Documente Academic
Documente Profesional
Documente Cultură
ABG Poster A3
Încărcat de
Araceli Ecot CalunodDescriere originală:
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
ABG Poster A3
Încărcat de
Araceli Ecot CalunodDrepturi de autor:
Formate disponibile
ABG...EASY AS...
1,2,3
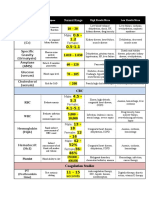
NORMAL VALUES & DEFINITIONS
NAME pH DEFINITION Refers to hydrogen ion (H+) levels, hence the H in pH. H+ levels are important because a lack of (deficit) or too much (excess) will tell you if the patient is acidotic or alkolotic. One confusing point about pH is that it is an INVERSE ratio, which means that the more H+ present, the lower the pH and vice versa. Can give away a H+ or can separate (dissociate) hydrogen from its ion, so the hydrogen is not positive and therefore no longer an acid. Acids are end products of metabolism and must be buffered or excreted to achieve a normal pH Unlike Acids, bases can accept a H+ and bond with hydrogen. They are all negative and like to buffer body acids. VALUE 7.35 - 7.45
3 STEPS TO ABG INTERPRETATION
1. What is the pH? Is it alkolotic (57.45) or acidotic (67.35)? 2. Whats happening with the respiratory system (CO2) and the metabolic systems (HCO3-)? If the problem is in the lungs (respiratory) the CO2 will be heading in the opposite direction of the pH. For example: respiratory acidosis: The pH will be low - 6pH 7.22 and the CO2 will be high - 5CO2 55mmhg If the problem is metabolic the HCO3 will head in the same direction as the pH For example: metabolic alkalosis: The pH will be high - 57.55 and the HCO3- will also be high HCO3- 535mmol/L. Note: an easy way to remember for a Metabolic problem, think M as in the pH will head in the saMe direction as the HCO3-. For respiratory the pH will head in the Opposite direction as the CO2. 3. Is there any (if any) compensation occurring? No compensation: pH remains abnormal, and the other value (where the problem isnt occurring, i.e. CO2 or HCO3-) will remain normal or has made no attempt to help normalise the pH. For example: in uncompensated metabolic acidosis: pH 67.23, HCO3- 6 15mmol/L, and the CO2 will be normal at 40mmHg. Partial compensation pH is still abnormal, and the other value is abnormal in an attempt to help normalise the pH. For example: in partially compensated respiratory alkolosis: pH 57.62, CO2 627 and the HCO3- will be abnormal at 617mmol/L Full compensation The pH is normal, as the other value is abnormal and has been successful in normalising the pH. For example: Fully compensated metabolic acidosis pH 7.38, HCO3- 615mmol/L and the CO2 630mmHg 6
Acid
20 parts base / 1 part acid
Base
WHAT CAUSES THESE CHANGES?
METABOLIC ACIDOSIS Can be caused by either an increase in circulating acids and or a loss of base (HCO3-). These include: Renal failure (unable to excrete acids or H+) Lactic acidosis (increase in circulating acids) Keto - acidosis (increase in circulating acids) Diarrhoea (HCO3- loss) METABOLIC ALKOLOSIS Can be caused by an increase in HCO3- or loss of metabolic acids. These include: Prolonged vomiting (acid loss) GI suctioning (acid loss) Hypokalaemia (H+ (an acid) excreted to maintain electrolyte balance) RESPIRATORY ACIDOSIS Caused by increased CO2 levels which is then converted to an acid (H+) as the body tries compensate by excreting acids via the kidneys. These include: Hypoventilation: - sedatives/sedation/opiates Depression of respiratory centre in brain stem via trauma Pneumonia Pulmonary oedema Asthma RESPIRATORY ALKALOSIS Caused by a hyperventilation, the body getting rid of too much CO2, for example: Anxiety Hypoxaemia (caused by heart failure)
Base excess / Base deficit
Represents an increase or decrease in the -2 to +2mmol/L amount of base compared with the amount of acids present Concentration of hydrogen carbonate in blood. Used to determine along with pH and CO2 source of acid base imbalance. 22-26mmol/L
HCO3-
pCO2
Carbon dioxide partial pressure (tension). 35-45 mmhg Reflects alveolar ventilation as it diffuses across the alveolar capillary membrane and blown off.
paO2
Arterial oxygen tension. In other words 75-100mmhg how well the lungs are able to pick up oxygen, i.e. supply, but not demand (this is shown in a mixed venous gas, discussed later). Lactate When cells no longer have enough O2 for 0.5 - 2.0mmol/L (Lactic Acid) normal aerobic metabolism (cell hypoxia) Anaerobic metabolism takes over resulting in lactate production, leading to lactic acidosis Hb Amount of haemoglobin in blood possibly 135 - 180g/L 7 (Haemoglobin) capable of carrying oxygen.
TREATMENT GOALS/GUIDELINES
As with both acidosis and alkolosis, there needs to be a diagnosis of why the patients acid base status is such. Treatment is then aimed at stabilising the initial/presenting problem as well the acid-base status. However, general guidelines include correcting the fluid balance and electrolyte status. Continuous regular ABG monitoring and recording for trends. Possible dialysis to remove excess lactate, manipulation of ventilation settings to adjust CO2 levels, but always maintaining tissue perfusion. Depending on severity of HCO3- levels and pH - possible sodium bicarbonate infusion (this is controversial however). Of course any of the adjustments made should only be done with an order from a medical officer, and must go through the intensive care team before any changes to treatments are applied. 4
MIXED VENOUS BLOOD GAS VALUES
NAME pH HCO3pCO2 paO2 sO2 VALUE 7.33 - 7.44 24-28mmol/L 41-57 mmhg 35-40mmhg 70 - 75%
Superior Vena Cava
OXYHAEMOGLOBIN DISSOCATION CURVE (ODC)
What is it and why is it important? The ODC looks at the relationship between oxygen tension (pressure) and oxygen saturation. It helps us better understand how our blood interacts with oxygen, i.e. how and why it picks up and lets oxygen go. The S shape tells us that after an amount of oxygen has accumulated in the blood, there isnt room for any more, no matter how much oxygen you throw at the haemoglobin molecule, it wont change Affinity basically means how much we (or blood) are attracted to someone (oxygen). The ODC shows us what changes the affinity of blood for oxygen. RIGHT SHIFT (ACIDOSIS) Shift of the curve to right decreases affinity - meaning that the Hb isnt very attracted to oxygen, and when it does pick up oxygen, it lets it go very quickly. Increased temperature and CO2 help this right shift. LEFT SHIFT (ALKALOSIS) Shift of the curve to the left increases affinity - meaning that the Hb is very attracted (oh la la) to oxygen and when oxygen is picked up, the Hb has a hard time letting it go at the cellular level. Decreased temperature and CO2 help the curve move to the left. 2
Pulmonary Artery
Mixed venous gases measures oxygen left in the blood as it returns to the heart (right side) after it has been pumped around the body supplying cells with oxygen. The body normally extracts 25% of available oxygen and leaves 75% in reserve in times of stress or illness.4 The heart above shows where our subclavian central lines sits - in the superior vena cava, it is here we can take venous blood gases. Samples from the pulmonary artery are however, more accurate and can only be performed if the patient has a PA catheter.
ALKALOSIS
ACIDOSIS
OTHER VALUES OFTEN OVERLOOKED
Anion gap - This value is used in metablic acidosis to find the cause. It reflects unmeasured anions (negatively charged ions) such as proteins, sulfates, phosphates etc. The equation to find the anion gap is (Na + K+) - (cl + [HCO3-]) a high value can be caused by keto or lactic acidosis, or renal failure. Low values may indicate hyponatremia or decreased plasma protiens. 10-20mmol/L OXYGEN STATUS p50a - oxygen tension at 50% saturation on ODC. This is used to reflect affinity of Hb for oxygen. 25-29mmhg FMetHb - This is the fraction of methaemoglobin. Think of methaemoglobin like haemoglobin, but we carry less than 1% of it in our blood. As it is unable to combine with oxygen and it also decreases the oxygen carrying capacity of blood. Exposure to certain drugs and chemicals can dangerously elevate levels. 0.2-0.6% FCOHb - Fraction of carboxyhaemoglobin. Much similar to FMetHb in its actions. Affinity of Hb for carbon monoxide is 200 times greater than that of oxygen and impairs oxygen transport and release (ODC shift to left, alkolosis). This level can be high in heavy smokers. 0.0-8.0% Fshunte - Relative physiological shunt. Basically the amount of venous (de-oxygenated) blood that did not receive oxygen whilst travelling through the lungs. This can be caused by atelectasis, a pulmonary embolism (PE), mucous plugs and pulmonary oedema, all of which reduces oxygen transport into the blood. 1.0-10% FO2Hb - fraction of oxyhaemoglobin. This measures just how much blood (Hb) is carrying oxygen compared to the total amount of Hb capable of carrying. Similar to your SO2, however FCOHb and FMetHb are not included as they are not capable of carrying oxygen. 94-98% Hct - Hematocrit. This shows us how much red blood cells there are in a sample of blood - i.e. how watered down (or not) blood is. 36-44%7
REFERENCE LIST 1. Coleman, n. and Houston, L. 1998 Demystifying acid-base regulation Australian nursing Journal 5, 8, 23-26 2. Dickson, S. 1995 Understanding the Oxyhemoglobin Dissociation Curve. Critical care Nurse 15, 10, 54-58. 3. Minor, J. and George, E. 2008 Using mixed venous oxygen saturation to improve patient assessments. Nursing2008 56, 1, 1-3. 4. McCance, K. and Heuther, S. 1998 Pathophysiology, 3rd edn, Mosby, St. Louis, Missouri. 5. Pruitt, W. 2004 Interpreting Arterial blood gases: Easy as ABC. Nursing2004 34, 2, 50-53. 6. Tastota, F. 1994 Assessing A.B.G.s: Maintaining the delicate balance. Nursing94 24, 5, 34-44. 7. The Blood Gas Handbook, 2005. Radiometer Medical ApS RadiometerCopenhagen, Bronshoj. 8. Wikipedia contributors, 2008 Pulmonary artery. n.p. Available URL: www.wikipedia.org/w/index.php?title=Pulmonary artery&oldid=183841779 <Accessed 2008 February 2> 9. Wikipedia contributors, 2008 Oxygen-haemoglobin dissociation curve. n.p. Available URL: wikipedia.org/w/index.php?title=Oxygen-haemoglobin dissociation curve&oldid=187503438 <Accessed 2008 February 2>
Hb
O2
O2
Hb
BICARBONATE/CARBONIC (HCO3-/H2CO3) BUFFERING SYSTEM
H2O + CO2 n H2CO3 nH+ + HCO3 The H2O and CO2 is regulated via the lungs and HCO3- and H+ via the kidneys. An increase in one value can shift the equation and helps maintain equilibrium. A problem in either the lungs or kidneys or both can throw this equation out of whack, resulting in an acid base imbalance. Other buffers include protein and phosphate buffers.
This is the most active buffering system. Needs good renal function (HCO3- regulation) Converts H+ (hydrogen) to H2CO3 (carbonic acid) which is then able to be blown off via the lungs as CO2.
RESPIRATORY REGULATION OF ACID BASE BALANCE
Eliminates volatile acids (CO2) Works within minutes Dependent on HCO3- stores and adequate gas exchange CO2 diffuses passively into the cerebrospinal fluid and the medulla controls rate and depth of respiration Eliminates fixed acids (harder to remove than volatile) H+ Regulates HCO3- depending on need Controls phosphate and ammonia buffer systems Bicarbonate/carbonic acid system can only work if bicarbonate stores are replaced by the kidneys.1 Works slowly, from hours to days
RENAL REGULATION OF ACID BASE BALANCE
Author: Amy ODonnell Date: 9th February, 2008
S-ar putea să vă placă și
- Nursing: Lab Values: a QuickStudy Laminated 6-Page Reference GuideDe la EverandNursing: Lab Values: a QuickStudy Laminated 6-Page Reference GuideÎncă nu există evaluări
- ABGs Respiratory/MetabolicDocument3 paginiABGs Respiratory/MetabolicJoe B100% (1)
- Arterial Blood Gas Analysis - making it easyDe la EverandArterial Blood Gas Analysis - making it easyEvaluare: 4.5 din 5 stele4.5/5 (4)
- Blood Gas InterpretationDocument36 paginiBlood Gas InterpretationMary Charmaine DivinagraciaÎncă nu există evaluări
- Fluid and Electrolytes for Nursing StudentsDe la EverandFluid and Electrolytes for Nursing StudentsEvaluare: 5 din 5 stele5/5 (12)
- ABG Interpretation - ATSDocument5 paginiABG Interpretation - ATSHAMMYER ALROKHAMIÎncă nu există evaluări
- Respiratory Acidosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDe la EverandRespiratory Acidosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsÎncă nu există evaluări
- Icu Nurse SheetDocument1 paginăIcu Nurse SheetJan MarcusÎncă nu există evaluări
- Nursing Care of PlanDocument16 paginiNursing Care of PlanDbyÎncă nu există evaluări
- The 12-Lead Electrocardiogram for Nurses and Allied ProfessionalsDe la EverandThe 12-Lead Electrocardiogram for Nurses and Allied ProfessionalsÎncă nu există evaluări
- ABG Practice Problems For N304Document4 paginiABG Practice Problems For N304dlneisha61100% (2)
- Dimensional Analysis For Nursing StudentsDe la EverandDimensional Analysis For Nursing StudentsÎncă nu există evaluări
- EKG Basics1Document16 paginiEKG Basics1Jamie Lemons100% (1)
- 14 Fun Facts About Your Heart: Educational VersionDe la Everand14 Fun Facts About Your Heart: Educational VersionÎncă nu există evaluări
- Cardiac Med ChartsDocument6 paginiCardiac Med ChartsNursingSchoolNotes100% (15)
- Schaum's Outline of Critical Care Nursing: 250 Review QuestionsDe la EverandSchaum's Outline of Critical Care Nursing: 250 Review QuestionsEvaluare: 5 din 5 stele5/5 (1)
- Shock Comparison ChartDocument2 paginiShock Comparison Chartlinnaete88% (8)
- CRITICAL CARE NURSE: Passbooks Study GuideDe la EverandCRITICAL CARE NURSE: Passbooks Study GuideÎncă nu există evaluări
- Respiratory PathophysDocument1 paginăRespiratory PathophysTori IkeharaÎncă nu există evaluări
- Lab ValuesDocument3 paginiLab Valuessurviving nursing school100% (1)
- Understanding ElectrolytesDocument2 paginiUnderstanding Electrolytessurviving nursing schoolÎncă nu există evaluări
- Heart FailureDocument1 paginăHeart FailureTrisha Vergara100% (1)
- Acid Base Who Is Your DaddyDocument66 paginiAcid Base Who Is Your Daddyjenn1722100% (14)
- Critical Care NursingDocument1 paginăCritical Care NursingMelissa David0% (1)
- ICU Cheat SheetDocument2 paginiICU Cheat SheetPrescilla Randazzo100% (1)
- ABG InterpretationDocument31 paginiABG Interpretationɹǝʍdןnos100% (12)
- My Cheat SheetDocument3 paginiMy Cheat SheetTenzin KyizomÎncă nu există evaluări
- Cardiac Study GuideDocument11 paginiCardiac Study Guidejenwiley318096% (73)
- Shock Study Guide NursingDocument4 paginiShock Study Guide NursingKory Christina100% (2)
- EKG Quick Reference ChartDocument4 paginiEKG Quick Reference ChartMildaÎncă nu există evaluări
- Acid-Base WorksheetDocument2 paginiAcid-Base WorksheetMayer Rosenberg100% (18)
- Arterial Blood Gases Made Easy PDFDocument66 paginiArterial Blood Gases Made Easy PDFTamjid Khan100% (5)
- Nursing Patho CardsDocument195 paginiNursing Patho Cardsgiogmail100% (1)
- Simple Method of Acid Base Balance Interpretation: UsefulnessDocument2 paginiSimple Method of Acid Base Balance Interpretation: UsefulnessPeej ReyesÎncă nu există evaluări
- ABG Made EasyDocument10 paginiABG Made EasyMayer Rosenberg100% (38)
- DYSRHYTHMIAS (A.k.a. Arrhythmias) Disorders in TheDocument3 paginiDYSRHYTHMIAS (A.k.a. Arrhythmias) Disorders in TheDarell M. Book100% (1)
- Arterial Lines in PACU: Presented by Autum Jacobs RN, BSNDocument34 paginiArterial Lines in PACU: Presented by Autum Jacobs RN, BSNinuko1212Încă nu există evaluări
- Med Surg Respiration-Cardiac NotesDocument11 paginiMed Surg Respiration-Cardiac Notesorganictallgirl50% (2)
- Acuterespiratorydistress Syndrome: Ventilator Management and Rescue TherapiesDocument16 paginiAcuterespiratorydistress Syndrome: Ventilator Management and Rescue TherapiessamuelÎncă nu există evaluări
- Alkalosis Acidosis ChartDocument1 paginăAlkalosis Acidosis ChartrobingailÎncă nu există evaluări
- Management of Mechanical VentilationDocument16 paginiManagement of Mechanical Ventilationyuliana muinÎncă nu există evaluări
- Arterial LinesDocument13 paginiArterial LinesberhanubedassaÎncă nu există evaluări
- Med Surg Cheat Sheet 1Document1 paginăMed Surg Cheat Sheet 1Figmentum FigmentumÎncă nu există evaluări
- Abg InterpretationDocument14 paginiAbg Interpretationmara5140100% (7)
- Sample Acls For DummiesDocument3 paginiSample Acls For DummiesTodd Cole100% (1)
- Approach To The Patient With Respiratory DiseaseDocument6 paginiApproach To The Patient With Respiratory DiseaseRem AlfelorÎncă nu există evaluări
- Critical CareDocument40 paginiCritical Carenkuligowski100% (6)
- Abg Made EasyDocument24 paginiAbg Made EasynbvillarazoÎncă nu există evaluări
- Ams 11Document702 paginiAms 11CrazyÎncă nu există evaluări
- Ecgs Made Easy 5th Edition Aehlert Test BankDocument14 paginiEcgs Made Easy 5th Edition Aehlert Test BankQuinn50% (2)
- Practice StripsDocument9 paginiPractice StripsErica Yamamoto50% (4)
- Arterial Blood GasesDocument44 paginiArterial Blood GasesRidhwan Mgt100% (1)
- Sepsis, Septic Shock, MODSDocument19 paginiSepsis, Septic Shock, MODSPaul Zantua80% (5)
- MedicalSurgical Nursing ReviewDocument86 paginiMedicalSurgical Nursing ReviewPopa D. SilviuÎncă nu există evaluări
- ACAQ Crit Care Nursing CurriculumDocument91 paginiACAQ Crit Care Nursing CurriculumAnne Julia Agustin100% (1)
- Vent Modes ChartDocument1 paginăVent Modes Chartladyhavocinc100% (1)
- Cardiac Meds ChartDocument1 paginăCardiac Meds ChartCharlotte Louise75% (4)
- ABG AnalysisDocument22 paginiABG Analysisrajan40dmcÎncă nu există evaluări
- Pathophysiology of Respiratory DiseasesDocument8 paginiPathophysiology of Respiratory DiseasesTONY GO AWAYÎncă nu există evaluări
- Catedral de SevillaDocument28 paginiCatedral de SevillaAnonymous LkgNmKeÎncă nu există evaluări
- Cambridge IGCSE™: Information and Communication Technology 0417/13 May/June 2022Document15 paginiCambridge IGCSE™: Information and Communication Technology 0417/13 May/June 2022ilovefettuccineÎncă nu există evaluări
- Sociology As A Form of Consciousness - 20231206 - 013840 - 0000Document4 paginiSociology As A Form of Consciousness - 20231206 - 013840 - 0000Gargi sharmaÎncă nu există evaluări
- SOL LogicDocument21 paginiSOL LogicJa RiveraÎncă nu există evaluări
- Development Developmental Biology EmbryologyDocument6 paginiDevelopment Developmental Biology EmbryologyBiju ThomasÎncă nu există evaluări
- Micro EvolutionDocument9 paginiMicro EvolutionBryan TanÎncă nu există evaluări
- Listen and Arrange The Sentences Based On What You Have Heard!Document3 paginiListen and Arrange The Sentences Based On What You Have Heard!Dewi Hauri Naura HaufanhazzaÎncă nu există evaluări
- Thesis PaperDocument53 paginiThesis PaperAnonymous AOOrehGZAS100% (1)
- Lesson 6 - Vibration ControlDocument62 paginiLesson 6 - Vibration ControlIzzat IkramÎncă nu există evaluări
- Lecture2 GranulopoiesisDocument9 paginiLecture2 GranulopoiesisAfifa Prima GittaÎncă nu există evaluări
- Leadership Styles-Mckinsey EdDocument14 paginiLeadership Styles-Mckinsey EdcrimsengreenÎncă nu există evaluări
- Unsuccessful MT-SM DeliveryDocument2 paginiUnsuccessful MT-SM DeliveryPitam MaitiÎncă nu există evaluări
- Workbook Group TheoryDocument62 paginiWorkbook Group TheoryLi NguyenÎncă nu există evaluări
- Hidrl1 PDFDocument7 paginiHidrl1 PDFRajesh Kumar100% (1)
- DLP - Light Science 7Document6 paginiDLP - Light Science 7Samara M. SalacayanÎncă nu există evaluări
- Amount of Casien in Diff Samples of Milk (U)Document15 paginiAmount of Casien in Diff Samples of Milk (U)VijayÎncă nu există evaluări
- Fire Protection in BuildingsDocument2 paginiFire Protection in BuildingsJames Carl AriesÎncă nu există evaluări
- Sem4 Complete FileDocument42 paginiSem4 Complete Fileghufra baqiÎncă nu există evaluări
- Biblical World ViewDocument15 paginiBiblical World ViewHARI KRISHAN PALÎncă nu există evaluări
- What's New in CAESAR II: Piping and Equipment CodesDocument1 paginăWhat's New in CAESAR II: Piping and Equipment CodeslnacerÎncă nu există evaluări
- 6GK74435DX040XE0 Datasheet enDocument3 pagini6GK74435DX040XE0 Datasheet enLuis CortezÎncă nu există evaluări
- Baseline Scheduling Basics - Part-1Document48 paginiBaseline Scheduling Basics - Part-1Perwaiz100% (1)
- ECE Companies ListDocument9 paginiECE Companies ListPolaiah Geriki100% (1)
- The RBG Blueprint For Black Power Study Cell GuidebookDocument8 paginiThe RBG Blueprint For Black Power Study Cell GuidebookAra SparkmanÎncă nu există evaluări
- Executive Summary-P-5 181.450 To 222Document14 paginiExecutive Summary-P-5 181.450 To 222sat palÎncă nu există evaluări
- Contents EEMUA Publication 190 Edition1 May 2015Document4 paginiContents EEMUA Publication 190 Edition1 May 2015Aditya JainÎncă nu există evaluări
- Lecture 14 Direct Digital ManufacturingDocument27 paginiLecture 14 Direct Digital Manufacturingshanur begulaji0% (1)
- Inside:: Issue 4 - February 2004 Bi-Monthly Warhammer E-ZineDocument40 paginiInside:: Issue 4 - February 2004 Bi-Monthly Warhammer E-ZineJoe BloggsÎncă nu există evaluări
- Activity Title: Learning Targets: Reference (S)Document5 paginiActivity Title: Learning Targets: Reference (S)Jhev LeopandoÎncă nu există evaluări
- Triaxial Shear TestDocument10 paginiTriaxial Shear TestAfiqah Nu'aimiÎncă nu există evaluări