Documente Academic
Documente Profesional
Documente Cultură
Warf Side Effects
Încărcat de
Pankaj SharmaDescriere originală:
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Warf Side Effects
Încărcat de
Pankaj SharmaDrepturi de autor:
Formate disponibile
Question
Warfarin: Any harm in long-term use?
Is there any harm in taking long-term, low-dose warfarin for an extended period after an episode of deep vein thrombosis?
Answer
from Martha Grogan, M.D.
Warfarin (Coumadin) is a blood-thinning medication (anticoagulant) used to treat and prevent blood clots. For most people with a single episode of deep vein thrombosis (DVT), treatment with full-dose blood thinners is usually for only a limited time. Taking warfarin at a high dose for a longer period of time is only recommended for people who are at a high risk of developing blood clots that could cause a heart attack, stroke or pulmonary embolism.
Long-term, low-dose treatment with warfarin may prevent future episodes of DVT, but it's not without risk. There's a risk of serious or even fatal bleeding especially when warfarin is taken in high doses or for long periods of time.
Ask your doctor to help you weigh the benefits and risks of long-term, low-dose warfarin therapy in your case. Also consider these self-care measures to prevent future episodes of DVT:
Avoid sitting, squatting or crossing your legs for long periods of time. If you must sit for long periods, such as during a plane or car trip, take a short walk every hour or two. It also helps to flex your ankles, curl your toes and tap your feet frequently.
Drink plenty of fluids to prevent dehydration. Wear support hosiery or compression stockings, available at medical supply stores. If you're taking warfarin to prevent blood clots that could cause a heart attack or stroke, make sure you take it exactly as prescribed. Warfarin is a powerful medication that can have dangerous side effects.
Warfarin side effects: Watch for interactions
Although commonly used to treat blood clots, warfarin (Coumadin) can have dangerous side effects or interactions that can place you at risk of bleeding. Here are precautions to take to avoid warfarin side effects.
By Mayo Clinic staff If you've been prescribed warfarin (Coumadin, Jantoven) to prevent blood clots, you probably already know that this powerful drug can save your life if you're at risk of or have had blood clots. But you may not realize how serious warfarin side effects can be. Warfarin, especially if taken incorrectly, increases your risk of dangerous bleeding. Warfarin side effects can also include interactions with some foods, prescription medicines and over-thecounter supplements.
If your doctor prescribes warfarin for you, make sure you understand all the potential warfarin side effects and interactions it could have.
When is warfarin prescribed?
You might be given warfarin if you have:
A blood clot in or near your heart that could trigger stroke, heart attack or organ damage A blood clot in your lungs (pulmonary embolism) A blood clot elsewhere in your body (venous thrombosis) A high risk of blood clots forming in the heart, such as in some heart rhythm abnormalities (arrhythmias) A mechanical artificial heart valve that is prone to forming blood clots
What warfarin side effects should you watch for?
When you take warfarin, your blood won't clot as easily. If you accidentally cut yourself while taking warfarin, you may bleed heavily. You're more likely to have bleeding problems if you're older than 75 or take other blood-thinning medications that can further increase your bleeding risk.
Warfarin side effects that require immediate medical attention
Severe bleeding Black stool or bleeding from the rectum Skin conditions such as hives, a rash or itching Swelling of the face, throat, mouth, legs, feet or hands Bruising that comes about without an injury you remember Chest pain or pressure Nausea or vomiting Fever or flu-like symptoms Joint or muscle aches
Diarrhea Difficulty moving Numbness or tingling in any part of your body Painful erection lasting four hours or longer Although rare, warfarin can also cause skin tissue death (necrosis) and gangrene requiring amputation. This complication most often happens three to eight days after you start taking warfarin. If you notice any sores, changes in skin color or temperature, or severe pain on your skin, notify your doctor immediately.
Less serious warfarin side effects to tell your doctor about
Gas Feeling cold Fatigue Pale skin Changes in the way foods taste Hair loss
What precautions can you take against warfarin side effects?
There are some key steps you can take to reduce your chance of developing warfarin side effects.
Tell your doctor about any other medications or supplements you take. Many medications and supplements can have a dangerous interaction with warfarin.
Tell your health care provider you take warfarin before you have any medical or dental procedures. Tell providers that you take warfarin even before minor procedures, such as vaccinations and routine dental cleanings. If you're going to have surgery, discuss what dosing changes might be necessary at least 10 days before the procedure. Your doctor may decrease your dose of warfarin or discontinue warfarin altogether before the procedure. Talk to the doctor who prescribed warfarin to find out if it's safe to discontinue for a few days. If you are at high risk of blood clots, you may need a shorter acting blood thinner, heparin, to keep a lower risk of blood clots while you're not taking warfarin.
Avoid situations that increase your risk of injury. Avoid contact sports or activities that could result in head injury. Make sure you tell your doctor if you are unsteady while walking or have a history of falling.
Consider wearing a bracelet or carrying a card that identifies that you take warfarin. This can be useful if emergency medical personnel need to know what medications you take.
Consider a warfarin sensitivity test. About a third of the people who take warfarin are at a higher risk of bleeding because their genes make them more sensitive to warfarin. If you're worried that you might be more sensitive to warfarin because a family member experienced side effects, talk to
your doctor about taking a genetic warfarin sensitivity test. The test can tell if you have the genes that can increase your risk of bleeding, although researchers are still looking into whether genetic tests are more effective than carefully monitoring your body's response to warfarin.
If you receive new prescriptions from someone other than your usual medical provider, make sure to remind him or her that you're taking warfarin. Ask if you'll need additional blood tests from your regular care provider to make sure your blood clotting hasn't been affected by the new medications you're taking. Next (1 of 2) page
Mayo Clinic products and services Warfarin side effects: Watch for interactions What drugs and supplements can interact with warfarin?
Warfarin, like any other medication, can interact with foods, other drugs, vitamins or herbal supplements. Be ready to provide your doctor with a complete list of everything you're taking.
Drugs that can interact with warfarin include:
Aspirin or aspirin-containing products Ibuprofen (Advil, Motrin, others) or naproxen (Aleve, Anaprox) Acetaminophen (Tylenol, others) or acetaminophen-containing products, especially when the dose of acetaminophen exceeds 1,500 milligrams a day Many antibiotics Heparin Cold or allergy medicines Birth control pills Medications that treat abnormal heart rhythms, such as amiodarone This isn't a complete list. Many other medications interact with warfarin. You should always consider that a new medication could interact with warfarin until your doctor, nurse or pharmacist tells you otherwise.
Supplements that can interact with warfarin include:
Fish oil and omega-3 supplements Vitamin K Alfalfa Bromelains, a type of supplement that comes from pineapples (pineapple itself doesn't interact with warfarin) Coenzyme Q10 (ubidecarenone)
Cranberry extracts Danshen Dong quai Evening primrose oil Garlic Ginkgo biloba Ginseng Glucosamine St. John's wort Willow bark Wintergreen
What foods and drinks might interact with warfarin?
If you sometimes eat foods that are high in vitamin K such as soybean and canola oils, spinach or broccoli tell your doctor. Vitamin K can affect how your blood clots and how warfarin protects you.
Garlic and black licorice also may interact with warfarin, so talk to your doctor if you eat a lot of these foods.
Eating cranberries or drinking cranberry juice can affect the way warfarin works and can increase your risk of bleeding. While an occasional glass of cranberry juice is unlikely to injure you, you should avoid drinking it regularly.
Drinking alcohol also can affect the way warfarin works. Talk to your doctor about drinking alcohol while taking warfarin. While having an occasional drink shouldn't create a problem, excessive drinking or binge drinking can greatly increase your bleeding risk.
What should you do if you forget a dose?
If you forget to take a dose of warfarin within 12 hours of when you were supposed to take it, take it as soon as you remember and get back on your daily dosing schedule. If you forget to take a dose and it has been more than 12 hours, wait until the next dose is due. Unlike some other medications, doubling your warfarin dose could greatly increase your risk of side effects.
Always talk to your doctor if you're unsure if you took your warfarin as directed. If you follow your doctor's dosing instructions and tell all your health care providers that you take warfarin, you'll be at a much lower risk of dangerous interactions and warfarin side effects. Talk to your doctor, nurse or pharmacist if you have any concerns about warfarin. They can be a valuable source of information. Previous (2 of 2) page
Mayo Clinic products and services
Book: Mayo Clinic Family Health Book, 4th Edition Newsletter: Mayo Clinic Health Letter Give today to find cures for tomorrow
See Also
Warfarin: Any harm in long-term use? Blood thinners: Can I still get blood clots?
S-ar putea să vă placă și
- IS67 WarfarinDocument5 paginiIS67 WarfarinEnayat AlkozaiÎncă nu există evaluări
- WarfarinDocument8 paginiWarfarinJahzeel Shayne LauronÎncă nu există evaluări
- What Is Warfarin/Coumadin ?Document5 paginiWhat Is Warfarin/Coumadin ?Juan AcostaÎncă nu există evaluări
- Warfarin Coumadin BookletDocument12 paginiWarfarin Coumadin BookletRkkvanjÎncă nu există evaluări
- Warfarin Patient"s HandbookDocument16 paginiWarfarin Patient"s HandbookNavojit ChowdhuryÎncă nu există evaluări
- 100429warfarinchildren PDFDocument16 pagini100429warfarinchildren PDFFian AldyÎncă nu există evaluări
- Advair Uses, Dosage & Side EffectsDocument6 paginiAdvair Uses, Dosage & Side EffectspatgarettÎncă nu există evaluări
- ATV PfizerDocument5 paginiATV PfizerFaizah Min FadhlillahÎncă nu există evaluări
- Warfarin NOTESDocument8 paginiWarfarin NOTESSarah :-)Încă nu există evaluări
- High Blood Pressure: Medicines To Help YouDocument24 paginiHigh Blood Pressure: Medicines To Help YourfbruneiÎncă nu există evaluări
- Drug Information Abjad QDocument7 paginiDrug Information Abjad Qfransiska labuÎncă nu există evaluări
- NSF1526 FactSheet Medication WEBDocument2 paginiNSF1526 FactSheet Medication WEBherbalizer33Încă nu există evaluări
- Chemistry Project LightDocument6 paginiChemistry Project LightcytrfÎncă nu există evaluări
- Generic Name: Quinupristin/Dalfopristin - Injection (Kwin-ue-PRIS-tin/DAL-foe-PRIS-tin)Document4 paginiGeneric Name: Quinupristin/Dalfopristin - Injection (Kwin-ue-PRIS-tin/DAL-foe-PRIS-tin)Jrose CuerpoÎncă nu există evaluări
- Before Taking Losartan,: What Special Dietary Instructions Should I Follow?Document8 paginiBefore Taking Losartan,: What Special Dietary Instructions Should I Follow?Hillary Ann AbuelÎncă nu există evaluări
- Atorvastatin Patient LeafletDocument8 paginiAtorvastatin Patient LeafletKrupali TrivediÎncă nu există evaluări
- MF Taking Anticoagulation MedicineDocument5 paginiMF Taking Anticoagulation MedicineElteyb Nor eldaimÎncă nu există evaluări
- Antidepressants: What Every Patient Needs to KnowDe la EverandAntidepressants: What Every Patient Needs to KnowEvaluare: 5 din 5 stele5/5 (1)
- Dianette Patient Information LeafletDocument16 paginiDianette Patient Information LeafletAnonymousÎncă nu există evaluări
- Pil 1359Document20 paginiPil 1359Mary Grace Fabula CalloÎncă nu există evaluări
- Warfarin LeafletDocument2 paginiWarfarin LeafletchampbeeÎncă nu există evaluări
- Methods of Administration: (Deep Vein Thrombosis, or DVT) (Pulmonary Embolism)Document1 paginăMethods of Administration: (Deep Vein Thrombosis, or DVT) (Pulmonary Embolism)NJ CullaÎncă nu există evaluări
- Amcardia 5mg, 10mg (Amlodipine)Document4 paginiAmcardia 5mg, 10mg (Amlodipine)Bhakti A MagdalenaÎncă nu există evaluări
- Literature Review On WarfarinDocument8 paginiLiterature Review On Warfarinelfgxwwgf100% (1)
- Medication After TIA and Stroke Fact Sheet - Stroke Foundation - AustraliaDocument3 paginiMedication After TIA and Stroke Fact Sheet - Stroke Foundation - AustraliaAnonymous EAPbx6Încă nu există evaluări
- Co DiovanDocument8 paginiCo DiovanPeter Rey Tanio TeopeÎncă nu există evaluări
- Anticoagulation TherapyDocument1 paginăAnticoagulation Therapyshailesh284Încă nu există evaluări
- ZiagenDocument3 paginiZiagenHannah KoÎncă nu există evaluări
- Voltfast: Diclofenac Potassium 50mg Powder For Oral SolutionDocument5 paginiVoltfast: Diclofenac Potassium 50mg Powder For Oral Solutionanna lauÎncă nu există evaluări
- How to Lower Blood Pressure Naturally With Essential Oil: What Hypertension Is, Causes of High Pressure Symptoms and Fast RemediesDe la EverandHow to Lower Blood Pressure Naturally With Essential Oil: What Hypertension Is, Causes of High Pressure Symptoms and Fast RemediesEvaluare: 5 din 5 stele5/5 (1)
- Consumer Medicine Information Arrow - Ranitidine: What Is in This LeafletDocument8 paginiConsumer Medicine Information Arrow - Ranitidine: What Is in This LeafletmustikaarumÎncă nu există evaluări
- HTTPDocument4 paginiHTTPTran Thi Thu DungÎncă nu există evaluări
- Taking Aspirin During Late Pregnancy May Cause Bleeding in The Mother or The Baby During Delivery. Tell Your Doctor If You Are PregnantDocument11 paginiTaking Aspirin During Late Pregnancy May Cause Bleeding in The Mother or The Baby During Delivery. Tell Your Doctor If You Are Pregnant'Prasada WedatamaÎncă nu există evaluări
- Atrial Fibrillation and WarfarinDocument5 paginiAtrial Fibrillation and WarfarinJayson TrajanoÎncă nu există evaluări
- Daunorubicin PDFDocument2 paginiDaunorubicin PDFmilahÎncă nu există evaluări
- Drug StudyDocument32 paginiDrug StudyPrincess Gutierrez RositaÎncă nu există evaluări
- RocvaliuDocument4 paginiRocvaliuFastabiqul KhairatÎncă nu există evaluări
- Aspirin and DipyridamoleDocument6 paginiAspirin and DipyridamoleRoxana Aldea-CiaciruÎncă nu există evaluări
- List of AnticoagulantsDocument9 paginiList of Anticoagulantschristianz39100% (1)
- Irinotekan QILU-plDocument10 paginiIrinotekan QILU-plSrechko MilichÎncă nu există evaluări
- Valtan 160mg Film-Coated Tablets: Page 1 of 7Document7 paginiValtan 160mg Film-Coated Tablets: Page 1 of 7Osama AhmedÎncă nu există evaluări
- PACKAGE LEAFLET - CORDARONE EngDocument17 paginiPACKAGE LEAFLET - CORDARONE Engvaka17Încă nu există evaluări
- Anticoagulants and Antiplatelet Agents Ucm 310825Document2 paginiAnticoagulants and Antiplatelet Agents Ucm 310825sagor9364Încă nu există evaluări
- AmiodaroneDocument8 paginiAmiodaroneIlyes FerenczÎncă nu există evaluări
- Depakine Chrono PDFDocument8 paginiDepakine Chrono PDFadil yousafÎncă nu există evaluări
- How To Store Vitafen: 1. What Vitafen Is and What It Is Used ForDocument7 paginiHow To Store Vitafen: 1. What Vitafen Is and What It Is Used FornurfaaaÎncă nu există evaluări
- How To Start Warfarin TherapyDocument4 paginiHow To Start Warfarin TherapyMahmoud SelimÎncă nu există evaluări
- Atrial Fibrillation and Pradaxa: Jaclyn Davis, RNDocument40 paginiAtrial Fibrillation and Pradaxa: Jaclyn Davis, RNJaclyn Mattes DavisÎncă nu există evaluări
- Drug Medicine WardDocument3 paginiDrug Medicine WardDawn NavarroÎncă nu există evaluări
- What Is Ativan?: Expanding..Document10 paginiWhat Is Ativan?: Expanding..'Prasada WedatamaÎncă nu există evaluări
- How Should I Take Alprazolam?Document11 paginiHow Should I Take Alprazolam?'Prasada WedatamaÎncă nu există evaluări
- Quinine MalariaDocument32 paginiQuinine MalariaWendy TangÎncă nu există evaluări
- RanolazineDocument6 paginiRanolazineKristen FieldsÎncă nu există evaluări
- Deadly Drug: How I Safely Switched to Natural Blood ThinnersDe la EverandDeadly Drug: How I Safely Switched to Natural Blood ThinnersÎncă nu există evaluări
- Interactions Between Your DrugsDocument13 paginiInteractions Between Your DrugsSahera NurhidayahÎncă nu există evaluări
- Online VIREAD Tenofovir Disoproxil Fumarate Purchase With DiscountDocument5 paginiOnline VIREAD Tenofovir Disoproxil Fumarate Purchase With Discountcena heyÎncă nu există evaluări
- Drug Study For Syntocinon Potassium Chloride, and BuscopanDocument4 paginiDrug Study For Syntocinon Potassium Chloride, and BuscopanRj AlmarioÎncă nu există evaluări
- Dietary Advice For People Taking Warfarin TabletsDocument5 paginiDietary Advice For People Taking Warfarin TabletsNicoletta OrphanouÎncă nu există evaluări
- Ren TacDocument3 paginiRen TacampworkindiaÎncă nu există evaluări
- Problems With Tourism in IndiaDocument2 paginiProblems With Tourism in IndiaPankaj SharmaÎncă nu există evaluări
- 8 Impact of Training and Development On Organizational PerformanceDocument7 pagini8 Impact of Training and Development On Organizational PerformanceHelen GabrielÎncă nu există evaluări
- Problems With Tourism in IndiaDocument2 paginiProblems With Tourism in IndiaPankaj SharmaÎncă nu există evaluări
- Problems With Tourism in IndiaDocument2 paginiProblems With Tourism in IndiaPankaj SharmaÎncă nu există evaluări
- Cad BuryDocument5 paginiCad BuryPankaj SharmaÎncă nu există evaluări
- Moffett PPT Lect Ch17Document29 paginiMoffett PPT Lect Ch17Pankaj SharmaÎncă nu există evaluări
- Test Container Form Lab Process Remarks HKL (Hospital Appointment Date - Specialist's SignatureDocument9 paginiTest Container Form Lab Process Remarks HKL (Hospital Appointment Date - Specialist's SignaturesyasyaÎncă nu există evaluări
- NCRP 160 PDFDocument81 paginiNCRP 160 PDFmarkÎncă nu există evaluări
- FlaxDocument9 paginiFlaxXeeshan Rafique MirzaÎncă nu există evaluări
- Msds ChloroformDocument9 paginiMsds ChloroformAhmad ArisandiÎncă nu există evaluări
- ERCPDocument4 paginiERCPbilly wilsonÎncă nu există evaluări
- Adler With BiographyDocument38 paginiAdler With BiographyRhalfÎncă nu există evaluări
- Inheritance Biology EDUNCLEDocument54 paginiInheritance Biology EDUNCLEEvita Almeida100% (1)
- 24 Bio Fertilization of BananaDocument6 pagini24 Bio Fertilization of Bananamiceli57Încă nu există evaluări
- PowersDocument14 paginiPowersIvan SokolovÎncă nu există evaluări
- Fat Soluble VitaminsDocument20 paginiFat Soluble VitaminsWati WindayaniÎncă nu există evaluări
- Principles - of - Genetics 6th Ed by Snustad - 20 (PDF - Io) (PDF - Io) - 12-14-1-2Document2 paginiPrinciples - of - Genetics 6th Ed by Snustad - 20 (PDF - Io) (PDF - Io) - 12-14-1-2Ayu JumainÎncă nu există evaluări
- GMO Pro Arguments (Gen-WPS OfficeDocument4 paginiGMO Pro Arguments (Gen-WPS OfficeFranchesca RevelloÎncă nu există evaluări
- LAN Party Skate Park by Shane Jesse ChristmassDocument91 paginiLAN Party Skate Park by Shane Jesse ChristmassPatrick TrottiÎncă nu există evaluări
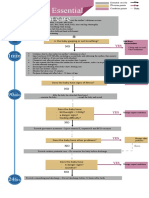
- Algorithm: Essential Newborn Care: Is The Baby Gasping or Not Breathing?Document1 paginăAlgorithm: Essential Newborn Care: Is The Baby Gasping or Not Breathing?Dela cruz KimberlyÎncă nu există evaluări
- Systemic Complications of Iv Therapy Complications Assessment Nursing Management Fluid OverloadDocument4 paginiSystemic Complications of Iv Therapy Complications Assessment Nursing Management Fluid OverloadMakagago And BruskoÎncă nu există evaluări
- Nursing Care of The Client With High-Risk Labor & DeliveryDocument10 paginiNursing Care of The Client With High-Risk Labor & DeliveryWilbert CabanbanÎncă nu există evaluări
- Farming Hirudo LeechesDocument46 paginiFarming Hirudo LeechesCatalin Cornel100% (1)
- University of Johannesburg MPH Reasearch Questionnaire Final Version JMDocument9 paginiUniversity of Johannesburg MPH Reasearch Questionnaire Final Version JMYvonne MankolaÎncă nu există evaluări
- CytokineDocument26 paginiCytokinePro KartuÎncă nu există evaluări
- Pathophysiology of Ischemic Stroke FinalDocument3 paginiPathophysiology of Ischemic Stroke FinalAcohCChao67% (3)
- Introduction of Magic Rose UpDocument21 paginiIntroduction of Magic Rose UpanggrainiÎncă nu există evaluări
- Development of The Vertebrate EyeDocument5 paginiDevelopment of The Vertebrate Eyezari_pak2010Încă nu există evaluări
- RUNDOWN ILMIAH TIPD 2021 29 SeptDocument8 paginiRUNDOWN ILMIAH TIPD 2021 29 SeptJessie AriniÎncă nu există evaluări
- ZFN, TALEN, and CRISPR-Cas-based Methods For Genome EngineeringDocument9 paginiZFN, TALEN, and CRISPR-Cas-based Methods For Genome EngineeringRomina Tamara Gil RamirezÎncă nu există evaluări
- CATHETERIZATIONDocument3 paginiCATHETERIZATIONrnrmmanphdÎncă nu există evaluări
- BELIZARIO VY Et Al Medical Parasitology in The Philippines 3e 158 226Document69 paginiBELIZARIO VY Et Al Medical Parasitology in The Philippines 3e 158 226Sharon Agor100% (1)
- Lesson 5 Core Elements Evidenced Based Gerontological Nursing PracticeDocument38 paginiLesson 5 Core Elements Evidenced Based Gerontological Nursing PracticeSam GarciaÎncă nu există evaluări
- DOPR Vision 2030Document36 paginiDOPR Vision 2030Hendi HendriansyahÎncă nu există evaluări
- Illness in The NewbornDocument34 paginiIllness in The NewbornVivian Jean TapayaÎncă nu există evaluări
- Cell Types Animal Tissue ReviewerDocument6 paginiCell Types Animal Tissue ReviewerShane LaluÎncă nu există evaluări