Documente Academic
Documente Profesional
Documente Cultură
Center For Personalized Medicine Pilot Project RFA
Încărcat de
Duke Department of MedicineTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Center For Personalized Medicine Pilot Project RFA
Încărcat de
Duke Department of MedicineDrepturi de autor:
Formate disponibile
1 2.1.
2013
Request for Applications Pilot Studies
This announcement introduces a funding opportunity for multidisciplinary, collaborative pilot projects that will
explore personalized medicine topics in the context of Duke Medicine. For this announcement, personalized
medicine means the application of proven medical interventions or therapies that are individualized to
patient characteristics or preferences. The members of the Center for Personalized Medicine (CPM) have
been working toward elucidating personalized medicine outcomes, including clinical, personal, behavioral,
economic and patient satisfaction outcomes, at the patient, provider, practice, and health systems level.
The CPM is interested in receiving proposals that address one or more of the following four topics within the
field of personalized medicine (a full description of each topic and examples follow these guidelines):
- Use of IT and/or Social Media To Promote Health
- Policy and Implementation
- Adoption of Personalized Medicine Concepts and Paradigms in the Clinical Setting
- Personalized Medicine Education
Up to 4 projects will be funded at a level of up to $50,000 each, pending the receipt of appropriate
proposals. There is no guarantee of an award within each topic category. The review will occur in two
stages, with preliminary proposals accepted from the date of this announcement until 5 PM, Monday, March
18. Notification and request for full proposals will be made in April. Final awards will be announced in May,
with earliest anticipated funding of June, 2013.
Preliminary/concept proposals, two (2) pages plus rough budget, should include the following details:
- The specific question to be addressed;
- The application to personalized medicine;
- The collaborative multidisciplinary nature of the project with detail about the contributing
researchers/groups;
- The potential for long term sustainability and funding once the goals of the project are completed.
Full proposals, five (5) pages maximum, plus a detailed budget, will require more detail on these items,
as well as study methods.
Formatting guidelines: minimum of Arial font 11 or equivalent and 1 inch margins
To meet the abovementioned goals, proposals should:
1. Be carried out by a multidisciplinary team of Duke personnel (we encourage collaboration from
multiple schools within Duke)
2. Specifically detail how the research addresses the definition of personalized medicine:
An integrated evidence-based approach to patient care across the continuum (from health to
disease), using multidisciplinary teams to promote health and wellness, patient education,
empowerment, and satisfaction, and to use the innovative tools to customize disease prevention,
detection, and treatment
3. Address at least one of the above topics
4. Be designed to generate preliminary data as a basis for follow on funding; and state explicitly what
sources of follow on funding will be sought.
Application should be addressed to:
Center for Personalized Medicine Research Committee
c/o Teji Rakhra-Burris
Email: teji.rb@duke.edu
Please reference "CPM RFA#2 in the email subject line
2 2.1.2013
Topic 1: The Use of IT and/or Social Media to Promote Health
Technological advances in areas such as mobile communications have brought handheld and web-based
interaction (through the use of smartphones, via social media, etc) to a majority of people in the US.
Hypothetically, these modes of communication hold potential for the delivery of personalized
medicine/behavioral health interventions, personalized data collection and self/provider monitoring of health
behaviors. Ultimately, these types of interactions may lead to improved health behaviors and clinical
outcomes.
The utility, effectiveness and clinical implementation of these technologies in the area of health behavior
change have not been extensively researched. Therefore, we invite proposals that address this emerging area
of research and healthcare.
Examples of potential areas of interest include:
x Smartphone apps for patient self-monitoring of health behaviors and/or interventions to support behavior
change.
x Web-based patient/health professional communication (e-medicine).
x Development and testing of patient support for healthy behaviors via web or mobile phone.
x Patient educational tools via web or mobile app/phone communication.
x Clinical implementation of web or mobile phone tools for patient and/or provider utilization in providing
personalized medicine.
Topic 2: Personalized Medicine Policy and Implementation Science
Implementation science, or the study of effectiveness, efficiency, and equity of health program selection, delivery,
and uptake in real-world settings, is facilitating the practice of personalized health care in diverse settings,
including primary and specialty clinics, health systems, and community-based programs. However, the adoption
of personalized health care into clinical settings has not been without its challenges. One barrier to wide
implementation of personalized health care has been the dearth of process data, and the policy implications
stemming from these data, which can provide applicable, generalizable support for the translation of knowledge
across practices and systems. f available, such data can provide a 'prescription' to others, including policy
makers for policy development, which supports or allows for personalized health care applications to be used and
feasible across diverse sites.
Therefore, one of the foci of this RFA is health policy and regulatory implications for personalized health care
implementation in clinical or community sites. For purposes of this RFP, policy includes all levels from individual
practice sites to health systems to state/federal. Proposed studies can explore policy issues related to
implementation of personalized health care or generate evidence to inform policy that supports real world
implementation of personalized health care into clinical settings.
Examples include:
x Exploration of provider understanding regarding public policies that would affect implementation of
pharmacogenomic testing (or other personalized health care strategies) in clinical practice.
x Analysis of policies and processes required for effective collection of personalized patient entered data
(i.e., psychosocial/behavioral data) in EMR.
x Studies of patients' or providers' understanding of policies regarding pharmacogenomics and how those
impact its role in health care delivery.
x Studies of consumers' interest in and understanding of whole genome/exome scanning, return of results,
and its potential role in their health and health care.
x Examination or survey of economic or policy barriers to implementation of personalized medicine in a
health system or broader health care arena.
Topic 3: Adoption of Personalized Medicine Concepts and Paradigms in the Clinical Setting.
There are several barriers that stand in the way of widespread adoption of personalized medicine.
First, clinicians are slow to adopt new paradigms for care, in particular those that involve assessing risk or
incorporation of new information that has to be integrated into established practice patterns and decision making.
Adoption is further hindered when the information is unfamiliar, e.g. genetic information.
Second, in a rapidly changing healthcare environment, it is likely that many of the personalized medicine
recommendations will take some time to get into guidelines and therefore supported by practice incentives.
3 2.1.2013
Clinical treatment guidelines, even for the most favorable results (e.g., Heart Protection Study; Merck;
simvastatin), depend on a number-to-treat to benefit ratio of 15:1 and usually in the range of 25:1. This creates
cognitive dissonance between population health versus personalized health practices where therapies targeted to
the individuals most likely to benefit are the goal.
We can learn a lot from our behavioral medicine colleagues about behavior change, as adoption of new practice
methods, tools, or approaches to practice require behavioral change and involve conscious or unconscious
choices by the clinician.
This call for applications seeks to develop more information about how clinical decisions are made in the clinical
environment, and how to overcome barriers to adoption of new paradigms for treatment that support the principles
of personalized medicine.
Proposal should: design experimental systems or survey tools that will permit investigators to explore and
support or disprove hypotheses generated from these concepts.
Examples of proposals responsive to this RFA question might approach these issues by:
x Performing literature searches or meta-analyses of studies that have addressed the issue of adoption of
new medical therapies, barriers, inducements, successes and failures.
x Performing surveys of clinicians that further knowledge of personalized medicine concepts and
paradigms.
x Establishing experimental systems or environments in which experiments can be conducted. These
might include real life or virtual simulations, or real-life practice.
x Conducting experiments to establish new knowledge in these areas.
Topic 4: Personalized Medicine - Education
The promise of personalized medicine will depend in large part on the appropriate use of new clinical applications.
To facilitate appropriate use, new tools and educational resources are needed to promote skills, knowledge, and
awareness for various populations, namely health professionals and patients. The diversity of both patients and
healthcare professionals poses significant challenges to the one-size-fits-all, passive approach toward education
and warrants new strategies to enhance skills and knowledge and highlight the significance of these tools for
improved health outcomes. Likewise, the development and implementation of new educational resources in this
area will often require a collaborative approach to integrate the use of new tests into various clinical practice
settings.
One of the major goals of this RFA is to enhance knowledge and skills of health professionals to facilitate the
implementation of personalized health care in clinical or community sites. Support will be provided to studies that
plan to develop, implement, and assess new educational strategies and tools to enhance health professional skills
and knowledge related to implementation of personalized health care. Proposals that focus solely on the
dissemination of information or conducting seminars are not responsive and will not be considered for further
review.
Examples include:
x "Train-the-trainer educational strategies to increase skills and knowledge of instructors, clinical leaders,
and others to promote skills and knowledge development, enabling integration of personalized medicine
subject matter into current curricula and/or training programs.
x Development of unique, collaborative partnerships to promote skills and knowledge development in
personalized medicine.
x Assessment of health professional knowledge and needs regarding personalized medicine and preferred
types/methods to enhance skills and knowledge of this field.
x Development, implementation, and assessment of point-of-care resources to aid professionals in
decisions regarding use and applications of certain tests utilized in implementation of personalized
medicine.
S-ar putea să vă placă și
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Duke University Department of Medicine Annual Report 2013Document21 paginiDuke University Department of Medicine Annual Report 2013Duke Department of MedicineÎncă nu există evaluări
- Karlawish Poster HMLDocument1 paginăKarlawish Poster HMLDuke Department of MedicineÎncă nu există evaluări
- Dci Survivorship Rfa1 FinalDocument2 paginiDci Survivorship Rfa1 FinalDuke Department of MedicineÎncă nu există evaluări
- 103-2013 State DM Poster FDocument1 pagină103-2013 State DM Poster FDuke Department of MedicineÎncă nu există evaluări
- DIHI Summit FlyerDocument1 paginăDIHI Summit FlyerDuke Department of MedicineÎncă nu există evaluări
- Boyarsky 2013 Flyer FinalDocument1 paginăBoyarsky 2013 Flyer FinalDuke Department of MedicineÎncă nu există evaluări
- Research Collaboration Pilot Projects RFP v03.04.13Document1 paginăResearch Collaboration Pilot Projects RFP v03.04.13Duke Department of MedicineÎncă nu există evaluări
- Mhealth2013 ProgramDocument2 paginiMhealth2013 ProgramDuke Department of MedicineÎncă nu există evaluări
- Boyarsky 2013 FlyerDocument1 paginăBoyarsky 2013 FlyerDuke Department of MedicineÎncă nu există evaluări
- Duke Heart Report 2012Document24 paginiDuke Heart Report 2012Duke Department of MedicineÎncă nu există evaluări
- DukeMed Magazine - Spring 2012Document58 paginiDukeMed Magazine - Spring 2012Duke Department of MedicineÎncă nu există evaluări
- Duke Internal Medicine Residents 2012Document5 paginiDuke Internal Medicine Residents 2012Duke Department of MedicineÎncă nu există evaluări
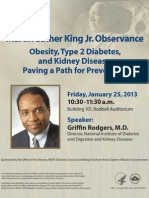
- NIEHS Hosts RodgersDocument1 paginăNIEHS Hosts RodgersDuke Department of MedicineÎncă nu există evaluări
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5795)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Reduction of Perioperative Anxiety Using A Hand-Held Video Game DeviceDocument7 paginiReduction of Perioperative Anxiety Using A Hand-Held Video Game DeviceFiorel Loves EveryoneÎncă nu există evaluări
- Inpatient Management of Adolescents With Eating Disorders ToolkitDocument191 paginiInpatient Management of Adolescents With Eating Disorders ToolkitAjutor Anorexie-BulimieÎncă nu există evaluări
- Pharmacology For Nurses A Pathophysiologic Approach 5th Edition Adams Test Bank 1Document34 paginiPharmacology For Nurses A Pathophysiologic Approach 5th Edition Adams Test Bank 1matthew100% (51)
- BNO72122 - v2 - 161956 Focal Spasticity Workbook - FINAL - PIDocument51 paginiBNO72122 - v2 - 161956 Focal Spasticity Workbook - FINAL - PIAli Radhi MutarÎncă nu există evaluări
- HayalllDocument41 paginiHayalllchalie tarekegnÎncă nu există evaluări
- Niche and Sub-NicheDocument3 paginiNiche and Sub-NichehoneybeeÎncă nu există evaluări
- Reflection PaperDocument7 paginiReflection Paperapi-590313144Încă nu există evaluări
- Carmen Best Background InformationDocument15 paginiCarmen Best Background InformationKING 5 NewsÎncă nu există evaluări
- Medical: MycologyDocument395 paginiMedical: MycologyEl Fatih MunexÎncă nu există evaluări
- Atividade TST TC e Tse Modal Verbs Warning SignsDocument1 paginăAtividade TST TC e Tse Modal Verbs Warning SignsMarcelo RochaÎncă nu există evaluări
- Nervous SystemDocument2 paginiNervous SystemMini Vijay0% (1)
- Evidence Based Medicine Needs A Reality Check - R - 4Document6 paginiEvidence Based Medicine Needs A Reality Check - R - 4Suresh ShottamÎncă nu există evaluări
- ICAM Dog Population ManagementDocument24 paginiICAM Dog Population ManagementJasmina SevicÎncă nu există evaluări
- Case 10 Shutter IslandDocument3 paginiCase 10 Shutter IslandAnkith ReddyÎncă nu există evaluări
- Briearra Kennedy: University of Cincinnati, Cincinnati, OHDocument1 paginăBriearra Kennedy: University of Cincinnati, Cincinnati, OHapi-664515503Încă nu există evaluări
- Borrescio-Higa Valenzuela - Gender Inequality and Mental Health.Document9 paginiBorrescio-Higa Valenzuela - Gender Inequality and Mental Health.Firdaus Silabi Al-AttarÎncă nu există evaluări
- CCO Invasive Fungal Disease Downloadable 1Document25 paginiCCO Invasive Fungal Disease Downloadable 1Vasantha KumarÎncă nu există evaluări
- Health Advert 2023Document14 paginiHealth Advert 2023tutorfelix777Încă nu există evaluări
- HYVC TTC Prospectus 2022 2023Document16 paginiHYVC TTC Prospectus 2022 2023Sreyashi BasuÎncă nu există evaluări
- RN MedSurgDocument685 paginiRN MedSurgArgyll Baye Ansuas100% (4)
- National Geographic March 2016Document148 paginiNational Geographic March 2016Anonymous Azxx3Kp9Încă nu există evaluări
- Paper 2 - Abisha AliDocument7 paginiPaper 2 - Abisha Aliapi-269596566Încă nu există evaluări
- Hussen Worku 2022 Quality of Antenatal Care Service and Factors Associated With Client Satisfaction at Public HealthDocument9 paginiHussen Worku 2022 Quality of Antenatal Care Service and Factors Associated With Client Satisfaction at Public HealthEkung EmmanuelÎncă nu există evaluări
- A2 1021V en Bowen w7Document47 paginiA2 1021V en Bowen w7Gareth GriffithsÎncă nu există evaluări
- All India Institute of Medical Sciences, New Delhi-110 029 (Examination Section)Document1 paginăAll India Institute of Medical Sciences, New Delhi-110 029 (Examination Section)Nitin SinghalÎncă nu există evaluări
- LESSON 1 Occupational Health and Safety Policies and ProceduresDocument11 paginiLESSON 1 Occupational Health and Safety Policies and Procedurescky yarteÎncă nu există evaluări
- Mini Case Study For MR ADocument3 paginiMini Case Study For MR Aapi-300133703Încă nu există evaluări
- Valproate SodiumDocument2 paginiValproate SodiumKhairul KhairulÎncă nu există evaluări
- Sultan Ali Akbar Sinenggayan High School: Program of Activities Activity Target Date Resources Need Expected OutputDocument5 paginiSultan Ali Akbar Sinenggayan High School: Program of Activities Activity Target Date Resources Need Expected OutputRAHIB SAMAYATINÎncă nu există evaluări
- Brach y TherapyDocument3 paginiBrach y Therapydincy danielÎncă nu există evaluări