Documente Academic
Documente Profesional
Documente Cultură
The Court
Încărcat de
Vanessa SantosDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
The Court
Încărcat de
Vanessa SantosDrepturi de autor:
Formate disponibile
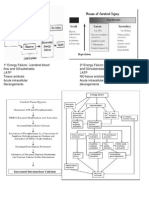
The court The game is played on a volleyball court 18 meters (59 feet) long and 9 meters (29.
5 feet) wide, divided into two 9 m 9 m halves by a one-meter (40-inch) wide net placed so that the top of the net is 2.43 meters (7 feet 11 5/8 inches) above the center of the court for men's competition, and 2.24 meters (7 feet 4 1/8 inches) for women's competition (these heights are varied for veterans and junior competitions). There is a line 3 meters from and parallel to the net in each team court which is considered the "attack line". This "3 meter" (or 10 foot) line divides the court into "back row" and "front row" areas (also back court and front court). These are in turn divided into 3 areas each: these are numbered as follows, starting from area "1", which is the position of the serving player: After a team gains the serve (also known as siding out), its members must rotate in a clockwise direction, with the player previously in area "2" moving to area "1" and so on, with the player from area "1" moving to area "6". The team courts are surrounded by an area called the free zone which is a minimum of 3 meters wide and which the players may enter and play within after the service of the ball.[9] All lines denoting the boundaries of the team court and the attack zone are drawn or painted within the dimensions of the area and are therefore a part of the court or zone. If a ball comes in contact with the line, the ball is considered to be "in". An antenna is placed on each side of the net perpendicular to the sideline and is a vertical extension of the side boundary of the court. A ball passing over the net must pass completely between the antennae (or their theoretical extensions to the ceiling) without contacting them.
Volleyball Court Dimensions The Volleyball court is 60 feet by 30 feet in total. The net in placed in the center of the court, making each side of the net 30 feet by 30 feet. Center Line A center line is marked at the center of the court dividing it equally into 30 feet squares, above which the net is placed. Attack Line An attack line is marked 10 feet of each side of the center line. Service Line A service line, the area from which the server may serve the volleyball, is marked 10 feet inside the right sideline on each back line. The Net The net is placed directly above the center line, 7 feet 4 inches above the ground for women and 8 feet above the ground for men. Poles Volleyball poles should be set at 36 feet apart, 3 feet further out from the sidelines. Ceiling Height The minimum ceiling height should be 23 feet, though they should preferably be higher.
Facilities & Equipment Used in Volleyball
Learn the regulation standards for the popular sport of volleyball. Volleyball is a popular NCAA and Olympic sport. The facilities and equipment used in collegiate and world class competition must meet regulation standards. Court 1. The entire in-play area of the court measures 60 by 30 feet and is painted a light color. All lines are painted white. As noted by Top End Sports, the ceiling of the indoor facility must be at least 23 feet high, but it's preferable to be higher. Net The net should be positioned 8 feet high for a men's game. Measuring from the ground to the top, the net is 7 feet 4 inches high for the women's game and 8 feet high for the men's game. Net poles are positioned 36 feet apart. Ball A competition volleyball will fall in the range of 25 to 27 inches in circumference.According to the International Federation of Volleyball (FIVB) rulebook, a competition ball must measure approximately 25 to 27 inches (64 to 67cm) in circumference and weigh 9 to 10 oz. (260 to 280g). It should be inflated to a pressure of approximately 4.5 psi. Primary Mediastinal B-Cell Lymphoma Case Presentation and Review Ali Moussa, M.D.
H&P
25 year old Hispanic female presented with 2 month history of chest discomfort and SOB. She also complained of weight loss, night sweats, fever and chills. These symptoms subsequently worsened, requiring ER visit, where a CXR was done and revealed a mediastinal mass. Further evaluation with CT scan revealed a mediastinal mass and left supraclavicular lymphadenopathy.
History
The patient underwent a biopsy of the supraclavicular lymph node. Two days later, the patient was noted to have chylous drainage from the biopsy site and injury to thoracic duct was suspected. She underwent reexploration and injury to thoracic duct was repaired.
History
PMH: Polycystic ovary disease Meds: None SH: patient was a housekeeper; no smoking, alcohol or drug abuse FH: Non-contributory
Physical Exam
T:98.0 BP:128/78 P:98 RR:12 General: Obese Hispanic female in NAD HEENT: PERRL, EOMI, anicteric sclerae Neck: Discharging wound from left supraclavicular area Heart: RRR, no rubs Lungs: clear to auscultation Abdomen: Soft, NO HSM, non-tender Ext: No edema, good pulses
Lab Findings
WBC 9.1 N78, L14, M5, E2 Hgb 13.6 Hct 40.0 Plt 244 Cr 0.7 Ca 8.0
Uric acid 5.8 TP 4.9 Alb 2.1 Tbil 0.5 Alk Phos 78 LDH 2733 -2 microglobulin <0.5
Patholgy
Diffuse infiltrate of neoplastic lymphoid cells, which are partially surrounded by bands of fibrous tissue. Population of CD19/CD20/CD22 positive lymphocytes with loss of surface expression of both kappa and lambda immunoglobulin light chain. Bone marrow aspirate & biopsy: no tumor infiltration.
Radiographic Findings
CT chest: 12 x 6 x 11 cm heterogenous mass in the anterior mediastinum displacing the great vessels. Nodular thickening of the pericardium. CT abdomen and pelvis: no lymphadenopathy, small amount of ascites. Gallium scan: Positive for uptake in hilar and mediastinal areas.
Hospital Course
The patient underwent 7 cycles of CHOP with decrease in the size of the mediastinal mass. However, repeat Gallium scan showed uptake in the mediastinal area. The patient was treated with ESHAP and subsequently peripheral stem cell collection. Later on she will undergo transplantation.
Primary Mediastinal B-Cell Lymphoma
Uncommon type of B-cell lymphoma. Predominant involvement of the mediastinum. Superior vena cava syndrome. Lack of diffuse lymphadenopathy. Young median age (30-40). Female predominance.
2-3% of all non-Hodgkins lymphoma cases. 6-12% of all diffuse large cell lymphoma cases. Other names: Diffuse histiocytic lymphoma with sclerosis, mediastinal large cell lymphoma with sclerosis.
Primary Mediastinal B-Cell Lymphoma
Histopathology
Uniformly large cell lymphoma. Major feature is presence of broad bands of dense fibrosis. Often associated with areas of necrosis. Express B-cell markers (CD19, CD20, CD22). Exhibit rearranged IG heavy and light chain genes. Negative: TDT, CD3, CD5, CD10, CD15.
Molecular Biology
1 of 16 cases had bcl-6 rearrangement (40-45% in DLCL). No bcl-2 rearrangement was found (20-25% in DLCL). Missense point mutations of P53 (3 of 16). Frequent gains involving chromosomes 2p, 9p, 12q, and Xq. No EBV association.
Molecular Biology
Recently MAL gene expression was demonstrated in 8/12 cases of PMBCL (no MAL in DLCL). Role of MAL is unknown, but it is speculated to be involved in membrane signaling, which may be related to PMBCL lymphomagenesis.
Clinical Features
Median age 30-40 Female predominance Median time to diagnosis 4-6 weeks Chest pain, cough, dyspnea 90-95% SVC syndrome 50-60% B symptoms 20-30%
Clinical Features
Elevated LDH 40-80% Splenomegaly is rare Pleural effusion 50% Supraclavicular adenopathy 30-35% Stage I/II 80-85% Bone marrow involvement <10% CNS involvement <5%
Clinical Features
Bulky disease is found in 70-80%. Local mediastinal relapse frequently accompanies distant extranodal dissemination. Low serum 2-microglobulin. At relapse, PMBCL often display an aggressive pattern of hematogenous dissemination.
2-Microglobulin
Cells exhibit defects in the expression of MHC class I antigens. These antigens are required for tumor cell recognition by cytotoxic T lymphocytes. Decreased MHC class I has been suggested as an escape mechanism from immune control. 2-microglobulin is the light chain common to MHC class I.
Treatment
Response to treatment varies among series as the result of small numbers of patients. Early studies suggested that PMBCL are a highly aggressive subgroup of NHL with poorer prognosis. More recent studies demonstrated that PMBCL is a curable disease.
Treatment A study by Lazzarino et al. reported treatment outcome for a large (N=106) cohort of PMBCL treated with CHOP at 4 European institutions: 1-Bulky disease was present in 73%.
2-SVC was present in 47%. 3-Pericardial and pleural effusion was present in 36% and 35%, respectively.
Lazzarino et al.
65% had response (CR 23%, PR 42%). Of those who responded, 49 (77%) received consolidative XRT to the mediastinum. 35% had refractory disease. 3 year survival rates for the entire series was 50%, 82% for the responders. For the non-responders, salvage therapy included second line chemotherapy with or without transplantation; median survival was 10 months.
Lazzarino et al.
Relapse rate for responders was 28%. Most relapses occurred within 18 months of diagnosis and were predominantly intrathoracic. No significant difference between patients who received or did not receive consolidative XRT. Median survival time after relapse was 7 months.
Italian Study
50 pts: 30F, 20M, median age 31, stage I-II 84%. All patients received MACOP-B. XRT to the mediastinum: 30-36 Gy. CR 86%, only 7 non-responders. Overall survival was 82% at 96 months. Gallium-scan negativity was an important prognostic factor in restaging patients treated for PMBCL.
Role of Transplantation
Because of unsatisfactory results of conventional chemotherapy salvage in patients refractory to treatment or relapsed, use of high dose chemotherapy (HDCT) has been advocated. HDCT is the preferred salvage treatment or as front-line consolidation in patients with poor prognostic factors (bulky disease, pleural or pericardial effusion, stage III or IV).
Transplantation
Popat et al. described the outcome of 31 patients with PMBCL: 14 had induction failures, 11 had chemosensitive relapse, 6 chemoresistant relapse. Conditioning regimens included BEAM, BEAC, CBV, TBC. 42% had previously undergone XRT.
Popat et al.
PMBCL was associated with significantly better 5-year overall survival as compared to diffuse large B-cell lymphoma (56% vs 35%). Interestingly, mediastinal localization was 1 of 3 factors associated with improved survival (the other 2 being LDH level and stage).
Sehn et al.
34 patients with PMBCL underwent transplantation: 4 CR, 8 PR, 11 first relapse, 12 primary refractory disease. Conditioning regimen: CBV. 18 patients received XRT. 5 yr survival was 57%.
Sehn et al.
Predictive factors for progression free survival were: Chemosensitive disease (75% vs 33%). Disease status at the time of transplant (83% for first response, 58% for primary refractory disease, and 27% for first relapse). Administration of XRT did not affect survival.
ASH 1999
52 pts: 33F, 19M, median age 40, stage II. After initial surgery, 3 courses of double CHOP-like regimen was given, then 40 Gray XRT. 46 CR (88%), 5 failures, 1 toxic death. 9 relapses. 10 yr disease free survival was 73.6% and overall survival rate was 78.6%.
Conclusion
PMBCL is a uncommon type of NHL. The prominent production of stroma with abundant fibrosis is a peculiar property (seen also in nodular sclerosis HD). Outcome of patients who have complete response is very good. Role of XRT remains to be defined.
Conclusion
It is probably appropriate to consider CHOP the standard first line chemotherapy. Consider HDCT/SCT: survival benefit may not be limited to patients with chemosensitive relapse, but also as consolidation for patients with poor risk factors and with primary refractory disease.
S-ar putea să vă placă și
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Instruments/ Assessments: AutismDocument27 paginiInstruments/ Assessments: AutismKadir Say'sÎncă nu există evaluări
- Anatomy & Physiology Bootcamp NotesDocument51 paginiAnatomy & Physiology Bootcamp Notesgeorgia robinsonÎncă nu există evaluări
- Clinical Examination and Applied Medicine, Volume I-Gastroenterology Series (Mar 7, 2018) - (1946646938) - (CRC Press)Document176 paginiClinical Examination and Applied Medicine, Volume I-Gastroenterology Series (Mar 7, 2018) - (1946646938) - (CRC Press)taher100% (1)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- Asian Recipes - Dessert Delights (With I - Ho, CharlesDocument154 paginiAsian Recipes - Dessert Delights (With I - Ho, CharlesVanessa Santos100% (4)
- Cellular ResponsesDocument19 paginiCellular ResponsesFu Xiao ShanÎncă nu există evaluări
- Critical Care Calculations Study GuideDocument6 paginiCritical Care Calculations Study GuideAja Blue100% (2)
- British Biology Olympiad 2021Document66 paginiBritish Biology Olympiad 2021Yinyin ZhuÎncă nu există evaluări
- Mike Adams - The Healing Power of Sunlight Vitamin DDocument26 paginiMike Adams - The Healing Power of Sunlight Vitamin DJOSEPHÎncă nu există evaluări
- 978 0323049092 Color Textbook of Pediatric Dermatology Color Textbook of Pediatric Dermatology WestonDocument61 pagini978 0323049092 Color Textbook of Pediatric Dermatology Color Textbook of Pediatric Dermatology Westonaudrey.walston606100% (41)
- Characteristics of Greek LiteratureDocument2 paginiCharacteristics of Greek LiteratureVanessa Santos100% (2)
- Common Communicable DiseasesDocument213 paginiCommon Communicable Diseasesɹǝʍdןnos100% (24)
- Bone HealingDocument2 paginiBone HealingGerardLum100% (2)
- Drug Study For HepatitisDocument4 paginiDrug Study For Hepatitisunyokies100% (1)
- 40 Items Comprehensive NCLEX ReviewDocument20 pagini40 Items Comprehensive NCLEX Reviewclumsy16Încă nu există evaluări
- Personality Drawing TestDocument1 paginăPersonality Drawing TestVanessa SantosÎncă nu există evaluări
- Personality Drawing TestDocument1 paginăPersonality Drawing TestVanessa SantosÎncă nu există evaluări
- Chicken and Rice: IngredientsDocument1 paginăChicken and Rice: IngredientsVanessa SantosÎncă nu există evaluări
- Y Study CalculusDocument5 paginiY Study CalculusVanessa SantosÎncă nu există evaluări
- Ps Calc GuideDocument30 paginiPs Calc GuideMzee321Încă nu există evaluări
- Chicken Mole EnchiladasDocument2 paginiChicken Mole EnchiladasVanessa SantosÎncă nu există evaluări
- A Spark of ExistenceDocument16 paginiA Spark of ExistenceVanessa SantosÎncă nu există evaluări
- Philippine Constitution PDFDocument53 paginiPhilippine Constitution PDFVanessa SantosÎncă nu există evaluări
- Vs Circumference X 3.5Document1 paginăVs Circumference X 3.5Vanessa SantosÎncă nu există evaluări
- Copar Final3Document4 paginiCopar Final3Vanessa SantosÎncă nu există evaluări
- Republic Act No 9173Document5 paginiRepublic Act No 9173Vanessa SantosÎncă nu există evaluări
- Spinal Disc HerniationDocument12 paginiSpinal Disc HerniationVanessa SantosÎncă nu există evaluări
- IMCIDocument57 paginiIMCIwyndzÎncă nu există evaluări
- Shock Case Presentation: General DataDocument1 paginăShock Case Presentation: General DataVanessa SantosÎncă nu există evaluări
- Stone LowOxalateDiet PDFDocument7 paginiStone LowOxalateDiet PDFVanessa Santos0% (1)
- Acute Abdominal Pain and Acute AppendicitisDocument8 paginiAcute Abdominal Pain and Acute AppendicitisdrtpkÎncă nu există evaluări
- LymphomaDocument15 paginiLymphomaVanessa SantosÎncă nu există evaluări
- GreekDocument7 paginiGreekVanessa SantosÎncă nu există evaluări
- FractureDocument58 paginiFractureVanessa SantosÎncă nu există evaluări
- AgingDocument9 paginiAgingVanessa SantosÎncă nu există evaluări
- 1º Energy FailureDocument1 pagină1º Energy FailureVanessa SantosÎncă nu există evaluări
- Adrenergic ReceptorsDocument6 paginiAdrenergic ReceptorsVanessa SantosÎncă nu există evaluări
- IMCIDocument57 paginiIMCIwyndzÎncă nu există evaluări
- CDPDocument9 paginiCDPVanessa SantosÎncă nu există evaluări
- Appl. Environ. Microbiol.-2011-Douglas-7365-71Document8 paginiAppl. Environ. Microbiol.-2011-Douglas-7365-71Nathan McCorkleÎncă nu există evaluări
- List+of+Greek+and+Latin+Roots+in+English+ +Wikipedia,+the+Free+EncyclopediaDocument46 paginiList+of+Greek+and+Latin+Roots+in+English+ +Wikipedia,+the+Free+EncyclopediaDyan SethupathiÎncă nu există evaluări
- 9700 m17 QP 22 PDFDocument16 pagini9700 m17 QP 22 PDFIG UnionÎncă nu există evaluări
- Application of Nanotechnology in PharmacyDocument13 paginiApplication of Nanotechnology in Pharmacykunasahu1Încă nu există evaluări
- Somatoform Disorder - DR - Ziad Arandi PowerpointDocument40 paginiSomatoform Disorder - DR - Ziad Arandi PowerpointNaji Z. ArandiÎncă nu există evaluări
- AlopeciaDocument10 paginiAlopeciaDr Vaishali MathapatiÎncă nu există evaluări
- Panayiotopoulos SyndromeDocument37 paginiPanayiotopoulos SyndromeZakaria MukallaÎncă nu există evaluări
- Amelogenesis Imperfecta Treatment Case ReviewDocument7 paginiAmelogenesis Imperfecta Treatment Case ReviewGeraldo LaurusÎncă nu există evaluări
- Legionella SPPDocument7 paginiLegionella SPPmtabatabaei20038889Încă nu există evaluări
- 9 JOHNSON BEHAVIOURAL SYSTEMfinalDocument11 pagini9 JOHNSON BEHAVIOURAL SYSTEMfinalRana VandanaÎncă nu există evaluări
- ArsenicDocument15 paginiArsenicIsabela PavălÎncă nu există evaluări
- CH 29Document39 paginiCH 29Jann Zaniel Allayne RiÎncă nu există evaluări
- Lactose Intolerance Pada AnakDocument11 paginiLactose Intolerance Pada AnakWilliam MakdinataÎncă nu există evaluări
- Bartonella in Benin 2016Document9 paginiBartonella in Benin 2016Yahya TfeilÎncă nu există evaluări
- HematDocument3 paginiHematMohit AbhyankarÎncă nu există evaluări
- Review: Lenat Joffe, Elena J LadasDocument11 paginiReview: Lenat Joffe, Elena J LadasGUSTAVO BELLOÎncă nu există evaluări
- 70791658786Document3 pagini70791658786gulcherrudisney259Încă nu există evaluări
- Public Speaking ScriptDocument2 paginiPublic Speaking Scriptsalbinarabi100% (1)
- Attention, Monotropism and Diagnosis Criteria For AutismDocument18 paginiAttention, Monotropism and Diagnosis Criteria For AutismyeyesÎncă nu există evaluări
- June 2016 (IAL) QP - Unit 3 Edexcel BiologyDocument16 paginiJune 2016 (IAL) QP - Unit 3 Edexcel BiologyRishita SinghÎncă nu există evaluări
- Biology Syllabus HSEBDocument2 paginiBiology Syllabus HSEBDipesh ShresthaÎncă nu există evaluări