Documente Academic
Documente Profesional
Documente Cultură
Chips Reference Guide
Încărcat de
Mia JacksonDescriere originală:
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Chips Reference Guide
Încărcat de
Mia JacksonDrepturi de autor:
Formate disponibile
QRG 0209
The best decision a family can make.
Texas Childrens Health Plan Provider Quick Reference Guide
Customer service
Claim inquiry, questions and information Information about CHIP or STAR products Eligibility/benefits questions on all products Phone: Telephone TouCHPoint: Fax: 832-828-1004 832-828-1007 832-825-8777
Provider Relations
Inquiries regarding Texas Childrens Health Plan (TCHP) policies and procedures Contract clarification/interpretation Fee schedule inquiries Change of address/phone number/tax identification number Requests for supplies (forms, directories, etc.) Information on provider educational in-services Phone: 832-828-1008 Toll free: 800-731-8527 Fax: 832-825-8750
Nurse help line
Members have access to registered nurses 24 hours a day, seven days a week. TCHP Nurse Help Line: 800-686-3831
For access to Provider TouCHPoint, TCHPs Web-based eligibility and claims system, please contact Provider Relations at 832-828-1008.
Electronic claims submission
HIPAA-compliant electronic claims filing. TCHP does not accept electronic UB92 claims for STAR through Availity. CHIP payor ID, WebMD and Availity 76048 CHIP payor ID, Legacy 76048C Medicaid (STAR) payor ID, WebMD 75228 Medicaid (STAR) payor ID, Availity TXCSM Medicaid (STAR) payor ID, Legacy 76048M
Pharmacy services
TCHP CHIP and STAR: 800-435-4165 (Vendor Drug Program)
Vision services
Vision services provided by Block Vision. TCHP STAR and CHIP: 800-879-6901
Dental services
TCHP STAR (under age 21): TCHP STAR (over 21): TCHP CHIP: 877-847-8377 (THSteps Dental Program) 866-548-8123 (STARDent) 866-561-5892 (Delta Dental)
Claims filing information
Filing deadlines for all products: 95 days from date of service TCHP CHIP Claims address PO Box 300125 Houston, TX 77230 Claims appeals TCHP Attn: Appeals PO Box 301011 Houston, TX 77230-1011
Use appeal coversheet from Provider Handbook.
Care Coordination, Case and Disease Management
Referrals for assistance with chronic, complex conditions, or maternity. Phone: 832-828-1270 or 832-828-1430 Fax: 832-825-8745 Nurse Family Partnership Phone: 832-828-1274 Fax: 832-825-8710 Maternal Child/Adolescent Transition Phone: 832-828-1004 Fax: 832-825-8705
TCHP STAR Claims address PO Box 300286 Houston, TX 77230-0286 Claims appeals TCHP Attn: Appeals PO Box 300286 Houston, TX 77230-0286
Use appeal coversheet from Provider Handbook.
QRG 0209
The best decision a family can make.
Texas Childrens Health Plan Provider Quick Reference Guide
Referrals
Patients should be referred to in-network specialists. When TCHP members are referred for speciality care to an in-network specialist, it is not necessary to complete a referral form. Members may self-refer for in-network OB/GYN services, behavioral health, family planning and any Texas Health Steps provider.
Prior authorizations
The prior authorization process is used to evaluate the medical necessity of a procedure, course of treatment, appropriate level of service and length of stay prior to the provision of services. A copy of the prior authorization request form can be found in the Provider Handbook. Prior authorizations should be requested 3 to 5 days prior to the scheduled date of service. A complete list of services requiring prior authorization is available in the Provider Handbook. Some of the services include: All out-of-network services Oral surgery Abortion Organ acquisition Ambulance services (non-emergent) Outpatient behavioral health visits Augmentative communication devices after the 30th session Behavioral health rehabilitation Partial hospitalization for behavioral Baclofen injections/pumps health services Botox injections PET/SPECT Canned nutritional supplements Psychological testing Chemotherapy non-FDA approved Prevnar for children older than Circumcision greater than 1 year of age 5 years of age Cochlear implant Private duty nursing at home Contact lenses, with disease Prosthetics Cosmetic surgery Physical therapy, speech therapy and Dental medically necessary occupational therapy (except for cleft palate) (excluding initial evaluation) Gait trainer Residential treatment facility (codes E8000, E8001, E8002) (behavioral health) Helmets Respiratory vest Home health care Skilled nursing facility Hospital beds and accessories Skills training (behavioral health) Hospital inpatient care TMJ diagnosis (physical and behavioral health) Transplant evaluation Intensive outpatient treatment Therapeutic foster care (behavioral health) Vision care, medically necessary Neurological testing Wheelchairs and accessories Obesity surgery
Imaging services
It is not necessary to use a referral form for imaging services. Providers should refer members for imaging services using an appropriate vendor requisition form. Participating providers, which may vary by product, include: UT Imaging Woodlake MRI & Diagnostics Universal MRI & Diagnostics Any contracted hospital
Laboratory services
It is not necessary to use a referral form for laboratory services. Providers should refer members for laboratory services using an appropriate vendor requisition form. Participating providers, which may vary by product, include: Quest Laboratories Laboratory Corporation of America Clinical Pathology Laboratory, Inc. Any contracted hospital
Phone numbers for state programs
CHIP Help Line: Early Childhood Intervention (ECI): Family Planning Program: Medicaid Program Member Verification (NAIS): Medical Transportation Program (MTP): Preferred Drug List/Prior Authorization Program: STAR Help Line: STARLink Advocate for Medicaid: Texas Health Steps: Women, Infants & Children Program (WIC): 800-647-6558 800-250-2246 512-458-7796 800-925-9126 877-MED-TRIP (633-8747) 877-728-3927 800-964-2777 866-566-8989 877-847-8377 800-942-3678
Utilization management
Urgent authorization requests: Fax: 832-828-1004 832-825-8760
Behavioral health services
Members and/or PCPs can self refer to a participating behavioral health provider. Phone: 832-828-1004
S-ar putea să vă placă și
- FamilyCare Final 2014 Provider Resource GuideDocument23 paginiFamilyCare Final 2014 Provider Resource GuideJoshuaFieldsDesignÎncă nu există evaluări
- Lista de Hospitais - Global HealthDocument16 paginiLista de Hospitais - Global HealthRuano Andreola StumpfÎncă nu există evaluări
- Medi AssistDocument11 paginiMedi Assistrak_arsenalÎncă nu există evaluări
- Ameriplan-Health Ameriplan BrochureDocument5 paginiAmeriplan-Health Ameriplan Brochureapi-242298828Încă nu există evaluări
- Telehealth Strategies, Techniques, Billing and Reimbursement Pre-And Post - COVID19Document20 paginiTelehealth Strategies, Techniques, Billing and Reimbursement Pre-And Post - COVID19Mary Joy LambinoÎncă nu există evaluări
- Health Information Exchange Fact SheetDocument4 paginiHealth Information Exchange Fact SheetDavid MarkÎncă nu există evaluări
- Yeshaswini Co-Operative Farmer's Health Care SchemeDocument11 paginiYeshaswini Co-Operative Farmer's Health Care SchemeDisha MorÎncă nu există evaluări
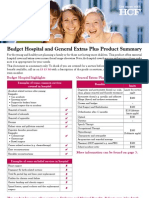
- Budget Hospital and General Extras Plus Product SummaryDocument4 paginiBudget Hospital and General Extras Plus Product SummaryJames SandersÎncă nu există evaluări
- Telehealth Best PracticesDocument4 paginiTelehealth Best Practicesdina kurniasariÎncă nu există evaluări
- CBM Wayne HandbookDocument19 paginiCBM Wayne HandbookCommunityBridgesÎncă nu există evaluări
- Faq On Group Mediclaim Policy: Cavinkare Private LimitedDocument19 paginiFaq On Group Mediclaim Policy: Cavinkare Private LimitedSamruddhi NaikÎncă nu există evaluări
- Chief Minister's Health Insurance SchemeDocument12 paginiChief Minister's Health Insurance SchemeDisha MorÎncă nu există evaluări
- DirectoryDocument2 paginiDirectoryasarkis3268Încă nu există evaluări
- Medicare Questions AnsweredDocument8 paginiMedicare Questions Answeredhazareerubina54Încă nu există evaluări
- Integrated Telehealth Solution - Dhanush Kenya - Connected KenyaDocument33 paginiIntegrated Telehealth Solution - Dhanush Kenya - Connected KenyaICT AUTHORITY100% (1)
- Academic Blue SHIP Brief SummaryDocument2 paginiAcademic Blue SHIP Brief SummaryAnonymous pWOoGdHZÎncă nu există evaluări
- Medical Coding For Dental PracticesDocument15 paginiMedical Coding For Dental Practicesghassan ahmedÎncă nu există evaluări
- HMO Proposal For Individual Family Account REGULAR-UPDATED AS OF JULY 2...Document11 paginiHMO Proposal For Individual Family Account REGULAR-UPDATED AS OF JULY 2...Arron BuenavistaÎncă nu există evaluări
- Brochures - Gradly Student World Elite Plus 2023 AetnaDocument18 paginiBrochures - Gradly Student World Elite Plus 2023 AetnaPragya SinhaÎncă nu există evaluări
- Medical Home: Care Coordination: The Patient-CenteredDocument23 paginiMedical Home: Care Coordination: The Patient-CenteredDwi Suranto100% (1)
- Wait Times To Medical Care and Treatment in Canada: LAWS-6046 - (34) - 22S - Emily PassanhaDocument10 paginiWait Times To Medical Care and Treatment in Canada: LAWS-6046 - (34) - 22S - Emily Passanhaemily passanhaÎncă nu există evaluări
- Rajiv Aarogyasri Health Insurance Scheme: Quality Medicare For AllDocument61 paginiRajiv Aarogyasri Health Insurance Scheme: Quality Medicare For Allsamir_sachdevaÎncă nu există evaluări
- Clinical Decision Support Systems: Syed Tirmizi, M.DDocument94 paginiClinical Decision Support Systems: Syed Tirmizi, M.DgopiÎncă nu există evaluări
- Membership Handbook PDFDocument44 paginiMembership Handbook PDFAli BariÎncă nu există evaluări
- M Health RevBDocument19 paginiM Health RevBcbhawsarÎncă nu există evaluări
- OPHCN Member HandbookDocument13 paginiOPHCN Member HandbookCommunityBridgesÎncă nu există evaluări
- PDF HealthDocument2 paginiPDF HealthFarwa KhalidÎncă nu există evaluări
- IEHP Medi-Cal Members Rights and Responsibilities PDFDocument11 paginiIEHP Medi-Cal Members Rights and Responsibilities PDFminipower50Încă nu există evaluări
- The Healthcare WorkforceDocument44 paginiThe Healthcare Workforcewelcome martinÎncă nu există evaluări
- Volunteer Ehealth Initiative: A Regional Demonstration ProjectDocument16 paginiVolunteer Ehealth Initiative: A Regional Demonstration ProjectotnawrupÎncă nu există evaluări
- Feedback For Answer ID 1604 (Rated-Not Helpful)Document3 paginiFeedback For Answer ID 1604 (Rated-Not Helpful)EmmaarkayÎncă nu există evaluări
- Documentation for Skilled Nursing & Long-Term Care: A Guide for Occupational TherapistsDe la EverandDocumentation for Skilled Nursing & Long-Term Care: A Guide for Occupational TherapistsÎncă nu există evaluări
- Day 2 Purpose UseDocument23 paginiDay 2 Purpose UseJoenabie Andoy EncantoÎncă nu există evaluări
- contentdamcenteneSunshinepdfsMMA Reg4 PDFDocument501 paginicontentdamcenteneSunshinepdfsMMA Reg4 PDFShawn SherwoodÎncă nu există evaluări
- AZ Provider Directory PDFDocument822 paginiAZ Provider Directory PDFArmoredDragoonÎncă nu există evaluări
- Hospital Adv Sav General Extras PlusDocument5 paginiHospital Adv Sav General Extras PlusferdiddleÎncă nu există evaluări
- Insurance Manual PDFDocument56 paginiInsurance Manual PDFesesmith108Încă nu există evaluări
- The Philippine Health AgendaDocument32 paginiThe Philippine Health Agendajustbeingclever100% (2)
- Apex 1complete Solution - 2 Page OverviewDocument2 paginiApex 1complete Solution - 2 Page OverviewUrmiÎncă nu există evaluări
- Query Health - Rich Elmore - HIT Policy Committee 2011-09-14Document20 paginiQuery Health - Rich Elmore - HIT Policy Committee 2011-09-14Rich ElmoreÎncă nu există evaluări
- Credentialing SpecialistDocument11 paginiCredentialing SpecialistMichael Variacion100% (1)
- Reading 7 - The Health Assessment ProcessDocument4 paginiReading 7 - The Health Assessment ProcessHani MasriÎncă nu există evaluări
- WBH Strategic Plan ProjectDocument62 paginiWBH Strategic Plan Projectapi-239845860Încă nu există evaluări
- JCR Content PDFDocument492 paginiJCR Content PDFShashiÎncă nu există evaluări
- The Business of Nur$ing: Telemedicine, DEA and FPA guidelines, A Toolkit for Nurse Practitioners Vol. 2De la EverandThe Business of Nur$ing: Telemedicine, DEA and FPA guidelines, A Toolkit for Nurse Practitioners Vol. 2Încă nu există evaluări
- Hospital Reform Implimentation and EvaluationDocument39 paginiHospital Reform Implimentation and EvaluationAdi MawardiÎncă nu există evaluări
- Unit 1 Health Care Information Regulations, Laws and StandardsDocument59 paginiUnit 1 Health Care Information Regulations, Laws and StandardsALEXANDRA MARIE BUNQUIN100% (1)
- Young Singles and Couples Product Summary: You Get With HCFDocument4 paginiYoung Singles and Couples Product Summary: You Get With HCFJames SandersÎncă nu există evaluări
- Physician Orientation Presentation3Document39 paginiPhysician Orientation Presentation3amitÎncă nu există evaluări
- The National Telehealth Webinar SeriesDocument69 paginiThe National Telehealth Webinar SeriesMarcÎncă nu există evaluări
- AHPRA Complaint FormDocument2 paginiAHPRA Complaint Formرها آزادÎncă nu există evaluări
- Incentive Payments For Meaningful Use' of Your Electronic Health RecordDocument22 paginiIncentive Payments For Meaningful Use' of Your Electronic Health Recorddnice408Încă nu există evaluări
- Guidelines NephrologyDocument1 paginăGuidelines NephrologyVicky HadiÎncă nu există evaluări
- A Presentation On Mediassist ProcessDocument19 paginiA Presentation On Mediassist Processassaassa2351Încă nu există evaluări
- Medical Aid ProposalDocument19 paginiMedical Aid ProposalTony Peterz Kurewa100% (1)
- DRG AssignmentDocument12 paginiDRG Assignmentavpnqvfng100% (1)
- Telemedicine and Its Application in Public Health: Dr. Preeti TiwariDocument54 paginiTelemedicine and Its Application in Public Health: Dr. Preeti Tiwariravishukla81Încă nu există evaluări
- Clinic Business PlanDocument41 paginiClinic Business PlanIshaan Kamal100% (6)
- The Quality of Health Care: SAW Source: HarveyDocument43 paginiThe Quality of Health Care: SAW Source: HarveyMardatillah WiranataÎncă nu există evaluări
- THMP Pic FormDocument2 paginiTHMP Pic FormMia JacksonÎncă nu există evaluări
- 1099Document1 pagină1099Mia JacksonÎncă nu există evaluări
- Express Client IntakeDocument1 paginăExpress Client IntakeMia JacksonÎncă nu există evaluări
- Tax Year 2013 DeskReferenceGuideDocument8 paginiTax Year 2013 DeskReferenceGuideMia JacksonÎncă nu există evaluări
- Success! Thank You For Applying!: Other Jobs You Might Be Interested inDocument6 paginiSuccess! Thank You For Applying!: Other Jobs You Might Be Interested inMia JacksonÎncă nu există evaluări
- Consumer Related Services ECI RFP Texas Medicaid Provider Enrollment Application 2008 FY2010Document51 paginiConsumer Related Services ECI RFP Texas Medicaid Provider Enrollment Application 2008 FY2010Mia JacksonÎncă nu există evaluări
- Eviction PetitionDocument1 paginăEviction PetitionMia JacksonÎncă nu există evaluări
- TexMedConnect Acute Care ManualDocument40 paginiTexMedConnect Acute Care ManualMia JacksonÎncă nu există evaluări
- I-SMART - Substance Abuse TX Service Desciptions and CPT CodesDocument2 paginiI-SMART - Substance Abuse TX Service Desciptions and CPT CodesMia JacksonÎncă nu există evaluări
- Resource Education Center Co. INSURANCE VERIFICATION FORM-PHONE INTAKE Referred ByDocument3 paginiResource Education Center Co. INSURANCE VERIFICATION FORM-PHONE INTAKE Referred ByMia JacksonÎncă nu există evaluări
- Medicare EnrollmentDocument361 paginiMedicare EnrollmentMia JacksonÎncă nu există evaluări
- Attachment E Substance Abuse Encounter Rpting HCPCS and Revenue Codes Chart FY10 287030 7Document10 paginiAttachment E Substance Abuse Encounter Rpting HCPCS and Revenue Codes Chart FY10 287030 7Mia JacksonÎncă nu există evaluări
- Texas State Board of Social Worker Examiners: Social Work Employment HistoryDocument2 paginiTexas State Board of Social Worker Examiners: Social Work Employment HistoryMia JacksonÎncă nu există evaluări
- CPT Primer For PsychiatristsDocument17 paginiCPT Primer For PsychiatristsMia JacksonÎncă nu există evaluări
- Chapter 001Document51 paginiChapter 001Mia JacksonÎncă nu există evaluări
- Cms 1500 InteractiveDocument1 paginăCms 1500 InteractiveMia JacksonÎncă nu există evaluări
- TexMedConnect Acute Care ManualDocument40 paginiTexMedConnect Acute Care ManualMia JacksonÎncă nu există evaluări
- Ssa ReleaseDocument2 paginiSsa ReleaseMia JacksonÎncă nu există evaluări
- Original Timely Filing AppealDocument1 paginăOriginal Timely Filing AppealMia JacksonÎncă nu există evaluări
- Poverty and Children's Personal RelationshipsDocument87 paginiPoverty and Children's Personal RelationshipsJoe OgleÎncă nu există evaluări
- Ethics, Privacy, and Security: Lesson 14Document16 paginiEthics, Privacy, and Security: Lesson 14Jennifer Ledesma-Pido100% (1)
- Dif Stan 3-11-3Document31 paginiDif Stan 3-11-3Tariq RamzanÎncă nu există evaluări
- Governance StructureDocument1 paginăGovernance StructureJoydip MukhopadhyayÎncă nu există evaluări
- Implementation of 5G - IoT Communication System 1 - RB - LAB EQUIPMENTDocument32 paginiImplementation of 5G - IoT Communication System 1 - RB - LAB EQUIPMENTMaitrayee PragyaÎncă nu există evaluări
- Qualitative Tests Organic NotesDocument5 paginiQualitative Tests Organic NotesAdorned. pearlÎncă nu există evaluări
- Rrs PresentationDocument69 paginiRrs PresentationPriyamvada Biju100% (1)
- Nursing Care Plan: Assessment Diagnosis Planning Interventions Rationale EvaluationDocument11 paginiNursing Care Plan: Assessment Diagnosis Planning Interventions Rationale EvaluationDa NicaÎncă nu există evaluări
- The Effect OfAdditional Nanoparticles Supplementation of Indonesian Bay Leaf (SyzigiumPolyanthum) On Blood Pressure in Pregnancy HypertensionDocument4 paginiThe Effect OfAdditional Nanoparticles Supplementation of Indonesian Bay Leaf (SyzigiumPolyanthum) On Blood Pressure in Pregnancy HypertensionInternational Journal of Innovative Science and Research TechnologyÎncă nu există evaluări
- LYON Conditions of Secondment 3500EUR enDocument4 paginiLYON Conditions of Secondment 3500EUR enabdu1lahÎncă nu există evaluări
- Ethnomedicinal Plants For Indigestion in Uthiramerur Taluk Kancheepuram District Tamilnadu IndiaDocument8 paginiEthnomedicinal Plants For Indigestion in Uthiramerur Taluk Kancheepuram District Tamilnadu IndiaGladys DjeugaÎncă nu există evaluări
- 1 Stra Bill FinalDocument41 pagini1 Stra Bill FinalRajesh JhaÎncă nu există evaluări
- OM Mannual FOsDocument38 paginiOM Mannual FOsAbdulmuqtadetr AhmadiÎncă nu există evaluări
- Environmental Research and Public Health: International Journal ofDocument12 paginiEnvironmental Research and Public Health: International Journal ofKarenÎncă nu există evaluări
- Pre-Operative Check Up of Farm Tools, ImplementsDocument19 paginiPre-Operative Check Up of Farm Tools, ImplementsLaurence Fabiala50% (2)
- 2 - Pizeo Electric SensorDocument33 pagini2 - Pizeo Electric SensorNesamaniÎncă nu există evaluări
- Sithpat006ccc019 A - 2021.1Document34 paginiSithpat006ccc019 A - 2021.1Mark Andrew Clarete100% (2)
- Toxic RelationshipDocument1 paginăToxic RelationshipwidyasÎncă nu există evaluări
- Meng Mammogram JulDocument4 paginiMeng Mammogram JulLivia MillÎncă nu există evaluări
- Rotary Vane PumpsDocument7 paginiRotary Vane PumpshebsonbezerraÎncă nu există evaluări
- Fortune Falls - Lou VaneDocument402 paginiFortune Falls - Lou VanetesteÎncă nu există evaluări
- Chemrite SP 200Document3 paginiChemrite SP 200ghazanfarÎncă nu există evaluări
- RIASEC Personality TestDocument2 paginiRIASEC Personality TestSarah Jane NomoÎncă nu există evaluări
- Ce Mark - Application FormDocument3 paginiCe Mark - Application Formrajivsinghal90Încă nu există evaluări
- English BeginnersDocument34 paginiEnglish BeginnersCristina ZamfirÎncă nu există evaluări
- Soft Tissue SarcomaDocument19 paginiSoft Tissue SarcomaEkvanDanangÎncă nu există evaluări
- RNW Position PaperDocument2 paginiRNW Position PaperGeraldene AcebedoÎncă nu există evaluări
- Topic 7: Respiration, Muscles and The Internal Environment Chapter 7B: Muscles, Movement and The HeartDocument4 paginiTopic 7: Respiration, Muscles and The Internal Environment Chapter 7B: Muscles, Movement and The HeartsalmaÎncă nu există evaluări
- Allison Weech Final ResumeDocument1 paginăAllison Weech Final Resumeapi-506177291Încă nu există evaluări
- Product Term and ConditionsDocument50 paginiProduct Term and Conditionsain2Încă nu există evaluări