Documente Academic
Documente Profesional
Documente Cultură
Efficacy of Antiplaque Mouthwashes A 5 Day Clinical Trial
Încărcat de
Henny Eka PutriDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Efficacy of Antiplaque Mouthwashes A 5 Day Clinical Trial
Încărcat de
Henny Eka PutriDrepturi de autor:
Formate disponibile
Caries Detection and Prevention
Efficacy of antiplaque mouthwashes: A five-day clinical trial
Muhammad Wasif Haq, BDS
n
Mehwish Batool, BDS
Syed Hammad Ahsan, MSc
Gaurav Sharma
The aim of this study was to evaluate and compare the efficacy of antiplaque mouthwashes. Plaque levels were determined by applying a plaque-disclosing solution using the Turesky et al modification of the Quigley Hein plaque index. The control group (n = 6) brushed twice per day with fluoride toothpaste for one minute and rinsed with water, while the study groups (n = 6) brushed once per day with fluoride toothpaste for one minute, followed by rinsing with 5.0 mL of mouthwash diluted with 10.0 mL of water for 30 seconds. The control group brushed and rinsed with water twice per day. The results indicated that cetylpyridinium chloride in combination with sodium fluoride offered maximum plaque
inhibition, followed by chlorhexidine gluconate and sodium monofluorophosphate, while plaque levels increased in the control group and with the combination of chlorhexidine gluconate and sodium fluoride. The only antiplaque agents to demonstrate a statistically significant difference from the control were cetylpyridinium chloride in combination with sodium fluoride, and chlorhexidine gluconate. Increasing the fluoride concentration had no impact on antiplaque activity. Received: April 20, 2010 Accepted: June 21, 2010
ental plaque (biofilm) formation is a naturally occurring process, resulting from bacterial interactions with the acquired salivary pellicle formed over the surface of the tooth shortly after brushing the tooth. Although the newly formed plaque lacks any pathogenic potential due to an insufficient number of microorganisms present, the persistence of dental plaque allows for multiple bacterial interactions, resulting in various pathologies such as gingivitis, caries, periodontitis, and peri-implantitis.1,2 Adequate plaque control will not only contribute toward optimal oral health, it also will reduce highly prevalent diseases such as gingivitis, caries, and periodontitis.3 For optimal oral hygiene, toothbrushing, flossing, and using mouthwashes is recommended. Mouthwashes with antiplaque agents such as chlorhexidine, fluoride, and cetylpyridinium chloride are recommended for use in conjunction with toothbrushing because rinsing with mouthwashes in addition to toothbrushing has
e110 May/June 2011
been found to impart superior plaque control compared to toothbrushing alone.4 Chlorhexidine, a bisguanide cationic molecule with broad-spectrum antimicrobial activity, is considered the gold standard in plaque control.5 This agent, depending on the concentration, can be bactericidal or bacteriostatic and exerts more potent action against Gram-positive microorganisms than Gram-negative microorganisms.6 Chlorhexidine causes a reduction in salivary pellicle formation through the inhibition of bacterial enzyme glucosyl-transferase needed for bacterial adherence to tooth structure; it also produces bacterial cell wall disruption and cytoplasmic precipitation.7,8 Recent studies have shown chlorhexidine to be an effective inhibitor of matrix metalloproteinases, proinflammatory cytokines, interleukins, and salivary cathepsin C, all of which play an important role in gingivitis and periodontitis.9-11 Fluoride is an anionic, anticariogenic agent that helps to
www.agd.org
reprecipitate minerals lost during demineralization and also promotes the formation of larger and more acid-resistant fluorapatite crystals. It exerts its antimicrobial action through the inhibition of bacterial enzymes such as enolase and glucosyl-transferase and also causes inhibition of glucose uptake and utilization by bacteria.12,13 As with chlorhexidine, fluoride has an inhibitory effect on salivary cathepsin C and can be bacteriostatic as well as bactericidal to oral bacteria.14,15 Cetylpyridinium chloride is a bactericidal, quartenary ammonium compound that denatures bacterial proteins, inactivates various metabolic enzymes of bacteria, and damages cell membranes.16 It has more potent activity against Gram-positive organisms than Gram-negative organisms. Cetylpyridinium chloride also has been shown to accumulate in dental plaque, thereby exerting its antimicrobial effect for a longer period.17 Several studies, both in vitro and
General Dentistry
in vivo, have evaluated the efficacy of the antiplaque agents mentioned above.18,19 The simultaneous use of chlorhexidine with fluoride has been a matter of debate due to inconclusive results.20,21 In some studies, this combination decreased the efficacy and substantivity of chlorhexidine, possibly due to inactivation of the cationic chlorhexidine by anionic fluoride.6,22 Because most toothpastes contain sodium fluoride or sodium monofluorophosphate, the fluoride in these sources could influence and interfere with the activity of chlorhexidine. Variable results on the efficacy of cetylpyridinium chloride as an antiplaque agent also have been reported.23 Similarly, to the authors knowledge, very few studies have evaluated the antiplaque combination of cetylpyridinium chloride with fluoride.24,25 The aim of this study was to determine and compare the efficacy of mouthwashes containing chlorhexidine, sodium monofluorophosphate, chlorhexidine in combination with sodium fluoride, and cetylpyridinium chloride in combination with sodium fluoride.
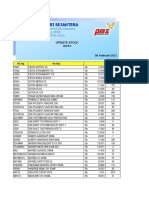
Table 1. Basic information about the mouthwashes used in this study. Group Product name (manufacturer) 1 Enziclor (Platinum Pharmaceuticals) 2 Secure (Platinum Pharmaceuticals) 3 Protect (Roomi Enterprises) 4 Aquafresh (GlaxoSmithKline) Control water Active agent 0.2% chlorhexidine gluconate 0.05% sodium monofluorophosphate 0.12% chlorhexidine gluconate and 0.05% sodium fluoride 0.05% cetylpyridinium chloride and 0.05% sodium fluoride -
Table 2. Initial and final plaque levels and the difference in plaque level among groups in this study. Group Initial plaque level Final plaque level Difference 0.89
1 11.89 11.0
2 11.22 10.95 0.27 3 13.37 13.41 -0.04 4 13.36 12.34 1.02 Control 11.61 14.23 -2.62
Materials and methods
The study was conducted at Liaquat College of Medicine & Dentistry, Karachi, Pakistan, where approval was received from the ethical committee. Thirty patients who attended the dental outpatient department were selected for this open-label, nonrandomized, controlled trial. The patients were allocated into four test groups and one control group (n = 6). Each participant was informed of the reason for the study, and informed consent was obtained. Participants were chosen for this study if they were from 1850 years of age (due to a greater likelihood of compliance and a lesser likelihood of co-morbidities and medicine
use) and had complete dentition through the second molars in all four quadrants. Participants were excluded from this study if any of their teeth had active dental caries or signs of periodontal involvement (visible on clinical examination and probing), they were taking any medications or showed signs of systemic disease, they were undergoing orthodontic treatment, or they had a prosthetic appliance. Following a clinical examination with a sterilized dental mirror and probe, participants were instructed to rinse their mouths with water repeatedly until it flushed without color. Two drops of plaquedisclosing solution (GDK Densell) were applied to a cotton pellet and patients were advised to apply the dye on the labial/buccal and lingual surfaces of all teeth.
www.agd.org
Preregimen plaque levels on the smooth surfaces of all teeth, excluding third molars, were estimated by using the Turesky et al modification of the Quigley-Hein plaque index. Participants in the test groups were instructed to brush with fluoride toothpaste (Close-Up, Church & Dwight Co., Inc.) once a day for one minute (30 seconds per jaw). Next, they rinsed their mouths for 30 seconds with 5.0 mL of mouthwash diluted with 10 mL of water. The mouthrinses, measuring cup, and fluoride toothpaste were provided to each participant for use during the five-day trial. Each mouthwash and its active antimicrobial agent(s) are listed in Table 1. The plaque scores for every group were calculated twice: at the time of examination and upon completion of the study. The difference between the initial and final readings was
May/June 2011 e111
General Dentistry
Caries Detection and Prevention Efficacy of antiplaque mouthwashes
Table 3. Results of the Bonferroni test for multiple comparisons among study groups and the control group. 95% confidence interval (I) group 1 (J) groups 2 3 4 control 2 1 3 4 control 3 1 2 4 control 4 1 2 3 control control 1 2 3 4 Mean difference (I-J) 0.10833 0.15500 -0.02167 0.55167* -0.10833 0.04667 -0.13000 0.44333 -0.15500 -0.04667 -0.17667 0.39667 0.02167 0.13000 0.17667 0.57333* -0.55167* -0.44333 -0.39667 -0.57333* Standard error 0.16900 0.16900 0.16900 0.16900 0.16900 0.16900 0.16900 0.16900 0.16900 0.16900 0.16900 0.16900 0.16900 0.16900 0.16900 0.16900 0.16900 0.16900 0.16900 0.16900 Significance 1.000 1.000 1.000 0.032 1.000 1.000 1.000 0.146 1.000 1.000 1.000 0.271 1.000 1.000 1.000 0.023 0.032 0.146 0.271 0.023 Lower bound -0.4119 -0.3652 -0.5419 0.0314 -0.6286 -0.4736 -0.6502 -0.0769 -0.6752 -0.5669 -0.6969 -0.1236 -0.4986 -0.3902 -0.3436 0.0531 -1.0719 -0.9636 -0.9169 -1.0936 Upper bound 0.6286 0.6752 0.4986 1.0719 0.4119 0.5669 0.3902 0.9636 0.3652 0.4736 0.3436 0.9169 0.5419 0.6502 0.6969 1.0936 -0.0314 0.0769 0.1236 -0.0531
*The mean difference is significant at the 0.05 level.
calculated and is presented in Table 2. The means and the standard deviations were calculated at the completion of the study. The confidence interval was set at 95%, with a level of significance of 0.05. The ANOVA and Bonferroni tests calculated the statistically significant differences between the study groups and the control and among the study groups (Table 3). SPSS software, version 17, was used for the analysis.
from the one-way ANOVA was less than 0.5 (P = 0.016), indicating a statistically significant difference. A Bonferroni multiple comparisons test assessed how much the study groups differed from each other and from the control; the results are presented in Table 3.
Discussion
Controlling plaque and preventing related diseases still pose a challenge for contemporary dentists. Finding an effective means of controlling plaque formation and maturation can result in a drastic decrease in the incidence and prevalence of plaque-associated
www.agd.org
Results
The differences between the initial and final plaque levels are presented in Table 2. The P value obtained
e112 May/June 2011
diseases and contribute toward improving overall patient oral health. Since few people use dental floss and many may not be aware of the proper flossing technique, it is imperative to recommend mouthwashes that are equally efficacious and compatible with dentifrices to prevent plaque maturation.26 This study evaluated the efficacy of antiplaque agents in mouthwashes in combination with the use of a fluoride-based toothpaste for five days. Results indicated that, when compared to the control, all study groups caused lesser plaque formation, reflecting the efficacy of antiplaque agents to various degrees.
General Dentistry
However, statistically significant differences compared to the control group were observed for only Groups 1 (P = 0.032) and 4 (P = 0.023). There were no statistically significant differences between the study groups. Group 4 showed the greatest plaque inhibition, followed by Groups 1 and 2, while Group 3 and the control displayed increased levels of plaque. The combination of chlorhexidine and fluoride was not found to be effective in reducing plaque levels; in fact, plaque levels were found to have increased at the completion of the study (differential = 0.04). Another study also concluded that the combination of chlorhexidine and fluoride was unable to contribute to any significant reduction in bacterial counts.27 Kohlahi and Soolari suggested that chlorhexidine forms salts with two agents in toothpaste, namely sodium monofluorophosphate and sodium lauryl sulfate, which could result in the decreased efficacy of chlorhexidine.28 They recommended that 30 minutes to two hours elapse between the use of a chlorhexidine mouthwash and brushing with a fluoride-based toothpaste.28 Since all groups in this study used the same toothpaste, the increase in plaque levels in Group 3 could reflect fluorides role in causing decreased antiplaque activity, since Group 3 was exposed to higher levels of fluoride from the toothpaste as well as from the mouthwash.6,29 Other studies also have reported the variability of chlorhexidine results.30,31 The synergistic activity observed in several studies from the simultaneous use of both chlorhexidine and fluoride was not observed in the current study.32-34 Many of the earlier studies involved the use of varnishes, while the current study evaluated antiplaque mouthrinses.
Different methods of delivering antiplaque agents could influence the outcome. At least one study has indicated that chlorhexidine varnish is more effective than chlorhexidine mouthrinses in reducing the level of Streptococcus mutans; this may be due to the longer exposure to chlorhexidine in varnishes.35,36 Fluoride also can be inactivated by its interaction with other agents. Not only can the efficacy of chlorhexidine be reduced by the presence of fluoride, chlorhexidine can influence fluorides activity as well. It has been found that chlorhexidine and fluoride have competitive binding on hydroxyapatite crystals in teeth, resulting in decreased binding of fluoride to hydroxyapatite crystals and rendering fluoride unable to play its role in the remineralization of carious teeth.37,38 However, the differences in the current study between Groups 1 and 3 were not found to be statistically significant (P = 1.000). Another finding obtained from the current study points to a limited antiplaque effect for all antiplaque agents, even after exposure to increased fluoride. In Group 2, sodium monofluorophosphate mouthrinse was used with a fluoride-based toothpaste; however, this group still did not demonstrate the reduction in plaque that was observed for Groups 1 and 4 (differential = 0.27). This finding is consistent with results obtained from a similar study.39 In high-risk caries patients, antiplaque agents in addition to fluoride are recommended. The maximum plaque inhibitory effect was observed in Group 4 (differential = 1.02). Although multiple studies have differed considerably regarding the antiplaque efficacy of cetylpyridinium chloride, it appears that this agent in combination with
www.agd.org
fluoride could offer the best antiplaque activity.40,41 Cetylpyridinium chloride facilitates better plaque removal when used in combination with toothbrushing.42 It has been documented that cetylpyridinium chloride in combination with sodium fluoride is more effective in inhibiting plaque than the combination of chlorhexidine with fluoride.43 Unfortunately, very few studies have been carried out to evaluate the combination of cetylpyridinium chloride and fluoride. It is extremely important that fluoride is included to assist with the remineralization of dental structure lost to decay. Group 1 did not offer as much plaque inhibition as Group 4; this could be attributed to a decrease in the efficacy of chlorhexidine caused by the fluoride in the toothpaste. If fluoride is not inactivated or is negatively influenced by cetylpyridinium chloride, then this combination could prove to be equivalent to chlorhexidine. One major factor limiting the regular use of antiplaque agents is their associated side effects. Chlorhexidine is known to cause brownish staining of the teeth, restorations, and mucosal surfaces; this is attributed to its attachment through the cationic group. Such stains can be removed only by scaling. For this reason, chlorhexidine use should be limited to no more than two weeks, and patients should be advised to limit their coffee and tea intake while using the product. Other side effects of chlorhexidine include alteration of taste perception and increased supragingival calculus.44 Recent data have shown chlorhexidine to have other side effects, such as its cytotoxic effects on odontoblasts, fibroblasts, and osteoblasts.45,46 Cytotoxic effects on fibroblasts, oral mucosal cells, and odonotoblast-like cells following
May/June 2011 e113
General Dentistry
Caries Detection and Prevention Efficacy of antiplaque mouthwashes
the use of sodium fluoride also have been documented.47,48 Also, the regular use of cetylpyridinium chloride has been shown to cause tooth staining similar to that of chlorhexidine.41 The next research challenges are to develop antiplaque agents with reduced or minimum side effects, limited interactions with other constituents found in dentifrices and mouthwashes, and increased efficacy. In the meantime, it is prudent to educate patients on all factors contributing to increased plaque formation. A very significant factor is limiting the patients sucrose consumption, which not only can prove beneficial in reducing plaque formation, it also would help to increase the efficacy of antimicrobial agents, because sucrose intake has been linked to decreased efficacy of antimicrobial agents.49 The authors suggest that more clinical trials be carried out to investigate the interaction of fluoride with chlorhexidine as well as the combination of cetylpyridinium chloride with fluoride in hampering plaque growth. The present study had certain limitations, the most important being the small sample size, which could have affected the overall results. Increasing the sample size could provide more accurate results. Also, toothbrushing could not be eliminated during this study, as restricting the mechanical cleaning beyond five days could lead to the development of gingivitis.50 A possible alternative could be to conduct the study on the teeth of laboratory animals with a controlled diet, using antimicrobial isolates. The possibilities of noncompliance among participants and nonuniformity of their dietary habits in different groups also could have influenced the outcome. Assessing the microbial growth of plaque
e114 May/June 2011
microorganisms and the inhibitory effect of antiplaque agents through microscopic analysis could have provided clearer results.
Conclusion
No synergistic action of chlorhexidine with fluoride was observed in the current study; instead, the simultaneous use of chlorhexidine and fluoride was associated with increased plaque levels. It seems likely that the efficacy of chlorhexidine is decreased in the presence of fluoride. Chlorhexidine and sodium monofluorophosphate acted to reduce plaque levels, although there was no statistical difference between these agents. Increasing the fluoride concentration did not lead to increased antiplaque activity. The combination of cetylpyridinium chloride and fluoride was most effective at reducing plaque levels.
Acknowledgements
The authors would like to thank the following people for their unlimited help and support during this study: Drs. Naheed Najmi, Asif Hussain, Nadeem Chand, and Temoor Moghul.
Author information
Drs. Haq and Batool are house officers, Department of Periodontology, Liaquat College of Medicine & Dentistry, Karachi, Pakistan, where Dr. Ahsan is an assistant professor of oral pathology. Mr. Sharma is an undergraduate kinesiology student at San Diego State University, California.
References
1. Marsh PD. Dental plaque as a biofilm and a microbial communityImplications for health and disease. BMC Oral Health 2006;6 Suppl 1:S14. 2. Sbordone L, Bortolaia C. Oral microbial biofilms and plaque-related diseases: Microbial communities and their role in the shift from oral health to disease.Clin Oral Investig 2003;7(4):181-188.
3. Pihlstrom BL, Michalowicz BS, Johnson NW. Periodontal diseases. Lancet 2005;366(9499): 1809-1820. 4. Feres M, Gursky LC, Faveri M, Tsuzuki CO, Figueiredo LC. Clinical and microbiological benefits of strict supragingival plaque control as part of the active phase of periodontal therapy. J Clin Periodontol 2009;36(10):857-867. 5. De Araujo Nobre M, Capelas C, Alves A, Almeida T, Carvalho R, Antunes E, Oliveira D, Cardador A, Malo P. Non-surgical treatment of peri-implant pathology. Int J Dent Hyg 2006;4(2):84-90. 6. de Freitas CS, Diniz HF, Gomes JB, Sinisterra RD, Cortes ME. Evaluation of the substantivity of chlorhexidine in association with sodium fluoride in vitro. Pesqui Odontol Bras 2003;17(1): 78-81. 7. Furiga A, Dols-Lafargue M, Heyraud A, Chambat G, Lonvaud-Funel A, Badet C. Effect of antiplaque compounds and mouthrinses on the activity of glucosyltransferases from Streptococcus sobrinus and insoluble glucan production. Oral Microbiol Immunol 2008;23(5):391-400. 8. Gronroos L, Matto J, Saarela M, Luoma AR, Luoma H, Jousimies-Somer H, Pyhala L, Asikainen S, Alaluusua S. Chlorhexidine susceptibilities of mutans streptococcal serotypes and ribotypes. Antimicrob Agents Chemother 1995; 39(4):894-898. 9. Gendron R, Grenier D, Sorsa T, Mayrand D. Inhibition of the activities of matrix metalloproteinases 2, 8, and 9 by chlorhexidine. Clin Diagn Lab Immunol 1999;6(3):437-439. 10. Sharma S, Saimbi CS, Koirala B, Shukla R. Effect of various mouthwashes on the levels of interleukin-2 and interferon-gamma in chronic gingivitis. J Clin Pediatr Dent 2008;32(2):111-114. 11. Dabrowska E, Letko M, Roszkowska-Jakimiec W, Letko R, Sadowski J. Effect of chlorhexidine mouthrinse on cathepsin C activity in human saliva. Adv Med Sci 2006;51 Suppl 1:96-99. 12. Guha-Chowdhury N, Clark AG, Sissons CH. Inhibition of purified enolases from oral bacteria by fluoride. Oral Microbiol Immunol 1997;12(2): 91-97. 13. Shani S, Friedman M, Steinberg D. The anticariogenic effect of amine fluorides on Streptococcus sobrinus and glucosyltransferase in biofilms. Caries Res 2000;34(3):260-267. 14. Dabrowska E, Letko M, Roszkowska-Jakimiec W, Letko R, Jamiolkowski J. Effect of fluoride preparations on the activity of human salivary cathepsin C. Rocz Akad Med Bialymst 2005;50 Suppl 1:160-162. 15. Summit. Fundamentals of operative dentistry. In: Burgess JO, Xu X. Fluoride releasing materials, ed. 3. Carol Stream, IL: Quintessence Publishing Co.; 2006:413-415. 16. Sandt C, Barbeau J, Gagnon MA, Lafleur M. Role of the ammonium group in the diffusion of quaternary ammonium compounds in Streptococcus mutans biofilms. J Antimicrob Chemother 2007;60(6):1281-1287. 17. Marcotte L, Therien-Aubin H, Sandt C, Barbeau J, Lafleur M. Solute size effects on the diffusion in biofilms of Streptococcus mutans. Biofouling 2004;20(4-5):189-201.
General Dentistry
www.agd.org
18. Pizzo G, La Cara M, Licata ME, Pizzo I, DAngelo M. The effects of an essential oil and an amine fluoride/stannous fluoride mouthrinse on supragingival plaque regrowth. J Periodontol 2008; 79(7):1177-1183. 19. Featherstone JD. The science and practice of caries prevention. J Am Dent Assoc 2000; 131(7):887-899. 20. Altenburger MJ, Klasser M, Schirrmeister JF, Hellwig E. Remineralisation of carious enamel lesions after application of a CHX/F-mouthrinse compared with sole CHX- and placebo-application. Oral Health Prev Dent 2006;4(4):255-263. 21. Mendieta C, Vallcorba N, Binney A, Addy M. Comparison of 2 chlorhexidine mouthwashes on plaque regrowth in vivo and dietary staining in vitro. J Clin Periodontol 1994;21(4):296-300. 22. Duarte AR, Peres MA, Vieira RS, Ramos-Jorge ML, Modesto A. Effectiveness of two mouth rinses solutions in arresting caries lesions: A short-term clinical trial. Oral Health Prev Dent 2008;6(3):231-238. 23. Gunsolley JC. A meta-analysis of six-month studies of antiplaque and antigingivitis agents. J Am Dent Assoc 2006;137(12):1649-1657. 24. White DJ, Barker ML, Klukowska M. In vivo antiplaque efficacy of combined antimicrobial dentifrice and rinse hygiene regimens. Am J Dent 2008;21(3):189-196. 25. Zimmer S, Kolbe C, Kaiser G, Krage T, Ommerborn M, Barthel C. Clinical efficacy of flossing versus use of antimicrobial rinses. J Periodontol 2006;77(8):1380-1385. 26. Knishkowy B, Sgan-Cohen HD. Oral health practices among adolescents: A study from family practice clinics in Israel. Int J Adolesc Med Health 2005;17(2):99-104. 27. Roldan S, Herrera D, Santa-Cruz I, OConnor A, Gonzalez I, Sanz M. Comparative effects of different chlorhexidine mouth-rinse formulations on volatile sulphur compounds and salivary bacterial counts. J Clin Periodontol 2004;31(12): 1128-1134. 28. Kolahi J, Soolari A. Rinsing with chlorhexidine gluconate solution after brushing and flossing teeth: A systematic review of effectiveness. Quintessence Int 2006;37(8):605-612. 29. Bascones A, Morante S, Mateos L, Mata M, Poblet J. Influence of additional active ingredients on the effectiveness of non-alcoholic chlorhexidine mouthwashes: A randomized controlled trial. J Periodontol 2005;76(9):1469-1475.
30. Forgie AH, Paterson M, Pine CM, Pitts NB, Nugent ZJ. A randomized controlled trial of the caries-preventive efficacy of a chlorhexidinecontaining varnish in high-caries-risk adolescents. Caries Res 2000;34:432-439. 31. Featherstone JD. Delivery challenges for fluoride, chlorhexidine and xylitol. BMC Oral Health 2006; 6 Suppl 1:S8. 32. de Amorim RG, Leal SC, Bezerra AC, de Amorim FP, de Toledo OA. Association of chlorhexidine and fluoride for plaque control and white spot lesion remineralization in primary dentition. Int J Paediatr Dent 2008;18(6):446-451. 33. Jayaprakash K, Veeresha KL, Hiremath SS. A comparative study of two mouthrinses on plaque and gingivitis in school children in the age group of 13-16 years in Bangalore city. J Indian Soc Pedod Prev Dent 2007;25(3):126-129. 34. Autio-Gold J. The role of chlorhexidine in caries prevention. Oper Dent 2008;33(6):710-716. 35. Newbrun E. Topical fluorides in caries prevention and management: A North American perspective. J Dent Educ 2001;65(10):1078-1083. 36. Torres-Lagares D, Infante-Cossio P, GutierrezPerez JL, Romero-Ruiz MM, Garcia-Calderon M, Serrera-Figallo MA. Intra-alveolar chlorhexidine gel for the prevention of dry socket in mandibular third molar surgery. A pilot study. Med Oral Patol Oral Cir Bucal 2006;11(2):E179-E184. 37. Ben-Yaakov D, Friedman M, Hirschfeld Z, Gedalia I. Fluoride enhancement of chlorhexidine uptake by hydroxyapatite and enamel powders. J Oral Rehabil 1984;11(1):65-70. 38. Ullsfoss BN, Ogaard B, Arends J, Ruben J, Rolla G, Afseth J. Effect of a combined chlorhexidine and NaF mouthrinse: An in vivo human caries model study. Scand J Dent Res 1994;102(2): 109-112. 39. Casals E, Boukpessi T, McQueen CM, Eversole SL, Faller RV. Anticaries potential of commercial dentifrices as determined by fluoridation and remineralization efficiency. J Contemp Dent Pract 2007;8(7):1-10. 40. Pizzo G, Guiglia R, Imburgia M, Pizzo I, DAngelo M, Giuliana G. The effects of antimicrobial sprays and mouthrinses on supragingival plaque regrowth: A comparative study. J Periodontol 2006;77(2):248-256. 41. Sheen S, Addy M. An in vitro evaluation of the availability of cetylpyridinium chloride and chlorhexidine in some commercially available mouthrinse products. Br Dent J 2003;194(4): 207-210.
42. Kozak KM, Gibb R, Dunavent J, White DJ. Efficacy of a high bioavailable cetylpyridinium chloride mouthrinse over a 24-hour period: A plaque imaging study. Am J Dent 2005;18 Spec No:18A-23A. 43. Santos S, Herrera D, Lopez E, OConnor A, Gonzalez I, Sanz M. A randomized clinical trial on the short-term clinical and microbiological effects of the adjunctive use of a 0.05% chlorhexidine mouth rinse for patients in supportive periodontal care. J Clin Periodontol 2004;31 (1):45-51. 44. Eley BM. Antibacterial agents in the control of supragingival plaqueA review. Br Dent J 1999; 186(6):286-296. 45. de Souza LB, de Aquino SG, de Souza PP, Hebling J, Costa CA. Cytotoxic effects of different concentrations of chlorhexidine. Am J Dent 2007; 20(6):400-404. 46. Giannelli M, Chellini F, Margheri M, Tonelli P, Tani A. Effect of chlorhexidine digluconate on different cell types: a molecular and ultrastructural investigation. Toxicol In Vitro 2008;22(2): 308-317. 47. Jeng JH, Hsieh CC, Lan WH, Chang MC, Lin SK, Hahn LJ, Kuo MY. Cytotoxicity of sodium fluoride on human oral mucosal fibroblasts and its mechanisms. Cell Biol Toxicol 1998;14(6):383-389. 48. He LF, Chen JG. DNA damage, apoptosis and cell cycle changes induced by fluoride in rat oral mucosal cells and hepatocytes. World J Gastroenterol 2006;12(7):1144-1148. 49. Kreth J, Zhu L, Merritt J, Shi W, Qi F. Role of sucrose in the fitness of Streptococcus mutans. Oral Microbiol Immunol 2008;23(3):213-219. 50. Mitchell DA, Mitchell L. Oxford handbook of clinical dentistry. In: Mitchell DA, Mitchell L. Periodontology, ed. 4. London: Oxford University Press;2005:202.
Manufacturers
Church & Dwight Co., Inc., Princeton, NJ 800.524.1328, www.churchdwight.com GDK Densell, Buenos Aires, Argentina 054.11.4962.1212, www.densell.com.ar GlaxoSmithKline, Research Triangle Park, NC 888.825.5249, www.gsk.com Platinum Pharmaceuticals, Karachi, Pakistan 92.21.4750.1123, www.platinumpharma.net Roomi Enterprises, Karachi, Pakistan 92.21.1110.16023, www.roomi.com.pk
Comment
www.agd.org
General Dentistry
May/June 2011
e115
S-ar putea să vă placă și
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- Precision Attachments For The 21st CenturyDocument6 paginiPrecision Attachments For The 21st CenturyMohsin Habib67% (3)
- Centric Relation: Handout AbstractsDocument21 paginiCentric Relation: Handout Abstractsizeldien5870Încă nu există evaluări
- Activa White Paper XF Vwp6 Rev 06 2017 3Document12 paginiActiva White Paper XF Vwp6 Rev 06 2017 3obee100% (1)
- Aggressive Periodontitis inDocument5 paginiAggressive Periodontitis inOctavian CiceuÎncă nu există evaluări
- Concepts of Normal OcclusionDocument73 paginiConcepts of Normal OcclusionAditi Singh100% (1)
- Pulpektomy Decidui PaperDocument13 paginiPulpektomy Decidui PaperHenny Eka PutriÎncă nu există evaluări
- Apoc Surg.2007Document23 paginiApoc Surg.2007Henny Eka PutriÎncă nu există evaluări
- Fletcher AM, Purnaveja S, Amin WM, S, Dodd AW. The Evaluation of Water Sorption/Solubility On Various Acrylic Resins. Eur J Dent 2008 2:191-97Document1 paginăFletcher AM, Purnaveja S, Amin WM, S, Dodd AW. The Evaluation of Water Sorption/Solubility On Various Acrylic Resins. Eur J Dent 2008 2:191-97Henny Eka PutriÎncă nu există evaluări
- J K A 2Document4 paginiJ K A 2Henny Eka PutriÎncă nu există evaluări
- Drg. Purwanto-Semen Kedokteran GigiDocument39 paginiDrg. Purwanto-Semen Kedokteran GigiHenny Eka PutriÎncă nu există evaluări
- Data 2003Document6 paginiData 2003Henny Eka PutriÎncă nu există evaluări
- Fletcher AM, Purnaveja S, Amin WM, S, Dodd AW. The Evaluation of Water Sorption/Solubility On Various Acrylic Resins. Eur J Dent 2008 2:191-97Document1 paginăFletcher AM, Purnaveja S, Amin WM, S, Dodd AW. The Evaluation of Water Sorption/Solubility On Various Acrylic Resins. Eur J Dent 2008 2:191-97Henny Eka PutriÎncă nu există evaluări
- Bad HabitDocument28 paginiBad HabitHenny Eka PutriÎncă nu există evaluări
- Paratiroid (PTH)Document23 paginiParatiroid (PTH)Henny Eka PutriÎncă nu există evaluări
- Cap 1Document9 paginiCap 1careÎncă nu există evaluări
- Bad HabitDocument28 paginiBad HabitHenny Eka PutriÎncă nu există evaluări
- Grape Seed Antioxidant ActivityDocument6 paginiGrape Seed Antioxidant ActivityRegina ErikaÎncă nu există evaluări
- 4 GingivitisDocument7 pagini4 GingivitisNur Camelia PragnandaÎncă nu există evaluări
- Silv-Air Classic 2200 - Product Flyer - EnglishDocument1 paginăSilv-Air Classic 2200 - Product Flyer - EnglishHenny Eka PutriÎncă nu există evaluări
- JudulDocument4 paginiJudulHenny Eka PutriÎncă nu există evaluări
- Jurnal 3 HariDocument7 paginiJurnal 3 HariHenny Eka PutriÎncă nu există evaluări
- 619Document1 pagină619Henny Eka PutriÎncă nu există evaluări
- JurnalDocument5 paginiJurnalHenny Eka PutriÎncă nu există evaluări
- Blok 8 LBM 3Document10 paginiBlok 8 LBM 3Henny Eka PutriÎncă nu există evaluări
- Indications, Clinical and Laboratory Stages of Manufacturing of Swaged-Soldered Dental BridgesDocument45 paginiIndications, Clinical and Laboratory Stages of Manufacturing of Swaged-Soldered Dental BridgesMihaela VasiliuÎncă nu există evaluări
- For Preparations of Esthetic Inlay/Onlay Restorations: Technique GuideDocument4 paginiFor Preparations of Esthetic Inlay/Onlay Restorations: Technique GuideliudifairÎncă nu există evaluări
- Voiceless Voiced: Bilabial BilabialDocument4 paginiVoiceless Voiced: Bilabial BilabialAhmed El-SaadanyÎncă nu există evaluări
- The Swing Lock Denture: 1-Too Few Remaining Teeth For A Conventional DesignDocument9 paginiThe Swing Lock Denture: 1-Too Few Remaining Teeth For A Conventional DesignEsmail AhmedÎncă nu există evaluări
- Prosthodontics - Removable Partial Denture: Prepared By: Michelle Ann Z. Zalzos, DMDDocument31 paginiProsthodontics - Removable Partial Denture: Prepared By: Michelle Ann Z. Zalzos, DMDMaryjoy PaladanÎncă nu există evaluări
- Fluoride and Fluoridation: Topical FluoridesDocument3 paginiFluoride and Fluoridation: Topical FluoridesmarkoÎncă nu există evaluări
- Esthetic Restorations-The Putty Matrix TechniqueDocument4 paginiEsthetic Restorations-The Putty Matrix Techniquedentace1Încă nu există evaluări
- Endo-Perio Inter Relationship PerioDocument30 paginiEndo-Perio Inter Relationship PerioFourthMolar.com67% (3)
- Tasaka 2021Document6 paginiTasaka 2021Mostafa EhsanÎncă nu există evaluări
- Waterpik Water Flosser Model WP-450 Hydropropulseur Waterpik Modèle WP-450 Irrigador Bucal Waterpik Modelo WP-450Document48 paginiWaterpik Water Flosser Model WP-450 Hydropropulseur Waterpik Modèle WP-450 Irrigador Bucal Waterpik Modelo WP-450darlene918Încă nu există evaluări
- An Overview of Frenal AttachmentsDocument4 paginiAn Overview of Frenal AttachmentsTrần ThưÎncă nu există evaluări
- Dental PracticeDocument6 paginiDental PracticeAljunBaetiongDiazÎncă nu există evaluări
- Penawaran Harga Cobra, Tatia, Bintang Saudara, AMS, Dental JayaDocument8 paginiPenawaran Harga Cobra, Tatia, Bintang Saudara, AMS, Dental JayanataliaÎncă nu există evaluări
- In The Dental Implant Era, Why Do We Still Bother Saving Teeth?Document8 paginiIn The Dental Implant Era, Why Do We Still Bother Saving Teeth?Gabriela ArgeseanuÎncă nu există evaluări
- Odontogenesis 3Document75 paginiOdontogenesis 3mennaitaÎncă nu există evaluări
- PT Pauh Mandiri Sejahtera: Jl. Manggis Raya No 41 RT 28 RW 06, Panorama, Singaran Pati, Kota Bengkulu, 38226Document3 paginiPT Pauh Mandiri Sejahtera: Jl. Manggis Raya No 41 RT 28 RW 06, Panorama, Singaran Pati, Kota Bengkulu, 38226AINAÎncă nu există evaluări
- 1-Anatomy and Morphology of PulpDocument48 pagini1-Anatomy and Morphology of PulpدرالجمانÎncă nu există evaluări
- LIt274 BL Cement Abut ImprTechniqueDocument2 paginiLIt274 BL Cement Abut ImprTechniqueJean-Christophe PopeÎncă nu există evaluări
- Intrusion of Incisors in Adult Patients With Marginal Bone LossDocument10 paginiIntrusion of Incisors in Adult Patients With Marginal Bone LossYerly Ramirez MuñozÎncă nu există evaluări
- ExtractionDocument89 paginiExtractionTayem KenawyÎncă nu există evaluări
- Nanda Archwires: Science Does Matter!Document2 paginiNanda Archwires: Science Does Matter!aung NaingmyoÎncă nu există evaluări
- WSLDocument67 paginiWSLSwathyÎncă nu există evaluări
- Plaque Control: Presented by DR - Annie Kitty George Dept of PeriodonticsDocument47 paginiPlaque Control: Presented by DR - Annie Kitty George Dept of PeriodonticsDilu DavisÎncă nu există evaluări
- Kelas XIIDocument4 paginiKelas XIINurÎncă nu există evaluări
- Dental Hygienist Schools in OhioDocument4 paginiDental Hygienist Schools in OhiodhsrayÎncă nu există evaluări