Documente Academic
Documente Profesional
Documente Cultură
DM NCP
Încărcat de
Caress Mae Gubaton CabudoyDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
DM NCP
Încărcat de
Caress Mae Gubaton CabudoyDrepturi de autor:
Formate disponibile
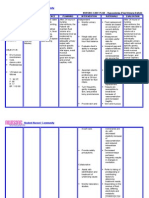
Impaired Physical Mobility Amputation
In general, amputation of limbs is the result of trauma, peripheral vascular disease, tumors, and congenital disorders. This is an amputation nursing care plan for a patient with impaired physical mobility. Nursing Diagnosis Impaired Physical Mobility Related to:
Loss of a limb (particularly a lower extremity); pain/discomfort; perceptual impairment (altered sense of balance) Possibly evidenced by
Reluctance to attempt movement Impaired coordination; decreased muscle strength, control, and mass Desired Outcomes:
Verbalize understanding of individual situation, treatment regimen, and safety measures. Maintain position of function as evidenced by absence of contractures. Demonstrate techniques/behaviors that enable resumption of activities. Display willingness to participate in activities. Nursing Interventions
Nursing Interventions Provide stump care on a routine basis, e.g., inspect area, cleanse and dry thoroughly, and rewrap stump with elastic bandage or air splint, or apply a stump shrinker (heavy stockinette sock), for delayed prosthesis. Measure circumference periodically Rewrap stump immediately with an elastic bandage, elevate if immediate/early cast is
Rationale Provides opportunity to evaluate healing and note complications (unless covered by immediate prosthesis). Wrapping stump controls edema and helps form stump into conical shape to facilitate fitting of prosthesis. Note: Air splint may be preferred, because it permits visual inspection of the wound Measurement is done to estimate shrinkage to ensure proper fit of sock and prosthesis. Edema will occur rapidly, and rehabilitation can be delayed
accidentally dislodged. Prepare for reapplication of cast. Assist with specified ROM exercises for both the affected and unaffected limbs beginning early in postoperative stage. Encourage active/isometric exercises for upper torso and unaffected limbs. Provide trochanter rolls as indicated. Instruct patient to lie in prone position as tolerated at least twice a day with pillow under abdomen and lowerextremity stump. Caution against keeping pillow under lower-extremity stump or allowing BKA limb to hang dependently over side of bed or chair. Demonstrate/assist with transfer techniques and use of mobility aids, e.g., trapeze, crutches, or walker. Assist with ambulation. Prevents contracture deformities, which can develop rapidly and could delay prosthesis usage.
Increases muscle strength to facilitate transfers/ambulation and promote mobility and more normal lifestyle. Prevents external rotation of lower-limb stump Strengthens extensor muscles and prevents flexion contracture of the hip, which can begin to develop within 24 hr of sustained malpositioning. Use of pillows can cause permanent flexion contracture of hip; a dependent position of stump impairs venous return and may increase edema formation. Facilitates self-care and patients independence. Proper transfer techniques prevent shearing abrasions/dermal injury related to scooting. Reduces potential for injury. Ambulation after lower-limb amputation depends on timing of prosthesis placement. Hardens the stump by toughening the skin and altering feedback of resected nerves to facilitate use of prosthesis. Provides for creation of exercise/activity program to meet individual needs and strengths, and identifies mobility functional aids to promote independence. Early use of a
Instruct patient in stumpconditioning exercises Refer to rehabilitation team
temporary prosthesis promotes activity and enhances general well-being/positive outlook. Note: Vocational counseling/retraining also may be indicated. Provide foam/flotation mattress. Reduces pressure on skin/tissues that can impair circulation, potentiating risk of tissueischemia/breakdown
Risk for Infection Amputation
In general, amputation of limbs is the result of trauma, peripheral vascular disease, tumors, and congenital disorders. This is an amputation nursing care plan for a patient with a risk for infection. Nursing Diagnosis Risk for Infection Risk factors may include
Inadequate primary defenses (broken skin, traumatized tissue) Invasive procedures; environmental exposure Chronic disease, altered nutritional status Desired Outcomes
Achieve timely wound healing; be free of purulent drainage or erythema; and be afebrile. Nursing Interventions & Rationale
Nursing Interventions Maintain aseptic technique when changing dressings/caring for wound. Inspect dressings and wound; note characteristics of drainage. bacteria.
Rationale Minimizes opportunity for introduction of
Early detection of developing infection provides opportunity for timely intervention and prevention of
more serious complications. Maintain patency and routinely empty drainage device. Hemovac, Jackson-Pratt drains facilitate removal of drainage, promoting wound healing and reducing risk of infection. Cover dressing with plastic when using the bedpan or if incontinent. Expose stump to air; wash with mild soap and water after dressings are discontinued. Monitor vital signs. Maintains cleanliness, minimizes skin contaminants, and promotes healing of tender/fragile skin. Temperature elevation/tachycardia may reflect developing sepsis. Obtain wound/drainage cultures and sensitivities as appropriate. Administer antibiotics as indicated. Identifies presence of infection/specific organisms and appropriate therapy. Wide-spectrum antibiotics may be used prophylactically, or antibiotic therapy may be geared toward specific organisms. Prevents contamination in lower-limb amputation.
Risk for Ineffective Tissue Perfusion Amputation
In general, amputation of limbs is the result of trauma, peripheral vascular disease, tumors, and congenital disorders. This is an amputation nursing care plan for a patient with a risk for ineffective tissue perfusion. Nursing Diagnosis:
Tissue Perfusion, risk for ineffective: peripheral Risk factors:
Reduced arterial/venous blood flow; tissue edema, hematoma formation Hypovolemia Desired Outcomes:
Patient will Maintain adequate tissue perfusion as evidenced by palpable peripheral pulses, warm/dry skin, and timely wound healing. Nursing Interventions & Rationale
Nursing Interventions Monitor vital signs. Palpate peripheral pulses, noting strength and equality. Perform periodic neurovascular assessments (sensation, movement, pulse, skin color, and temperature). Inspect dressings/drainage device, noting amount and characteristics of drainage. Apply direct pressure to bleeding site if hemorrhage occurs. Contact physician immediately. Investigate reports of persistent/unusual pain in operative site. Evaluate nonoperated lower limb for inflammation, positive Homans sign. Encourage/assist with early ambulation. Administer IV fluids/blood products as indicated.
Rationale General indicators of circulatory status and adequacy of perfusion. Postoperative tissue edema, hematoma formation, or restrictive dressings may impair circulation to stump, resulting in tissue necrosis. Continued blood loss may indicate need for additional fluid replacement and evaluation for coagulation defect or surgical intervention to ligate bleeder. Direct pressure to bleeding site may be followed by application of a bulk dressing secured with an elastic wrap once bleeding is controlled. Hematoma can form in muscle pocket under the flap, compromising circulation and intensifying pain Increased incidence of thrombus formation in patients with preexisting peripheral vascular disease/diabetic changes. Enhances circulation, helps prevent stasis and associated complications. Promotes sense of general well-being. Maintains circulating volume to maximize tissue perfusion.
Apply antiembolic/sequential compression hose to nonoperated leg, as indicated. Administer low-dose anticoagulant as indicated. Monitor laboratory studies, e.g.: Hb/Hct; PT/activated partial thromboplastin time (aPTT).
Enhances venous return, reducing venous pooling and risk of thrombophlebitis. May be useful in preventing thrombus formation without increasing risk of postoperative bleeding/hematoma formation. Indicators of hypovolemia/dehydration that can impair tissue perfusion.
Evaluates need for/effectiveness of anticoagulant therapy and identifies developing complication, e.g., posttraumatic disseminated intravascular coagulation (DIC)
Situational Low Self-Esteem Amputation
Nursing Diagnosis Self-Esteem, situational low May be related to
Loss of body part/change in functional abilities Possibly evidenced by
Anticipated changes in lifestyle; fear of rejection/reaction by others Negative feelings about body, focus on past strength, function, or appearance Feelings of helplessness, powerlessness Preoccupation with missing body part, not looking at or touching stump Perceived change in usual patterns of responsibility/physical capacity to resume role Desired Outcomes
Begin to show adaptation and verbalize acceptance of self in situation (amputee).
Recognize and incorporate changes into self-concept in accurate manner without negating self-esteem. Develop realistic plans for adapting to new role/role modifications. Nursing Interventions & Rationale
Nursing Interventions Assess/consider patients preparation for and view of amputation.
Rationale Research shows that amputation poses serious threats to patients psychological and psychosocial adjustment.Patient who views amputation as life-saving or reconstructive may be able to accept the new self more quickly.Patient with sudden traumatic amputation or who considers amputation to be the result of failure in other treatments is at greater risk for selfconcept disturbances. Venting emotions helps patient begin to deal with the fact and reality of life without a limb. Provides opportunity for patient to question and assimilate information and begin to deal with changes in body image and function, which can facilitate postoperative recovery.
Encourage expression of fears, negative feelings, and grief over loss of body part. Reinforce preoperative information including type/location of amputation, type of prosthetic fitting if appropriate (i.e., immediate, delayed), expected postoperative course, including pain control and rehabilitation. Assess degree of support available to patient. Ascertain individual strengths and identify previous positive coping behaviors. Encourage participation in ADLs. Provide opportunities to view/care for stump, using the moment to point out positive signs of healing.
Sufficient support by SO and friends can facilitate rehabilitation process. Helpful to build on strengths that are already available for patient to use in coping with current situation. Promotes independence and enhances feelings of selfworth. Although integration of stump into body image can take months or even years, looking at the stump and hearing positive comments (made in a normal, matter-offact manner) can help
patient with this acceptance. Encourage/provide for visit by another amputee, especially one who is successfully rehabilitating. Note withdrawn behavior, negative self-talk, use of denial, or overconcern with actual/perceived changes. Provide open environment for patient to discuss concerns about sexuality. Discuss availability of various resources, e.g., psychiatric/ sexual counseling, occupational therapist. A peer who has been through a similar experience serves as a role model and can provide validity to comments and hope for recovery and a normal future. Identifies stage of grief/need for interventions.
Promotes sharing of beliefs/values about sensitive subject, and identifies misconceptions/myths that may interfere with adjustment to situation. May need assistance for these concerns to facilitate optimal adaptation and rehabilitation.
S-ar putea să vă placă și
- Diagnostic TestDocument57 paginiDiagnostic TestPam ArauneÎncă nu există evaluări
- Risk For Impaired Skin IntegrityDocument2 paginiRisk For Impaired Skin IntegrityKarl JoseÎncă nu există evaluări
- Impaired Physical Mobility NCPDocument3 paginiImpaired Physical Mobility NCPYan ReyesÎncă nu există evaluări
- Glaucoma NCPDocument4 paginiGlaucoma NCPChantal CaraganÎncă nu există evaluări
- Burns - Tissue Perfusion, IneffectiveDocument3 paginiBurns - Tissue Perfusion, Ineffectivemakyofrancis20100% (1)
- Diarrhea Care PlanDocument2 paginiDiarrhea Care Planzepoli_zepoly6232100% (1)
- NCP PpwardDocument15 paginiNCP PpwardKarl Vincent Soso100% (1)
- NCP - Acute PainDocument2 paginiNCP - Acute PainsAm_300% (1)
- Mpaired Physical Mobility (Amputation) : Nursing Care PlanDocument3 paginiMpaired Physical Mobility (Amputation) : Nursing Care PlanTheSweetpea5010% (2)
- Acute Pain NCPDocument1 paginăAcute Pain NCPJed AvesÎncă nu există evaluări
- NCP Acute PainDocument3 paginiNCP Acute PainSheene Lysethea Sioteco AguilosÎncă nu există evaluări
- Burns - Airway Clearance, Risk For IneffectiveDocument2 paginiBurns - Airway Clearance, Risk For Ineffectivemakyofrancis20Încă nu există evaluări
- Activity IntoleranceDocument2 paginiActivity IntoleranceMaze Reyes40% (5)
- NCP OrthoDocument1 paginăNCP Orthoroger0% (1)
- NCP For Surgical CasesDocument10 paginiNCP For Surgical Caseslouie roderosÎncă nu există evaluări
- Gi-Rle - NCP For Deficient Fluid VolumeDocument2 paginiGi-Rle - NCP For Deficient Fluid VolumeEvangeline Villa de Gracia100% (1)
- R.O. Appendicitis.: Nursing Care Plan (NCP)Document2 paginiR.O. Appendicitis.: Nursing Care Plan (NCP)Karen Joy ItoÎncă nu există evaluări
- NCP PainDocument2 paginiNCP PainJun TangonanÎncă nu există evaluări
- Eamc Problem PrioritizationDocument3 paginiEamc Problem PrioritizationAnnaMae Paula Fababier NaguitÎncă nu există evaluări
- NCP For Impaired Skin IntegrityDocument3 paginiNCP For Impaired Skin IntegrityAemz Alacasnap Ainegud100% (1)
- SJMC - xi-nCP&HTP - Impaired Skin IntegrityDocument10 paginiSJMC - xi-nCP&HTP - Impaired Skin IntegrityJoy CompetenteÎncă nu există evaluări
- NCP Impaired Skintissue IntegrityDocument5 paginiNCP Impaired Skintissue IntegrityArt Christian RamosÎncă nu există evaluări
- Ineffective Tissue PerfusionDocument2 paginiIneffective Tissue PerfusionDiane ReyÎncă nu există evaluări
- Nursing Care Plans For AppendicitisDocument2 paginiNursing Care Plans For AppendicitisRodnie Insauriga GonzalesÎncă nu există evaluări
- NCP Acute PainDocument3 paginiNCP Acute PainAlex MarieÎncă nu există evaluări
- NCP HyperthermiaDocument6 paginiNCP HyperthermiaGrax DeeÎncă nu există evaluări
- Case Study Ugib Lower MBDocument65 paginiCase Study Ugib Lower MBQuolette Constante100% (1)
- Cu 5Document2 paginiCu 5Clareze AbadÎncă nu există evaluări
- Compartment Syndrome NCP (PAIN)Document2 paginiCompartment Syndrome NCP (PAIN)eunica16Încă nu există evaluări
- NCP For CHF 3 Activity IntoleranceDocument2 paginiNCP For CHF 3 Activity IntoleranceAngelyn ArdinesÎncă nu există evaluări
- NCP AlteredDocument3 paginiNCP AlteredShaira TillahÎncă nu există evaluări
- Impaired Physical Mobility...Document3 paginiImpaired Physical Mobility...Christy BerryÎncă nu există evaluări
- Fluid Volume DeficitDocument3 paginiFluid Volume Deficitprickybiik100% (1)
- Activity IntoleranceDocument3 paginiActivity Intolerancelouie roderos0% (1)
- NCP - Risk Impaired Skin RT Altered Circulation (Spinal Injury)Document2 paginiNCP - Risk Impaired Skin RT Altered Circulation (Spinal Injury)yanny0350% (2)
- Identified Nursing Diagnoses and PrioritizationDocument4 paginiIdentified Nursing Diagnoses and Prioritizationrheinz-marlon-m-carlos-7771Încă nu există evaluări
- Cues Nursing Diagnosis Scientific Reason Objective Nursing Intervention Rationale EvaluationDocument4 paginiCues Nursing Diagnosis Scientific Reason Objective Nursing Intervention Rationale Evaluationjomsportg0% (1)
- NCP and Drug Study For Case in SleDocument34 paginiNCP and Drug Study For Case in SlePaolo Vittorio Perdigueros GonzalesÎncă nu există evaluări
- NCP (Or) ThyroidectomyDocument3 paginiNCP (Or) ThyroidectomyChiz CorreÎncă nu există evaluări
- NCP HemothoraxDocument3 paginiNCP HemothoraxMichael John F. NatividadÎncă nu există evaluări
- NCP Risk For Infection IntraopDocument3 paginiNCP Risk For Infection IntraopAngelica Mae ArenzanaÎncă nu există evaluări
- NCP Impaired Physical MobilityDocument1 paginăNCP Impaired Physical MobilityCharmaine SolimanÎncă nu există evaluări
- NCP For CTTDocument1 paginăNCP For CTTJen Rhae LimÎncă nu există evaluări
- NCPDocument4 paginiNCPDaniel Garraton0% (1)
- NCP Activity Intolerance Related To Decreased in Oxygen SupplyDocument3 paginiNCP Activity Intolerance Related To Decreased in Oxygen SupplyKyle Stephen TancioÎncă nu există evaluări
- Deficit)Document2 paginiDeficit)Lee DeeÎncă nu există evaluări
- Discharge PlanDocument2 paginiDischarge PlanJen Recto PaladÎncă nu există evaluări
- Aaa Gastrectomy NCP FinalDocument13 paginiAaa Gastrectomy NCP Finallexzaf100% (1)
- NCPDocument6 paginiNCPyupipsjamÎncă nu există evaluări
- NCP (Riskforimpairedskinintegrity)Document3 paginiNCP (Riskforimpairedskinintegrity)Ma Kaye Gelizabeth Corpuz-DauloÎncă nu există evaluări
- NCP Liver CirrhosisDocument5 paginiNCP Liver CirrhosisEsther O. CorreaÎncă nu există evaluări
- NCP and Fdar Wk2 Sarscov-19Document4 paginiNCP and Fdar Wk2 Sarscov-19Jamaica Malicdem0% (1)
- NCP For HHSDocument1 paginăNCP For HHSLizzuly Galindo100% (1)
- NCP For Aspiration PnuemoniaDocument11 paginiNCP For Aspiration PnuemoniaChristy Rose AgrisÎncă nu există evaluări
- NCPDocument3 paginiNCPJezza RequilmeÎncă nu există evaluări
- Amputation: Impaired Physical MobilityDocument5 paginiAmputation: Impaired Physical MobilityAhmad EfendiÎncă nu există evaluări
- Nursing Diagnosis May Be Related To Possibly Evidenced byDocument37 paginiNursing Diagnosis May Be Related To Possibly Evidenced byLea TanÎncă nu există evaluări
- Nursing Diagnosis Related ToDocument9 paginiNursing Diagnosis Related ToGrape JuiceÎncă nu există evaluări
- Nursing Care PlansDocument22 paginiNursing Care PlansAnonymous 0C4OZmR0% (1)
- 8 Sample Care Plans For ACDFDocument11 pagini8 Sample Care Plans For ACDFacasulla98Încă nu există evaluări
- Presider: Jessa Tocaldo PresentDocument4 paginiPresider: Jessa Tocaldo PresentCaress Mae Gubaton CabudoyÎncă nu există evaluări
- Presider: Jessa Tocaldo PresentDocument5 paginiPresider: Jessa Tocaldo PresentCaress Mae Gubaton CabudoyÎncă nu există evaluări
- Presider: Jessa Tocaldo Present:: TH TH TH THDocument5 paginiPresider: Jessa Tocaldo Present:: TH TH TH THCaress Mae Gubaton CabudoyÎncă nu există evaluări
- Remotivational TherapyDocument10 paginiRemotivational TherapyCaress Mae Gubaton Cabudoy100% (2)
- Seat PlanDocument4 paginiSeat PlanCaress Mae Gubaton CabudoyÎncă nu există evaluări
- NURSING CARE PLAN Problem: Body Malaise Nursing Diagnosis: Activity IntoleranceDocument2 paginiNURSING CARE PLAN Problem: Body Malaise Nursing Diagnosis: Activity IntoleranceLaGlaGan Group60% (5)
- Ch50 NCP IneffAirClear 1395-1396Document2 paginiCh50 NCP IneffAirClear 1395-1396Caress Mae Gubaton CabudoyÎncă nu există evaluări
- Dance TherapyDocument13 paginiDance TherapyCaress Mae Gubaton Cabudoy100% (2)
- Medical Marijuana TincturesDocument15 paginiMedical Marijuana TincturesCaress Mae Gubaton CabudoyÎncă nu există evaluări
- International Journal of Diabetes MellitusDocument3 paginiInternational Journal of Diabetes MellitusCaress Mae Gubaton CabudoyÎncă nu există evaluări
- English 27 - NeDocument2 paginiEnglish 27 - NeCaress Mae Gubaton CabudoyÎncă nu există evaluări
- Vehicular Accidents Top Cause of InjuriesDocument1 paginăVehicular Accidents Top Cause of InjuriesCaress Mae Gubaton CabudoyÎncă nu există evaluări
- Product English 6Document16 paginiProduct English 6rpepÎncă nu există evaluări
- Rose Pharmacy JaipurDocument6 paginiRose Pharmacy JaipurAmit KochharÎncă nu există evaluări
- Journal Reading Radiologi EllaDocument44 paginiJournal Reading Radiologi EllaElla Putri SaptariÎncă nu există evaluări
- Parts of The Body and Health ProblemDocument13 paginiParts of The Body and Health ProblemSonia Tri AgustinaÎncă nu există evaluări
- Biology SPMDocument17 paginiBiology SPMbloptra18Încă nu există evaluări
- TRMDLDocument5 paginiTRMDLrizkaÎncă nu există evaluări
- Disclosure and Attestation Form - SPEAKERDocument1 paginăDisclosure and Attestation Form - SPEAKERwethreeÎncă nu există evaluări
- Documentary Requirements and Format of Simplified CSHPDocument1 paginăDocumentary Requirements and Format of Simplified CSHPRhalf AbneÎncă nu există evaluări
- Galvus (Vildagliptin) : How Does It Work?Document5 paginiGalvus (Vildagliptin) : How Does It Work?Radhakrishna KurupÎncă nu există evaluări
- ClubbingDocument4 paginiClubbingAlfrin AntonyÎncă nu există evaluări
- © 2019. All Rights Reserved. 1Document20 pagini© 2019. All Rights Reserved. 1Julianne Bsc100% (2)
- Aceclofenac Vs Diclofenac On Hexosamine LevelsDocument11 paginiAceclofenac Vs Diclofenac On Hexosamine LevelsMartin MoranÎncă nu există evaluări
- Neurology Case SheetDocument9 paginiNeurology Case SheetAshwaq TpÎncă nu există evaluări
- Drug Therapy For PicuDocument32 paginiDrug Therapy For PicuNeethu Mariya MathewÎncă nu există evaluări
- Hidradenitis Suppurativa - Treatment - UpToDate PDFDocument24 paginiHidradenitis Suppurativa - Treatment - UpToDate PDFjandroÎncă nu există evaluări
- Gordon'S Health Pattern: Submitted To: Marjorie L. Apao, RNDocument6 paginiGordon'S Health Pattern: Submitted To: Marjorie L. Apao, RNEnrique LuÎncă nu există evaluări
- 24 Stem Cell Therapy in Neurological Disorders 4th EditionDocument362 pagini24 Stem Cell Therapy in Neurological Disorders 4th EditionIbraaheem RafeeuÎncă nu există evaluări
- AIDS in The Workplace LawDocument30 paginiAIDS in The Workplace LawPacific SpectrumÎncă nu există evaluări
- PlacentaDocument21 paginiPlacentaAttiqaQureshiÎncă nu există evaluări
- FP TrainedProviders 2Document9 paginiFP TrainedProviders 2Bharma LogisticsÎncă nu există evaluări
- Kriya Yoga Lessons - 1and 2 - Initiation.Document4 paginiKriya Yoga Lessons - 1and 2 - Initiation.broxie93% (15)
- Kegawatan Pada Diare Dehidrasi BeratDocument40 paginiKegawatan Pada Diare Dehidrasi BeratAkram BatjoÎncă nu există evaluări
- Biochemistry Reagents - ITA Kits - Promotional Tool 27th - August-2019-2Document23 paginiBiochemistry Reagents - ITA Kits - Promotional Tool 27th - August-2019-2Ajay DataniyaÎncă nu există evaluări
- Anaesthesia For Medical Students-Review QuestionsDocument20 paginiAnaesthesia For Medical Students-Review QuestionsJohnny Lee100% (6)
- Antimicrobial Properties of Allicin From GarlicDocument3 paginiAntimicrobial Properties of Allicin From GarlicEdward Kenneth DragasÎncă nu există evaluări
- UNIVERSITY OF DELHI - Student Hand BookDocument75 paginiUNIVERSITY OF DELHI - Student Hand Bookvfxindia100% (1)
- 1999 CQfirstphaseallotments PDFDocument73 pagini1999 CQfirstphaseallotments PDFISMAIL KHANÎncă nu există evaluări
- Exam 1Document13 paginiExam 1Ashley NhanÎncă nu există evaluări
- 861 Drug Prescribing For Dentistry 2 Web 2 Email PDFDocument94 pagini861 Drug Prescribing For Dentistry 2 Web 2 Email PDFRaphaela TravassosÎncă nu există evaluări
- Stroke (Cerebrovascular Accident) : 1. QXCI Treatment PossibilitiesDocument5 paginiStroke (Cerebrovascular Accident) : 1. QXCI Treatment PossibilitiesEnrique Gonzalez Marquier100% (1)