Documente Academic
Documente Profesional
Documente Cultură
Pathophysiology of DM II
Încărcat de
Julie SimaurioTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Pathophysiology of DM II
Încărcat de
Julie SimaurioDrepturi de autor:
Formate disponibile
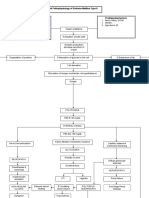
Normal Physiology Pancreas (Located in the upper abdomen)
Endocrine function (Islets of Langerhans)
Exocrine function
Alpha cells Glucagon
Beta cells Insulin
Delta cells Somastatin
Secretion of digestive pancreatic enzymes to GI tract
Pancreas continuously releases small amounts of insulin (basal insulin)
*during fasting periods (between meals and overnight)* Glucagon stimulates the liver to release stored glucose
*when meal is taken*
Exerts a hypoglycemic effect by interfering with the release of growth hormone from pituitary and glucagon from pancreas Insulin binds to special receptors on cell surfaces and initiates series of actions involved in glucose metabolism
Insulin secretion increases and moves glucose from blood into the muscle, liver and fat cells
- transport and metabolize glucose for energy -Stimulate storage of glucose in the liver and muscle (glucogen) -Signals the liver to stop the release of glucose -Enhances the storage of dietary fat in adipose tissues -Accelerates transport of amino acids into cells -Inhibits the breakdown of stored glucose, protein and fat
Maintain the constant level of glucose in the blood
Pathophysiology: Predisposing factors: - Hereditary factor (familial history of DM, fathers side) Precipitating factors: -diet (high sugar)
Diabetes mellitus is a group of metabolic diseases characterized by increase level of glucose in the blood Oral antihyperglycemics Insulin resistance (decrease tissue sensitivity to insulin) Impaired insulin secretion
Insulin
Intracellular reactions are diminished Cell starvation Insulin is less effective at stimulating glucose uptake by the tissues and at regulating glucose release by the liver Compensatory mechanism: increased amounts of insulin must be secreted to maintain the glucose level at normal or slightly elevated level Overtime, beta cells cannot keep up with the increased demand for insulin Management: Nutritional support Exercise Blood glucose monitoring Social and psychological support
Increased secretion of glucagon to stimulate liver to release stored glucose through breakdown of glycogen (glycogenolysis)
Metabolic syndrome: hypertension, hypercholesterolemia, and abdominal obesity Risk for unstable blood glucose level
Stored glucose runs out, liver forms glucose from breakdown of non carbohydrate substances including amino acids and fats
Glucose produced may not be enough for normal metabolic needs Brain interprets as need for food Polyphagia Decreased ATP production Decreased energy, weakness Risk for Activity Intolerance
Glucose level rises and builds up in the blood
Increase blood concentration
Increase in the viscosity of the blood (hyperviscosity)
Increased extracellular osmolarity Osmotic diuresis Polyuria
Decrease ability to perfuse effectively
Sluggish blood flow Polydipsia
Risk for ineffective tissue perfusion
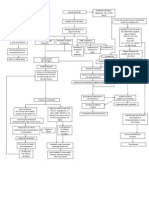
Damage to macro and microvascular circulation
Risk for fluid and electrolyte imbalance
Injury to blood vessel wall
Attempt to repair
Activation of inflammatory process
Release of chemical mediators
Vascular changes
Increased blood flow
Increased capillary permeability
Leakage of plasma and protein components to injured tissue
Migration of leukocytes
Release of biochemical substances
Further damage to vascular tissue
Necrosis of injured tissue
Retinopathy
Nephropathy
Neuropathy
Decrease in sensory
Damage on the capillaries causing opacity
Increased stressed in glumerular filtration
Management: Nutrition: regulate CHON, Fluid, Na, K, increase caloric intake, and vitamins Avoid or delay complications
Numbness tingling sensation
Cataract
Prolonged inflammatory response (attempt to repair)
Scarring and loss of glumerular filtration membrane
Damage in capillary membrane
Ketoanalogues
Decrease glumerular filtration rate
Plasma protein leaked into the urine
Loss of protein
Decrease ability of kidney to remove bodys metabolic wastes
Decrease ability to perform regulatory functions Decrease ability to release erythropoietin Decrease stimulation of bone marrow to produce RBCs
Stimulates synthesis of lipoproteins
hypoalbuminemia
Build up of metabolic wastes in the body
hyperlipidemia
Decrease oncotic pressure
Further damage in the kidney and other parts of the body
Erythropoietin
Fluid shifting from intravascular to interstitial
Subjected to peritoneal dialysis
Unable to keep up with erythrocyte demand Risk for ineffective tissue perfusion
Risk for fluid and electrolyte imbalance
Creation of access
Anemia
Impaired tissue and skin integrity
Fe Sulfate
Acute pain/ impaired comfort
Risk for infection
Disturbed sleep pattern
Poor appetite
Imbalanced nutrition: less than body requirements
S-ar putea să vă placă și
- Pathophysiology of DMDocument5 paginiPathophysiology of DMRgn Mckl100% (3)
- Pathophysiology of Diabetes Mellitus Type 2Document7 paginiPathophysiology of Diabetes Mellitus Type 2jnrue_aerith96% (28)
- Pathophysiology of Diabetes Mellitus Type 2Document1 paginăPathophysiology of Diabetes Mellitus Type 2faula rocamora100% (3)
- Diabetes Mellitus Type 2 Schematic DiagramDocument1 paginăDiabetes Mellitus Type 2 Schematic DiagramJhe Lyn82% (11)
- Pathophysiology of Diabetes Mellitus Type 2Document4 paginiPathophysiology of Diabetes Mellitus Type 2jo_annamae4413100% (3)
- Pathophysiology of Type 2 Diabetes MellitusDocument7 paginiPathophysiology of Type 2 Diabetes MellitusarbyjamesÎncă nu există evaluări
- Pathophysiology - Diabetes Mellitus Type 2Document3 paginiPathophysiology - Diabetes Mellitus Type 2Francis Kevin Sagudo100% (10)
- Pathophysiology of Diabetes Mellitus Type 2Document5 paginiPathophysiology of Diabetes Mellitus Type 2LesValenzuelaÎncă nu există evaluări
- Pathophysiology in Liver CirrhosisDocument4 paginiPathophysiology in Liver CirrhosisCyrus Ortalla RobinÎncă nu există evaluări
- DM Type 2 PathophysiologyDocument3 paginiDM Type 2 PathophysiologyuzumakiruleÎncă nu există evaluări
- CKD PathoDocument5 paginiCKD PathoJohn MIchael AusaÎncă nu există evaluări
- Pathophysiology: Precipitating FactorDocument6 paginiPathophysiology: Precipitating FactorMark Anthony YabresÎncă nu există evaluări
- Pathophysiology ESRDDocument9 paginiPathophysiology ESRDJaye DangoÎncă nu există evaluări
- Pathophysiology of CVA D/T DMDocument3 paginiPathophysiology of CVA D/T DMDanielle Marie SamblacenoÎncă nu există evaluări
- Pathophysiology of Heart FailureDocument4 paginiPathophysiology of Heart FailureTiger Knee100% (2)
- Pathophysiology DMDocument1 paginăPathophysiology DMMJ AmarilloÎncă nu există evaluări
- Pathophysiology of Diabetes Mellitus Type 1Document3 paginiPathophysiology of Diabetes Mellitus Type 1CajRofuli100% (2)
- Diabetes Insipidus Pathophys DiagramDocument1 paginăDiabetes Insipidus Pathophys Diagrampaupaulala100% (4)
- Chronic Renal FailureDocument3 paginiChronic Renal FailureIvana Yasmin Bulandres100% (2)
- Chronic Kidney Disease Pathophysiology - Schematic DiagramDocument3 paginiChronic Kidney Disease Pathophysiology - Schematic DiagramJake CaballoÎncă nu există evaluări
- Pathophysiology HypertensionDocument1 paginăPathophysiology HypertensionAlinor Abubacar100% (3)
- Pathophysiology of Rheumatoid ArthritisDocument1 paginăPathophysiology of Rheumatoid ArthritisGerardeanne ReposarÎncă nu există evaluări
- Pathophysiology CVDDocument1 paginăPathophysiology CVDPamela Shiermaine FilomenoÎncă nu există evaluări
- Chronic Kidney Disease Stage 5Document21 paginiChronic Kidney Disease Stage 5Kristine Anne Soriano100% (1)
- PatofkuDocument3 paginiPatofkunisaaa88Încă nu există evaluări
- Stroke PathophysiologyDocument3 paginiStroke PathophysiologyMaureen EricaÎncă nu există evaluări
- Pathophysio CRF RevisedDocument2 paginiPathophysio CRF Revisedroseanne18Încă nu există evaluări
- Sle FinalDocument41 paginiSle FinalAsniah Hadjiadatu Abdullah100% (1)
- Pathophysiology Hemorrhagic StrokeDocument1 paginăPathophysiology Hemorrhagic StrokeJeffrey Dela CruzÎncă nu există evaluări
- Diabetes Mellitus Type 2 Schematic DiagramDocument1 paginăDiabetes Mellitus Type 2 Schematic DiagramChristelle GarciaÎncă nu există evaluări
- Patof DMDocument1 paginăPatof DMxerwaneÎncă nu există evaluări
- Pathophysiology of DMDocument4 paginiPathophysiology of DMNicole Louise N. VillanuevaÎncă nu există evaluări
- Pathophysiology of StrokeDocument4 paginiPathophysiology of StrokeACe JAyÎncă nu există evaluări
- Pathophysiology of Chronic Kidney Disease: Predisposing Factors: Precipitating FactorsDocument1 paginăPathophysiology of Chronic Kidney Disease: Predisposing Factors: Precipitating FactorsReina SamsonÎncă nu există evaluări
- Pathophysiology CKDDocument1 paginăPathophysiology CKDReymon Mary JanineÎncă nu există evaluări
- Pathophysiology of Acute Kidney InjuryDocument4 paginiPathophysiology of Acute Kidney InjuryJane Arian Berzabal0% (1)
- Individual Case Study Acute GlomerulonephritisDocument26 paginiIndividual Case Study Acute GlomerulonephritisBatrisyia HalimsÎncă nu există evaluări
- Pathophysiology CHFDocument3 paginiPathophysiology CHFKim Franzel M. Rabe100% (1)
- Pathophysiology of HCVD, DM2, CVD (Left Basal Ganglia)Document1 paginăPathophysiology of HCVD, DM2, CVD (Left Basal Ganglia)rexale ria100% (1)
- Pathophysiology of Chronic Kidney DiseaseDocument2 paginiPathophysiology of Chronic Kidney DiseaseKeij AranetaÎncă nu există evaluări
- Pathophysiology CVADocument1 paginăPathophysiology CVANenette Aquino100% (2)
- Pathophysiology On DementiaDocument2 paginiPathophysiology On Dementiaiamjulzcurtis50% (2)
- Pathophysio Chronic GlomerulonephritisDocument1 paginăPathophysio Chronic GlomerulonephritisRan Ma100% (1)
- Hypertension PathophysiologyDocument1 paginăHypertension PathophysiologyZaida Eunice EstabayaÎncă nu există evaluări
- Pathophysiology - HyperthyroidismDocument2 paginiPathophysiology - HyperthyroidismCaren Reyes100% (5)
- Pathophysiology Renal FailureDocument3 paginiPathophysiology Renal FailureHampson Malekano100% (2)
- Case Study CKD DM Type 2Document7 paginiCase Study CKD DM Type 2Brian Cornel0% (3)
- Qtsoi Concept MapDocument5 paginiQtsoi Concept MapGenella BabantoÎncă nu există evaluări
- PathophysiologyDocument1 paginăPathophysiologynitlihpÎncă nu există evaluări
- Endocrine Pancreas Functions and DiabetesDocument53 paginiEndocrine Pancreas Functions and DiabetesDr.Gomathi sivakumarÎncă nu există evaluări
- The Endocrine Functions of The Pancreas4923 160122104950Document26 paginiThe Endocrine Functions of The Pancreas4923 160122104950Nancy Akunna100% (1)
- Hormones in Metabolism: The Roles of Insulin and GlucagonDocument45 paginiHormones in Metabolism: The Roles of Insulin and GlucagonAciÎncă nu există evaluări
- Diabetic Ketoacidosis and Hyperglycemic Hyperosmolar SyndromeDocument59 paginiDiabetic Ketoacidosis and Hyperglycemic Hyperosmolar Syndromenatalieshirley100% (1)
- Pancreas & parathyroid gland regulate calcium, phosphate metabolismDocument40 paginiPancreas & parathyroid gland regulate calcium, phosphate metabolismahmad aliÎncă nu există evaluări
- Pancreas: Cells and Secretions of The Pancreatic IsletsDocument8 paginiPancreas: Cells and Secretions of The Pancreatic IsletsansahÎncă nu există evaluări
- The Pancreas: Roles of Key Hormones Like Insulin, Glucagon and Somatostatin in Glucose HomeostasisDocument54 paginiThe Pancreas: Roles of Key Hormones Like Insulin, Glucagon and Somatostatin in Glucose HomeostasisandreÎncă nu există evaluări
- 8.0 CarbohydratesDocument11 pagini8.0 CarbohydratesHry WkÎncă nu există evaluări
- DiabetesDocument2 paginiDiabetespaul andrew laranjo asuncionÎncă nu există evaluări
- Dr. Solomon Sathishkumar, MD Department of Physiology Christian Medical College Vellore, IndiaDocument48 paginiDr. Solomon Sathishkumar, MD Department of Physiology Christian Medical College Vellore, IndiaKrairat KomdeeÎncă nu există evaluări
- Diabetic Cooking for One and TwoDe la EverandDiabetic Cooking for One and TwoEvaluare: 3 din 5 stele3/5 (1)
- HCCM System Technical Specification v1Document12 paginiHCCM System Technical Specification v1Ankita ChowdhuryÎncă nu există evaluări
- Recent Developments in Ultrasonic NDT Modelling in CIVADocument7 paginiRecent Developments in Ultrasonic NDT Modelling in CIVAcal2_uniÎncă nu există evaluări
- CE ProblemDocument5 paginiCE ProblemJho FÎncă nu există evaluări
- Canopen-Lift Shaft Installation: W+W W+WDocument20 paginiCanopen-Lift Shaft Installation: W+W W+WFERNSÎncă nu există evaluări
- Institutional Competency Assessment Instrument (ICAI)Document12 paginiInstitutional Competency Assessment Instrument (ICAI)Bea EtacÎncă nu există evaluări
- Assignment of A Glass Transition Temperature Using Thermomechanical Analysis: Tension MethodDocument4 paginiAssignment of A Glass Transition Temperature Using Thermomechanical Analysis: Tension MethodEric GozzerÎncă nu există evaluări
- Handout CalmAlphaDocument2 paginiHandout CalmAlphaDave SnowdenÎncă nu există evaluări
- Asian Studies For Filipinos The Philippines in The Asian CenturyDocument15 paginiAsian Studies For Filipinos The Philippines in The Asian CenturyGlaizza QuintonÎncă nu există evaluări
- Preparatory Lights and Perfections: Joseph Smith's Training with the Urim and ThummimDocument9 paginiPreparatory Lights and Perfections: Joseph Smith's Training with the Urim and ThummimslightlyguiltyÎncă nu există evaluări
- Short Answers Class 9thDocument14 paginiShort Answers Class 9thRizwan AliÎncă nu există evaluări
- Bolt Jul 201598704967704 PDFDocument136 paginiBolt Jul 201598704967704 PDFaaryangargÎncă nu există evaluări
- Psalms Magick of The Old Testament PDFDocument129 paginiPsalms Magick of The Old Testament PDFirrrs100% (1)
- Nutritional support through feeding tubesDocument76 paginiNutritional support through feeding tubesKryzza LeizellÎncă nu există evaluări
- Teaching TrigonometryDocument20 paginiTeaching Trigonometryapi-21940065Încă nu există evaluări
- Chapter 7 - The Political SelfDocument6 paginiChapter 7 - The Political SelfJohn Rey A. TubieronÎncă nu există evaluări
- MacEwan APA 7th Edition Quick Guide - 1Document4 paginiMacEwan APA 7th Edition Quick Guide - 1Lynn PennyÎncă nu există evaluări
- Sight Reduction Tables For Marine Navigation: B, R - D, D. SDocument12 paginiSight Reduction Tables For Marine Navigation: B, R - D, D. SGeani MihaiÎncă nu există evaluări
- GBM Auction Versus English Auction A Large-Scale Empirical Study - E. Bessire, K. Elhadji Tchiambou (October 2021)Document18 paginiGBM Auction Versus English Auction A Large-Scale Empirical Study - E. Bessire, K. Elhadji Tchiambou (October 2021)Guillaume GonnaudÎncă nu există evaluări
- SIM7020 Series - HTTP (S) - Application Note - V1.04Document15 paginiSIM7020 Series - HTTP (S) - Application Note - V1.04Vinicius BarozziÎncă nu există evaluări
- English For Academic Purposes (EAP) : Lecture 5: Past SimpleDocument11 paginiEnglish For Academic Purposes (EAP) : Lecture 5: Past Simplealmastar officeÎncă nu există evaluări
- SPSS-TEST Survey QuestionnaireDocument2 paginiSPSS-TEST Survey QuestionnaireAkshay PatelÎncă nu există evaluări
- Department of Education Doña Asuncion Lee Integrated School: Division of Mabalacat CityDocument2 paginiDepartment of Education Doña Asuncion Lee Integrated School: Division of Mabalacat CityRica Tano50% (2)
- Degree and Order of ODEDocument7 paginiDegree and Order of ODEadiba adibÎncă nu există evaluări
- Vonovia 9M2021 Presentation 20211118Document76 paginiVonovia 9M2021 Presentation 20211118LorenzoÎncă nu există evaluări
- Soft StarterDocument6 paginiSoft StarterEric Maglinte TolosaÎncă nu există evaluări
- J-Garlic in CheeseDocument12 paginiJ-Garlic in CheeseMary GinetaÎncă nu există evaluări
- PS Neo HSK2LCD ICON LED RF Keypad v1 0 Installation Guide R001 en FR Es PoDocument40 paginiPS Neo HSK2LCD ICON LED RF Keypad v1 0 Installation Guide R001 en FR Es Po7seguridadÎncă nu există evaluări
- Administrations whose CoCs are accepted for CECDocument1 paginăAdministrations whose CoCs are accepted for CECGonçalo CruzeiroÎncă nu există evaluări
- STS Syllabus 2020Document27 paginiSTS Syllabus 2020AndreaDimaculangan100% (1)
- Ultimate Guide To Construction SubmittalsDocument10 paginiUltimate Guide To Construction SubmittalsDavid ConroyÎncă nu există evaluări