Documente Academic
Documente Profesional
Documente Cultură
Marasmus
Încărcat de
Rojanisa Baculi RomathoTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Marasmus
Încărcat de
Rojanisa Baculi RomathoDrepturi de autor:
Formate disponibile
Marasmus occurs when energy intake, intake of carbohydrates, is insufficient for the body's energy requirements.
The body forced to draw on its own emergency stores. Liver glycogen is exhausted within a few hours, and skeletal muscle protein is then used via gluconeogenesis to maintain adequate amounts of blood glucose in the bloodstream. At the same time, triglycerides in fat depots are broken down into free fatty acids, which provide some energy for most tissues, but not for the nervous system, especially neurons in the brain, who rely on .
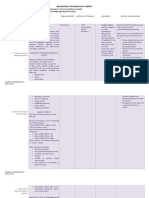
Pathophysiology In marasmus, energy intake is insufficient for the body's requirements, and the body draws on its own stores. Liver glycogen is exhausted within a few hours, and skeletal muscle protein is then used via gluconeogenesis to maintain adequate plasma glucose. At the same time, triglycerides in fat depots are broken down into free fatty acids, which provide some energy for most tissues, but not for the nervous system. When near starvation is prolonged, fatty acids are incompletely oxidized to ketone bodies, which can be used by the brain and other organs for energy. Thus, in the severe energy deficiency of marasmus, adaptation is facilitated by high cortisol and growth hormone levels and depression of insulin and thyroid hormone secretion. Because amino acids are mobilized from muscle to provide the liver with substrate for protein synthesis, plasma protein levels decrease less in marasmus than in kwashiorkor. Related Topics: Cortisol - Insulin - Thyroid hormone - Amino acid ~~~~~~~~~~ In kwashiorkor, relatively increased carbohydrate intake with decreased protein intake leads to decreased visceral protein synthesis. The resulting hypoalbuminemia causes dependent edema, and impaired -lipoprotein synthesis causes fatty liver. Insulin secretion is initially stimulated but is reduced later in the disease. Fat mobilization and amino acid release from muscle are reduced, so that less amino acid substrate is available to the liver. In marasmus and kwashiorkor, the insulin response to a glucose load is poor, possibly due to chromium deficiency. Related Topics: ~~~~~~~~~~ Total body protein synthesis is about 300 g/day or 5 (g/kg)/day in the average adult male. The daily obligatory loss is only about 60 to 75 g (9 to 12 g nitrogen), because 75 to 80% is reused. The RDA of protein for an adult is about 0.8 g/kg; infants and children require 1 to 2 (g/kg)/day . Thus, infants require a higher proportion of essential amino acids in their diet than do adults. Related Topics: ~~~~~~~~~~ In protein deficiency, adaptive enzyme changes occur in the liver, amino acid synthetases increase, and urea formation diminishes, thus conserving nitrogen and reducing its loss in urine. Homeostatic mechanisms initially operate to maintain the level of plasma albumin and other transport proteins. The rates of albumin synthesis eventually decrease, and plasma levels fall, leading to reduced oncotic pressure and edema. Growth, immune response, repair, and production of some enzymes and hormones are impaired in severe protein deficiency.
I. Nutritional deficiency Problems a) Malnutrition The primary cause of malnutrition is inadequate and faulty diet. Apart from poverty and other socio economic factors, environmental factors also play an important role in aggravating the dietary deficiency diseases. These precipitating factors are the widespread chronic infections among the poor living under conditions of poor environmental sanitation and personal hygiene. Malnutrition continues to be a major health problem in the world today, particularly in children younger than 5 years of age. Lack of food; however is not always the primary cause for malnutrition. In many developing and underdeveloped nations, diarrhea is a major factor. Additional factors are bottle feeding (in poor sanitary conditions), inadequate knowledge of proper child care practices, parental illiteracy, economic and political factors, and simply the lack of adequate food for children. Levels of Malnutrition India has among the highest levels of child malnutrition in the world, and the persistence of the problem has led to the formulator of the National Nutrition policy by the government of India. UNICEF reports auch programmes through strategies promote BF and to timely introduction of complementary foods, encouraging clean environment with portable water, and tackling diarrhoeal and other infections. Reasons for the problems of Malnutrition in India Food availability and Related Problems Low per capita food availability Low purchasing capacity of the masses Mal distribution of the available food Limited choice of food articles. Poverty and Malnutrition Ramification of poverty Low income of the masses Poverty malnutrition interaction Population Problem and Malnutrition Population explosion Effects on food availability Effects of uncontrolled fertility on nutrition. Social Factors Affecting Nutritional Status
Customs, superstitions and taboos. Diet during illness Caste and false social status. Food tastes and faulty cooking methods. Food combinations. Influence of industrialization and urbanization and modernization. Ignorance and lack of education. Alcohol and malnutrition. Protein Energy Malnutrition Protein Energy Malnutrition is defined as a range of pathological conditions arising from coincident lack of varying proportions of protein and calorie, occurring most frequently in infants and young children and often associated with infection. -WHO 1973 PEM has been identified since long as a major nutritional problem in India. Insufficiency of food the so called food gap appears to be the chief cause of PEM, which is a major health problem particularly in the first years of life. Various studies on dietary intake reveal that the gap intake among children on habitual cereal pulse based diet is primarily due to inadequate intake of such diets and not the quality of protein. Severe form of malnutrition (PEM) leads to two clinical forms of disorders. They are as follows: Kwashiorkor Kwashiorkor is the condition of deficiency of protein with an adequate supply of calories. A diet consisting mainly of starch grains or tubers provides adequate calories in the form of carbohydrates but an inadequate amount of high quality proteins. The child with kwashiorkor has thin, wasted extremities and a prominent abdomen from edema (ascites). The edema often masks the severe muscular atrophy, making the child appear less debilitated than he or she actually is. The skin is scaly and dry and has areas of depigmentation. Diarrhoea commonly occurs from lowered resistance to infection and produces electrolyte imbalance. Protein deficiency increases the childs susceptibility to infection, which eventually results in death. Marasmus
Marasmus results from general malnutrition of both calories and protein. It is common occurrence in underdeveloped countries during the times of the drought, especially in cultures where adults eat first, the remaining food is often in sufficient in quality and quantity for the children.
Marasmus is usually a syndrome of physical and emotional deprivation and is not confined to geographic areas where food supplies are inadequate. Marasmus is characterized by gradual wasting and atrophy of body tissues, especially of subcutaneous fat. The child appears to be very old, with flabby and wrinkled skin. The child is fretful, apathetic, withdrawn and so lethargic Causes of Protein Energy Malnutrition a) Nutritional Factors Poor caring practices include
Not feeding the sick children. Not providing the adequate complementary feeding. Not supporting mothers to breast- feed adequately. Non breastfed. Late weaning. Inadequate supplementation. Failure to feed during illness. Failure to increase to caloric intake immediately after the illness. b) Non Nutritional Factors Due to poverty, mother is not able to provide sufficient food to the child resulting in under nutrition.
Non- immunization Improper growth monitoring. Poor weight gain during adolescence Poor environmental and personal hygiene Illiteracy Large family
False beliefs Failure to utilize Health/Hospital care. Low agricultural inputs, marketing, distribution of food and income. Poor and inadequate water and sanitation facilities. Political Problems Inadequate resources include money, material and manpower refers to the poor quality, expensive and non convenience.
Lack of health care services and information regarding maternal and child care practices on basis of inadequate time and resources for taking care of health diet, emotional and psychological needs of women and children. Poor caring practices include
Poor antenatal care. Food taboos during and after pregnancy. Inadequate management of sick and malnourished. Infestation like ascariasis particularly giardiasis may lead to anorexia. Signs and Symptoms of different types of PEM Kwashiorkor
Oedema of the face and lower limbs Failure to thrive Anorexia Diarrhoea Apathy Dermatosis ( hypo and hyper- pigmentation) Sparce Soft and thin hair Angular stomatitis Cheilosis Anemia Marasmus
Failure to thrive Irritability Fretfulness and apathy are common Diarrhoea is frequent Many are hungry but some may be anorexic The child is shrunk and there is little or no subcutaneous fat. There is often dehydration Temperature is subnormal Watery diarrhea and acid stools may be present.
Muscles are weak and atrophic Limbs appear as skin and bones Marasmic Kwashiorkor These children exhibit a mixture of some of the features of both marasmus and kwashiorkor. Management of PEM Therapeutic Management
Adequate nutritious diet either by breastfeeding or a proper weaning diet. Five grams of protein/ kg body weight/day should be given for the existing weight. Rehydration with an oral rehydration solution that also replaces electrolytes. Treatment of infections. Medications such as antibiotics and antidiarrheals. Health education Fats: Forty percent of total calories can be from fat which can be tolerated by children. Saturated fats such as butter, milk and coconut oil are preferred because unsaturated fatty acids worsen diarrhea. Energy: It is important that there should be enough calories in the diet; otherwise proteins will be utilized for energy purposes and not for building the tissues. Vitamin A should be supplied immediately. Anemia: Folic acid should be given
Nursing Care Management Provision of essential physiologic needs, such as protection from infection, adequate hydration, skin care and restoration of physiologic integrity because children usually weak and withdrawn, they depend on others for feeding. Oral rehydration with an approved oral rehydration solution is commonly used in cases of PEM where diarrhea and infection are not immediately life threatening. Health education concerning the importance of proper nutrition, whether breastfeeding or bottle feeding, when being weaned to semisolid foods. Children with marasmus may suffer from emotional starvation as well; care should be consistent with care of the child with failure to thrive )Vitamin Deficiency Vitamin A deficiency Vitamin A deficiency is a major nutritional problem affecting young children leading to blindness. In India about 5 7 percent children suffer annually from eye damage caused by vitamin A Deficiency, Recent evidence suggests that mild vitamin A deficiency probably increases morbidity and mortality in children, highlighting the public health importance of this disorder. Surveys show, that 1-5 percent of children have clinical signs of vitamin A deficiency. The prevalence rates are higher in school age children than in younger age groups, but severe forms of the deficiency resulting in blindness are confined to children below 3 years.
The causes of severe form of vitamin A deficiency like Xerophthalmia arises when the diet contains practically no whole milk and butter and very limited amounts of fresh vegetables and fruit so lacks both retinol and carotenes.Xerophthalmia and keratomalacia both occur in the first year of life amongst artificially fed infants but rare amongst the breast fed. If the mothers diet during pregnancy is low in vitamin A, the child is born with low stores of vitamin A. Protein energy Malnutrition further aggravates the partial deficiency because absorption and plasma transport of vitamin A are impaired.Diarrhoea is known to be a precipitating factor in keratomalacia. The major factors contributing to low availability of vitamin A are lack of awareness of the importance of consuming vitamin A rich food and poverty leading to limited accessibility to vitamin A rich food. The Clinical Forms of the Deficiency will include:Vitamin A Deficiency: - Vitamin A deficiency is seen more commonly in younger children i.e. between 6 months and 3 years. Vitamin A is indispensable for normal functioning of the eyes. It helps in the production of retinal pigments which are required for vision in dim light. Conjunctival Xerosis:-.The conjunctiva becomes dry, appears muddy and wrinkled due to failure to shed the epithelial cells and consequent keratinisation. The pigmentation gives the conjunctiva a peculiar smoky appearance. This symptom in children under 5 years is more likely to be due to dietary deficiency. Night blindness:- This is the first sign of Xerophthalmia. The child is not able to see in darkness in a dark room or when it gets dark in the late evening. This is due to lack of retinal pigments. Bitots spots:- Although Bitots spots differ somewhat in size, location and shape, they have similar appearance. They are accumulations of fomy cheesy material on the conjunctiva on either side of the cornea, often in association with other signs of Xerophthalmia, such as blindness. In children under 5 years of age they are usually due to vitamin A deficiency. Corneal Xerosis/ ulceration: - The cornea becomes dry (xerosis). If the disease is not treated, the xerosis can progress within hours to an ulcer of the cornea. Corneal Xerosis may progress suddenly and rapidly to keratomalacia. Keratomalacia:- In this softening and dissolution of the cornea occurs. If the process is not stopped by treatment, perforation of the corneal leads to prolapsed of the iris, extrusion of the lens and infection of the whole eyeball which almost invariably occurs. The chance of saving any useful vision are slight. Heating results in scarring of the whole eye and frequently in total blindness. Xerophthalmia fundus:-In school children or young adults with prolonged vitamin A deficiency ophthalmoscopic examination may show lesions appearing as spots, either white or yellow scattered along the sides of the blood vessels. The spots may fuse and the lesions are most numerous on the periphery of the fundus ( boral portion) and never appear on the macula (the yellow spot on the retina. Corneal scars:- These are white, opaque patches on the cornea as a result of healing of an older ulcer. Vision may be affected seriously, depending on the size of
the scars. Management of Vitamin A Deficiency Immediately on diagnosis, water soluble 1, 00,000 IU of vitamin A intramuscularly can be given for corneal xerosis, ulcer, keratomalcia, xerophthalmia, severe infection and malnutrition. Immediately on diagnosis for less severe forms like night blindness, conjunctival xerosis, Bitots spot, oil solutions as palmitate 2, 00,000 IU can be given orally. On second day oil solution of 2, 00, 000 IU orally should be given prior to the discharge from the hospital. Preventive Measures Nutrition and health education should be given to the mothers. Pregnant and lactating mothers should be encouraged to consume dark green leafy vegetables and yellow or orange fruits so that there is sufficient storage in vitamin A in the liver of new born. Mothers should be motivated to feed their children as vitamin A present in the milk is adequate for 3 to 6 months of infants life. The weaning diet should be consist of dark green leafy vegetables, yellow or orange fruits, whole milk, butter, fish and egg. National Vitamin A supplementation programme is a more effective alternate approach. Other measures:Medical paramedical personnel should be trained to detect and treat xerophthalmia They should know the importance of giving vitamin A oily solution once in 6 months at the door steps of the beneficiaries as community approach but not at hospital as clinical approach. They should monitor periodically National Vitamin A prophylaxis programme. Medical and paramedical personnel should be given nutrition education. To prevent vitamin A deficiency intake of green leafy vegetables, yellow fruits its and vegetables like papaya, mango, pumpkin and carrots should be promoted for long term measures kitchen garden should be encouraged. Vitamin D Deficiency Deficiency of vitamin D causes rickets in young children in the age group of 6 months to 2 years. It reduces calcifications of bones which affects growth of bones and cause deformity of bones such as curved legs, pigeon chest, rickety rosary, deformed pelvis. There is delayed teething, standing and walking. It is no more a serious problem because of improvement in child health care services, socio-cultural practices, plenty of available sunshine. Rickets is preventable by simple methods like exposure of children to sunshine regularly and administration of vitamin D as prophylaxis periodically. It requires education of mothers and family members about the importance of exposure of children to sunshine regularly and to give food rich in vitamin D such as butter, cheese, egg yolk, liver, fortified food such as milk, vanaspati oil etc. Fish liver oil is very good source of vitamin D and is available in the form of capsule which can be given under the direction of medical officer. Excessive intake of vitamin D is harmful. It may cause loss of appetite, nausea, vomiting, excessive thirst and drowsiness. There may be renal failure, cardiac arrythemias and unconsciousness. All this is due to increased level of calcium in the blood due to increased absorption of calcium. It is very important to recognize the signs of rickets and refer the child to PHC/ Hospital etc. for therapeutic treatment as early as possible. The mothers and family
members need to be educated about the observations of signs and reporting in the health center to treat and vitamin d deficiency in children. c) Iron Deficiency The iron deficiency causes nutritional anaemia in children. About 50 percent of children have anaemia. It is due to malnutrition. It usually leads to various others problems such as general weakness affecting work performance, reduced immunity and resistance to infections resulting in increased morbidity and mortality. It affects physical and psychological behaviour of the children. There is decrease in the concentration of hemoglobin and it is lower than the normal cut off point set up by WHO, which is 11 g/dl in children 6 months to 6 years. Anaemia is aggravated by worm infestation and malarial parasites. It may also be caused because of these infections. Another factor which causes anaemia is folic acid (folate) deficiency. Anaemia in children can be prevented by preventing and controlling of anaemia in pregnant and nursing mothers by improvement in diet and prophylactic treatment by iron folic acid, and nursing mothers by improvement of diet of children emphasizing on breast feeding, proper weaning and supplementation etc, iron folic acid drops/ tablets as prophylaxis, prevention and treatment of worm infestation and malaria. Fortified salt with iron has been tried out by National Institute of Nutrition to control anemia in regions with high prevalence of anaemia and is accepted by the government as a public health approach to prevent anaemia. Commercially Iron fortified salt is available in the market. The mothers and family members and community people need to be educated by health workers about all these preventive measures. Monitoring of growth and development and anaemia is very important to make an assessment of malnutrition and anaemia and accordingly take corrective measures.
S-ar putea să vă placă și
- Sexually Transmitted InfectionsDocument5 paginiSexually Transmitted InfectionsKANT JAMES D. MAHANÎncă nu există evaluări
- Malnutrition - Group 1Document39 paginiMalnutrition - Group 1Maryam AhmariÎncă nu există evaluări
- COPAR Tally SheetDocument3 paginiCOPAR Tally SheetAnna SarmientoÎncă nu există evaluări
- MARCOS - Legal Issues of ElderlyDocument2 paginiMARCOS - Legal Issues of ElderlyArian May MarcosÎncă nu există evaluări
- SWADDLINGDocument4 paginiSWADDLINGksjsellsÎncă nu există evaluări
- Narrative ReportDocument2 paginiNarrative ReportJanina Cate D TorrecampoÎncă nu există evaluări
- Electronic Health RecordsDocument2 paginiElectronic Health RecordsEdwyn OmondiÎncă nu există evaluări
- Health Teaching Plan General Objectives: After One Hour of Nurse-Patient Interaction, The Patient Will Be Able To Acquire Knowledge, Skills and Attitude RegardingDocument3 paginiHealth Teaching Plan General Objectives: After One Hour of Nurse-Patient Interaction, The Patient Will Be Able To Acquire Knowledge, Skills and Attitude RegardingJAMES PATRICK MONTEMAYORÎncă nu există evaluări
- Reflection PaperDocument2 paginiReflection PapershanoiapowelllÎncă nu există evaluări
- Impact of Pandemic To The Psychological Aspects of Nursing StudentsDocument25 paginiImpact of Pandemic To The Psychological Aspects of Nursing StudentsBrandon AreteÎncă nu există evaluări
- Developing a Teaching Plan on ObesityDocument6 paginiDeveloping a Teaching Plan on ObesityAntonette Africa MercadoÎncă nu există evaluări
- Involving Family, Domestic Relations, Women and Children. (2015) - Philippine JudicialDocument10 paginiInvolving Family, Domestic Relations, Women and Children. (2015) - Philippine JudicialAngel MayÎncă nu există evaluări
- Framework For Maternal and Child Health NursingDocument18 paginiFramework For Maternal and Child Health NursingKristil ChavezÎncă nu există evaluări
- Fatima 121 ThesisDocument144 paginiFatima 121 ThesisNecesario BanaagÎncă nu există evaluări
- Cultural Beliefs On Disease Causation in The PhilippinesDocument19 paginiCultural Beliefs On Disease Causation in The PhilippinesDexter ReyesÎncă nu există evaluări
- Nursing Care of A Family With A Toddler Child: Christine M. Fiel, RN MN LPT MaedDocument25 paginiNursing Care of A Family With A Toddler Child: Christine M. Fiel, RN MN LPT MaedJrose CuerpoÎncă nu există evaluări
- NCPDocument6 paginiNCPgenevieve kryzleiÎncă nu există evaluări
- The High-Risk Pregnant Client:: NCM 109 Handout # 1Document3 paginiThe High-Risk Pregnant Client:: NCM 109 Handout # 1ApRil Anne BalanonÎncă nu există evaluări
- Problem With The PassageDocument3 paginiProblem With The PassageLuiciaÎncă nu există evaluări
- Chapter IIDocument31 paginiChapter IIyssa_03Încă nu există evaluări
- Teaching PlanDocument6 paginiTeaching PlanAngel Damo100% (1)
- Coxsackievirus NCP W Patho 3Document3 paginiCoxsackievirus NCP W Patho 3Chryst Louise SaavedraÎncă nu există evaluări
- Teaching PlanDocument1 paginăTeaching PlanUnis OwtwoÎncă nu există evaluări
- Transient Tachypnea of The NewbornDocument6 paginiTransient Tachypnea of The NewbornTarquin TomadaÎncă nu există evaluări
- Week 8 - Activity (Case Scenario)Document7 paginiWeek 8 - Activity (Case Scenario)Jollan Marie BuenvenidaÎncă nu există evaluări
- Breastfeeding and Complementary FeedingDocument20 paginiBreastfeeding and Complementary FeedingJohn Christian LasalitaÎncă nu există evaluări
- Famacion - CHN - General Requirements Week 3Document3 paginiFamacion - CHN - General Requirements Week 3Kyra Bianca R. FamacionÎncă nu există evaluări
- Phototherapy For Neonatal JaundiceDocument5 paginiPhototherapy For Neonatal JaundiceMichael RameresÎncă nu există evaluări
- Nutrition for pregnant and lactating womenDocument3 paginiNutrition for pregnant and lactating womenmo'niqueÎncă nu există evaluări
- Chapter 8: Nursing Care of The Subfertile CoupleDocument10 paginiChapter 8: Nursing Care of The Subfertile CoupleAlyssaGrandeMontimorÎncă nu există evaluări
- Elec 121Document14 paginiElec 121MARITONI MEDALLAÎncă nu există evaluări
- Kap Model 2 PDFDocument7 paginiKap Model 2 PDFirahkubÎncă nu există evaluări
- Introduction To Community Health Nursing ExposureDocument33 paginiIntroduction To Community Health Nursing ExposureRay LaderaÎncă nu există evaluări
- Aquino Health AgendaDocument41 paginiAquino Health AgendaJannine Mae Zaragosa MosquisaÎncă nu există evaluări
- Clubfoot Definition, Types, and TreatmentDocument5 paginiClubfoot Definition, Types, and TreatmentcrisolandÎncă nu există evaluări
- COPAR: Community Participatory Action ResearchDocument5 paginiCOPAR: Community Participatory Action ResearchEdezer CariasÎncă nu există evaluări
- Handwashing QuestionsDocument2 paginiHandwashing Questionsknicky FranciscoÎncă nu există evaluări
- Public Health Nursing in SchoolsDocument45 paginiPublic Health Nursing in SchoolsdaveÎncă nu există evaluări
- Critical Reading, Writing and Thinking: Lady Ciane L. CruzDocument5 paginiCritical Reading, Writing and Thinking: Lady Ciane L. CruzROBERT JOHN PATAG0% (2)
- Module 14Document5 paginiModule 14camille nina jane navarroÎncă nu există evaluări
- St. Paul University Philippines: School of Nursing and Allied Health Sciences College of NursingDocument5 paginiSt. Paul University Philippines: School of Nursing and Allied Health Sciences College of NursingChristian UmosoÎncă nu există evaluări
- Administering An EnemaDocument2 paginiAdministering An EnemaJazzmin Angel ComalingÎncă nu există evaluări
- Community Health SurveyDocument14 paginiCommunity Health Surveyapi-273787321Încă nu există evaluări
- CHN Case Analysis Case ScenarioDocument7 paginiCHN Case Analysis Case ScenarioNathalie kate petallarÎncă nu există evaluări
- Funda HandwashingDocument4 paginiFunda HandwashingPichi PichiÎncă nu există evaluări
- Coughs and Colds Nurse Management of Upper Respiratory Tract InfectionDocument3 paginiCoughs and Colds Nurse Management of Upper Respiratory Tract InfectionMichael Anthony ErmitaÎncă nu există evaluări
- Nursing Informatics: Connecting Technology and Patient Care (First Edition)Document21 paginiNursing Informatics: Connecting Technology and Patient Care (First Edition)Praveen LoniÎncă nu există evaluări
- Examining root causes of poor health and diseaseDocument1 paginăExamining root causes of poor health and diseaseDONITA DALUMPINESÎncă nu există evaluări
- Placino HIRSCHPRUNG DX PDFDocument15 paginiPlacino HIRSCHPRUNG DX PDFSiena PlacinoÎncă nu există evaluări
- Health Education Seminar ReportDocument2 paginiHealth Education Seminar ReportNova Kristine Maglupay100% (1)
- Sample 3Document42 paginiSample 3VeniceÎncă nu există evaluări
- Evidence-Based Practice in Maternal & Child HealthDocument15 paginiEvidence-Based Practice in Maternal & Child HealthJan Oliver YaresÎncă nu există evaluări
- Health Teaching DengueDocument3 paginiHealth Teaching DenguearjeighÎncă nu există evaluări
- Nursing care plan for malnourished patientDocument5 paginiNursing care plan for malnourished patientbbarnes0912Încă nu există evaluări
- HYDROCELEDocument3 paginiHYDROCELESean Patrick Acoba100% (2)
- Gordons Functional Health Patterns GuideDocument4 paginiGordons Functional Health Patterns GuideteuuuuÎncă nu există evaluări
- Intendido - Mae-Joy - Q. - crwT111 - The Boons and Banes of Academic Freeze in Time of PandemicDocument3 paginiIntendido - Mae-Joy - Q. - crwT111 - The Boons and Banes of Academic Freeze in Time of PandemicMae Joy IntendidoÎncă nu există evaluări
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDe la EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsÎncă nu există evaluări
- Gastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDe la EverandGastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsÎncă nu există evaluări
- Anatomy and Physiology of The GallbladderDocument1 paginăAnatomy and Physiology of The GallbladderRojanisa Baculi RomathoÎncă nu există evaluări
- 13 Principles of Sterile TechniqueDocument13 pagini13 Principles of Sterile TechniqueRojanisa Baculi Romatho80% (5)
- 13 Principles of Sterile TechniqueDocument13 pagini13 Principles of Sterile TechniqueRojanisa Baculi Romatho80% (5)
- Nursing ResearchDocument14 paginiNursing ResearchRojanisa Baculi RomathoÎncă nu există evaluări
- PrefixesDocument11 paginiPrefixesRojanisa Baculi RomathoÎncă nu există evaluări
- Grain GroupDocument7 paginiGrain GroupRojanisa Baculi RomathoÎncă nu există evaluări
- 13 Principles of Sterile TechniqueDocument13 pagini13 Principles of Sterile TechniqueRojanisa Baculi Romatho80% (5)
- 13 Principles of Sterile TechniqueDocument13 pagini13 Principles of Sterile TechniqueRojanisa Baculi Romatho80% (5)
- Abbreviations and Symbols of Medical TermsDocument16 paginiAbbreviations and Symbols of Medical TermsRainida Catherine Romatho100% (1)
- Protein Energy MalnutritionDocument48 paginiProtein Energy MalnutritionG Trinity DeepakÎncă nu există evaluări
- The Open University of Sri Lanka-Department of Health SciencesDocument9 paginiThe Open University of Sri Lanka-Department of Health SciencesDeepal PrasankaÎncă nu există evaluări
- Nutritiona L Disorders: Paulette Benjamin-Chin MD Diplomate, Philippine Pediatric SocietyDocument102 paginiNutritiona L Disorders: Paulette Benjamin-Chin MD Diplomate, Philippine Pediatric SocietygailÎncă nu există evaluări
- Modular Ncma215 Nutrition and Diet Therapy CM 1 Cu 1 Week 1 PandemicDocument15 paginiModular Ncma215 Nutrition and Diet Therapy CM 1 Cu 1 Week 1 PandemicKATHERINE RAMIREZÎncă nu există evaluări
- Activity 2 Midterm Worksheet Proteins Nutrition and Diet Therapy LabDocument11 paginiActivity 2 Midterm Worksheet Proteins Nutrition and Diet Therapy LabckkyleÎncă nu există evaluări
- Nutrition Guide: Calorie Needs, Food Groups, Diet PlansDocument36 paginiNutrition Guide: Calorie Needs, Food Groups, Diet PlansinshÎncă nu există evaluări
- DR Ghamry MCQsDocument29 paginiDR Ghamry MCQsBeshoy AdelÎncă nu există evaluări
- Falcon SPM Paper 1Document20 paginiFalcon SPM Paper 1175 Yellamraju VidhatriÎncă nu există evaluări
- IGNOU Block 2 Unit 4 Nutritional Deficiency DisordersDocument22 paginiIGNOU Block 2 Unit 4 Nutritional Deficiency Disorderserice.research100% (3)
- AsuhanDocument52 paginiAsuhanDedi KurniawanÎncă nu există evaluări
- India Development ProgressDocument90 paginiIndia Development ProgressAnju RaniÎncă nu există evaluări
- Protein Energy MalnutritionDocument72 paginiProtein Energy MalnutritionBahaa ShaabanÎncă nu există evaluări
- Extended Only: CIE IGCSE BiologyDocument1 paginăExtended Only: CIE IGCSE BiologyNour HafezÎncă nu există evaluări
- Macronutrients and MicronutrientsDocument78 paginiMacronutrients and MicronutrientsPATRIZJA YSABEL REYESÎncă nu există evaluări
- Chapter 6: Proteins and Amino Acids: © 2010 Pearson Education, IncDocument53 paginiChapter 6: Proteins and Amino Acids: © 2010 Pearson Education, InclordniklausÎncă nu există evaluări
- Short Atlas in Pediatrics Spot Diagnosis of The Most Common Pediatric Diseases 2nd EditionDocument113 paginiShort Atlas in Pediatrics Spot Diagnosis of The Most Common Pediatric Diseases 2nd Editiondeycallmebud100% (2)
- Pestilence and Disease in The History of AfricaDocument24 paginiPestilence and Disease in The History of AfricaAnonymous 61MXKNtKx100% (1)
- Nutrition Unit I 2021Document145 paginiNutrition Unit I 2021Anuchithra RadhakrishnanÎncă nu există evaluări
- Management of Severe MalnutritionDocument77 paginiManagement of Severe Malnutritionfranklin ifioraÎncă nu există evaluări
- Underweight and MalnutritionDocument61 paginiUnderweight and MalnutritionJack Sinaga100% (1)
- 6.malnutrition inDocument129 pagini6.malnutrition inCHALIE MEQU100% (1)
- Vitamins and nutritional deficiency diseasesDocument2 paginiVitamins and nutritional deficiency diseasesGhubaya CopÎncă nu există evaluări
- Protein Deficiency Diseases ExplainedDocument8 paginiProtein Deficiency Diseases ExplainedGingkaÎncă nu există evaluări
- Dietary Deficiency DiseasesDocument7 paginiDietary Deficiency DiseasesAMIN BUHARI ABDUL KHADER100% (2)
- Nutritional Assessment - PPTXFGRTDocument54 paginiNutritional Assessment - PPTXFGRTAmanuel MaruÎncă nu există evaluări
- Tanda, Ciri-Ciri Dan Perbedaan Versi B InggrisDocument2 paginiTanda, Ciri-Ciri Dan Perbedaan Versi B Inggriselama natilaÎncă nu există evaluări
- Maternal and Child Health ProblemsDocument71 paginiMaternal and Child Health ProblemsQudrat Un Nissa100% (2)
- 321 E Lesson 6Document20 pagini321 E Lesson 6hk_scribd100% (2)
- Unit 1 14.04.20 IIIDocument26 paginiUnit 1 14.04.20 IIIDeepak GuptaÎncă nu există evaluări
- Objectives:: Module On Basic NutritionDocument56 paginiObjectives:: Module On Basic NutritionMomhai Mhaimo100% (1)