Documente Academic
Documente Profesional
Documente Cultură
Clinical Trials, 6 Principles: N.B. Patients Must Now Give Written Consent Before Entering A Clinical Trial
Încărcat de
drsamnTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Clinical Trials, 6 Principles: N.B. Patients Must Now Give Written Consent Before Entering A Clinical Trial
Încărcat de
drsamnDrepturi de autor:
Formate disponibile
Clinical trials, 6 principles
1. Is the proposed treatment safe and therefore unlikely to bring harm to the patient ?
- no treatment is devoid of side effects and this must not be used to withold treatment
2. For the sake of a clinical trial can a Rx be ethically witheld from a patient. In other words can there be a control group on placebo treatment ? - mastectomy or not in Ca breast - antihypertensives vs control in raised BP
- analgesics in pain
If compared with 'standard' treatment, what is the standard? eg. morphine in postop pain, beta blockers in angina. 3. Can patients be randomly allocated to either treatment group ? - are exclusions going to alter the randomisation and therefore, will we end up with different groups where no comparison can be made ? - rigid definition of patient population before starting so that any patient can receive any treatment. This may involve restricting the age limits, health limits, sex and so on.
Randomisation ensures that local factors do not influence judgment as to effectiveness of treatment. 4. Is it necessary to obtain the patient's consent ? - some forms of treatment are more invasive than others in producing the same end result (until proven that the invasive treatment is better than the non-invasive) this exposes the patient to a greater risk, eg. epidural opioids vs systemic opioids for postop pain, CAVG for angina vs. medical treatment, SWIFT trial. - any discomfort that the patient may have, eg. repeated blood samples, lumbar punctures etc. must be explained. N.B. Patients must now give written consent before entering a clinical trial.
5. It is necessary to get ethical committee approval. The Royal college guidelines in the UK demand this approval. It will ensure that the guidelines presented by the MRC and the Declaration of Helsinki are observed, i.e. with reference to proper scientific observations, qualified practitioners conducting the trial, and so on.
6. There must be no bias on the part of the observer for or against one form of treatment. This usually necessitates the trial being double-blind, i.e. where neither the patient nor the doctor know which treatment is being undertaken. Obviously, there must be a randomisation code available should an untoward reaction occur, or, of course, for subsequent analysis of results. Some treatments, such as surgery cannot be carried out in this way. Assessment of results by an impartial observer is necessary, who, hopefully does not know what treatment the patient has received.
S-ar putea să vă placă și
- The Slim Book of Health Pearls: The Prevention of Medical ErrorsDe la EverandThe Slim Book of Health Pearls: The Prevention of Medical ErrorsÎncă nu există evaluări
- Clinicaltrialsbooklet WebDocument5 paginiClinicaltrialsbooklet Webzberger1087Încă nu există evaluări
- Preoperative Evaluation Guide for SurgeonsDocument65 paginiPreoperative Evaluation Guide for Surgeonsdr_trialÎncă nu există evaluări
- Situational Analysis - EthicsDocument2 paginiSituational Analysis - EthicsDeejune TorrinoÎncă nu există evaluări
- Prostate Cancer: 10. Palliative Care: Clinical BasicsDocument7 paginiProstate Cancer: 10. Palliative Care: Clinical Basicsdoriana-grayÎncă nu există evaluări
- Surgical Preoperative Assessment - What To Do and Why? Student BMJDocument3 paginiSurgical Preoperative Assessment - What To Do and Why? Student BMJEd FitzgeraldÎncă nu există evaluări
- Situational Analysis Lague, Inah Krizia O. BSN 2ADocument3 paginiSituational Analysis Lague, Inah Krizia O. BSN 2Ainah krizia lagueÎncă nu există evaluări
- OriginalDocument21 paginiOriginalavanir1012Încă nu există evaluări
- 508-Prowell-Final Slides5Document25 pagini508-Prowell-Final Slides5dfsdjgflksjgnawÎncă nu există evaluări
- Reversals of Established Medical Practices: Evidence To Abandon ShipDocument4 paginiReversals of Established Medical Practices: Evidence To Abandon ShipuoleoauÎncă nu există evaluări
- Coordinating FDA, CMS, and NIH processes can help prevent premature medical approvals and ensure evidence-based patient careDocument17 paginiCoordinating FDA, CMS, and NIH processes can help prevent premature medical approvals and ensure evidence-based patient careSpit FireÎncă nu există evaluări
- Clinical Trial Endpoints ExplainedDocument19 paginiClinical Trial Endpoints ExplainedSAURABH SINGHÎncă nu există evaluări
- Pregnancy Testing Prior To Anesthesia and SurgeryDocument4 paginiPregnancy Testing Prior To Anesthesia and SurgeryelliasÎncă nu există evaluări
- Management of Adult Pancreatic Injuries A Practice Management Guideline From The Eastern Association For The Surgery of Trauma.Document11 paginiManagement of Adult Pancreatic Injuries A Practice Management Guideline From The Eastern Association For The Surgery of Trauma.Madalina TalpauÎncă nu există evaluări
- 10 Commandments of ConsultationDocument4 pagini10 Commandments of ConsultationZlatan KurjakovicÎncă nu există evaluări
- Arguments for testing new drugs without consent: ethics vs accelerated developmentDocument1 paginăArguments for testing new drugs without consent: ethics vs accelerated developmentIftime VasileÎncă nu există evaluări
- What Are Clinical TrialsDocument6 paginiWhat Are Clinical TrialsutorrentÎncă nu există evaluări
- Pharmacist Contraception Prescriptions ExplainedDocument2 paginiPharmacist Contraception Prescriptions Explainedbillah jeptanuiÎncă nu există evaluări
- Review 20 - 03 - 20 - 001Document18 paginiReview 20 - 03 - 20 - 001Ulices QuintanaÎncă nu există evaluări
- Introduction To ClinicalDocument13 paginiIntroduction To ClinicalSuryaÎncă nu există evaluări
- Clinical TrialDocument26 paginiClinical TrialCandela NewtonÎncă nu există evaluări
- Pros and cons of experimental medicineDocument3 paginiPros and cons of experimental medicinekingfish1021Încă nu există evaluări
- Experimental (Or Interventional) Studies: ConfoundingDocument4 paginiExperimental (Or Interventional) Studies: ConfoundingRiza AlfianÎncă nu există evaluări
- Interview Question Clinical TrialsDocument20 paginiInterview Question Clinical Trialshruday100% (3)
- Sas 1 Cabahug, Victoria Mae IDocument5 paginiSas 1 Cabahug, Victoria Mae Ibekbekk cabahugÎncă nu există evaluări
- Phase Iii Trials: G.Arun JyothiDocument45 paginiPhase Iii Trials: G.Arun JyothiP meruguÎncă nu există evaluări
- Lorne Basskin - Practical PE ArticleDocument5 paginiLorne Basskin - Practical PE ArticleCatalina Dumitru0% (1)
- 3737s 03 NaderDocument13 pagini3737s 03 NaderSiddharth SikariaÎncă nu există evaluări
- Clinical TrialsDocument24 paginiClinical Trialsmahnoor fatimaÎncă nu există evaluări
- Clinical TrialDocument25 paginiClinical TrialHernawati Bagenda100% (1)
- Controlled Trial Methodology ChecklistDocument4 paginiControlled Trial Methodology ChecklistriiaayuÎncă nu există evaluări
- 00542-Nida CPDD ReportDocument24 pagini00542-Nida CPDD ReportlosangelesÎncă nu există evaluări
- Critical Appraisal: Prof. Dr. Mohammad Hakimi, Spog (K), PHDDocument37 paginiCritical Appraisal: Prof. Dr. Mohammad Hakimi, Spog (K), PHDFebbty KuswantiÎncă nu există evaluări
- Statins and OverDocument4 paginiStatins and Overlika_09Încă nu există evaluări
- Translet Farmakoterapi LanjutanDocument3 paginiTranslet Farmakoterapi LanjutanAlexander KwaitotaÎncă nu există evaluări
- Clinical Pharmacology For LUSUMA NotesDocument110 paginiClinical Pharmacology For LUSUMA NotesTausif Huq100% (1)
- Exercise Principles of HTA - DownloadDocument4 paginiExercise Principles of HTA - DownloadStavros TheodoridisÎncă nu există evaluări
- ComplianceDocument13 paginiCompliancextremist2001Încă nu există evaluări
- The Role of Physical Therapists in Patient CareDocument39 paginiThe Role of Physical Therapists in Patient Carepihabo3594Încă nu există evaluări
- CUI Texto Examen Multimedia Nivel 6 Curso BasicoDocument2 paginiCUI Texto Examen Multimedia Nivel 6 Curso BasicobertoniramiroÎncă nu există evaluări
- Compensation Guidelines COMMENTSDocument3 paginiCompensation Guidelines COMMENTSTarun BatraÎncă nu există evaluări
- Epidemiology Lec 9Document24 paginiEpidemiology Lec 9اسامة محمد السيد رمضانÎncă nu există evaluări
- Causality Assessment of Adverse Drug Reactions (ADR)Document21 paginiCausality Assessment of Adverse Drug Reactions (ADR)suhas reddy0% (1)
- Social Tract: Module OnDocument15 paginiSocial Tract: Module Onpschileshe9472Încă nu există evaluări
- Clinical Trials: What You Need To KnowDocument29 paginiClinical Trials: What You Need To KnowPadmitha Krishnakumar100% (1)
- Synthesis PaperDocument14 paginiSynthesis Paperapi-284053760Încă nu există evaluări
- Evidence-Based Laboratory Medicine: From Evidence to Best PracticeDocument14 paginiEvidence-Based Laboratory Medicine: From Evidence to Best PracticeatouyaÎncă nu există evaluări
- Towards Better Patient Care Drugs To Avoid in 2018Document9 paginiTowards Better Patient Care Drugs To Avoid in 2018Mabvan SarraÎncă nu există evaluări
- Adherence Evidence-Based - C BehrensDocument65 paginiAdherence Evidence-Based - C Behrensriena456Încă nu există evaluări
- Basic Adult Arv PDFDocument10 paginiBasic Adult Arv PDFpschileshe9472Încă nu există evaluări
- Protocols - Discussion 3Document2 paginiProtocols - Discussion 3api-633434674Încă nu există evaluări
- Clinical Trial - What We Need To KnowDocument28 paginiClinical Trial - What We Need To KnowRahadian Nugi SutrisnoÎncă nu există evaluări
- 1998 doukas AD oncology patient case studyDocument9 pagini1998 doukas AD oncology patient case studydrabellollinasÎncă nu există evaluări
- Post Marketing SurveillanceDocument15 paginiPost Marketing SurveillanceSundar Karuna100% (1)
- CR IntroDocument21 paginiCR Introsivaram_12213443Încă nu există evaluări
- Perioperative Laboratorytesting - The ClinicsDocument6 paginiPerioperative Laboratorytesting - The Clinicsapi-265532519Încă nu există evaluări
- Rational Prescribing & Prescription Writing: IntroductionDocument3 paginiRational Prescribing & Prescription Writing: IntroductionAnmol KudalÎncă nu există evaluări
- Rational Use of Drugs and Evidence Based Medicine: Department of Pharmacology NEIGRIHMS, ShillongDocument31 paginiRational Use of Drugs and Evidence Based Medicine: Department of Pharmacology NEIGRIHMS, Shillongdbrahma100% (1)
- Epidemiology Lecture 7mmDocument29 paginiEpidemiology Lecture 7mmSherif AliÎncă nu există evaluări
- Management and Legal Issues 1Document42 paginiManagement and Legal Issues 1Victor FabunmiÎncă nu există evaluări
- IELTS Speaking Criteria Public Version PDFDocument1 paginăIELTS Speaking Criteria Public Version PDFDiana Laura Durán Chablé100% (1)
- Simple EmergenciesDocument177 paginiSimple Emergenciesharsh89100% (1)
- Articles PracticalDocument4 paginiArticles PracticaldrsamnÎncă nu există evaluări
- Public Writing Band DescriptorsDocument2 paginiPublic Writing Band DescriptorsKaveh JalaliÎncă nu există evaluări
- Layers of Abdominal Wall When Performing An AppendicectomyDocument2 paginiLayers of Abdominal Wall When Performing An AppendicectomydrsamnÎncă nu există evaluări
- Common Antibiotic Questions and TopicsDocument2 paginiCommon Antibiotic Questions and TopicsdrsamnÎncă nu există evaluări
- Heart FailureDocument10 paginiHeart FailuredrsamnÎncă nu există evaluări
- Approaches To Management of Acute Pain 1Document22 paginiApproaches To Management of Acute Pain 1drsamnÎncă nu există evaluări
- Oxygen Therapy and Oxygen ToxicityDocument8 paginiOxygen Therapy and Oxygen ToxicitydrsamnÎncă nu există evaluări
- Acute Respiratory FailureDocument8 paginiAcute Respiratory FailureCayunk NorlianaÎncă nu există evaluări
- Arterial Blood Gases and Acid Base BalanceDocument12 paginiArterial Blood Gases and Acid Base BalancedrsamnÎncă nu există evaluări
- Science 2009-03-13Document112 paginiScience 2009-03-13drsamnÎncă nu există evaluări
- Airway, Drips and ECGDocument17 paginiAirway, Drips and ECGdrsamnÎncă nu există evaluări
- Skin As An Organizing Model: What Is It? (Anatomy)Document11 paginiSkin As An Organizing Model: What Is It? (Anatomy)Chemist Mary MouresÎncă nu există evaluări
- Head and NeckDocument11 paginiHead and NeckdrsamnÎncă nu există evaluări
- r4f Pastest MnemonicsDocument23 paginir4f Pastest MnemonicsplayuhzÎncă nu există evaluări
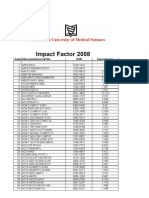
- Impact Factor 2008Document119 paginiImpact Factor 2008abood127Încă nu există evaluări
- Lab FaqsDocument384 paginiLab FaqsPriyanka SinghÎncă nu există evaluări
- Biology Under Construction - in Vitro Reconstitution of Cellular FunctionDocument8 paginiBiology Under Construction - in Vitro Reconstitution of Cellular FunctiondrsamnÎncă nu există evaluări
- MRCS1 2brochureDocument12 paginiMRCS1 2brochuredrsamn100% (2)
- Science 2009-01-30Document96 paginiScience 2009-01-30drsamnÎncă nu există evaluări
- Wound Repair and RegenerationDocument8 paginiWound Repair and RegenerationdrsamnÎncă nu există evaluări
- Revised Dyadic Adjustment Scale (RDAS) Relationship AssessmentDocument3 paginiRevised Dyadic Adjustment Scale (RDAS) Relationship AssessmentMihaelaLuca100% (1)
- Educational Status of Tribal Women Among Toda, Kota and Irula Tribal Communities of The Nilgiri District, Tamil Nadu, IndiaDocument4 paginiEducational Status of Tribal Women Among Toda, Kota and Irula Tribal Communities of The Nilgiri District, Tamil Nadu, IndiaarcherselevatorsÎncă nu există evaluări
- OM-Lecture 2 (Heritage & Productivity)Document22 paginiOM-Lecture 2 (Heritage & Productivity)Ismatullah ButtÎncă nu există evaluări
- D. G. Rupa D. G. Rupa D. G. Rupa D. G. Rupa D. G. Ruparrrrrel Colleg El Colleg El Colleg El Colleg El CollegeeeeeDocument48 paginiD. G. Rupa D. G. Rupa D. G. Rupa D. G. Rupa D. G. Ruparrrrrel Colleg El Colleg El Colleg El Colleg El Collegeeeeerah98Încă nu există evaluări
- Procedure For The Subject'S ReexaminationDocument2 paginiProcedure For The Subject'S ReexaminationMa Estrellene OrcalesÎncă nu există evaluări
- M.E. Qem FT & PTDocument63 paginiM.E. Qem FT & PTramasamy rÎncă nu există evaluări
- Synopsis MCDDocument7 paginiSynopsis MCDRupal KadiyanÎncă nu există evaluări
- Teacher's Speaking Strategies at Vocational High SchoolDocument18 paginiTeacher's Speaking Strategies at Vocational High SchoolKFÎncă nu există evaluări
- Sociology: Tension Between Science and Militant Activism?: Sandro SerpaDocument8 paginiSociology: Tension Between Science and Militant Activism?: Sandro SerpaHamza ButtÎncă nu există evaluări
- Differences in Perceptions of Training by Coaches and AthletesDocument5 paginiDifferences in Perceptions of Training by Coaches and AthletesPootrain ConductorÎncă nu există evaluări
- IT Strategic Plan PDFDocument8 paginiIT Strategic Plan PDFendeÎncă nu există evaluări
- Applied Optimal Control: Optimization, Estimation, and ControlDocument3 paginiApplied Optimal Control: Optimization, Estimation, and ControlisraelÎncă nu există evaluări
- Automatic Dismissal Alarm for Time AwarenessDocument54 paginiAutomatic Dismissal Alarm for Time AwarenessArnie John P. MendozaÎncă nu există evaluări
- IBM Big Data and Analytics PDFDocument24 paginiIBM Big Data and Analytics PDFSameer ParadkarÎncă nu există evaluări
- UNICEF WASH Officer Job ProfileDocument5 paginiUNICEF WASH Officer Job ProfileazizrbgÎncă nu există evaluări
- Chapter16 PDFDocument23 paginiChapter16 PDFAbdullah BingaziÎncă nu există evaluări
- Preferences and Positivist Methodology in EconomicsDocument21 paginiPreferences and Positivist Methodology in EconomicsAndrés GarcíaÎncă nu există evaluări
- Manoj Kumar M Project MB182357 PDFDocument79 paginiManoj Kumar M Project MB182357 PDFManoj KumarÎncă nu există evaluări
- Chapter#7 (Evaluation of Training)Document21 paginiChapter#7 (Evaluation of Training)Sadakalo ShopnooÎncă nu există evaluări
- Chemometrics and The Medieval Scriptorium LopesDocument1 paginăChemometrics and The Medieval Scriptorium LopesKita de AzevedoÎncă nu există evaluări
- Brownsville Learn Phase ReportDocument28 paginiBrownsville Learn Phase ReportJennifer LeeÎncă nu există evaluări
- Quality Management: Section 5Document3 paginiQuality Management: Section 5IberisÎncă nu există evaluări
- Ervin Laszlo Akashic Field PDFDocument2 paginiErvin Laszlo Akashic Field PDFBenjaminÎncă nu există evaluări
- Philadelphia City Council Resolution Condemning Academic Boycott of IsraelDocument4 paginiPhiladelphia City Council Resolution Condemning Academic Boycott of IsraelLegal InsurrectionÎncă nu există evaluări
- Disease Detectives NotesDocument5 paginiDisease Detectives NotesErica Weng0% (1)
- Content Writer ResumeDocument6 paginiContent Writer Resumekylopuluwob2100% (2)
- HOME LOANS OF HDFC BANK Research Report Finance 2017Document63 paginiHOME LOANS OF HDFC BANK Research Report Finance 2017GAGAN KANSALÎncă nu există evaluări
- TLN - Apa Citingexercise FullDocument4 paginiTLN - Apa Citingexercise FullBianca Denise Bagkus IledanÎncă nu există evaluări
- University of Health Sciences Lahore: Theory Date SheetDocument1 paginăUniversity of Health Sciences Lahore: Theory Date SheetNayabÎncă nu există evaluări
- Inquiries Investigations and Immersion LDocument3 paginiInquiries Investigations and Immersion LJovel PaycanaÎncă nu există evaluări