is a thin mucous membrane that lines the inner aspect
of the eyelids and is reflected onto the anterior surface of the eyeball.
2. Eyelashes and eyebrows help protect the eyeballs from foreign objects, perspiration, and
the direct rays of the sun.
3. The lacrimal apparatus consists of structures that produce and drain tears.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
4. The six extrinsic eye muscles move the eyeballs laterally, medially, superiorly, and
inferiorly.
C. Anatomy of the Eyeball 1. The eye is constructed of three layers. a. The fibrous tunic is the outer coat of the eyeball. It can be divided into two
regions: the posterior sclera and the anterior cornea. At the junction of the sclera and cornea is an opening known as the scleral venous sinus or canal of Schlemm.
1) The sclera, the white of the eye, is a white coat of dense fibrous
tissue that covers all the eyeball, except the most anterior portion, the iris; the sclera gives shape to the eyeball and protects its inner parts. Its posterior surface is pierced by the optic nerve.
2) The cornea is a nonvascular, transparent, fibrous coat through which
the iris can be seen; the cornea acts in refraction of light.
3) Corneal transplants are the most common organ transplant operation,
and they are considered to be the most successful type of transplant since they are rarely rejected. This is because the cornea is a vascular, and antibodies that might cause rejection do not circulate there (the cornea receives nourishment from tears and aqueous humor). (Clinical Application)
b. The vascular tunic is the middle layer of the eyeball and is composed of three
portions: choroid, ciliary body, and iris.
1) The choroid absorbs light rays so that they are not reflected and
scattered within the eyeball; it also provides nutrients to the posterior surface of the retina.
2) The ciliary body consists of the ciliary processes and ciliary muscle. a) The ciliary processes consist of protrusions or folds on the
internal surface of the ciliary body where epithelial lining cells secrete aqueous humor.
b) The ciliary muscle is a smooth muscle that alters the shape of
the lens for near or far vision.
3) The iris is the colored portion seen through the cornea and consists of
circular iris and radial iris smooth muscle fibers (cells) arranged to form a doughnut-shaped structure.
a) The black hole in the center of the iris is the pupil, the area
through which light enters the eyeball.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
b) A principal function of the iris is to regulate the amount of
light entering the posterior cavity of the eyeball
c. The third and inner coat of the eye, the retina (nervous tunic), lines the
posterior three-quarters of the eyeball and is the beginning of the visual pathway.
1) The surface of the retina is the only place in the body where blood
vessels can be viewed directly and examined for pathological changes.
a) The optic disc is the site where the optic nerve enters the
eyeball.
b) The vessels of the retina are the central retinal artery and
vein. They are bundled together with the optic nerve with branches across the retinal surface.
2) The retina consists of a pigment epithelium (nonvisual portion) and a
neural portion (visual portion).
a) The pigment epithelium aids the choroid in absorbing stray
light rays.
b) The neural portion contains three zones of neurons that are
named in the order in which they conduct nerve impulses: photoreceptor neurons, bipolar neurons, and ganglion neurons.
(1) The photoreceptor neurons are called rods or cones
because of the differing shapes of their outer segments.
(2) Rods are specialized for black-and-white vision in dim
light; they also allow us to discriminate between different shades of dark and light and permit us to see shapes and movement.
(3) Cones are specialized for color vision and sharpness
of vision (high visual acuity) in bright light; cones are most densely concentrated in the central fovea, a small depression in the center of the macula lutea.
(a) The macula lutea is in the exact center of
the posterior portion of the retina, corresponding to the visual axis of the eye.
(b) The fovea is the area of sharpest vision
because of the high concentration of cones.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
(c) Rods are absent from the fovea and macula
and increase in density toward the periphery of the retina.
2. The eyeball contains the nonvascular lens, just behind the pupil and iris. The lens fine
tunes the focusing of light rays for clear vision.
3. The interior of the eyeball is a large space divided into two cavities by the lens: the
anterior cavity and the vitreous chamber.
a. The anterior cavity is subdivided into the anterior chamber (which lies behind
the cornea and in front of the iris) and the posterior chamber (which lies behind the iris and in front of the suspensory ligaments and lens).
1) The anterior cavity is filled with a watery fluid called the aqueous
humor that is continually secreted by the ciliary processes behind the iris.
2) The aqueous humor flows forward from the posterior chamber
through the pupil into the anterior chamber and drains into the scleral venous sinus (canal of Schlemm) and then into the blood.
a) The pressure in the eye, called intraocular pressure, is
produced mainly by the aqueous humor. The intraocular pressure, along with the vitreous body, maintains the shape of the eyeball and keeps the retina smoothly applied to the choroid so the retina will form clear images.
b) Excessive intraocular pressure, called glaucoma, results in
degeneration of the retina and blindness.
b. The second, and larger, cavity of the eyeball is the vitreous chamber (posterior
cavity). It lies between the lens and the retina and contains a gel called the vitreous body. It is formed during embryonic life and is not replaced thereafter.
4. Table 16.1 summarizes the structures associated with the eyeball. 5. Age related macular disease is a degenerative disorder of the retina and the pigmented
layer in persons 50 years of age or older (Clinical application).
D. Image Formation 1. Image formation on the retina involves refraction of light rays by the cornea and lens,
accommodation of the lens, and constriction of the pupil.
a. The bending of light rays at the interface of two different media is called
refraction; the anterior and posterior surfaces of the cornea and of the lens refract entering light rays so they come into exact focus on the retina.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
1) Images are focused upside-down (inverted) on the retina and also
undergo mirror reversal; these inverted images are rearranged by the brain to produce perception of images in their actual orientation.
2) The lens fine tunes image focus and changes the focus for near or
distant objects.
b. Accommodation and Near Point of Vision 1) Accommodation is an increase in the curvature of the lens, initiated by
ciliary muscle contraction, which allows the lens to focus on near objects. To focus on far objects, the ciliary muscle relaxes and the lens flattens.
2) The near point of vision is the minimum distance from the eye that an
object can be clearly focused with maximum effort.
3) With aging the lens loses elasticity and its ability to accommodate
resulting in a condition known as presbyopia (Clinical application).
c. Refraction Abnormalities 1) Myopia is nearsightedness. 2) Hyperopia is farsightedness. 3) Astigmatism is a refraction abnormality due to an irregular curvature
of either the cornea or lens.
d. Constriction of the pupil means narrowing the diameter of the hole through
which light enters the eye; this occurs simultaneously with accommodation of the lens and functions to prevent light rays from entering the eye through the periphery of the lens.
2. In convergence, the eyeballs move medially so they are both directed toward an object
being viewed; the coordinated action of the extrinsic eye muscles bring about convergence.
E. Physiology of Vision 1. The first step in vision transduction is the absorption of light by photopigments (visual
pigments) in rods and cones (photoreceptors).
a. Photopigments are colored proteins that undergo structural changes upon
light absorption.
b. The single type of photopigment in rods is called rhodopsin. A cone
contains one of three different kinds of photopigments so there are three types of cones.
1) All photopigments involved in vision contain a glycoprotein called
opsin and a derivative of vitamin A called retinal.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
2) Retinal is the light absorbing part of all visual photopigments. 3) There are four different opsins, one for each cone photopigment
and another for rhodopsin.
2. Bleaching and regeneration of the photopigments accounts for much but not all of the
sensitivity change during light and dark adaptation.
3. Once receptor potentials develop in rods and cones, they release neurotransmitters that
induce graded potentials in bipolar cells and horizontal cells.
4. Most forms of colorblindness (inability to distinguish certain colors) result from an
inherited absence of or deficiency in one of the three cone photopigments and are more common in males. A deficiency in rhodopsin may cause night blindness (nyctalopia) (Clinical application).
F. Visual Pathway 1. Horizontal cells transmit inhibitory signals to bipolar cells; bipolar or amacrine cells
transmit excitatory signals to ganglion cells, which depolarize and initiate nerve impulses.
2. Impulses from ganglion cells are conveyed through the retina to the optic nerve, the
optic chiasma, the optic tract, the thalamus, and the occipital lobes of the cortex.
V. HEARING AND EQUILIBRIUM A. The ear consists of three anatomical subdivisions. 1. The external (outer) ear collects sound waves and passes them inwards; it consists of the
auricle (pinna), external auditory canal (meatus), and tympanic membrane (eardrum)
a. Ceruminous glands in the external auditory canal secrete cerumen (earwax) to
help prevent dust and foreign objects from entering the ear.
b. Excess cerumen may become impacted, causing temporary partial hearing loss
before it is removed.
2. The middle ear (tympanic cavity) is a small, air-filled cavity in the temporal bone that is
lined by epithelium. It contains the auditory (Eustachian) tube, auditory ossicles (middle ear bones, the malleus, incus, and stapes), the oval window, and the round window.
3. The internal (inner) ear is also called the labyrinth because of its complicated series of
canals. Structurally it consists of two main divisions: an outer bony labyrinth that encloses an inner membranous labyrinth.
a. The bony labyrinth is a series of cavities in the petrous portion of the temporal
bone.
1) It can be divided into three areas named on the basis of shape: the
semicircular canals and vestibule, both of which contain receptors for equilibrium, and the cochlea, which contains receptors for hearing.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
2) The bony labyrinth is lined with periosteum and contains a fluid called
perilymph. This fluid, chemically similar to cerebrospinal fluid, surrounds the membranous labyrinth.
b. The membranous labyrinth is a series of sacs and tubes lying inside and having
the same general form as the bony labyrinth.
1) The membranous labyrinth is lined with epithelium. 2) It contains a fluid called endolymph, chemically similar to intracellular
fluid.
c. The vestibule constitutes the oval central portion of the bony labyrinth. The
membranous labyrinth in the vestibule consists of two sacs called the utricle and saccule.
d. Projecting upward and posteriorly from the vestibule are the three bony
semicircular canals. Each is arranged at approximately right angles to the other two.
1) The anterior and posterior semicircular canals are oriented vertically;
the lateral semicircular canal is oriented horizontally.
2) One end of each canal enlarges into a swelling called the ampulla. 3) The portions of the membranous labyrinth that lie inside the
semicircular canals are called the semicircular ducts (membranous semicircular canals).
e. The vestibular branch of the vestibulocochlear nerve consists of ampullary,
utricular, and saccular nerves.
f. Anterior to the vestibule is the cochlea, which consists of a bony spiral canal
that makes almost three turns around a central bony core called the modiolus.
1) Cross sections through the cochlea show that it is divided into three
channels by partitions that together have the shape of the letter Y.
a) The channel above the bony partition is the scala vestibuli,
which ends at the oval window.
b) The channel below is the scala tympani, which ends at the
round window. The scala vestibuli and scala tympani both contain perilymph and are completely separated except at an opening at the apex of the cochlea called the helicotrema.
c) The third channel (between the wings of the Y) is the cochlear
duct (scala media). The vestibular membrane separates the cochlear duct from the scala vestibuli, and the basilar membrane separates the cochlear duct from the scala tympani.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
2) Resting on the basilar membrane is the spiral organ (organ of Corti),
the organ of hearing.
3) Projecting over and in contact with the hair cells of the spiral organ is
the tectorial membrane, a delicate and flexible gelatinous membrane.
B. Sound waves result from the alternate compression and decompression of air molecules. 1. The sounds heard most acutely by human ears are from sources that vibrate at
frequencies between 1000 and 4000 Hertz (Hz; cycles per minute).
2. The frequency of a sound vibration is its pitch; the greater the intensity (size) of the
vibration, the louder the sound (as measured in decibels, dB).
3. Exposure to loud sounds can damage hair cells of the cochlea and possibly lead to
deafness. (Clinical Application)
C. Physiology of Hearing 1. The events involved in hearing are: a. The auricle directs sound waves into the external auditory canal. b. Sound waves strike the tympanic membrane, causing it to vibrate back and
forth.
c. The vibration conducts from the tympanic membrane through the ossicles
(through the malleus to the incus and then to the stapes).
d. The stapes moves back and forth, pushing the membrane of the oval
window in and out.
e. The movement of the oval window sets up fluid pressure waves in the
perilymph of the cochlea (scala vestibuli).
f. Pressure waves in the scala vestibuli are transmitted to the scala tympani
and eventually to the round window, causing it to bulge outward into the middle ear.
g. As the pressure waves deform the walls of the scala vestibuli and scala
tympani, they push the vestibular membrane back and forth and increase and decrease the pressure of the endolymph inside the cochlear duct.
h. The pressure fluctuations of the endolymph move the basilar membrane
slightly, moving the hair cells of the spiral organ against the tectorial membrane; the bending of the hairs produces receptor potentials that lead to the generation of nerve impulses in cochlear nerve fibers.
i. Pressure changes in the scala tympani cause the round window to bulge
outward into the middle ear.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
2. Differences in pitch are related to differences in the width and stiffness of the basilar
membrane and sound waves of various frequencies that cause specific regions of the basilar membrane to vibrate more intensely than others.
a. High-frequency or high-pitched sounds cause the basilar membrane to
vibrate near the base of the cochlea.
b. Low-frequency or low-pitched sounds cause the basilar membrane to
vibrate near the apex of the cochlea.
3. Hair cells convert a mechanical force (stimulus) into an electrical signal (receptor
potential); hair cells release neurotransmitter, which initiates nerve impulses.
4. The cochlea can produce sounds called otoacoustic emissions. They are caused by
vibrations of the outer hair cells that occur in response to sound waves and to signals from motor neurons.
D. Auditory Pathway 1. Nerve impulses from the cochlear branch of the vestibulocochlear nerve pass to the
cochlear nuclei in the medulla. Here, most impulses cross to the opposite side and then travel to the midbrain, to the thalamus, and finally to the auditory area of the temporal lobe of the cerebral cortex.
2. Cochlear implants are devices that translate sounds into electronic signals that can be
interpreted by the brain. (Clinical Application)
E. Physiology of Equilibrium 1. There are two kinds of equilibrium. a. Static equilibrium refers to the maintenance of the position of the body (mainly
the head) relative to the force of gravity.
b. Dynamic equilibrium is the maintenance of body position (mainly the head) in
response to sudden movements, such as rotation, acceleration, and deceleration.
2. Otolithic Organs: Saccule and Utricle a. The maculae of the utricle and saccule are the sense organs of static
equilibrium; they also contribute to some aspects of dynamic equilibrium.
b. The maculae consist of hair cells, which are sensory receptors, and supporting
cells.
3. Membranous Semicircular Ducts a. The three semicircular ducts, along with the saccule and utricle maintain
dynamic equilibrium.
b. The cristae in the semicircular ducts are the primary sense organs of dynamic
equilibrium.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
4. Equilibrium Pathways a. Most vestibular branch fibers of the vestibulocochlear nerve enter the brain
stem and terminate in the medulla; the remaining fibers enter the cerebellum.
b. Various pathways between the vestibular nuclei, cerebellum, and cerebrum
enable the cerebellum to play a key role in maintaining static and dynamic equilibrium.
DEVELOPMENT OF THE EYES AND EARS
A. Eyes 1. Eyes begin to develop when the ectoderm of the lateral walls of the prosencephalon
bulges to form a pair of optic grooves
2. As the neural tube closes the optic grooves enlarge and move toward the surface of the
ectoderm and are known as optic vesicles
3. When the optic vesicles reach the surface, the surface ectoderm thichens to form the
lens placodes and the distal portions of the optic vesicles invaginate to form the optic cups.
4. The optic cups remain attached to the prosencephalon by the optic stalks. B. Ears 1. Inner ear develops from a thickening of surface ectoderm called the otic placode. 2. Otic placodes invaginate to form otic pits 3. Optic pits pinch off from the surface ectoderm to form otic vesicles 4. Otic vesicles will form structures associated with the membranous labyrinth of the inner
ear.
5. Middle ear develops from the first pharyngeal (branchial) pouch. 6. The extermal ear develops from the first pharyngeal cleft.
DISORDERS: HOMEOSTATIC IMBALANCES A. A cataract is a loss of transparency of the lens that can lead to blindness. B. Glaucoma is abnormally high intraocular pressure, due to a buildup of aqueous humor inside the eyeball, which destroys neurons of the retina. It is the second most common cause of blindness (after cataracts), especially in the elderly. C. Deafness is significant or total hearing loss. It is classified as sensorineural (caused by impairment of the cochlear or cochlear branch of the vestibulocochlear nerve) or conduction (caused by impairment of the external and middle ear mechanisms for transmitting sounds to the cochlea). D. Meniere s syndrome is a malfunction of the inner ear that may cause deafness and loss of equilibrium.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
E.
Otitis media is an acute infection of the middle ear, primarily by bacteria. It is characterized by pain, malaise, fever, and reddening and outward bulging of the eardrum, which may rupture unless prompt treatment is given. Children are more susceptible than adults.
Critical Thinking Questions 1. The seventh grade class of a junior high school has just completed its annual eye examination. The examiner determines that there are only two abnormal cases. One child has myopia and the other hypermetropia. What is myopia? Why does it occur. How should it be corrected? What is hypermetropia? Why does it occur? How should it be corrected? 2. A sixteen-year-old boy has been diagnosed with partial deafness in both of his ears. Prior to the diagnosis, he spent most of his free time listening to loud music from the earphones he always wore. Explain what might be the cause of his deafness.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
THE ENDOCRINE SYSTEM
I. COMPARISON of the CONTROL by the NERVOUS and ENDOCRINE SYSTEM
A. Together the nervous and endocrine systems coordinate functions of all body systems. 1. The nervous system controls body actions through nerve impulses. 2. The endocrine system controls body activities by releasing mediator molecules called
hormones.
3. The science concerned with the structure and function of the endocrine glands and the
diagnosis and treatment of endocrine disorders is called endocrinology.
B. The nervous and endocrine systems act as a coordinated interlocking supersystem, the
neuroendocrine system.
1. Parts of the nervous system stimulate or inhibit the release of hormones. 2. Hormones may promote or inhibit the generation of nerve impulses. C. The nervous system causes muscles to contract or glands to secrete. The endocrine system
affects virtually all body tissues by altering metabolism, regulating growth and development, and influencing reproductive processes.
D. Table 18.1 compares the characteristics of the nervous and endocrine systems. II. ENDOCRINE GLAND A. The body contains two kinds of glands: exocrine and endocrine. 1. Exocrine glands secrete their products into ducts, and the ducts carry the secretions to
the target site.
2. Endocrine glands secrete their products (hormones) into the interstitial fluid surrounding
the secretory cells from which they diffuse into capillaries to be carried away by blood.
B. Endocrine glands constitute the endocrine system and include the pituitary, thyroid, parathyroid,
adrenal, and pineal glands
III. HORMONE ACTIVITY A. Hormones have powerful effects when present in very low concentrations. B. Hormone Receptors 1. Although hormones travel in blood throughout the body, they affect only specific target
cells.
2. Target cells have specific protein or glycoprotein receptors to which hormones bind. 3. Receptors are constantly being synthesized and broken down. a. When a hormone is present in excess, down-regulation, the decrease in the
number of receptors, may occur.
b. When a hormone is deficient, up-regulation, an increase in the number of
receptors, may occur.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
4. Synthetic hormones that block the receptors for particular naturally occurring hormones
are available as drugs. (Clinical Application)
C. Circulating and Local Hormones 1. Hormones that travel in blood and act on distant target cells are called circulating
hormones or endocrines.
2. Hormones that act locally without first entering the blood stream are called local
hormones.
a. Those that act on neighboring cells are called paracrines. b. Those that act on the same cell that secreted them are termed autocrines. 3. Figure 18.2 compares the site of action of circulating and local hormones. D. Chemical Classes of Hormones 1. Lipid-soluble hormones include the steroids, thyroid hormones, and nitric oxide, which
acts as a local hormone in several tissues.
2. Water-soluble hormones include the amines; peptides, proteins, and glycoproteins; and
eicosanoids.
E. Hormone Transport in Blood 1. Most water-soluble hormones circulate in plasma in a free, unattached form. 2. Most lipid-soluble hormones bind to transport proteins to be carried in blood. 3. The transport proteins improve the transportability of lipid-soluble hormones by making
them temporarily water-soluble, retard passage of the small hormone molecules through the kidney filter thus slowing the rate of hormone loss in urine, and provide a ready reserve of hormone already present in blood.
4. Protein and peptide hormones, such as insulin, will be destroyed by digestive enzymes
and must be given by injection (Clinical Application).
IV. MECHANISMS OF HORMONE ACTION A. The response to a hormone depends on both the hormone and the target cell; various target cells
respond differently to different hormones.
B. Action of Lipid-Soluble Hormone 1. Lipid-soluble hormones bind to and activate receptors within cells. 2. The activated receptors then alter gene expression which results in the formation of new
proteins.
3. The new proteins alter the cells activity and result in the physiological responses of
those hormones.
C. Action of Water-Soluble Hormones 1. Water-soluble hormones alter cell functions by activating plasma membrane receptors,
which set off a cascade of events inside the cell.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
a. The water-soluble hormone that binds to the cell membrane receptor is the
first messenger.
b. A second messenger is released inside the cell where hormone stimulated
response takes place.
2. A typical mechanism of action of a water-soluble hormone using cyclic AMP as the
second messenger.
a. The hormone binds to the membrane receptor. b. The activated receptor activates a membrane G-protein which turns on
adenylate cyclase.
c. Adenylate cyclase converts ATP into cyclic AMP which activates protein kinases. d. Protein kinases phosphorylate enzymes which catalyze reactions that produce
the physiological response.
3. Since hormones that bond to plasma membrane receptors initiate a cascade of events,
they can induce their effects at very low concentrations.
4. The cholera toxin modifies G-proteins in epithelial cells lining the intestine so they
become locked in an activated state which results in the massive fluid loss this toxin causes. (Clinical Application)
D. Hormonal Interactions 1. The responsiveness of a target cell to a hormone depends on the hormone s
concentration, the abundance of the target cell s hormone receptors, and influences exerted by other hormones.
2. Three hormonal interactions are the permissive effect, the synergistic effect, and the
antagonist effect.
V. CONTROL OF HORMONE SECRETIONS A. Most hormones are released in short bursts, with little or no release between bursts. Regulation
of hormone secretion normally maintains homeostasis and prevents overproduction or underproduction of a particular hormone; when these regulating mechanisms do not operate properly, disorders result.
B. Hormone secretion is controlled by signals from the nervous system, by chemical changes in the
blood, and by other hormones.
C. Most often, negative feedback systems regulate hormonal secretions. VI. HYPOTHALAMUS AND PITUITARY GLAND A. The hypothalamus is the major integrating link between the nervous and endocrine systems. B. The hypothalamus and the pituitary gland (hypophysis) regulate virtually all aspects of growth,
development, metabolism, and homeostasis.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
C. The pituitary gland is located in the sella turcica of the sphenoid bone and is differentiated into
the anterior pituitary (adenohypophysis), the posterior pituitary (neurohypophysis), and pars intermedia (avascular zone in between.
1. Anterior Pituitary Gland (Adenohypophysis) a. Hormones of the anterior pituitary are controlled by releasing or inhibiting
hormones produced by the hypothalamus.
b. The blood supply to the anterior pituitary is from the superior hypophyseal
arteries.
c. Hormones of the anterior pituitary and the cells that produce them are as
follows.
1) Human growth hormone (hGH) is secreted by somatotrophs. 2) Thyroid-stimulating hormone (TSH) is secreted by thyrotrophs. 3) Follicle-stimulating hormone (FSH) and luteinizing hormone (LH) are
secreted by gonadotrophs.
4) Prolactin (PRL) is secreted by lactrotrophs. 5) Adrenocorticotrophic hormone (ACTH) and melanocyte-stimulating
hormone (MSH) are secreted by corticotrophs.
d. Secretion of anterior pituitary gland hormones is regulated by hypothalamic
regulating hormones and by negative feedback mechanisms.
e. Human Growth Hormone and Insulinlike Growth Factors 1) Human growth hormone (hGH) is the most plentiful anterior pituitary
hormone.
2) It acts indirectly on tissues by promoting the synthesis and secretion of
small protein hormones called insulinlike growth factors (IGFs).
3) IGFs stimulate general body growth and regulate various aspects of
metabolism.
4) Various stimuli promote and inhibit hGH production. 5) One symptom of excess hGH is hyperglycemia. (Clinical Application) g. Thyroid-stimulating hormone (TSH) regulates thyroid gland activities and is
controlled by TFH (thyrotropin releasing hormone).
h. Follicle-Stimulating Hormone (FSH) 1) In females, FSH initiates follicle development and secretion of
estrogens in the ovaries.
2) In males, FSH stimulates sperm production in the testes. i.
Luteinizing Hormone (LH)
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
1) In females, LH stimulates secretion of estrogen by ovarian cells to
result in ovulation and stimulates formation of the corpus luteum and secretion of progesterone.
2) In males, LH stimulates the interstitial cells of the testes to secrete
testosterone.
j.
Prolactin (PRL), together with other hormones, initiates and maintains milk secretion by the mammary glands.
k. Adrenocorticotrophic hormone (ACTH) controls the production and secretion of
hormones called glucocorticoids by the cortex of the adrenal gland.
l.
Melanocyte-stimulating hormone (MSH) increases skin pigmentation although its exact role in humans is unknown.
m. Table 18.4 summarizes the principal actions of the anterior pituitary gland
hormones.
2. Posterior Pituitary Gland (Neurohypophysis) a. Although the posterior pituitary gland does not synthesize hormones, it does
store and release two hormones.
b. The neural connection between the hypothalamus and the neurohypophysis is
via the hypothalamohypophyseal tract (Figure 18.8).
c. Hormones made by the hypothalamus and stored in the posterior pituitary are
oxytocin (OT) and antidiuretic hormone (ADH).
1) Oxytocin stimulates contraction of the uterus and ejection (let-down)
of milk from the breasts.
2) Nursing a baby after delivery stiumlates oxytocin release promoting
uterine contractions and the expulsion of the placenta (Clinical Application).
3) Antidiuretic hormone stimulates water reabsorption by the kidneys
and arteriolar constriction.
a) The effect of ADH is to decrease urine volume and conserve
body water.
b) ADH is controlled primarily by osmotic pressure of the blood. VII. THYROID GLAND A. The thyroid gland is located just below the larynx and has right and left lateral lobes. B. Histologically, the thyroid consists of the thyroid follicles composed of follicular cells, which
secrete the thyroid hormones thyroxine (T4) and triiodothyronine (T3), and parafollicular cells, which secrete calcitonin (CT).
C. Formation, Storage, and Release of Thyroid Hormones
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
1. Thyroid hormones are synthesized from iodine and tyrosine within a large glycoprotein
molecule called thyroglobulin (TGB) and are transported in the blood by plasma proteins, mostly thyroxine-binding globulin (TBG).
2. The formation, storage, and release steps include iodide trapping, synthesis of
thyroglobulin, oxidation of iodide, iodination of tyrosine, coupling of T1 and T2, pinocytosis and digestion of colloid, secretion of thyroid hormones, and transport in blood.
D. Thyroid hormones regulate oxygen use and basal metabolic rate, cellular metabolism, and
growth and development.
E. Secretion of thyroid hormone is controlled by the level of iodine in the thyroid gland and by
negative feedback systems involving both the hypothalamus and the anterior pituitary gland.
F. Calcitonin lowers the blood level of calcium. Secretion is controlled by calcium levels in the
blood.
VIII. PARATHYROID GLANDS A. The parathyroid glands are embedded on the posterior surfaces of the lateral lobes of the thyroid
and contain principal cells, which produce parathyroid hormone, and oxyphil cells, whose function is unknown.
B. Parathyroid hormone (PTH) regulates the homeostasis of calcium and phosphate by increasing
blood calcium level and decreasing blood phosphate level.
1. PTH increases the number and activity of osteoclasts, increases the rate of Ca+2 and
Mg+2 from reabsorption from urine and inhibits the reabsorption of HPO4-2 so more is secreted in the urine, and promotes formation of calcitriol, which increases the absorption of Ca , Mg ,and HPO4 from the GI tract.
+2 +2 -2
2. Blood calcium level directly controls the secretion of calcitonin and parathyroid
hormone via negative feedback loops that do not involve the pituitary gland
IX. ADRENAL GLANDS A. The adrenal glands are located superior to the kidneys; they consists of an outer cortex and
an inner medulla.
B. Adrenal Cortex 1. The adrenal cortex is divided into three zones, each of which secretes different
hormones.
a. The zona glomerulosa (outer zone) secretes mineralocorticoids. b. The zona fasciculata (middle zone) secretes glucocorticoids. c. The zona reticularis (inner zone) secretes androgens. 2. Mineralocorticoids
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
a. Mineralocorticoids (e.g., aldosterone) increase sodium and water
reabsorption and decrease potassium reabsorption, helping to regulate sodium and potassium levels in the body.
b. Secretion is controlled by the renin-angiotensin pathway and the blood
level of potassium.
3. Glucocorticoids a. Glucocorticoids (e.g., cortisol) promote breakdown of proteins, formation
of glucose, lipolysis, resistance to stress, anti-inflammatory effects, and depression of the immune response.
b. Secretion is controlled by CRH (corticotropin releasing hormone) and ACTH
(adrenocorticotropic hormone) from the anterior pituitary.
4. Androgens secreted by the adrenal cortex usually have minimal effects. C. Adrenal Medulla 1. The adrenal medulla consists of hormone-producing cells, called chromaffin cells, which
surround large blood-filled sinuses.
2. Medullary secretions are epinephrine and norepinephrine (NE), which produce effects
similar to sympathetic responses.
3. They are released under stress by direct innervation from the autonomic nervous
system. Like the glucocorticoids of the adrenal cortex, these hormones help the body resist stress. However, unlike the cortical hormones, the medullary hormones are not essential for life.
X. PANCREATIC ISLETS A. The pancreas is a flattened organ located posterior and slightly inferior to the stomach and can
be classified as both an endocrine and an exocrine gland.
B. Histologically, it consists of pancreatic islets or islets of Langerhans and clusters of cells (acini)
(enzyme-producing exocrine cells).
C. Cell Types in the Pancreatic Islets 1. Alpha cells secrete the hormone glucagon which increases blood glucose levels. 2. Beta cells secrete the hormone insulin which decreases blood glucose levels. 3. Delta cells secrete growth hormone inhibiting hormone or somatostatin, which acts as a
paracrine to inhibit the secretion of insulin and glucagon.
4. F-cells secrete pancreatic polypeptide, which regulates release of pancreatic digestive
enzymes.
D. Regulation of glucagon and insulin secretion is via negative feedback mechanisms.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
XI. OVARIES AND TESTES A. Ovaries are located in the pelvic cavity and produce sex hormones (estrogens and progesterone)
related to development and maintenance of female sexual characteristics, reproductive cycle, pregnancy, lactation, and normal reproductive functions. The ovaries also produce inhibin and relaxin.
B. Testes lie inside the scrotum and produce sex hormones (primarily testosterone) related to the
development and maintenance of male sexual characteristics and normal reproductive functions. The testes also produce inhibin.
XII. PINEAL GLAND A. The pineal gland (epiphysis cerebri) is attached to the roof of the third ventricle, inside the brain. B. Histologically, it consists of secretory parenchymal cells called pinealocytes, neuroglia cells, and
scattered postganglionic sympathetic fibers. The pineal secrets melatonin in a diurnal rhythm linked to the dark-light cycle.
C. Seasonal affective disorder (SAD), a type of depression that arises during the winter months when
day length is short, is thought to be due, in part, to over-production of melatonin. Bright light therapy, repeated doses of several hours exposure to artificial light as bright as sunlight, may provide relief for this disorder and for jet lag.
XIII. THYMUS GLAND A. The thymus gland secretes several hormones related to immunity . B. Thymosin, thymic humoral-factor, thymic factor, and thymopoietin promote the proliferation and
maturation of T cells, a type of white blood cell involved in immunity.
XIV. OTHER HORMONES and GROWTH FACTORS A. Other endocrine cells 1. Several body tissues other than those usually classified as endocrine glands also contain
endocrine tissue and thus secrete hormones.
2. Table 18.11 summarizes these hormones and their actions. B. Eicosanoids 1. Eicosanoids, (prostaglandins [PGs] and leukotrienes [LTs]) act as paracrines and
autocrines in most body tissues by altering the production of second messengers, such as cyclic AMP.
2. Prostaglandins have a wide range of biological activity in normal physiology and
pathology.
3. Aspirin and related nonsteroidal anti-inflammatory drugs (NSAIDS), such as ibuprofen
and acetaminophen, inhibit a key enzyme in prostaglandin synthesis and are used to treat a wide variety of inflammatory disorders.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
C. Growth Factors 1. Growth factors are hormones that stimulate cell growth and division. 2. Examples include epidermal growth factor (EGF), platelet-derived growth factor (PDGF),
fibroblast growth factor (FGF), nerve growth factor (NGF), tumor angiogenesis factors (TAFs), insulinlike growth factor (IFG), and cytokines.
XV. STRESS RESPONSE A. Homeostatic mechanisms attempt to counteract the everyday stresses of living. If successful, the
internal environment maintains normal physiological limits of chemistry, temperature, and pressure. If a stress is extreme, unusual, or long-lasting, however, the normal mechanisms may not be sufficient, triggering a wide-ranging set of bodily changes called the stress response or general adaptation syndrome (GAS).
1. Unlike the homeostatic mechanisms, this syndrome does not maintain a constant
internal environment. It does just the opposite to prepare the body to meet an emergency.
2. Productive stress is termed eustress; whereas, harmful stress is termed distress. 3. The stimuli that produce the general adaptation syndrome are called stressors. 4. Stressors include almost any disturbance: heat or cold, surgical operations, poisons,
infections, fever, and strong emotional responses.
B. Stages of the General Adaptation Syndrome 1. Fight or Flight Response a. The alarm reaction is initiated by nerve impulses from the hypothalamus to the
sympathetic division of the autonomic nervous system and adrenal medulla
b. Responses are the immediate and brief flight-or-flight reactions that increase
circulation, promote catabolism for energy production, and decrease nonessential activities.
2. The Resistance Reaction a. The resistance reaction is initiated by regulating hormones secreted by the
hypothalamus.
b. The regulating hormones are CRH (corticotropin releasing hormone), GHRH
(growth hormone releasing hormone), and TRH (thyrotropin releasing hormone).
c. CRH stimulates the adenohypophysis (anterior pituitary) to increase its
secretion of ACTH (adrenocorticotropic hormone), which in turn stimulates the adrenal cortex to secrete hormones.
d. Resistance reactions are long-term and accelerate catabolism to provide energy
to counteract stress.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
e. Glucocorticoids are produced in high concentrations during stress. They create
many distinct physiological effects.
3. Exhaustion a. The stage of exhaustion results from dramatic changes during alarm and
resistance reactions.
b. Exhaustion is caused mainly by loss of potassium, depletion of adrenal
glucocorticoids, and weakened organs. If stress is too great, it may lead to death.
C. Stress and Disease 1. It appears that stress can lead to certain diseases. 2. Among stress-related conditions are gastritis, ulcerative colitis, irritable bowel
syndrome, peptic ulcers, hypertension, asthma, rheumatoid arthritis, migraine headaches, anxiety, and depression.
3. It has also been shown that people under stress are at a greater risk of developing
chronic disease or of dying prematurely.
4. A very important link between stress and immunity is interleukin-1 (IL-1) produced by
macrophages; it stimulates secretion of ACTH.
5. Post-traumatic Stress Disease may be related to the stress reaction and its effects on the
endocrine system (Clinical Application).
XVI. DEVELOPMENTAL ANATOMY OF THE ENDOCRINE SYSTEM A. The pituitary gland originates from two different regions of the ectoderm. 1. The anterior pituitary derives from the neurohypophyseal bud, located on the floor of
the hypothalamus.
2. The anterior pituitary is derived from an outgrowth of ectoderm from the mouth called
the hypophyseal (Rathke s) pouch.
B. The thyroid gland develops as a midventral outgrowth of endoderm, called the thyroid
diverticulum, from the floor of the pharynx at the level of the second pair of pharyngeal pouches.
C. Parathyroid glands develop from endoderm as outgrowths from the third and fourth pharyngeal
pouches.
D. The adrenal cortex is derived from intermediate mesoderm from the same region that produces
the gonads. The adrenal medulla is ectodermal in origin and derives from the neural crest, which also gives rise to sympathetic ganglion and other nervous system structures.
E. The pancreas develops from the outgrowth of endoderm from the part of the foregut that later
becomes the duodenum.
F. The pineal gland arises as an outgrowth between the thalamus and colliculi from ectoderm
associated with the diencephalon.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
G. The thymus gland arises from endoderm of the third pharyngeal pouch. XVII. AGING AND THE ENDOCRINE SYSTEM A. Pituitary gland production of hGH decreases with age, but production of gonadotropins and of
TSH increases with age. ACTH levels are unchanged with age.
B. The thyroid gland decreases its output of thyroxin with age. C. The thymus gland begins to atrophy at puberty. Adrenal glands produce less cortisol and
aldosterone with age.
D. The pancreas releases insulin more slowly with age, and receptor sensitivity to glucose declines. E. Ovaries reduce in size and no longer respond to gonadotropins. Testosterone production
decreases with age but does not present a serious problem.
XVIII. DISORDERS: HOMEOSTATIC IMBALANCES A. Pituitary Gland Disorders 1. Pituitary Dwarfism, Giantism, and Acromegaly a. Hyposecretion of hGH results in pituitary dwarfism. b. Hypersecretion of hGH during childhood results in giantism and during
adulthood results in acromegaly.
2. A disorder associated with dysfunction of the posterior pituitary is diabetes insipidus.
Hyposecretion of ADH causes excretion of large amounts of dilute urine and subsequent dehydration and thirst.
B. Thyroid Gland Disorders 1. Hyposecretion of thyroid hormones during fetal life or infancy results in cretinism. 2. Hypothyroidism during adult years produces myxedema. 3. The most common form of hyperthyroidism is Graves disease, an autoimmune disease. 4. A goiter is an enlarged thyroid gland. C. Parathyroid Gland Disorders 1. Hypoparathyroidism results in muscle tetany. 2. Hyperparathyroidism produces osteitis fibrosa cystica. D. Adrenal Gland Disorders 1. Cushing s syndrome results from a hypersecretion of cortisol by the adrenal cortex. 2. Hyposecretion of glucocorticoids and aldosterone results in Addison s disease. 3. Pheochromocytomas, benign tumors of the adrenal medulla, cause hypersecretion of
medullary hormones and a prolonged fight-or-flight response.
E. Pancreatic Disorders 1. Diabetes Mellitus a. This is a group of disorders caused by an inability to produce or use insulin.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
b. Type I diabetes or insulin-dependent diabetes mellitus is caused by an absolute
deficiency of insulin.
c. Type II diabetes or insulin-independent diabetes is caused by a down-regulation
of insulin receptors.
2. Hyperinsulinism results when too much insulin is present and causes hypoglycemia and
possibly insulin shock. Critical Thinking Questions
1. A patient has just undergone surgery for removal of a portion of his lungs. The nurse in the recovery room
observes that the patient has internal bleeding and is losing a considerable quantity of blood. Assuming that the stressor is heavy blood loss, answer the following questions. What portion of the brain is stimulated first in response to the stressor? What signs of the alarm reaction could the nurse observe and/or measure? What are some of the body responses of the resistance reaction to the stressor? What conditions might cause the patient to reach the stage of exhaustion?
2. The results of a urinalysis show a large quantity of glucose in the urine (this was fasting urine). What
would the presence of an excessive amount of glucose in the urine indicate?
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
THE CARDIOVASCULAR SYSTEM: BLOOD
I. INTRODUCTION A. Blood inside blood vessels, interstitial fluid around body cells, and lymph inside lymph vessels
constitute one s internal environment.
B. To obtain nutrients and remove wastes, cells must be serviced by blood and interstitial fluid. 1. Blood, a connective tissue, is composed of plasma and formed elements. 2. Interstitial fluid bathes body cells. C. The branch of science concerned with the study of blood, blood-forming tissues, and the
disorders associated with them is called hematology.
II. FUNCTIONS OF BLOOD A. Blood transports oxygen, carbon dioxide, nutrients, heat, wastes, and hormones. B. It helps regulate pH, body temperature, and water content of cells. C. It prevents blood loss through clotting and combats toxins and microbes through certain
phagocytic white blood cells or specialized plasma proteins.
III. PHYSICAL CHARACTERISTICS OF BLOOD A. Physical characteristics of blood include a viscosity greater than that of water; temperature, 38oC
(100.4 ); and a pH of 7.35 to 7.45.
o
B. Blood constitutes about 8% of body weight; volume ranges from 4 to 6 liters. C. Blood samples for laboratory testing may be obtained by venipuncture, finger-stick, or arterial
stick.
IV. COMPONENTS OF BLOOD A. Blood consists of 55% plasma and 45% formed elements. B. Blood plasma consists of 91.5% water and 8.5% solutes. 1. Principal solutes include proteins (albumins, globulins, fibrinogen), nutrients, enzymes,
hormones, respiratory gases, electrolytes, and waste products.
2. Table 19.1 summarizes the chemical composition of plasma. C. Formed Elements 1. The formed elements in blood include erythrocytes (red blood cells or RBCs), leukocytes
(white blood cells or WBCs), and thrombocytes (platelets).
2. The percentage of total blood volume occupied by red blood cells is called the
hematocrit. A hematocrit measures the percentage of red blood cells in whole blood.
a. A significant drop in hematocrit indicates anemia, due to a lower than normal
number of RBCs.
b. In polycythemia the percentage of RBC is abnormally high with a higher than
normal hematocrit.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
D. There are several means for athletes to increase their hematocrit (induced polycythemia) in an
attempt to boost the oxygen-carrying capacity of their blood before an athletic event. Although evidence suggests that there may be performance benefits related to the procedure, the potential risks from higher blood viscosity are unknown and the practice is considered dishonest by the International Olympics Committee.
V. FORMATION OF BLOOD CELLS A. Blood cells are formed from pluripotent hematopoietic stem cells (Figure 19.3). 1. Originating from the pluripotent stem cells are the myeloid stem cells and lymphoid
stem cells.
a. Myeloid stem cells give rise to RBCs, platelets, and all WBCs except for
lymphocytes.
b. Lymphoid stem cells give rise to lymphocytes. 2. Myeloid stem cells differentiate into progenitor cells or precursor cells (blast cells) which
will develop into the actual formed elements of blood.
3. Lymphoid stem cells differentiate into pre-B and prothymocytes which develop into Blymphocytes and T-lymphocytes, respectively.
B. This process of hemopoiesis (or hematopoiesis) is stimulated by several hematopoietic growth
factors. These hematopoietic growth factors stimulate differentiation and proliferation of the various blood cells.
1. Erythropoietin increases the number of RBC precursors. 2. Thrombopoietin increases the number of platelet precursors. 3. Cytokins (colony-stimulating factors and interleukins) increase the number of WBC
precursors.
C. Growth factors, available through recombinant DNA technology, hold great potential for use in
patients who cannot normally form the blood cells. (Clinical Application)
VI. RED BLOOD CELLS A. Red blood cells or erythrocytes (RBCs) contain the oxygen-carrying protein hemoglobin and
number about 5.4 million cells/microliter of blood.
B. RBCs are biconcave discs without nuclei that contain hemoglobin. C. RBC Physiology 1. The function of the hemoglobin in RBCs is to transport oxygen and some carbon dioxide.
Hemoglobin molecules are specialized components of the red blood cell plasma membrane that combine with oxygen (as oxyhemoglobin) or with carbon dioxide (as carbaminohemoglobin) in this transport process.
2. Hemoglobin also functions in blood pressure regulation. a. The gaseous hormone NO binds to hemoglobin.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
b. Hemoglobin can release NO c. Released NO causes vasodilation which improves blood flow and enhances
oxygen delivery to the area.
D. RBC Life Cycle 1. Red blood cells only live about 120 days because of the wear and tear on their plasma
membranes as they squeeze through blood capillaries.
2. In the RBC life cycle, after phagocytosis of worn-out RBCs by macrophages, hemoglobin
is recycled; the globin portion is split from the heme with the amino acids being reused for protein synthesis. The iron in the heme portion is reclaimed with the rest of the heme molecule; the rest becomes a component of bile in the digestive process.
3. Under normal conditions plasma contains almost no free iron. If the amount of iron
present in the body builds up, iron overload results causing diseases of the liver, heart, pancreatic islets, and gonads. Iron overload also permits iron dependent microbes to flourish (Clinical Application).
E. Erythropoiesis: Production of RBCs 1. Erythrocyte formation, called erythropoiesis, occurs in adult red bone marrow of certain
bones.
2. The main stumulus for erythropoiesis is hypoxia. 3. A reticulocyte count (average 0.5 - 1.5% of all RBCs) is a diagnostic test that indicates the
rate of erythropoiesis and is useful in diagnosing and treating anemia. (Clinical Application)
VII. WHITE BLOOD CELLS A. Leukocytes (white blood cells or WBCs) are nucleated cells and do not contain hemoglobin. Two
principal types are granular (neutrophils, eosinophils, basophils) and agranular (lymphocytes and monocytes).
B. Granular leukocytes include eosinophils, basophils, and neutrophils based on the straining of the
granules.
C. Agranular leukocytes do not have cytoplasmic granules and include the lymphocytes and
monocytes, which differentiate into macrophages (fixed and wandering).
D. Leukocytes have surface proteins, as do erythrocytes. They are called major histocompatibility
antigens (MHC), are unique for each person (except for identical siblings), and can be used to identify a tissue.
E. Function of WBCs 1. White blood cells usually live for only a few hours or a few days. Normal blood contains
5,000-10,000 leukocytes/mm .
3
a. Leukocytosis refers to an increase in the number of WBCs.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
b. Leukopenia refers to an abnormally low number of WBCs. 2. The general function of leukocytes is to combat inflammation and infection. a. WBCs leave the blood stream by emigration (Figure 19.8). b. Some WBCs, particularly neutrophils and macrophages, are active in
phagocytosis.
c. The chemical attraction of WBCs to a disease or injury site is termed
chemotaxis.
d. Different WBCs combat inflammation and infection in different ways. 1) Neutrophils and wandering or fixed macrophages (which develop from
monocytes) do so through phagocytosis.
2) Eosinophils combat the effects of histamine in allergic reactions,
phagocytize antigen-antibody complexes, and combat parasitic worms.
3) Basophils develop into mast cells that liberate heparin, histamine, and
serotonin in allergic reactions that intensify the inflammatory response.
4) B lymphocytes, in response to the presence of foreign substances
called antigens, differentiate into tissue plasma cells that produce antibodies.
5) T lymphocytes destroy foreign invaders directly. e. A differential white blood cell count is a diagnostic test in which specific white
blood cells are enumerated. Because each type of WBC plays a different role, determining the percentage of each type in the blood assists in diagnosing the condition.
3. Bone marrow transplants may be used to treat several types of anemia, leukemia, and
numerous other blood disorders. (Clinical Application)
VIII. PLATELETS A. Thrombopoietin stimulates myeloid stem cells to produce platelets. 1. Myeloid stem cells develop into megakaryocyte-colony-forming cells that develop into
megakaryoblasts.
2. Megakaryoblasts transform into megakaryocytes which fragment. 3. Each fragment, enclosed by a piece of cell membrane, is a platelet (thrombocyte). B. Normal blood contains 250,000 to 400,000 platelets/mm3. Platelets have a life span of only 5 to 9
days; aged and dead platelets are removed by fixed macrophages in the spleen and liver.
C. Platelets help stop blood loss from damaged vessels by forming a platelet plug. Their granules
also contain chemicals that promote blood clotting.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
D. A complete blood coount (CBC) is a test that screens for anemia and various infections. It usually
includes counts of RBCs, WBCs, and platelets per L of whole blood; hematocrit and differential white blood cell count. The amount of hemoglobin in grams per ml is also determined.
IX. HEMOSTASIS A. Hemostasis refers to the stoppage of bleeding. When blood vessels are damaged or ruptured, the
hemostatic response must be quick, localized to the region of damage, and carefully controlled.
B. It involves vascular spasm, platelet plug formation, and blood coagulation (clotting). 1. In vascular spasm, the smooth muscle of a blood vessel wall contracts to stop bleeding. 2. Platelet plug formation involves the clumping of platelets around the damage to stop
the bleeding.
3. A clot is a gel consisting of a network of insoluble protein fibers (fibrin) in which formed
elements of blood are trapped.
a. The chemicals involved in clotting are known as coagulation (clotting) factors;
most are in blood plasma, some are released by platelets, and one is released from damaged tissue cells.
b. Blood clotting involves a cascade of reactions that may be divided into three
stages: formation of prothrombinase (prothrombin activator), conversion of prothrombin into thrombin, and conversion of soluble fibrinogen into insoluble fibrin.
c. The clotting cascade can be initiated by either the extrinsic pathway or the
intrinsic pathway.
C. Normal coagulation requires vitamin K and also involves clot retraction (tightening of the clot)
and fibrinolysis (dissolution of the clot).
1. The fibrinolytic system dissolves small, inappropriate clots and clots at a site of damage
once the damage is repaired.
2. Plasmin (fibrinolysin) can dissolve a clot by digesting fibrin threads and inactivating
substances such as fibrinogen, prothrombin, and factors V, VIII, and XII.
D. Homeostatic Control Mechanisms 1. Clots are generally localized due to fibrin absorbing thrombin into the clot, clotting
factors diffusing through blood, and the production of prostacyclin, a powerful inhibitor of platelet adhesion and release.
2. Substances that inhibit coagulation, called anticoagulants, are also present in blood. An
example is heparin.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
3. Patients who are at increased risk of forming blood clots may receive an anticoagulant
drug such as heparin or warfarin. To prevent clots in donated blood, a substance that removes Ca such as EDTA or CPD may be added to the blood (Clinical Application).
+2
E. Despite the anticoagulating and fibrinolytic mechanisms, blood clots sometimes form within the
cardovascular system.
1. Clotting in an unbroken blood vessel is called thrombosis. 2. A thrombus (clot), bubble of air, fat from broken bones, or piece of debris transported by
the bloodstream that moves from its site of origin is called an embolus.
3. At low doses aspirin inhibits vasoconstriction and platelet aggregation thereby reducing
the chance of thrombus formation. Thrombolytic agents are injected into the body to dissolve clots that have already formed. Streptokinase or tissue plasminogen activator (TPS) are thrombolytic agents (Clinical Application)
X. BLOOD GROUPS AND BLOOD TYPES A. The surfaces of red blood cells contain genetically determined blood group antigens, called
agglutinogens or isoantigens.
1. Blood is categorized into different blood groups based on the presence or absence of
various isoantigens.
2. Within a blood group there may be two or more different blood types. 3. Major blood groups are the ABO and Rh groups. Other blood groups include the Lewis,
Kell, Kidd, and Duffy systems.
B. ABO Group 1. In the ABO system, agglutinogens (antigens) A and B determine blood types. 2. Plasma contains agglutinins (antibodies), designated as a and b, that react with
agglutinogens that are foreign to the individual.
3. Table 19.5 indicates the incidence of ABO and Rh blood types. C. Rh Blood Group 1. In the Rh system, individuals whose erythrocytes have Rh agglutinogens are classified as
Rh+. Those who lack the antigen are Rh- .
D. A disorder due to Rh incompatibility between mother and fetus is called hemolytic disease of the
newborn; it is treatable, but also preventable (Clinical Application).
E. Transfusions 1. Knowledge of blood types is essential to safe transfusion of blood and may also be used
in proving or disproving paternity, linking suspects to crimes, or as a part of anthropology studies to establish a relationship among races.
F. Typing and Cross-Matching Blood for Transfusion
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
1. The Rh and ABO blood groups may be detected by a simple medical test, blood typing, in
which a sample of blood is mixed with serum containing agglutinins to each of the major agglutinogens (AB, B, and Rh).
2. Typing is the determination of blood types, whereas cross-matching is the mixing of
donor and recipient blood for compatibility.
XI. DISORDERS: HOMEOSTATIC IMBALANCES A. Anemia is a condition in which the oxygen-carrying capacity of the blood is reduced; it is a sign,
not a diagnosis and is usually characterized by a decreased erythrocyte count or hemoglobin deficiency. Kinds of anemia include iron-deficiency, pernicious, hemorrhagic, hemolytic, Thalassemia, and aplastic.
B. Sickle-cell disease is an inherited disorder due to an abnormal kind of hemoglobin. RBCs show a
characteristic sickle shape, rupture easily, and show a reduced oxygen carrying capacity which results in hemolytic anemia.
C. Hemophilia is an inherited deficiency of clotting in which bleeding may occur spontaneously or
after only minor trauma.
D. Disseminated intravascular clotting is a disorder of hemostasis characterized by simultaneous and
unregulated blood clotting and hemorrhage.
E. Acute leukemia is a malignant disease of blood-forming tissues characterized by uncontrolled
production and accumulation of immature leukocytes. In chronic leukemia, there is an accumulation of mature leukocytes in the bloodstream because they do not die at the end of their normal life span.
Critical Thinking Questions
1. A patient undergoing some diagnostic tests is ordered to have differential white blood cell and total blood
counts done. The results of the total blood count indicate leukocytosis; the results of the differential white blood cell count indicate 75-85% neutrophils and 15-18% monocytes. What is the significance of the leukocytosis? How would you interpret the results of the neutrophil and monocyte counts?
2. A laboratory test of a patient s blood reveals a hematocrit of 15%. Microscopic examination of the blood
also reveals several distorted and ruptured red blood cells. In addition, the reticulocyte count is 2%. Based on all of these findings, from what disorder do you think the patient is suffering?
3. Individuals with type AB blood can theoretically receive blood from individuals with types A, B, AB, and O
blood. Conversely, individuals with type O blood can theoretically give blood to individuals with type A, B, AB, and O blood. Explain why both situations are possible on the basis of the antigen-antibody response. Can you relate this response to hemolytic disease of the newborn? How is this condition treated? How can it be prevented?
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
THE CARDIOVASCULAR SYSTEM: THE HEART
I. INTRODUCTION A. The cardiovascular system consists of the blood, heart, and blood vessels. B. The heart is the pump that circulates the blood through an estimated 60,000 miles of blood vessels. C. The study of the normal heart and diseases associated with it is known as cardiology.
II. ANATOMY OF THE HEART A. Location of the heart 1. The heart is situated between the lungs in the mediastinum with about two-thirds of its mass to the left of the midline. 2. Because the heart lies between two rigid structures, the vertebral column and the sternum, external compression on the chest can be used to force blood out of the heart and into the circulation. (Clinical Application) B. Pericardium 1. The heart is enclosed and held in place by the pericardium. a. The pericardium consists of an outer fibrous pericardium and an inner serous pericardium. b. c. The serous pericardium is composed of a parietal layer and a visceral layer. Between the parietal and visceral layers of the serous pericardium is the pericardial cavity, a potential space filled with pericardial fluid that reduces friction between the two membranes. 2. An inflammation of the pericardium is known as pericarditis. Associated bleeding into the pericardial cavity compresses the heart (cardiac tamponade) and is potentially lethal (Clinical Application). C. Layers of the Heart Wall
1. The wall of the heart has three layers: epicardium, myocardium, and endocardium. 2. The epicardium consists of mesothelium and connective tissue, the myocardium is
composed of cardiac muscle, and the endocardium consists of endothelium and connective tissue. D. Chambers of the Heart
1. The chambers of the heart include two upper atria and two lower ventricles. 2. On the surface of the heart are the auricles and sulci. a. The auricles are small pouches on the anterior surface of each atrium that
slightly increase the capacity of each atrium.
b. The sulci are grooves that contain blood vessels and fat and separate the
chambers.
3. Right Atrium
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
a. The right atrium receives blood from the superior and inferior vena cava and
the coronary sinus.
b. In the septum separating the right and left atria is an oval depression, the fossa
ovalis, which is the remnant of the foramen ovale.
c. Blood passes from the right atrium into the right ventricle through the tricuspid
valve.
4. Right Ventricle a. The right ventricle forms most of the anterior surface of the heart. b. Blood passes from the right ventricle to the pulmonary trunk via the pulmonary
semilunar valve.
5. Left Atrium a. The left atrium receives blood from the pulmonary veins. b. Blood passes from the left atrium to the left ventricle through the bicuspid
(mitral) valve.
6. Left Ventricle a. The left ventricle forms the apex of the heart. b. Blood passes from the left ventricle through the aortic semilunar valve into the
aorta.
c. During fetal life the ductus arteriosus shunts blood from the pulmonary trunk
into the aorta. At birth the ductus arteriosus closes and becomes the ligamentum arteriosum. E. Myocardial Thickness and Function
1. The thickness of the myocardium of the four chambers varies according to the function
of each chamber.
2. The atria walls are thin because they deliver blood to the ventricles. 3. The ventricle walls are thicker because they pump blood greater distances. a. The right ventricle walls are thinner than the left because they pump blood into
the lungs, which are nearby and offer very little resistance to blood flow.
b. The left ventricle walls are thicker because they pump blood through the body
where the resistance to blood flow is greater. F. The fibrous skeleton of the heart forms the foundation for which the heart valves attach, serves as points of insertion for cardiac muscle bundles, prevents overstretching of the valves as blood passes through them, and acts as an electrical insulator that prevents direct spread of action potentials from the atria to the ventricles. III. HEART VALVES AND CIRCULATION OF BLOOD
A. Valves open and close in response to pressure changes as the heart contracts and relaxes.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
B. Operation of the atrioventricular valves 1. Atrioventricular (AV) valves prevent blood flow from the ventricles back into the atria. 2. Back flow is prevented by the contraction of papillary muscles tightening the chordae
tendinae which prevent the valve cusps from everting.
C. Operation of the semilunar valves 1. The semilunar (SL) valves allow ejection of blood from the heart into arteries but prevent
back flow of blood into the ventricles.
2. Semilunar valves open when pressure in the ventricles exceeds the pressure in the
arteries.
3. Certain infectious diseases, such as rheumatic fever, can damage or destroy heart valves.
(Clinical Application).
D. Systemic and Pulmonary Circulations 1. The left side of the heart is the pump for the systemic circulation. It pumps oxygenated
blood from the lungs out into the vessels of the body.
2. The right side of the heart is the pump for the pulmonary circulation. It receives
deoxygenated blood from the body and sends it to the lungs for oxygenation.
3. Figure 20.7 reviews the route of blood flow through the chambers and valves of the
heart and the pulmonary and systemic circulations.
E. Coronary Circulation 1. The flow of blood through the many vessels that pierce the myocardium of the heart is
called the coronary (cardiac) circulation; it delivers oxygenated blood and nutrients to and removes carbon dioxide and wastes from the myocardium.
2. The principal arteries, branching from the ascending aorta and carrying oxygenated
blood, are the right and left coronary arteries.
3. Deoxygenated blood returns to the right atrium primarily via the principal vein, the
coronary sinus.
4. When blockage of a coronary artery deprives the heart muscle of oxygen, reperfusion
may damage the tissue further. This damage is due to free radicals. Drugs that lessen reperfusion damage after a heart attack are being developed (Clinical Application). IV. CARDIAC MUSCLE AND THE CARDIAC CONDUCTION SYSTEM
A. Histology of Cardiac Muscle 1. Compared to skeletal muscle fibers, cardiac muscle fibers are shorter in length,
larger in diameter, and squarish rather than circular in transverse section.
2. Cardiac muscles have the same arrangement of actin and myosin, and the same
bands, zones, and Z discs as skeletal muscles.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
3. They do have less sarcoplasmic reticulum than skeletal muscles and require Ca+2
from extracellular fluid for contraction.
4. They form two separate functional networks in the heart: the atrial and the
ventricular networks.
a. Fibers within the networks are connected by intercalated discs, which
consist of desmosomes and gap junctions.
b. The intercalated discs allow the fibers in the network to work together so
that each network serves as a functional unit.
B. Autorhythmic Cells: The Conduction System 1. Cardiac muscle cells are autorhythmic cells because they are self-excitable. They
repeatedly generate spontaneous action potentials that then trigger heart contractions.
a. These cells act as a pacemaker to set the rhythm for the entire heart. b. They form the conduction system, the route for propagating action
potential through the heart muscle.
2. Components of this system are the sinoartrial (SA) node (pacemaker), atrioventricular
(AV) node, atrioventricular bundle (bundle of His), right and left bundle branches, and the conduction myofibers (Purkinje fibers)
3. Signals from the autonomic nervous system and hormones, such as epinephrine, do
modify the heartbeat (in terms of rate and strength of contraction), but they do not establish the fundamental rhythm.
4. Sometimes a site other than the SA node becomes the pacemaker because it develops
self-excitability. Such a site is called an ectopic pacemaker (Clinical Application).
C. Action potential and contraction of contractile fibers 1. An impulse in a ventricular contractile fiber is characterized by rapid depolarization,
plateau, and repolarization.
2. The refractory period of a cardiac muscle fiber (the time interval when a second
contraction cannot be triggered) is longer than the contraction itself.
D. ATP production in cardiac muscle 1. Cardiac muscle relies on aerobic cellular respiration for ATP production. 2. Cardiac muscle also produces some ATP from creatine phosphate 3. The presence of creatine kinase (CK) in the blood indicates injury of cardiac muscle
usually caused by a myocardial infarction.
E. Electrocardiogram 1. Impulse conduction through the heart generates electrical currents that can be detected
at the surface of the body. A recording of the electrical changes that accompany each cardiac cycle (heartbeat) is called an electrocardiogram (ECG or EKG).
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
a. The ECG helps to determine if the conduction pathway is abnormal, if the
heart is enlarged, and if certain regions are damaged.
2. In a typical Lead II record, three clearly visible waves accompany each heartbeat. a. A normal ECG consists of a P wave (atrial depolarization - spread of impulse
from SA node over atria), QRS complex (ventricular depolarization - spread of impulse through ventricles), and T wave (ventricular repolarization).
b. The P-Q (PR) interval represents the conduction time from the beginning of
atrial excitation to the beginning of ventricular excitation.
c. The S-T segment represents the time when ventricular contractile fibers are
fully depolarized, during the plateau phase of the impulse.
V. THE CARDIAC CYCLE
A. A cardiac cycle consists of the systole (contraction) and diastole (relaxation) of both atria, rapidly
followed by the systole and diastole of both ventricles.
B. Pressure and volume changes during the cardiac cycle 1. During a cardiac cycle atria and ventricles alternately contract and relax forcing blood
from areas of high pressure to areas of lower pressure.
2. The pahses of the cardiac cycle are: atrial systole, ventricular systole, and the relaxation
period.
C. The act of listening to sounds within the body is called auscultation, and it is usually done with a
stethoscope. The sound of a heartbeat comes primarily from the turbulence in blood flow caused by the closure of the valves, not from the contraction of the heart muscle.
1. The first heart sound (lubb) is created by blood turbulence associated with the closing of
the atrioventricular valves soon after ventricular systole begins.
2. The second heart sound (dupp) represents the closing of the semilunar valves close to
the end of the ventricular systole.
3. A heart murmur is an abnormal sound that consists of a flow noise that is heard before,
between, or after the lubb-dupp or that may mask the normal sounds entirely. Some murmurs are caused by turbulent blood flow around valves due to abnormal anatomy or increased volume of flow. Not all murmurs are abnormal or symptomatic, but most indicate a valve disorder (Clinical Application). VI. CARDIAC OUTPUT
A. Since the body s need for oxygen varies with the level of activity, the heart s ability to discharge
oxygen-carrying blood must also be variable. Body cells need specific amounts of blood each minute to maintain health and life.
B. Cardiac output (CO) is the volume of blood ejected from the left ventricle (or the right ventricle)
into the aorta (or pulmonary trunk) each minute.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
1. cardiac output equals the stroke volume, the volume of blood ejected by the ventricle
with each contraction, multiplied by the heart rate, the number of beats per minute.
2. Cardiac reserve is the ratio between the maximum cardiac output a person can achieve
and the cardiac output at rest.
C. Regulation of Stroke Volume 1. Three factors regulate stroke volume: preload, the degree of stretch in the heart before
it contracts; contractility, the forcefulness of contraction of individual ventricular muscle fibers; and afterload, the pressure that must be exceeded if ejection of blood from the ventricles is to occur.
a. Preload: Effect of Stretching 1) According to the Frank-Starling law of the heart, a greater preload
(stretch) on cardiac muscle fibers just before they contract increases their force of contraction during systole.
2) The Frank-Starling law of the heart equalizes the output of the right
and left ventricles and keeps the same volume of blood flowing to both the systemic and pulmonary circulations.
b. Myocardial contractility, the strength of contraction at any given preload, is
affected by positive and negative inotropic agents.
1) Positive inotropic agents increase contractility and negative
inotropic agents decrease contractility.
2) Thus, for a constant preload, the stroke volume increases when
positive inotropic agents are present and decreases when negative inotropic agents are present.
c. The pressure that must be overcome before a semilunar valve can open is the
afterload.
2. In congestive heart failure, blood begins to remain in the ventricles increasing the
preload and ultimately causing an overstretching of the heart and less forceful contraction (Clinical Application).
D. Regulation of Heart Rate 1. Cardiac output depends on heart rate as well as stroke volume. Changing heart rate is
the body s principal mechanism of short-term control over cardiac output and blood pressure. Several factors contribute to regulation of heart rate.
2. Autonomic regulation of the heart a. Nervous control of the cardiovascular system stems from the cardiovascular
center in the medulla oblongata.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
b. Proprioceptors, baroreceptors, and chemoreceptors monitor factors that
influence the heart rate.
c. Sympathetic impulses increase heart rate and force of contraction;
parasympathetic impulses decrease heart rate.
3. Chemical regulation of heart rate a. Heart rate affected by hormones (epinephrine, norepinephrine, thyroid
hormones).
b. Ions (Na+, K+, Ca+2) also affect heart rate. 4. Other factors such as age, gender, physical fitness, and temperature also affect heart
rate. VII. EXERCISE AND THE HEART
A. Sustained exercise increases oxygen demand in muscles. B. Among the benefits of aerobic exercise (any activity that work large body muscles for at least 20
minutes, preferably 3-5 times per week) are increased cardiac output, increased HDL and decreased triglycerides, improved lung function, decreased blood pressure, and weight control.
C. As a heart fails, a person s mobility decreases. Heart transplants may help such individuals.
Other possibilities include cardiac assist devices and surgical procedures. VIII. DEVELOPMENT OF THE HEART
A. The heart develops from mesoderm before the end of the third week of gestation. B. The endothelial tubes develop into the four-chambered heart and great vessels of the heart.
IX. DISORDERS: HOMEOSTATIC IMBALANCES
A. Coronary artery disease (CAD), or coronary heart disease (CHD), is a condition in which the heart
muscle receives an inadequate amount of blood due to obstruction of its blood supply. It is the leading cause of death in the United States each year. The principal causes of obstruction include atherosclerosis, coronary artery spasm, or a clot in a coronary artery.
1. Risk factors for development of CAD include high blood cholesterol levels, high blood
pressure, cigarette smoking, obesity, diabetes, type A personality, and sedentary lifestyle.
2. Atherosclerosis is a process in which smooth muscle cells proliferate and fatty
substances, especially cholesterol and triglycerides (neutral fats), accumulate in the walls of the medium-sized and large arteries in response to certain stimuli, such as endothelial damage.
3. Diagnosis of CAD includes such procedures as cardiac catherization and cardiac
angiography.
4. Treatment options for CAD include drugs and coronary artery bypass grafting B. Myocardial Ischemia and Infarction
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
1. Partial obstruction of blood flow in the coronary arteries may cause myocardial
ischemia.
a. Ischemia usually causes hypoxia which may weaken cells without killing them. b. Angina pectoris is a severe pain that usually, but not always, accompanies
myocardial ischemia.
2. A complete obstruction to blood flow may result in myocardial infarction (MI),
commonly called a heart attack.
a. Infarction means death of an area of tissue because of an interrupted blood
supply.
b. The resulting damage may be so extensive that death results. C. Congenital Heart Defects 1. A congenital defect is a defect that exists at birth, and usually before birth. 2. Congenital defects of the heart include coarctation of the aorta, patent ductus
arteriosus, septal defects (interatrial or interventricular), valvular stenosis, and tetralogy of Fallot.
a. Some congenital defects are not serious or remain asymptomatic; others heal
themselves.
b. A few congenital defects are life threatening and must be corrected surgically.
Fortunately, surgical techniques are highly refined for most of the defects listed.
D. Arrhythmia is an irregularity in heart rhythm resulting from a defect in the conduction system of
the heart.
E. Congestive heart failure is a chronic or acute state that results when the heart is not capable of
supplying the oxygen demands of the body. Critical Thinking Questions
1. The results of a routine physical examination of a young adult male indicate the following: systolic blood
pressure = 120 mm Hg, diastolic pressure = 80 mm Hg, and pulse rate = 75 pulsations per minute. What is the clinical meaning of systolic pressure, diastolic pressure, and pulse? Are these values within normal limits?
2. Impulse transmission through the conduction system of the heart generates electrical charges that may be
detected on the surface of the body. What is a recording of these charges called? What is a deflection wave? What is the significance of each of the following: P wave, P-R interval, QRS wave, S-T segment, and T wave?
3. A 55-year-old male is admitted into the hospital complaining of chest pains. His ECG shows an enlarged Q
wave. What would be the initial diagnosis for the patient? What tests might be run to confirm the diagnosis?
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
THE CARDIOVASCULAR SYSTEM: BLOOD VESSELS AND HEMODYNAMICS
I. INTRODUCTION A. One main focus of this chapter considers hemodynamics, the means by which blood flow is altered and distributed and by which blood pressure is regulated. B. The histology of blood vessels and anatomy of the primary routes of arterial and venous systems are surveyed. II. STRUCTURE AND FUNCTION OF BLOOD VESSELS
A. Blood vessels form a closed system of tubes that carry blood away from the heart, transport it to
the tissues of the body, and then return it to the heart.
1. Arteries carry blood from the heart to the tissues. 2. Arterioles are small arteries that connect to capillaries. 3. Capillaries are the site of substance exchange between the blood and body tissues. 4. Venules connect capillaries to larger veins. 5. Veins convey blood from the tissues back to the heart. 6. Vasa vasorum are small blood vessels that supply blood to the cells of the walls of the
arteries and veins. B. Arteries
1. Arteries carry blood away from the heart to the tissues. a. The wall of an artery consists of a tunica interna, tunica media (which maintains
elasticity and contractility), and a tunic externa.
b. The functional properties of arteries are elasticity and contractility. 1) Elasticity, due to the elastic tissue in the tunica internal and media,
allows arteries to accept blood under great pressure from the contraction of the ventricles and to send it on through the system.
2) Contractility, due to the smooth muscle in the tunica media, allows
arteries to increase or decrease lumen size and to limit bleeding from wounds.
2. Elastic Arteries a. Large arteries with more elastic fibers and less smooth muscle are called elastic
arteries and are able to receive blood under pressure and propel it onward.
b. They are also called conducting arteries because they conduct blood from the
heart to medium sized muscular arteries.
c. They function as a pressure reservoir. 3. Muscular arteries have a large amount of smooth muscle in their walls and distribute
blood to various parts of the body.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
C. Arterioles 1. Arterioles are very small, almost microscopic, arteries that deliver blood to capillaries. 2. Through vasoconstriction (decrease in the size of the lumen of a blood vessel) and
vasodilation (increase in the size of the lumen of a blood vessel), arterioles assume a key role in regulating blood flow from arteries into capillaries and in altering arterial blood pressure.
D. Capillaries are microscopic vessels that usually connect arterioles and venules. 1. The flow of blood through the capillaries is called the microcirculation. 2. Capillaries are found near almost every cell in the body, but their distribution varies with
the metabolic activity of the tissue.
3. The primary function of capillaries is to permit the exchange of nutrients and wastes
between the blood and tissue cells through interstitial fluid.
4. Capillary walls are composed of only a single layer of cells (endothelium) and a
basement membrane.
5. Capillaries branch to form an extensive capillary network throughout the tissue. This
network increases the surface area, allowing a rapid exchange of large quantities of materials.
a. The flow of blood through capillaries is regulated by vessels with smooth
muscle in their walls.
b. Rings of smooth muscle fibers (cells) called precapillary sphincters regulate
blood flow through true capillaries.
c. There are three types of capillaries: continuous, fenestrated, and sinusoids. E. Venules 1. Venules are small vessels that are formed from the union of several capillaries; venules
merge to form veins.
2. They drain blood from capillaries into veins. F. Veins 1. Veins consist of the same three tunics as arteries but have a thinner tunica interna and
media and a thicker tunica externa; they have less elastic tissue and smooth muscle and are therefore thinner-walled than arteries. They contain valves to prevent the backflow of blood.
2. Vascular (venous) sinuses are veins with very thin walls with no smooth muscle to alter
their diameters. Examples are the brain s superior sagittal sinus and the coronary sinus of the heart.
3. Weak valves can lead to varicose veins. (Clinical Application)
G. Anastomoses
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
1. Anastomoses are the union of the branches of two or more arteries supplying the same
region.
2. They provide alternate routes for blood to reach a tissue or organ. 3. The collateral circulation is the alternate flow of blood to a body part through an
anastomosis.
4. Arteries that do not anastomose are know as end arteries. Occlusion of an end artery
interrupts the blood supply to a whole segment of an organ, producing necrosis (death) of that segment.
5. Anastomoses can also consist of two veins or a vein and an artery. H. Blood Distribution 1. At rest, the largest portion of the blood is in systemic veins and venules, collectively
called blood reservoirs.
a. They store blood and, through venous vasoconstriction, can move blood to
other parts of the body if the need arises.
b. In cases of hemorrhage, when blood pressure and volume decrease,
vasoconstriction of veins in venous reservoirs helps to compensate for the blood loss.
2. The principal reservoirs are the veins of the abdominal organs (liver and spleen) and
skin. III. CAPILLARY EXCHANGE A. Substances enter and leave capillaries by diffusion, transcytosis, and bulk flow (filtration and absorption). B. The most important method of capillary exchange is simple diffusion. 1. Substances such as O2, CO2, glucose, amino acids, hormones, and others diffuse down their concentration gradients. 2. 3. All plasma solutes, except larger proteins, pass freely across most capillary walls. The prime exception of diffusion of water-soluble materials across capillary walls is in the brain where the blood-brain barrier exists. C. Some materials cross the capillary membrane by transcytosis, the enclosing of substances within tiny vesicles that enter cells by endocytosis. D. Bulk Flow: Filtration and Reabsorption
1. Whereas diffusion is more important for solute exchange between plasma and
interstitial fluid, bulk flow is more important for regulation of the relative volumes of blood and interstitial fluid.
2. The movement of water and dissolved substances (except proteins) through capillaries is
dependent upon hydrostatic and osmotic pressures.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
3. The near equilibrium at the arterial and venous ends of a capillary by which fluids exit
and enter is called Starling s law of the capillaries.
4. Occasionally, the balance of filtration and reabsorption between interstitial fluid and
plasma is disrupted, allowing an abnormal increase in interstitial fluid called edema. Edema may be caused by several factors including increased blood hydrostatic pressure in capillaries due to an increase in venous pressure, decreased concentration of plasma proteins that lower blood colloid osmotic pressure, increased permeability of capillaries which allows greater amounts of plasma proteins to leave the blood and enter tissue fluid, increased extracellular fluid volume as a result of fluid retention, and blockage of lymphatic vessels postoperatively or due to filarial worm infection (Clinical Application).
IV. HEMODAYNAMICS: FACTORS AFFECTING BLOOD FLOW
A. The distribution of cardiac output to various tissues depends on the interplay of the pressure
difference that drives the blood flow and the resistance to blood flow.
B. Blood pressure (BP) is the pressure exerted on the walls of a blood vessel; in clinical use, BP
refers to pressure in arteries.
1. Cardiac output (CO) equals mean aortic blood pressure (MABP) divided by total
resistance (R).
2. Factors that affect blood pressure include cardiac output, blood volume, viscosity,
resistance, and elasticity of arteries.
3. As blood leaves the aorta and flows through systemic circulation, its pressure
progressively falls to 0 mm Hg by the time it reaches the right atrium.
C. Resistance refers to the opposition to blood flow as a result of friction between blood and the
walls of the blood vessels.
1. Vascular resistance depends on the diameter of the blood vessel, blood viscosity, and
total blood vessel length.
2. Systemic vascular resistance (also known as total peripheral resistance) refers to all of
the vascular resistances offered by systemic blood vessels; most resistance is in arterioles, capillaries, and venules due to their small diameters.
D. Venous Return 1. Venous return occurs because of the pressure gradient between the venules and the
right atrium.
2. Blood return to the heart is maintained by several factors, including skeletal muscular
contractions, valves in veins (especially in the extremities) and pressure changes associated with breathing.
E. Velocity of Blood Flow 1. The volume that flows through any tissue in a given period of time is blood flow.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
2. The velocity of blood flow is inversely related to the cross-sectional area of blood
vessels; blood flows most slowly where cross-sectional area is greatest.
3. Blood flow decreases from the aorta to arteries to capillaries and increases as it returns
to the heart.
F. Syncope, or fainting, refers to a sudden, temporary loss of consciousness followed by
spontaneous recovery. It is most commonly due to cerebral ischemia but it may occur for several other reasons (Clinical Application) V. CONTROL OF BLOOD PRESSURE AND BLOOD FLOW
A. Role of the Cardiovascular Center 1. The cardiovascular center (CV) is a group of neurons in the medulla that regulates heart
rate, contractility, and blood vessel diameter.
2. The CV receives input from higher brain regions and sensory receptors (baroreceptors
and chemoreceptors).
3. Output from the CV flows along sympathetic and parasympathetic fibers. a. Sympathetic impulses along cardioaccelerator nerves increase heart rate and
contractility.
b. Parasympathetic impulses along vagus nerves decrease heart rate. c. The sympathetic division also continually sends impulses to smooth muscle in
blood vessel walls via vasomotor nerves. The result is a moderate state of tonic contraction or vasoconstriction, called vasomotor tone.
B. Neural Regulation of Blood Pressure 1. Baroreceptors are important pressure-sensitive sensory neurons that monitor stretching
of the walls of blood vessels and the atria.
a. The cardiac sinus reflex is concerned with maintaining normal blood pressure in
the brain and is initiated by baroreceptors in the wall of the carotid sinus.
b. The aortic reflex is concerned with general systemic blood pressure and is
initiated by baroreceptors in the wall of the arch of the aorta or attached to the arch.
c. If blood pressure falls, the baroreceptor reflexes accelerate heart rate, increase
force of contraction, and promote vasoconstriction.
d. Carotid sinus massage can slow heart rate in paroxysmal superventricular
tachycardia. (Clinical Application)
2. Receptors sensitive to chemicals are called chemoreceptors. a. These receptors are located close to the baroreceptors of the carotid sinus and
arch of the aorta.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
b. They monitor blood levels of oxygen, carbon dioxide, and hydrogen ion
concentration.
C. Hormonal Regulation 1. Hormones such as angiotensin II, epinephrine, norepinephrine, antidiuretic hormone,
and atrial natriuretic peptide affect blood pressure and blood flow by altering cardiac output, changing systemic vascular resistance, or adjusting the total blood volume.
D. Autoregulation of Blood Pressure 1. The ability of a tissue to automatically adjust its own blood flow to match its metabolic
demand for supply of O2 and nutrients and removal of wastes is called autoregulation.
2. In most body tissues, oxygen is the principal, though not direct, stimulus for
autoregulation.
3. Researchers have identified two general types of stimuli that cause autoregulatory
changes in blood flow: physical and chemical. VI. CHECKING CIRCULATION
A. Pulse 1. Pulse is the alternate expansion and elastic recoil of an artery wall with each heartbeat.
It may be felt in any artery that lies near the surface or over a hard tissue and is strongest in the arteries closest to the heart; the radial artery is most commonly used to feel the pulse depicts the most common pulse points.
2. A normal resting pulse (heart) rate is between 70 to 80 beats per minute. a. Tachycardia means a rapid resting heart or pulse rate (> 100 beats/min). b. Bradycardia indicates a slow resting heart or pulse rate (< 60 beats/min). B. Measurement of Blood Pressure 1. Blood pressure is the pressure exerted by blood on the wall of an artery when the left
ventricle undergoes systole and then diastole. It is measured by the use of a sphygmomanometer, usually in one of the brachial arteries.
a. Systolic blood pressure is the force of blood recorded during ventricular
contraction.
b. Diastolic blood pressure is the force of blood recorded during ventricular
relaxation.
c. The various sounds that are heard while taking blood pressure are called
Korotkoff sounds.
d. The normal blood pressure of a young adult male is 120/80 mm Hg (8-10 mm
Hg less in a young adult female). The range of average values varies with many factors.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
2. Pulse pressure is the difference between systolic and diastolic pressure. It normally is
about 40 mm Hg and provides information about the condition of the arteries. VII. SHOCK AND HOMEOSTASIS
A. Shock is an inadequate cardiac output that results in failure of the cardiovascular system to
deliver adequate amounts of oxygen and nutrients to meet the metabolic needs of body cells. As a result, cellular membranes dysfunction, cellular metabolism is abnormal, and cellular death may eventually occur without proper treatment.
B. Types of Shock 1. Hypovolemic shock is due to decreased blood volume. 2. Cardiogenic shock is due to poor heart function. 3. Vascular shock is due to inappropriate vasodilation. 4. Obstructive shock is due to obstruction of blood flow. C. Homeostatic responses to shock include activation of the renin-angiotensin-aldosterone system,
secretion of ADH, activation of the sympathetic division of the ANS, and release of local vasodilators.
D. Signs and symptoms of shock include clammy, cool, pale skin; tachycardia; weak, rapid pulse;
sweating; hypotension (systemic pressure < 90 mm HG); altered mental status; decreased urinary output; thirst; and acidosis. VIII. CIRCULATORY ROUTES
A. Introduction 1. The blood vessels are organized into routes that deliver blood throughout the body. 2. The largest circulatory route is the systemic circulation. 3. Other routes include pulmonary circulation (Figure 21.30) and fetal circulation. B. Systemic Circulation 1. The systemic circulation takes oxygenated blood from the left ventricle through the
aorta to all parts of the body, including some lung tissue (but does not supply the air sacs of the lungs) and returns the deoxygenated blood to the right atrium.
a. The aorta is divided into the ascending aorta, arch of the aorta, and the
descending aorta.
b. Each section gives off arteries that branch to supply the whole body. 2. Blood returns to the heart through the systemic veins. All the veins of the systemic
circulation flow into the superior or inferior venae caveae or the coronary sinus, which in turn empty into the right atrium.
3. Blood vessels are organized in the exhibits according to regions of the body. C. Hepatic Portal Circulation
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
1. The hepatic portal circulation collects blood from the veins of the pancreas, spleen,
stomach, intestines, and gallbladder and directs it into the hepatic portal vein of the liver before it returns to the heart.
2. A portal system carries blood between two capillary networks, in this case from
capillaries of the gastrointestinal tract to sinusoids of the liver.
3. This circulation enables nutrient utilization and blood detoxification by the liver. D. Pulmonary Circulation 1. The pulmonary circulation takes deoxygenated blood from the right ventricle to the air
sacs of the lungs and returns oxygenated blood from the lungs to the left atrium.
2. The pulmonary and systemic circulations differ from each other in several more ways. a. Blood in the pulmonary circulation is not pumped so far as in the systemic
circulation and the pulmonary arteries have a larger diameter, thinner walls, and less elastic tissue. As a result, resistance to blood flow is very low meaning that less pressure is needed to move blood through the lungs.
b. Because resistance in the pulmonary circulation is low, normal pulmonary
capillary hydrostatic pressure is lower than systemic capillary hydrostatic pressure which tends to prevent pulmonary edema.
E. Fetal Circulation 1. The fetal circulation involves the exchange of materials between fetus and mother. 2. The fetus derives its oxygen and nutrients and eliminates its carbon dioxide and wastes
through the maternal blood supply by means of a structure called the placenta.
3. Blood passes from the fetus to the placenta via two umbilical arteries and returns from
the placenta via a single umbilical vein.
4. At birth, when pulmonary, digestive, and liver functions are established, the special
structures of fetal circulation are no longer needed.
a. The ductus arteriosus becomes the ligamentum arteriosum shortly after birth. b. The foramen ovale becomes the fossa ovalis shortly after birth. c. The ductus venosus becomes the ligamentum venosum shortly after birth. d. The umbilical arteries become the medial umbilical ligaments. e. The umbilical vein becomes the ligamentum teres (round ligament). IX. DEVELOPMENT OF BLOOD VESSELS AND BLOOD A. Blood vessels develop from isolated masses of mesenchyme in the mesoderm called blood
islands.
1. Spaces soon appear in the islands and become the lumens of the blood vessels.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
2. Some of the mesenchymal cells immediately around the spaces give rise to the
endothelial lining of the blood vessels.
B. Blood plasma and blood cells are produced by the endothelial cells of blood vessels, a function
later assumed by the liver, spleen, bone marrow, and lymph nodes.
X. AGING AND THE CARDIOVASCULAR SYSTEM A. General changes associated with aging and the cardiovascular system include loss of compliance
(extensibility) of the aorta, reduction in cardiac muscle fiber size, progressive loss of cardiac muscular strength, reduced cardiac output, a decline in maximum heart rate, and increased systolic blood pressure.
B. The incidence of coronary artery disease, congestive heart failure, and arteriosclerosis increases
with age.
XI. FOCUS ON HOMEOSTASIS: THE CARDIOVASCULAR Discusses the role of the cardiovascular system in
maintaining homeostasis.
XII. DISORDERS: HOMEOSTATIC IMBALANCES A. Hypertension, or persistently high blood pressure, is defined as systolic blood pressure of 140 mm
Hg or greater and diastolic blood pressure of 90 mm Hg or greater.
1. Primary hypertension (approximately 90-95% of all hypertension cases) is a persistently
elevated blood pressure that cannot be attributed to any particular organic cause.
2. Secondary hypertension (the remaining 5-10% of cases) has a identifiable underlying
cause such as obstruction of renal blood flow or disorders that damage renal tissue, hypersecretion of aldosterone, or hypersecretion of epinephrine and norepinephrine by pheochromocytoma, a tumor of the adrenal gland.
B. High blood pressure can cause considerable damage to the blood vessels, heart, brain, and
kidneys before it causes pain or other noticeable symptoms.
C. Lifestyle changes that can reduce elevated blood pressure include losing weight, limiting alcohol
intake, exercising, reducing sodium intake, maintaining recommended dietary intake of potassium, calcium, and magnesium, not smoking, and managing stress.
D. Various drugs including diuretics, beta blockers, vasodilators, and calcium channel blockers have
been used to successfully treat hypertension.
Critical Thinking Questions
1. Start with the right ventricle and trace a drop of blood through the lungs and back to the left atrium,
naming all of the parts of the heart and names of the blood vessels through which blood passes. What is the name and purpose of this circulatory route?
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
2. Assume a large embolus lodges in the left common iliac artery. List at least five other arteries that would
have a reduced blood supply because of the embolus. Also list at least five parts of the body that would have a reduced blood supply because of the embolus.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
THE LYMPHATIC and IMMUNE SYSTEM and RESISTANCE to DISEASE
I.
INTRODUCTION
A. The ability to ward off the pathogens that produce disease is called resistance. B. Lack of resistance is called susceptibility. C. Resistance to disease can be grouped into two broad areas. 1. Nonspecific resistance to disease includes defense mechanisms that provide general
protection against invasion by a wide range of pathogens.
2. Immunity involves activation of specific lymphocytes that combat a particular pathogen
or other foreign substance.
D. The body system that carries out immune responses is the lymphatic system. II. LYMPHATIC AND IMMUNE SYSTEM A. The lymphatic system consists of a fluid called lymph flowing within lymphatic vessels, several
structures and organs that contain lymphatic tissue (specialized reticular tissue containing large numbers of lymphocytes), and bone marrow, which is the site of lymphocyte production
1. Interstitial fluid and lymph are basically the same. 2. Their major difference is location. B. The lymphatic system functions to drain interstitial fluid, return leaked plasma proteins to the
blood, transport dietary fats, and protect against invasion by nonspecific defenses and specific immune responses.
C. Lymphatic Vessels and Lymph Circulation 1. Lymphatic vessels begin as blind-ended lymph capillaries in tissue spaces between cells a. Interstitial fluid drains into lymphatic capillaries, thus forming lymph. b. Lymph capillaries merge to form larger vessels, called lymphatic vessels, which
convey lymph into and out of structures called lymph nodes
2. Lymphatic Capillaries a. Lymphatic capillaries are found throughout the body except in avascular tissue,
the CNS, portions of the spleen, and red bone marrow.
b. Lymphatic capillaries have a slightly larger diameter than blood capillaries and
have overlapping endothelial cells which work as one-way valves for fluid to enter the lymphatic capillary.
c. Anchoring filaments attach endothelial cells to surround tissue d. A lymphatic capillary in the villus of the small intestine is the lacteal. It functions
to transport digested fats from the small intestine into blood.
3. Lymph Trunk and Ducts
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
a. The principal lymph trunks, formed from the exiting vessels of lymph nodes, are
the lumbar, intestinal, bronchomediastinal, subclavian, and jugular trunks
b. The thoracic duct begins as a dilation called the cisterna chyli and is the main
collecting duct of the lymphatic system.
1) The thoracic duct receives lymph from the left side of the head, neck,
and chest, the left upper extremity, and the entire body below the ribs.
2) It drains lymph into venous blood via the left subclavian vein. c. Right Lymphatic Duct 1) The right lymphatic duct drains lymph from the upper right side of the
body.
2) It drains lymph into venous blood via the right subclavian vein. 4. Formation and Flow of Lymph a. Interstitial fluid drains into lymph capillaries. b. The passage of lymph is from arteries and blood capillaries (blood) to interstitial
spaces (interstitial fluid) to lymph capillaries (lymph) to lymphatic vessels to lymph trunks to the thoracic duct or right lymphatic duct to the subclavian veins (blood)
1) Lymph flows as a result of the milking action of skeletal muscle
contractions and respiratory movements.
2) It is also aided by lymphatic vessel valves that prevent backflow of
lymph.
5. An excessive accumulation of interstitial fluid may be caused by an obstruction to lymph
flow (Clinical Application).
D. Lymphatic Organs and Tissues 1. Introduction a. The primary lymphatic organs are the red bone marrow and the thymus gland
that produces B and T cells.
b. The secondary lymphatic organs are the lymph nodes and spleen. c. Included as secondary lymphatic organs are the lymphatic nodules which are
clusters of lymphocytes that stand guard in all mucous membranes.
d. Most immune responses occur in secondary lymphatic organs. 2. Thymus Gland a. The thymus gland lies between the sternum and the heart and functions in
immunity as the site of T cell maturation.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
b. The thymus gland is large in the infant and after puberty is replaced by adipose
and areolar connective tissue.
3. Lymph Nodes a. Lymph nodes are encapsulated oval structures located along lymphatic vessels. b. They contain T cells, macrophages, follicular dendritic cells, and B cells. c. Lymph enters nodes through afferent lymphatic vessels, is filtered to remove
damaged cells and microorganisms, and exits through efferent lymphatic vessels.
1) Foreign substances filtered by the lymph nodes are trapped by nodal
reticular fibers.
2) Macrophages then destroy some foreign substances by phagocytosis
and lymphocytes bring about the destruction of others by immune responses.
d. Lymph nodes are the site of proliferation of plasma cells and T cells. e. Knowledge of the location of the lymph nodes and the direction of lymph flow
is important in the diagnosis and prognosis of the spread of cancer by metastasis; many cancer cells are spread by way of the lymphatic system, producing clusters of tumor cells where they lodge. (Clinical Application)
4. Spleen a. The spleen is the largest mass of lymphatic tissue in the body and is found in
the left hypochondriac region between the fundus of the stomach and the diaphragm.
b. The spleen consists of white and red pulp. 1) The white pulp is lymphatic tissue. a) Its T lymphocytes directly attack and destroy antigens in
blood.
b) Its B lymphocytes develop into antibody producing plasma
cells, and the antibodies inactivate antigens in blood.
c) Macrophages destroy antigens in blood by phagocytosis. 2) The red pulp consists of venous sinuses filled with blood and splenic
cords consisting of RBCs, macrophages, lymphocytes, plasma cells, and granulocytes.
a) Macrophages remove worn-out or defective RBCs, WBCs, and
platelets.
b) The spleen stores blood platelets in the red pulp.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
c) The red pulp is involved in the production of blood cells
during the second trimester of pregnancy.
3) The spleen is often damaged in abdominal trauma. A splenectomy
may be required to prevent excessive bleeding (Clinical Application).
5. Lymphatic Nodules a. Lymphatic nodules are oval-shaped concentrations of lymphatic tissue. 1) They are scattered throughout the lamina propria of mucous
membranes lining the GI tract, respiratory airways, urinary tract, and reproductive tract.
2) This is the mucosa-associated lymphatic tissue (MALT). b. Peyer s patches are lymphatic nodules in the ileum of the small intestine. c. Tonsils are multiple aggregations of large lymphatic nodules embedded in a
mucous membrane at the junction of the oral cavity and the pharynx.
1) They include the pharyngeal (adenoid), palatine, and lingual tonsils. 2) They are situated strategically to protect against invasion of foreign
substances and participate in immune responses by producing lymphocytes and antibodies.
III. DEVELOPMENT OF THE LYMPH TISSUES A. Lymphatic vessels develop from lymph sacs, which develop from veins. Thus, they are derived
from mesoderm.
B. Lymph nodes develop from lymph sacs that become invaded by mesenchymal cells. IV. NONSPECIFIC RESISTANCE: INNATE DEFENSES A. First Line of Defense: Skin and Mucous Membranes 1. Nonspecific resistance refers to a wide variety of body responses against a wide range of
pathogens (disease producing organisms) and their toxins.
2. Mechanical protection includes the intact epidermis layer of the skin, mucous
membranes, the lacrimal apparatus, saliva, mucus, cilia, the epiglottis, and the flow of urine. Defecation and vomiting also may be considered mechanical processes that expel microbes.
3. Chemical protection is localized on the skin, in loose connective tissue, stomach, and
vagina.
a. The skin produces sebum, which has a low pH due to the presence of
unsaturated fatty acids and lactic acid.
b. Lysozyme is an enzyme component of sweat that also has antimicrobial
properties.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
c. Gastric juice renders the stomach nearly sterile because its low pH (1.5-3.0) kills
many bacteria and destroys most of their toxins; vaginal secretions also are slightly acidic.
B. Second Line of Defense: Internal Defenses 1. The second line of defense involves internal antimicrobial proteins, phagocytic and
natural killer cells, inflammation, and fever.
2. Antimicrobial Proteins a. Body cells infected with viruses produce proteins called interferons (IFNs). Once
produced and released from virus-infected cells, IFN diffuses to uninfected neighboring cells and binds to surface receptors, inducing uninfected cells to synthesize antiviral proteins that interfere with or inhibit viral replication. INFs also enhance the activity of phagocytes and natural killer (NK) cells, inhibit cell growth, and suppress tumor formation; they may hold promise as clinical tools in AIDS and cancer treatment once they are more fully understood.
b. A group of about 20 proteins present in blood plasma and on cell membranes
comprises the complement system; when activated, these proteins complement or enhance certain immune, allergic, and inflammatory reactions.
3. Natural Killer Cells and Phagocytes a. Natural killer (NK) cells are lymphocytes that lack the membrane molecules that
identify T and B cells.
1) They have the ability to kill a wide variety of infectious microbes plus
certain spontaneously arising tumor cells.
2) NK cells sometimes release perforins that insert into the plasma
membrane of a microbe and make the membrane leaky so that cytolysis occurs or bind to a target cell and inflict damage by direct contact.
b. Phagocytes are cells specialized to perform phagocytosis and include
neutrophils and macrophages.
1) The three phases of phagocytosis include chemotaxis, adherence, and
ingestion.
2) After phagocytosis has been accomplished, a phagolysosome is
formed and the lysosome in the phagolysosome, along with lethal oxidants produced by the phagocyte, quickly kills many types of microbes.
c. Some of the reasons why a microbe may evade phagocytosis include: capsule
formation, toxin production, interference with lysozyme secretion, and the
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
microbe s ability to counter oxidants produced by the phagocytes (Clinical Application).
4. Inflammation a. Inflammation occurs when cells are damaged by microbes, physical agents, or
chemical agents. The injury may be viewed as a form of stress.
1) Inflammation is usually characterized by four symptoms: redness, pain,
heat, and swelling. Loss of function may be a fifth symptom, depending on the site and extent of the injury.
2) The three basic stages of inflammation are vasodilation and increased
permeability of blood vessels, phagocyte migration, and tissue repair.
3) Substances that contribute to inflammation are histamines, kinins,
prostaglandins, leukotrienes, and complement.
b. After phagocytes engulf damaged tissue and microbes, they eventually die,
forming a pocket of dead phagocytes and damaged tissue and fluid called pus. Pus must drain out of the body or it accumulates in a confined space, causing an abscess. (Clinical Application)
5. Fever is usually caused by infection from bacteria (and their toxins) and viruses. The high
body temperature inhibits some microbial growth and speeds up body reactions that aid repair. V. SPECIFIC RESISTANCE: IMMUNITY
A. Immunity is the ability of the body to defend itself against specific invading agents.
1. Antigens are substances recognized as foreign by the immune responses. 2. The distinguishing properties of immunity are specificity and memory. 3. The branch of science that deals with the responses of the body when challenged by
antigens is called immunology. B. Maturation of T Cells and B Cells
1. Both T cells and B cells derive from stem cells in bone marrow. a. B cells complete their development in bone marrow. b. T cells develop from pre-T cells that migrate to the thymus. 2. Before T cells leave the thymus or B cells leave bone marrow, they acquire several
distinctive surface proteins; some function as antigen receptors, molecules capable of recognizing specific antigens. C. Types of Immune Response
1. Cell-mediated immunity (CMI) refers to destruction of antigens by T cells. It is
particularly effective against intracellular pathogens, such as fungi, parasites, and viruses; some cancer cells; and foreign tissue transplants. CMI always involves cells attacking cells.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
2. Antibody-mediated (humoral) immunity (AMI) refers to destruction of antigens by
antibodies. It works mainly against antigens dissolved in body fluids and extracellular pathogens, primarily bacteria, that multiply in body fluids but rarely enter body cells.
3. Often a pathogen provokes both types of immune response.
D. Antigens and Antigen Receptors
1. Antigens are chemical substances that are recognized as foreign by antigen receptors
when introduced into the body. Antigens are both immunogenic and reactive. An antigen that gets past the nonspecific defenses can get into lymphatic tissue by entering an injured blood vessel and being carried to the spleen, penetrating the skin and entering lymph vessels leading to lymph nodes, or penetrating mucous membranes and lodging in mucosa-associated lymphoid tissue.
2. Antigens are large, complex molecules. They are most often proteins, but sometimes are
nucleoproteins, lipoproteins, glycoproteins, and certain large polysaccharides.
3. Specific portions of antigen molecules, called antigenic determinants, or epitopes, trigger
immune responses.
4. Antigen receptors exhibit great diversity due to genetic recombination. 5. Major histocompatibility complex (MHC) antigens (also called human leucocyte
associated, or HLA, antigens) are unique to each person s body cells. These self-antigens aid in the detection of foreign invaders. All cells except red blood cells display MHC class I antigens. Some cells also display MHC class II antigens.
6. The success of a proposed organ or tissue transplant depends on histocompatibility.
Tissue typing (histocompatibility testing) is done before any organ transplant. (Clinical Application)
E. Pathways of Antigen Processing 1. For an immune response to occur, B and T cells must recognize that a foreign antigen is
present.
a. B cells can recognize and bind to antigens in extracellular fluid. b. T cells, however, can only recognize fragments of antigenic proteins that first
have been processed and presented in association with MHC self-antigens.
c. Peptide fragments from foreign antigens help stimulate MHC molecules. 2. Processing of Exogenous Antigens a. Cells called antigen-presenting cells (APCs) process exogenous antigens
(antigens formed outside the body) and present them together with MHC class II molecules to T cells.
b. APCs include macrophages, B cells, and dendritic cells.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
c. Steps in processing and presenting an exogenous antigen by an APC include
ingestion of the antigen, digestion of antigen into peptide fragments, fusion of vesicles, binding of peptide fragments to MHC-II molecules, and insertion of antigen-MHC-II complex into the plasma membrane.
3. Most cells of the body can process and present endogenous antigens, antigens that were
synthesized in a body cell (e.g., viral proteins from virus-infected cells).
F. Cytokines 1. Cytokines are small protein hormones needed for many normal cell functions. 2. Some cytokines have been used to treat certain types of cancer. (Clinical Application) VI. CELL-MEDIATED IMMUNITY A. In a cell-mediated immune response, an antigen is recognized (bound), a small number of specific
T cells proliferate and differentiate into a clone of effector cells (a population of identical cells that can recognize the same antigen and carry out some aspect of the immune attack), and the antigen (intruder) is eliminated.
B. Activation, Proliferation, and Differentiation of T Cells 1. T cell receptors recognize antigen fragments associated with MHC molecules on the
surface of a body cell.
2. Proliferation of T cells requires costimulation, by cytokines such as interleukin-1 (IL-1)
and interleukin-2 (IL-2), or by pairs of plasma membrane molecules, one on the surface of the T cell and a second on the surface of an APC.
C. Types of T Cells 1. Helper T (TH) cells, or T4 cells, display CD4 protein, recognize antigen fragments
associated with MHC-II molecules, and secrete several cytokines, most important, interleukin-2, which acts as a costimulator for other helper T cells, cytotoxic T cells, and B cells.
2. Cytotoxic T (TC) cells, or T8 cells, develop from T cells that display CD8 protein and
recognize antigen fragments associated with MHC-I molecules.
3. Memory T cells are programmed to recognize the original invading antigen, allowing
initiation of a much swifter reaction should the pathogen invade the body at a later date.
4. Cytotoxic T cells fight foreign invaders by killing the target cell (the cell that bears the
same antigen that stimulated activation or proliferation of their progenitor cells) without damaging the cytotoxic T cell itself.
1) One killing mechanism uses perforin to cause cytolysis of the target cell. 2) The second mechanism uses lymphotoxin to activate damaging enzymes
within the target cell.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
D. Immunological Surveillance 1. Immunological surveillance is carried out by cytotoxic T cells. 2. They recognize tumor antigens and destroy the tumor cell. 3. The immune system can recognize proteins in transplanted organs as foreign and
mount a graft rejection. (Clinical Application)
VI. ANTIBODY-MEDIATED IMMUNITY A. The body contains not only millions of different T cells but also millions of different B cells, each
capable of responding to a specific antigen.
B. Activation, Proliferation, and Differentiation of B Cells 1. During activation of a B cell, an antigen binds to antigen receptors on the cell surface. a. B cell antigen receptors are chemically similar to the antibodies that will
eventually be secreted by their progeny.
b. Some antigen is taken into the B cell, broken down into peptide fragments and
combined with the MHC-II self-antigen, and moved to the B cell surface.
2. Helper T cells recognize the antigen-MHC-II combination and deliver the costimulation
needed for B cell proliferation and differentiation.
3. Some activated B cells become antibody-secretion plasma cells. Others become memory
B cells.
B. Antibodies 1. An antibody is a protein that can combine specifically with the antigenic determinant on
the antigen that triggered its production.
2. Antibody Structure a. Antibodies consist of heavy and light chains and variable and constant portions. b. Based on chemistry and structure, antibodies are grouped into five principal
classes each with specific biological roles (IgG, IgA, IgM, IgD, and IgE).
3. The functions of antibodies include neutralizing antigen, immobilization of bacteria,
agglutination and precipitation of antigen, activation of complement, enhancing phagocytosis, and providing fetal and newborn immunity.
4. Monoclonal antibodies are pure antibodies produced by fusing a B cell with a tumor cell
that is capable of proliferating endlessly. The resulting cell is called a hybridoma. Monoclonal antibodies are important in measuring levels of a drug in a patient s blood and in the diagnosis of pregnancy, allergies, and diseases such as hepatitis, rabies, and some sexually transmitted diseases. They have also been used in early detection of cancer and assessment of extent of metastasis. They may be useful in preparing vaccines to counteract transplant rejection, to treat autoimmune diseases, and perhaps to treat AIDS. (Clinical Application)
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
D. A group of about 20 proteins present in blood plasma and on cell membranes comprises the
complement system; when activated, these proteins complement or enhance certain immune, allergic, and inflammatory reactions.
E. Immunological Memory a. Immunological memory is due to the presence of long-lived antibodies and very longlived lymphocytes that arise during proliferation and differentiation of antigenstimulated B and T cells.
b. Immunization against certain microbes is possible because memory B cells and memory
T cells remain after the primary response to an antigen.
c. The secondary response (immunological memory) provides protection should the same
microbe enter the body again. There is rapid proliferation of memory cells, resulting in a far greater antibody titer (amount of antibody in serum) than during a primary response.
VII. SELF-RECOGNIZITON AND SELF-TOLERANCE A. T cells undergo both positive and negative selection to ensure that they can recognize self-MHC
antigens (self-recognition) and that they do not react to other self-proteins (tolerance). Negative selection involves both deletion and anergy.
B. B cells develop tolerance through deletion and anergy. C. Much research has centered on cancer immunology, the study of ways to use the immune system
for detecting, monitoring, and treating cancer (Clinical Application). STRESS AND IMMUNITY
A. The field of psychoneuroimmunology (PNI) deals with common pathways that link the nervous,
endocrine, and immune systems.
B. PNI has shown that thoughts, feelings, moods, and beliefs influence the level of health and the
course of a disease. AGING AND THE IMMUNE SYSTEM
A. With advancing age, the immune system functions less effectively. Individuals become more
susceptible to infections and malignancies, response to vaccines is decreased, and more autoantibodies are produced.
B. Cellular and humoral responses also diminish.
DISORDERS: HOMEOSTATIC IMBALANCES
A. AIDS: Acquired Immunodeficiency Syndrome 1. AIDS is a condition in which a person experiences a telltale assortment of infections as a
result of the progressive destruction of immune cells by the human immunodeficiency virus (HIV).
2. Although HIV has been isolated from several body fluids, the only documented
transmissions are by way of blood, semen, vaginal secretions, and breast milk from an
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
infected nursing mother. It does not appear that people become infected as a result of routine, nonsexual contacts.
a. The AIDS virus is generally thought to be quite fragile outside of the body and
easily eliminated with standard disinfecting techniques.
b. At present, the only means of preventing AIDS is to block transmission of the
virus, including abstinence from sex with infected individuals, use of condoms during intercourse, use of sterile hypodermic needles, and avoidance of pregnancy in HIV-infected women. Until there is an effective drug therapy or an effective vaccine, preventing the spread of AIDS must rely on education and safer sexual practices.
3. HIV is a form of retrovirus with a protein coat wrapped by an envelope of glycoproteins. a. HIV enters T cells where it sheds its protein coat. b. New HIV DNA is produced in the T cell along with new protein coats and then
released.
c. The T cells are ultimately destroyed. 4. Common signs and symptoms of infection are fever, fatigue, rash, headache, joint pain,
sore throat, and swollen lymph nodes. The infected individual ultimately develops antibodies to HIV.
5. Progression to AIDS occurs because of reduced numbers of T cells and resulting
immunodeficiency. AIDS lowers the body s immunity by decreasing the number of helper T cells; the result is progressive collapse of the immune system, making the person susceptible to opportunistic infections (invasion of normally harmless microorganisms that now proliferate wildly because of the defective immune system).
6. Treatment of HIV infection with reverse transcriptase inhibitors and protease inhibitors
has shown to delay the progression of HIV infection to AIDS.
B. A person who is overly reactive to a substance that is tolerated by most others is said to be
hypersensitive (allergic). Whenever an allergic reaction occurs, there is tissue injury. The antigens that induce an allergic reaction are called allergens.
1. There are four basic types of hypersensitivity reactions. a. Type I (anaphylaxis) reactions are the most common and occur with a few
minutes after a person sensitized to an allergen is reexposed to it. Anaphylaxis results from the interaction of allergens with IgE antibodies on the surface of mast cells and basophils. In anaphylactic shock, which may occur in a susceptible individual who has just received a triggering drug or been stung by a wasp, wheezing and shortness of breath as airways constrict are usually accompanied by shock due to vasodilation and fluid loss from blood. This is a life-threatening emergency.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
b. Type II (cytotoxic) reactions are caused by antibodies (IgG or IgM) directed
against a person s blood cells or tissue cells. The reaction of antibodies and antigens usually leads to activation of complement. Type II reaction, which may occur in incompatible blood transfusion reactions, damage cells by causing lysis.
c.
Type III (immune complex) reactions involve antigens (not part of a host tissue cell), antibodies (IgA or IgM), and complement. Some type II conditions include glomerulonephritis, systemic lupus erythematosus, and rheumatoid arthritis.
d. Type IV (cell-mediated) reactions or delayed hypersensitivity reactions usually
appear 12-72 hours after exposure to an allergen and occur when allergens are taken up by antigen-presenting cells that migrate to lymph nodes and present the allergen to T cells. Intracellular bacteria, such as the one that causes tuberculosis, trigger this type of cell-mediated immune response.
C. In an autoimmune disease the immune system fails to display self-tolerance and attacks the
person s own tissue.
D. Severe Combined Immunodeficiency Disease (SCID) is an inherited disorder in which both B and T
cells are missing or inactive in providing immunity.
E. Infectious mononucleosis is a contagious disease primarily affecting lymphatic tissue throughout
the body but also affecting the blood. It is caused by the Epstein-Barr virus which multiplies in B cells. There is no cure, and treatment consists of watching for and treating complications. Usually the disease runs its course in a few weeks.
F. Lymphomas are cancers of the lymphatic organs especially the lymph nodes. The two main types
are: Hodgkin disease and non-Hodgkin lymphoma.
G. Systemic lupus erythematosus is a chronic autoimmune, inflammatory disease that affects
multiple body systems.
Critical Thinking Questions
1. You have been asked to speak to a high school biology class about AIDS. What points do you plan to stress
to these teenagers about this disease? What information do you want these teenagers to know for their own protection and for the protection of others?
2. Draw a flowchart to indicate the steps the body takes when invaded by a virus. Include in your chart both
the nonspecific and specific defense mechanisms.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
THE RESPIRATORY SYSTEM I. INTRODUCTION A. The two systems that cooperate to supply O2 and eliminate CO2 are the cardiovascular and the
respiratory system.
1. The respiratory system provides for gas exchange. 2. The cardiovascular system transports the respiratory gases. 3. Failure of either system has the same effect on the body: disruption of homeostasis and
rapid death of cells from oxygen starvation and buildup of waste products.
B. Respiration is the exchange of gases between the atmosphere, blood, and cells. It takes place in
three basic steps: ventilation (breathing), external (pulmonary) respiration, and internal (tissue) respiration.
II. RESPIRATORY SYSTEM ANATOMY A. The respiratory system consists of the nose, pharynx, larynx, trachea, bronchi, and lungs. 1. The upper respiratory system refers to the nose, pharynx, and associated structures. The
lower respiratory system refers to the larynx, trachea, bronchi, and lungs.
2. The conducting system consists of a series of cavities and tubes - nose, pharynx, larynx,
trachea, bronchi, bronchiole, and terminal bronchioles - that conduct air into the lungs. The respiratory portion consists of the area where gas exchange occurs - respiratory bronchioles, alveolar ducts, alveolar sacs, and alveoli.
3. The branch of medicine that deals with the diagnosis and treatment of diseases of the
ear, nose, and throat is called otorhinolaryngology.
B. The external portion of the nose is made of cartilage and skin and is lined with mucous
membrane. Openings to the exterior are the external nares.
1. The external portion of the nose is made of cartilage and skin and is lined with mucous
membrane.
2. The bony framework of the nose is formed by the frontal bone, nasal bones, and
maxillae.
3. The interior structures of the nose are specialized for warming, moistening, and filtering
incoming air; receiving olfactory stimuli; and serving as large, hollow resonating chambers to modify speech sounds.
4. The internal portion communicates with the paranasal sinuses and nasopharynx through
the internal nares.
5. The inside of both the external and internal nose is called the nasal cavity. It is divided
into right and left sides by the nasal septum. The anterior portion of the cavity is called the vestibule.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
6. Rhinoplasty ( nose job ) is a surgical procedure in which the structure of the external
nose is altered for cosmetic or functional reasons. (Clinical Application)
C. Pharynx 1. The pharynx (throat) is a muscular tube lined by a mucous membrane. 2. The anatomic regions are the nasopharynx, oropharynx, and laryngopharynx. 3. The nasopharynx functions in respiration. Both the oropharynx and laryngopharynx
function in digestion and in respiration (serving as a passageway for both air and food).
D. Larynx 1. The larynx (voice box) is a passageway that connects the pharynx with the trachea. 2. It contains the thyroid cartilage (Adam s apple); the epiglottis, which prevents food from
entering the larynx; the cricoid cartilage, which connects the larynx and trachea; and the paired arytenoid, corniculate, and cuneiform cartilages.
E. The Structures of Voice Production 1. The larynx contains vocal folds (true vocal cords), which produce sound. Taunt vocal
folds produce high pitches, and relaxed vocal folds produce low pitches.
2. Sound originates from the vibration of the vocal folds, but other structures are necessary
for converting the sound into recognizable speech.
3. Laryngitis is an inflammation of the larynx that is usually caused by respiratory infection
or irritants. Cancer of the larynx is almost exclusively found in smokers (Clinical Application).
F. Trachea 1. The trachea (windpipe) extends from the larynx to the primary bronchi. 2. It is composed of smooth muscle and C-shaped rings of cartilage and is lined with
pseudostratified ciliated columnar epithelium.
a. The cartilage rings keep the airway open. b. The cilia of the epithelium sweep debris away from the lungs and back to the
throat to be swallowed.
3. Two methods of bypassing obstructions from the respiratory passageways are
tracheostomy and intubation. (Clinical Application)
G. Bronchi 1. The trachea divides into the right and left pulmonary bronchi. 2. The bronchial tree consists of the trachea, primary bronchi, secondary bronchi, tertiary
bronchi, bronchioles, and terminal bronchioles.
a. Walls of bronchi contain rings of cartilage. b. Walls of bronchioles contain smooth muscle. H. Lungs
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
1. Lungs are paired organs in the thoracic cavity; they are enclosed and protected by the
pleural membrane.
a. The parietal pleura is the outer layer which is attached to the wall of the
thoracic cavity.
b. The visceral pleura is the inner layer, covering the lungs themselves. c. Between the pleurae is a small potential space, the pleural cavity, which
contains a lubricating fluid secreted by the membranes.
d. The lungs extend from the diaphragm to just slightly superior to the clavicles
and lie against the ribs anteriorly and posteriorly.
e. The lungs almost totally fill the thorax. 2. The right lung has three lobes separated by two fissures; the left lung has two lobes
separated by one fissure and a depression, the cardiac notch.
a. The secondary bronchi give rise to branches called tertiary (segmental) bronchi,
which supply segments of lung tissue called bronchopulmonary segments.
b. Each bronchopulmonary segment consists of many small compartments called
lobules, which contain lymphatics, arterioles, venules, terminal bronchioles, respiratory bronchioles, alveolar ducts, alveolar sacs, and alveoli.
3. Alveoli a. Alveolar walls consist of type I alveolar (squamous pulmonary epithelial) cells,
type II alveolar (septal) cells, and alveolar macrophages (dust cells).
b. Type II alveolar cells secrete alveolar fluid, which keeps the alveolar cells moist
and which contains a component called surfactant. Surfactant lowers the surface tension of alveolar fluid, preventing the collapse of alveoli with each expiration.
c. Gas exchange occurs across the alveolar-capillary membrane. d. Nebulization, a procedure for administering medication as small droplets
suspended in air into the respiratory tract, is used to treat many different types of respiratory disorders (Clinical Application).
3. The lungs have a double blood supply. a. Blood enters the lungs via the pulmonary arteries (pulmonary circulation) and
the bronchial arteries (systemic circulation). Most of the blood leaves by the pulmonary veins, but some drains into the bronchial veins.
b. In the lungs vasoconstriction in response to hypoxia diverts pulmonary blood
from poorly ventilated areas to well ventilated areas. This phenomenon is known as ventilation perfusion coupling.
II. PULMONARY VENTILATION
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
A. Respiration occurs in three basic steps: pulmonary ventilation, external respiration, and internal
respiration.
B. Inspiration (inhalation) is the process of bringing air into the lungs. 1. The movement of air into and out of the lungs depends on pressure changes governed in
part by Boyle s law, which states that the volume of a gas varies inversely with pressure, assuming that temperature is constant.
2. The first step in expanding the lungs involves contraction of the main inspiratory muscle,
the diaphragm
3. Inhalation occurs when alveolar (intrapulmonic) pressure falls below atmospheric
pressure. Contraction of the diaphragm and external intercostal muscles increases the size of the thorax, thus decreasing the intrapleural (intrathoracic) pressure so that the lungs expand. Expansion of the lungs decreases alveolar pressure so that air moves along the pressure gradient from the atmosphere into the lungs
4. During forced inhalation, accessory muscles of inspiration (sternocleidomastoids,
scalenes, and pectoralis minor) are also used.
C. Expiration (exhalation) is the movement of air out of the lungs. 1. Exhalation occurs when alveolar pressure is higher than atmospheric pressure.
Relaxation of the diaphragm and external intercostal muscles results in elastic recoil of the chest wall and lungs, which increases intrapleural pressure, decreases lung volume, and increases alveolar pressure so that air moves from the lungs to the atmosphere. There is also an inward pull of surface tension due to the film of alveolar fluid.
2. Exhalation becomes active during labored breathing and when air movement out of the
lungs is impeded. Forced expiration employs contraction of the internal intercostals and abdominal muscles
D. Alveolar Surface Tension 1. In the lungs, surface tension causes the alveoli to assume the smallest diameter possible. a. During breathing, surface tension must be overcome to expand the lungs during
each inspiration. It is also the major component of lung elastic recoil, which acts to decrease the size of the alveoli during expiration.
b. The presence of surfactant, a phospholipid produced by the type II alveolar
(septal) cells in the alveolar walls, allows alteration of the surface tension of the alveoli and prevents their collapse following expiration.
2. Injuries to the chest wall that allow air to enter the intrapleural space either from the
outside or from the alveoli cause pneumothorax, filling the pleural cavity with air. (Clinical Application)
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
E. Compliance is the ease with which the lungs and thoracic wall can be expanded. Any condition
that destroys lung tissue causes it to become filled with fluid, produces a deficiency in surfactant, or in any way impedes lung expansion or contraction, decreases compliance.
F. The walls of the respiratory passageways, especially the bronchi and bronchioles, offer some
resistance to the normal flow of air into the lungs. Any condition that obstructs the air passageway increases resistance, and more pressure to force air through is required.
G. Breathing Patterns and Modified Respiratory Movements 1. Breathing Patterns a. Eupnea is normal variation in breathing rate and depth. b. Apnea refers to breath holding. c. Dyspnea relates to painful or difficult breathing. d. Tachypnea involves rapid breathing rate. e. Costal breathing requires combinations of various patterns of intercostal and
extracostal muscles, usually during need for increased ventilation, as with exercise.
f. Diaphragmatic breathing is the usual mode of operation to move air by
contracting and relaxing the diaphragm to change the lung volume
2. Modified respiratory movements are used to express emotions and to clear air
passageways. Table 23.1 lists some of the modified respiratory movements.
IV. LUNG VOLUMES AND CAPACITIES A. Air volumes exchanged during breathing and rate of ventilation are measured with a
spiromometer, or respirometer, and the record is called a spirogram
B. Among the pulmonary air volumes exchanged in ventilation are tidal (500 ml), inspiratory reserve
(3100 ml), expiratory reserve (1200 ml), residual (1200 ml) and minimal volumes. Only about 350 ml of the tidal volume actually reaches the alveoli, the other 150 ml remains in the airways as anatomic dead space.
C. Pulmonary lung capacities, the sum of two or more volumes, include inspiratory (3600 ml),
functional residual (2400 ml), vital (4800 ml), and total lung (6000 ml) capacities.
D. The minute volume of respiration is the total volume of air taken in during one minute (tidal
volume x 12 respirations per minute = 6000 ml/min).
V. EXCHANGE OF OXYGEN AND CARBON DIOXIDE A. To understand the exchange of oxygen and carbon dioxide between the blood and alveoli, it is
useful to know some gas laws.
1. According to Dalton s law, each gas in a mixture of gases exerts its own pressure as if all
the other gases were not present.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
a. The partial pressure of a gas is the pressure exerted by that gas in a mixture of
gases. The total pressure of a mixture is calculated by simply adding all the partial pressures. It is symbolized by P.
b. The partial pressures of the respiratory gases in the atmosphere, alveoli, blood,
and tissues cells are shown in the text.
c. The amounts of O2 and CO2 vary in inspired (atmospheric), alveolar, and expired
air.
2. Henry s law states that the quantity of a gas that will dissolve in a liquid is proportional
to the partial pressure of the gas and its solubility coefficient (its physical or chemical attraction for water), when the temperature remains constant.
a. Nitrogen narcosis and decompression sickness (caisson disease, or bends) are
conditions explained by Henry s law.
b. A major clinical application of Henry s law is hyperbaric oxygenation. This
technique uses pressure to cause more oxygen to dissolve in the blood and is used to treat anaerobic bacterial infections (such as tetanus and gangrene) and a number of other disorders and injuries.
B. External and Internal Respiration 1. In internal and external respiration, O2 and CO2 diffuse from areas of their higher partial
pressures to areas of their lower partial pressures and results in the conversion of deoxygenated blood (more CO2 than O2) coming from the heart to oxygenated blood (more O2 than CO2) returning to the heart.
2. It depends on partial pressure differences, a large surface area for gas exchange, a small
diffusion distance across the alveolar-capillary (respiratory) membrane, and the solubility and molecular weight of the gases.
3. Internal (tissue) respiration is the exchange of gases between tissue blood capillaries and
tissue cells and results in the conversion of oxygenated blood into deoxygenated blood.
4. At rest only about 25% of the available oxygen in oxygenated blood actually enters
tissue cells. During exercise, more oxygen is released.
VI. TRANSPORT OF OXYGEN AND CARBON DIOXIDE IN THE BLOOD A. Oxygen Transport 1. In each 100 ml of oxygenated blood, 1.5% of the O2 is dissolved in the plasma and 98.5%
is carried with hemoglobin (Hb) inside red blood cells as oxyhemglobin (HbO2) (Figure 23.19).
a. Hemoglobin consists of a protein portion called globin and a pigment called
heme.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
b. The heme portion contains 4 atoms of iron, each capable of combining with a
molecule of oxygen.
2. Hemoglobin and Oxygen Partial Pressure a. The most important factor that determines how much oxygen combines with
hemoglobin is PO2.
b. The relationship between the percent saturation of hemoglobin and PO2 is
illustrated in the oxygen-hemoglobin dissociation curve.
c. The greater the PO2, the more oxygen will combine with hemoglobin, until the
available hemoglobin molecules are saturated.
3. Other Factors Affecting Hemoglobin Affinity for Oxygen a. In an acid (low pH) environment, O2 splits more readily from hemoglobin. This is
referred to as the Bohr effect.
b. Low blood pH (acidic conditions) results from high PCO2. c. Within limits, as temperature increases, so does the amount of oxygen released
from hemoglobin. Active cells require more oxygen, and active cells (such as contracting muscle cells) liberate more acid and heat. The acid and heat, in turn, stimulate the oxyhemoglobin to release its oxygen.
d. BPG (2, 3-biphosphoglycerate) is a substance formed in red blood cells during
glycolysis. The greater the level of BPG, the more oxygen is released from hemoglobin.
4. Fetal hemoglobin has a higher affinity for oxygen because it binds BPG less strongly and
can carry more oxygen to offset the low oxygen saturation in maternal blood in the placenta.
5. Because of the strong attraction of carbon monoxide (CO) to hemoglobin, even small
concentrations of CO will reduce the oxygen carrying capacity leading to hypoxia and carbon monoxide poisoning. (Clinical Application)
B. Carbon Dioxide Transport 1. CO2 is carried in blood in the form of dissolved CO2 (7%), carbaminohemoglobin (23%),
and bicarbonate ions (70%).
2. The conversion of CO2 to bicarbonate ions and the related chloride shift maintains the
ionic balance between plasma and red blood cells.
C. Summary of Gas Exchange and Transport in Lungs and Tissues 1. CO2 in blood causes O2 to split from hemoglobin. 2. Similarly, the binding of O2 to hemoglobin causes a release of CO2 from blood. VII. CONTROL OF RESPIRATION A. Respiratory Center
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
1. The area of the brain from which nerve impulses are sent to respiratory muscles is
located bilaterally in the reticular formation of the brain stem. This respiratory center consists of a medullary rhythmicity area (inspiratory and expiratory areas), pneumotaxic area, and apneustic area.
2. Medullary Rhythmicity Area a. The function of the medullary rhythmicity area is to control the basic rhythm of
respiration.
b. The inspiratory area has an intrinsic excitability of autorhythmic neurons that
sets the basic rhythm of respiration.
c. The expiratory area neurons remain inactive during most quiet respiration but
are probably activated during high levels of ventilation to cause contraction of muscles used in forced (labored) expiration.
3. Pneumotaxic Area a. The pneumotaxic area in the upper pons helps coordinate the transition
between inspiration and expiration.
b. The apneustic area sends impulses to the inspiratory area that activate it and
prolong inspiration, inhibiting expiration.
B. Regulation of the Respiratory Center 1. Cortical Influences a. Cortical influences allow conscious control of respiration that may be needed to
avoid inhaling noxious gasses or water.
b. Breath holding is limited by the overriding stimuli of increased [H+] and [CO2]. 2. Chemoreceptor Regulation of Respiration a. Central chemoreceptors (located in the medulla oblongata) and peripheral
chemoreceptors (located in the walls of systemic arteries) monitor levels of CO2 and O2 and provide input to the respiratory center.
1) Central chemoreceptors respond to change in H+ concentration or PCO2,
or both in cerebrospinal fluid.
2) Peripheral chemoreceptors respond to changes in H+, PCO2, and PO2 in
blood.
b. A slight increase in PCO2 (and thus H+), a condition called hypercapnia, stimulates
central chemoreceptors.
1) As a response to increased PCO2, increased H+ and decreased PO2, the
inspiratory area is activated and hyperventilation, rapid and deep breathing, occurs.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
2) If arterial PCO2 is lower than 40 mm Hg, a condition called hypocapnia,
the chemoreceptors are not stimulated and the inspiratory area sets its own pace until CO2 accumulates and PCO2 rises to 40 mm Hg.
c. Severe deficiency of O2 depresses activity of the central chemoreceptors and
respiratory center.
d. Hypoxia refers to oxygen deficiency at the tissue level and is classified in several
ways (Clinical Application).
1) Hypoxic hypoxia is caused by a low PO2 in arterial blood (high altitude,
airway obstruction, fluid in lungs).
2) In anemic hypoxia, there is too little functioning hemoglobin in the
blood (hemorrhage, anemia, carbon monoxide poisoning).
3) Stagnant hypoxia results from the inability of blood to carry oxygen to
tissues fast enough to sustain their needs (heart failure, circulatory shock).
4) In histotoxic hypoxia, the blood delivers adequate oxygen to the
tissues, but the tissues are unable to use it properly (cyanide poisoning).
3. Proprioceptors of joints and muscles activate the inspiratory center to increase
ventilation prior to exercise induced oxygen need.
4. The inflation (Hering-Breuer) reflex detects lung expansion with stretch receptors and
limits it depending on ventilatory need and prevention of damage.
5. Other influences include blood pressure, limbic system, temperature, pain, stretching
the anal sphincter, and irritation to the respiratory mucosa. VIII. EXERCISE AND THE RESPIRATORY SYSTEM A. The respiratory system works with the cardiovascular system to make appropriate adjustments for different exercise intensities and durations. B. As blood flow increases with a lower O2 and higher CO2 content, the amount passing through the lung (pulmonary perfusion) increases and is matched by increased ventilation and oxygen diffusion capacity as more pulmonary capillaries open. C. Ventilatory modifications can increase 30 times above resting levels, in an initial rapid rate due to neural influences and then more gradually due to chemical stimulation from changes in cell metabolism. A similar, but reversed, effect occurs with cessation of exercise. D. Smokers have difficulty breathing for a number of reasons, including nicotine, mucous, irritants, and that fact that scar tissue replaces elastic fibers. IX. DEVELOPMENT OF THE RESPIRATORY SYSTEM A. The respiratory system begins as an outgrowth of endoderm called the laryngotracheal bud, part of which divides into two lung buds that grow into the bronchi and lungs.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
B.
The smooth muscle, cartilage, and connective tissue of the bronchial tubes and pleural sacs develop from mesenchyma (mesodermal) cells.
X. AGING AND THE RESPIRATORY SYSTEM A. Aging results in decreased vital capacity, decreased blood oxygen level, diminished alveolar macrophage activity, and decreased ciliary action of the epithelium lining the respiratory tract. B. Elderly people are more susceptible to pneumonia, bronchitis, emphysema, and other pulmonary disorders. XI. FOCUS ON HOMEOSTASIS: THE RESPIRATORY SYSTEM Examines the role of the respiratory system in maintaining homeostasis. XII. DISORDERS: HOMEOSTATIC IMBALANCES A. Asthma is characterized by the following: spasms of smooth muscle in bronchial tubes that result in partial or complete closure of air passageways; inflammation; inflated alveoli; and excess mucus production. A common triggering factor is allergy, but other factors include emotional upset, aspirin, exercise, and breathing cold air or cigarette smoke. B. Chronic obstructive pulmonary disease (COPD) is a type of respiratory disorder characterized by chronic and recurrent obstruction of air flow, which increases airway resistance.
1. The principal types of COPD are emphysema and chronic bronchitis. 2. Bronchitis is an inflammation of the bronchial tubes, the main symptom of which is a
productive (raising mucus or sputum) cough. C. In bronchogenic carcinoma (lung cancer), bronchial epithelial cells are replaced by cancer cells after constant irritation has disrupted the normal growth, division, and function of the epithelial cells. Airways are often blocked and metastasis is very common. It is most commonly associated with smoking. D. Pneumonia is an acute infection of the alveoli. The most common cause in the pneumococcal bacteria but other microbes may be involved. Treatment involves antibiotics, bronchodilators, oxygen therapy, and chest physiotherapy. E. Tuberculosis (TB) is an inflammation of pleurae and lungs produced by the organism Mycobacterium tuberculosis. It is communicable and destroys lung tissue, leaving nonfunctional fibrous tissue behind. F. Coryza (common cold) is caused by viruses and usually is not accompanied by a fever, whereas influenza (flu) is usually accompanied by a fever greater than 101 F G.
o .
Pulmonary edema refers to an abnormal accumulation of interstitial fluid in the interstitial spaces and alveoli of the lungs. It may be pulmonary or cardiac in origin.
H. Cystic fibrosis is an inherited disease of secretory epithelia that affects the respiratory passageways, pancreas, salivary glands, and sweat glands. I. Acute respiratory distress syndrome is a from of respiratory failure characterized by excessive leakiness of respiratory membranes and severe hypoxia.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
Critical Thinking Questions
1.
You are the captain of a miniature submarine that is being sent on a voyage through the body. Your assignment is to plot the course taken by molecules of oxygen from the atmosphere to the heart and the reverse course taken by molecules of carbon dioxide from the heart to the atmosphere. Diagram and explain how you would organize the course.
2.
A five-year-old child threatens to hold his breath until he dies if his mother does not buy him an ice cream cone. Would you advise the mother to let the child hold his breath or to give in to his demand? Your advice should be based only on any possible physiological damage to the child.
3.
You have been asked to assist an 80-year-old resident of a nursing home who is hyperventilating. You want to be sure she does not faint and lose consciousness. What are you going to do to help this individual?
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
THE DIGESTIVE SYSTEM
I. INTRODUCTION
A. Food contains substances and energy the body needs to construct all cell components. The food
must be broken down through digestion to molecular size before it can be absorbed by the digestive system and used by the cells.
B. The organs that collectively perform these functions compose the digestive system. C. The medical professions that study the structures, functions, and disorders of the digestive tract
are gastroenterology for the upper end of the system and proctology for the lower end.
II. OVERVIEW OF THE DIGESTIVE SYSTEM A. Organization 1. The two major sections of the digestive system perform the processes required to
prepare food for use in the body.
2. The gastrointestinal tract is the tube open at both ends for the transit of food during
processing. The functional segments of the GI tract include the mouth, esophagus, stomach, small intestine, and large intestine.
3. The accessory structures that contribute to the food processing include the teeth,
tongue, salivary glands, liver, gallbladder, and pancreas.
B. Digestion includes six basic processes. 1. Ingestion is taking food into the mouth (eating). 2. Secretion is the release, by cells within the walls of the GI tract and accessory organs, of
water, acid, buffers, and enzymes into the lumen of the tract.
3. Mixing and propulsion result from the alternating contraction and relaxation of the
smooth muscles within the walls of the GI tract.
4. Digestion a. Mechanical digestion consists of movements of the GI tract that aid chemical
digestion.
b. Chemical digestion is a series of catabolic (hydrolysis) reactions that break
down large carbohydrate, lipid, and protein food molecules into smaller molecules that are usable by body cells.
5. Absorption is the passage of end products of digestion from the GI tract into blood or
lymph for distribution to cells.
6. Defecation is emptying of the rectum, eliminating indigestible substances from the GI
tract.
III. LAYERS OF THE GI TRACT A. The basic arrangement of layers in the gastrointestinal tract from the inside outward includes the
mucosa, submucosa, muscularis, and serosa (visceral peritoneum).
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
B. The mucosa consists of an epithelium, lamina propria, and muscularis mucosa. 1. The epithelium consists of a protective layer of non-keratinized stratified cells, simple
cells for secretion and absorption, and mucus secreting cells, as well as some enteroendocrine cells that put out hormones that help regulate the digestive process.
2. The lamina propria consists of three components, including loose connective tissue that
adheres the epithelium to the lower layers, the system of blood and lymph vessels through which absorbed food is transported, and nerves and sensors.
a. The lymph system is part of the mucosa-associated lymph tissues (MALT) that
monitor and produce an immune response to pathogens passing with food through the GI tract.
b. It is estimated that there are as many immune cells associated with the GI tract
as in all the rest of the body.
3. The muscularis mucosa causes local folding of the mucosal layer to increase surface are
for digestion and absorption.
C. The submucosa consists of aerolar connective tissue. It is highly vascular, contains a part of the
submucosal plexus (plexus of Meissner), and contains glands and lymphatic tissue.
1. The submucosal plexus is a part of the autonomic nervous system. 2. It regulates movements of the mucosa, vasoconstriction of blood vessels, and innervates
secretory cells of mucosal glands.
D. Muscularis 1. The muscularis of the mouth, pharynx, and superior part of the esophagus contains
skeletal muscle that produces voluntary swallowing. Skeletal muscle also forms the external anal sphincter.
2. Through the rest of the tract, the muscularis consists of smooth muscle in an inner sheet
of circular fibers and an outer sheet of longitudinal fibers.
3. The muscularis also contains the major nerve supply to the GI tract - the myenteric
plexus (plexus of Auerbach), which consists of fibers from both divisions of the ANS. This plexus mostly controls GI tract motility.
E. The serosa is the superficial layer of those portions of the GI tract that are suspended in the
abdominoplevic cavity.
1. The esophagus is covered by an adventitia. 2. Inferior to the diaphragm, the serosa is also called the visceral peritoneum. IV. PERITONEUM A. The peritoneum is the largest serous membrane of the body. 1. The parietal peritoneum lines the wall of the abdominal cavity. 2. The visceral peritoneum covers some of the organs and constitutes their serosa.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
3. The potential space between the parietal and visceral portions of the peritoneum is
called the peritoneal cavity and contains serous fluid.
4. Some organs, such as the kidneys and pancreas, lie on the posterior abdominal wall
behind the peritoneum and are called retroperitoneal.
5. The peritoneum contains large folds that weave between the viscera, functioning to
support organs and to contain blood vessels, lymphatic vessels, and nerves of the abdominal organs.
6. Extensions of the peritoneum include the mesentery, meoscolon, falciform ligament,
lesser omentum, and greater omentum.
B. Peritonitis is an acute inflammation of the peritoneum. (Clinical Application) V. MOUTH A. Introduction 1. The mouth (oral or buccal cavity) is formed by the cheeks, hard and soft palate, lips, and
tongue.
2. The vestibule of the oral cavity is bounded externally by the cheeks and lips and
internally by the gums and teeth.
3. The oral cavity proper is a space that extends from the gums and teeth to the fauces, the
opening between the oral cavity and the pharynx or throat.
B. Salivary Glands 1. The major portion of saliva is secreted by the salivary glands, which lie outside the
mouth and pour their contents into ducts that empty into the oral cavity; the remainder of saliva comes from buccal glands in the mucous membrane that lines the mouth.
2. There are three pairs of salivary glands: parotid, submandibular (submaxillary), and
sublingual glands.
3. Saliva lubricates and dissolves food and starts the chemical digestion of carbohydrates.
It also functions to keep the mucous membranes of the mouth and throat moist.
4. Chemically, saliva is 99.5% water and 0.5% solutes such as salts, dissolved gases, various
organic substances, and enzymes.
5. Salivation is entirely under nervous control. 6. Mumps is an inflammation and enlargement of the parotid salivary glands caused by
infection with the mumps virus (myxovirus). Symptoms include fever, malaise, pain, and swelling of one or both glands. If mumps is contracted by a male past puberty, it is possible to experience inflammation of the testes and, occasionally, sterility. (Clinical Application)
C. Structure and Function of the Tongue
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
1. The tongue, together with its associated muscle, forms the floor of the oral cavity. It is
composed of skeletal muscle covered with mucous membrane.
2. Extrinsic and intrinsic muscles permit the tongue to be moved to participate in food
manipulation for chewing and swallowing and in speech.
3. The lingual frenulum is a fold of mucous membrane that attaches to the midline of the
undersurface of the tongue.
4. The upper surface and sides of the tongue are covered with papillae. Some papillae
contain taste buds.
5. On the dorsum of the tongue are glands that secrete lingual lipase, which initiates
digestion of triglycerides.
D. Structure and Function of the Teeth 1. The teeth project into the mouth and are adapted for mechanical digestion. 2. A typical tooth consists of three principal portions: crown, root, and neck. 3. Teeth are composed primarily of dentin, a calcified connective tissue that gives the tooth
its basic shape and rigidity; the dentin of the crown is covered by enamel, the hardest substance in the body, which protects the tooth from the wear of chewing.
a. The dentin of the root is covered by cementum, another bone-like substance,
which attaches the root to the periodontal ligament (the fibrous connective tissue lining of the tooth sockets in the mandible and maxillae).
b. The dentin encloses the pulp cavity in the crown and the root canals in the root. c. The branch of dentistry that is concerned with the prevention, diagnosis, and
treatment of diseases that affect the pulp, root, periodontal ligament, and alveolar bone is known as endodontics. Orthodontics is a dental branch concerned with the prevention and correction of abnormally aligned teeth. Periodontics is a dental branch concerned with the treatment of abnormal conditions of tissues immediately around the teeth.
4. There are two dentitions, or sets of teeth, in an individual s lifetime: deciduous
(primary), milk teeth, or baby teeth; and permanent (secondary) teeth.
5. There are four different types of teeth based on shape: incisors (used to cut food),
cuspids or canines (used to tear or shred food), premolars or bicuspids (absent in the deciduous dentition and used for crushing and grinding food), and molars (also used for crushing and grinding food).
6. In root canal therapy all traces of pulp tissue are removed from the pulp cavity and root
canal of a badly diseased tooth (Clinical Application).
E. Mechanical and Chemical Digestion in the Mouth
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
1. Through mastication (chewing), food is mixed with saliva and shaped into a bolus that is
easily swallowed.
2. The enzyme salivary amylase converts polysaccharides (starches) to disaccharides
(maltose). This is the only chemical digestion that occurs in the mouth.
VI. PHARYNX A. The pharynx is a funnel-shaped tube that extends from the internal nares to the esophagus
posteriorly and the larynx anteriorly.
1. It is composed of skeletal muscle and lined by mucous membrane. 2. The nasopharynx functions in respiration only, whereas the oropharynx and
laryngopharynx have digestive as well as respiratory functions.
B. Deglutition, or swallowing, moves a bolus from the mouth to the stomach. It is facilitated by
saliva and mucus and involves the mouth, pharynx, and esophagus.
1. Deglutition consists of a voluntary state, pharyngeal stage (involuntary), and esophageal
stage (involuntary).
2. Receptors in the oropharynx stimulate the deglutition center in the medulla and the
lower pons of the brain stem.
VII. ESOPHAGUS A. The esophagus is a collapsible, muscular tube that lies behind the trachea and connects the
pharynx to the stomach.
B. The wall of the esophagus contains mucosa, submucosa, and muscularis layers. The outer layer is
called the adventitia rather than the serosa due to structural differences.
C. Physiology of the Esophagus 1. The esophagus contains an upper and a lower esophageal sphincter. 2. During the esophageal stage of swallowing progressive contractions of the muscularis
push the bolus onward. There propulsive contractions are termed peristalsis.
D. Gastroesophageal reflux disease occurs when the lower esophageal sphincter fails to close
adequately after food has entered the stomach, resulting in stomach contents refluxing into the inferior portion of the esophagus. HCl from the stomach contents irritates the esophageal wall resulting in heartburn. (Clinical Application)
VIII. STOMACH A. Introduction 1. The stomach is a J-shaped enlargement of the GI tract that begins at the bottom of the
esophagus and ends at the pyloric sphincter.
2. It serves as a mixing and holding area for food, begins the digestion of proteins, and
continues the digestion of triglycerides, converting a bolus to a liquid called chyme. It can also absorb some substances.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
B. Anatomy of the Stomach 1. The gross anatomical subdivisions of the stomach include the cardia, fundus, body, and
pyloris.
2. When the stomach is empty, the mucosa lies in folds called rugae. 3. Pylorospasm and pyloric stenosis are two abnormalities of the pyloric sphincter that can
occur in newborns. Both functionally block or partially block the exit of food from the stomach into the duodenum and must be treated with drugs or surgery (Clinical Application).
C. Histology of the Stomach 1. The surface of the mucosa is a layer of simple columnar epithelial cells called mucous
surface cells.
a. Epithelial cells extend down into the lamina propria forming gastric pits and
gastric glands.
b. The gastric glands consist of three types of exocrine glands: mucous neck cells
(secrete mucus), chief or zymogenic cells (secrete pepsinogen and gastric lipase), and parietal or oxyntic cells (secrete HCl).
c. Gastric glands also contain enteroendocrine cells which are hormone producing
cells. G cells secrete the hormone gastrin into the bloodstream.
2. The submucosa is composed of areolar connective tissue. 3. The muscularis has three layers of smooth muscle: longitudinal, circular, and an inner
oblique layer.
4. The serosa is a part of the visceral peritoneum. a. At the lesser curvature, the visceral peritoneum becomes the lesser omentum. b. At the greater curvature, the visceral peritoneum becomes the greater
omentum.
D. Mechanical and Chemical Digestion in the Stomach 1. Mechanical digestion consists of peristaltic movements called mixing waves. 2. Chemical Digestion a. Chemical digestion consists mostly of the conversion of proteins into
peptides by pepsin, an enzyme that is most effective in the very acidic environment (pH 2) of the stomach. The acid (HCl) is secreted by the stomach s parietal cells.
b. Gastric lipase splits certain molecules in butterfat of milk into fatty acids
and monoglycerides and has a limited role in the adult stomach.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
3. The stomach wall is impermeable to most substances; however, some water,
electrolytes, certain drugs (especially aspirin), and alcohol can be absorbed through the stomach lining.
E. Regulation of Gastric Secretion and Motility 1. Gastric secretion is regulated by nervous and hormonal mechanisms. Stimulation occurs
in three overlapping phases: cephalic (reflex), gastric, and intestinal.
2. Cephalic Phase a. The cephalic phase consists of reflexes initiated by sensory receptors in the
head.
b. The cephalic phase stimulates gastric secretion and motility. 3. Gastric Phase a. The gastric phase begins when food enters the stomach. b. When the stomach walls are distended or when pH increases because proteins
have entered the stomach and buffered some of the stomach acid, the stretch receptors and chemoreceptors are activated resulting in waves of peristalsis and continual flow of gastric juice.
c. Hormonal negative feedback also regulates gastric secretions during the gastric
phase.
1) Chemoreceptors and stretch receptors stimulate the ANS to release
acetylcholine which stimulates the release of gastrin by G cells.
2) Gastrin stimulates growth of the gastric glands and secretion of large
amounts of gastric juice. It also strengthens contraction of the lower esophageal sphincter, increases motility of the stomach, and relaxes the pyloric and ileocecal sphincters.
3) Acetylcholine released by parasympathetic fibers and gastrin secreted
by G cells stimulate parietal cells to secrete more HCl when histamine is present. In other words, histamine enhances the effects of acetylcholine and gastrin.
4. Intestinal Phase a. The intestinal phase is due to activation of receptors in the small intestine. b. When partially digested food enters the small intestine, it triggers the
enterogastric reflex and the secretion of gastric inhibitory peptide (GIP), secretin, and cholecystokinin (CCK) by the intestinal mucosa. The effect is inhibition of gastric secretion.
5. Regulation of Gastric Emptying
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
a. Gastric emptying is the periodic release of chyme from the stomach into the
duodenum.
b. Gastric emptying is stimulated by two factors: nerve impulses in response to
distention of the stomach and stomach gastrin in response to the presence of certain types of foods.
c. Most food leaves the stomach 2-6 hours after ingestion. Carbohydrates leave
earliest, followed by proteins and then fats.
d. Gastric emptying is inhibited by the enterogastric reflex and by the hormones
CCK and GIP.
e. Vomiting is the forcible expulsion of the contents of the upper GI tract
(stomach and sometimes duodenum) through the mouth. Prolonged vomiting, especially in infants and elderly people, can be serious because the loss of gastric juice and fluids can lead to disturbances in fluid and acid-base balance. (Clinical Application)
IX. PANCREAS A. The pancreas is divided into a head, body, and tail and is connected to the duodenum via the
pancreatic duct (duct of Wirsung) and accessory duct (duct of Santorini).
B. Pancreatic islets (islets of Langerhans) secrete hormones and acini secrete a mixture of fluid and
digestive enzymes called pancreatic juice.
C. Pancreatic Juice 1. Pancreatic juice contains enzymes that digest starch (pancreatic amylase), proteins
(trypsin, chymotrypsin, and carboxypeptidase), fats (pancreatic lipase), and nucleic acids (ribonuclease and deoxyribonuclease).
2. It also contains sodium bicarbonate which converts the acid stomach contents to a
slightly alkaline pH (7.1-8.2), halting stomach pepsin activity and promoting activity of pancreatic enzymes.
3. Inflammation of the pancreas is called pancreatitis and can result in trypsin beginning to
digest pancreatic cells. (Clinical Application)
D. Pancreatic secretion is regulated by nervous and hormonal mechanisms. X. LIVER AND GALLBLADDER A. The liver is the heaviest gland in the body and the second largest organ in the body after the skin. B. Anatomy of the Liver and Gallbladder 1. The liver is divisible into left and right lobes, separated by the falciform ligament.
Associated with the right lobe are the caudate and quadrate lobes.
2. The gallbladder is a sac located in a depression on the posterior surface of the liver. C. Histology of the Liver and Gallbladder
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
1. The lobes of the liver are made up of lobules that contain hepatic cells (liver cells or
hepatocytes), sinusoids, stellate reticuloendothelial (Kupffer s) cells, and a central vein.
2. The mucosa of the gallbladder is simple columnar epithelium arranged in rugae. There is
no submucosa. The smooth muscle of the muscularis ejects bile into the cystic duct. The outer layer is the visceral peritoneum. Functions of the gallbladder are to store and concentrate bile until it is needed in the small intestine.
3. Jaundice is a yellowish coloration of the sclera, skin, and mucous membranes due to a
buildup of bilirubin. The main catergories of jaundice are prehepatic, hepatic, and enterohepatic (Clinical Application).
D. The liver receives a double supply of blood from the hepatic artery and the hepatic portal vein. All
blood eventually leaves the liver via the hepatic vein.
E. Hepatic cells (hepatocytes) produce bile that is transported by a duct system to the gallbladder
for concentration and temporary storage.
1. Bile is partially an excretory product (containing components of worn-out red blood
cells) and partially a digestive secretion.
2. Bile s contribution to digestion is the emulsification of triglycerides. F. The rate of bile secretion is regulated by nervous and hormonal mechanisms as well as by volume
of hepatic blood flow and the concentration of bile salts in the blood.
G. The liver also functions in carbohydrate, lipid, and protein metabolism; removal of drugs and
hormones from the blood; excretion of bilirubin; synthesis of bile salts; storage of vitamins and minerals; phagocytosis; and activation of vitamin D.
H. The fusion of individual crystals of cholesterol is the beginning of 95% of all gallstones. Gallstones
can cause obstruction to the outflow of bile in any portion of the duct system. Treatment of gallstones consists of using gallstone-dissolving drugs, lithotripsy, or surgery (Clinical Application).
XII. SUMMARY OF DIGESTIVE HORMONES A. The effects of the four major digestive hormones - gastrin, secretin, CCK, and GIP - are to regulate
gastric secretion and motility, as well as secretion of the pancreas, liver, and gallbladder.
1. Gastrin promotes secretion of gastric juice and increases gastric motility. 2. Secretin promotes secretion of bicarbonate ions into pancreatic juice and bile. It inhibits
secretion of gastric juice and promotes normal growth and maintenance of the pancreas. It enhances the effects of CCK. Overall, it causes buffering of acid in chyme.
3. CCK stimulates secretion of pancreatic juice rich in digestive enzymes and ejection of bile
into the duodenum. It also slows gastric emptying.
B. There are other hormones secreted by and having effects on the GI tract. They include motilin,
substance P, bombesin, vasoactive intestinal polypeptide, gastrin-releasing peptide, and somatostatin.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
XIII. SMALL INTESTINE A. Introduction 1. The major events of digestion and absorption occur in the small intestine. 2. The small intestine extends from the pyloric sphincter to the ileocecal sphincter. B. Anatomy of the Small Intestine 1. The small intestine is divided into the duodenum, jejunum, and ileum. 2. Projections called circular folds, or plicae circularies, are permanent ridges in the mucosa
that enhance absorption by increasing surface area and causing chyme to spiral as it passes through the small intestine.
C. Histology of the Small Intestine 1. The mucosa forms fingerlike villi which increase the surface area of the epithelium
available for absorption and digestion
a. Embedded in the villus is a lacteal (lymphatic capillary) for fat absorption. b. The cells of the mucosal epithelium include absorptive cells, goblet cells,
enteroendocrine cells, and Paneth cells.
c. The free surface of the absorptive cells feature microvilli, which increase the
surface area. They form the brush border which also contains several enzymes.
d. The mucosa contains many cavities lined by glandular epithelium. These cavities
form the intestinal glands (crypts of Lieberkuhn).
2. The submucosa of the duodenum contains duodenal (Brunner s) glands which secrete an
alkaline mucus that helps neutralize gastric acid in chyme. The submucosa of the ileum contains aggregated lymphatic nodules (Peyer s patches).
D. Intestinal Juice and Brush Border Enzymes 1. Intestinal juice provides a vehicle for absorption of substances from chyme as they come
in contact with the villi.
2. Some intestinal enzymes (brush border enzymes) break down foods inside epithelial
cells of the mucosa on the surfaces of their microvilli.
3. Some digestion also occurs in the lumen of the small intestine. E. Mechanical Digestion in the Small Intestine 1. Segmentation, the major movement of the small intestine, is a localized contraction in
areas containing food.
2. Peristalsis propels the chyme onward through the intestinal tract. F. Chemical Digestion in the Small Intestine 1. Carbohydrates are broken down into monosaccharides for absorption. a. Intestinal enzymes break down starches into maltose, maltotriose, and alphadextrins (pancreatic amylase); alpha-dextrins into glucose (alphadestrinase);
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
maltose to glucose (maltase); sucrose to glucose and fructose (sucrase); and lactose to glucose and galactose (lactase).
b. In some individuals, there is a failure of the intestinal mucosal cells to produce
the enzyme lactase. This results in lactose intolerance, the inability to digest the sugar lactose found in milk and other dairy products. It may be a temporary or long-lasting condition and is characterized by diarrhea, gas, bloating, and abdominal cramps after ingestion of diary products.
2. Protein digestion starts in the stomach. a. Proteins are converted to peptides by trypsin and chymotrypsin. Also, enzymes
break peptide bonds that attach terminal amino acids to carboxyl ends of peptides (carboxypeptidases) and peptide bonds that attach terminal amino acids to amino ends of peptides (aminopeptidases).
b. Finally, enzymes split dipeptides to amino acids (dipeptidase). 3. Most lipid digestion, in an adult, occurs in the small intestine. a. Bile salts break the globules of triglycerides (fats) into droplets, a process called
emulsification.
b. Pancreatic lipase, due to the increase exposed surface area of the droplets, can
hydrolyze more triglycerides into fatty acids and monoglycerides.
4. Nucleic acids are broken down into nucleotides for absorption. G. Regulation of Intestinal Secretion and Motility 1. The most important mechanism for regulating small intestinal secretion is the action of
local reflexes in response to the presence of chyme.
2. Hormones (vasoactive intestinal polypeptide or VIP) also assume a role. 3. Parasympathetic impulses increase motility; sympathetic impulses decrease motility. H. Absorption in the Small Intestine 1. Absorption is the passage of the end products of digestion from the GI tract into blood
or lymph and occurs by diffusion, facilitated diffusion, osmosis, and active transport.
2. Absorption of Monosaccharides a. Essentially all carbohydrates are absorbed as monosaccharides. b. They are absorbed into blood capillaries. 3. Absorption of Amino Acids, Dipeptides, and Tripeptides a. Most proteins are absorbed as amino acids by active transport processes. b. They are absorbed into the blood capillaries in the villus. 4. Absorption of Lipids a. Dietary lipids are all absorbed by simple diffusion.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
b. Long-chain fatty acids and monoglycerides are absorbed as part of micelles,
resynthesized to triglycerides, and formed into protein-coated spherical masses called chylomicrons.
1) Chylomicrons are taken up by the lacteal of a villus. 2) From the lacteal they enter the lymphatic system and then pass into
the cardiovascular system, finally reaching the liver or adipose tissue.
c. The plasma lipids - fatty acids, triglycerides, cholesterol - are insoluble in water
and body fluids.
1) In order to be transported in blood and utilized by body cells, the lipids
must be combined with protein transporters called lipoproteins to make them soluble.
2) The combination of lipid and protein is referred to as a lipoprotein. 5. Absorption of Electrolytes a. Many of the electrolytes absorbed by the small intestine come from
gastrointestinal secretions and some are part of digested foods and liquids.
b. Active transport mechanisms are primarily used for electrolyte absorption. 6. Absorption of Vitamins a. Fat-soluble vitamins (A, D, E, and K) are included along with ingested dietary
lipids in micelles and are absorbed by simple diffusion.
b. Water-soluble vitamins (B and C) are absorbed by simple diffusion. 7. Absorption of Water a. All water absorption in the GI tract occurs by osmosis from the lumen of the
intestines through epithelial cells and into blood capillaries.
b. The absorption of water depends on the absorption of electrolytes and
nutrients to maintain an osmotic balance with the blood.
c. Alcohol begins to be absorbed in the stomach. The longer alcohol remains in
the stomach, the slower it is absorbed. Blood alcohol levels rise more slowly when fat rich foods are consumed with alcohol (Clinical Application).
XIV. LARGE INTESTINE A. Anatomy of the Large Intestine 1. The large intestine (colon) extends from the ileocecal sphincter to the anus. 2. Its subdivisions include the cecum, colon, rectum, and anal canal. 3. Hanging inferior to the cecum is the appendix. a. Inflammation of the appendix is called appendicitis. (Clinical Application) b. A ruptured appendix can result in gangrene or peritonitis, which can be lifethreatening conditions.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
4. The colon is divided into the ascending, transverse, descending, and sigmoid portions. B. Histology of the Large Intestine 1. The mucosa of the large intestine has no villi or permanent circular folds. It does have a
simple columnar epithelium with numerous globlet cells.
2. The muscularis contains specialized portions of the longitudinal muscles called taeniae
coli, which contract and gather the colon into a series of pouches called haustra.
C. Mechanical movements of the large intestine include haustral churning, peristalsis, and mass
peristalsis.
D. The last stages of chemical digestion occur in the large intestine through bacterial, rather than
enzymatic, action. Substances are further broken down and some vitamins are synthesized by bacterial action and absorbed by the large intestine.
E. Absorption and Feces Formation in the Large Intestine 1. The large intestine absorbs water, electrolytes, and some vitamins. 2. Feces consist of water, inorganic salts, sloughed-off epithelial cells, bacteria, products of
bacterial decomposition, and undigested parts of food.
3. Although most water absorption occurs in the small intestine, the large intestine absorbs
enough to make it an important organ in maintaining the body s water balance.
4. The main diagnostic value of the occult blood test is to screen for colorectal cancer
(Clinical Application).
F. Defecation Reflex 1. The elimination of feces from the rectum is called defecation. 2. Defecation is a reflex action aided by voluntary contractions of the diaphragm and
abdominal muscles. The external anal sphincter can be voluntarily controlled (except in infants) to allow or postpone defecation.
3. Diarrhea refers to frequent defecation of liquid feces. It is caused by increased motility
of the intestine and can lead to dehydration and electrolyte imbalances.
4. Constipation refers to infrequent or difficult defecation and is caused by decreased
motility of the intestines, in which feces remain in the colon for prolonged periods of time. It may be alleviated by increasing one s intake of dietary fiber and fluids.
5. Dietary fiber may be classified as insoluble (does not dissolve in water) and soluble
(dissolves in water). Both types affect the speed of food passage through the GI tract and may produce a number of benefits in the GI tract as well as elsewhere in the body. There is evidence that insoluble fiber may help protect against colon cancer and that soluble fiber may help lower blood cholesterol level. (Clinical Application)
XV. DEVELOPMENT OF THE DIGESTIVE SYSTEM
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
A. The endoderm of the primitive gut forms the epithelium and glands of most of the
gastrointestinal tract.
B. The mesoderm of the primitive gut forms the smooth muscle and connective tissue of the GI
tract.
XVI. AGING AND THE DIGESTIVE TRACT A. General changes associated with aging of the digestive system include decreasing secretory
mechanisms, decreasing motility of the digestive organs, loss of strength and tone of digestive muscular tissue and its supporting structures, changes in neurosecretory feedback, and diminished response to pain and internal sensations.
B. Specific changes include reduced sensitivity to mouth irritations and sores, loss of taste,
periodontal disease, difficulty in swallowing, hiatal hernia, cancer of the esophagus, gastritis, peptic ulcer, gastric cancer, duodenal ulcers, appendicitis, malabsorption, maldigestion, gallbladder problems, cirrhosis, acute pancreatitis, constipation, cancer of the colon or rectum, hemorrhoids, and diverticular disease of the colon.
XVII. DISORDERS: HOMEOSTATIC IMBALANCES A. Dental caries, or tooth decay, is started by acid-producing bacteria that reside in dental plaque,
act on sugars, and demineralize tooth enamel and dentin with acid.
B. Periodontal diseases are characterized by inflammation and degeneration of the gingivae (gums),
alveolar bone, periodontal ligament, and cementum.
C. Peptic ulcers are crater-like lesions that develop in the mucous membrane of the GI tract in areas
exposed to gastric juice. The most common complication of peptic ulcers is bleeding, which can lead to anemia if blood loss is serious. The three well-defined causes of peptic ulcer disease (PUD) are the bacterium Helicobacter pylori; nonsteroidal anti-inflammatory drugs, such as aspirin; and hypersecretion of HCl.
D. Diverticula are saclike outpouchings of the wall of the colon in places where the muscularis has
become weak. The development of diverticula is called diverticulosis. Inflammation within the diverticula, known as diverticulitis, may cause pain, nausea, vomiting, and either constipation or an increased frequency of defecation. High fiber diets help relieve the symptoms.
E. Tumors, both benign and malignant, may occur in any portion of the GI tract. One of the most
common and deadly malignancies is colorectal cancer, second only to lung cancer in males and third after lung and breast cancer in females. Screening for colorectal cancer includes fecal occult blood testing, digital rectal examination, sigmoidoscopy, colonoscopy, and barium enema.
F. Hepatitis is an inflammation of the liver and can be caused by viruses, drugs, and chemicals,
including alcohol.
1. Hepatitis A (infectious hepatitis) is caused by hepatitis A virus and is spread by fecal
contamination. It does not cause lasting liver damage.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
2. Hepatitis B is caused by hepatitis B virus and is spread primarily by sexual contact and
contaminated syringes and transfusion equipment. It can produce cirrhosis and possibly cancer of the liver. Vaccines are available to prevent hepatitis B infection.
3. Hepatitis C is caused by the hepatitis C virus. It is clinically similar to hepatitis B and is
often spread by blood transfusions. It can cause cirrhosis and possibly liver cancer.
4. Hepatitis D is caused by hepatitis D virus. It is transmitted like hepatitis B and, in fact, a
person must be coinfected with hepatitis B before contracting hepatitis D. It results in severe liver damage and has a high fatality rate.
5. Hepatitis E is caused by hepatitis E virus and is spread like hepatitis A. It is responsible
for a very high mortality rate in pregnant women.
G. Anorexia nervosa is a chronic disorder characterized by self-induced weight loss, body-image and
other perceptual disturbances, and physiologic changes that result from nutritional depletion. The disorder is found predominantly in young, single females and may be inherited. Individuals may become emaciated and may ultimately die of starvation or one of its complications. Treatment consists of psychotherapy and dietary regulation. Critical Thinking Questions 1. You have just eaten a sausage and egg sandwich for breakfast. Explain the chemical changes that occur in the sandwich as it passes through the parts of the GI tract. Be sure to name all enzymes or secretions involved and their source. 2. Assume that you have radioactively labeled an amino acid in a glass of milk. Also assume that you have all of the necessary instruments to follow the course of the amino acid throughout the body. Describe the path that would be taken by the amino acid from the mouth to the aorta. In your response, be sure to indicate how the amino acid moves from one area to the next.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
FLUID, ELECTROLYTE, AND ACID-BASE HOMEOSTASIS
I. INTRODUCTION
A. Body fluid refers to body water and its dissolved substances. B. Regulatory mechanisms insure homeostasis of body fluids since their malfunction may seriously
endanger nervous system and organ functioning. II. FLUID COMPARTMENTS AND FLUID BALANCE
A. Introduction 1. In lean adults body fluids comprise about 55-60% of total body weight. 2. Water is the main component of all body fluids. 3. About two-thirds of the body s fluid is located in cells and is called intracellular fluid
(ICF).
4. The other third is called extracellular fluid (ECF). a. About 80% of the ECF is interstitial fluid and 20% is blood plasma. b. Some of the interstitial fluid is localized in specific places, such as lymph;
cerebrospinal fluid; gastrointestinal tract fluids; synovial fluid; fluids of the eyes (aqueous humor and vitreous body) and ears (endolymph and perilymph); pleural, pericardial, and peritoneal fluids between serous membranes; and glomerular filtrate in the kidneys.
5. Selectively permeable membranes separate body fluids into distinct compartments.
Plasma membranes of individual cells separate intracellular fluid from interstitial fluid. Blood vessel walls divide interstitial fluid from blood plasma. Although fluids are in constant motion from one compartment to another, the volume of fluid in each compartment remains fairly stable another example of homeostasis.
6. Fluid balance means that the various body compartments contain the required amount
of water, proportioned according to their needs.
a. Osmosis is the primary way in which water moves in and out of body
compartments. The concentrations of solutes in the fluids is therefore a major determinant of fluid balance.
b. Most solutes in body fluids are electrolytes, compounds that dissociate into
ions.
c. Fluid balance, then, means water balance, but also implies electrolyte balance;
the two are inseparable.
B. Sources of Body Water Gain and Loss 1. Water is the largest single constituent in the body, varying from 45% to 75% of body
weight, depending on age and the amount of fat present.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
2. Fluid intake (gain) normally equals fluid output (loss), so the body maintains a constant
volume.
C. Regulation of Water Gain 1. Metabolic water volume depends mostly on the level of aerobic cellular respiration,
which reflects the demand for ATP in body cells.
2. The main way to regulate body water balance is by adjusting the volume of water intake. 3. When water loss is greater than water gain, dehydration occurs. 4. The stimulus for fluid intake (gain) is dehydration resulting in thirst sensations; one
mechanism for stimulating the thirst center in the hypothalamus is the renin-angiotensin II pathway, which responds to decreased blood volume (therefore, decreased blood pressure).
D. Regulation of Water and Solute Loss 1. Although increased amounts of water and solutes are lost through sweating and
exhalation during exercise, loss of body water or excess solutes depends mainly on regulating how much is lost in the urine
2. Under normal conditions, fluid output (loss) is adjusted by antidiuretic hormone (ADH),
atrial natriuretic peptide (ANP), and aldosterone, all of which regulate urine production.
E. Movement of Water Between Body Fluid Compartments 1. A fluid imbalance between the intracellular and interstitial fluids can be caused by a
change in their osmolarity.
2. Most often a change in osmolarity is due to a change in the concentration of Na+. 3. When water is consumed faster than the kidneys can excrete it, water intoxication may
result.
4. Repeated use of enemas can increase the risk of fluid and electrolyte imbalances.
(Clinical Application)
III. ELECTROLYTES IN BODY FLUIDS A. Electrolytes serve four general functions in the body. 1. Because they are more numerous than nonelectrolytes, electrolytes control the osmosis
of water between body compartments.
2. They help maintain the acid-base balance required for normal cellular activities. 3. They carry electrical current, which allows production of action potentials and graded
potentials and controls secretion of some hormones and neurotransmitters. Electrical currents are also important during development.
4. Several ions are cofactors needed for optimal activity of enzymes. B. Concentrations of Electrolytes in Body Fluids
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
1. To compare the charge carried by ions in different solutions, the concentration is
typically expressed in milliequivalents/liter (mEg/Liter), which gives the concentration of cations or anions in a solution.
2. The chief difference between plasma and interstitial fluid is that plasma contains quite a
few protein anions, where interstitial fluid has hardly any since plasma proteins generally cannot move out of impermeable blood vessel walls. Plasma also contains slightly more sodium ions but fewer chloride ions than the interstitial fluid. In other respects, the two fluids are similar.
3. Intracellular fluid (ICF) differs considerably from extracellular fluid (ECF), however. C. Sodium (Na+) is the most abundant extracellular ion. 1. It is involved in impulse transmission, muscle contraction, and participates in fluid and
electrolyte balance by creating most of the osmotic pressure of extracellular fluid.
2. The average daily intake of sodium far exceeds the body s normal daily requirements.
The kidneys excrete excess sodium and conserve it during periods of sodium restriction.
3. Its level in the blood is controlled by aldosterone, antidiuretic hormone, and atrial
natriuretic peptide.
4. Excess Na+ in the body can result in edema. Excess loss of Na+ causes excessive loss of
water, which results in hypovolemia, an abnormally low blood volume. (Clinical Application)
D. Chloride (Cl-) is the major extracellular anion. 1. It plays a role in regulating osmotic pressure between compartments and forming HCl in
the stomach.
2. Regulation of Cl- balance in body fluids is indirectly controlled by aldosterone.
Aldosterone regulate sodium reabsorption; the negatively charged chloride follows the positively charged sodium passively by electrical attraction.
E. Potassium (K+) is the most abundant cation in intracellular fluid. 1. It is involved in maintaining fluid volume, impulse conduction, muscle contraction, and
regulating pH.
2. The plasma level of K+ is under the control of mineralocorticoids, mainly aldosterone. F. Bicarbonate (HCO3-) is a prominent ion in the plasma. 1. It is a significant plasma anion in electrolyte balance. 2. It is a major component of the plasma acid-base buffer system. 3. The kidney reabsorbs or secretes bicarbonate to make the final balance for acid-base
conditions.
G. Calcium (Ca+2), the most abundant ion in the body, is principally an extracellular ion.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
1. It is a structural component of bones and teeth. It also functions in blood coagulation,
neurotransmitter release, maintenance of muscle tone, and excitability of nervous and muscle tissue.
2. The level of calcium in plasma is regulated principally by parathyroid hormone and
calcitonin.
H. Magnesium (Mg+2) is primarily an intracellular cation. 1. It activates several enzyme systems involved in the metabolism of carbohydrates and
proteins and is needed for operation of the sodium pump. It is also important in neuromuscular activity, neural transmission within the central nervous system, and myocardial functioning.
2. Several factors regulate magnesium ion concentration in plasma. They include hypo- or
hypercalcemia, hypo- or hypermagnesemia, an increase or decrease in extracellular fluid volume, an increase or decrease in parathyroid hormone, and acidosis or alkalosis.
J. Individuals at risk for fluid and electrolyte imbalances include those dependent on others for fluid
and food needs; those undergoing medical treatment involving intravenous infusions, drainage or suction, and urinary catheters, those receiving diuretics, and post-operative individuals, burned individuals, individuals with chronic disease, and those with altered states of consciousness. (Clinical Application)
IV. ACID-BASE BALANCE A. The overall acid-base balance of the body is maintained by controlling the H+ concentration of
body fluids, especially extracellular fluid.
1. The normal pH of extracellular fluid is 7.35-7.45. 2. Homeostasis of pH is maintained by buffer systems, exhalation of carbon dioxide, and
kidney excretion.
B. The Actions of Buffer Systems 1. Most buffer systems of the body consist of a weak acid and the salt of that acid (which
functions as a weak base); together they function to prevent rapid, drastic changes in the pH of a body fluid by changing strong acids and bases into weak acids and bases. Buffers work within fractions of a second.
2. The important buffer systems include the protein system, the carbonic acid-bicarbonate
system, and the phosphate system.
a. The protein buffer system is the most abundant buffer in body cells and plasma.
Inside red blood cells the protein hemoglobin is an especially good buffer for carbonic acid.
b. The carbonic acid-bicarbonate buffer system is an important regulator of blood
pH and is based on the bicarbonate ion.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
c. The phosphate buffer system is an important regulator of pH, both in red blood
cells and in the kidney tubular fluids.
C. Exhalation of Carbon Dioxide 1. The pH of body fluids may be adjusted by a change in the rate and depth of respirations,
which usually takes from 1 to 3 minutes.
a. An increase in the rate and depth of breathing causes more carbon dioxide to
be exhaled, thereby increasing pH.
b. A decrease in respiration rate and depth means that less carbon dioxide is
exhaled, causing the blood pH to fall.
2. The pH of body fluids, in turn, affects the rate of breathing. D. The kidneys excrete H+ and reabsorb HCO3- to aid in maintaining pH. 1. Cells in the PCT and collecting ducts secrete hydorgen ions into the tubular fluid. 2. In the PCT Na+/H+ antiporters secrete H+ and reabsorb Na+ . 3. The apical surfaces of some intercalated cells include proton pumps (H+ ATPases) that
secrete H+ into the tubular fluid and HCO3 antiporters in their basolateral membranes to reabsorb HCO3 (Figure 27.8).
4. Other intercalated cells have proton pumps in their basolateral membranes and Cl
/HCO3 antiporters in their apical membranes.
5. These two types of cells help maintain body fluid pH by excreting excess H+ when pH is
too low or by excreting excess HCO3 when the pH is too high.
E. Acid-Base Imbalances 1. The normal pH range of systemic arterial blood is between 7.35-7.45. a. Acidosis is a blood pH below 7.35. Its principal effect is depression of the central
nervous system through depression of synaptic transmission.
b. Alkalosis is a blood pH above 7.45. Its principal effect is overexcitability of the
central nervous system through facilitation of synaptic transmission.
c. A change in blood pH that leads to acidosis or alkalosis can be compensated to
return pH to normal. Compensation refers to the physiological response to an acid-base imbalance.
d. Respiratory acidosis and respiratory alkalosis are primary disorders of blood
PCO2. On the other hand, metabolic acidosis and metabolic alkalosis are primary disorders of bicarbonate concentration.
2. Respiratory acidosis is characterized by an elevated PCO2 and decreased pH and is caused
by hypoventilation or other causes of reduced gas exchange in the lungs.
3. Respiratory alkalosis is characterized by a decreased arterial blood PCO2 and increased pH
and is caused by hyperventilation.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
4. Metabolic acidosis is characterized by a decreased bicarbonate level and decreased pH,
and results from an abnormal increase in acid metabolic products (other than CO2), loss of bicarbonate, or failure of the kidneys to excrete H ions derived from metabolism of dietary proteins
+
5. Metabolic alkalosis is characterized by increased bicarbonate concentration and results
from nonrespiratory loss of acid (e.g., excessive vomiting) or excess intake of alkaline drugs.
G. Diagnosis of acid-base imbalances employs a general four-step process. 1. Note whether the pH is high or low relative to the normal range. 2. Decide which value of PCO2 or HCO3- could cause the abnormality. 3. Specify the problem source as respiratory or metabolic. 4. Look at the noncausative value and determine if it is compensating for the problem. V. AGING AND FLUID, ELECTROLYTE, AND ACID-BASE HOMEOSTASIS
A. Infants experience more problems than adults with respect to fluid distribution, regulation of fluid and electrolyte balance, and acid-base homeostasis. B. The differences are related to proportion and distribution of water, metabolic rate, functional development of the kidneys, body surface area, breathing rate, and ion concentration. C. Older adults often have impaired ability to maintain fluid, electrolyte, and acid-base balance due to declining skeletal muscle mass and increasing mass of adipose tissue (which includes very little water), age-related respiratory and renal diseases, and both sensible and insensible water loss from the skin. Older adults are susceptible to dehydration and hypernatremia, hyponatremia, hypokalemia, and acidosis.
Critical Thinking Questions 1. You are planning to complete in a 10K run. You notice that along the route of the run are designated water stops. Explain why it would be in your best interest to take advantage of the water made available to you during the run. 2. Your 2-month-old baby has been suffering from diarrhea for several hours. Should you be concerned about dehydration or not? Give reasons for your answer.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
THE REPRODUCTIVE SYSTEMS
I. INTRODUCTION A. Sexual reproduction is a process in which organisms produce offspring by means of germ cells called gametes. B. The organs of reproduction are grouped as gonads (produce gametes and secrete hormones), ducts (transport, receive, and store gametes), and accessory sex glands (produce materials that support gametes). C. Gynecology is the specialized branch of medicine concerned with the diagnosis and treatment of diseases of the female reproductive system. Urology is the study of the urinary system but also includes diagnosis and treatment of diseases and disorders of the male reproductive system. II. THE CELL CYCLE IN THE GONADS A. The cell cycle in the gonads produces gametes by a special type of nuclear division called meiosis that reduces the number of chromosomes by one half. B. Chromosomes in Gametes 1. 2. A gamete has only 23 chromosomes, one member of each chromosome pair. The two chromosomes that make up a chromosome pair are called homologous chromosomes or homologs. a. They contain similar genes arranged in the same or almost the same order and look very similar. b. The exception is the sex chromosomes. The female contains two X chromosomes; and the male, an X and a Y chromosome. c. 3. The other 22 pairs of chromosomes are called autosomes.
A cell with a full set of chromosomes is called a diploid cell. One with only one chromosome from each pair is termed haploid.
C. Meiosis 1. Meiosis results in the production of haploid cells that contain only 23 chromosomes. 2. Meiosis I a. Meiosis I consists of four phases: prophase I, metaphase I, anaphase I, and
telophase I.
1) During prophase I, the chromosomes become arranged in homologous
pairs.
2) During metaphase I, the homologous pairs of chromosomes line up
along the metaphase plate of the cell, with the homologous chromosomes side by side.
3) During anaphase I, the members of each homologous pair separate,
with one member of each pair moving to an opposite pole of the cell.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
4) Telophase I and cytokinesis are similar to telophase and cytokinesis of
mitosis.
b. During prophase I, the two chromatids of each pair of homologous
chromosomes pair off, an event called synapsis. The resulting four chromatids form a tetrad. Portions of one chromatid may be exchanged with portions of another, an event called crossing-over.
1) This process permits an exchange of genes among homologous
chromosomes.
2) It results in genetic recombination, the formation of new combinations
of genes.
3. Meiosis II a. Meiosis II consists of prophase II, metaphase II, anaphase II, and telophase II. b. These phases are similar to those in mitosis, but result in four haploid cells. III. MALE REPRODUCTIVE SYSTEM A. The male structures of reproduction include the testes, a system of ducts (ductus epididymis,
ductus deferens, ejaculatory duct, urethra), accessory sex glands (seminal vesicles, prostate gland, bulbourethral glands), and several supporting structures, including the penis.
B. Scrotum 1. The scrotum is a cutaneous outpouching of the abdomen that supports the testes;
internally, a vertical septum divides it into two sacs, each containing a single testis.
2. The reproduction and survival of spermatozoa require a temperature that is lower than
normal core body temperature. The temperature of the testes is regulated by the cremaster muscle, which elevates them and brings them closer to the pelvic cavity or relaxes, causing the testes to move farther from the pelvic cavity.
C. Testes 1. The testes, or testicles, are paired oval-shaped glands (gonads) in the scrotum. a. The testes develop high on the embryo s posterior abdominal wall and usually
begin their descent into the scrotum through the inguinal canals during the latter half of the seventh month of fetal development.
b. The testes contain seminiferous tubules (in which sperm cells are made). c. Embedded among the spermatogenic cells in the tubules are large Sertoli cells
or sustentacular cells.
1) The tight junctions of these cells form the blood-testis barrier that
prevents an immune response against the surface antigens on the spermatogenic cells.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
2) The sustentacular cells also nourish spermatocytes, spermatids, and
spermatozoa; mediate the effects of testosterone and follicle stimulating hormone on spermatogenesis; phagocytose excess spermatids cytoplasm as development proceeds; control movements of spermatogenic cells and the release of spermatozoa into the lumen of the seminiferous tubule; and secrete fluid for sperm transport and the hormone inhibin.
d. The Leydig cells or interstitial endocrinocytes found in the spaces between
adjacent seminiferous tubules secrete testosterone.
e. Failure of the testes to descend is called cryptorchidism, involving one or both
testes. (Clinical Application)
2. Spermatogenesis is the process by which the seminiferous tubules of the testes produce
haploid sperm.
a. It begins in the diploid spermatogia (stem cells). They undergo mitosis to
reserve future stem cells and to develop cells (2n primary spermatocytes) for sperm production.
b. The diploid primary spermatocytes undergo meiosis I forming haploid
secondary spermatocytes.
c. Meiosis II results in the formation of the haploid spermatids. The spermatids
are connected by cytoplasmic bridges.
d. The final stage of spermatogenesis is spermiogenesis which is the maturation of
the spermatids into sperm.
e. The release of a sperm from its connection to a Sertoli cell is known as
spermiation.
3. Mature sperm consist of a head, midpiece, and tail. They are produced at the rate of
about 300 million per day and, once ejaculated, have a life expectancy of 48 hours within the female reproductive tract. Their function is to fertilize a secondary oocyte.
4. Hormonal Control of spermatogenesis a. At puberty, gonadotropin releasing hormone stimulates anterior pituitary
secretion of follicle-stimulating hormone (FSH) and luteinizing hormone (LH). FHS initiates spermatogenesis, and LH assists spermatogenesis and stimulates production of testosterone.
b. Testosterone controls the growth, development, functioning, and maintenance
of sex organs; stimulates bone growth, protein anabolism, and sperm maturation; and stimulates development of male secondary sex characteristics. Negative feedback systems regulate testosterone production.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
c. Inhibin is produced by sustentacular (Sertoli) cells. Inhibition of FSH by inhibin
helps to regulate the rate of spermatogenesis.
D. Reproductive System Ducts in Males 1. The duct system of the testes includes the seminiferous tubules, straight tubules, and
rete testis.
2. Epididymis a. The epididymis is a comma-shaped organ that lies along the posterior border of
the testis.
b. Sperm are transported out of the testes through the efferent ducts in the
epididymis which empty into a single tube called the ductus epididymis.
c. The ductus epididymis is lined by stereocilia and is the site of sperm maturation
and storage; sperm may remain in storage here for at least a month, after which they are either expelled or degenerated and reabsorbed.
3. Ductus Deferens a. The ductus (vas) deferens, or seminal duct, stores sperm and propels them
toward the urethra during ejaculation.
b. The spermatic cord is a supporting structure of the male reproductive system,
consisting of the ductus deferens, the testicular artery, autonomic nerves, veins that drain the testes, lymphatic vessels, and the cremaster muscle.
c. The inguinal canal represents a weak spot in the abdominal wall. It is frequently
the site of an inguinal hernia - a rupture or separation of a portion of the abdominal wall resulting in the protrusion of a part of an organ (most commonly the small or large intestine). Since the inguinal canal is smaller in females, women have inguinal hernias much less often. (Clinical Application)
4. The ejaculatory ducts are formed by the union of the ducts from the seminal vesicles and
ducti deferens; their function is to eject spermatozoa into the prostatic urethra.
5. The male urethra is the shared terminal duct of the reproductive and urinary systems
which serves as a passageway for semen and urine. The male urethra is subdivided into three portions: prostatic, membranous, and spongy (cavernous).
E. Accessory Sex Glands 1. The seminal vesicles secrete an alkaline, viscous fluid that contains fructose,
prostaglandins, and clotting proteins.
a. The alkaline nature of the fluid helps to neutralize acid in the male urethra and
female reproductive tract.
b. The fructose is for ATP production by sperm. c. Prostaglandins contribute to sperm motility and viability.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
d. Semenogelin is the main protein that causes coagulation of semen after
ejaculation.
2. The prostate gland (Figure 28.11) secretes a milky, slightly acidic fluid that contains: (1)
citric acid, which can be used by sperm for ATP production; (2) acid phosphatase; and (3) several proteolytic enzymes, such as prostate-specific antigen (PSA), pepsinogen, lysozyme, amylase, and hyaluronidase which liquefy coagulated semen.
3. The bulbourethral (Cowper s) glands secrete mucus for lubrication and an alkaline
substance that neutralizes acid.
F. Semen (seminal fluid) is a mixture of spermatozoa and accessory sex gland secretions that
provides the fluid in which spermatozoa are transported, provides nutrients, and neutralizes the acidity of the male urethra and female vagina.
1. Semen contains an antibiotic, seminal plasmin, and prostatic enzymes that coagulate
and then liquefy semen to aid in its movement through the uterine cervix.
2. Once ejaculated, liquid semen coagulates within 5 minutes due to the presence of
clotting proteins from the seminal vesicles.
3. After about 10-20 minutes, semen reliquifies because PSA and other proteolytic
enzymes produced by the prostate gland break down the clot.
G. Penis 1. The penis is the male organ of copulation that consists of a root, body, and glans penis. It
is used to introduce spermatozoa into the vagina.
2. Expansion of its blood sinuses under the influence of sexual excitation is called erection;
ejaculation, propulsion of semen from the urethra to the exterior, is a sympathetic reflex.
3. Covering the glans penis is the loosely fitting prepuce, or foreskin. Circumcision is a
surgical procedure in which part of the entire prepuce is removed (for either religious or hygienic reasons). There is no consensus among physicians regarding the need for circumcision or the use of anesthesia during the procedure (Clinical Application).
IV. FEMALE REPRODUCTION SYSTEM A. The female organs of reproduction include the ovaries (gonads), uterine (Fallopian) tubes, uterus,
vagina, vulva, and mammary glands.
B. Ovaries 1. The ovaries are paired glands that are homologous to the testes. 2. The ovaries are located in the upper pelvic cavity, on either side of the uterus. They are
maintained in position by a series of ligaments.
3. The histology of the ovary
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
a. The germinal epithelium covers the surface of the ovary but does not give rise
to ova. It is followed by the tunica albuginea, ovarian cortex (contains ovarian follicles), and ovarian medulla (contains blood vessels, lymphatics, and nerves).
b. Ovarian follicles lie in the cortex and consist of oocytes in various stages of
development.
c. A mature (Graafian) follicle expels a secondary oocyte by a process called
ovulation.
d. A corpus luteum contains the remnants of an ovulated follicle and produces
progesterone, estrogens, relaxin, and inhibin until it degenerates into a corpus albicans.
4. Oogenesis and follicular development a. Oogenesis occurs in the ovaries. It results in the formation of a single haploid
secondary oocyte.
b. The oogenesis sequence includes reduction division (meiosis I), equatorial
division (meiosis II), and maturation.
c. While oogenesis is occurring, the follicle cells surrounding the oocyte are also
undergoing developmental changes. The sequence of follicular cell changes is: primordial, primary, secondary, and mature (Graffian) follicles, and corpus luteum and corpus albicans.
C. Uterine Tube 1. The uterine (Fallopian) tubes transport ova from the ovaries to the uterus and are the
normal sites of fertilization.
2. Histologically the uterine tubes are composed of three layers: the internal mucosa, the
middle muscularis, and the outer serosa.
3. Ciliated cells and peristaltic contractions help move a secondary oocyte toward the
uterus.
D. Uterus 1. The uterus (womb) is an organ the size and shape of an inverted pear that functions in
the transport of spermatozoa, menstruation, implantation of a fertilized ovum, development of a fetus during pregnancy, and labor.
2. Anatomical subdivisions of the uterus include the fundus, body, isthmus, and cervix. 3. The uterus is normally held in position by a series of ligaments. 4. Uterine prolapse is a downward displacement of the uterus. It has many causes and
may be characterized as first degree (mild), second degree (marked), or third degree (complete). The treatment depends on the degree of prolapse (Clinical Application).
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
5. Histologically, the uterus consists of an outer promethium, middle myometrium, and
inner endometrium.
a. The myometrium consists of three muscle layers. b. The endometrium is divided into the stratum functionalis (shed during
menstruation) and the stratum basalis (gives rise to a new stratum functionalis after each menstruation).
6. Blood is supplied to the uterus by the uterine arteries and their numerous branches and
is drained by the uterine veins.
7. Secretory cells of the mucosa of the cervix produce a cervical mucus (a mixture of water,
glycoprotein, serum-type proteins, lipids, enzymes, and inorganic salts) which, when thin, is more receptive to sperm and which, when thick, forms a cervical plug that physically impedes sperm penetration.
a. The cervical mucus supplements the energy needs of the sperm. b. Both the cervix and the mucus serve as a sperm reservoir, protect sperm from
the hostile environment of the vagina, and protect sperm from phagocytes.
c. The cervix and the mucus also play a role in capacitation. 8. Hysterectomy refers to surgical removal of the uterus and is the most common
gynecological operation (Clinical Application).
E. Vagina 1. The vagina functions as a passageway for spermatozoa and the menstrual flow, the
receptacle of the penis during sexual intercourse, and the lower portion of the birth canal.
2. The mucosa of the vagina is continuous with that of the uterus and lies in a series of
transverse folds called rugae.
a. Mucosa dendritic cells are APCs (antigen-presenting cells) that participate in the
transmission of viruses, such as HIV, to a female during intercourse with an infected male.
b. The mucosa contains large stores of glycogen which decompose into organic
acids which set up a hostile acid environment for sperm. Alkaline components of semen neutralize the acidity and increase sperm viability.
3. The vaginal orifice is often partially covered by a thin fold of vascularized mucous
membrane called the hymen. If the orifice is completely covered, this imperforate hymen must be surgically opened to permit menstrual flow.
F. Vulva 1. The term vulva, or pudendum, refers to the external genitalia of the female.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
2. It consists of the mons pubs, labia majora, labia minora, clitoris, vestibule, vaginal and
urethral orifices, hymen, bulb of the vestibule, and the paraurethral (Skene s), greater vestibular (Bartholin s), and lesser vestibular glands.
G. Perineum
1. The perineum is the diamond-shaped area between the thighs and buttocks of both males and females that contains the external genitals and anus. 2. During childbirth the emerging fetus may cause excessive stretching and tearing of the perineum. A physician may make a surgical incision (episiotomy) in this region to prevent excessive, jagged tears (Clinical Application).
H. Mammary Glands 1. The mammary glands are modified sudoriferous (sweat) glands that lie over the
pectoralis major and serratus anterior muscles.
2. Milk-secreting cells, referred to as alveoli, are clustered in small compartments (lobules)
within the breasts.
3. The essential functions of the mammary glands are synthesis of milk, secretion and
ejection of milk, which constitute lactation.
4. Fibrocystic disease is the most common cause of a breast lump in which one or more
cysts (fluid-filled sacs) and thickening of alveoli (clusters of milk-secreting cells) develop. (Clinical Application)
V. FEMALE REPRODUCTIVE CYCLE A. The general term female reproductive cycle encompasses the ovarian and uterine cycles, the
hormonal changes that regulate them, and cyclical changes in the breasts and the cervix.
1. The ovarian cycle is a series of events associated with the maturation of an ovum. 2. The uterine (menstrual) cycle involves changes in the endometrium to prepare for the
reception of a fertilized ovum.
B. Hormonal Regulation of the Female Reproductive Cycle 1. The menstrual and ovarian cycles are controlled by GnRH from the hypothalamus, which
stimulates the release of FSH and LH by the anterior pituitary gland.
a. FSH stimulates the initial development of ovarian follicles and secretion of
estrogens by the ovaries.
b. LH stimulates further development of ovarian follicles, ovulation, and the
secretion of estrogens and progesterone by the ovaries.
2. At least six different estrogens have been isolated from the plasma of human females,
with three in significant quantities: beta-estradiol, estrone, and estriol.
a. Estrogens have several important functions:
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
1) Promotion of the development and maintenance of female
reproductive structures, secondary sex characteristics, and the breasts.
2) Increase protein anabolism and build strong bones. 3) Lower blood cholesterol. b. Moderate levels of estrogens in the blood inhibit the release of GnRH by the
hypothalamus and secretion of LH and FSH by the anterior pituitary gland.
3. Progesterone works with estrogens to prepare the endometrium for implantation and
the mammary glands for milk synthesis.
4. A small quantity of relaxin is produced monthly to relax the uterus by inhibiting
contractions (making it easier for a fertilized ovum to implant in the uterus). During pregnancy, relaxin relaxes the pubic symphysis and helps dilate the uterine cervix to facilitate delivery.
5. Inhibin inhibits secretion of FHS and GnRH and, to a lesser extent, LH. It might be
important in decreasing secretion of FHS and LH toward the end of the uterine cycle.
C. Phases of the Female Reproductive Cycle 1. The female reproductive cycle may be divided into four phases. a. The menstrual cycle (menstruation) lasts for approximately the first 5 days of
the cycle.
1) During this phase, small secondary follicles in each ovary begin to
develop.
2) Also during this phase, the stratum functionalis layer of the
endometrium is shed, discharging blood, tissue fluid, mucus, and epithelial cells.
b. The preovulatory phase, or proliferative phase, is the time between
menstruation and ovulation. This phase is more variable in length that the other phases, lasting from days 6-13 in a 28-day cycle.
1) During this phase, primary follicles develop into secondary follicles and
a single secondary follicle (occasionally more than one) develops into a vesicular ovarian (Graafian) follicle, or mature follicle. This follicle produces a bulge on the surface of the ovary.
2) The dominant follicle continues to increase its estrogen production
under the influence of an increasing level of LH
3) During this phase, endometrial repair occurs. c. Ovulation is the rupture of the vesicular ovarian (Graafian) follicle with release
of the secondary oocyte into the pelvic cavity, usually occurring on day 14 in a 28-day cycle.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
1) The high levels of estrogen during the last part of the preovulatory
phase exert a positive feedback on both LH and GnRH to cause ovulation.
a) GnRH promotes release of FHS and more LH by the anterior
pituitary gland.
b) The LH surge brings about the ovulation. 2) Following ovulation, the vesicular ovarian follicle collapses (and blood
within it forms a clot) to become the corpus hemorrhagicum. The clot is eventually absorbed by the remaining follicle cells. In time, the follicular cells enlarge, change character, and form the corpus luteum, or yellow body, under the influence of LH. Stimulated by LH, the corpus luteum secretes estrogens and progesterone.
d. The postovulatory phase is the most constant in duration and lasts from days
15-28 in a 28-day cycle, the time between ovulation and onset of the next menstrual period.
1) With reference to the ovaries, this phase of the cycle is also called the
luteal phase, during which both estrogen and progesterone are secreted in large quantities by the corpus luteum.
A) If fertilization and implantation do not occur, the corpus
luteum degenerates and becomes the corpus albicans, or white body. The decreased secretion of progesterone and estrogens then initiates another menstrual phase (uterine and ovarian cycle).
b) If fertilization and implantation do occur, the corpus luteum is
maintained until the placenta takes over its hormoneproducing function. During this time, the corpus luteum, maintained by human chorionic gonadotropin (hCG) from the developing placenta, secretes estrogens and progesterone to support pregnancy and breast development for lactation. Once the placenta begins its secretion, the role of the corpus luteum becomes minor.
2) With reference to the uterus, this phase is also called the secretory
phase because of the secretory activity of the endometrial glands as the endometrium thickens in anticipation of implantation.
2. Women athletes who train intensively may develop three conditions which disrupt their
reproductive cycle. This is known as female athlete triad and consists of amenorrhea, disordered eating, and premature osteoporosis (Clinical Application)
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
VI. THE HUMAN SEXUAL RESPONSE A. Sexual intercourse, or copulation (in humans, called coitus), is the process by which spermatozoa
are deposed in the vagina.
B. The four stages of human sexual response are related to the physical and physiological states that
occur to both men and women during sexual intercourse.
1. In the arousal phase parasympathetic impulses pass through the sacral region to cause
vasocongestion and secretion by the genitalia.
a. Arousal is in response to mental and tactile stimulation. b. There is also increased activity in the cardiovascular, respiratory, and muscular
systems.
2. The plateau stage is characterized by a sexual flush due to cutaneous vasodilation. 3. Sympathetic nervous stimulation of the whole body leads to the orgasm stage,
accompanied by an intense sensation of pleasure, in addition to rhythmic somatic and smooth muscle contractions.
4. The resolution stage occurs as the aroused systems relax. C. The changes of the male in the sex act involve erection, minimal lubrication, and ejaculation, a
component of orgasm.
D. The female changes also involve erection, lubrication, and orgasm (climax). E. Erectile dysfunction, previously termed impotence, is the consistent inability of an adult male to
ejaculate or to attain or hold an erection long enough for sexual intercourse (Clinical Application).
VII. BIRTH CONTROL METHODS A. Several methods of birth control are available, each with advantages and disadvantages. B. The only method of preventing pregnancy that is 100% reliable is total abstinence, avoidance of
sexual intercourse.
C. Methods of birth control discussed in the text include surgical sterilization (vasectomy, tubal
ligation), hormonal methods (oral contraception, the Norplant implant, Depo-Provera injection, the vaginal ring), intrauterine devices (IUDs), spermacides, barrier methods (condom, vaginal pouch, diaphragm, cervical cap), periodic abstinence (rhythm method, sympto-thermal method), coitus interruptus (withdrawal), and induced abortion (including the drug RU 486, or mifepristone).
D. A summary of methods of birth control is presented in Table 28.3. VIII. DEVELOPMENT OF THE REPRODUCTIVE SYSTEMS A. The gonads develop from intermediate mesoderm and are differentiated into ovaries or testes by
about the seventh week of fetal development
B. The external genitalia develop from the genital tubercle
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
C. Deficiency of 5-alpha-reductase results in a female external appearance at birth, but the
development of male characteristics at puberty. (Clinical Application)
IX. AGING AND THE REPRODUCTIVE SYSTEMS A. Puberty refers to the period of time when secondary sexual characteristics begin to develop and
the potential for sexual reproduction is reached.
B. In females, the reproductive cycle normally occurs once each month from menarche, the first
menses, to menopause, the last menses.
1. Between the ages of 40 and 50 the ovaries become less responsive to the stimulation of
gonadotropic hormones from the anterior pituitary. As a result, estrogen and progesterone production decline, and follicles do not undergo normal development.
2. In addition to the symptoms of menopause, such as hot flashes, copious sweating,
headache, vaginal dryness, depression, weight gain, and emotional fluctuations, with age females also experience increased incidence of osteoporosis, uterine cancer, and breast cancer.
C. In males, declining reproduction function is more subtle, with males often retaining reproductive
capacity into their 80s or 90s.
1. In males, decreasing levels of testosterone decrease muscle strength, sexual desire, and
viable sperm.
2. Prostate disorders are increasingly common with age, particularly benign hypertrophy. X. DISORDERS: HOMEOSTATIC IMBALANCES A. Reproductive System Disorders in Males 1. Testicular cancer originates in the sperm-producing cells. a. It occurs most commonly in young men between the ages of 15 and 34. b. An early sign is a mass in the testis, often associated with pain or discomfort. All
males should perform regular testicular self-exams.
2. Prostate Disorders a. In acute prostatitis, the prostate gland becomes swollen and tender. b. In chronic prostatitis, one of the most common chronic infections in men of the
middle and later years, the gland feels enlarged, soft, and very tender with an irregular surface outline.
c. Prostate cancer is the leading cause of cancer deaths in men in the United
States.
1) A blood test can measure the level of prostate-specific antigen (PSA) in
the blood.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
2) The amount of PSA increases with the enlargement of the prostate
gland and may indicate infection, benign enlargement, or prostate cancer.
3) Treatment for prostate cancer may involve surgery, radiation,
hormonal therapy, or chemotherapy.
B. Reproductive System Disorders in Females 1. Premenstrual syndrome (PMS) refers to severe physical and emotional distress that
occurs during the postovulatory (luteal) phase of the female reproductive cycle.
2. Endometriosis is characterized by the growth of endometrial tissue outside the uterus. a. The tissue enters the pelvic cavity via the open uterine tubes and may be found
in any of several sites - on ovaries, rectouterine pouch, surface of the uterus, sigmoid colon, pelvic and abdominal lymph nodes, cervix, abdominal wall, kidneys, and/or urinary bladder.
b. Symptoms include premenstrual pain or unusual menstrual pain. 3. Breast cancer is the second-leading cause of death from cancer in United States women. a. It is seldom seen before age 30, but its occurrence rises rapidly after
menopause.
b. Two genes increase susceptibility to breast cancer: BRCA1 (breast cancer 1) and
BRCA2. Mutation of BRCA1 also confers high risk for ovarian cancer.
c. Early detection - especially by breast self-examination and mammography - is
still the most promising method to increase the survival rate for breast cancer.
d. The factors that increase the risk of breast cancer development include family
history of breast cancer, especially in a mother or sister; never having a child or having a first child after age 35; previous cancer in one breast; exposure to ionizing radiation, such as x-rays; excessive alcohol intake; and cigarette smoking.
e. Treatment for breast cancer may involve hormone therapy, chemotherapy,
radiation therapy, lumpectomy (removal of just the tumor and immediate surrounding tissue), a modified or radical mastectomy (removal of part or all of the affected breast, along with underlying pectoral muscles and the axillary lymph nodes in the latter case), or a combination of these. Radiation treatment and chemotherapy may follow the surgery.
4. Ovarian cancer is the sixth most common form of cancer in females. a. It is difficult to detect before it metastasizes beyond the ovaries. b. Risk factors include age (usually over age 50); race (white are at greatest risk);
family history of ovarian cancer; never having children or first pregnancy after
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
age 30; high-fat, low-fiber, vitamin A-deficient diet; and prolonged exposure to asbestos or talc.
c. Early ovarian cancer has no symptoms or only mild ones associated with other
common problems.
d. Later-stage signs and symptoms include an enlarged abdomen, abdominal
and/or pelvic pain, persistent gastrointestinal disturbances, urinary complications, menstrual irregularities, and heavy menstrual bleeding.
5. Cervical cancer starts with cervical dysplasia and can be diagnosed in its earliest stages
with a Pap smear.
a. There is some evidence linking cervical cancer to the virus that produces genital
warts (papilloma virus).
b. Other risk factors are increased incidence associated with an increased number
of sexual partners, young age at first intercourse, and cigarette smoking.
6. Vulvovaginal candidiasis is the most common form of vaginitis and is caused by the yeast
like fungus Candida albicans.
a. Candidiasis is characterized by severe itching; a thick, yellow, cheesy discharge;
a yeasty odor; and pain.
b. The disorder, experienced at least once by about 75% of females, is usually a
result of proliferation of the fungus following antibiotic therapy for another condition
C. Sexually transmitted diseases (STDs) are disease spread by sexual contact and include chlamydia,
gonorrhea, syphilis, and genital herpes.
1. Chlaymdia is a STD caused by the bacterium Chlamydia trachomatis. At present
chlamydia is the most prevalent and one of the most damaging of the STDs.
a. In most cases, the initial infection is asymptomatic and difficult to recognize
clinically.
b. In males, urethritis is the principal result. c. In females, urethritis may spread through the reproductive tract and develop
into inflammation of the uterine tubes, which increases the risk of ectopic pregnancy and sterility.
2. Gonorrhea ( clap ) is an infectious STD that affects primarily the mucous membrane of
the urogenital tract, the rectum, and occasionally the eyes. The disease is caused by the bacterium Neisseria gonorrhoreae.
a. Males usually suffer inflammation of the urethra with pus and painful urination. b. In females, infection may occur in the urethra, vagina, and cervix, and their may
be a discharge of pus. However, infected females often harbor the disease
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
without any symptoms until it has progressed to a more advanced stage. If the uterine tubes become involved, pelvic inflammation may follow, often causing sterility and occasionally causing peritonitis.
c. If the bacteria are transmitted to the eyes of a newborn in the birth canal,
blindness can result. Administration of a 1% silver nitrate solution or penicillin or erythromycin in the neonate s eyes prevents infection.
3. Syphilis is an STD caused by the bacterium Treponema pallidum. a. It is acquired through sexual contact, exchange of blood, or transmitted
through the placenta to a fetus.
b. The disease progresses through several stages: primary, secondary, latent, and
tertiary. 1) During the primary stage, the chief symptom is a painless open sore, called a chanker. 2) A skin rash, fever, and aches in the joints usher in the secondary stage: a systemic infection. 3) The tertiary stage occurs when signs of organ degeneration appear.
4. Genital herpes is an incurable STD caused by the type II herpes simplex virus (HSV-2). a. HSV-2 causes genital infections such as painful blisters on the prepuce, glans
penis, and penile shaft in males and on the vulva or sometimes high up in the vagina in females.
b. The blisters disappear and reappear in most patients, but the virus itself
remains in the body.
Critical Thinking Questions 1. Assume that a 30-year-old male is able to produce sufficient spermatozoa, but because of an obstruction in his duct system, the spermatozoa cannot be discharged through the urethra. If each duct in the system had to be examined to locate the obstruction, explain the sequence in which the ducts would have to be examined, starting with the urethra and termination in the seminiferous tubules. 2. Make a flowchart explaining the hormonal relationships that exist among the pituitary gland, ovarian cycle, and uterine (menstrual) cycle.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
DEVELOPMENT AND INHERITANCE
I. INTRODUCTION A. Developmental anatomy is the study of the sequence of events from the fertilization of a secondary oocyte to the formation of an adult organism.
1. The first two months following fertilization is the period of embryonic development and
the developing human is an embryo.
2. From week nine until birth is the fetal development period and the individual is a fetus. B. Embryology is the study of development from fertilization to the fetal period. C. Obstetrics is the branch of medicine that deals with the management of pregnancy, labor, and
the neonatal period (the first 42 days after birth).
D. Prenatal development is the time from fertilization until birth. It is divided into three trimesters.
EMBRYONIC PERIOD
A. First Week of Development 1. Fertilization a. During fertilization, the genetic material from a haploid sperm cell
(spermatozoon) and a haploid secondary oocyte merges into a single diploid nucleus.
1) Fertilization normally occurs in the uterine (Fallopian) tube when the
oocyte is about one-third of the way down the tube to the uterus, usually within 12 to 24 hours after ovulation.
2) The process leading to fertilization begins as peristaltic contractions
and the actions of cilia transport the oocyte through the uterine tube.
3) Sperm swim up the uterus and into the uterine tube by the whip like
movements of their tails and muscular contractions of the uterus.
b. The functional changes that sperm undergo in the female reproductive tract
that allow them to fertilize a secondary oocyte are referred to as capacitation.
c. To fertilize an oocyte, a sperm must penetrate the corona radiata and zona
pellucida around the oocyte.
1) A glycoprotein in the zona pellucida (ZP3) acts as a sperm receptor,
binds to specific membrane proteins in the sperm head and triggers the acrosomal reaction, the release of the contents of the acrosome.
2) The acrosomal enzymes digest a path through the zona pellucida
allowing only one sperm to make its way through the barrier and reach the oocyte s plasma membrane. a.) Fusion of a sperm with a secondary oocyte is called syngamy.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
b.) Polyspermy is prevented by chemical changes that prevent a second sperm from entering the oocyte.
d. Once a sperm enters a secondary oocyte, the oocyte completes meiosis, and
the male pronucleus and female pronucleus fuse forming the fertilized ovum or zygote.
1) Dizgyotic (fraternal) twins are produced from the independent release
of two ova and the subsequent fertilization of each by different spermatozoa. They are the same age and are in the uterus at the same time but are as genetically dissimilar as other siblings.
2) Monozygotic (identical) twins are derived from a single fertilized ovum
that splits at an early stage in development. They contain exactly the same genetic material and are always the same sex.
2. Cleavage of the zygote a. Early rapid mitotic cell division of a zygote is called cleavage. b. The cells produced by cleavage are called blastomeres. c. Successive cleavages produce a solid mass of cells, called the morula. 3. Blastocyst formation a. As the number of cells in the morula increases, it moves from the site of
fertilization down through the ciliated uterine tube toward the uterus and enters the uterine cavity.
b. The morula develops into a blastocyst, a hollow ball of cells that is
differentiated into a trophoblast (which will form the future embryonic membranes), an inner cell mass or embryoblast (the future embryo), and an internal fluid-filled cavity called the blastocele.
c. Pluripotent cells currently being used in research are derived from embryos
that were to be used for infertility treatment but are no longer needed and from fetuses aborted during the first trimester. Both methods are being investigated as means to treat various diseases (Clinical Application).
4. Implantation a. The blastocyst remains free with the cavity of the uterus for two to four days
before it actually attaches to the uterine wall.
b. The attachment of a blastocyst to the endometrium occurs seven to eight days
after fertilization and is called implantation.
c. Following implantation the endometrium is known as the decidua and consists
of three regions: the decidua basalis, decidua capuslaris, and decidua parietalis.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
1) The decidua basalis lies between the chorion and the stratum basalis
of the uterus. It becomes the maternal part of the placenta.
2) The decidua capsularis covers the embryo and is located between the
embryo and the uterine cavity.
3) The decidua parietalis lines the noninvolved areas of the entire
pregnant uterus.
5. Ectopic pregnancy refers to the development of an embryo or fetus outside the uterine
cavity. Most occur in the uterine tube, usually in the ampullar or infundibular portions. Some occur in the ovaries, abdomen, uterine cervix, or broad ligaments. Depending on the location of the ectopic pregnancy, the condition can become life threatening to the mother. (Clinical Application)
B. Second Week of Development 1. Development of the trophoblast a. The trophoblast develops into a syncytiotrophoblast and a cytotrophoblast. b. These two layers become part of the chorion as they undergo further growth. c. The syncytiotrophoblast cells secrete enzymes that enable the blastocyst to
penetrate the uterine lining.
d. The trophoblast also secretes human chorionic gonadotropin, which rescues the
corpus luteum from degeneration and sustains its function.
2. The cells of the inner cell mass differentiate into two layers the hypoblast (primitive
endoderm) and the epiblast (primitive ectoderm); these two layers form a flattened disc referred to as the bilaminar embryonic disc.
3. Development of the amnion a. A thin, protective membrane called the amnion develops from the epiblast b. Initially the amnion overlies only the bilaminar embryonic disc; as the embryo
grows it eventually surrounds the entire embryo creating the amniotic cavity.
c. The amniotic cavity becomes filled with amniotic fluid. d. Amniotic fluid protects the developing fetus and can be examined in a
procedure known as amniocentesis.
4. Development of the yolk sac a. The hypoblast cells migrate and become the exocoelomic membrane. b. The hypoblast and the exocoelomic membrane form the yolk sac. c. The yolk sac has several important functions. It transfers nutrients to the
embryo, is an early source of blood cells, and produced primitive germ cells, which will become spermatogonia and oogonia.
5. Development of sinusoids
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
a. On the ninth day after fertilization the coagulation plug seals the site of
implantation.
b. The syncytiotrophoblast expands and small spaces called lacunae develop
within it.
c. By the twelfth the lacunae fuse to form lacunar networks. d. Endometrial capillaries around the developing embryo become dilated and are
referred to as sinusoids.
e. The synctiotrophoblast erodes the sinusoids and endometrial glands permitting
maternal blood to enter the lacunar networks.
6. After the extraembryonic mesoderm develops, several large cavities develop in the
mesoderm. These cavities fuse to form the extraembryonic coelom
7. Development of the chorion a. The chorion develops from extraembryonic mesoderm and the two layers of
the trophoblast.
b. The chorion becomes the principal embryonic part of the placenta. c. The chorion secretes hCG, an important hormone of pregnancy. C. Third Week of Development 1. Gastrulation a. During gastrulation the two-dimensional bilaminar embryonic disc transforms
into a two-dimensional trilaminar embryonic disc consisting the three primary germ layers: the ectoderm, mesoderm, and endoderm.
b. Gastrulation begins with the development of the primitive streak. c. Cells of the epiblast move inward below the primitive streak and detach from
the epiblast.
d. The primary germ layers, ectoderm, mesoderm, and endoderm, form all tissues
and organs of the developing organism
e. A solid cylinder of cells the notochord also develops. It plays an important role
in the process of induction.
f. The oropharyngeal membrane that will eventually connect the mouth cavity to
the pharynx and the remainder of the gastrointestinal tract appears.
g. The cloacal membrane that will form the openings of the anus and urinary and
reproductive tracts also appears.
h. The allantois, a vascularized out pouching of the yolk sac extends into the
connecting body stalk. It is not a prominent structure in humans.
2. Neurulation a. The notochord induces the ectodermal cells over it to form the neural plate
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
b. The neural plate gives rise to the neural folds and neural groove that will fuse to
form the neural tube.
c. Ectodermal cells from the neural tube migrate to form the neural crest which
give rise spinal and cranial nerves and their ganglia, autonomic nervous system ganglia, the meninges of the brain and spinal cord, the adrenal medullae, and several skeletal and muscular components of the head.
d. The head of the neural tube develops into the three primary vesicles: the
prosencephalon, mesencephalon, and the rhombencephalon.
e. Later the secondary vesicles will develop. They are the telencephalon,
diencephalon, metencephalon, and myelencephalon.
f. Neural tube defects (NTDs) are caused by arrest of the normal development
and closure of the neural tube. These include anencephaly and spina bifida (Clinical Application).
3. Development of somites a. The somites, a series of paired, cube-shaped structures, develop from the
mesoderm.
b. Eventually 42-44 pairs of somites will develop. c. Each somite has three regions, a myotome, dermatome, and sclerotome. 4. Development of the intraembryonic coelom a. Small spaces in the lateral plate mesoderm fuse to form a larger cavity, the
intraembryonic coelom.
b. This cavity splits the lateral plate mesoderm into two parts called the splanchnic
mesoderm and the somatic mesoderm.
c. The intraembryonic mesoderm divides into the pericardial, pleural, and
peritoneal cavities.
d. Splanchnic mesoderm forms portions of the heart, respiratory and digestive
systems.
e. Somatic mesoderm gives rise to bones, ligaments, and dermis of the limbs and
the parietal layer of the serous membranes.
5. Development of the cardiovascular system a. Angiogenesis, the formation of blood vessels, begins in the extraembryonic
mesoderm in the yolk sac, connecting stalk, and chorion.
1.) Angiogenesis is initiated when angioblasts aggregate to form isolated
masses of cells referred to a blood islands.
2.) Spaces in the blood islands from the lumen of blood vessels. 3.) Angioblasts form the walls of the blood vessels
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
b. The heart forms in the cardiogenic area of the splanchnic mesoderm. 1.) The mesodermal cells form a pair of endocardial tubes. 2.) The tubes fuse to form a single primitive heart. 6. Development of the chorionic villi and placenta a. Chorionic villi develop as projections of the cytotrophoblast that eventually
contain blood filled capillaries.
b. Blood vessels in the chorionic villi connect to the embryonic heart by way of
umbilical arteries and veins.
c. The placenta has a fetal portion formed by the chorionic villi of the chorion and
a maternal portion formed by the decidua basalis of the endometrium
1.) Functionally the placenta allows oxygen and nutrients to diffuse from
maternal blood to fetal blood that carbon dioxide and wastes diffuse from fetal blood into maternal blood.
2.) The placenta also serves as a protective barrier, stores nutrients, and
secretes several important hormones necessary to maintain the pregnancy.
d. The connection between the placenta and the embryo is the umbilical cord. e. After the birth of the baby, the placenta detaches from the uterus and is
therefore termed the afterbirth.
f. Placenta previa is a condition in which part or the entire placenta becomes
implanted in the lower portion of the uterus, near or over the internal os of the cervix. If detected during pregnancy (either by ultrasound or as a result of sudden painless bright red vaginal bleeding during the third trimester), cesarean section is the preferred method of delivery. (Clinical Application)
D. Fourth week of Development 1. Embryonic folding converts the embryo from a flat, two-dimensional trilaminar
embryonic disc to a three-dimensional cylinder.
2. Development of the somites and the neural tube occurs during the fourth week. 3. Several pharyngeal (branchial) arches develop on each side of the future head and neck
regions. With the pharyngeal clefts and pouches they will form structures of the head and neck.
4. The otic placode is the first sign of a developing ear. 5. The lens placode is the first sign of a developing eye. 6. The upper limb buds appear in the middle of the fourth week and the lower limb buds
appear at the end of the fourth week.
E. Fifth Through Eight Weeks of Development
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
1. During the fifth week there is rapid brain development and considerable head growth. 2. During the sixth week the head grows even larger in relation to the trunk, there is
substantial limb growth, the neck and truck begin to straighten, and the heart is now four-chambered.
3. During the seventh week the various regions of the limbs become distinct and the
beginnings of the digits appear.
4. By the end of the eighth week all regions of the limbs are apparent, the digits are
distinct, the eyelids come together, the tail disappears, and the external genitals begin to differentiate. FETAL PERIOD
A. During the fetal period, tissue and organs that developed during the embryonic period grow
and differentiate. The rate of body growth is remarkable. PRENATAL DIAGNOSTIC TESTS
A. In fetal ultrasonography, an image of the fetus, called a sonogram, is displayed on a screen. It is
used most often to determine true fetal age when the date of conception is uncertain. It is also used to evaluate fetal viability and growth, determine fetal position, ascertain multiple pregnancies, identify fetal-maternal abnormalities, and serve as an adjunct to special procedures such as amniocentesis and chorionic villus sampling.
B. Amniocentesis is the transabdominal withdrawal of some of the amniotic fluid that bathes the
developing fetus and subsequent analysis of the fetal cells and dissolved substances. It is used to test for the presence of certain genetic disorders, such as Down syndrome, spina bifida, hemophilia, Tay-Sachs disease, Sickle-cell disease, and certain muscular dystrophies or to determine fetal maturity and well-being near the time of delivery. The test is usually done at 1416 weeks gestation to detect suspected genetic abnormalities. To asses fetal maturity, it is usually done after the 35 week of gestation.
th
C. Chorionic villi sampling (CVS) involves withdrawal of chorionic villi for chromosomal analysis. CVS
can be done earlier than amniocentesis (at 8-10 weeks gestation), and the results are available more quickly. The sampling is normally done transvaginally using an ultrasound-guided catheter; transabdominal sampling, similar to amniocentesis, is also possible.
D. The first noninvasive prenatal test was maternal alphafetoprotein (AFP) test. This test analyzes
the maternal blood for the presence of AFP. A high level of AFP after 16 weeks indicates that the fetus has a neural tube defect. This test is used to screen for Down syndrome, trisomy 18, and neural tube defects. It also helps predict delivery date and may reveal the presence of twins.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
MATERNAL CHANGES DURING PREGNANCY Hormones of Pregnancy
1. During the first 3-4 months of pregnancy, the corpus luteum continues to secrete
progesterone and estrogens to maintain the uterine lining and prepare the mammary glands to secrete milk.
2. From the third month on, the placenta provides the high levels of estrogens and
progesterones necessary to maintain the pregnancy.
3. The chorion of the placenta secretes human chorionic gonadotropin (hGH), relaxin, and
human somatomammotropin (hCS).
a. Human chorionic gonadotropin (hCG) mimics LH; its primary role is to stimulate
continued production by the corpus luteum of estrogens and progesterone - an activity necessary for the continued attachment of the embryo and fetus to the lining of the uterus.
b. Relaxin, produced by the ovaries, testes, and placenta, inhibits secretion of FSH
and might regulate secretion of hGH.
c. Human chorionic somatomammotropin (hCS) (also known as human placental
lactogen, or hPL), also produced by the chorion, assumes a role in breast development for lactation, protein anabolism, and catabolism of glucose and fatty acids.
4. Corticotropin-releasing hormone (CRH) is thought to be the clock that establishes the
timing of birth.
5. Early pregnancy tests detect the tiny amounts of hCG in the urine that begin to show up
about 8 days after fertilization. (Clinical Application)
B. Anatomical and Physiological Changes During Pregnancy 1. During gestation, several anatomical and physiological changes occur. a. The uterus continuously enlarges, filling first the pelvic and then the abdominal
cavity, displacing and compressing a number of structures.
b. Pregnancy-induced physiological changes include weight gain; increased
protein, fat, and mineral storage; marked breast enlargement; and lower back pain.
c. Cardiovascular modifications include increase in stroke volume by
approximately 30%, rise in cardiac output by approximately 20-30%, increase in heart rate by 10-15%, and increase in blood volume up to 30-50% (mostly during the latter half of pregnancy). The uterus may compress large blood vessels, diminishing blood flow and return to the heart.
d. Pulmonary function alternations include increased tidal volume (30-40%),
decreased expiratory reserve volume (by up to 40%), increased minute volume
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
of respiration (by up to 40%), decreased airway resistance in the bronchial tree (by up to 36%), and increase in total body oxygen consumption (by 10-20%). Dyspnea also occurs.
e. With regard to the gastrointestinal tract, there is an increase in appetite and
decreased motility that can result in constipation and delayed gastric emptying. Nausea, vomiting, and heartburn also occur.
f. Pressure on the urinary bladder increases frequency and urgency of urination;
stress incontinence may occur. Glomerular filtration rate rises up to 40%.
g. The skin may display increased pigmentation, striae (stretch marks) over the
abdomen occur as the uterus enlarges, and hair loss increases.
h. In the reproductive system, there is edema and increased vascularity of the
vulva and increased pliability and vascularity of the vagina. The weight of the uterus increases 15 to 20-fold during pregnancy due to hyperplasia of muscle fibers (cells) in the myometrium in early pregnancy and hypertrophy of muscle fibers during the second and third trimesters.
2. Approximately 10-15% of all pregnant women in the United States experience
pregnancy-induced hypertension, elevated blood pressure associated with pregnancy. The major cause is preeclampsia, in which the hypertension seems to result from impaired renal function. It typically occurs after the 20 week of gestation and there are large amounts of protein in the blood. When associated with convulsions and coma, the condition is termed eclampsia (Clinical Application) EXERCISE AND PREGNANCY
th
A. Exercise may need to be modified during pregnancy to accommodate the changes in the female s
body.
B. Moderate physical activity does not endanger the fetuses of healthy females who have a normal
pregnancy and is beneficial in many aspects. LABOR
A. Labor is the process by which the fetus is expelled from the uterus through the vagina to the
outside. Parturition also means giving birth.
1. A decrease in progesterone levels and elevated levels of estrogens, prostaglandins,
oxytocin, and relaxin are all probably involved in the initiation and progression of labor.
2. True labor begins when uterine contractions occur at regular intervals, usually producing
pain. As the interval between contractions shortens, the contractions intensify. Other signs of true labor may be localization of pain in the back, which in intensified by walking; show (discharge of blood-containing mucus from the cervical canal); and dilation of the cervix. In false labor, pain is felt in the abdomen at irregular intervals. The
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
pain does not intensify and is not altered significantly by walking. There is no show and no cervical dilation.
B. The birth of a baby involves three stages: dilation of the cervix, expulsion of the fetus, and
delivery of the placenta.
1. The stage of dilation is the time from the onset of labor to the complete dilation of the
cervix. During this stage, there are regular contractions of the uterus, usually a rupturing of the amniotic sac, and complete dilation (10cm) of the cervix. If the amniotic sac does not rupture spontaneously, it is done artificially.
2. The stage of expulsion is the time from complete cervical dilation to delivery. 3. The placental stage is the time after delivery until the placenta or afterbirth is expelled
by powerful uterine contractions. These contractions also constrict blood vessels that were torn during delivery, reducing the possibility of hemorrhage.
C. During labor, the fetus is squeezed through the birth canal for up to several hours, resulting in
compression of the fetal head and some intermittent hypoxia due to compression of the umbilical cord and placenta during uterine contractions. In response to this compression, the adrenal medullae of a fetus secrete very high levels of epinephrine and norepinephrine. These hormones afford the fetus protection against the stresses of the birth process and prepare the infant to survive extrauterine life.
D. After delivery of the baby and placenta, there is a period of time, called the puerperium that lasts
about six weeks. During this time the reproductive organs and maternal physiology return to the prepregnancy state. The uterus undergoes a remarkable reduction in size called involution and there is a uterine discharge (lochia) of blood and serous fluid for two to four weeks after delivery.
E. Dystocia, or difficult labor, may result from impaired uterine forces, an abnormal position
(presentation) of the fetus, or a birth canal of inadequate size to permit vaginal birth. In these instances, and in certain conditions of fetal or maternal distress during labor, it my be necessary to deliver the baby via cesarean section (C-section). Even a history of multiple C-sections need not preclude a pregnant woman from attempting a vaginal delivery. (Clinical Application) ADJUSTMENTS OF THE INFANT AT BIRTH
A. During pregnancy, the embryo (and later, the fetus) depends on the mother for oxygen and
nutrients, removal of wastes, and protection against shocks, temperature changes, and certain harmful microbes. At birth, a physiologically mature baby becomes self-supporting, and the newborn s body systems must make various adjustments.
B. Respiratory Adjustments 1. After delivery the baby s supply of oxygen from the mother is stopped. 2. Circulation in the baby continues, and as the blood level of carbon dioxide increases, the
respiratory center in the medulla is stimulated. This causes the respiratory muscles to
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
contract, and the baby draws its first breath. Since the first inspiration is unusually deep because the lungs contain no air, the baby exhales vigorously and naturally cries.
3. A full-term baby may breathe 45 times a minute for the first two weeks after birth. The
rate is gradually reduced until it approaches a normal rate.
C. Cardiovascular Adjustments 1. The foramen ovale between the atria of the fetal heart closes at the moment of birth.
This diverts deoxygenated blood to the lungs for the first time.
a. Two flaps of heart tissue that folds together and permanently fuse close the
foramen ovale.
b. The remnant of the foramen ovale is the fossa ovalis. 2. Once the lungs begin to function, the ductus arteriosus is shut off by contractions of the
muscles in its wall.
a. The ductus arteriosus generally does not completely and irreversibly close for
about three months following birth.
b. The ligamentum arteriosum is the remnant of the ductus arteriosus. 3. When the umbilical cord is severed, all visceral blood of the fetus goes directly to the
infant heart via the inferior vena cava.
a. This shunt of blood usually occurs within minutes after birth but may take a
week or two to complete.
b. The ligamentum venosum, the remnant of the ductus venosus, is well
established by the eighth postnatal week.
4. At birth, the infant s pulse may be from 120 to 160 per minute and may go as high as
180 following excitation.
5. Several days after birth, there is a greater independent need for oxygen, which
stimulates an increase in the rate of erythrocyte and hemoglobin production. This increase usually lasts for only a few days.
6. The white blood cell count at birth is very high, sometimes as much as 45,000 cells per
cubic millimeter, but this decreases rapidly by the seventh day.
D. Delivery of a physically immature baby carries certain risks. Major problems faced by a premature
infant include respiratory distress syndrome, blindness, brain hemorrhages, and digestive disorders. The problems related to survival of premature infants are due to the fact that they are not yet ready to take over functions the mother s body should be performing. (Clinical Application) PHYSIOLOGY OF LACTATION
A. Lactation refers to the secretion and ejection of milk by the mammary glands.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
1. A principal hormone in promoting lactation is prolactin (PRL) from the anterior pituitary
gland.
a. PRL levels increase as the pregnancy progresses, but there is no milk secretion
because estrogens and progesterone inhibit PRL from being effective.
b. Following delivery, estrogens and progesterone decrease, removing their
inhibitory effect.
c. The principal stimulus in maintaining prolactin secretion during lactation is the
sucking action of the infant.
2. Oxytocin (OT) causes release of milk into mammary ducts by the milk ejection reflex. a. OT induces smooth muscle cells surrounding the outer walls of the alveoli to
contract, thereby compressing the alveoli and ejecting milk. The compression moves milk from the alveoli of the mammary gland into the ducts, where it can be sucked. This process is referred to a milk ejection (let-down).
b. Although the actual ejection of milk does not occur from 30 seconds to 1
minute after nursing begins, some milk is stored in lactiferous sinuses near the nipple. Thus, some milk is available during the latent period.
B. During late pregnancy and the first few days after birth, the mammary glands secrete a cloudy
fluid called colostrum. It is not as nutritious as true milk but serves adequately until the appearance of true milk on about the fourth postpartum day. Colostrum and maternal milk are thought to contain antibodies that protect the infant during the first few months of life.
C. Nursing causes neural feedback to the hypothalamus and the anterior pituitary gland that
stimulates the production of PRF (prolactin releasing factor) and PRL, causing the mammary glands to prepare for the next nursing period.
1. Milk secretion can continue for several years if the child continues to suckle. Milk
secretion normally decreases considerably within seven to nine months.
2. The mammary glands can lose their ability to secrete milk in a period of only a few days
if nursing is discontinued or hormonal release is blocked by injury or disease.
D. Lactation often prevents the occurrence of female ovarian cycles for the first few months
following delivery if the frequency of nursing is about 8-10 times a day. However, there is no guarantee of contraception.
E. A primary benefit of breast-feeding is nutritional. Other benefits include the baby receiving
beneficial cells and molecules from the breast milk, showing a decreased incidence of diseases later in life, as well as other benefits.
F. Nursing stimulates the release of oxytocin and helps promote expulsion of the placenta and the
uterus to regain its smaller size. (Clinical Application) INHERITANCE
A. Inheritance is the passage of hereditary traits from one generation to another.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
1. The branch of biology that deals with inheritance is called genetics. 2. The area of health care that offers advice on genetic problems is called genetic
counseling.
B. Genotype and Phenotype 1. Nuclei of all human cells except gametes contain 23 pairs of chromosomes (diploid
number).
a. One chromosome in each pair came from the mother, and the other came from
the father.
b. Homologues, the two chromosomes in a pair, contain genes that control the
same traits.
c. The two genes that code for the same trait and are at the same location on
homologous chromosomes are termed alleles.
d. A mutation is a permanent heritable change in a gene that causes it to have a
different effect than it had previously.
2. The genetic makeup of an organism is called its genotype. a. Dominant genes control a particular trait; expression of recessive genes is
inhibited by the presence of dominant genes.
b. An individual with the same genes on homologous chromosomes (e.g., PP or
pp) is said to be homozygous for the trait. An individual with different genes on homologous chromosomes (e.g., Pp) is said to be heterozygous for the trait. (By convention, the dominant gene is expressed by a capital letter; and the recessive gene, by a lower case letter.)
3. The traits that are expressed are called its phenotype. 4. Most genes give rise to the same phenotype whether they are inherited from the
mother or father; although, in a few cases, the phenotype is dramatically different. This phenomenon is called genomic imprinting.
5. To determine the possible ways that haploid gametes can unite to form diploid fertilized
eggs, special charts called Punnett squares are used.
6. Meiosis errors can result in inheritance abnormalities. a. Nondisjunction results in an abnormal number of chromosomes. b. A cell that has one or more chromosomes of a set added or deleted is called an
aneuploid.
c. In translocation, the location of a chromosome segment is changed, being
moved either to another chromosome or to another location within the same chromosome.
C. Variations on Dominant-Recessive Inheritance
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
1. Most patterns of inheritance do not conform to the simple dominant-recessive patterns
in which only dominant and recessive genes interact.
2. In fact, the phenotypic expression of a particular gene is influenced not only by the
alleles of the genes present, but also by other genes and by the environment. Most inherited traits are influenced by more than one gene, and most genes can influence more than a single trait.
3. In incomplete dominance, neither member of an allelic pair dominates; phenotypically
the heterozygote is intermediate between the homozygous dominant and homozygous recessive. An example is sickle-cell disease.
4. In multiple-allele inheritance, some genes have more than two alternate forms. An
example is the inheritance of ABO blood groups.
5. In polygenic inheritance, the combined effects of many genes control an inherited trait.
An example is skin color.
6. Complex inheritance refers to the combined effects of many genes and environmental
factors.
D. Autosomes, Sex Chromosomes, and Sex Determination 1. In 22 of the 23 pairs of chromosomes, the homologous chromosomes look alike and
have the same appearance in both males and females; these 22 pairs are called autosomes. The two members of the 23 pair are termed the sex chromosomes.
rd
a. In females, the 23rd pair consists of two chromosomes designated as X
chromosomes.
b. One X chromosome is also present in the male sex chromosomes, but its mate
is a smaller chromosome called a Y chromosome.
c. If an X-bearing sperm fertilizes the secondary oocyte, the offspring normally will
be female (XX). Fertilization by a Y-bearing sperm normally produces a male (XY). Thus, gender (sex) is determined by the father s sex chromosome.
2. Sex is determined by the presence or absence of an SRY (sex-determining region of the Y
chromosome) gene on the Y chromosome at fertilization.
E. Sex-Linked Inheritance 1. The sex chromosomes also are responsible for the transmission of several nonsexual
traits. Genes for these traits appear on X chromosomes, but many of them are absent from Y-chromosomes. Traits inherited in this manner are called sex-linked or X-linked traits.
2. Red-green color blindness and hemophilia primarily affect males because there are no
counterbalancing dominant genes on the Y-chromosome. Other sex-linked traits in humans are fragile X syndrome, nonfunctional sweat glands, certain forms of diabetes, some types of deafness, uncontrollable rolling of the eyeballs, absence of central
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
incisors, night blindness, one form of cataract, juvenile glaucoma, and juvenile muscular dystrophy.
a. Whereas females have two X chromosomes in every cell, they actually use only
one. X-chromosome inactivation or lyonization inactivates one X-chromosome so that its genes are not expressed.
b. The inactivated X chromosome shows up as a Barr body in cells. F. Teratogens 1. A given phenotype is the result of the interactions of genotype and the environment. A
teratogen is any agent or influence that causes developmental defects in the embryo.
2. Chemicals and Drugs a. Because the placenta is a porous barrier between the maternal and fetal
circulations, any drug or chemical dangerous to an infant may be considered potentially dangerous to the fetus when given to the mother.
b. Alcohol is by far the number one fetal teratogen. Intrauterine exposure to even
a small amount of alcohol may result in fetal alcohol syndrome, one of the most common causes of mental retardation and one of the most common preventable causes of birth defects in the United States.
c. Other fetal teratogens include pesticides, industrial chemicals, some hormones,
antibiotics, some prescription drugs, and street drugs.
3. Cigarette Smoking a. Cigarette smoking is implicated as a cause of low birth weight and a higher fetal
and infant mortality rate.
b. Cigarette smoke may be teratogenic and cause cardiac abnormalities and
anencephaly.
4. Ionizing radiations are potent teratogens.
DISORDERS: HOMEOSTATIC IMBALANCES
A. Infertility 1. Female infertility may be caused by ovarian disease, uterine tube obstruction, conditions
in which the uterus is not adequately prepared to receive the fertilized ovum, and inadequate body fat.
2. Male infertility is an inability to fertilize a secondary oocyte. 3. Many fertility-expanding techniques now exist for assisting infertile couples to have a
baby.
a. In vitro fertilization (IVF) refers to the fertilization of a secondary oocyte outside
the body and the subsequent introduction of an 8-cell or 16-cell embryo for implantation and subsequent growth.
Selected Topic Summaries for A&P Readings taken from: Principles of Anatomy & Physiology, 10 ed. Tortora, Grobawski.
b. In intracytoplasmic sperm injection, an oocyte may be fertilized by suctioning a
sperm or even a spermatid obtained from the testis into a tiny pipette and then injecting it into the oocyte s cytoplasm.
c. In embryo transfer, a husband s sperm is used to artificially inseminate a fertile
secondary oocyte donor.
d. In gamete intrafallopian transfer, a sperm and secondary oocyte are united in
the prospective mother s uterine tube.
B. Down syndrome (DS) is a disorder that results from an error in cell division called nondisjunction,
involving chromosome pair #21. This syndrome is caused by trisomy of an autosome rather than aneuploidy of a sex chromosome. Although it is more common as the mother approaches age 35 and beyond, many women under the age of 35 give birth to children with DS.
C. Trinucleotide repeat diseases are caused by repeating triplets of nucleotides. A specific sequence
of three DNA nucleotides that normally repeats several times within a gene becomes greatly expanded during gametogenesis. Sometimes the number of repeats expands with each succeeding generation. Huntington disease (HD) and fragile X syndrome are trinucleotide repeat diseases.
Critical Thinking Questions 1. An X-linked trait is one that appears more frequently in one sex than in the other. Hemophilia is an example of such a trait; it occurs more frequently in males. Explain by using a Punnett square how hemophilia is inherited. Assume that the father is normal and that the mother is normal, but carries the recessive gene for hemophilia. 2. Jan has a history of miscarriage in the first trimester. Her physician thinks that her problem might be hormonal. What hormones could be implicated in failing to maintain the pregnancy during the first trimester? 3. Doris wants to have her child born n a particular day. She asks her physician if he can induce labor on that day. Is this procedure possible? If so, what will the physician have to do? Are there any negative consequences to having labor induced?
S-ar putea să vă placă și
- Fluid Mechanics FundamentalsDocument32 paginiFluid Mechanics FundamentalsMark Paulo AlcalaÎncă nu există evaluări
- Caring for Mothers, Children, Families & At-Risk PopulationsDocument14 paginiCaring for Mothers, Children, Families & At-Risk PopulationsBing58Încă nu există evaluări
- A&p I Case StudiesDocument10 paginiA&p I Case StudiesJohn Nino0% (2)
- STS-Introduction to Science, Technology and SocietyDocument4 paginiSTS-Introduction to Science, Technology and SocietyAngela Danielle Tan100% (1)
- Chapter 52 - Drugs Affecting The Urinary Tract and The BladderDocument12 paginiChapter 52 - Drugs Affecting The Urinary Tract and The BladderJonathonÎncă nu există evaluări
- Assessing The Thorax and Lungs: Return Demonstration Evaluation Tool ForDocument3 paginiAssessing The Thorax and Lungs: Return Demonstration Evaluation Tool Forclint xavier odangoÎncă nu există evaluări
- ELC151 W1 Skimming and ScanningDocument9 paginiELC151 W1 Skimming and ScanningNatasya BayumiÎncă nu există evaluări
- 2syllogisms EnthymemesDocument19 pagini2syllogisms EnthymemesNiña Chris BuenÎncă nu există evaluări
- Theories of Ageing: Presented by DR - Pratyusha KaligotlaDocument13 paginiTheories of Ageing: Presented by DR - Pratyusha KaligotlaSHAIK SHABEENAÎncă nu există evaluări
- Chapter 1: Human Anatomy Divisions of Human PhysiologyDocument16 paginiChapter 1: Human Anatomy Divisions of Human PhysiologyBeverly A PanganibanÎncă nu există evaluări
- Trace of Oxygen from Nose to Lungs to BodyDocument3 paginiTrace of Oxygen from Nose to Lungs to Bodyaznknight323Încă nu există evaluări
- 10 Ways To Boost Your Emotional Health Through Improving Your SelfDocument6 pagini10 Ways To Boost Your Emotional Health Through Improving Your SelfDOLORES LEE CORPUZÎncă nu există evaluări
- Cell MetabolismDocument6 paginiCell MetabolismelsayidÎncă nu există evaluări
- STUDENT NOTES - Foundation and Principles of Bioethics in NursingDocument5 paginiSTUDENT NOTES - Foundation and Principles of Bioethics in NursingBlaiseÎncă nu există evaluări
- Bachelor of Science in NursingDocument3 paginiBachelor of Science in NursingTrixie Adaley Xen Heirencia100% (1)
- Epidemiology Matching Terms and ActivitiesDocument4 paginiEpidemiology Matching Terms and Activitiesazkha_knowles3279Încă nu există evaluări
- Lab 13: Reflex Arc and Reflexes: Learning Outcomes of The Lab ExercisesDocument6 paginiLab 13: Reflex Arc and Reflexes: Learning Outcomes of The Lab ExercisesNellyWataÎncă nu există evaluări
- Prof. Hilaria M. Barsabal Cagayan State UniversityDocument35 paginiProf. Hilaria M. Barsabal Cagayan State UniversityDarlene Andres PonceÎncă nu există evaluări
- Jenkins CTQ Ch01 - Anatomy & PhysiologyDocument3 paginiJenkins CTQ Ch01 - Anatomy & Physiologyjavnas100% (1)
- College of Crimininal Justice Education: NSTP - Cwts 1Document5 paginiCollege of Crimininal Justice Education: NSTP - Cwts 1Katherine Marie BerouÎncă nu există evaluări
- Sanders 2003 - Application of Colaizzi's MethodDocument11 paginiSanders 2003 - Application of Colaizzi's MethodEricson Mitra100% (1)
- Child's Head Growth ConcernDocument8 paginiChild's Head Growth ConcernAlden MendozaÎncă nu există evaluări
- Unit 2 Topic 4 STSDocument6 paginiUnit 2 Topic 4 STSRachell AvecillaÎncă nu există evaluări
- Essay On The Importance of Mental Health ParityDocument1 paginăEssay On The Importance of Mental Health ParityPrince BatiocoÎncă nu există evaluări
- Week 14 - OBF Analysis (Gastric Fluid)Document19 paginiWeek 14 - OBF Analysis (Gastric Fluid)Astrud LabradorÎncă nu există evaluări
- ResearchDocument8 paginiResearchKiana RamosaÎncă nu există evaluări
- TFNDocument27 paginiTFNim. EliasÎncă nu există evaluări
- NSTPDocument8 paginiNSTPHanna TrocioÎncă nu există evaluări
- Functions of BloodDocument5 paginiFunctions of BloodsecretÎncă nu există evaluări
- CaseDocument7 paginiCaseAia JavierÎncă nu există evaluări
- CHN PRELIM Quiz 1 (2011)Document5 paginiCHN PRELIM Quiz 1 (2011)Amiel Francisco ReyesÎncă nu există evaluări
- Concept 3 Notes - Anatomy Basics For StudentsDocument39 paginiConcept 3 Notes - Anatomy Basics For StudentsKaranÎncă nu există evaluări
- Module 6 - IV Calculations, Solutions, EquipmentDocument3 paginiModule 6 - IV Calculations, Solutions, Equipmentlool89175% (4)
- Historical Development of TheoriesDocument5 paginiHistorical Development of TheoriesMichael100% (3)
- Laparotomy Procedure ExplainedDocument3 paginiLaparotomy Procedure ExplainedAleeya SarajanÎncă nu există evaluări
- Work-Related Musculoskeletal Disorders Among Health Care Professionals - A Cross-Sectional Assessment of Risk Factors in A Tertiary Hospital, IndiaDocument14 paginiWork-Related Musculoskeletal Disorders Among Health Care Professionals - A Cross-Sectional Assessment of Risk Factors in A Tertiary Hospital, IndiaAqilah MahabirÎncă nu există evaluări
- Case 2 Acute Ischemic Stroke wk.6Document3 paginiCase 2 Acute Ischemic Stroke wk.6Nader AbdurasadÎncă nu există evaluări
- Bacte Lab - Laboratory Act 1Document4 paginiBacte Lab - Laboratory Act 1Eloisa LacanilaoÎncă nu există evaluări
- Session #1 SAS - AnaPhy (Lab)Document6 paginiSession #1 SAS - AnaPhy (Lab)Nicole Ken AgdanaÎncă nu există evaluări
- Context-Environment To Which Nursing Act Takes Place Content - Subject of Theory Process - Method by Which Nurse Acts in Nursing Theory NursingDocument22 paginiContext-Environment To Which Nursing Act Takes Place Content - Subject of Theory Process - Method by Which Nurse Acts in Nursing Theory NursingShyenÎncă nu există evaluări
- Formulating HypothesisDocument3 paginiFormulating HypothesisMatthew Lim MontenegroÎncă nu există evaluări
- Checklist Assessment of The Eyes and Visual Acuity2021 22Document3 paginiChecklist Assessment of The Eyes and Visual Acuity2021 22Trisha SabaÎncă nu există evaluări
- NSTP LawDocument3 paginiNSTP LawChan ReyÎncă nu există evaluări
- The 5 Steps of The Nursing ProcessDocument2 paginiThe 5 Steps of The Nursing ProcessManish DafdaÎncă nu există evaluări
- Anaphy Lab 1-4Document9 paginiAnaphy Lab 1-4Krisha Mae PascuaÎncă nu există evaluări
- Nursing Care of at RiskDocument7 paginiNursing Care of at RiskdominicjimenezÎncă nu există evaluări
- Legal Aspects of Nursing Study GuideDocument9 paginiLegal Aspects of Nursing Study GuideZsyd GelladugaÎncă nu există evaluări
- UNIT-6 Muscular SystemDocument48 paginiUNIT-6 Muscular SystemChandan ShahÎncă nu există evaluări
- Marc Johanna L. Villacora Activity 2.1 Citizenship TrainingDocument6 paginiMarc Johanna L. Villacora Activity 2.1 Citizenship TrainingDhision VillacoraÎncă nu există evaluări
- Fundamentals of Nursing p.1-37Document38 paginiFundamentals of Nursing p.1-37Wik Wik PantuaÎncă nu există evaluări
- Adrenocortical AgentsDocument14 paginiAdrenocortical AgentsFredie O HadjimudinÎncă nu există evaluări
- PR1Document2 paginiPR1John ReyÎncă nu există evaluări
- FluidDocument3 paginiFluidcruzjuan58Încă nu există evaluări
- Reviewer - (Ncma 217) - Q&aDocument10 paginiReviewer - (Ncma 217) - Q&aJeannelle UngrianoÎncă nu există evaluări
- Unit 5 Test - Muscular SystemDocument5 paginiUnit 5 Test - Muscular SystemAmanuelÎncă nu există evaluări
- MEMORIZE NOTES AND IMPROVE RECALL WITH THESE TECHNIQUESDocument34 paginiMEMORIZE NOTES AND IMPROVE RECALL WITH THESE TECHNIQUESJerwin SamsonÎncă nu există evaluări
- Children's Respiratory NursingDe la EverandChildren's Respiratory NursingJanice MightenÎncă nu există evaluări
- BME205 - Lecture 2 - Intro To Ana and PhyDocument26 paginiBME205 - Lecture 2 - Intro To Ana and Phyahmed rifatÎncă nu există evaluări
- Introduction to Human Anatomy and PhysiologyDocument28 paginiIntroduction to Human Anatomy and PhysiologyMahar1986Încă nu există evaluări
- Intro To Human Anatomy & Physiology: Quick Review Notes Chapter 1De la EverandIntro To Human Anatomy & Physiology: Quick Review Notes Chapter 1Încă nu există evaluări
- Complementary and Alternative MedicineDocument35 paginiComplementary and Alternative MedicineJSeasharkÎncă nu există evaluări
- Nose, Mouth & Throat A&pDocument13 paginiNose, Mouth & Throat A&pJSeashark83% (6)
- Eyes A&pDocument18 paginiEyes A&pJSeashark100% (1)
- Nursing Care For Patients With Ear, Eye, Nose &throat2Document37 paginiNursing Care For Patients With Ear, Eye, Nose &throat2JSeashark100% (1)
- Intergumentary SystemDocument8 paginiIntergumentary SystemJSeasharkÎncă nu există evaluări
- Drugs in Psychiatric NursingDocument38 paginiDrugs in Psychiatric NursingJSeasharkÎncă nu există evaluări
- David Phelps - Revetion AlbumDocument11 paginiDavid Phelps - Revetion AlbumJSeasharkÎncă nu există evaluări
- Head & Neck A&pDocument15 paginiHead & Neck A&pJSeashark100% (6)
- Ears A&pDocument11 paginiEars A&pJSeasharkÎncă nu există evaluări
- Selecting The Population and Sample: Welcome A. RavonoDocument21 paginiSelecting The Population and Sample: Welcome A. RavonoJSeasharkÎncă nu există evaluări
- Du 63 OpioidDocument2 paginiDu 63 OpioidJSeasharkÎncă nu există evaluări
- Class 2012 - Muscular System - 2Document47 paginiClass 2012 - Muscular System - 2JSeasharkÎncă nu există evaluări
- Introduction To Research 2Document27 paginiIntroduction To Research 2JSeasharkÎncă nu există evaluări
- Overvriew: Antidepressants Analgesics: Central Peripheral Mechanisms ActionDocument9 paginiOvervriew: Antidepressants Analgesics: Central Peripheral Mechanisms ActionJSeasharkÎncă nu există evaluări
- Muscular SystemDocument29 paginiMuscular SystemJSeasharkÎncă nu există evaluări
- Chapter 8 Appendicular Skeleton MariebDocument21 paginiChapter 8 Appendicular Skeleton MariebJSeasharkÎncă nu există evaluări
- Cellular & Tissue Level of OrganizationDocument44 paginiCellular & Tissue Level of OrganizationJSeashark100% (1)
- Chemical Level of IonDocument20 paginiChemical Level of IonJSeasharkÎncă nu există evaluări
- Chap 01 OutDocument11 paginiChap 01 OutJSeasharkÎncă nu există evaluări
- Glascow Coma ScaleDocument10 paginiGlascow Coma ScaleJSeasharkÎncă nu există evaluări
- Step 10 Communicting FindingsDocument10 paginiStep 10 Communicting FindingsJSeasharkÎncă nu există evaluări
- Brjcancersuppl00077 0015Document2 paginiBrjcancersuppl00077 0015JSeasharkÎncă nu există evaluări
- WK3 FNPDocument12 paginiWK3 FNPJSeasharkÎncă nu există evaluări
- Nursing Care For Patients With Ear, Eye, Nose &throat2Document37 paginiNursing Care For Patients With Ear, Eye, Nose &throat2JSeashark100% (1)
- Theme 1 Week 1 Yr 2Document80 paginiTheme 1 Week 1 Yr 2JSeasharkÎncă nu există evaluări
- Management of Musculoskeletal DisordersDocument69 paginiManagement of Musculoskeletal DisordersJSeasharkÎncă nu există evaluări
- WK 4 NFP 202Document35 paginiWK 4 NFP 202JSeasharkÎncă nu există evaluări
- WK 3 Nervous System 202Document67 paginiWK 3 Nervous System 202JSeasharkÎncă nu există evaluări
- Home VisitingDocument55 paginiHome VisitingJSeasharkÎncă nu există evaluări
- Whois contact details list with domainsDocument35 paginiWhois contact details list with domainsPrakash NÎncă nu există evaluări
- Hume's Standard TasteDocument15 paginiHume's Standard TasteAli Majid HameedÎncă nu există evaluări
- Inferences Worksheet 6Document2 paginiInferences Worksheet 6Alyssa L0% (1)
- HRM Unit 2Document69 paginiHRM Unit 2ranjan_prashant52Încă nu există evaluări
- Miriam Garcia Resume 2 1Document2 paginiMiriam Garcia Resume 2 1api-548501562Încă nu există evaluări
- Hbo Chapter 6 Theories of MotivationDocument29 paginiHbo Chapter 6 Theories of MotivationJannelle SalacÎncă nu există evaluări
- Unit 2 - Programming of 8085 MicroprocessorDocument32 paginiUnit 2 - Programming of 8085 MicroprocessorSathiyarajÎncă nu există evaluări
- Agriculture Term Paper TopicsDocument5 paginiAgriculture Term Paper Topicsfuhukuheseg2100% (1)
- Financial Management Module - 3Document2 paginiFinancial Management Module - 3Roel AsduloÎncă nu există evaluări
- Booklet - CopyxDocument20 paginiBooklet - CopyxHåkon HallenbergÎncă nu există evaluări
- Tattva Sandoha PujaDocument2 paginiTattva Sandoha PujaSathis KumarÎncă nu există evaluări
- 9 Specific Relief Act, 1877Document20 pagini9 Specific Relief Act, 1877mostafa faisalÎncă nu există evaluări
- Message and Responses From TaoshobuddhaDocument4 paginiMessage and Responses From TaoshobuddhaTaoshobuddhaÎncă nu există evaluări
- AL E C Usda S W P: OOK AT THE Ngineering Hallenges OF THE Mall Atershed RogramDocument6 paginiAL E C Usda S W P: OOK AT THE Ngineering Hallenges OF THE Mall Atershed RogramFranciscoÎncă nu există evaluări
- Asian Paints SmartCare Damp Proof Warranty for TerracesDocument11 paginiAsian Paints SmartCare Damp Proof Warranty for Terracesiman.krisman2109Încă nu există evaluări
- Evolution of The Indian Legal System 2Document7 paginiEvolution of The Indian Legal System 2Akhil YarramreddyÎncă nu există evaluări
- General Physics 1: Activity Title: What Forces You? Activity No.: 1.3 Learning Competency: Draw Free-Body DiagramsDocument5 paginiGeneral Physics 1: Activity Title: What Forces You? Activity No.: 1.3 Learning Competency: Draw Free-Body DiagramsLeonardo PigaÎncă nu există evaluări
- Investigation of Cyber CrimesDocument9 paginiInvestigation of Cyber CrimesHitesh BansalÎncă nu există evaluări
- Case Digest in Special ProceedingsDocument42 paginiCase Digest in Special ProceedingsGuiller MagsumbolÎncă nu există evaluări
- Module 3 - Risk Based Inspection (RBI) Based On API and ASMEDocument4 paginiModule 3 - Risk Based Inspection (RBI) Based On API and ASMEAgustin A.Încă nu există evaluări
- Special Blood CollectionDocument99 paginiSpecial Blood CollectionVenomÎncă nu există evaluări
- Alluring 60 Dome MosqueDocument6 paginiAlluring 60 Dome Mosqueself sayidÎncă nu există evaluări
- CA - Indonesia Digital Business Trend Final 2 Agust 2017Document38 paginiCA - Indonesia Digital Business Trend Final 2 Agust 2017silver8700Încă nu există evaluări
- Math 8 1 - 31Document29 paginiMath 8 1 - 31Emvie Loyd Pagunsan-ItableÎncă nu există evaluări
- M8 UTS A. Sexual SelfDocument10 paginiM8 UTS A. Sexual SelfAnon UnoÎncă nu există evaluări
- Court Reviews Liability of Staffing Agency for Damages Caused by Employee StrikeDocument5 paginiCourt Reviews Liability of Staffing Agency for Damages Caused by Employee StrikeDenzhu MarcuÎncă nu există evaluări
- FI - Primeiro Kfir 1975 - 1254 PDFDocument1 paginăFI - Primeiro Kfir 1975 - 1254 PDFguilhermeÎncă nu există evaluări
- Archives of Gerontology and Geriatrics: Naile Bilgili, Fatma ArpacıDocument7 paginiArchives of Gerontology and Geriatrics: Naile Bilgili, Fatma ArpacıIsyfaun NisaÎncă nu există evaluări
- Presentations - Benefits of WalkingDocument1 paginăPresentations - Benefits of WalkingEde Mehta WardhanaÎncă nu există evaluări
- Álvaro García Linera A Marxist Seduced BookDocument47 paginiÁlvaro García Linera A Marxist Seduced BookTomás TorresÎncă nu există evaluări