Documente Academic
Documente Profesional
Documente Cultură
Disorders of Water and Sodium Homeostasis
Încărcat de
Jafer DetamoDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Disorders of Water and Sodium Homeostasis
Încărcat de
Jafer DetamoDrepturi de autor:
Formate disponibile
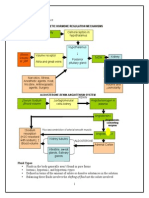
DISORDERS OF WATER AND SODIUM HOMEOSTASIS Regulation of water balance and sodium disorders Water intake and the
excretion of water are tightly regulated processes that are able to maintain a nearconstant serum osmolality. Sodium disorders (dysnatraemiashyponatraemia or hypernatraemia) are almost always due to an imbalance between water intake and water excretion. Understanding the etiology of sodium disorders depends on understanding the concept of electrolyte-free water clearancethis is a conceptual amount of water that represents the volume that would need to be subtracted (if electrolyte-free water clearance is positive) or added (if negative) to the measured urinary volume to make the electrolytes contained within the urine have the same tonicity as the plasma electrolytes. It is the concentration of the electrolytes in the urine, not the osmolality of the urine, which ultimately determines the net excretion of water. Hyponatraemia Hyponatraemia, defined as serum sodium concentration of less than 135mmol/litre, is a common electrolyte disorder. It is almost invariably due to impaired water excretion, often in states where ADH release is: 1. A normal response to a physiological stimulus such as pain, nausea, volume depletion, postoperative state, or congestive heart failure; or 2. A pathophysiological response as occurs with thiazide diuretics, other types of medications, or in the syndrome of inappropriate diuresis; with both often exacerbated in hospital by Inappropriate iatrogenic administration of water (or 5% dextrose). Clinical features These can range from the patient who is entirely asymptomatic at one end of the spectrum to Hyponatraemic encephalopathymost commonly manifesting with nausea, vomiting, and headacheat the other. Cerebral demyelination is a serious complication associated with hyponatraemia and its treatment, at its worst manifesting as pseudo coma with a locked in state. Children and premenopausal women are at particular risk of poor outcomes, as are those who are hypoxic at presentation. Management approach The first priority is to exclude a hyperosmolar state and verify whether the patient is hypotonic, by (when possible) measuring the serum osmolality. The diagnostic approach is further based on the history, clinical assessment of the patients volume status, and estimation of urinary electrolytes. Key iss ues are to recognize that: 1. Hyponatraemic encephalopathy is a medical emergency that should be diagnosed and treated promptly with hypertonic saline to prevent death or devastating neurological complications; but also 2. Those patients who are asymptomatic do not require treatment with hypertonic saline, whatever their level of serum sodium. Precipitating causes (e.g. thiazide diuretics) should be withdrawn when possible.
Practical managementalgorithms, even if complex, cannot accurately predict a patients response to treatment of hyponatraemia: close monitoring of serum sodium is essential. Patients with severe manifestations of hyponatraemic encephalopathy (active seizures or respiratory failure) should be given a bolus of 100ml of 3% saline (over 10min) to abruptly increase the serum sodium by about 2 to 4mmol/litre, following which an infusion of 3% saline should be given at a rate of 1ml/kg body weight per hour with the aim of raising the serum sodium to a mildly hyponatraemic level, but the total change in serum sodium should not exceed 15 to 20mmol/litre over 48h. For patients with less severe neurological manifestations, the bolus should be omitted. Cerebral demyelination This is a serious complication that has been associated with the correction of hyponatraemia, hence all patients receiving an infusion of 3% saline should have their serum sodium measured at least every 2h until they are clinically stable and the serum sodium values are stable, with appropriate modification of treatment in response to the measurements. Failure to do so, and reliance on a calculated infusion rate, can lead to significant patient injury. Preventionhyponatraemia is usually iatrogenic and can be avoided or detected as follows: 1. hypotonic fluids should never be administered following surgery unless used to correct a freewater deficit0.9% (normal) saline (NaCl) should be given postoperatively if parenteral fluids are indicated; 2. All hospitalized patients should be considered at risk for the development of hyponatraemia and should not be given hypotonic fluids unless a free-water deficit is present or if ongoing free-water losses are being replaced 3. Patients taking thiazide diuretics, especially older people, should be weighed before and after starting therapy and serum electrolytes monitored to detect water retention and the development of hyponatraemia. Hypernatraemia Hypernatraemia, defined as serum sodium concentration > 145mmol/liter, is a common electrolyte disorder that occurs when water intake is inadequate to keep up with water losses. Since the thirst mechanism is such a powerful stimulus, the almost invariable context is illness and care that restrict the patients access to water. Clinical features These are mainly related to central nervous system dysfunction caused by cerebral dehydration and cell shrinkage. Management approach The first step in evaluation is to take a detailed history focusing on fluid intake and losses. To assess urinary water losses, it is necessary to measure the urinary cationic electrolytes (sodium and potassium) and the urinary osmolality, remembering that the urinary osmolality alone cannot always determine the
presence or absence of electrolyte-free water losses in the urine, the reason being that water can be excreted with non-electrolyte osmoles or with electrolyte osmoles. Practical managementneeds to be guided by the following principles: 1. Correction of underlying deficits in circulatory blood volume by infusion of 0.9% saline; 2. Correction of chronic Hypernatraemia at a pace that avoids therapy-induced cerebral edema, which requires an understanding of both the initial water deficit and of ongoing water losses if the patient is polyuric; 3. Administration of water by drinking or feeding tube is preferable to treatment with intravenous fluids if possible; 4. Glucose-containing solutions should be avoided if possible; 5. As for the treatment of hyponatraemia, algorithms cannot accurately predict the response to treatment of hypernatraemia, hence regular monitoring of serum sodium with appropriate adjustment of treatment in response to the values obtained is mandatory. Prevention 1. Patients with impaired access to water (e.g. infants, elderly, and hospitalized patients) should be considered at risk for the development of hypernatraemia, and their serum sodium should be monitored; 2. Urinary electrolytes should be measured in conjunction with urinary osmolality in patients with polyuria to assess water losses in the urine and urinary concentrating ability
S-ar putea să vă placă și
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- PointDocument1 paginăPointJafer DetamoÎncă nu există evaluări
- BiostatDocument13 paginiBiostatJafer DetamoÎncă nu există evaluări
- PCPDocument19 paginiPCPJafer DetamoÎncă nu există evaluări
- IVIVCDocument20 paginiIVIVCJafer DetamoÎncă nu există evaluări
- Proc No. 218-2000 Medical Practitioners Registration (Repealing)Document1 paginăProc No. 218-2000 Medical Practitioners Registration (Repealing)Jafer Detamo0% (1)
- Randomized Controlled TrialsDocument1 paginăRandomized Controlled TrialsJafer DetamoÎncă nu există evaluări
- Pharmacology Re ExamDocument2 paginiPharmacology Re ExamJafer DetamoÎncă nu există evaluări
- PrednisoneDocument2 paginiPrednisoneJafer DetamoÎncă nu există evaluări
- Basic Pharmacology OralDocument8 paginiBasic Pharmacology OralJafer DetamoÎncă nu există evaluări
- Specific AgentsDocument1 paginăSpecific AgentsJafer DetamoÎncă nu există evaluări
- Please Select The One BEST Answer.: Gastrointestinal Pathophysiology Exam 2005 Tufts University School of MedicineDocument8 paginiPlease Select The One BEST Answer.: Gastrointestinal Pathophysiology Exam 2005 Tufts University School of MedicineJafer DetamoÎncă nu există evaluări
- Opr 003 E8Document2 paginiOpr 003 E8Jafer DetamoÎncă nu există evaluări
- Which of The Following H1 Antihistamines Is Non SedatingDocument7 paginiWhich of The Following H1 Antihistamines Is Non SedatingJafer DetamoÎncă nu există evaluări
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Facts About Dihydrogen MonoxideDocument11 paginiFacts About Dihydrogen Monoxideapi-368121935Încă nu există evaluări
- Intravenous Fluids: Balancing Solutions: Ewout J. HoornDocument8 paginiIntravenous Fluids: Balancing Solutions: Ewout J. HoornbagusÎncă nu există evaluări
- Management of Hyponatremia: KIAN PENG GOH, M.R.C.P., Alexandra Hospital, SingaporeDocument8 paginiManagement of Hyponatremia: KIAN PENG GOH, M.R.C.P., Alexandra Hospital, SingaporeDea IrbahÎncă nu există evaluări
- Journal Club CompleteDocument2 paginiJournal Club Completeapi-534233456Încă nu există evaluări
- IV FluidsDocument6 paginiIV FluidsAr-jay PorrasÎncă nu există evaluări
- Maintenance Fluid Therapy in ChildrenDocument4 paginiMaintenance Fluid Therapy in ChildrenNicole_0Încă nu există evaluări
- When "Warteg" Gives Him More: Group 7Document46 paginiWhen "Warteg" Gives Him More: Group 7Daniel Hans JayaÎncă nu există evaluări
- Fluid and ElectrolyteDocument46 paginiFluid and Electrolyteapi-76740522Încă nu există evaluări
- Running To DeathDocument1 paginăRunning To DeathThe London Free PressÎncă nu există evaluări
- Test Bank For Wilkins Clinical Assessment in Respiratory Care 8th Edition HeuerDocument15 paginiTest Bank For Wilkins Clinical Assessment in Respiratory Care 8th Edition Heueraaronraymd15012001cew100% (14)
- Acute Decompensated Heart Failure: ReviewDocument11 paginiAcute Decompensated Heart Failure: ReviewFercee PrimulaÎncă nu există evaluări
- Fluid & ElectrolyteDocument26 paginiFluid & Electrolytesanjana bhatia100% (1)
- Fluids and ElectrolytesDocument102 paginiFluids and Electrolytesfelxhu50% (2)
- 110-Dehydration and Disorders of Sodium BalanceDocument5 pagini110-Dehydration and Disorders of Sodium BalancepelinÎncă nu există evaluări
- Posttest UrinaryDocument7 paginiPosttest UrinaryAilatiLiamÎncă nu există evaluări
- Test Bank For Essentials of Pathophysiology 3rd Edition, PorthDocument23 paginiTest Bank For Essentials of Pathophysiology 3rd Edition, PorthILL110100% (1)
- Hyponatremia in The Neurocritical Care PatientDocument10 paginiHyponatremia in The Neurocritical Care PatientAli JENDOUBIÎncă nu există evaluări
- SIADH, DI and Cerebral Salt Wasting: Karim Rafaat, MDDocument54 paginiSIADH, DI and Cerebral Salt Wasting: Karim Rafaat, MDMahendra PrasetyoÎncă nu există evaluări
- Dementia and Prehospital ImplicationsDocument11 paginiDementia and Prehospital ImplicationsIlyes FerenczÎncă nu există evaluări
- Chapter62 1Document34 paginiChapter62 1Mozart OlarioÎncă nu există evaluări
- SamscaDocument2 paginiSamscaJOANNA MAE ABIA SALOMONÎncă nu există evaluări
- Cerebral Salt Wasting Syndrome ReviewDocument6 paginiCerebral Salt Wasting Syndrome ReviewSoewira Sastra100% (1)
- Fluctuation To Achieve Beter Blood Glucose Level, Oral Agent Need Dose Adj in Renal ImpairedDocument35 paginiFluctuation To Achieve Beter Blood Glucose Level, Oral Agent Need Dose Adj in Renal ImpairedQasim Al-OrjaniÎncă nu există evaluări
- Fluids and Electrolytes 3Document8 paginiFluids and Electrolytes 3Potchiee Pfizer100% (1)
- NCLEX HomeostasisDocument10 paginiNCLEX HomeostasisAngie MandeoyaÎncă nu există evaluări
- SterilizationDocument6 paginiSterilizationasfwegereÎncă nu există evaluări
- Fluid and Electrolyte Therapy in NewbornsDocument10 paginiFluid and Electrolyte Therapy in NewbornsJaner BanosÎncă nu există evaluări
- Siadh Patient Case - Final1Document43 paginiSiadh Patient Case - Final1api-589685298Încă nu există evaluări
- Management of Diabetes Insipidus Following Surgery For Pituitary and Suprasellar TumoursDocument11 paginiManagement of Diabetes Insipidus Following Surgery For Pituitary and Suprasellar TumoursAnggun RosalinaÎncă nu există evaluări
- Mtap421 ElectrolytesDocument9 paginiMtap421 ElectrolytesNhelomar ManlinconÎncă nu există evaluări