Documente Academic
Documente Profesional
Documente Cultură
Hearing Aids Final
Încărcat de
Vishal GauravDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Hearing Aids Final
Încărcat de
Vishal GauravDrepturi de autor:
Formate disponibile
HEARING AIDS
INTRODUCTORY CONCEPTS Hearing aids are the principal means of auditory rehabilitation for patients with sensorineural hearing loss (SNHL). Hearing aids may also play a role in the management of conductive hearing losses, particularly those that result from pathologies that are not amenable to medical and surgical treatment. Hearing aids only partially overcome the deficits associated with a hearing loss. The range of levels between the weakest and the most intense sound heard is less for a person with sensorineural hearing loss than for a normal hearing person. A person with a sensorineural hearing loss needs a signal-to-noise ratio greater than normal. By contrast, a conductive impairment simply attenuates sounds as they pass through the middle ear. A hearing aid therefore more exactly compensates for the changes created by the conductive hearing loss. The amplifiers inside hearing aids can be classified as linear or nonlinear. Linear amplifiers amplify by the same amount no matter what the level of the signal is. The highest level of amplification produced by a hearing aid is known as the saturation sound pressure level (SSPL). Hearing aids are described according to where they are worn. In order of decreasing size these categories are: body, spectacle, behind-the-ear, in-the-ear, in-the-canal and completelyin-the-canal. Recent improvements in signal processing capabilities and increasing miniaturization of hearing aids have increased their acceptance among patients. Yet, there is no denying that hearing aids remain a "tough sell" to many who could potentially benefit from them, due to expense, complications of external auditory canal occlusion, cosmetic concerns, and lack of sufficient perceived benefit. These inherent limitations in hearing aids, combined with the social stigma of their use, have led to the development of implantable hearing aids. Implantable hearing aids offer patients with hearing loss (HL) several potential advantages over conventional hearing aids. These include increased gain and dynamic range, reduced feedback, reduced maintenance, improved appearance, and freedom from ear canal occlusion. Of course, these potential benefits must be weighed against the possible downsides of hearing aid use, including the risk of surgical implantation, difficulty of maintenance, and increased initial device cost. HEARING AID COMPONENTS Microphone converts sound to electricity. Directional microphones, are more sensitive to frontal sound. Dual-microphone hearing aids can be omnidirectional. Small signals produced by microphones are made more powerful by the hearing aid Amplifier. To avoid distortion, compression amplifiers are used in many hearing aids. These amplifiers decrease their gain as the level of the signal put into them increases. Amplifiers can represent sound in an analogue or a digital manner. Filters can be used to change the relative amplitude of the low-, mid- and high frequency components in a signal and also to break the signal into different frequency ranges. Receivers are miniature headphones that use electromagnetism to convert the amplified, modified electrical signals back into sound. A damper, inside the receiver absorbs energy at the frequencies corresponding to the peaks, and this improves sound quality and listening comfort by smoothening these peaks and troughs.
HEARING AID SYSTEMS Hearing aids can be classified by their technology into analogue, digitally programmable analogue and fully digital types. Digitally programmable hearing aids employ conventional analogue circuits for changing the sound, but use a digital control circuit to alter the characteristics of the analogue circuit. ELECTROACOUSTIC PERFORMANCE AND MEASUREMENT OF HEARING AIDS The performance of hearing aids is measured by couple (small cavity that connects the hearing aid sound outlet to a microphone) or a more complex ear simulator. The measurements most commonly performed using these sounds are curves of gain or output versus frequency at different input levels, and curves of output versus input at different frequencies. Many factors can lead to incorrect measurement of real-ear gain. These factors include incorrect positioning of the probe, squashing of the probe, blockage of the probe by cerumen, background noise and hearing aid saturation. EARMOULDS, EARSHELLS AND COUPLING SYSTEMS The earmould or earshell (called an otoplastic) is moulded to fit an individual's ear and retains the hearing aid on the head. It also provides the sound bore, which is the sound path from the receiver to the ear canal. In many cases, the otoplastic provides a second sound path, referred to as a vent, between the air outside and the ear canal. Where no vent exists, as in high-gain hearing aids, the mould or shell is said to be occluding. One unwanted consequence of a hearing aid can be an occlusion effect, in which the aid wearer's own voice is excessively amplified by bone-conducted sound. For most hearing aid fittings, vent selection is a careful juggle between choosing a vent that is big enough to avoid an unacceptable occlusion effect, but not so big that it causes feedback oscillations (hearing aid generated whistling). The shape of the sound bore that connects the receiver to the ear canal affects the highfrequency gain and output of hearing aids. Sound bores that widen as they progress inwards (horns) increase the high-frequency output. Conversely, those that narrow (constrictions) decrease the high-frequency output. Well-fitting earmould (medium viscosity silicone is good for most purposes). Tighter earmoulds or shells that allow less sound to leak from the ear canal can be achieved by a variety of techniques. These techniques include taking an impression with the patient's jaw open, patting down the impression material before it sets, using viscous impression material and building up the impression in the patient's ear. Soft materials provide a better seal to the ear. On the other hand, they deteriorate more rapidly and are more difficult to modify and repair. COMPRESSION SYSTEMS IN HEARING AIDS The benefits of compression can be summarized as follows: Compression can make low-level speech more intelligible, by increasing gain, and hence audibility. Compression can make high-level sounds more comfortable and less distorted (In mid level environments, compression offers little advantage). Compression's major disadvantages are: Excessive amplification of unwanted lower level background noises. ADVANCED SIGNAL PROCESSING SCHEMES FOR HEARING AIDS Multi-microphone directional arrays (including directional microphones) are the most effective way to improve intelligibility in noisy environments.
Feedback oscillation can be made less by: a) decreasing the gain only for those frequencies and input levels at which oscillation is likely. b) For people with severe or profound hearing loss at high frequencies, one way to make the high-frequency components of speech audible is to shift these components to lower frequencies. ASSESSING CANDIDACY FOR HEARING AIDS Initial motivation to obtain hearing aids. Disability (also called activity limitation) Handicap Hearing aids help more in quiet, so hearing aids are more likely to be valued and used if the patient needs help hearing in quiet places. People with tinnitus often find that hearing aid use diminishes their problems, so tinnitus positively affects candidacy. People with a severe to profound hearing loss are likely to receive more benefit from cochlear implants than from hearing aids. Vibrotactile or electrotactile aids are a worthwhile alternative for those too deaf to receive useful auditory stimulation from hearing aids, but who do not wish to receive a cochlear implant. PRESCRIBING HEARING AID PERFORMANCE Prescription formulae can be based on hearing thresholds, suprathreshold loudness judgements and the situations in which the hearing aids are to be worn. For linear hearing aids half-gain rule (in which gain equals half of hearing loss, in dB). SELECTING AND ADJUSTING HEARING AIDS The first decision when a clinician and patient select a hearing aid is whether CIC, lTC, ITE, BTE, spectacle or body hearing aids would be most suitable. Next, a signal-processing scheme appropriate to the needs of the patient must be selected. Compression limiting is a more appropriate form of limiting than peak clipping if it can provide a high enough maximum output. Feedback management or reduction schemes are most beneficial for patients with a severe or profound hearing loss, and for patients who have near-normal hearing or a mild hearing loss in the low frequencies combined with a severe loss in the high frequencies. PROBLEM SOLVING AND FINE TUNING OF HEARING AIDS Complaints about the patient's own-voice quality are particularly common. The most common cause is the physical blocking of the ear canal, so the best cure is to add a vent or increase the size of an existing vent. ASSESSING THE OUTCOMES OF HEARING REHABILITATION Outcome assessment can be based on an objective speech discrimination test or on a subjective self-report and/or the report of significant other people. While outcomes can be assessed any time after hearing aid fitting, the extent of benefit does not appear to stabilize until approximately six weeks after fitting. BINAURAL AND BILATERAL CONSIDERATIONS IN HEARING AID FITTING Helps a person to locate the source of sounds (Accurate horizontal localization is possible) and increases speech intelligibility in noisy situations, improved sound quality, suppression of tinnitus in both ears and greater convenience when one hearing aid breaks down.
SPECIAL HEARING AID ISSUES FOR CHILDREN Evidence exists that hearing aids should be provided prior to six months of age to maximize later language acquisition. BTE hearing aids are most likely to be provided, in conjunction with a soft earmould, until the child is atleast eight years old (and possibly much older). Hearing aid fittings can be evaluated by speech testing (for those over three years of age) , paired-comparison preference testing (for those over six years of age), and subjective reporting by the child, the parents or the teachers. Hazards include battery ingestion, excessive exposure to noise and failure to detect warning sounds if amplification is not functioning correctly. CONTRALATERAL ROUTING OF SIGNALS, BONE-CONDUCTION AND IMPLANTED HEARING AIDS Basic CROS aids are most suitable for people with unilateral loss. Such aids consists of a microphone on the side of the head with a deaf ear, combined with an amplifier, receiver and open earmould or shell, on the side with a normal-hearing ear. Bone-conduction hearing aids output a mechanical vibration instead of an airborne sound wave. They are most suited to people who, for medical reasons, cannot wear a hearing aid that occludes the ear in any way. An alternative form of bone-conduction hearing aid is the bone-anchored hearing aid, in which the vibrations are transmitted to the skull via an embedded titanium screw. LIMITATIONS (NON-IDEAL FEATURES) OF AUDITORY REHABILITATION USING TRADITIONAL HEARING AIDS a) Physical Factors Traditional hearing aids are limited in their ability to amplify sound without imparting distortion b) Insufficient Gain For patients with severe to profound hearing loss, sound amplification (or gain) is a primary concern. For a patient with air conduction thresholds of 80-dB HL to perceive quiet sounds at a normal threshold of 0-dB HL, a hearing aid must amplify sound intensity by 80 dB, generating a 10,000-fold increase in sound pressure wave amplitude and a 100,000,000fold increase in sound power intensity. This represents the limit of existing traditional hearing aids. c) Acoustic Feedback d) Spectral distortion e) Nonlinear/harmonic distortion f) Occlusion of external auditory canal g) Appearance/visibility h) Lack of directionality i) Poor Transduction Efficiency Loss of energy due to impedance mismatching and transduction losses is another inherent drawback of conventional aids. The mechanical impedance (change in pressure for a given displacement flow) of the air-filled external auditory canal differs from that of the fluid-filled cochlea. Without a middle ear mechanism, a majority of the acoustic energy striking the stapes footplate reflects back into the air. When the tympanic membrane and ossicular chain are functioning normally, they act as an impedance-matching transformer by virtue of the relative areas of the tympanic membrane and stapes footplate and by the lever action of the ossicular chain. The relatively large-displacement, low-pressure movements of air against
the tympanic membrane are transduced to the relatively small-displacement, high-pressure movements of the footplate. Except for bone-conducting aids, all traditional hearing aids use a speaker to output an (amplified) acoustic wave into the air of the external auditory canal. When this middle ear apparatus is malfunctioning, as occurs in otosclerosis, tympanic in membrane perforation, or in a canal-wall-down mastoidectomy, traditional hearing aids must overcome the impedance mismatch. The result is either reduced effective gain, increased distortion, or both. Even when the ossicular chain is functioning normally, the transduction of acoustic energy from air at the input of a traditional hearing aid to stapes footplate motion is imperfect. Whenever a signal flows from one physical realm (e.g. electrical current in a speaker) to another (e.g., acoustic waves in air), some energy is lost (e.g. to heat) and noise or distortion can add to the desired signal. There are several transduction steps for a traditional hearing aid. Most are unavoidable (although cochlear implants bypass these steps through direct cochlear nerve stimulation). However, directly coupling a hearing aid actuator movement of the ossicular chain can delete some of these transduction steps, boosting gain and reducing distortion. Nearly all implantable hearing aids make use of this approach. j) Human Factors k) Recruitment and Compression of Dynamic Range One of the primary sources of frustration of patients with SNHL is reduced speech intelligibility. This problem relates to abnormal frequency resolution and aberrant patterns of growth in loudness, each of which reduces speech intelligibility in noisy surroundings. SNHL also imposes severe constraints on the dynamic range of perceived sound. For normal listeners, the dynamic range from sensing soft sounds to the loudest tolerable noise is more than 100 dB. Within this wide dynamic range of hearing lies an approximately 35-dB dynamic range of conversational speech. In contrast, the dynamic range of patients with SNHL is often narrowed. This compaction of dynamic range leads to "recruitment," an abnormal growth in loudness as sound intensity increases. In effect, there is a much narrower range of sound intensity that a patient with recruitment can tolerate. Further adding to the difficulty, recruitment is observed in those frequencies that are most impaired, in the high frequencies, which also carry critical information for speech understanding. Recruitment thus remains one of the principle challenges of hearing aid rehabilitation. l) Disordered Perception of Pitch and Sound Localization All of these aformentioned factors play a role to various degrees in patients and combine to increase the noncompliance rate in hearing aid users. For most, these are the principle reasons why hearing aids are unacceptable. THE PROMISE OF IMPLANTABLE HEARING AIDS These limitations of traditional air conduction hearing aids have constituted the driving force behind the new generation of implantable hearing aids. Their advantages includes the possibility of improved signal/noise ratios, greater amplification/gain potential, invisibility, loss of distortion and feedback, getting the aid out of the canal with the associated occlusion effect, greater dynamic range, improved cosmetics, broader frequency response, less distortion, reduction or elimination of feedback, and better speech understanding, without reducing residual hearing, limiting patient activities, or predisposing patients to infection. For some who simply cannot wear a hearing aid because of underlying medical problems or extreme discomfort, they may be the only option. Bone-anchored hearing aids
Bone-anchored hearing aid (BAHA) is the registered trademark of a bone-conduction hearing aid system currently manufactured by Cochlear. It consists of a titanium screw that becomes osseointegrated in the skull with transcutaneous titanium abutment coupled with a boneconduction vibrator. All the alternative commercially available boneconduction aids require to be fitted to a headband, which is uncomfortable and unsightly. The BAHA can also be fitted to a headband and this is the method recommended in infants with congenital atresias until they are old enough for surgery at about three years. INDICATIONS FOR BONE-CONDUCTION AIDS/ BAHA 1. One absolute indication: bilateral canal atresia. Unilateral atresias are more frequent but do not usually require aiding. 2. Any patient using a conventional bone conduction (BC) hearing-aid 3. Any air conduction (AC) hearing aid user with chronic otorrhea 4. Any AC hearing aid user experiencing too much discomfort because of chronic otitis media/externa 5. Any AC hearing aid user experiencing uncontrollable feedback due to a radical mastoidectomy or large meatoplasty 6. Otosclerosis, tympanosclerosis, canal atresia with a contraindication to repair, such as in an only hearing ear; also, otosclerosis in combination with items 2, 3, and 4 above 7. Unilateral sensorineural hearing loss with >90 dBHL and speech discrimination score (SDS) <20 Contraindications 1. Pure-tone average BC thresholds (0.53.0 kHz) worse than 45 dB hearing loss, SDS >60% 2. Emotional instability, development delay, or drug abuse 3. Age younger than 5 years ELIGIBILITY FOR A BAHA There should be adequate bone-conduction, pure-tone thresholds. bone-conduction averaged over 0.5, 1, 2 and 3 kHz should be equal to or better than 45 dB HL for an ear-level aid and better than 58 dB HL for a body-level aid. Bone-conduction thresholds should be poorer at the high compared with the low frequencies. SURGICAL TECHNIQUE It is performed under local or general anaesthetic. The bone posterosuperior to the ear canal behind the pinna is usually of sufficient thickness over the age of three years to take an implant and allow osseo integration. In adults, but not children, most surgeons now use a one-stage procedure and fit the transcutaneous abutment at the same time rather than wait three months for osseo integration to occur before fitting it at a second operation. If a one-stage procedure is preferred, three months is also usually allowed before fitting the aid. Thin skin is necessary to lessen the risk of inflammation and crusting ; lack of hair makes hygiene easier. SURGICAL COMPLICATIONS Damage to the dura in children with craniofacial abnormalities, especially when multiple abutments are being inserted for a prosthetic pinna. Long-term problem is crusting and inflammation around the peg, which sometimes progresses to granulation tissue. Osseointegration resulting in the screw falling out is uncommon.
More frequently, the abutment works itself loose from the screw and has to be reattached. Children are more liable to problems. OUTCOMES BAHA COMPARISON WITH CONVENTIONAL BONE-CONDUCTION AIDS If a patient has previously used a conventional boneconduction aid, they almost invariably prefer the BAHA because it is cosmetically more acceptable, more comfortable to wear and gives better, less distorted amplification. BAHA COMPARISON WITH AN AIR-CONDUCTION AID The acoustical benefit of a BAHA over a well-prescribed and fitted air-conduction aid is marginal when assessed both by audiometry and by patient report. Most patients who previously wore an air-conduction aid, but were troubled by a discharge, report that with a BAHA the discharge improved. It is concluded that if a patient is benefiting acoustically from an air-conduction aid then the disability from the wearing of an ear-mould has to be sufficiently great for a BAHA to be substituted as this may give poorer acoustical benefit. BILATERAL BAHA FOR PATIENTS WITH A BILATERAL CONDUCTIVE IMPAIRMENT In those with a bilateral hearing impairment, binaural aiding is accepted as the ideal fitting for air-conduction aids because of better sound localization and central loudness summation. lesser audiometric benefit. UNILATERAL BAHA FOR PATIENTS WITH A UNILATERAL TOTAL IMPAIRMENT like a CROS aid there is a paucity of good evidence to support the use of a BAHA. MIDDLE EAR IMPLANTS Basic Design Features Transducer Design Conventional hearing aids function by receiving acoustic energy through a microphone, processing and amplifying the signal (in either an analog or digital fashion), and transmitting the signal through a speaker adjacent to the eardrum. This amplified sound then travels through the normal auditory pathway of the tympanic membrane and ossicles to the inner ear. Implantable middle ear hearing aids also use a microphone that senses sounds and a signal processor that amplifies and alters the sound signal, just as in a conventional aid. From here they differ from conventional aids. In one of several mechanisms unique to each device, the implantable middle ear hearing aids convert the electric signal into a mechanical energy that is then is coupled directly to the ossicular chain. The critical components of these systems are the transducer, which enables the device to output a signal that can be received by the ossicles, and the mechanism by which the transducer is coupled to the ossicles, which can either be a direct or indirect contact. There are two basic types of transducers that have been incorporated into the middle ear implantable hearing aids: piezoelectric and electromagnetic. Piezoelectric implantable hearing aids function by connecting the ossicles to an amplifier using a piezoelectric crystal vibrator. Piezoelectric materials are dielectric materials with coupled electrical and mechanical properties. Applying a voltage across an appropriately designed piezoelectric rod will cause it to bend or lengthen, with a predictable change in deflection based on the voltage applied. Within the implant, sounds picked up by a microphone are converted by the signal processor to an electrical signal and are sent to the piezoelectric rod. As this rod vibrates
in response to the converted auditory signal, it lies in direct contact with the ossicles. In this manner, sound waves are transferred directly to the ossicles, which then travel along the normal auditory pathway. Thus, a critical feature of implants that use a piezoelectric transducer is direct contact between the piezoelectric unit and the ossicles. Implantable middle ear hearing aids may also incorporate an electromagnetic transducer. These transducers generate a magnetic field using a coil carrying a current that encodes the microphone output. This magnetic field from the coil can then cause motion in a ferromagnetic substance that is nearby, causing it to vibrate. As applied to middle ear implants, sound received from a microphone is converted by the signal processor, amplified, and sent to the electromagnetic transducer. The electromagnetic field that is set up then vibrates a ferromagnetic unit coupled directly to the ossicles. In contrast to the piezoelectric unit that must be in direct contact with the ossicles, electromagnetic transducers only need to be near the ossicles, which have attached to them the ferromagnetic device that will transmit the auditory signal to the ossicles. These two types of amplification have different advantages for use in an implantable hearing aid. Electromagnetic transducers do not directly contact the ossicular chain but rely on electromagnetic transmission to a ferromagnetic unit that is attached to the ossicles. Furthermore, electromagnetic transducers can be packaged in a smaller housing, an important factor in the ear. In contrast, piezoelectric devices are larger and directly couple to the ossicular chain. Ossicular Coupling To obtain optimal efficiency in implantable hearing aids, the aids must adapt to the mechanics of the middle ear and ossicular chain. As the third ossicle in the chain, and the one in continuity with the inner ear, the motion of the stapes is critically important in sound transmission. The stapes moves in a piston-like fashion. [24] Therefore, the ideal motion of the stapes by a prosthesis would be in this piston-like fashion. Any implant that directly attached to the stapes would thus function best by mimicking this motion. Total vs Partially Implantable Hearing Aids The partially implantable devices consist of an external microphone and speech processor that are connected to a transmitter with an external coil that transmits electrical energy transcutaneously to the internal device in much the same way cochlear implants are now powered. The battery-powered system is contained within the external device, decreasing the size of the implanted components. The internal device consists of an internal receiving coil, which provides electrical energy to the mechanical driver connected to the ossicular chain. In contrast, the fully implantable systems house all of the aforementioned components within the implanted portion of the device, including the battery pack. although this does increase the size and complexity of the implanted components, it also reduces the visibility of the device, a feature that is desirable among hearing aid users. Piezoelectric Middle Ear Implantable Hearing Aids Totally Implantable Communication Assistance, Implex AG The advantage of this placement is that it allows the microphone to incorporate the sound processing effects of the auricle and ear canal, which are important for sound localization. The sensor is a hermetically sealed titanium cylinder measuring 4.5 mm in diameter with a stiff but flexible titanium membrane. Sound-induced movement of the skin in the medial canal is picked up by the microphone housed within the sensor. The implanted electronic circuitry allows sound amplification and processing.
The actuator uses a circular heteromorph system that consists of a piezoelectric disc adjacent to a titanium disc. The actuator includes a 0.5-mm titanium probe that is coupled to the incus for sound energy transfer to the ossicles. A significant benefit of the TICA is that, unlike many other implantable hearing devices, it is magnetic resonance imaging (MRI) compatible. Because the components are made of pure titanium without magnetic susceptibility, there is no torque produced by a large magnetic field. Thus, although the implant may cause some scattering and distortion of an MRI scan, there is little risk to the ossicular chain or inner ear. A significant potential drawback of the TICA design is the potential for feedback from the actuator backward through the ossicular chain and tympanic membrane to the subcutaneous microphone. Implantation of the TICA involves placement of three distinct but connected components: the piezoelectric actuator, the sensor, and a processing module that includes the battery and digital sound processor. The surgical approach involves a standard mastoidectomy. The actuator can be coupled to the incus body, reachable via the aditus ad antrum, or the long process of the incus, approached via a standard facial recess/posterior tympanotomy approach. The actuator is fixed to mastoid bone using a fixing plate and is then coupled to the incus using a positioning system. Alternatively, a titanium clip is used if attachment is to be made to the long process of the incus. For attachment to the incus body, a 0.5-mm trephine is made in the incus, and the transducer is inserted with ionomeric cement for added stability. The processor is placed in a drilled trough in the squamous portion of the temporal bone and fixed with sutures, similar to the placement of the electronics in a cochlear implant surgery. The sensor is slid subcutaneously in the posterior canal after drilling a small hole in the posterior canal wall. The leads from the transducer and sensor are then connected to the processor. References: Scott-Brown's Otorhinolaryngology, Head and Neck Surgery Vol III Cummings Otolaryngology, Head & Neck Surgery 4th ed
S-ar putea să vă placă și
- Hearing AidDocument4 paginiHearing AiddnllkzaÎncă nu există evaluări
- Hearing Aid PPT BaruDocument21 paginiHearing Aid PPT BaruJimmy AnwarÎncă nu există evaluări
- An Economical Hearing Aid LoopDocument10 paginiAn Economical Hearing Aid LoopTimotheus Michael VowlesÎncă nu există evaluări
- Otoacoustic Emissions From MedscapeDocument5 paginiOtoacoustic Emissions From MedscapeMin-Joo Esther ParkÎncă nu există evaluări
- Audiometric Testing of AdultsDocument6 paginiAudiometric Testing of AdultssofiameÎncă nu există evaluări
- ASSR Thresholds PDFDocument7 paginiASSR Thresholds PDFDaniela Garrido GonzálezÎncă nu există evaluări
- Head-Shaking Nystagmus (04.04.2005)Document11 paginiHead-Shaking Nystagmus (04.04.2005)r.boniver524Încă nu există evaluări
- Airway Obstruction Final2Document33 paginiAirway Obstruction Final2Mahindra KumarÎncă nu există evaluări
- Samsung Bluetooth Hearing Aid Test Results (FCC Application)Document53 paginiSamsung Bluetooth Hearing Aid Test Results (FCC Application)Gina SmithÎncă nu există evaluări
- Hearing Aid PDFDocument43 paginiHearing Aid PDFBILAL DIFÎncă nu există evaluări
- HEARING LOSS GUIDEDocument46 paginiHEARING LOSS GUIDEgibreilÎncă nu există evaluări
- Ototoxicity LatestDocument37 paginiOtotoxicity LatestSucdi CabdiÎncă nu există evaluări
- Slow Auditory Evoked Potentials (1 InterligneDocument8 paginiSlow Auditory Evoked Potentials (1 Interligner.boniver524Încă nu există evaluări
- Individualizing The Hearing Aids Needs AssessmentDocument36 paginiIndividualizing The Hearing Aids Needs Assessmentapi-349133705100% (1)
- BERA Test Explained: What is Brainstem Evoked Response AudiometryDocument34 paginiBERA Test Explained: What is Brainstem Evoked Response Audiometryassumpta0% (1)
- Medical Surgical NursingDocument38 paginiMedical Surgical NursingTripti PunÎncă nu există evaluări
- Auditory Neuropathy MorletDocument20 paginiAuditory Neuropathy MorletOxanaBitcaÎncă nu există evaluări
- Aural RehabilitationDocument28 paginiAural Rehabilitationapi-403585640100% (1)
- Cochlear ImplantDocument33 paginiCochlear ImplantNithiyah DevarajuÎncă nu există evaluări
- Anatomy and Physiology of Hearing SystemDocument63 paginiAnatomy and Physiology of Hearing SystemKharenza Vania Azarine Bachtiar100% (1)
- Osce EarexamDocument2 paginiOsce EarexamminhaapÎncă nu există evaluări
- Newborn Hearing Screening: Why It's ImportantDocument8 paginiNewborn Hearing Screening: Why It's ImportantAhiawortor Kplorla100% (1)
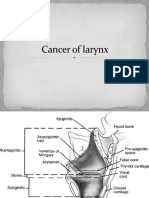
- Cancer of LarynxDocument46 paginiCancer of LarynxVIDYAÎncă nu există evaluări
- Acute Otitis Media: Symptoms, Causes, DiagnosisDocument11 paginiAcute Otitis Media: Symptoms, Causes, DiagnosisAnkita BramheÎncă nu există evaluări
- Hearing With Bone-Anchored Hearing Aid BAHA PDFDocument8 paginiHearing With Bone-Anchored Hearing Aid BAHA PDFpro4ksaÎncă nu există evaluări
- Binaural Loudness Balance Test ExplainedDocument4 paginiBinaural Loudness Balance Test ExplainedAnish RajÎncă nu există evaluări
- Cholesteatoma FinalDocument56 paginiCholesteatoma FinalDr.Bharathi M.BÎncă nu există evaluări
- MyelographyDocument22 paginiMyelographyKarylleÎncă nu există evaluări
- Non Organic Hearing LossDocument59 paginiNon Organic Hearing LossAakritiÎncă nu există evaluări
- Hearing AidDocument1 paginăHearing AidGyan ChaharÎncă nu există evaluări
- Cochlear ImplantsDocument53 paginiCochlear ImplantsSovitJungBaralÎncă nu există evaluări
- Functional Endoscopic Sinus Surgery - Overview, Preparation, TechniqueDocument10 paginiFunctional Endoscopic Sinus Surgery - Overview, Preparation, TechniqueHendra SusantoÎncă nu există evaluări
- Recurrent Ear Infection Diagnosis and Treatment ScenarioDocument23 paginiRecurrent Ear Infection Diagnosis and Treatment ScenarioAakashÎncă nu există evaluări
- Part 2 - The Physiology of Hearing - Handout PDFDocument8 paginiPart 2 - The Physiology of Hearing - Handout PDFMike PosktovaÎncă nu există evaluări
- Cardiac MonitoringDocument6 paginiCardiac MonitoringAIMÎncă nu există evaluări
- Impedance Audiometry - Overview, Indications, ContraindicationsDocument8 paginiImpedance Audiometry - Overview, Indications, ContraindicationsSorin AilincaiÎncă nu există evaluări
- Therapeutic Management of Laryngectomy - PDF / KUNNAMPALLIL GEJO JOHNDocument31 paginiTherapeutic Management of Laryngectomy - PDF / KUNNAMPALLIL GEJO JOHNKUNNAMPALLIL GEJO JOHNÎncă nu există evaluări
- CT ScanningDocument24 paginiCT ScanningMurary S PottyÎncă nu există evaluări
- MENINGITIS Lesson PlanDocument12 paginiMENINGITIS Lesson PlannidhiÎncă nu există evaluări
- CT Scans: and Their ApplicationDocument44 paginiCT Scans: and Their ApplicationAmi JeebaÎncă nu există evaluări
- Resident Physics Lectures: Digital Subtraction Angiography (DSA)Document41 paginiResident Physics Lectures: Digital Subtraction Angiography (DSA)Lajja Parikh PatelÎncă nu există evaluări
- Laryngeal Cancer: Anatomy, Risk Factors, Symptoms and Treatment OptionsDocument36 paginiLaryngeal Cancer: Anatomy, Risk Factors, Symptoms and Treatment OptionsTito PÎncă nu există evaluări
- Digital Hearing Aid DevelopmentDocument10 paginiDigital Hearing Aid Developmentaka_1010Încă nu există evaluări
- The Effects of Earphone Use On The Incidence of Noise-Induced Hearing Loss An Empirical Study of Senior High School Students in Banda AcehDocument8 paginiThe Effects of Earphone Use On The Incidence of Noise-Induced Hearing Loss An Empirical Study of Senior High School Students in Banda AcehInternational Journal of Innovative Science and Research TechnologyÎncă nu există evaluări
- Lung Sounds Guide: Vesicular, Bronchial, Crackles & MoreDocument24 paginiLung Sounds Guide: Vesicular, Bronchial, Crackles & MoreAswinÎncă nu există evaluări
- Auditory Brain Stem ImplantDocument2 paginiAuditory Brain Stem ImplantSuprit SnÎncă nu există evaluări
- Ent Hearing Tests, Vestibular TestsDocument13 paginiEnt Hearing Tests, Vestibular TestsSuleman MuhammadÎncă nu există evaluări
- MastoiditisDocument5 paginiMastoiditisJessica Fredelina0% (1)
- Open Access Guide To Audiology and Hearing Aids For OtolaryngologistsDocument5 paginiOpen Access Guide To Audiology and Hearing Aids For OtolaryngologistsSami MoqbelÎncă nu există evaluări
- Auditory Brain Stem ImplantsDocument7 paginiAuditory Brain Stem Implantsabirajalakshmix9395Încă nu există evaluări
- The Compression HandbookDocument48 paginiThe Compression HandbookStephan KhodyrevÎncă nu există evaluări
- Endotracheal TubeDocument19 paginiEndotracheal TubeSarvess Muniandy100% (1)
- Design of Portable Hearing Aid Based On FPGADocument4 paginiDesign of Portable Hearing Aid Based On FPGAsenthilvlÎncă nu există evaluări
- Hearing Aid System Using MatlabDocument6 paginiHearing Aid System Using MatlabAbhishek ChedeÎncă nu există evaluări
- DYSPHAGIA Lecture NotesDocument84 paginiDYSPHAGIA Lecture Notesmcmak357Încă nu există evaluări
- Cochlear Rotation and Its RelevanceDocument7 paginiCochlear Rotation and Its RelevanceDrTarek Mahmoud Abo KammerÎncă nu există evaluări
- Sudden Sensorineural Hearing Loss: Christopher D. Muller, M.D. Jeffrey Vrabec, M.DDocument64 paginiSudden Sensorineural Hearing Loss: Christopher D. Muller, M.D. Jeffrey Vrabec, M.DDrKunal KaradeÎncă nu există evaluări
- Embryology of The Ear and Its AnatomyDocument20 paginiEmbryology of The Ear and Its AnatomyElisa NÎncă nu există evaluări
- Your Guide To Hearing AidsDocument20 paginiYour Guide To Hearing AidsMarhama FitrianiÎncă nu există evaluări
- Voice and Speech DisordersDocument2 paginiVoice and Speech DisordersVishal Gaurav100% (1)
- Stridor in ChildrenDocument30 paginiStridor in ChildrenVishal GauravÎncă nu există evaluări
- Evaluation of A Case of StridorDocument17 paginiEvaluation of A Case of StridorVishal GauravÎncă nu există evaluări
- VII Nerve Palsy - Sensory, Motor & Secretomotor FunctionsDocument8 paginiVII Nerve Palsy - Sensory, Motor & Secretomotor FunctionsVishal GauravÎncă nu există evaluări
- References 1Document2 paginiReferences 1Vishal GauravÎncă nu există evaluări
- Scott Brown Vol 3Document6 paginiScott Brown Vol 3Vishal GauravÎncă nu există evaluări
- Stridor in Children: By: Maj Vishal Gaurav Moderator: DR A SethiDocument33 paginiStridor in Children: By: Maj Vishal Gaurav Moderator: DR A SethiVishal GauravÎncă nu există evaluări
- SB Ci RolDocument5 paginiSB Ci RolVishal GauravÎncă nu există evaluări
- Deep Neck Infection 051005Document43 paginiDeep Neck Infection 051005Vishal GauravÎncă nu există evaluări
- 01-06-05 Entgr Head and Neck AidsDocument38 pagini01-06-05 Entgr Head and Neck AidsVishal GauravÎncă nu există evaluări
- Opinion About The Drug WarDocument1 paginăOpinion About The Drug WarAnonymous JusFNTÎncă nu există evaluări
- Creative Writing 12 July Monthly TestDocument4 paginiCreative Writing 12 July Monthly TestMichelle Labajo Maunes100% (1)
- 02 Samss 012Document10 pagini02 Samss 012bmkaleÎncă nu există evaluări
- Tecnodiesel AC350 Cummins 6LTAA9.5-G1 LS TAL 440VDocument10 paginiTecnodiesel AC350 Cummins 6LTAA9.5-G1 LS TAL 440VJose DarioÎncă nu există evaluări
- XA2ED33 DATASHEET SA en-SADocument2 paginiXA2ED33 DATASHEET SA en-SASalmanÎncă nu există evaluări
- K85001-0646 - Intelligent Smoke DetectorDocument4 paginiK85001-0646 - Intelligent Smoke Detectorafie pio pioÎncă nu există evaluări
- Iran Syria AllianceDocument45 paginiIran Syria AllianceOlga LazinÎncă nu există evaluări
- Sexism EssayDocument5 paginiSexism Essayd3gpmvqw100% (2)
- Genetics Case Study - MicrocephalyDocument4 paginiGenetics Case Study - MicrocephalyHeru WÎncă nu există evaluări
- History Taking - Progress NotesDocument21 paginiHistory Taking - Progress Notestwgp6pg5gh100% (1)
- About Nestle IndiaDocument5 paginiAbout Nestle IndiaSAMBHAVI SINGH 1827653Încă nu există evaluări
- Split Ac Repair Trainer: InstructionDocument10 paginiSplit Ac Repair Trainer: InstructionSingh ShubhamÎncă nu există evaluări
- Gsef 2021 Research Plan Project Summary InstructionsDocument1 paginăGsef 2021 Research Plan Project Summary Instructionsapi-550508557Încă nu există evaluări
- BS BuzzDocument6 paginiBS BuzzBS Central, Inc. "The Buzz"Încă nu există evaluări
- RGPH Specification Sheets PDFDocument0 paginiRGPH Specification Sheets PDFITLHAPNÎncă nu există evaluări
- Thermal Death Kinetics of MicroorganismsDocument6 paginiThermal Death Kinetics of MicroorganismsShubham MannaÎncă nu există evaluări
- Extensor Tendon Injury ProtocolDocument11 paginiExtensor Tendon Injury ProtocoltasneempichoriÎncă nu există evaluări
- BMA Catalog 2012Document30 paginiBMA Catalog 2012Born SatanistÎncă nu există evaluări
- GEOTHERMAL POWER (Aashutosh Tiwari)Document17 paginiGEOTHERMAL POWER (Aashutosh Tiwari)Aashutosh TiwariÎncă nu există evaluări
- PimafucortDocument6 paginiPimafucortenglish-exactlyÎncă nu există evaluări
- Practical 1: Determination of Reducing Sugar Using The Dinitrosalicylic (DNS) Colourimetric MethodDocument8 paginiPractical 1: Determination of Reducing Sugar Using The Dinitrosalicylic (DNS) Colourimetric MethodNurSyazaHaniÎncă nu există evaluări
- West Bengal police pay slipDocument1 paginăWest Bengal police pay slipBiswajit DasÎncă nu există evaluări
- Risk - Threat - Vulnerability Primary Domain ImpactedDocument4 paginiRisk - Threat - Vulnerability Primary Domain ImpactedDuong Chi Hung (K15 HCM)Încă nu există evaluări
- A Family of SlutsDocument9 paginiA Family of Slutsmayzin167100% (2)
- Allweiler 3 spindle screw pump installation docsDocument4 paginiAllweiler 3 spindle screw pump installation docsPriyanka KumariÎncă nu există evaluări
- Instrument Transformer CVT TransformerDocument6 paginiInstrument Transformer CVT Transformerkajrare_1947Încă nu există evaluări
- MoistScan 8pp Brochure LoResDocument8 paginiMoistScan 8pp Brochure LoResLuis PurisÎncă nu există evaluări
- PDQ 39Document8 paginiPDQ 39Wenderson MoraisÎncă nu există evaluări
- VK Newsletter April 2016 - March 2017Document27 paginiVK Newsletter April 2016 - March 2017HMIS VKBORLÎncă nu există evaluări
- Eisma 2013. From Formalin To Thiel EmbalmingDocument8 paginiEisma 2013. From Formalin To Thiel EmbalmingArmin AriasÎncă nu există evaluări