Documente Academic
Documente Profesional
Documente Cultură
Screening For Delirium in An Adult Intensive Care Unit: Brigit Roberts
Încărcat de
Carmem SilvaDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Screening For Delirium in An Adult Intensive Care Unit: Brigit Roberts
Încărcat de
Carmem SilvaDrepturi de autor:
Formate disponibile
Intensive and Critical Care Nursing (2004) 20, 206213
ORIGINAL ARTICLE
Screening for delirium in an adult intensive care unit
Brigit Roberts*
Department of Intensive Care, 4th Floor G Block, Sir Charles Gairdner Hospital, Hospital Avenue, Nedlands, WA 6009, Australia
Accepted 6 April 2004
KEYWORDS
Delirium; Intensive care; Screening; Implication
Summary Delirium is an acute, reversible disorder of attention and cognition and may be viewed as cerebral dysfunction similar to the failure of any other organ. The development of delirium is associated with increased morbidity and mortality, extended length-of-stay in the intensive care unit and longer time spent sedated and ventilated. Nearly every clinical, pharmacological and environmental factor present and necessary in the ICU setting has the potential to cause delirium. Since all of these factors cannot be removed, it is paramount to increase the awareness amongst health care professionals so as to minimise under-recognition and encourage future research into factors that may improve the long-term outcome for ICU patients. There is a need for user-friendly, validated assessment tools for the intubated and ventilated ICU patient, which can be applied at the time of ICU admission without the need for lengthy psychiatric assessment. Nursing professionals are at the forefront of those who are able to provide holistic care through meaningful conversation and empathetic touch. A 6-month Quality Improvement (QI) project screening patients for signs of delirium provided a foundation for discussion. All patients admitted to ICU for more than 72 h, with a hospital length-of-stay less than 96 h prior to ICU admission were screened. Patients admitted following neurological insults or with pre-existing altered mental state were excluded. The QI project showed the incidence of delirium to be 40% of the total sample (n = 73) in a mixed medical/surgical and elective/emergency patient population. 2004 Elsevier Ltd. All rights reserved.
Background
Until recently only little emphasis has been placed on the close monitoring of brain function in intensive care unit (ICU) patients. Conversely, most organs such as the pulmonary and cardiovascular
*Tel.: +61-8-9346-1010; fax: +61-8-9346-4431. E-mail address: brigit.roberts@health.wa.gov.au (B. Roberts).
systems are continuously and rigorously observed in the ICU, in order to detect any early changes and deterioration in the patients condition. The incidence and outcome of ICU delirium is now gaining increasing interest in the literature. Delirium is an acute, uctuating, reversible disorder of attention and cognition or an altered level of consciousness (Roberts, 2001). The development of delirium in the ICU is associated with an underlying medical condition, such as sepsis, hypoxaemia or metabolic disturbances (Cardy and
0964-3397/$ see front matter 2004 Elsevier Ltd. All rights reserved. doi:10.1016/j.iccn.2004.04.003
Screening for delirium in an adult intensivecare unit Matta, 1997; Haskell et al., 1997). The causes of delirium are multi-factorial and often divided into three categories (Ely et al., 2001b). Firstly, advanced age, underlying primary cerebral illnesses (e.g. dementia or substance abuse) and chronic illnesses (e.g. cardiovascular, metabolic, respiratory and renal) increase the risk for developing delirium (Dubois et al., 2001). Secondly, pharmacological agents appear to be a critical element in the aetiology of delirium and although almost any drug can precipitate the development of delirium, certain classes of drugs such as opioids, anticholinergic agents and benzodiazepines are more commonly implicated (Adis International Limited, 1997; Easton and MacKenzie, 1988). Thirdly, environmental factors may also play a part in the disease process and add to the cerebral dysfunction. Sleep disruption, noise, pain, sensory overload and ineffective communication are examples of the special environment that may predispose patients to the development of delirium in ICU (Justic, 2000). There are three manifestations of delirium, the hyperactive or agitated patients, who may experience visual hallucinations and whose behaviour may be agitated or even bizarre and out of character. This may be frightening and disturbing for both patients and their relatives (Roberts, 2001). Patients may think that they are going crazy and worry that they will be labelled psychiatrically unstable, whilst relatives may be bewildered at seeing their loved ones acting in a bizarre and at times obnoxious manner (Blacher, 1997). In contrast, patients may display hypoactivity or lethargy, which often will go unnoticed because the patients appear not to pose difculties in their clinical management (Laitinen, 1996). The third manifestation is a combination of hyperand hypoactivity. In all three variants, patients symptoms will usually uctuate between lucid and disturbed periods over the course of a day. Whether patients display delirious manifestations or not they may nevertheless experience vivid dreams or suffer from delusions and hallucinations that are often persecutory in nature (Rundshagen et al., 2002). The reported incidences of ICU delirium vary greatly from 16% up to 85% of patients observed to be affected (Bergeron et al., 2001; Jacobson and Schreibman, 1997; Truman and Ely, 2003). Traditional psychiatric evaluation of the sedated and ventilated ICU patient is difcult (Bergeron et al., 2002). A number of assessment tools have been evaluated in the non-ICU population. These tools rely on verbal interaction and/or lengthy professional consultation with the patients and are there-
207 fore not suitable for the ICU population (Breibart et al., 1997; Trzepacz et al., 1988). Some tests only provide a snapshot of the patients real condition because of uctuating symptoms, whereas testing is performed at a specic time (Robertsson, 1999). Hence, the results depend on the period of assessment. Different screening tools emphasise various aspect of delirium (Skrobik, 2003). The Intensive Care Delirium Screening Checklist (ICDSC) focuses on thought content whereas the Confusion Assessment Method-ICU (CAM-ICU) concentrates on arousal and thus may be inuenced by factors such as variation in administration of sedation, which may cause uctuation in levels of consciousness. Bergeron et al. (2001, 2002) were using the ICDSC and reported the incidence of delirium between 16 and 19% in a mixed medical/surgical ICU population with mean APACHE II scores of 14 and 15. In contrast, when Ely et al. (2001a,c) used the CAM-ICU they reported the incidence of delirium at 87 and 83%, respectively, in a medical ICU patient population with a mean APACHE II score of 19. These gures are likely to rise even further with the current trend for older patients with more complex co-morbidity to be admitted to ICUs and offered increasingly sophisticated treatment modalities (McNicoll et al., 2003; St Pierre, 1996). The length of ICU stay may also inuence delirium incidence with patients staying less than 24 h reporting fewer hallucination events (8%) than patients remaining in excess of 24 h (38%) (Rundshagen et al., 2002). Psychiatrists are rarely involved in ICU care, yet research has shown that ICU patients who would be diagnosed as delirious by a psychiatrist remain undiagnosed by the ICU nursing and medical staff in up to 70% of cases (Eden and Foreman, 1996; Truman and Ely, 2003). Although previously thought to be benign, it is now recognised that the development of delirium in ICU is associated with a 1560% increase in morbidity and mortality (McCusker et al., 2002; McGuire et al., 2000). ICU and hospital length-of-stay (LOS) are prolonged and there is a higher requirement for nursing care together with a greater likelihood of the delirious patient being institutionalised after discharge (Geary, 1994; Inaba-Roland and Maricle, 1992). The agitated patient is at risk of removing life-preserving devices such as endotracheal tubes and indwelling catheters, whereas the lethargic patient is prone to the development of decubitus ulcers and nosocomial pneumonia (Ely et al., 2001b). While most ICU health care professionals can identify when a patient becomes agitated, confused and irrational, diagnosing the lethargic patient as delirious is difcult. Failure by health professionals to
208 recognise the developing signs of delirium may have an adverse effect on long-term outcomes and therefore a comprehensive nursing assessment should be started at admission (Justic, 2000).
B. Roberts
Patient delirium assessment
At the time of this project (January 2001July 2001) no ICU-specic delirium assessment tools existed, and as previously stated, the existing generic delirium tools were unable to be applied to ICU patients. Therefore, based on subjective measurements the researcher performed daily direct patient observations and review of the nursing and medical notes, using a framework grounded in the literature. The researcher noted signs of agitation (e.g. plucking in the air or catching non-existing objects), patients ability to concentrate and follow commands, and general behaviour such as restlessness and sleep/wake disturbances. Similarly assessment of patients with psychomotor slowing/retardation (e.g. staring into the room and lack of response to stimuli in the absence of sedatives) were recorded. Patients displaying either agitation or psychomotor slowing were classied as delirious and patients with none of the above symptoms were ranked as non-delirious.
Denitions
Hallucination
Trying to catch a non-existing object; seeing a non-existing object (Bergeron et al., 2001).
Delusion
Refusing medication or treatment due to fear of being harmed; believing he/she is being mistreated by secret enemies.
Quality Improvement project
To increase the awareness of delirium in the ICU setting amongst health care professionals the author conducted a prospective Quality Improvement (QI) project. The objective of a QI project is to establish the performance of quality care in an institution by identication of issues or problems; collection and assessment of information about important aspects of care and service provided; implementation of actions to improve standards of care; and measurement of outcomes (Western Australian Consolidated Legislation, Western Australian Health Services Act, 1994). The QI project was chosen as a pilot study with a view to establish the incidence and outcome of delirium in an 18-bed tertiary Australian ICU. This unit admits in excess of 1300 general medical and surgical adult patients per year.
Other data
Demographic data including gender, age, admission category (emergency/elective), and the Acute Physiology and Chronic Health Evaluation II (APACHE II) score (Knaus et al., 1985) were collected on admission. ICU and hospital LOS and outcome were also recorded.
Patient characteristics
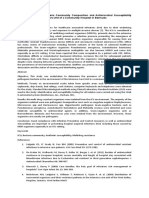
The total number of ICU admissions for the 6-month period was 632 patients. Fig. 1 describes the tracking of patients included in the sample, the frequency of delirium and reasons for exclusion in the nal sample. The major reason for exclusion was short-term (<72 h) ICU stay, e.g., post-operative patients, but other reasons such as prolonged hospital stay prior to ICU admission and brain trauma were also noted. There were 44 emergency admissions and 29 elective admissions in the nal sample (n = 73). The QI project identied 29 (40%) patients who showed signs of delirium and 44 (60%) patients without signs of delirium. Table 1 displays demographic and clinical data of the patient sample. There was a wide range of ages represented in both the delirious and non-delirious groups. The disproportion between male and female in both groups reects the overall ICU population in this particular unit. ICU and hospital length-of-stay was similar for the two
Framework of quality improvement assessment
The researcher screened all ICU patients admitted for more than 72 h over a 6-month period. The 72-h time frame was chosen to exclude routine post-operative patients (Granberg et al., 1998). Individuals who had a hospital LOS greater than 96 h prior to ICU admission were excluded in order to ensure that the observed behaviour was a result of the ICU admission and not caused by prolonged prior hospital admission. Likewise, those admitted following neurological insults or pre-existing altered mental state were also excluded.
Screening for delirium in an adult intensivecare unit
209
Total number of all ICU admissions 632
Patients excluded
Patients included
ICU LOS <72 hours 485
Hospital admission >92 hours prior to ICU admission 30
Patients excluded due to brain insult 44
Number of patients in survey 73
Patient showing signs of Delirium 29 (40%)
Patients without signs of delirium 44 (60%)
Figure 1
Track of patients included in QI project.
Table 1 Demographic data.
Characteristics Age, mean (range) Gender, n = male/female ICU death, n (%) Hospital death, n (%) APACHE II, mean (range) Medical/emergency surgical/elective surgical admissions (n) ICU LOS days, mean (range) Hospital LOS days, mean (range) Delirious (n = 29) (40%) 58 (1783) 22/7 0 (0) 2 (7) 16 (234) 14/5/10 9 (236) 25 (456) Non-delirious (n = 44) (60%) 62 (1684) 26/18 8 (18) 6 (14) 16 (238) 24/1/19 8 (233) 23 (380)
groups and notably fewer patients displaying signs of delirium died in ICU.
Discussion
The reports in the professional literature of a high incidence of delirium in ICU, the frequency of under-recognition and the associated poor outcome demand that much more effort go into gaining further knowledge and understanding of the phenomenon. We must be able to provide the best care for patients both physically, psychologically and emotionally, show empathy to the relatives and offer support and treatment options for our colleagues. The agitated and restless patient can be difcult to care for and many healthcare professionals
approach the patient with trepidation. The patient may be termed cantankerous and health professionals may become angry and frustrated with the patient. On the other hand, the patient, Russell (1999) suggests, who lies still in bed and does not attempt any eye contact or movement, is easily overlooked whilst more acute treatment pre-occupies carers. Health professionals may be unable to identify delirium in such patients due to a lack of understanding of the complexity of delirium. Tanios et al. (2004) comment that the inadequacy of delirium monitoring in ICU may reect the absence of proven preventative or therapy modalities except in severe cases. They conclude that there is a strong case for delirium monitoring once effective interventions are in place. It must be ascertained as part of a holistic assessment whether the patient is suffering from delir-
210 ium with hallucinatory and delusional thoughts or whether there are other reasons for the patients behaviour such as pain; frustration due to an inability to communicate effectively; fear of unfamiliar surroundings and procedures; or lack of external stimuli.
B. Roberts ing a medical condition appear to have a higher risk of developing delirium than less sick surgical patients. Medical ICU patients are known to be amongst the sickest in the hospital system, with complex co-morbidities and poly-pharmacological treatments (Ely et al., 2001b).
Incidence
The great variation in the reported rates of delirium incidence in the literature may relate to differing patient case-mix and acuity between ICUs. Emergency ICU admissions usually require multiple pharmacological agents and invasive therapy such as renal replacement therapy and prolonged mechanical ventilation. In contrast, units which predominantly admit elective surgical patients may have a lower rate of delirium. This QI project found the incidence of delirium in the sample to be 40% (n = 29), two thirds of whom were emergency admissions with an average APACHE II score of 16. This falls within previously reported levels (1085%) and characteristics reported in the literature. Bergeron et al. (2001) described a 16% incidence of delirium in a group of patients (n = 93) with a mean APACHE II score 14 and of whom 53% were medical admissions. Aldemir et al. (2001) showed delirium to occur in 11% in a sample of solely surgical admissions, in particular male emergency admission, but he did not dene the sample acuity. Dubois et al. (2001) found delirium in 19% of patients (n = 198), 16% of whom were medical, and 23% surgical admissions, with an average APACHE II score of 15. In contrast, two studies by Ely et al. (2001a,c) (n = 96 and 38, respectively) found the incidence of delirium to be in the mid-eighties percentile. Both studies were conducted in only medical admissions and the mean APACHE II score was 23 in the rst study and 17 in the second. Granberg et al. (2002) found in a study of 19 patients with a mean TISS score of 34 that 74% (n = 19) developed delirium of whom 43% (n = 6) suffered severe delirium. The ndings from these studies have been summarised in Table 2. It seems that patients with higher acuity and suffer-
Under-recognition
Delirium in the ICU remains an under-recognised syndrome and early recognition of signs and symptoms could reduce the associated morbidity and mortality (Justic, 2000; Rabinowitz, 2002). In a study of non-ICU patients (n = 797), Inouye et al. (2001) reported that nurses failed to recognise delirium in 69% (n = 91) of the cases (n = 131) noted by the researcher. They identied four risk factors for under-recognition of delirium as (1) patients displaying the hypoactive variant of delirium, (2) advanced age, (3) vision impairment and (4) dementia. Eden and Foreman (1996) echoed these ndings in a case study where only 50% of critical care nurses interviewed were able to recognise the changes in mental state associated with the development of delirium. Furthermore the nurses reported frustration and difculties with medical staff being reluctant to act on the reported symptoms. Armstrong et al. (1997) cited 69% of delirium misdiagnosis in the ICU setting versus 41% in general wards. They concluded that agitated behaviour in ICU was so common that health professionals perceived it to be normal ICU behaviour. In a recent study by Ely et al. (2004) most healthcare professionals considered ICU delirium a very serious problem, yet 78% of study participants acknowledged that delirium was an under-diagnosed syndrome. Information about the pre-morbid mental state of the ICU patient is often scant and health professionals must frequently rely on relatives for assessment of precipitating factors for the development of delirium (Roberts, 2001). Formal assessment skills and lectures about delirium should not only be part of the post-graduate ICU courses but
Table 2 Summary of publications on incidence of delirium in ICU.
Authors The researcher Bergeron et al. (2001) Aldemir et al. (2001) Dubois et al. (2001) Granberg et al. (2002) Ely et al. (2001a) Ely et al. (2001c) Incidence of delirium (%) 40 16 11 19 74 83 87 Number of participants (n) 73 93 818 198 19 96 38 APACHE II 16 14 Not recorded 15 TISS 34 23 17
Screening for delirium in an adult intensivecare unit taught at under-graduate level to both nursing and medical students.
211 setting and also validated in two studies (n = 93) and (n = 216) (Bergeron et al., 2001; Dubois et al., 2001). Ely et al. (2004) reported on a survey of 912 participants (ICU medical staff (n = 753) and ICU allied health professionals (n = 159)) only 40% (n = 365) routinely screened for delirium. Only 16% (n = 58 of 365) reported use of a formal assessment tool, and of these only 7% (n = 4 of 58) used an ICU-specic screening tool. It must nevertheless be noted that the survey period fell at the same time as the above mentioned ICU-specic screening tools were rst published. This would have been a strong factor in the infrequent use of such a tool. The QI project was limited in that no formal assessment tools were available for use as neither of the subsequent studies validating ICU-specic tools had been published at the time of conducting the delirium assessment project. Although formal tools were not used, validity and reliability were promoted through the use of a single rater for all patients, who was an experienced ICU nurse and had thoroughly reviewed the literature pertaining to ICU delirium and delirium diagnostic criteria, including existing generic screening tools. The project is now being repeated as a study in a multi-centre ICU population using an ICU validated tool.
Diagnosis of delirium
There are many different terms for delirium. Some professionals refer to delirium as Acute Confusional State (Lipowski, 1987), ICU syndrome (Granberg et al., 1998) and some use the term ICU Psychosis (Easton and MacKenzie, 1988; Justic, 2000). There is a need for standardised terminology and most researchers today use the term delirium as dened in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (American Psychiatric Association, 1994) to avoid confusion, minimise under-recognition and enhance further research. ICU-specic delirium assessment tools are necessary. Conventional tools rely on verbal interaction between the patient and the assessor, and in addition, the assessment is often very time consuming. Most patients in ICU are intubated and ventilated and their movement often restricted by catheters and tubes. The physical care of patients seldom allows time for lengthy psychological assessment in the daily routine, nor are ICU health professionals generally given formal mental assessment training. Ely et al. (2001c) comment that our knowledge regarding the clinical signicance of delirium in the ICU is limited by the fact that few investigations have included mechanically ventilated patients in their delirium studies. Ely et al. (2001b) continue that oxygenation, blood pressure and a myriad of other physiological factors are aggressively monitored, yet the scales to monitor the development of delirium remain crude and poorly validated. Two objective tools have been developed to detect delirium specically in the ventilated and sedated patient, the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) (Ely et al., 2001a,c) and the Intensive Care Delirium Screening Checklist (Bergeron et al., 2001). The CAM-ICU is a modication of the Confusion Assessment Method (Inouye et al., 1990) adapted to the ICU setting so that it does not require patient verbalisation. Both tools are based on the DSM IV (1994) criteria for delirium, and can quickly and easily be applied by ICU health professionals without formal psychiatric training to screen ICU patients, even when patient communication is compromised. In two studies with 38 and 116 participants the CAM-ICU was shown to be reliable and valid for diagnosing delirium in ICU patients (Ely et al., 2001a,c). The Intensive Care Delirium Screening Checklist ICDSC is a checklist of eight items and likewise was found to be easily applied to the ICU
Nursing implications
The frequent occurrence of delirium in ICU and increasing knowledge of its consequences should make the use of a validated screening tool compulsory in daily patient assessment. This may help early detection of ICU delirium and as a result facilitate appropriate intervention to reduce this phenomenon. Nursing staff are often the rst to recognise subtle changes in the patients mental state in their daily round-the-clock care of the patients (Roberts, 2001). They need to understand and recognise the symptoms, assess patients, and alleviate the stress that patients may suffer from this experience in order to minimise adverse events. This may avoid a prolonged ICU or hospital stay, possible detrimental psychological sequelae or even a fatal outcome. Validated ICU-specic delirium screening tools should become mandatory in the routine care and ongoing assessment of the ICU patient and ICU health professionals need to monitor for patients who require ongoing psychological counselling. Further research and exploration into optimal ICU screening tools are warranted (Ely et al., 2004) as well as promoting their uses in the clinical setting. The causes of delirium are multi-factorial and much emphasis has been placed on the ICU environ-
212 ment. Whilst it may not elude the development of delirium it is important as far as possible to maintain a daynight cycle, re-orientate the patient to time and place, allow the patient time to rest and reduce excessive noise and light especially at night time (Geary, 1994). More important may be consideration of empathetic communication and touch (Russell, 1999), maintenance of patients dignity both personally and spiritually (Halm and Alpen, 1993; Todres et al., 2000), and adequate pain control (Szokol and Vender, 2001). Patients interviews after ICU discharge in Russells (1999) study revealed a high degree of anxiety and psychological problems even after 6 months. This was particularly related to poor communication between staff and patients. The professional literature is now focusing on the long-term sequelae of the ICU admission, with delirium sometimes linked to post-traumatic stress disorder (Jones et al., 2001; Rotondi et al., 2002; Rundshagen et al., 2002; Schelling et al., 1998). Through teaching and staff orientation we must change the attitude of ICU health professionals away from a preoccupation with the physical aspects of the ICU patient, however, important these may be (Tanios et al., 2004). We must learn to think of the patient in a holistic manner and to provide dignity during daily care such as bed baths and heed the need for privacy when possible. We must offer communication of relevance to the patient other than explanation of procedures but rather talk about their loved ones and hold the patients hand with empathy and care not merely to avoid them pulling out tubes. The uncharacteristic behaviour these patients display may also have a profound impact on the relatives, when their beloved one acts aggressively or anxiously, is abusive, or lies lethargically in the bed (Blacher, 1997; Geary, 1994; Roberts, 2001). Nurses will often be the rst to broach and discuss this phenomenon with the relatives and it is important that the relatives understand that the condition is reversible and that we, as health professionals, understand that this is not the patients normal behaviour. Nursing care should focus on managing the stressors that can be alleviated such as sleep deprivation and level of noise whilst simultaneously assisting the patients to cope with the factors that cannot be eliminated such as anxiety and immobilisation.
B. Roberts gaining more awareness in both the nursing and medical communities. At the same time all steps must be taken to minimise the associated rise in morbidity and mortality. ICU patients are generally difcult to assess for delirium due to the administration of psychoactive drugs and an inability to speak due to endotracheal tubes and other restraining treatment modalities. The high incidence of delirium in ICU warrants further exploration of the development of user-friendly and validated assessment tools. This QI project found the incidence of delirium within the limits of that reported in the literature despite the small sample size and the absence of a formally validated ICU delirium assessment tool. This project provides a foundation for the further evaluation of patients subjective experiences of their ICU stay in order for ICU health professionals to provide holistic, quality care for patients.
Acknowledgements
The author wishes to thank Claire Rickard, Monash University School of Rural Health and Latrobe Regional Hospital, Traralgon, Australia for her revision of and input into this article.
References
Adis International Limited. Drug-induced delirium: diagnosis, management, and prevention. Drugs Ther Perspect 1997;10(3):59. Aldemir M, Ozen S, Kara IH, Sir A, Bac B. Predisposing factors for delirium in the surgical intensive care unit. Crit Care 2001;5:26570. American Psychiatric Association. Diagnostic and statistical manual of mental disorders: fourth edition (DSM IV). Washington DC: American Psychiatric Association; 1994. Armstrong SC, Cozza KL, Watanabe KS. The misdiagnosis of delirium. Psychosomatics 1997;38:4339. Bergeron N, Dubois M-J, Dumont M, Dial S, Skrobik Y. Intensive care delirium screening checklist: evaluation of a new screening tool. Intensive Care Med 2001;27:85964. Bergeron N, Skrobik Y, Dubois MJ. Delirium in critically ill patients. Crit Care 2002;6(3):1812. Blacher RS. The psychological and psychiatric consequences of the ICU stay. Eur J Anaesthesiol 1997;14(Suppl 15):457. Breibart W, Rosenfeld B, Roth A, Smith MJ, Cohen K, Passik S. The Memorial Delirium Assessment Scale. J Pain Symptoms Manage 1997;13:12837. Cardy J, Matta B. Brain failure. Curr Opin Crit Care 1997;3: 2738. Dubois M, Bergeron N, Dumont M, Dial S, Skrobik Y. Delirium in an intensive care unit: a study of risk factors. Intensive Care Med 2001;27:1297304. Easton C, MacKenzie F. Delirium in the ICU. Heart Lung 1988;17:22937. Eden BM, Foreman MD. Problems associated with underrecognition of delirium in critical care: a case study. Heart Lung 1996;25(5):388400.
Conclusion
The incidence and circumstances of the development of delirium are becoming increasingly important in the management of ICU patients, and are
Screening for delirium in an adult intensivecare unit
Ely EW, Inouye SK, Bernard GR, Francis J, May L, Truman B, et al. Delirium in mechanically ventilated patients. JAMA 2001a;286(21):270310. Ely EW, Siegel MD, Inouye SK. Delirium in the intensive care unit: an under-recognized syndrome of organ dysfunction. Semin Respir Crit Care Med 2001b;22(2):115 26. Ely EW, Margolin R, Francis J, May L, Truman B, Dittus R, et al. Evaluation of delirium in critically ill patients: validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). Crit Care Med 2001c;29(7):13709. Ely EW, Stephens RK, Jackson JC, Thomason JWW, Truman B, Gordon S, et al. Current opinions regarding the importance, diagnosis, and management of delirium in the intensive care unit: a survey of 912 healthcare professionals. Crit Care Med 2004;32(1):10612. Geary SM. Intensive care unit psychosis revisited: Understanding and managing delirium in the critically care setting. Crit Care Nurse Q 1994;17(1):5163. Granberg A, Bergbom Engberg I, Lundberg D. Patients experience of being critically ill or severely injured and cared for in an intensive care unit in relation to the ICU syndrome. Part I. Intensive Crit Care Nursing 1998;14:294 307. Granberg AIR, Malmros CW, Bergbom IL, Lundberg DBA. Intensive care unit syndrome/delirium is associated with anemia, drug therapy and duration of ventilatory treatment. Acta Anaesthesiol Scand 2002;46:72631. Halm MA, Alpen MA. The impact of technology on patients and families. Nurs Clin N Am 1993;28(2):44357. Haskell RM, Frankel HL, Rotondi MF. Agitation. AACN Clin Issues 1997;8(3):33550. Inaba-Roland KE, Maricle RA. Assessing delirium in the acute care setting. Heart Lung 1992;21(1):4855. Inouye SK, Foreman MD, Mion LC, Katz KH, Cooney Jr LM. Nurses recognition of delirium and its symptoms: comparison of nurse and researcher ratings. Arch Intern Med 2001;161(20):246773. Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the Confusion Assessment Method. A new method for detection of delirium. Ann Intern Med 1990;113:9418. Jacobson S, Schreibman B. Behavioral and pharmacologic treatment of delirium. Am Fam Physician 1997;56(8):2005 12. Jones C, Grifth RD, Humphries G, Skirrow PM. Memory, delusions, and the development of acute posttraumatic stress disorder-related symptoms after intensive care. Crit Care Med 2001;29(3):57380. Justic M. Does ICU psychosis really exist? Crit Care Nurse 2000;20(3):2837. Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classication system. Crit Care Med 1985;13:81829.
213
Laitinen H. Patients experience of confusion in the intensive care unit following cardiac surgery, Intensive. Intensive Crit Care Nurs 1996;12(2):7983. Lipowski ZJ. Delirium (acute confusional states). JAMA 1987;258:178992. McCusker J, Cole M, Abrahamowicz M, Primeau F, Belzile E. Delirium predicts 12-month mortality. Arch Intern Med 2002;162(4):45763. McGuire BE, Basten CJ, Ryan CJ, Gallagher J. Intensive care unit syndrome. A dangerous misnomer. Arch Intern Med 2000;160:9069. McNicoll L, Pisani MA, Zhang Y, Ely EW, Siegel MD, Inouye SK. Delirium in the intensive care unit: occurrence and clinical course in older patients. J Am Geriatr Soc 2003;51(5):5918. Rabinowitz T. Delirium: an important (but often unrecognized) clinical syndrome. Curr Psychiatry Rep 2002;4(3):2028. Roberts BL. Managing delirium in adult intensive care patients. Crit Care Nurse 2001;21(1):4855. Robertsson B. Assessment scales in delirium. Dement Geriatr Cogn Disord 1999;10:36879. Rotondi AJ, Chelluri L, Sirio C, Mendelsohn A, Schulz R, Belle S, et al. Patients recollections of stressful experiences while receiving prolonged mechanical ventilation in an intensive care unit. Crit Care Med 2002;30(4):74652. Rundshagen I, Schnabel K, Wegner C, Schulte am Esch J. Incidence of recall, nightmares, and hallucinations during analgosedation in intensive care. Intensive Care Med 2002;28:3843. Russell S. An exploratory study of patients perceptions, memories and experiences of an intensive care unit. J Adv Nurs 1999;29(4):78391. Schelling G, Stoll C, Haller M, Briegel J, Manert W, Hummel T, et al. Health-raleated quality of life and posttraumatic stress disorder in survivors of the acute respiratory distress syndrome. Crit Care Med 1998;26(4):6519. Skrobik Y. An overview of delirium in the critical care setting, Geriatrics. Geriatr Aging 2003;6(10):305. St Pierre J. Delirium in hospitatlized elderly patients: off track. Crit Care Clin N Am 1996;8(1):5360. Szokol JW, Vender JS. Anxiety, delirium, and pain in the intensive care unit. Crit Care Clin 2001;17(4):82142. Tanios MA, Epstein SK, Teres D. Are we ready to monitor for delirium in the intensive care unit? Crit Care Med 2004;32(1):2956. Todres L, Fullbrook P, Albarran J. On the receiving end: a hermeneutic-phenomenological analysis of a patients struggle to cope while going through intensive care. Nurs Crit Care 2000;5(6):27787. Truman B, Ely EW. Monitoring delirium in critically ill patients. Crit Care Nurse 2003;23(2):2538. Trzepacz PT, Baker RW, Greenhouse J. A symptom rating scale for delirium. Psychiatr Res 1988;23:8997. Western Australian Health Services (Quality Improvement) Act 1994. Western Australian Consolidated Legislation.
S-ar putea să vă placă și
- Critical Care Study Guide: Text and ReviewDe la EverandCritical Care Study Guide: Text and ReviewGerard J. CrinerÎncă nu există evaluări
- Delirium in The Intensive Care Unit: ReviewDocument9 paginiDelirium in The Intensive Care Unit: ReviewCristopher Castro RdÎncă nu există evaluări
- Int J Geriat Psychiatry - 2017 - Velthuijsen - Detection and Management of Hyperactive and Hypoactive Delirium in OlderDocument9 paginiInt J Geriat Psychiatry - 2017 - Velthuijsen - Detection and Management of Hyperactive and Hypoactive Delirium in OlderAntonieta Cuevas GarcinuñoÎncă nu există evaluări
- PrognosisDocument9 paginiPrognosisKarinaWijayantiÎncă nu există evaluări
- Delirium - A Common Condition Associated With Negative Outcome in The ElderlyDocument8 paginiDelirium - A Common Condition Associated With Negative Outcome in The ElderlyVika RatuÎncă nu există evaluări
- Icu Delirium Final PaperDocument12 paginiIcu Delirium Final Paperapi-348346538Încă nu există evaluări
- DeliriumDocument15 paginiDeliriumRobin gruÎncă nu există evaluări
- Differentiation of Delirium, Dementia and Delirium Superimposed On Dementia in The Older Person-2018Document5 paginiDifferentiation of Delirium, Dementia and Delirium Superimposed On Dementia in The Older Person-2018Juan Paredes100% (1)
- Sedation, Delirium, and Cognitive Function After Criticall IlnessDocument14 paginiSedation, Delirium, and Cognitive Function After Criticall IlnessPsiquiatría CESAMEÎncă nu există evaluări
- Delirium in The Intensive Care UnitDocument9 paginiDelirium in The Intensive Care Uniton miniÎncă nu există evaluări
- HHS Public AccessDocument17 paginiHHS Public AccessChika SabaÎncă nu există evaluări
- Alteraciones Adultos MayoresDocument12 paginiAlteraciones Adultos MayoresGabriel Zúñiga MartinezÎncă nu există evaluări
- Nur 111 Session 20 Sas 1Document6 paginiNur 111 Session 20 Sas 1Zzimply Tri Sha UmaliÎncă nu există evaluări
- Critical CareDocument7 paginiCritical CareOanamikaela VaidaÎncă nu există evaluări
- CC 12736Document8 paginiCC 12736Neneng HumairohÎncă nu există evaluări
- SdarticleDocument16 paginiSdarticleHerbert Baquerizo VargasÎncă nu există evaluări
- Car Gade Delirium e Nuc IDocument20 paginiCar Gade Delirium e Nuc INataly Audrey Romero DiazÎncă nu există evaluări
- Physical Restraint Use in Adult Patients Presenting To A General Emergency DepartmentDocument10 paginiPhysical Restraint Use in Adult Patients Presenting To A General Emergency DepartmentBeatrizÎncă nu există evaluări
- Kid 0004662020Document8 paginiKid 0004662020Rian KurniawanÎncă nu există evaluări
- Cost MGT of DizzinessDocument6 paginiCost MGT of Dizzinesszappo7919Încă nu există evaluări
- A Clinical Update On Delirium: From Early Recognition To Effective ManagementDocument13 paginiA Clinical Update On Delirium: From Early Recognition To Effective ManagementNabila MarsaÎncă nu există evaluări
- MCQ Anaesthesia QuestionsDocument8 paginiMCQ Anaesthesia QuestionsOanamikaela VaidaÎncă nu există evaluări
- iCU Delirium-A Diagnostic and Therapeutic Challenge in The Intensive Care UnitDocument13 paginiiCU Delirium-A Diagnostic and Therapeutic Challenge in The Intensive Care UnitTai rascunhos TaiÎncă nu există evaluări
- Demencia FrontotemporalDocument10 paginiDemencia FrontotemporalIsaac EliasÎncă nu există evaluări
- Final Draft-Long-Term Cognitive ImpairmentDocument6 paginiFinal Draft-Long-Term Cognitive Impairmentapi-237094717Încă nu există evaluări
- ABCDEF Critical CareDocument19 paginiABCDEF Critical CarealbaÎncă nu există evaluări
- Lee2021 Article SuccinctApproachToDeliriumInThDocument8 paginiLee2021 Article SuccinctApproachToDeliriumInThFideoPereÎncă nu există evaluări
- Guidelines For The Management of Accidental Tetanus in Adult PatientsDocument16 paginiGuidelines For The Management of Accidental Tetanus in Adult PatientsWiro AlexanderÎncă nu există evaluări
- Kart Tune N 2010Document10 paginiKart Tune N 2010AndreiaÎncă nu există evaluări
- Technical Report Writing AssignmentDocument9 paginiTechnical Report Writing AssignmentMuhammad AwaisÎncă nu există evaluări
- Consciencia y Anestesia AdvDocument15 paginiConsciencia y Anestesia AdvJavier LugoÎncă nu există evaluări
- A2 - Loi, 2021Document8 paginiA2 - Loi, 2021bayu seno ajiÎncă nu există evaluări
- Healthcare: Related Factors and Treatment of Postoperative Delirium in Old Adult Patients: An Integrative ReviewDocument18 paginiHealthcare: Related Factors and Treatment of Postoperative Delirium in Old Adult Patients: An Integrative ReviewAleksandar VilaÎncă nu există evaluări
- 2017 Article 695Document13 pagini2017 Article 695Makhda Nurfatmala LubisÎncă nu există evaluări
- Maldonado 2013Document33 paginiMaldonado 2013martin najeraÎncă nu există evaluări
- Delirium Management in The Icu: Evidence DefinitionsDocument10 paginiDelirium Management in The Icu: Evidence DefinitionsparamithadianÎncă nu există evaluări
- Delirium Management in The Icu: Evidence DefinitionsDocument10 paginiDelirium Management in The Icu: Evidence DefinitionsRosa AlersÎncă nu există evaluări
- An EJourney Through The Life Cycle of Spinal Cord Injusry-Nov-21-2013-0208Document12 paginiAn EJourney Through The Life Cycle of Spinal Cord Injusry-Nov-21-2013-0208irsyad120Încă nu există evaluări
- Edlow 2018Document15 paginiEdlow 2018arianaÎncă nu există evaluări
- Anciano - Niño en Urg Emerg Med Clin Ona Ago 17 PDFDocument15 paginiAnciano - Niño en Urg Emerg Med Clin Ona Ago 17 PDFLuis ParraÎncă nu există evaluări
- Changing Profile of 7,519 Neurologic Outpatients Evaluated Over 20 YearsDocument10 paginiChanging Profile of 7,519 Neurologic Outpatients Evaluated Over 20 YearsNicole AguilarÎncă nu există evaluări
- Neurology WardDocument5 paginiNeurology WardSara Garzón BermúdezÎncă nu există evaluări
- Icu Journal. FinalDocument6 paginiIcu Journal. FinalJoehoney BarreraÎncă nu există evaluări
- Literature Review of Post-Traumatic Stress Disorder in The Critical Care PDFDocument14 paginiLiterature Review of Post-Traumatic Stress Disorder in The Critical Care PDFOriza Zara SativaÎncă nu există evaluări
- Sample of Research ProposalDocument9 paginiSample of Research Proposaliqbalmustapa319Încă nu există evaluări
- A Prospective Observational Cohort Study To Detect Occurrence, Risk Factors and Outcomes of Delirium in Intensive Care UnitDocument7 paginiA Prospective Observational Cohort Study To Detect Occurrence, Risk Factors and Outcomes of Delirium in Intensive Care UnitInternational Journal of Innovative Science and Research TechnologyÎncă nu există evaluări
- Lupusto Suddenly Have A Name For This Thing. - . WasDocument8 paginiLupusto Suddenly Have A Name For This Thing. - . WasMicaela AlvesÎncă nu există evaluări
- Fneur 12 598777Document8 paginiFneur 12 598777Miguel HuangÎncă nu există evaluări
- Final Paper DoneDocument42 paginiFinal Paper DoneMzito Jnr MzitoÎncă nu există evaluări
- Man 238Document10 paginiMan 238Ujjwal MaharjanÎncă nu există evaluări
- A Retrospective Cohort Study On The Clinical Outcomes of Patients Admitted To Intensive Care Units With DysnatremiaDocument10 paginiA Retrospective Cohort Study On The Clinical Outcomes of Patients Admitted To Intensive Care Units With DysnatremiaEdo RezaprasgaÎncă nu există evaluări
- End of LifeDocument3 paginiEnd of LifeSiti Fatimahtusz07Încă nu există evaluări
- On December 20, 2019, This Report Was Posted As An MMWR Early Release On The MMWR Website (HTTPS://WWW - Cdc.gov/mmwr)Document6 paginiOn December 20, 2019, This Report Was Posted As An MMWR Early Release On The MMWR Website (HTTPS://WWW - Cdc.gov/mmwr)jose restrepoÎncă nu există evaluări
- Delirium in Intensive CareDocument8 paginiDelirium in Intensive CareAna Elizabeth Gangotena CoralÎncă nu există evaluări
- Delirium in Older AdultsDocument21 paginiDelirium in Older AdultsSergio DiasÎncă nu există evaluări
- 3 What Happens To Critically IllDocument17 pagini3 What Happens To Critically IllAbdul RaufÎncă nu există evaluări
- Predicting Dementia From Primary Care Records: A Systematic Review and Meta-AnalysisDocument23 paginiPredicting Dementia From Primary Care Records: A Systematic Review and Meta-AnalysisDeedee RenovaldiÎncă nu există evaluări
- Intruduccion 1Document9 paginiIntruduccion 1BLANCA TATIANA PONCIANO MERINOÎncă nu există evaluări
- International Journal of Health Sciences and Research: A Focus On Absconding in Mental Health: A Review of The LiteratureDocument10 paginiInternational Journal of Health Sciences and Research: A Focus On Absconding in Mental Health: A Review of The Literaturedkumar_100Încă nu există evaluări
- Delirium in Elderly Patients and The Risk of Postdischarge Mortality, Institutionalization, and DementiaDocument9 paginiDelirium in Elderly Patients and The Risk of Postdischarge Mortality, Institutionalization, and DementiaDeddy TrimarwantoÎncă nu există evaluări
- Sustainable Building: Submitted By-Naitik JaiswalDocument17 paginiSustainable Building: Submitted By-Naitik JaiswalNaitik JaiswalÎncă nu există evaluări
- Arendi v. GoogleDocument16 paginiArendi v. GooglePriorSmartÎncă nu există evaluări
- Low Steam Cane - Almoiz Industries Road To SuccessDocument9 paginiLow Steam Cane - Almoiz Industries Road To SuccessArif ShafiÎncă nu există evaluări
- QinQ Configuration PDFDocument76 paginiQinQ Configuration PDF_kochalo_100% (1)
- Old Book Buy or SellDocument41 paginiOld Book Buy or SellPallavi Pallu50% (4)
- EARTH SCIENCE NotesDocument8 paginiEARTH SCIENCE NotesAlthea Zen AyengÎncă nu există evaluări
- Project Documentation - Sensorflex 30G Data SheetDocument15 paginiProject Documentation - Sensorflex 30G Data SheetOmar HectorÎncă nu există evaluări
- A Proposed Approach To Handling Unbounded Dependencies in Automatic ParsersDocument149 paginiA Proposed Approach To Handling Unbounded Dependencies in Automatic ParsersRamy Al-GamalÎncă nu există evaluări
- FABM 1-Answer Sheet-Q1 - Summative TestDocument2 paginiFABM 1-Answer Sheet-Q1 - Summative TestFlorante De Leon100% (2)
- The Board-Management RelationshipDocument32 paginiThe Board-Management RelationshipAlisha SthapitÎncă nu există evaluări
- Theories of EmotionDocument11 paginiTheories of EmotionNoman AÎncă nu există evaluări
- IHE ITI Suppl XDS Metadata UpdateDocument76 paginiIHE ITI Suppl XDS Metadata UpdateamÎncă nu există evaluări
- Carim JR Et Al (2016) - Using Procedures Doens't Mean Follow It - A Cognitive Approach To How A Cockpit Manages EmergenciesDocument11 paginiCarim JR Et Al (2016) - Using Procedures Doens't Mean Follow It - A Cognitive Approach To How A Cockpit Manages EmergenciesFrancisco SilvaÎncă nu există evaluări
- MacDonald, J.& MacDonald, L. (1974)Document17 paginiMacDonald, J.& MacDonald, L. (1974)Mariuca PopescuÎncă nu există evaluări
- SQL Interview QuestionsDocument89 paginiSQL Interview QuestionsVaneet Arora100% (2)
- NEGRETE vs. COURT OF FIRST INSTANCE OF MARINDUQUEDocument1 paginăNEGRETE vs. COURT OF FIRST INSTANCE OF MARINDUQUELeo TumaganÎncă nu există evaluări
- Family Advent Devotions 1Document3 paginiFamily Advent Devotions 1collingdalenazÎncă nu există evaluări
- Understanding The School Curriculum Close Encounter With The School Curriculum SPARK Your InterestDocument12 paginiUnderstanding The School Curriculum Close Encounter With The School Curriculum SPARK Your InterestJoshua Lander Soquita CadayonaÎncă nu există evaluări
- Modelling The Relationship Between Hotel Perceived Value, CustomerDocument11 paginiModelling The Relationship Between Hotel Perceived Value, Customerzoe_zoeÎncă nu există evaluări
- C Programming Bit Bank U-1, U-2Document17 paginiC Programming Bit Bank U-1, U-2HariahÎncă nu există evaluări
- Natureview Case StudyDocument3 paginiNatureview Case StudySheetal RaniÎncă nu există evaluări
- Notice: Agency Information Collection Activities Proposals, Submissions, and ApprovalsDocument2 paginiNotice: Agency Information Collection Activities Proposals, Submissions, and ApprovalsJustia.comÎncă nu există evaluări
- Evolve Instagram Marketing Guide - From Zero To 10k PDFDocument132 paginiEvolve Instagram Marketing Guide - From Zero To 10k PDFAnjit Malviya100% (2)
- Flex Design Guide - 2020 DigitalDocument15 paginiFlex Design Guide - 2020 Digitalzahi xddÎncă nu există evaluări
- Karbohidrat: Gula, Pati & SeratDocument20 paginiKarbohidrat: Gula, Pati & SeratAlfi Syahrin SiregarÎncă nu există evaluări
- Chapter 1Document25 paginiChapter 1Aditya PardasaneyÎncă nu există evaluări
- Eliminate Zombie Nouns and Minimize Passive Voice: Plain LanguageDocument2 paginiEliminate Zombie Nouns and Minimize Passive Voice: Plain LanguagePădure IonuțÎncă nu există evaluări
- Case Study TemplateDocument4 paginiCase Study Templateapi-355498849Încă nu există evaluări
- Intj MbtiDocument17 paginiIntj Mbti1985 productionÎncă nu există evaluări
- MNDCS-2024 New3 - 231101 - 003728Document3 paginiMNDCS-2024 New3 - 231101 - 003728Dr. Farida Ashraf AliÎncă nu există evaluări