Documente Academic
Documente Profesional
Documente Cultură
Gardner Manuscript
Încărcat de
fundj22Descriere originală:
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Gardner Manuscript
Încărcat de
fundj22Drepturi de autor:
Formate disponibile
J Neurosurg 100:965973, 2004
Historical vignette
W. James Gardner: pioneer neurosurgeon and inventor
NARENDRA NATHOO, M.D., PH.D., MARC R. MAYBERG, M.D., AND GENE H. BARNETT, M.D.
Brain Tumor Institute and Department of Neurosurgery, Cleveland Clinic Foundation, Cleveland, Ohio
W. James Gardner, a skillful neurosurgeon and inventor, is best remembered for his cervical tongs and hydrodynamic theory of syringomyelia. A pioneer of modern neurosurgery, Gardner trained under Charles Frazier in Philadelphia, and in 1929 he moved to Ohio where he became chief of neurosurgery at the Cleveland Clinic, a position he was to hold for the next 33 years. A large surgical practice made it imperative for Gardner to develop surgical methods that were quick, effective, and advantageous for patient and surgeon. He was an early proponent of the sitting position for patients undergoing cranial surgery, which led to the development of a neurosurgical chair with a head fixation device. To reduce the risks of hypotension and air embolism when the patient is in the sitting position, Gardner invented the clinical G suit. He was the first to advocate and use induced arterial hypotension for intracranial surgery and the first neurosurgeon in the US to publish his experiences performing lumbar discography. He converted an operating table so that he could induce hypothermia during aneurysm surgery and then applied pneumatic cuffs to occlude the major arterial supply to the brain. His pioneering work has been documented in many other areas such as hemifacial spasm and trigeminal neuralgia, for which he performed the first vascular decompression, in cervical sympathectomy for treatment of various ailments, and in the use of intrathecally delivered steroid drugs for sciatica. During his career, he authored 256 publications and one book on the dysraphic states. Many of his contributions to the discipline of neurosurgery are now taken for granted.
KEY WORDS W. James Gardner hydromyelia trigeminal neuralgia skull tongs neurological history JAMES Gardner (18981987) is best remembered for his skull tongs and his theories on congenital hindbrain abnormalities and hydromyelia. Few of todays practitioners, however, know about the breadth and depth of the accomplishments of this great teacher and pioneer neurosurgeon. Gardners career straddled the transition of neurosurgery from an art practiced by few individuals to a science that has evolved into the current complex array of subspecialities. Through his diverse activities in the academic neurosurgical arenas of patient care, education, and clinically relevant research, Gardner helped to strengthen the fledgling discipline. During his three decades at the Cleveland Clinic, he served actively in many important capacities and strongly believed in and enjoyed the concept of group practice. In addition, the tradition of clinical research and academic excellence established by Gardner laid the foundation for the accomplishments of the neurosurgery department at his institution and continues to be an important part of its mission.
Biographical Sketch W. James Gardner was born in McKeesport, Pennsylvania on June 12, 1898, and attended McKeesport High
Abbreviations used in this paper: CSF = cerebrospinal fluid; LP = lumbar puncture; TN = trigeminal neuralgia.
School. He spent his boyhood summers hunting and fishing in the Allegheny forest and maintained this love of outdoor activity throughout his life. Both of Gardners parents, his two sisters, and their housekeeper died of tuberculosis before he finished high school. He received a B.A. degree from Washington and Jefferson College in 1920 and on graduating from medical school in 1924 was appointed to a 2-year rotating internship at the University of Pennsylvania. Gardners father, Gardner, and his son (William James Gardner III) all graduated from the University of Pennsylvania in (1894, 1924, and 1954, respectively), thereby keeping intact the family tradition of graduating a James Gardner every 30 years from the University of Pennsylvania. He married a clinical psychologist, Ann Ray Kieffer, in 1928. He participated in sports with the same zeal and energy that he gave to his scientific pursuits. He took up tennis and ice skating, whereas his skiing career was cut short when he broke his tibia in an accident. He was an excellent dancer, even inventing shoes for dancing on carpet, was a member of a barbershop quartet of colleagues from the Clinic, and thoroughly enjoyed giving and attending a good party. Gardner and Frazier: The University of Pennsylvania (19261929) Two key events were to occur in Gardners life that led to
965
J. Neurosurg. / Volume 100 / May, 2004
N. Nathoo, M. R. Mayberg, and G. H. Barnett
his interest in neurosurgery and his subsequent move to the Cleveland Clinic. In a sense, both were related to his association with Professor Charles H. Frazier, who was the chairman of the surgical department at the University of Pennsylvania. Frazier was a pioneer neurosurgeon, who also maintained a busy general surgical practice, with a special interest in thyroid problems. The first event that impacted his life and career was an unexpected vacancy on Fraziers service that coincided with the beginning of Gardners mandatory 3-month rotation in neurosurgery in April 1926. This was created by the decision of Fraziers assistant, Temple Fay, to spend 2 years on William G. Spillers neurology service. Rotation on Fraziers service had become unpopular among the interns because of its demanding nature and the Chiefs stern demeanor. Gardners plan was to practice general surgery as his father had done, and he believed that he could weather this experience. To Gardners dismay, however, he found himself, a neophyte, alone in an extremely busy clinical sevice. He worked very hard, day and night, to keep up with the workload, and gradually found himself becoming impressed with Fraziers personality, dedication, and surgical skilland with neurosurgery. When Frazier still had not found a new assistant at the end of his initial rotation, Gardner volunteered for another 3 months. At the end of that second rotation Frazier still had not found a new assistant, so Gardner, having enjoyed his stint in neurosurgery, volunteered for a third 3-month rotation. After this, he wrote, the die was cast, as he became Fraziers assistant for the next 3 years at a salary of $125 a month.16 One of Gardners highlights during his residency was to attend clinical consultations between Frazier and Spiller, at which, despite their respect for each other, there was almost certain to be an argumentespecially on where to turn the bone flap. As a resident, Gardner conducted considerable research, such as studying the effect of various substances on intracranial pressure and a comprehensive review of an extended family from Pennsylvania whose members had hereditary bilateral acoustic neuromas. In 1930, with Frazier as coauthor, he reported a field survey of five generations of a family in which central neurofibromatosis was found, showing clearly mendelian dominant-type inheritance.38 They performed surgery on a seventh-generation family member54 and finally managed to convince Dr. Eldridge of the National Institutes of Health to study this family.73 This was the first report of hereditary deafness resulting from bilateral acoustic neuromas. The Cleveland Clinic Years
The Interview
the now busy service. Clinic records show that George Crile Sr. (one of the four Cleveland Clinic founders and a cofounder of the American College of Surgeons) had written to Frazier, expressing interest in Francis Chubby Grant. Frazier, though, who had approximately 5 years left until his retirement, wanted Grant to take over the unit at the University of Pennsylvania. Frazier instead recommended Gardner for the position. By coincidence, Gardner was scheduled to present a paper on the therapeutic effects of encephalography at a meeting of the Pennsylvania State Medical Society in Erie in September 1929. Dr. Lower, a urologist and another of the Clinics founders, was in attendance specifically to invite Gardner for a visit to the Clinic. Gardner accepted and was entertained that evening by the Criles and Lowers. The following morning he was escorted to the Clinic by Dr. Lower, purportedly to meet the staff. Instead Gardner was taken to the bed of a patient who 2 weeks previously had been surgically treated by a general surgeon for an unlocalized brain tumor. A right subtemporal decompression had been performed but no tumor had been disclosed. On clinical examination, Gardner found that the patient exhibited papilledema with a Broca aphasia and made a diagnosis of a left temporal tumor. Lower then suggested that Gardner remove the tumor; however, Gardner declined because he had commitments in Philadelphia the next day. Lower then led Gardner to the surgical pavilion where an operating room was prepared for a craniotomy. Unable to resist the opportunity to demonstrate his surgical skills, Gardner performed a large left-sided osteoplastic flap, removed a large globular meningioma, and finished the surgery in 2 hours and 20 minutes. With this display of his clinical acumen and surgical skill, the job was his with a salary of $6000 per year.16 Luck was on Gardners side; the stock market crashed 30 days later and the Great Depression began in the US. So began his career as Chief of Neurological Surgery at the Cleveland Clinic, an association that was to last for 33 years. After he stepped down as chief in 1962, he was a senior consultant with the department until his first retirement in 1964. Postretirement Years (19641974) After mandatory retirement from the Cleveland Clinic in 1964 at the age of 65 years, Gardner opened a private practice in the Greater Cleveland area, was the head of neurosurgery at the Fairview General Hospital (19641967), and was on the staff at the Huron Road Hospital from 1964 to 1974. With the establishment of an emeritus program at the Cleveland Clinic, he rejoined the Department of Neurosurgery staff after his second retirement in 1974. Gardners Contributions to Neurological Surgery Gardners busy and diverse practice at the Clinic placed him in a unique position to make contributions in many aspects of neurosurgery. A brief review of some of his important contributions follows. Neurotrauma Chronic Subdural Hematomas In 1946, while he was operating with Albert LaLonde (a
J. Neurosurg. / Volume 100 / May, 2004
The second happenstance to alter Gardners life was the Cleveland Clinic disaster. On May 15, 1929, an explosion of smoldering x-ray films occurred in the basement of the outpatient department of the Clinic. The poisonous gas that was released took the lives of 123 people, including the clinics first neurosurgeon, Charles E. Locke, who had trained with Harvey Cushing. This accident led to the development of a new composition for x-ray films and to new regulatory processes regarding their storage. The clinic, as the result of this catastrophe, found itself badly in need of a neurosurgeon to assume the leadership of
966
W. James Gardner: pioneer neurosurgeon and inventor
resident) on a brain tumor, a nurse from the ward mentioned to them that a patient who had undergone evacuation of a chronic subdural hematoma the previous day was dying. Gardner sent LaLonde to assess the patient and to perform an LP to rule out recurrent bleeding. The resident found the patient in a CheyneStokes respiratory pattern and the LP revealed a very low pressure. Gardner then requested that LaLonde repeat the LP and inject saline until the pressure was restored. The resident reported that after he had injected 60 ml of normal saline into the lumbar subarachnoid space, the previously comatose patient awoke, looked over his shoulder, and said, What the hell is going on back there? From then on the compressed hemisphere was reexpanded during surgery in each patient with a chronic subdural hematoma.62 Gardner also described the latency period of these lesions by performing animal experiments.30,49 Spinal Surgery
Lumbar Discography
encounter. He therefore made an impassioned plea . . . that less qualified surgeons in spine must be discouraged from expanding into this essentially neurosurgical field which is fraught with pitfalls for the inexperienced. Hydrodynamic Theory for Congenital Hindbrain Anomalies Gardners hydrodynamic theory on the pathophysiology of syringomyelia and other dysraphic states was based on his clinical experiences.16 In brief, Gardner believed that each systolic pulse generated a pressure gradient throughout the CSF (Bering effect) that tended to force the CSF out of the ventricles. He suggested that this hydrodynamic effect was responsible for the formation of the subarachnoid pathways when the rhombic membrane ruptured, but that it also played a role in shaping the developing brain. If failure or inadequate rupture of the rhombic membrane occurred (fourth ventricular outlet obstruction), the pulsatile CSF would then flow through the patent obex and enter the central canal with the resultant water-hammer pulse effect causing dilation of the central canal, leading to syringomyelia, whereas an open neural tube was due to overdistension and rupture rather than failure to close.7,8,12,21,27,33,35,36, 41,43 Therefore, depending on the delicate balance between lateral ventricle and fourth ventricular choroid plexus pulsatility, he believed that the DandyWalker and Chiari malformations were part of the same spectrum of disease, and that both were caused by embryonal hydrocephalus. Gardner was a steadfast believer in and defender of the hydromyelic theory of Morgagni, which was proposed in 1769. In his 1960 paper on myelomeningocele Gardner22 starts off with a quote from Roger Bacon (ca. 12141294) about the four stumbling blocks of truth, and goes on to criticize Von Recklinghausen, who in 1886 discredited Morgagnis hydromyelic theory. Furthermore, Gardner believed that solely on the basis of appearance, Von Recklinghausen assumed that myeloschisis represented a failure of neural tube closure rather than rupture, as Gardner believed. He goes on to state that Therefore to this day, because of custom and influence of the great Von Recklinghausens authority, the araphic theory has gone unchallenged even though embryological, pathological, clinical, and experimental evidence favors Morgagnis less fragile hypothesis. In 1973, using a combination of his clinical experience as well as expertise in physics, physiology, embryology, anatomy, and ultrastructure, Gardner published his monograph called The Dysraphic States: From Syringomyelia to Anencephaly. Recently, Gardners hydrodynamic theory has been partially corroborated with magnetic resonance imaging findings.66 Functional Neurosurgery Hemifacial Spasm and TN Gardners lifelong interest in TN began during his residency in 1926. As early as 1915, Frazier began to practice subtotal sectioning of the sensory root and in 1918 he proposed sparing the motor root. This latter technique was put to the test when a distinguished lady from Lima, Peru, who had been surgically treated by Frazier in 1917, returned with pain on the contralateral side. During the previous sur967
After Lindbloms initial description in 1948, the first lumbar discography in the US was performed at the Cleveland Clinic by Wise and Weiford in 1951, with Gardner, et al.,42 following shortly thereafter in March 1952 with the second paper. The next 89 cases in which this modality was used were reported by Wise, et al.,72 in June 1952; an additional 165 lumbar discographies were later reported in 1957.71 In 1962, Collis and Gardnes2 described their experience examining 1014 cases, the largest series reported at that time. Four hundred ninety-three of 1014 patients who underwent lumbar discography subsequently underwent surgery in which fewer interspaces were explored surgically, resulting in less trauma to nerve roots, while the incidence of multiple herniations was 1.5% (410 surgically verified herniated discs in 404 patients). In the discussions that followed its publication, the paper received mixed reviews, with Ralph Cloward strongly endorsing the results. In 1951, both Gardner and Cloward independently exhibited their technique of lumbar discography at the American Medical Association convention in Atlantic City.
Epidural Steroid Delivery/Pantopaque Arachnoiditis
Based on his previous work with Seghal on corticosteroid agents administered intradurally for relief of sciatica,67 Gardner, Sehgal, and Dohn15 published in a nonpeer reviewed journal their experience with subarachnoid injections of methylprednisone acetate for patients suffering from Pantopaque arachnoiditis. In 60 of 100 patients they managed to reduce the radicular pain with no adverse effects for a period of up to 2 years.
Spinal Specialization
By the 1960s, after a neurosurgical career spanning more than 3 decades and having witnessed the increasing specialization of surgery for spinal degenerative diseases, Gardner sent out a questionnaire to all neurosurgical chiefs to evaluate current trends in disc surgery in their units. In an invited editorial published in Surgery Gynecology and Obstetrics in 1965, Gardner12 wrote, The surgeon who operates within the spinal canal should be prepared by training and experience to handle any type of surgical lesion that he may
J. Neurosurg. / Volume 100 / May, 2004
N. Nathoo, M. R. Mayberg, and G. H. Barnett
gery, Frazier had not attempted to spare the motor root. Gardner described the atmosphere in the operating room on the morning of surgery as tense and electric, and despite Fraziers flawless surgery with positive faradic stimulation of the motor root prior to closure, the patients chin was seen to be resting on her sternum postoperatively. Much to everyones relief, voluntary contractions began to appear in the masseter 10 days later.16 Based on clinical experience, Gardner believed that TN is a symptom rather than a disease, which may present in conditions such as multiple sclerosis, basilar impression, or in relation to tumor or vascular compression, either in the posterior fossa or the middle cranial fossa.9,20,37,45 Expanding on the hypothesis supported by Olivecrona,65 Lee,63 and Taarnhj,69 Gardner initially believed that the pain of TN was caused by the development of an artificial synapse in the sensory root fibers where the nerve crossed the apex of the petrous bone.11 This artificial synapse was caused by demyelination secondary to the development of a sagging tentorium, which was accompanied by advancing age and humans upright posture. This sagging tentorium, which may be further influenced by the mild platybasia secondary to osteoporosis, transformed the normally oval-shaped dural foramen that transmits the nerve into a relatively flat slit.31,44,53 This change in shape led to neural distortion that resulted in focal demyelination, leading to short circuiting of sensory action potentials, thereby forming, in effect, an artificial synapse. Although Dandy in 1934 had made the observation that the trigeminal nerve was often cross-compressed by a neighboring elongated artery or sometimes a vein, the first reported vascular decompression of the nerve was performed by Gardner. In 1959, Gardner and his Fellow, Miklos,25 published their results of decompression of the sensory root in a series of 200 patients with TN who were followed up for as long as 6 years. One hundred of the patients made up the Cleveland series, in which the approach was primarily extradural, whereas the other 100 patients (Copenhagen series) underwent an intradural approach. In the combined series, 62% of the patients reported a complete response, 11.5% had a mild recurrence, and 26.5% had severe recurrences. Sensory loss was present in 26% of the patients with complete response and in 28% of those in whom treatment failed. This led Gardner to believe that neither surgical trauma to the nerve root nor incision of its dural sleeve was essential to the success of the surgery. He believed that hemifacial spasm, on the other hand, lacked the characteristics of self limitation and a refractory period typical of a reflex, and that these motor paroxysms could best be explained on the basis of a peripheral reverberating circuit set up between the afferent (proprioceptive) and efferent fibers at the point of compression.15 Gardner also showed that paroxysms of hemifacial spasm, like TN, may be stopped immediately and with no impairment of function by a nontraumatic manipulation of the nerve root.47 Gardner found that in 19 patients with hemifacial spasm, eight had vascular compression of the seventh cranial nerve. His work preceded the use of the intraoperative microscope, however, and therefore he was unable to inspect the dorsal root entry zone adequately.15,47
Surgery for the Autonomic Nervous System
sympathetic blocks for cerebral embolus, thrombosis, and causalgia of the upper limbs, and for trauma to the brain. In 1946, Karnosh (a neuropsychiatrist at the Cleveland Clinic), Gardner, and Stowell62 reported the effects of temporary cerebral sympathectomy accomplished by bilateral stellate ganglion blocks on organic brain diseases and psychoses.60,61 This discovery occurred incidentally in January 1946 when a 38-year-old woman received bilateral stellate blocks for cerebral embolus accompanied by hemiplegia and DejerineRoussy syndrome. This led to the implementation of this procedure in a series of patients with cerebral vascular disease, brain atrophy, and Parkinson disease. Most patients were enthusiastic about the improvement that they claimed the procedure produced, although motion picture analysis revealed no improvement in motor function and it was believed that this apparently impressive improvement in mood was caused by the sympatholytic effects. Karnosh and Gardner decided to try bilateral stellate ganglion procaine blocks in a small group of patients suffering from depression and anxiety and in patients with known schizophrenia. In three patients with depression, the temporary sympathetic block resulted in an improvement of affect, a relative euphoria, transient relief from suicidal ideation, and psychomotor retardation. No effect was observed in psychotic patients.59 Gardner: As Inventor Gardner believed that his research had to have a direct clinical application, otherwise he would pay the issue scant attention. Despite his immense clinical workload, he still had the energy to explain clinical phenomena and help sick patients, and never went without some project to occupy his time. Each problem was followed through with dogged determination even though the initial results were often enough to discourage the most enthusiastic researcher. His inventiveness, combined with hard work and determiation, was among his greatest attributes. We briefly review some of his inventions.
The Gardner Neurosurgical Chair (1938)
Gardner routinely practiced cervical and stellate ganglion
968
During his residency, Gardner learned that Frazier had recognized the tremendous advantage of placing a patient in the sitting position while performing surgery for TN.16,19 Frazier commented that this position prevented a puddle of blood from covering the nerve filaments, placed the operative field comfortably at the level of the surgeons eyes, and that smaller amounts of anesthetic agents could be used. In addition, de Martel started using the sitting position in 1911 and found that it decreased hemorrhage and aided respiration. De Martel favored operating with the patient in the sitting position after induction of local anesthesia so that early recognition of syncope could be corrected by lowering the patients head. Gardner mentions one occasion when Frazier, on returning from a visit to de Martels clinic in Paris, recounted what he saw when the famous French neurosurgeon performed surgery while the patient received local anesthesia. De Martel had apparently performed a suboccipital craniectomy for a cerebellar tumor in an 11-year-old girl whom he made straddle a wooden chair, cross her arms on its back, and rest her head on her forearms. Frazier described this as a horrible exhibition.16
J. Neurosurg. / Volume 100 / May, 2004
W. James Gardner: pioneer neurosurgeon and inventor
Gardner started using the sitting position in 1930 and soon came to realize its benefits, especially when he performed surgery on the posterior fossa or the posterior neck region. Gardner reviewed his series of 56 suboccipital craniectomies and 78 supratentorial craniotomies performed with patients in the sitting position.19 From this experience he recognized the dangers of hypotension and air embolism when using this position; as a result, Gardner developed a neurosurgical chair equipped with a head clamp for rigid fixation that could be used to position the patients head firmly in any position during surgery. He built the first model of the Gardner chair in 1938 and then a later version in 1955.22 A modified version of the Gardner chair (Fig. 1) is still used today by the senior author (G.H.B.) for selected cases.
Tantalum Cranioplasty (1944)
Although Fulcher was the first to report the use of tantalum in repairing a cranial defect, it was Gardner who popularized this material (pure metal: 73rd element in the Periodic Table). Using a thinner sheet (to reduce the degree of radiopacity) cut by conventional scissors and molded, Gardner advocated its use in primary repair of cranial defects,29,70 even in the presence of intracranial infection.32
Constant Traction Dressing (1945)
Gardners war experience fueled his interest in cranial wounds.14,25,29 Together with Seitz, a research engineer at the Cleveland Clinic, he developed the constant traction dressing which was more comfortable than the usual gauze dressing.45 More importantly, however, the skin edges underwent progressive approximation resulting in a narrower scar, in some cases averting the need for secondary suturing and/or skin grafting.13 The dressing consisted of two metal members (0.004 in thick) connected by a sheet of latex. The metal spurs were short so that they only penetrated the stratum corneum and did not cause pain. As approximation of the wound occurred, shorter dressings were applied.48
Induced Hypotension for Hemostasis (1946)
FIG. 1. Photograph showing the Gardner neurosurgical chair. The chair could be raised or lowered by a foot pump and also rotated around a vertical axis. Using a crank, it was tilted backward like a rocking chair so that the patients feet could be higher than the head. It still provides more favorable positioning for cranial surgery with the patient sitting than most modern surgical tables. A slot in the back allowed the surgeon to perform an LP during surgery, if required. By adding a table top to the backward-tilted chair and a three-point head fixation device, the supine patient could be readied for craniotomies. The chair was also accompanied by a lifter that could lower the patient into an adjacent bed.
Gardner was the first to apply the method of controlled hypotension during surgery as an aid to hemostasis.10,39 He believed that intravenous transfusions given to a patient in severe shock must pump the intravenous injected blood through the pulmonary circulation and then out into the aorta, before the heart itself can benefit. Believing that the primary function of the heart was to maintain a normal level of pressure in the elastic aorta and that patients in severe shock who were given intravenous fluids would experience an additional strain on an already ischemic heart, he thought that intraarterial infusion of fluids would restore the cerebral and coronary blood flow more rapidly before the burden of an increase in venous pressure and blood volume are thrown onto the weakened heart (Page procedure). This, according to Gardner, appeared to be a more physiological than intravenous infusion of the blood in severe hemorrhagic shock. He reported the beneficial effects of controlled hypotension in 161 patients during a 6-year period (1946 1953). Forty-six of 161 patients with difficult intracranial meningiomas who were treated using the Page procedure were compared with another group of 44 patients in whom intracranial meningiomas were surgically treated during
J. Neurosurg. / Volume 100 / May, 2004
the same period. A mortality rate of 8.7% (Page procedure) compared with 13.6% (without the technique) was recorded. For cerebral aneurysms, Gardner preferred to induce hypotension with one of the ganglion blocking drugs rather than the Page technique. In his paper on meningioma and hypotension, Gardner mentions that surgeons with their natural repugnance to blood loss have been slow to adopt a procedure which entails deliberate removal of blood from the circulation. Illustrative of this reluctance, Gardner notes that one advocate of the total spinal method had referred shudderingly to the Page procedure as the oligemic shock method.42
Alternating Pressure Pad (1948)
Gardner developed the alternating pressure pad (Fig. 2) and used it first at the Clinic in July 1947. He analyzed 100 consecutive patients in whom the mattress was used and found the value of the pressure pad to be so obvious that all patients who required the pad were given this form of care, so that he was unable to perform a subsequent randomized study. Gardner calculated that he saved 1 hour of a nurses time per patient per day with the pressure pad.23,43
The Clinical G Suit (1956)
Following his service in World War II, Gardner realized the potential of the antigravity suit that prevented blackouts in fighter pilots. He modified the G suit to consist of two sheets of vinyl plastic sealed at the edges to form a large inflatable bladder that was placed beneath the patient. The edges were folded over so that the patient was enclosed from the rib cage to the ankles, and the entire contraption
969
N. Nathoo, M. R. Mayberg, and G. H. Barnett
FIG. 2. Photograph showing alternating pressure pad. The alternating pressure pad mattress is constructed of a flexible waterproof plastic material. The apparatus consists of a pneumatic mattress with air cells 3 cm in diameter that run transversely the width of the mattress, with alternate cells connected to a manifold that constitutes the edge of each side of the mattress. Alternating inflation and deflation of the transverse cells occurs at intervals of 2 to 3 minutes so that the patients body is alternately resting on the odd-numbered cells and then on the even-numbered cells. The inflation and deflation of the two air systems is driven by a small air pump.
FIG. 3. Photograph showing the clinical G suit, which consisted of two sheets of vinyl plastic sealed at the edges to form a large inflatable bladder, so that the patient was enclosed from the rib cage to the ankles; the entire contraption was drawn snug by lacing. The system included a manometer and the suit was inflated by a gas tank.
was drawn snug by lacing. The system had a manometer and was inflated by a gas tank (Fig. 3). If a patient experienced hypotension while in the sitting position or if Gardner anticipated hypotension in any position, the clinical G suit could be inflated in a matter of seconds.17,50 The clinical G suit helped save the life of a staff members wife after she developed postpartum hemorrhaging which, after 11 hours of futile surgical efforts to control intraabdominal bleeding, had resulted in 56 blood transfusions administered over a period of 18 hours. She was placed in the G suit at a pressure of 20 mm Hg and this raised her blood pressure, stopped the bleeding, and saved her life.52 In their 1956 paper, Gardner and Dohn wrote that while doing a literature search, they discovered that one of the earliest descriptions of the antigravity suit had been made by George Crile Sr.3 in 1903. He abandoned this work, however, because of technical difficulties with his suit (constructed from India rubber), while at the same time improving methods that had been developed for blood transfusion. The principle of applying the G suit to combat hypotension has been documented in many publications.4,6,17,50
Hypothermia With Temporary Occlusion of Major Brain Arteries by Pneumatic Cuffs (1956)
expanded the cellophane tube, thus occluding the artery. In applying the device, the cellophane tubing was passed twice around the common carotid artery with the distal end tied to the proximal end, where it was fastened to the catheter. To occlude the vertebral artery, it was only necessary to expose a cervical vertebral foramen and draw the cellophane cuff partly through it. The four catheters were then connected by a series of T-tubes to an ordinary blood pressure apparatus so that all four arterial cuffs could be simultaneously activated.46 To induce hypothermia, Gardner, Wasmuth (an anesthesiologist), and Hale35 converted an operating table into a refrigerating trough by enclosing the patient in a watertight plastic sheet draped over a rectangular frame and then submerging only the body in ice water.
GardnerWells Cervical Traction Tongs (1959)
Gardner developed pneumatic cuffs that were used to occlude the four major arterial vessels to the brain simultaneously during aneurysmal rupture so that the surgeon could ligate or clip the aneurysm while the patient was in a state of hypothermia.46 One end of moistened cellophane tubing (1 cm in flat width and 8 cm in length) was tied to the amputated end of a No. 8 French gauge soft rubber catheter into which a 16-gauge syringe had been previously inserted on the opposite end. The other end of the cellophane tubing was ligated and both proximal and distal ends were tied, thus forming a loop with the No. 8 French catheter protruding from one end of the tubing with the syringe on its opposite end. Air from the syringe introduced into the catheter
970
In 1959 Gardner developed his cervical skull traction tongs and later, with Wells, improved the design for emergency bedside application under antiseptic rather than aseptic conditions. His design maximized the mechanical efficiency of the tong for cervical traction by repositioning the upward-directed tapering pins to engage in the outer table of the temporal bones at points between the ears and the skulls equator (Fig. 4). The principal advantage over the Crutchfield tongs was that no shaving was necessary, and after application of a local anesthetic agent, advancing the tapered points through the scalp caused the stretched skin to fit snugly about the pins, thereby sealing their point of entry, which prevented bleeding. One of the points was rendered retractable by an enclosed spring that was calibrated to indicate the pressure. On encountering bone, the stiff spring yielded until the outer end of the spring-loaded point barely protruded beyond the flat surface of the knurled end. Gardner later simplified the construction and developed safeguards against perforations of the inner table.1,24 The Gardner tongs are now widely used in many institutions.
J. Neurosurg. / Volume 100 / May, 2004
W. James Gardner: pioneer neurosurgeon and inventor
FIG. 4. Photograph showing the GardnerWells cervical traction tongs. The main structural element is a rigid C-shaped metal bar that roughly conforms to the coronal suture of the skull. Sharp tapered pins positioned at an upward angle at the ends of the C-shaped metal structure are screwed into the skull.
Waterbed and Hammock (1961)
Gardner developed a waterbed for children who were prone to pressure sores due to hydrocephalus. The infant was floated on a bag of water, which was made redundant and relaxed by placing it in a box or crib. An alarm system was incorporated to detect leakage and the water temperature could be thermostatically controlled. Gardner also developed a hammock that prevented an infant with scaphocephaly from resting on the flat side of its head, thereby preventing an increase in the deformity.40
The G Splint (1962)
FIG. 5. Photographic portrait of W. James Gardner.
Other Gardner Inventions and Contributions
The G splint (Immobil-Air), developed in 1962, was a spinoff from the clinical G suit. This pneumatic splint, inflated by mouth in a matter of seconds, was designed as a first-aid device to be used in an emergency to stabilize the patient from hemorrhaging in the extremity and to immobilize the broken limb. This pneumatic splint was a doublewalled sleeve of transparent plastic film in which air was forced between the two layers, resulting in compression of the limb by the inner layer, whereas the outer layer tended to elongate, exerting a splinting effect and traction.18 After delivering a lecture on syringomyelia to the neurosurgery staff at McGill University in Canada, Gardner noticed Wilder Penfield walking with a slight limp in the cafeteria. While picking up his food tray, Penfield experienced a sudden pain in his knee. Raising his trouser leg, a rapid swelling in the knee due to spontaneous hemorrhage was diagnosed; this occurred in an old knee injury sustained when a torpedo in World War I struck Penfields destroyer. An orthopedist present in the cafeteria ordered immediate bed rest and a compression bandage. Gardner, however, had a sample of the G splint with him, and he quickly applied it directly over the trouser on Penfields leg, thus stopping the bleeding. Penfield subsequently wrote to Gardner requesting another splint and in his letter of thanks he mentioned that he never subsequently left home without it.16
J. Neurosurg. / Volume 100 / May, 2004
His pioneering contributions to neurosurgery occurred in several other areas such as cerebral hemispherectomy26 in the treatment of glioma, and treatment of carotidcavernous fistula by muscle embolization.58 Among Gardners other lesser known inventions was his adaptation of the Souttar craniotome (1929) soon after arriving at the Cleveland Clinic (this was used until power tools for opening the skull were introduced in the 1960s);16 the development of a neurosurgical suction irrigator;64 modification of the respirator with D. E. Hale (1948);57 recording time on roentgenograms (1954);51 and a ventriculomastoid shunt in which a Holter valve was used for the treatment of hydrocephalus (1962).5 Conclusions W. James Gardner was a pioneer neurosurgeon, scientist, inventor, and educator (Fig. 5). Many of his contributions to the field are now taken for granted. His theories on the pathogenesis of several neurological disorders have stood the test of time or have served as the foundation on which contemporary theories rest. In total, Gardner trained 28 neurosurgeons and 14 others served their fellowships with him; this was in addition to the many general surgical residents who passed through his service. His genius has not gone unrecognized by neurosurgical organizations and the Cleveland Clinic. During his neurosurgical career, Gardner was active in many national and regional organizations. He was President of the Society of Neurological Surgeons, Vice President of the Cushing Society, on the Board of Governors of the American College of
971
N. Nathoo, M. R. Mayberg, and G. H. Barnett
Surgeons, and a member of the American Board of Neurological Surgery for 6 years. He was an honorary guest of the Congress of Neurological Surgeons in 1987 and in 1982 received the Cushing Medal from the American Association of Neurological Surgeons for his contributions to neurosurgery. The Cleveland Clinic and the Department of Neurological Surgery established the annual Gardner lectureship in his honor in June 1978.
Acknowledgments We thank Ms. Martha Tobin (Department of Neurosurgery, Cleveland Clinic Foundation) for helping to edit the manuscript, Fred K. Lautzenheiser and Carol Tomer from the Cleveland Clinic Archives Department for providing access to the archival material (Dr. Gardners personal notes and original reprints), for providing assistance with the figures, and for verifying historical accuracy. We also thank Dr. Donald Dohn (former resident and colleague of Dr. Gardner) for verification of historical accuracy. References 1. Barnett GH, Hardy RW: Gardner tongs and cervical traction. Med Instrum 16:291292, 1982 2. Collis JS Jr, Gardner WJ: Lumbar discography. An analysis of one thousand cases. J Neurosurg 19:452461, 1962 3. Crile G Sr: Blood Pressure in Surgery: an Experimental and Clinical Research. Philadelphia: Lippincott, 1903, pp 288289 4. Dohn DF, Gardner WJ: The antigravity suit (G suit) in surgery; control of blood pressure in the sitting position and in hypotensive anesthesia. JAMA 162:274276, 1956 5. Dohn DF, Gardner WJ: The treatment of hydrocephalus by ventriculo-mastoid shunt utilizing the Holter valve. Surg Forum 13: 440441, 1962 6. Ferrario CM, Nadzam G, Fernandez LA, et al: Effects of pneumatic compression on the cardiovascular dynamics in the dog after hemorrhage. Aerosp Med 41:411415, 1970 7. Gardner WJ: Anatomic anomalies common to myelomeningocele of infancy and syringomyelia of adulthood suggest a common origin. Cleve Clin Q 26:118133, 1959 8. Gardner WJ: Anatomic features common to the Arnold-Chiari and the Dandy-Walker malformations suggest a common origin. Cleve Clin Q 26:206222, 1959 9. Gardner WJ: Concerning the mechanism of trigeminal neuralgia and hemifacial spasm. J Neurosurg 19:947958, 1962 10. Gardner WJ: The control of bleeding during operation by induced hypotension. JAMA 132:572574, 1946 11. Gardner WJ: Cross-talkthe paradoxical transmission of a nerve impulse. Arch Neurol 14:149156, 1966 12. Gardner WJ: Diastematomyelia and the Klippel-Feil syndrome. Relationship to hydrocephalus, syringomyelia, meningocoele, meningomyelocele, and iniencephalus. Cleve Clin Q 31:1944, 1964 13. Gardner WJ: Electrical burn of the brain. J Neurosurg 5:9094, 1948 14. Gardner WJ: Experiences of a US Naval Mobile Hospital Unit no. 4 in the Southwest Pacific. Ohio State Med J 39:570573, 1943 15. Gardner WJ: Five-year cure of hemifacial spasm. Report of a case. Cleve Clin Q 27:219221, 1960 16. Gardner WJ: Half century of neurosurgery. Surg Clin North Am 58:945956, 1978 17. Gardner WJ: Hemostasis by pneumatic compression. Am Surg 35:635637, 1969 18. Gardner WJ: An inflatable emergency splint. Clevel Clin Q 29: 5456, 1962 19. Gardner WJ: Intracranial operations in the sitting position, in Ravdin IS, Adson AW, Grant FC (eds): Surgery in two Parts. Part II. General Surgery and Allied Subjects. Comprising Contributions in Surgery in Honor of C.H. Frazier. Philadelphia: Lippincott, 1935, pp 138145 20. Gardner WJ: The mechanism of tic doloureux. Trans Am Neurol Assoc 3:168173, 1953 21. Gardner WJ: Myelomeningocele, the result of rupture of the embryonal neural tube. Cleve Clin Q 27:88100, 1960 22. Gardner WJ: A neurosurgical chair. J Neurosurg 12:8186, 1955 23. Gardner WJ: Prevention and treatment of bedsores. An air mattress accomplishing alternation of pressure points. JAMA 138: 583, 1948 24. Gardner WJ: The principle of spring-loaded points for cervical traction. Technical note. J Neurosurg 39:543544, 1973 25. Gardner WJ: Progress in neurosurgical treatment of war wounds. Ohio State Med J 43:936938, 1944 26. Gardner WJ: Removal of the right cerebral hemisphere for infiltrating glioma. Report of a case. JAMA 101:823826, 1933 27. Gardner WJ: Rupture of the neural tube. Arch Neurol 4:17, 1961 28. Gardner WJ: Specialization in intraspinal surgery. Surg Gynecol Obstet 121:838839, 1965 29. Gardner WJ: Tantalum in the immediate repair of traumatic skull defects: method of immobilizing the wounded brain. US Nav M Bull 43:11001106, 1944 30. Gardner WJ: Traumatic subdural hematoma. With particular reference to the latent interval. Arch Neurol Psychiatry 27: 847858, 1932 31. Gardner WJ: Trigeminal neuralgia in elderly women. Geriatrics 18:731739, 1963 32. Gardner WJ: The use of tantalum for repair of cranial defects in infected cases. Cleve Clin Q 13:7287, 1946 33. Gardner WJ, Abdullah AF, McCormack LJ: The varying expressions of embryonal atresia of the fourth ventricle in adults. Arnold-Chiari malformation, Dandy-Walker syndrome, arachnoid cyst of the cerebellum, and syringomyelia. J Neurosurg 14: 591605, 1957 34. Gardner WJ, Anderson RM, Lyden M: The alternating pressure pad: an aid to the proper handling of decubitus ulcers. Arch Phys Med Rehabil 35:578580, 1954 35. Gardner WJ, Angel J: The mechanism of syringomyelia and its surgical correction. Clin Neurosurg 6:131140, 1958 36. Gardner WJ, Collis JS: Klippel-Feil syndrome. Syringomyelia, disastematomyelia and myelomeningoceleone disease? Arch Surg 83:638644, 1961 37. Gardner WJ, Dohn DF: Trigeminal neuralgiahemifacial spasm Pagets disease: significance of this association. Brain 89: 555562, 1966 38. Gardner WJ, Frazier CH: Bilateral acoustic neurofibromas. A clinical study and field survey of a family of five generations with bilateral deafness in thirty-eight members. Arch Neurol Psychiatry 23:266300, 1930 39. Gardner WJ, Hale DE: Arterial bloodletting during operation as aid in hemostasis. Am J Surg 79:635644, 1950 40. Gardner WJ, Holmok DE: The water-bed and the hammock. Use in hydrocephalus and scaphocephaly. Am J Dis Child 102: 237238, 1961 41. Gardner WJ, Karnosh LJ, Angel J: Syringomyelia; a result of embryonal atresia of the foramen of the Magendie. Trans Am Neurol Assoc 82:144145, 1957 42. Gardner WJ, Ling A: Controlled hypotension by the bleeding method in operations for intracranial meningiomas. Surg Gynecol Obstet 98:343346, 1954 43. Gardner WJ, McCormick LJ, Dohn DF: Embryonal atresia of the fourth ventricle. The cause of arachnoid cyst of the cerebellopontine angle. J Neurosurg 17:226237, 1960 44. Gardner WJ, Miklos MV: Response of trigeminal neuralgia to decompression of sensory root; discussion of cause of trigeminal neuralgia. JAMA 170:17731776, 1959 45. Gardner WJ, Pinto JP: Taarnhj operation: relief of trigeminal neuralgia without numbness. Cleve Clin Q 20:364367, 1953 46. Gardner WJ, Salmoiraghi GC: Pneumatic cuff for temporary occlusion of arteries. JAMA 160:1224, 1956 47. Gardner WJ, Sava GA: Hemifacial spasma reversible pathophysiological state. J Neurosurg 19:240270, 1962
972
J. Neurosurg. / Volume 100 / May, 2004
W. James Gardner: pioneer neurosurgeon and inventor
48. Gardner WJ, Seitz VB: Constant traction dressing. Am J Surg 70: 232323, 1945 49. Gardner WJ, Shannon EW: A study of 27 cases of chronic subdural hematomas. Ohio State Med J 39:835, 1943 50. Gardner WJ, Storer J: The use of the G suit in control of intraabdominal bleeding. Surg Gynecol Obstet 123:792798, 1966 51. Gardner WJ, Takiguchi R: A method of recording time on a roentgenogram. AJR 71:1060, 1954 52. Gardner WJ, Taylor HP, Dohn DF: Acute blood loss requiring fifty-eight transfusions: use of antigravity suit as aid in postpartum intra-abdominal hemorrhage. JAMA 167:985986, 1958 53. Gardner WJ, Todd EM, Pinto JP: Roentogenographic findings in trigeminal neuralgia. AJR 76:346350, 1956 54. Gardner WJ, Turner OA: Bilateral acoustic neurofibromas. Further clinical and pathological data on hereditary deafness and Recklinghausens disease. Arch Neurol Psychiatry 44:7699, 1940 55. Gardner WJ, Wasmuth CE, Hale DE: A method of converting an operating table into a refrigerating trough. J Neurosurg 13: 122123, 1956 56. Gardner WJ, Wise ER, Hughs CR, et al: X-ray visualization of the intervertebral disk. With a consideration of the morbidity of disk puncture. Arch Surg 64:355364, 1952 57. Hale DE, Gardner WJ: A modification of the respirator. JAMA 136:984985, 1948 58. Hamby WB, Gardner WJ: Treatment of pulsating exophthalmos. With report of two cases. Arch Surg 27:676685, 1933 59. Karnosh LJ, Gardner WJ: The effects of bilateral stellate ganglion block on mental depression; report of 3 cases. Cleve Clin Q 14: 133138, 1947 60. Karnosh LJ, Gardner WJ: Observations on mood after stellate ganglionectomy. South Med J 41:631636, 1948 61. Karnosh LJ, Gardner WJ, Stowell A: The effect of cerebral sympathectomy on organic brain diseases and psychoses. Trans Am Neurol Assoc 72:157160, 1947 62. LaLonde AA, Gardner WJ: Chronic subdural hematoma. Expansion of compressed cerebral hemisphere and relief of hypotension by spinal injection of physiologic saline solution. N Engl J Med 239:493496, 1948 Lee FC: Trigeminal neuralgia. J Med Assoc Ga 26:431, 1937 Nosik WA, Gardner WJ: A neurosurgical suction-irrigator. Am J Surg 44:477478, 1939 Olivecrona H: Cholesteatomas of the cerebello-pontine angle. Acta Psychiatry Neurol 24:639643, 1949 Pillay PK, Awad IA, Hahn JF: Gardners hydrodynamic theory of syringomyelia revisited. Cleve Clin J Med 59:373380, 1992 Sehgal AD, Gardner WJ: Corticosteroids administered intradurally for relief of sciatica. Cleve Clin Q 27:198201, 1960 Sehgal AD, Gardner WJ, Dohn DF: Pantopaque arachnoditis treatment with subarachnoid injections of corticosteroids. Cleve Clin Q 29:177188, 1962 Taarnhj P: Decompression of the trigeminal root. J Neurosurg 11:299305, 1954 Weiford EC, Gardner WJ: Tantalum cranioplasty: review of 106 cases in civilian practice. J Neurosurg 6:1332, 1949 Wise RE, Gardner WJ, Hosier RB: X-ray visualization of the intervertebral disk. N Engl J Med 257:610, 1957 Wise RE, Gardner WJ, Hughes CR, et al: X-ray visualization of the intervertebral disk. Modern Med 20:104112, 1952 Young DF, Eldridge R, Gardner WJ: Bilateral acoustic neuroma in a large kindred. JAMA 214:347353, 1970
63. 64. 65. 66. 67. 68. 69. 70. 71. 72. 73.
Manuscript received September 24, 2003. Accepted in final form January 12, 2004. This paper will be presented in part at the 72nd Annual Meeting of the American Association of Neurological Surgeons May 16, 2004, Orlando, Florida. Address reprint requests to: Gene H. Barnett, M.D., Brain Tumor Institute, Cleveland Clinic Foundation, 9500 Euclid Avenue, Cleveland, Ohio 44195. email: barnett@neus.ccf.org.
J. Neurosurg. / Volume 100 / May, 2004
973
S-ar putea să vă placă și
- KabatDocument9 paginiKabatStefanie VilelaÎncă nu există evaluări
- Diagnosis of Stupor and Coma-1-250!1!125Document125 paginiDiagnosis of Stupor and Coma-1-250!1!125Crhistian Andreé Cervantes CartagenaÎncă nu există evaluări
- Vladimir Janda, MD, DSC: Tribute To A Master of RehabilitationDocument5 paginiVladimir Janda, MD, DSC: Tribute To A Master of RehabilitationSean DrewÎncă nu există evaluări
- Plum and Posner's Diagnosis of Stupor and ComaDocument416 paginiPlum and Posner's Diagnosis of Stupor and Comakikotido8100% (1)
- The Clinical and Scientific Basis of Myalgic Encephalomyelitis/ Chronic Fatigue Syndrome Byron M. Hyde, M.D.Document753 paginiThe Clinical and Scientific Basis of Myalgic Encephalomyelitis/ Chronic Fatigue Syndrome Byron M. Hyde, M.D.Gènia100% (2)
- Imaging Skeletal Trauma Rogers 4e PDFDocument229 paginiImaging Skeletal Trauma Rogers 4e PDFCarmen PopaÎncă nu există evaluări
- John GibbonDocument4 paginiJohn GibbonCIRUGIA CARDIOTORÁCICA MINIMAMENTE INVASIVAÎncă nu există evaluări
- Harold Schuknecht and Pathology of The Ear - Baloh 2001Document10 paginiHarold Schuknecht and Pathology of The Ear - Baloh 2001J WÎncă nu există evaluări
- Christiaan BarnardDocument5 paginiChristiaan BarnardfrawatÎncă nu există evaluări
- History of SurgeryDocument5 paginiHistory of SurgeryjbahalkehÎncă nu există evaluări
- Chiropractic Day: A Historical Review of A Day Worth CelebratingDocument10 paginiChiropractic Day: A Historical Review of A Day Worth CelebratingcdjohnsondcÎncă nu există evaluări
- Clinical Neurophysiology 3 e 2009Document915 paginiClinical Neurophysiology 3 e 2009Eldar Sulejmanovic100% (11)
- V Courtney Broaddus Joel D Ernst Talmadge E King JR Et Al Murray 1Document50 paginiV Courtney Broaddus Joel D Ernst Talmadge E King JR Et Al Murray 1angelomabaÎncă nu există evaluări
- Download ebook The Md Anderson Manual Of Medical Oncology Pdf full chapter pdfDocument67 paginiDownload ebook The Md Anderson Manual Of Medical Oncology Pdf full chapter pdfsummer.stephens690100% (20)
- CH 20 Manter Gatz S Essentials of Clinical Neuroanatomy and NeurophysiologyDocument27 paginiCH 20 Manter Gatz S Essentials of Clinical Neuroanatomy and Neurophysiologyasarg214100% (1)
- Manual of Neurologic TherapeuticsDocument534 paginiManual of Neurologic TherapeuticsDefault User100% (1)
- Parkinson S Disease and Related Disorders Part II PDFDocument570 paginiParkinson S Disease and Related Disorders Part II PDFskyclad_21Încă nu există evaluări
- Personalizing Illenss and ModernityDocument29 paginiPersonalizing Illenss and ModernityChristos PapasÎncă nu există evaluări
- Gonstead Chiropractic Pioneer BiographyDocument6 paginiGonstead Chiropractic Pioneer Biographystansimpson1122Încă nu există evaluări
- Boala Cardiaca CoronarianaDocument557 paginiBoala Cardiaca CoronarianaLivia Gudac100% (1)
- Interventional UrologyDe la EverandInterventional UrologyArdeshir R. RastinehadÎncă nu există evaluări
- ANOMALOuS HEALiNg ExPEriENCESDocument29 paginiANOMALOuS HEALiNg ExPEriENCESGyula VattamányÎncă nu există evaluări
- Charles Miller FisherDocument3 paginiCharles Miller FisherMacho MarcelloÎncă nu există evaluări
- Walsh&Hoyt Clinical Neuro-OphthalmologyDocument3.527 paginiWalsh&Hoyt Clinical Neuro-OphthalmologyDaniela RuedaÎncă nu există evaluări
- Homosexuality Aversion Therapy: Case of Treated BYDocument3 paginiHomosexuality Aversion Therapy: Case of Treated BYIonelia PașaÎncă nu există evaluări
- Jasper Evan Sadler - LancetDocument1 paginăJasper Evan Sadler - LancetlariialvezÎncă nu există evaluări
- Alexa CanadyDocument5 paginiAlexa Canadyns786Încă nu există evaluări
- Indian MedicineDocument1 paginăIndian MedicineMilton BiswasÎncă nu există evaluări
- Dr. Aunali S Khaku, MD, Letter of Recommendation, Sleep Fellowship, DR Richard BerryDocument1 paginăDr. Aunali S Khaku, MD, Letter of Recommendation, Sleep Fellowship, DR Richard Berryask1288Încă nu există evaluări
- Bernard Jensen - Iridology PDFDocument610 paginiBernard Jensen - Iridology PDFAurora Miko100% (7)
- BALOWClinical Neurophysiology of The Vestibular SystemDocument478 paginiBALOWClinical Neurophysiology of The Vestibular SystemRodrigo CabreraÎncă nu există evaluări
- Dismantling The Ketogenic Diet With DR - NicholasgonzalezDocument49 paginiDismantling The Ketogenic Diet With DR - NicholasgonzalezCristina100% (3)
- Ch119 HFN ExamDocument12 paginiCh119 HFN ExamAbhishek Kumar RamadhinÎncă nu există evaluări
- History of Evidence-Based Medicine: Roger L. Sur, Philipp DahmDocument3 paginiHistory of Evidence-Based Medicine: Roger L. Sur, Philipp DahmSamuel LopesÎncă nu există evaluări
- Flies in the Ointment: Medical Quacks, Quirks and OdditiesDe la EverandFlies in the Ointment: Medical Quacks, Quirks and OdditiesEvaluare: 4 din 5 stele4/5 (1)
- A 5-Year-Old With Fever, Headache, Neck Stiffness, and Leg PainDocument7 paginiA 5-Year-Old With Fever, Headache, Neck Stiffness, and Leg PainKarma AkiraÎncă nu există evaluări
- Clinical Neurophysiology Contemporary NeurologyDocument916 paginiClinical Neurophysiology Contemporary NeurologyTim AroscoÎncă nu există evaluări
- Neuroendocrinology: Volume IDe la EverandNeuroendocrinology: Volume ILuciano MartiniÎncă nu există evaluări
- ClinicalNeurophysiology3e2009 PDFDocument915 paginiClinicalNeurophysiology3e2009 PDFriddhi100% (2)
- Have Scalpel - Will Travel: Tales of an Itinerant SurgeonDe la EverandHave Scalpel - Will Travel: Tales of an Itinerant SurgeonÎncă nu există evaluări
- MD Anderson Medical Oncology 4th Edition 2022Document1.694 paginiMD Anderson Medical Oncology 4th Edition 2022Iskandar414100% (6)
- Spine: Essential Neurosurgery For Medical StudentsDocument29 paginiSpine: Essential Neurosurgery For Medical StudentsAndreea IduÎncă nu există evaluări
- WTG Morton PDFDocument7 paginiWTG Morton PDFrkÎncă nu există evaluări
- Human Genes and Genomes: Science, Health, SocietyDe la EverandHuman Genes and Genomes: Science, Health, SocietyEvaluare: 5 din 5 stele5/5 (1)
- Caso RciuDocument13 paginiCaso RciuMarcela HincapiéÎncă nu există evaluări
- Henry Kaplan and the Story of Hodgkin's DiseaseDe la EverandHenry Kaplan and the Story of Hodgkin's DiseaseEvaluare: 5 din 5 stele5/5 (1)
- Bernard Grad The Legacy Live OnDocument4 paginiBernard Grad The Legacy Live OnKelvin Gutierrez100% (1)
- Kuru: An Incurable Degenerative Neurological Disorder: February 2013Document3 paginiKuru: An Incurable Degenerative Neurological Disorder: February 2013IlmanÎncă nu există evaluări
- Medicinus Agustus 2014 PDFDocument68 paginiMedicinus Agustus 2014 PDFfile fileÎncă nu există evaluări
- Edgar Cayce On HealingDocument132 paginiEdgar Cayce On Healinganca_dinca0% (1)
- VA Anesthesia 2022 Guide To A Career in Anesthesiology For Medical Students Part 1 Pages 1 24Document25 paginiVA Anesthesia 2022 Guide To A Career in Anesthesiology For Medical Students Part 1 Pages 1 24mohananprasad27Încă nu există evaluări
- 57-Year-Old Woman With Covid-19 and DelusionsDocument9 pagini57-Year-Old Woman With Covid-19 and DelusionsNazly ÁlvarezÎncă nu există evaluări
- Reference Management for Medical PapersDocument37 paginiReference Management for Medical PapersregarskidÎncă nu există evaluări
- Courage and Character, Leaders and Legends: An Interview With Richard LowerDocument2 paginiCourage and Character, Leaders and Legends: An Interview With Richard LowerAli RajaÎncă nu există evaluări
- In Memoriam: Carl C. Pfeiffer, - ., PH.D., - .: B A M DDocument2 paginiIn Memoriam: Carl C. Pfeiffer, - ., PH.D., - .: B A M DSchwab RealHumanÎncă nu există evaluări
- Migraine. e BookDocument532 paginiMigraine. e BookfaisalÎncă nu există evaluări
- Gastrointestinal DiseasesDocument853 paginiGastrointestinal DiseasesCiobanasu Denisa100% (1)
- MAdness Adn MedDocument6 paginiMAdness Adn MedAngie MoralesÎncă nu există evaluări
- P 249Document7 paginiP 249fundj22Încă nu există evaluări
- SoapDocument7 paginiSoapfundj22Încă nu există evaluări
- 128 E112-ADocument2 pagini128 E112-Afundj22Încă nu există evaluări
- Paper 26Document4 paginiPaper 26fundj22Încă nu există evaluări
- Lumbar Stenosis 2006Document12 paginiLumbar Stenosis 2006fundj22Încă nu există evaluări
- 128 E112-ADocument2 pagini128 E112-Afundj22Încă nu există evaluări
- Acute Appendicitis The Reliability of DiagnosisDocument6 paginiAcute Appendicitis The Reliability of DiagnosisHarun NasutionÎncă nu există evaluări
- MHGap Intervention Guide PDFDocument107 paginiMHGap Intervention Guide PDFfundj22100% (1)
- Nasopharyngeal CancerDocument27 paginiNasopharyngeal CancerTheQueensafa90Încă nu există evaluări
- Algorithm Febrile SeizuresDocument32 paginiAlgorithm Febrile SeizuresSi Puput100% (1)
- Pediatrics 1992 Casteels Van Daele 129Document3 paginiPediatrics 1992 Casteels Van Daele 129fundj22Încă nu există evaluări
- Jurnal IKADocument6 paginiJurnal IKAfundj22Încă nu există evaluări
- Insiden KNF Di AsiaDocument4 paginiInsiden KNF Di AsiaArdhan PutraÎncă nu există evaluări
- Breech Presentation and DeliveryDocument60 paginiBreech Presentation and DeliverySilvy Amalia100% (1)
- Chiari MalformationDocument22 paginiChiari Malformationapi-28517738067% (3)
- Scoliosis A Case Study in An Adolescent BoyDocument9 paginiScoliosis A Case Study in An Adolescent BoyJAZMYNN ANNE ALCANTARAÎncă nu există evaluări
- Tanta Neuro MCQDocument9 paginiTanta Neuro MCQBadr Diham100% (1)
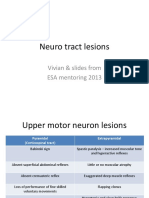
- Neuro tract lesions guide for UMN, LMN deficitsDocument16 paginiNeuro tract lesions guide for UMN, LMN deficitsসোমনাথ মহাপাত্রÎncă nu există evaluări
- Gardner ManuscriptDocument9 paginiGardner Manuscriptfundj22Încă nu există evaluări
- Pathophysiology of SyringomyeliaDocument14 paginiPathophysiology of SyringomyeliaGerardo100% (2)
- Boli Vertebro MedulareDocument12 paginiBoli Vertebro MedulareHalit DianaÎncă nu există evaluări
- High-Yield Neurology and Senses ReviewDocument72 paginiHigh-Yield Neurology and Senses ReviewMahmoud Abu MayalehÎncă nu există evaluări
- Pediatric RehabDocument32 paginiPediatric RehabRainy DaysÎncă nu există evaluări
- Cong Anomalies and Tumors of SpineDocument120 paginiCong Anomalies and Tumors of SpineSunny SbaÎncă nu există evaluări
- SyringomyeliaDocument3 paginiSyringomyeliaAndi SanapatiÎncă nu există evaluări
- Sensory and Its DisordersDocument8 paginiSensory and Its Disordersjalan_zÎncă nu există evaluări
- Motor neurone disease د.رشاد عبدالغنيDocument18 paginiMotor neurone disease د.رشاد عبدالغنيMohammad BelbahaithÎncă nu există evaluări
- Arnold Chiari Malformation & SyringomyeliaDocument38 paginiArnold Chiari Malformation & SyringomyeliaBojan PavlovicÎncă nu există evaluări
- Syringomyelia, Arachnoiditis and SpasticityDocument53 paginiSyringomyelia, Arachnoiditis and SpasticitySam OlukaÎncă nu există evaluări
- Rare spinal cord disease syringomyelia definition causes symptoms treatmentDocument8 paginiRare spinal cord disease syringomyelia definition causes symptoms treatmentNurfadiyah YasinÎncă nu există evaluări
- Causes of Weakness of Lower Limbs by DR Bashir Ahmed Dar Chinkipora Sopore KashmirDocument23 paginiCauses of Weakness of Lower Limbs by DR Bashir Ahmed Dar Chinkipora Sopore KashmirProf Dr Bashir Ahmed Dar Chinki Pora Sopore Kashmir100% (1)
- Syringomyelia in Neuromyelitis Optica Seropositive For Aquaporin-4 Antibody: A Case ReportDocument4 paginiSyringomyelia in Neuromyelitis Optica Seropositive For Aquaporin-4 Antibody: A Case ReportIJAR JOURNALÎncă nu există evaluări
- Chiari Malformation: An Overview: Rick Labuda, Executive DirectorDocument18 paginiChiari Malformation: An Overview: Rick Labuda, Executive DirectornsurgeonÎncă nu există evaluări
- SyringomyeliaDocument17 paginiSyringomyeliaAkash Marathakam100% (2)
- Bmjopen 2020 January 10 1 Inline Supplementary Material 1Document31 paginiBmjopen 2020 January 10 1 Inline Supplementary Material 1mazen alkarras100% (1)
- Dias 2013Document12 paginiDias 2013Santiago Diaz PinillosÎncă nu există evaluări
- Intramedullary Spinal Cord Tumors: Part II - Management Options and OutcomesDocument10 paginiIntramedullary Spinal Cord Tumors: Part II - Management Options and OutcomeszixzaxoffÎncă nu există evaluări
- SpinaBifida ManagementDocument4 paginiSpinaBifida ManagementDimple GoyalÎncă nu există evaluări
- Osmotic demyelination syndromes: Two case reports of central and extrapontine myelinolysis with normal sodiumDocument5 paginiOsmotic demyelination syndromes: Two case reports of central and extrapontine myelinolysis with normal sodiumNontaphon PiyawattanamethaÎncă nu există evaluări
- Case Study Intramedullary Spinal Cord TumorDocument13 paginiCase Study Intramedullary Spinal Cord TumorCitra KristiÎncă nu există evaluări
- SyringomyeliaDocument3 paginiSyringomyeliaImran TagalaÎncă nu există evaluări
- Spinal Cord Disease by GadisaDocument128 paginiSpinal Cord Disease by GadisaGadisa DejeneÎncă nu există evaluări
- SYRINGOMYELIADocument16 paginiSYRINGOMYELIAkyki ab100% (2)
- Term 2 Fall 2018Document90 paginiTerm 2 Fall 2018Artemio ZavalaÎncă nu există evaluări