Documente Academic
Documente Profesional
Documente Cultură
Palliative Treatment in Nasopharyngeal Carcinoma
Încărcat de
Muhamad Amar'sTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Palliative Treatment in Nasopharyngeal Carcinoma
Încărcat de
Muhamad Amar'sDrepturi de autor:
Formate disponibile
Cita Herawati Murjantyo ENT DEPT DHARMAIS CANCER CENTRE HOSPITAL
INTRODUCTION : INDONESIA : NPC ENT 1st ALL OF CANCER IVth EARLY STAGE DIFFICULT !! - NO SPESIFIC SYMPTOM - PHYSICAL EXT. NOT VISIBLE
NASOPHARYNX : THE TRANSITIONAL ZONE BETWEEN NASAL CAVITY & OROPHARYNX : ANATOMICAL BLIND SPOT
4 5 2 1 5 5 3 1. LUMEN / NASOPHARYNX CHAMBER 2. RETROPHRYNX 3. PARAPHARYNX 4. INTRACRANICAL 5. PARANASAL SINUS 6. DISTANT METASTATIC
MONGOLOID RACE : SOUTHERN CHINESE, HONGKONG, VIETNAMESE, THAIS, MALAYS, INDONE SIANS.
INDONESIA :
RSCM RSHS UJUNG PANDANG PALEMBANG DENPASAR PADANG DHARMAIS HOSPITAL 100 NEW CASES / YEAR 60 25 25 15 11 70
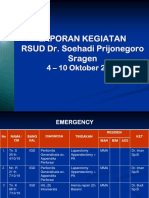
No. 1 DIAGNOSA BREAST ICD-X C501 C509 JUMLAH 1661 2 3 CERVIX BRONCHUS & LUNG C530 C539 C340 C349 708 390 4 5 6 7 8 PHARYNX COLORECTUM LYMPH NODES LEUKIMIA OVARY C100 C148 C180 C209 C770 C779 C420 C424 C569 380 353 320 270 223 9 10 THYROID GLAND HEPAR C739 C220 C221 183 170 Sumber : Instalasi Rekam Medis & Admission RSKD
10 BESAR KANKER TERSERING RS KANKER DHARMAIS RAWAT JALAN (KASUS BARU) TAHUN 2005 - 2007
No. 1 DIAGNOSA BREAST ICD-X C501 C509 JUMLAH 227 2 3 PHARYNX COLORECTUM C100 C148 C180 C209 264 203 4 5 6 7 8 LYMPH NODES LEUKIMIA HEPAR ORAL CAVITY PROSTATE GLAND C770 C779 C420 C424 C220 C221 C000 C609 C619 191 151 126 78 60 9 10 SKIN SOFT TISSUE C440 C449 C490 C499 58 55 Sumber : Instalasi Rekam Medis & Admission RSKD
10 BESAR KANKER TERSERING RS KANKER DHARMAIS RAWAT JALAN (KASUS BARU) MALE TAHUN 2005 - 2007
Etiology Epstein-Barr Virus (EBV) - 100% association with NPC - Elevated high titer of EBV-EA, VCA for early diagn osis Enviromental factors - Salted fish, nitrosamine, N-nitrosodimethyamine - Herbal medicines: promoter a nd initiator in plants Genetic factors - Somatic changes: activation of oncogenes and inactivation of tumor suppressor genes - Heritable genetic changes: Susceptibility genes in high risk family (fam ilial aggregation and immigration)
Agent/Factors Epstein-Barr virus Implication Raised antibody Viral genome in tumor cells Cigarette smoking Chinese herbal med icine EBV activating properties/co-factors Salted fish Preserved vegetables, fer mented food stuff Nitrosamines & nitro-precursors Tunisian preserved spice meat and stewing base Chemical-Tobacco Drugs Plant Products Diet
Agent/Factors Cooking Habits Religious Practice Occupation Implication Household smoke and fumes Incense and joss stick smoke Industrial fumes and chemicals Metal smelting Forma ldehyde Wood dust
1. EPISTAXIS & NASORESPIRATORY SYMPTOMS - BLOOD STAINED, NASAL MUCUS & SALIVA(PO ST NASAL DRIP) - EPISTAXIS / NOSE BLEEDING - NOSE BLOCKAGE 2. TINITUS & AURAL SY MPTOMS - OTITIS MEDIA WITH EFFUSION - TINNITUS - OTALGIA - DISCOMFORT EAR
3. NEUROLOGICAL PALSIES - DOUBLE VISION (+ + +) N III, IV, VI, V (LACERUM FORM.) - TRIGEMINAL NEURALGIA - VOICE & SWALLOWING CAN BE AFFECTED (N. IX, X, XI, XII, JUGULARE FORM) 4. CERVICAL LYMPHADENOPATHY - EARLY LYMPHATIC SPREAD
EARLY DIAGNOSIS : IMPORTANT !! EARLY SYMPTOMS : BLOOD STAINED MUCUS EUSTC.TUBE BLOCKAGE COLDS/ SINUSITIS OTHER SYMPTOMS MAY BE : A LUMP IN THE NECK NOSEBLEEDS MUFFLED HEARING RINGING IN THE EAR HEADACHE DOUBLE VISION
Number of patients
Symptoms / Sign Others Epistaxis Neck Mass 9 27 9 Neck Mass + Epistaxis + Ear Disorder 6 18 Neck Mass + Ear Fullness / Tinitus Others = Diplopi / Cephalgi Neck Mass + Epistaxis 4
NASOPHARYNX
POST OR RHINOSCOPY POST OR RHINOSCOPY + CATHETER NASOENDOSCOPY/NASOPHARYNGOSCOPY
LOCAL ANESTHETIA
GENERAL ANESTHETIC (SPESIFIC CIRCUMTANCES)
THE GOLD STANDART WHO : Type I Type II Type III - Squamous cell carcinoma - Non keratinizing carcinoma - Undifferentiated carcin oma
CT Scan (MRI) USG distant metast Bone scans distant metast EBV serology
IgA anti VCA (viral carsid antigen) IgA anti EA (early antigen) IgA anti EBNA (nucle ar antigen) Serological screening in endemic region Conjunction with nasoendosco py & radiological evaluation
NPC Diagram Pretreatment staging 1. Nasoparyngeal tumor biopsy 2. Chest radiograph 3. Plane radiograph of skull and nasopharynx 4. CT scan of nasopharynx 5. Fibreoptic endo scopic examination 6. Clinical assesment for level and size of cervical lymph no dal metastases (if any) 7. Liver ultrasound 8. Bone 99m Tc-scintigram 9. Fine ne edle aspiration of doubtful cervical lymph nodes Bulky cervical N1-N3 ( 4 cm in maximal diameter) Non-bulky cervical nodes N1N3 (< 4 cm in maximal diameter) Neoadjuvant chemotherap y Pretreatmen t bulky parapharyng eal disease (T2p and T 3p) Local residual disease for T1 or T2n No distans metastasi s (M0) Parapharyngeal boost ERT* ICT Negative cervical nodes N0 Distant metastasis (M1) Palliative treatment
Stg I T1 N0 M0 T2 N0 M0 External Rad. Brachyterapy 6000cgy(30x) + 4-6 x 300cgy Radiosentisizer - Cisplat in 20-25 - Giemsar 200 Stg IIB Stg III T3 N0 M0 T1 N1 M0 Chemorad Rad.ext 6000 BrachyTx 4-6x300 Cisplatin 40mg/m2/mgg Docetaxel 25mg/m2/mgg Paclit axel 90mg/m2/mgg
Stg IV T4 N0 M0 Chemorad Rad.ext 6600 - 7000 Cisplatin 40mg/m2/mgg Docetaxel 25mg/m2/mgg Paclitaxel 90mg/ m2/mgg Stg IV T1-3 N3 M0 T4 N3 M0 NeoAdjuvan Cisplatin 40mg/m2/mgg Taxotere 20-25mg/m2/mgg 5 FU 1000mg/m2/mgg every 3 weeks continue : Chemorad 4 cycles External Rad. + BrachyTx -Cisplatin 40mg/m2/mgg -5FU oral 100mg 1-2hour before
Stg IV T1-4 N3 M1 Full dose Response Response Cisplatin + 5FU 3 sesi Response continue until 6 cycles Response 2nd line :
2nd line chemotx Carboplatin Taxan (docetaxel 75mg/m2/3mmg Paclituxel 175.200mg/ m2/3mmg)
Salvation Surgery
Reccurant local
Hemimaxilectomy swing Mid facial degloving Transpalatal app Regional lymphnodes : Neck dissection
DISTANT METASTASIS FAILED OF CURED TO RELIEVE SYMPTOMS & IMPROVE QUALITY OF LIFE LONGER & LIVE COMFORTABLY NOT JUST MEAN PAINKILLERS & ANTI SICKNESS DRUGS TO LIVE
CHEMOTHERAPY RADIOTHERAPY SURGICAL CAN ALL BE USED
BENEFIT OF CHEMOTHERAPY
LOCOREGIONAL TUMOUR CONTROL CONTROL OF PAIN RESTORATION OF SWALLOWING & APPETITE IMPROVEMENT OF WEIGHT LOSS & FATIGUE INCREASED DISEASE FREE SURVIVAL
PALLIATIVE RADIOTHERAPY USEFUL FOR METASTASES IN BONE,BRAIN & SKIN RELIEVING BLEEDING AUSEDTHE BULK OF TUMOR RELIEVING PRESSURE SYMPTOM SUCH AS PAIN OR OBSTRUCTION C
SURGERY
FOR PALLIATION : DEBULKING : LESION MUST BE RESECTABLE MUST BE RECONSTRUCTIVE TO FUNCTION LEVEL PATIENT MUST BE AGREE, FULL INFORMATION
LOSS OF FUNCTION POTENTIAL MUTILATION/ COMPLICATION
CONTROL
PAIN
OF HEMORRHAGE CONTROL : INFRA TEMPORAL FOSSA : MANDIBULAR NEURALGIA, TRISMUS, TEMPORAL PAIN N DISTRIBUTION OF N.X & XI NEURALGIAS I
NUTRITIONAL
PROBLEM :
DIFFICULTY IN MASTICATION : PAIN, DRY MOUTH, XEROSTOMIA POOR ORAL HYGIENE PROGRE SSIVE LOCAL DISEASE CHRONIC NAUSEA CHANGES IN TASTE ASPIRATION
DYSPNEA :
UPPER AIRWAY OBSTRUCTION: HUMIDIFIED AIR TO REDUCE STICKY TRACHEOSTOMY SUPERIOR VENA CAVA OBSTRUCTION : RADIOTHERAPY LUNG METASTASE : SYMPTOMATIC TREATMENT PULM ONARY EMBOLI BRONCHOPNEUMONI
TX
T0
T1
T2a
T2b
T3
T4 Primary tumor unable to be assessed No primary tumor detected Confined to nasoph arynx Tumor extend to nasal cavity, oropharynx Tumor extend to parapharyngeal sp ace Tumor involves sinuses, orbit, skull base, hypopharynx or bony erosion Intra cranial involvement, cranial nerve palsy
N0 N2 N3
N1
M0
M1
Stage
Stage
Stage
Stage
No nodal involvement Nodes confined to ipsilateral neck, not greater than 3cm Ip silateral node greater than 3cm but not greater than 6cm, bilateral nodes or con tra lateral nodes Ipsilateral node greater than 6cm, supraclavicular nodes No di stant metastasis Distant metastasis (includes mediastinal nodes) I T1 N0 M0 II T 2 N0 M0, T1 N1 M0, T2 N0M0 III T3 N0 M0, T3 N1 M0, T1 N2 M0, T2 N2 M0 IV T4 N0 M 0, any T N3 M0,any T any N M1
No. 1 DIAGNOSA BREAST ICD-X C501 C509 JUMLAH 1637 2 3 CERVIX UTERI OVARY C530 C539 C569 700 221 4 5 6 7 8 COLORECTUM THYROID GLAND LYMPH NODES LEUKIMIA PHARYNX C180 C209 C739 C770 C779 C420 C424 C100 C148 147 138 127 119 114 9 10 BRONCHUS & LUNG CORPUS UTERI C340 C349 C540 C549 112 100 Sumber : Instalasi Rekam Medis & Admission RSKD
10 BESAR KANKER TERSERING RUMAH SAKIT DHARMAIS RAWAT JALAN (KASUS BARU) FEMALE TAH UN 2005 - 2007
History and Examination Obvious Tumour Clinically Suspicious Radiologicall y Suspicious Unexplaine Persi stentl y Raised d SOM IgA Biopsy NP (GA) Suspicious Neck Node Normal looking NP Clinicaly not Suspicious Biopsy NP (LA) Other Diagnosis NPC Proven Diagnosis Uncertain FNA Cytology Squamous Cell or Undifferentiared Carcinoma Other Diagnosis Treatment Treatment Repeat Biopsy (LA/GA ) Other Tretment Biopsy NP (GA) +/- Other Treatment Panendoscopy SOM = Serous otitis media LA = Local anaesthesia GA = General anaesthesia NP = Nasopharynx FNA = Fine-needle aspiration
Tabel. 3 Stage NPC Stage classification Hos (1978) T1 NP Only T2 T2n Nasal fossa T20 Oropharynx T2p Parapharyngeal region T3 T3a Bo ne involvement below the base of the skull including floor of the sphenoid sinus T3b Base of the skull T3c Cranial nerve(s) palsy T3d Orbits, larygopharynx (hyp opharynx) or infratemporal fossa N0 No nodes N1 Node(s) above skin crease at lar yngeal cartilage N2 Node(s) below skin crease but above supraclavicular fossa N3 Supraclavicular node(s) N0 Nb distant metastase M1 Distant metastaces Huangs (1985) T Ts Primary soft tissue tumour only Tb basal skull destruction evident on radio graphs Tn cranical nerve involvement Tc direct invasion to the adjecent brain ev ident on CT scan (newly added item) T-Stage N-Stage N Cervival lymph node N0 No palpable node N1 Unilateral (ipsilateral) small lymp h nodes with total diameter 5cm N2 Bilateral (contralateral) large lymph nodes w ith total diameter > 5cm M Distant metastasis evident clinically M M0 No distant metastasis M1 Clinically evident distant metastasis beyond cervical lymph node involvement M-Stage Stage Grouping I TIN0 II T2 and/or N1 III T3 and/or N2 IV N3 (any T) V M1 I TsN0M0 (prymary soft tissue only) II TsN1M0 or TbN0-1M0 (any condition with N1 and /or Tb) III TsN2M0 or TbN2M0 or TnN0-2M0 or TcN0-2M0 or TcN0-2M0 or TbnN0-2 M0 or TbcN0-2M0 or TbncN0-2M0 (any condition involving N2 or Tn or TC or more co mbinations) IV M1 (any of the above conditions with distant metastasis evident c linically)
Tabel. 3 Stage NPC Stage classification Changsha (1983) T0 Subclinical T1 One wall or corner betwen 2 walls T2 2 walls T3 Nasal fossa, o ropharynx (including parapharyngeal region) T4 2 features of T3 UICC (1987) T1 One wall NP T2 2 walls NP T3 Nasal cavity, oropharynx (including parapharynge al region) T4 Skull base and /or cranial nerve T-Stage N-Stage N0 No nodes N1 Mobile and /or < 3 cm above supraclavicular fossa N2 Fixed and/or (3-8) cm and above supraclavicular fossa N3 Supraclavicular and /or > 8cm N0 No metastase M1 Distant metastaces N0 No node N1 Single homolateral node 3cm N2 N2a single homolateral node > 3 - 6 cm N2c bilateral or contralateral nodes 6cm N3 > 6cm node(s) N0 No metastase M1 Distant metastaces M-Stage Stage Grouping I TIN0 II T2N0; T0-2N1 III T3N0-1; T0-3N2 IV T4N0-2; T0-4N3; M1 I TIN0 II T2N0 III T3N0; T1-3N1 IV T4N0-1 N2-3 (any T); M1 (any T, any N)
Alur Diagnosis Anamnesis : 1. GEJALA HIDUNG : a. Ingus campur darah (sedikit) / epistaksis ringan unilatera l b. Sumbatan hidung unilateral bilateral c. Post nasal drip 2. GEJALA TELINGA : a . Rasa penuh/gangguan pendengaran unilateral menetap b. Tinitus unilateral c. Ot algia/Otorea unilateral 3. GEJALA LEHER : a. Benjolan leher unilateral bilateral 4. GEJALA MATA & SYARAF : a. Sakit kepala b. Diplopia (N3&6) c. Ptosis (N4) d. Trismus (N5) e. Parese lidah (N12) f. Parese Saraf Otak lain PF Penunjang Penentuan Stadium
Alur Diagnosis Pemeriksaan Pemeriksaan lengkap THT-Kepala Leher: 1. Pemeriksaan hidung & nasofaring (THT le ngkap) : a. Rinoskopi anterior & posterior b. Nasoendoskopi/nasolaringoskopi kak u/fleksibel 2. Perhatian pada : a. OMS, Lesi Intrakranial, Limfadenopati Servika l 3. Pemeriksaan kelenjar leher: Anamnesis Penunjang lokasi, ukuran, kekenyalan, mobilitas 4. Pemeriksaan lesi intrakranial: a. Gangguan gerak bola mata (Diplopia N3&6) b. Ptosis (N4) c. Trismus (N5) d. Parese lidah (N12) Penentuan Stadium
Alur Diagnosis Pemeriksaan Penunjang 1. CT scan/MRI 2. Serologi: a) IgA VCA b) IgA EA c) EBNA total Tentukan Stadium : 1. Ro Toraks 2. Laboratorium: fungsi hati, ginjal, kimia drh 3. Konsul saraf dan mata 4. USG abdm atas & bone scan 5. Audiogram Anamnesis & PF
GAMBARAN KLINIS WORK UP CT scan NF Curiga (+) PENEMUAN KNF(-) ulangi 3x/eksplorasi (-) bukan KNF Biopsi NF KNF (+)
Anamnesis : KGB leher >> Keluhan hidung,telinga, sakit kepala kronis PF Kls curiga : CT scan NF Serologi OM Serosa e.c. tidak jelas Pe IgA KGB leher curiga FNAB KSS/Ca undiff
PENEMUAN STAGING Stadium I Hasil PA WHO Pemeriksaan 3 hr Stadium II KNF (+) Staging persiapan terapi Stadium III Stadium IV
STAGING TERAPI Radiasi ekst 60 Gy + brakiterapi 4-6 x 3 Gy PR : cisplatin + 5 FU TR : ci splatin + 5FU + Docetaxel + atau Carboplatin + Docetaxel + gemcitabin Rekurensi : < 1 thn Kemoterapi > 1 thn Kemoradiasi Radiasi ekst 60 Gy + brakiterapi 4-6 x 3 Gy PR : cisplatin + 5 FU TR : cisplatin + 5FU + Docetaxel atau Carboplatin + D ocetaxel + gemcitabin Rekurensi : < 1 thn Kemoterapi > 1 thn Kemoradiasi FOLLOW UP Thn I : setiap 1-2 bln Thn II: setiap 2-3 bln Thn III: setiap 4-6 bln Thn IV & V : setiap 12 bln Setiap follow up: Anamnesis & PF Nasofaringoskopi Set iap 6 bln ( th.I & II) Lab, R toraks, CT scan NF Seromarker, Bonescan USG abdomen Stadium I T1 N0 M0 Stadium IIA T2a N0 M0 Biopsi ulang stlh 6 bln/thn 1 Rehabilitasi minggu ke-2 stlh radiasi
STAGING TERAPI Radiasi ekst 60 Gy + brakiterapi 4-6 x 3 Gy + kemoterapi PR : cisplatin + 5 FU TR : cisplatin + 5 FU + Docetaxel atau Carboplatin + Docetaxel + gemcitabi n Rekurensi : < 1 thn Kemoterapi > 1 thn Kemoradiasi Neoadjuvan + kemoradiasi Re seksi KGB bl primer bersih Bila T3 CT scan u/ radiasi Bila N2 CT scan u/ booster KGB 5-10 x 2 Gy FOLLOW UP Thn I : setiap 1-2 bln Thn II: setiap 2-3 bln Thn III: setiap 4-6 bln Thn IV & V : setiap 12 bln Setiap follow up: Anamnesis & PF Nasofaringoskopi Set iap 6 bln ( thn.I & II ) Lab, R toraks, CT scan NF Seromarker, Bonescan USG abdom en Stadium IIB T1 N1 M0 T2a N1 M0 T2b N0-1 M0 Stadium III T1 N2 M0 T2a N2 M0 T2b N2 M0 T3 N0-2M0 Biopsi ulang stlh 6 bln/thn 1 Rehabilitasi minggu ke-2 stlh radiasi
STAGING Stadium III T1 N2 M0 T2a N2 M0 T2b N2 M0 T3 N0-2M0 TERAPI FOLLOW UP Thn I : setiap 1-2 bln Thn II: setiap 2-3 bln Thn III: setiap 4-6 bln Thn IV & V : setiap 12 bln Setiap follow up: Anamnesis & PF Nasofaringoskopi Set iap 6 bln ( th. I & II ) Lab, R toraks, CT scan NF Seromarker, Bonescan USG abdom en Neoadjuvan + radiasi Reseksi KGB bl primer bersih Bila T3 a N2 CT scan u/ booster KGB 510 x 2 Gy Neoadjuvan + radiasi 60 Gy Bila penekanan saraf mata (+) Stadium IVa T4 N0-3 M0 T berapa pun, N3, M0 Stadium IVb T berapa pun, N berapa pun, M1 Neoadjuvan + radiasi paliatif 40-60 Gy Untuk lokasi tumor pd weight bearing bone radioterapi dahulu Biopsi ulang stlh 6 bln/thn 1 Rehabilitasi minggu ke-2 stlh radiasi CT scan u/ radiasi Bil Radioterapi cito
S-ar putea să vă placă și
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (120)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- Gambar Klasifikasi FR PDFDocument12 paginiGambar Klasifikasi FR PDFAditya Chandra ForestaÎncă nu există evaluări
- Imaging of The ThyroidDocument4 paginiImaging of The ThyroidMuhamad Amar'sÎncă nu există evaluări
- Pabi Jna Makassar Final 2Document18 paginiPabi Jna Makassar Final 2Muhamad Amar'sÎncă nu există evaluări
- No BED Nama U RM Diagnosis Non Ortho MRS STA TUS OP Tindakan Plan Biaya Raber LAB PP DS DPJ PDocument3 paginiNo BED Nama U RM Diagnosis Non Ortho MRS STA TUS OP Tindakan Plan Biaya Raber LAB PP DS DPJ PMuhamad Amar'sÎncă nu există evaluări
- File Weekly 24-31 Mei 2019 20.30Document39 paginiFile Weekly 24-31 Mei 2019 20.30Muhamad Amar'sÎncă nu există evaluări
- SabbbjDocument8 paginiSabbbjMuhamad Amar'sÎncă nu există evaluări
- Uro 16 Nov EditDocument1 paginăUro 16 Nov EditMuhamad Amar'sÎncă nu există evaluări
- Uro Oktober 2018Document4 paginiUro Oktober 2018Muhamad Amar'sÎncă nu există evaluări
- 97042.14foot S89 S94 PDFDocument6 pagini97042.14foot S89 S94 PDFMuhamad Amar'sÎncă nu există evaluări
- Preop BS 10-17Document2 paginiPreop BS 10-17Muhamad Amar'sÎncă nu există evaluări
- Uro Oktober 2018Document7 paginiUro Oktober 2018Muhamad Amar'sÎncă nu există evaluări
- Mandibular JurnalDocument7 paginiMandibular JurnalMuhamad Amar'sÎncă nu există evaluări
- 97042.15metatarsals S95 S98 PDFDocument4 pagini97042.15metatarsals S95 S98 PDFMuhamad Amar'sÎncă nu există evaluări
- Mandible AoDocument1 paginăMandible AoMuhamad Amar'sÎncă nu există evaluări
- Tumor Resection by Stereotactic Craniotomy Using The Brown Roberts Wells SystemDocument10 paginiTumor Resection by Stereotactic Craniotomy Using The Brown Roberts Wells SystemMuhamad Amar'sÎncă nu există evaluări
- Brain EdemaDocument27 paginiBrain EdemaarininisaulÎncă nu există evaluări
- Urologi 7 Nov 18Document1 paginăUrologi 7 Nov 18Muhamad Amar'sÎncă nu există evaluări
- Orto 2Document5 paginiOrto 2Muhamad Amar'sÎncă nu există evaluări
- Comparison of Plate VS. Nail FixationDocument20 paginiComparison of Plate VS. Nail FixationMuhamad Amar'sÎncă nu există evaluări
- Orto 2Document5 paginiOrto 2Muhamad Amar'sÎncă nu există evaluări
- Skingraft Jurnal PDFDocument6 paginiSkingraft Jurnal PDFMuhamad Amar'sÎncă nu există evaluări
- Jurnal PlastikDocument8 paginiJurnal PlastikMuhamad Amar'sÎncă nu există evaluări
- Plastic JournalDocument7 paginiPlastic JournalMuhamad Amar'sÎncă nu există evaluări
- 3290 12632 1 PBDocument6 pagini3290 12632 1 PBMuhamad Amar'sÎncă nu există evaluări
- Daftar Pustaka FIXDocument4 paginiDaftar Pustaka FIXMuhamad Amar'sÎncă nu există evaluări
- Floating ShoulderDocument10 paginiFloating ShoulderMuhamad Amar'sÎncă nu există evaluări
- 3d Printing Technique To Aid Surgical Planning in Treatment of Floating Shoulder Injury A Case Report 2167 1222 1000272Document3 pagini3d Printing Technique To Aid Surgical Planning in Treatment of Floating Shoulder Injury A Case Report 2167 1222 1000272Muhamad Amar'sÎncă nu există evaluări
- Wjco 6 25Document6 paginiWjco 6 25Muhamad Amar'sÎncă nu există evaluări
- A Technique of Endoscopic Nipple-Sparing Mastectomy For Breast CancerDocument8 paginiA Technique of Endoscopic Nipple-Sparing Mastectomy For Breast CancerMuhamad Amar'sÎncă nu există evaluări
- APJCP - Volume 17 - Issue S3 - Pages 43-46 PDFDocument4 paginiAPJCP - Volume 17 - Issue S3 - Pages 43-46 PDFMuhamad Amar'sÎncă nu există evaluări