Documente Academic
Documente Profesional
Documente Cultură
Ecg 1
Încărcat de
Lindsay Ann Garcia MariacaDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Ecg 1
Încărcat de
Lindsay Ann Garcia MariacaDrepturi de autor:
Formate disponibile
ECG INTERPRETATION
Definition of terms: 1. Electrocardiogram is an essential tool in evaluating the hearts rhythm and signs of ischemia. 2. Electrocardiography a transthoracic interpretation of the electrical activity of the heart over a period of time, as detected by electrodes attached to the outer space of the skin and recorded by a device external to the body. 3. ECG complex waveform representing electrical events of one cardiac cycle - consists of 5 main waveform: P,Q, R,S,T 4. Rhythm Strip length of ECG paper that shows multiple ECG complexes representing a picture of the hearts electrical activity in a specific lead. 5. Electrodes a conductor through which electricity enters/leaves something such as battery/ a piece of electrical equipment. 6. Lead provides a view of the hearts electrical activity between 2 points/poles 7. Plane is a cross section of the heart which provides a different view of the hearts electrical activity. 8. Depolarization response of a myocardial cell to an electrical impulse that causes movement of ions across the cell membrane which triggers myocardial contraction. 9. Repolarization recovery of the myocardial cells after depolarization during which the cell membrane returns to its resting potential.
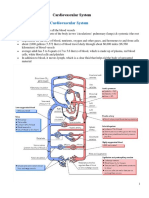
ANATOMY AND PHYSIOLOGY HEART - a hollow,muscular organ that works like a mechanical pump - delivers oxygenated blood to the body through the arteries - located between the lungs and in front of the spine - the bottom of the heart called the apex Heart wall (3 layers) 1. Epicardium 2. Myocardium - thickest later; contracts with each heartbeat 3. Endocardium - thin layer of the endothelial tissue Pericardium - fluid filled sac that envelopes heart and acts as tough protective coating 2 types:
1. fibrous pericardium 2. serous pericardium 2 layers: a. parietal layer - envelopes the visceral pericardium b. visceral layer - adheres to the pericardium Pericardial space - separates the visceral and parietal layer - contains 10-20mL of thin, clear pericardial fluid that lubricates the 2 surfaces. Heart chambers - 4 chambers, 2 atria, 2 ventricles 1. Right atrium - deoxygenated blood 2. Left atrium - oxygenated blood 3. Right ventricle 4. Left ventricle Heart valves - to keep blood flowing through the heart 2 AV valves 1. Tricuspid valve - separates the right atrium from right ventricle 2. Mitral valve - separates the left atrium from the left ventricle 2 Semilunar valves 1. pulmonic valve 2. aortic valve Coronary blood supply - main coronary arteries lie on the surfaces of the heart - the heart receiver its blood supply almost coordinating through the coronary arteries. Coronary arteries Right coronary arteries - supplies blood to the right atrium, right ventricles the inferior wall of the left ventricle Posterior descending artery - supplies blood
Left main coronary artery - splits into 2 major branches a. left anterior descending artery - supplies blood to the anterior wall b. left circumflex artery - provides blood to the lateral wall of the left ventricle and left atrium
TRANSMISSION OF ELECTRICAL IMPLUSES: 1. Automaticity - pacemaker - a cells ability to spontaneously initiates on electrical impulse 2. Excitability - the cells ability to respond to an electrical stimulus 3. Conductivity - ability of a cell to transmit an electrical impulse from one 4. Contractility - the cells ability to contract after receiving a stimulus by shortening and lengthening its muscle fibers. Depolarization and Repolarization - cardiac cells at rest are considered polarized, meaning that no electrical activity false places. Depolarization and Repolarization cycle 1. Phase 0 RAPID DEPOLARIZATION - the cell receives a stimulus, usually from a neighboring cell. 2. Phase 1 EARLY REPOLARIZATION - Na channels close and Na stops flowing into the cell. 3. Phase 2 PLATEAU PHASE - Ca continues 4. Phase 3 RAPID REPOLARIZATION - cell membrane is impermeable to Na - K more our of the cell
- by the end of this phase, the cell is ready for another stimulus
Cardiac Veins - the heart has its own veins, which remove oxygen depleted blood for the myocardium approximately 75% of the total coronary venous blood flow leaves. Cardiac Cycle: Ventricular Diastole(relaxation) - blood flows from from the atria into the relaxed ventricles. - atrial contraction(atrial kick) contributes to another 25% to ventricular filling Ventricular systole(contraction) - the ventricle contract ad blood is ejected into the pulmonic and systemic circulation PHASES OF THE CARDIAC CYCLE 1. Isovolumetric ventricular contraction - in response to ventricular depolarization tension in the ventricles increases. 2. Ventricular ejection - when ventricular pressure falls below the pressures in the aorta and pulmonary artery pressure, the aorta and pulmonic valves open and the ventricles eject blood. 3. Isovolumetric relaxation - when ventricular pressure falls below the pressures in the aorta and pulmonary artery, the aortic and pulmonic valves close. - cells valves are closed during this place. 4. Ventricular filling - atrial pressure exceeds ventricular pressure, which causes the mitral and tricuspid valves to open. - blood then flow passively into the ventricles - about 70% of ventricular filling takes. 5. Atrial systole(atrial kick) - atrial systole(considering the take ventricular diastole) supplies the ventricles with the remaining 30% of the blood.
S-ar putea să vă placă și
- Powermatic 58480438-Millrite-Mvn-Manual PDFDocument54 paginiPowermatic 58480438-Millrite-Mvn-Manual PDFJason Willis75% (4)
- 6th Grade Spelling ListsDocument10 pagini6th Grade Spelling Listsapi-326416336Încă nu există evaluări
- Anatomy & Physiology of Heart: BY: Mr. Anurag Lecturer College of Nursing DMC & H, LudhianaDocument56 paginiAnatomy & Physiology of Heart: BY: Mr. Anurag Lecturer College of Nursing DMC & H, Ludhianapreet kaurÎncă nu există evaluări
- Regulation of Heart Rate, Stroke Volume, Cardiac Output, Blood FlowDocument20 paginiRegulation of Heart Rate, Stroke Volume, Cardiac Output, Blood FlowShveta MahajanÎncă nu există evaluări
- Physiology of The Cardiovascular System-CVSDocument56 paginiPhysiology of The Cardiovascular System-CVSAmanuel MaruÎncă nu există evaluări
- Pharmacology SummaryDocument32 paginiPharmacology Summaryminikatiting95% (22)
- Lecture 3 Cardiovascular System 1Document54 paginiLecture 3 Cardiovascular System 1hafiz patah100% (1)
- NCM 103-Cardio Anatomy & PhysioDocument56 paginiNCM 103-Cardio Anatomy & Physiolouradel100% (1)
- Physiology of The Cardiovascular System-CVSDocument56 paginiPhysiology of The Cardiovascular System-CVSAmanuel MaruÎncă nu există evaluări
- Heart Anatomy: LocationDocument45 paginiHeart Anatomy: LocationZaira100% (1)
- Cardiovascular System - Lecture 3-2018-2019 PDFDocument27 paginiCardiovascular System - Lecture 3-2018-2019 PDFMary100% (1)
- Lecture - 3 Properties of Cardiac MuscleDocument35 paginiLecture - 3 Properties of Cardiac MuscleMRM7MDÎncă nu există evaluări
- Republic Act No. 10070Document3 paginiRepublic Act No. 10070Ganiela MCÎncă nu există evaluări
- Reading Test - 3 Clinical Depression Text ADocument17 paginiReading Test - 3 Clinical Depression Text AJisha JanardhanÎncă nu există evaluări
- Chapter 16 Anatomy of The HeartDocument5 paginiChapter 16 Anatomy of The Heartphotojockey18Încă nu există evaluări
- Anatomy and Physiology of The HeartDocument9 paginiAnatomy and Physiology of The HeartNina Anne ParacadÎncă nu există evaluări
- Contoh Perhitungan DDD Excell - IRNADocument8 paginiContoh Perhitungan DDD Excell - IRNAMaya DamanikÎncă nu există evaluări
- Lesson 3Document71 paginiLesson 3Angel joyce ValenciaÎncă nu există evaluări
- NICUDocument15 paginiNICUkavyarkrnagarÎncă nu există evaluări
- Linkage 2 Lab ReportDocument25 paginiLinkage 2 Lab Reportapi-25176084883% (6)
- NCM Responses To Altered Oxygenation Cardiac FunctionDocument14 paginiNCM Responses To Altered Oxygenation Cardiac FunctionJeson Vien GuerraÎncă nu există evaluări
- Cardiovascular System: Claire R. Hatton, RN, MANDocument63 paginiCardiovascular System: Claire R. Hatton, RN, MANrhimineecat71Încă nu există evaluări
- Cardiovascular SystemDocument8 paginiCardiovascular Systemomar farooqÎncă nu există evaluări
- Cardiovascular System SheetDocument11 paginiCardiovascular System SheetBetsy Brown ByersmithÎncă nu există evaluări
- Cardiovascular System SheetDocument11 paginiCardiovascular System SheetBetsy Brown ByersmithÎncă nu există evaluări
- HeartDocument7 paginiHeartKaryll AguilaÎncă nu există evaluări
- The Circulatory SystemDocument53 paginiThe Circulatory SystemVera June RañesesÎncă nu există evaluări
- Care of Patient With 1Document12 paginiCare of Patient With 1jrjr88Încă nu există evaluări
- CardioDocument30 paginiCardioPamela LusungÎncă nu există evaluări
- Pharmacology SummaryDocument31 paginiPharmacology Summarydesshe09Încă nu există evaluări
- Structure and Function of The Cardiovascular System PDFDocument9 paginiStructure and Function of The Cardiovascular System PDFteuuuuÎncă nu există evaluări
- Heart Physiology and DisordersDocument9 paginiHeart Physiology and DisordersLottie EvansÎncă nu există evaluări
- Cardiac AssessmentDocument54 paginiCardiac AssessmentAthira PSÎncă nu există evaluări
- 1 Anatomy and PhysiologyDocument25 pagini1 Anatomy and PhysiologyMichelle Dona MirallesÎncă nu există evaluări
- Cardiovascular System BSN 1Document16 paginiCardiovascular System BSN 1Arianne Jen GenotivaÎncă nu există evaluări
- Chapter 20 - Introduction To The Cardiovascular System: Away From To BetweenDocument6 paginiChapter 20 - Introduction To The Cardiovascular System: Away From To Betweentomorrow.today.yesterday .yesterdayÎncă nu există evaluări
- Components of The Cardiovascular SystemDocument23 paginiComponents of The Cardiovascular SystemMr. DummyÎncă nu există evaluări
- Lecture 2: The Heart: Prof. Magidah Alaudi, M.SCDocument62 paginiLecture 2: The Heart: Prof. Magidah Alaudi, M.SCMonicaÎncă nu există evaluări
- Lab 9 - Circulatory SystemDocument3 paginiLab 9 - Circulatory SystemClobelle Marie SiachuaÎncă nu există evaluări
- Cardiovascular System (Report)Document2 paginiCardiovascular System (Report)Arlan AbraganÎncă nu există evaluări
- NCMMSN Notes - Sacramento, Karl SebastianDocument96 paginiNCMMSN Notes - Sacramento, Karl SebastianRHEA MAY CAPORÎncă nu există evaluări
- CARDIOVASCULARDocument41 paginiCARDIOVASCULARNor Jeannah PolaoÎncă nu există evaluări
- Cardiac Ana & DxticsDocument3 paginiCardiac Ana & Dxticsjames garciaÎncă nu există evaluări
- Lecture 5 (Heart)Document10 paginiLecture 5 (Heart)Άγγελος ΧαβέλαςÎncă nu există evaluări
- Electrical Conduction System of The HeartDocument27 paginiElectrical Conduction System of The HeartAnonymous gUjimJKÎncă nu există evaluări
- Animal Physiolgy. Lec4Document22 paginiAnimal Physiolgy. Lec4ao868598Încă nu există evaluări
- Week 9 CVS WorkbookDocument24 paginiWeek 9 CVS Workbooksupriyakunwar2019Încă nu există evaluări
- Physiology of The Cardiovascular System-CVSDocument56 paginiPhysiology of The Cardiovascular System-CVSAmanuel MaruÎncă nu există evaluări
- Pedrajeta-Heart and Neck Vessels AssessmentDocument4 paginiPedrajeta-Heart and Neck Vessels AssessmentAndrei PedrajetaÎncă nu există evaluări
- L6 7 CVS (2022) PDFDocument51 paginiL6 7 CVS (2022) PDFFung Shan CheungÎncă nu există evaluări
- Heart ChambersDocument14 paginiHeart Chambersberniebernie20Încă nu există evaluări
- Conduction System of HeartDocument7 paginiConduction System of HeartThakur KanchanÎncă nu există evaluări
- EKG Study Guide RevisedDocument29 paginiEKG Study Guide Revisedflashyboy506Încă nu există evaluări
- Circulatory System - Deliver Oxygen and Nutrients - Carries Waste Products - Circulates Electrolytes (Na, K, Ca) andDocument4 paginiCirculatory System - Deliver Oxygen and Nutrients - Carries Waste Products - Circulates Electrolytes (Na, K, Ca) andyoonie catÎncă nu există evaluări
- Functional Human Physiology: For The Exercise and Sport Sciences The Cardiovascular System: Cardiac FunctionDocument186 paginiFunctional Human Physiology: For The Exercise and Sport Sciences The Cardiovascular System: Cardiac FunctionBery Agana F. PurbaÎncă nu există evaluări
- Cardiovascular SystemDocument7 paginiCardiovascular SystemJoão EusébioÎncă nu există evaluări
- Oral RevDocument6 paginiOral RevjjolaguerÎncă nu există evaluări
- Cardio PulmonaryDocument4 paginiCardio PulmonaryAyessa CortesÎncă nu există evaluări
- Cardiac - Lect 1Document14 paginiCardiac - Lect 1كسلان اكتب اسميÎncă nu există evaluări
- Cardiovascular SystemDocument77 paginiCardiovascular SystemAyesha100% (1)
- Basic Principles of ECG InterpretationDocument26 paginiBasic Principles of ECG Interpretationgosai83Încă nu există evaluări
- Heart 2018 - Part IDocument57 paginiHeart 2018 - Part Iwww.hudevaa6Încă nu există evaluări
- Group 4-6: Electrocardiogram: AuriclesDocument2 paginiGroup 4-6: Electrocardiogram: AuriclesValeriaÎncă nu există evaluări
- Module 5 CardioVascular SystemDocument7 paginiModule 5 CardioVascular SystemWai KikiÎncă nu există evaluări
- Cardiovascular System LectureDocument5 paginiCardiovascular System LectureMarci MunirÎncă nu există evaluări
- Continuations of Report by Ritz and QuinnyDocument7 paginiContinuations of Report by Ritz and QuinnyLindsay Ann Garcia MariacaÎncă nu există evaluări
- Open Reduction and Internal Fixation SurgerybyDocument3 paginiOpen Reduction and Internal Fixation SurgerybyLindsay Ann Garcia MariacaÎncă nu există evaluări
- Digestive SystemDocument7 paginiDigestive SystemLindsay Ann Garcia MariacaÎncă nu există evaluări
- Preparing DisinfectantsDocument16 paginiPreparing DisinfectantsLindsay Ann Garcia MariacaÎncă nu există evaluări
- Adrenal GlandsDocument26 paginiAdrenal GlandsLindsay Ann Garcia MariacaÎncă nu există evaluări
- HTP AmoebiasisDocument5 paginiHTP AmoebiasisLindsay Ann Garcia MariacaÎncă nu există evaluări
- Fourth Stage of LaborDocument13 paginiFourth Stage of LaborLindsay Ann Garcia Mariaca0% (1)
- Mongan Method For Hypnobirth: HypnobirthingDocument3 paginiMongan Method For Hypnobirth: HypnobirthingLindsay Ann Garcia MariacaÎncă nu există evaluări
- Textile Reinforced - Cold Splice - Final 14 MRCH 2018Document25 paginiTextile Reinforced - Cold Splice - Final 14 MRCH 2018Shariq KhanÎncă nu există evaluări
- OPzS Solar - Power En0213Document2 paginiOPzS Solar - Power En0213janiankoÎncă nu există evaluări
- Chuyên Anh S Hà N I 2021Document5 paginiChuyên Anh S Hà N I 2021Jennifer WatsonÎncă nu există evaluări
- Pengaruh Pembangunan Center Point of IndDocument11 paginiPengaruh Pembangunan Center Point of IndSumitro SafiuddinÎncă nu există evaluări
- What Is A Solar Storm?Document2 paginiWhat Is A Solar Storm?Shawn SriramÎncă nu există evaluări
- GLYSANTIN+G48+bg+IN 000000000030667689 SDS GEN US en 8-1Document11 paginiGLYSANTIN+G48+bg+IN 000000000030667689 SDS GEN US en 8-1Ali RidloÎncă nu există evaluări
- 5219-PRP Support Tool CounsellingDocument10 pagini5219-PRP Support Tool CounsellingRodhi AnshariÎncă nu există evaluări
- 936-Article Text-2359-1-10-20211003Document6 pagini936-Article Text-2359-1-10-20211003Geka KusumoÎncă nu există evaluări
- EC Type-Examination Certificate: Reg.-No.: 01/205/5192.02/18Document11 paginiEC Type-Examination Certificate: Reg.-No.: 01/205/5192.02/18Orlando Ortiz VillegasÎncă nu există evaluări
- DoDough FriedDocument7 paginiDoDough FriedDana Geli100% (1)
- 9701 w03 QP 4Document12 pagini9701 w03 QP 4Hubbak KhanÎncă nu există evaluări
- EarthWear Clothier MaterialsDocument1 paginăEarthWear Clothier MaterialsZhining LimÎncă nu există evaluări
- MCQSDocument25 paginiMCQSAsifa Liaqat0% (1)
- SCL NotesDocument4 paginiSCL NotesmayaÎncă nu există evaluări
- Copd 9 027Document13 paginiCopd 9 027Yussuf MuhammadÎncă nu există evaluări
- The Many Uses of Transmission Line ArrestersDocument8 paginiThe Many Uses of Transmission Line ArrestersVK DharmikaÎncă nu există evaluări
- Strep Throat FactsDocument2 paginiStrep Throat FactsFactPaloozaÎncă nu există evaluări
- ANNEX I of Machinery Directive 2006 - 42 - EC - Summary - Machinery Directive 2006 - 42 - CE - Functional Safety & ATEX Directive 2014 - 34 - EUDocument6 paginiANNEX I of Machinery Directive 2006 - 42 - EC - Summary - Machinery Directive 2006 - 42 - CE - Functional Safety & ATEX Directive 2014 - 34 - EUAnandababuÎncă nu există evaluări
- Man Wah Ranked As Top 10 Furniture Sources For U.S. MarketDocument2 paginiMan Wah Ranked As Top 10 Furniture Sources For U.S. MarketWeR1 Consultants Pte LtdÎncă nu există evaluări
- Ronnel Del RioDocument5 paginiRonnel Del Rioamity balweg100% (2)
- CW Catalogue Cables and Wires A4 En-2Document1.156 paginiCW Catalogue Cables and Wires A4 En-2Ovidiu PuieÎncă nu există evaluări
- Boge FLEX PET SystemsDocument4 paginiBoge FLEX PET SystemsAir Repair, LLCÎncă nu există evaluări
- CA02 ParchamentoJVMDocument6 paginiCA02 ParchamentoJVMJohnrey ParchamentoÎncă nu există evaluări