Documente Academic
Documente Profesional
Documente Cultură
Postoperative Nursing Care Plan For Cesarian Section Patient Case Pres or
Încărcat de
Loren EstefanDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Postoperative Nursing Care Plan For Cesarian Section Patient Case Pres or
Încărcat de
Loren EstefanDrepturi de autor:
Formate disponibile
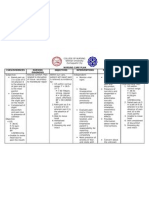
XI. NURSING CARE PLAN Post-operative NCP ASSESSMENT Subjective: Sobrang sakit, as verbalized by the patient.
Objective: -Pain scale= 8/10 -Teary eyed -(+) guarding behavior -(+) facial grimace -Irritable -Pale palpebral conjunctiva -Skin warm to touch follows: BP= 110/80 PR= 80 RR= 22 T= 37.6 DIAGNOSIS Acute pain r/t disruption of skin and tissue secondary to cesarean section. PLANNING INTERVENTION STG: Independent: After 1-2hr of nursing - Established rapport. intervention, patient will verbalize - Monitored vital decrease intensity signs. of pain from 8/10 to 3/10. - Assessed quality, characteristics, severity of pain. RATIONALE OUTCOME Goal met. After 2hrs of nursing intervention, the patient verbalized pain decreased from a scale of 8/10 3/20 as evidenced by (-) facial grimace (-) guarding behavior. Frequent small talks with significant others
-To have a good nurse-client relationship -To establish a baseline data -To establish baseline data for comparison in making evaluation and to assess for possible internal bleeding. -Calm environment helps to decrease the anxiety of the patient and promote likelihood of decreasing pain. - To check for diastasis recti and protect the area of the incision to improve comfort. And to initiate nonstressful muscle-
Provided comfortable environment changed bed linens and turned on the fan.
Instructed to put pillow on the abdomen when coughing or moving.
setting techniques and progress as tolerated, based on the degree of separation. Instructed patient to do deep breathing and coughing exercise. - For pulmonary ventilation, especially when exercising, and to relieve stress and promote relaxation. - To promote circulation, prevent venous stasis, prevent pressure on the operative site.
Provided diversionary activities. Initiate ankle pumping, active lower extremity ROM, and walking Collaborative: Administer analgesic as per doctors order.
-Relieves pain felt by the patient
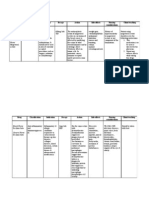
ASSESSMENT Subjective: - none Objective: - dressing dry and intact follows: T: 37.3 P: 80 R: 19 BP: 120/80
DIAGNOSIS Risk for infection related inadequate primary defenses secondary to surgical incision
NURSING ANALYSIS Due to an elective cesarean section, patients skin and tissue were mechanically interrupted. Thus, the wound is at risk of developing infection.
PLANNING STG: After 4 hours of nursing intervention, patient will be able to understand causative factors, identify signs of infection and report them to health care provider accordingly. LTG: After 2-3 days of nursing intervention, patient will achieve timely wound healing, be free of purulent drainage or erythema, be afebrile and be free of infection.
INTERVENTION Independent -Monitor vital signs -Inspect dressing and perform wound care - Monitor white blood count (WB
RATIONALE
EVALUATION
-To establish a baseline data -Moist from drainage can be a source of infection - Rising WBC indicates bodys efforts to combat pathogens; normal values: 4000 to 11,000 mm3 -these are signs of infection
Patient is expected to be free of infection, as evidenced by normal vital signs and absence of purulent drainage from wounds, incisions, and tubes.
- Monitor Elevated temperature, Redness, swelling, increased pain, or purulent drainage at incisions - Wash hands and teach other caregivers to wash hands
-Friction and running water effectively remove microorganisms
before contact with patient and between procedures with patient.
from hands. Washing between procedures reduces the risk of transmitting pathogens from one area of the body to another - Fluids promote diluted urine and frequent emptying of bladder; reducing stasis of urine, in turn, reduces risk of bladder infection or urinary tract infection (UTI). - These measures reduce stasis of secretions in the lungs and bronchial tree. When stasis occurs, pathogens can cause upper respiratory infections, including pneumonia. -Antibiotics have bactericidal effect that combats
- Encourage fluid intake of 2000 ml to 3000 ml of water per day (unless contraindicated).
- Encourage coughing and deep breathing; consider use of incentive spirometer.
Independent: - Administer antibiotics
pathogens
ASSESSMENT Objective Cues: Patient has not yet eliminated since delivery Absence of bruit sounds Normal pattern of bowel has not yet returned
NURSING DIAGNOSIS Risk for constipation r/t post pregnancy 2 cesarean section
PLANNING Short Term Goal: Within 8 of nursing interventions, the patient will be able to demonstrate behaviors or lifestyle changes to prevent developing problem
INTERVENTIONS INDEPENDENT INTERVENTIONS: Ascertain normal bowel functioning of the patient, about how many times a day does she defecate Encourage intake of foods rich in fiber such as fruits
RATIONALE
EVALUATION
Long Term Goal: Within 3 days of
Promote adequate fluid intake. Suggest drinking of warm fluids, especially in the morning to stimulate peristalsis Encourage ambulation such as
After 8 of nursing interventions, This is to determine the the patient was normal bowel able to identify pattern measures to prevent infection To increase the as manifested by bulk of the clients stool and verbalization of: facilitate the Iinom ako ng passage through the maraming tubig colon at kakain ng To promote prutas para moist soft stool makadumi ako.
To stimulate contractions of the intestines
nursing interventions, the patient will be able to maintain usual pattern of bowel functioning
walking within individual limits However, since she has had cesarean, also encourage adequate rest periods
and prevent post operative complications To avoid stress on the cesarean incision/ wound
COLLABORATIVE: Administer bulkforming agents or stool softeners such as laxatives as indicated or prescribed by the physician To promote defecation
S-ar putea să vă placă și
- NCP and DrugsDocument13 paginiNCP and DrugsApRil ANn ChUa BingcangÎncă nu există evaluări
- NCP Acute PainDocument2 paginiNCP Acute PainMimi Nacor100% (3)
- Acute Pain Related To Body Response To An Infective AgentDocument2 paginiAcute Pain Related To Body Response To An Infective AgentSheril Sularte CasanesÎncă nu există evaluări
- NCPDocument3 paginiNCPNika LoÎncă nu există evaluări
- Nursing Care Plan: Silliman UniveristyDocument17 paginiNursing Care Plan: Silliman UniveristyKassandra LabeÎncă nu există evaluări
- NCPDocument6 paginiNCPSarah Younes AtawnehÎncă nu există evaluări
- NURSING CARE PLAN For TB 2003Document6 paginiNURSING CARE PLAN For TB 2003Princess Andrea Bulatao100% (1)
- CHOLElithiasisDocument93 paginiCHOLElithiasisfranciscomaricris13Încă nu există evaluări
- Assessme NT Nursing Diagnosis Planning Nursing Interventions Rationale Evaluation Subjective CuesDocument3 paginiAssessme NT Nursing Diagnosis Planning Nursing Interventions Rationale Evaluation Subjective CuesTricia100% (1)
- NCP Impaired SkinDocument2 paginiNCP Impaired Skinarjay2306_obcq100% (1)
- Buddy WorksDocument3 paginiBuddy WorksJamaica Leslie NovenoÎncă nu există evaluări
- NCP - Acute Pain Stomach CancerDocument2 paginiNCP - Acute Pain Stomach CancerJohn Michael TaylanÎncă nu există evaluări
- ARCOXIADocument22 paginiARCOXIATeresa JunioÎncă nu există evaluări
- Drug Study Pedia WardDocument2 paginiDrug Study Pedia WardCayanne ChuaÎncă nu există evaluări
- Cues Nursing Diagnosis Scientific Reason Objective Nursing Intervention Rationale EvaluationDocument4 paginiCues Nursing Diagnosis Scientific Reason Objective Nursing Intervention Rationale Evaluationjomsportg0% (1)
- NCP Gastric CancerDocument6 paginiNCP Gastric Cancerhayascent hilarioÎncă nu există evaluări
- Case Presentation Station 3B Drug Study TramadolDocument3 paginiCase Presentation Station 3B Drug Study TramadolhahahahaaaaaaaÎncă nu există evaluări
- Impaired Skin IntegrityDocument2 paginiImpaired Skin IntegrityEli AyaseÎncă nu există evaluări
- Drug Study (Paracetamol, Lactulose, Ascorbic Acid)Document6 paginiDrug Study (Paracetamol, Lactulose, Ascorbic Acid)Roland Mark Rodel LagosÎncă nu există evaluări
- Impaired Skin IntegrityDocument4 paginiImpaired Skin IntegrityMarjorie Jofel Cerrudo PaciaÎncă nu există evaluări
- Drug Study - CaDocument3 paginiDrug Study - Casaint_ronald8Încă nu există evaluări
- Ineffective Tissue PerfusionDocument2 paginiIneffective Tissue PerfusionDiane ReyÎncă nu există evaluări
- NCP ImpairedDocument3 paginiNCP ImpairedLyka NgayanÎncă nu există evaluări
- NCP (BPH)Document8 paginiNCP (BPH)NataCo50% (2)
- Drugs Mechanism of Action Nursing Responsibilities OMXDocument5 paginiDrugs Mechanism of Action Nursing Responsibilities OMXEmmanuelRodriguezÎncă nu există evaluări
- CefuroximeDocument2 paginiCefuroximekaijeiÎncă nu există evaluări
- NCP For Pre-Op Incision CaseDocument8 paginiNCP For Pre-Op Incision CaseFAt TyÎncă nu există evaluări
- Nursing Care Plan: Risk For Disuse SyndromeDocument2 paginiNursing Care Plan: Risk For Disuse SyndromeRozsy FakhrurÎncă nu există evaluări
- Infectious Process Secondary To Acute Gastroenteritis Nagtatae Na Talaga Siya", Changed Diaper 3x With Loose and DeformedDocument1 paginăInfectious Process Secondary To Acute Gastroenteritis Nagtatae Na Talaga Siya", Changed Diaper 3x With Loose and DeformedJoshua MendozaÎncă nu există evaluări
- NCPDocument2 paginiNCPNaidin Catherine De Guzman-AlcalaÎncă nu există evaluări
- Impaired Physical Mobility...Document3 paginiImpaired Physical Mobility...Christy BerryÎncă nu există evaluări
- NCP Skin IntegityDocument3 paginiNCP Skin Integityclydell joyce masiarÎncă nu există evaluări
- NCP Sleep DisturbanceDocument1 paginăNCP Sleep DisturbanceIsrael Soria EsperoÎncă nu există evaluări
- NCP InfectionDocument3 paginiNCP InfectionPrince AhmirÎncă nu există evaluări
- This Study Resource Was Shared Via: Nursing Care Plan FormDocument3 paginiThis Study Resource Was Shared Via: Nursing Care Plan FormissaiahnicolleÎncă nu există evaluări
- Problem List Cues Problems Priority JustificationDocument3 paginiProblem List Cues Problems Priority JustificationgrazheÎncă nu există evaluări
- Rheumatoid Arthritis: Case Presentation & Health Teaching PlanDocument32 paginiRheumatoid Arthritis: Case Presentation & Health Teaching PlanJune Faith HacheroÎncă nu există evaluări
- NCP For DRDocument1 paginăNCP For DRvalencia222Încă nu există evaluări
- Surgical NCPDocument6 paginiSurgical NCPAreeya SushmitaÎncă nu există evaluări
- NCPDocument3 paginiNCPJoevelyn LaynoÎncă nu există evaluări
- Acute Pain NCPDocument2 paginiAcute Pain NCPkrz05Încă nu există evaluări
- NCP HyperthermiaDocument2 paginiNCP HyperthermiaMeljonesDaanÎncă nu există evaluări
- Drug Study: CNS: DizzinessDocument1 paginăDrug Study: CNS: Dizzinessmarsh155Încă nu există evaluări
- Acute PainDocument3 paginiAcute PainGerardeanne ReposarÎncă nu există evaluări
- AnxietyDocument3 paginiAnxietyJenny Pearl Pasal100% (1)
- Child - Major Burn PDFDocument3 paginiChild - Major Burn PDFAldith GrahamÎncă nu există evaluări
- NCPDocument6 paginiNCPNoemi GarciaÎncă nu există evaluări
- Fistula NCPDocument1 paginăFistula NCPHasna LisnaÎncă nu există evaluări
- Chicken Pox NCPDocument3 paginiChicken Pox NCPrshin96Încă nu există evaluări
- Drug Study and NCP (Craniotomy)Document2 paginiDrug Study and NCP (Craniotomy)Deinielle Magdangal Romero100% (1)
- NCP Mandibular)Document5 paginiNCP Mandibular)yellarfÎncă nu există evaluări
- Teething:diaper Dermatitis NCPDocument2 paginiTeething:diaper Dermatitis NCPMARK OLVIER E. MELCHORÎncă nu există evaluări
- Case Study NCPDocument4 paginiCase Study NCPKelly OstolÎncă nu există evaluări
- NCP PainDocument2 paginiNCP PainJun TangonanÎncă nu există evaluări
- 5NCPDocument4 pagini5NCPSara ThorntonÎncă nu există evaluări
- NCP CSDocument9 paginiNCP CSFreida Marie PiczonÎncă nu există evaluări
- Nursing Care PlanDocument4 paginiNursing Care PlanJessa BorreÎncă nu există evaluări
- Nursing Care Plan FinalDocument16 paginiNursing Care Plan FinalErickson OcialÎncă nu există evaluări
- Cue Problem Scientific Explanation Planning Interventions Rationale EvaluationDocument5 paginiCue Problem Scientific Explanation Planning Interventions Rationale EvaluationJanyn Abella ReyesÎncă nu există evaluări
- Case Study: Patient With Appendicitis: Submitted By: Farzaneh Yeganeh Submitted To: Ms. Amara SabriDocument19 paginiCase Study: Patient With Appendicitis: Submitted By: Farzaneh Yeganeh Submitted To: Ms. Amara Sabrifarzaneh yeganehÎncă nu există evaluări
- LLM01v5 0Document12 paginiLLM01v5 0Alan LeungÎncă nu există evaluări
- Marlinespike - Rope Breaking StrengthDocument7 paginiMarlinespike - Rope Breaking StrengthAnonymous ycFeyuLAt100% (1)
- PVC Duct DesignDocument10 paginiPVC Duct DesigncitramuaraÎncă nu există evaluări
- A Butterfly Effect Volume 1 (Years 1 - 2)Document362 paginiA Butterfly Effect Volume 1 (Years 1 - 2)xdyj2005Încă nu există evaluări
- Read The Following Paragraphs and Answer The Questions That FollowDocument18 paginiRead The Following Paragraphs and Answer The Questions That FollowMary Ann RanayÎncă nu există evaluări
- 0900-9914 I1 201012 PDFDocument132 pagini0900-9914 I1 201012 PDFIvan Arjona50% (2)
- HP 300s+ Scientific Calculator: Sophisticated Design Ideal For Math and Science StudentsDocument3 paginiHP 300s+ Scientific Calculator: Sophisticated Design Ideal For Math and Science StudentsgemaÎncă nu există evaluări
- Volume 15, Number 2 February 2011Document154 paginiVolume 15, Number 2 February 2011Nicolai BabaliciÎncă nu există evaluări
- User Manual For Emvólio: WWW - Blackfrog.InDocument22 paginiUser Manual For Emvólio: WWW - Blackfrog.InmariaÎncă nu există evaluări
- School of Chemical Engineering - 20Document372 paginiSchool of Chemical Engineering - 20biroutiÎncă nu există evaluări
- Mat11 PDFDocument13 paginiMat11 PDFRaquel Martins E SilvaÎncă nu există evaluări
- A Ongc HRM Summer ProjectDocument58 paginiA Ongc HRM Summer ProjectAmit SunsaraÎncă nu există evaluări
- Handwriting Analysis EbookDocument154 paginiHandwriting Analysis EbookG.100% (5)
- Business Description: Apollo TyresDocument4 paginiBusiness Description: Apollo TyresSrijit SahaÎncă nu există evaluări
- QB Som He306 2015 2016Document23 paginiQB Som He306 2015 2016etayhailuÎncă nu există evaluări
- Book of Bible Answers (Volume 1) - by Doug-BatchelorDocument138 paginiBook of Bible Answers (Volume 1) - by Doug-BatchelorAdventist_Truth100% (3)
- Polymer Structures: Issues To Address..Document34 paginiPolymer Structures: Issues To Address..Eugene Embalzado Jr.Încă nu există evaluări
- Sri Vidya College of Engineering & Technology Virudhunagar: Department: Semester: Vi SUBJECT CODE / Name: CE 6602Document34 paginiSri Vidya College of Engineering & Technology Virudhunagar: Department: Semester: Vi SUBJECT CODE / Name: CE 6602JEYA KUMARÎncă nu există evaluări
- V + V Plus - EN1Document6 paginiV + V Plus - EN1james.anitÎncă nu există evaluări
- Enzymes MCQsDocument2 paginiEnzymes MCQsNobody's PerfectÎncă nu există evaluări
- A. Desplat: Godzilla (2014) - Film Score AnalysisDocument18 paginiA. Desplat: Godzilla (2014) - Film Score AnalysisR.PercacciÎncă nu există evaluări
- MEC Threads ChartDocument12 paginiMEC Threads ChartenricoÎncă nu există evaluări
- Ultrafast Lasers Technology and Applications (Optical Science and CRC 1st Ed., 2002) (ISBN 0824708415), Martin E. Fermann, Almantas Galvanauskas Gregg SuchaDocument797 paginiUltrafast Lasers Technology and Applications (Optical Science and CRC 1st Ed., 2002) (ISBN 0824708415), Martin E. Fermann, Almantas Galvanauskas Gregg SuchaRokas DanilevičiusÎncă nu există evaluări
- Installation Instructions: Harley-Davidson Softail Saddlebag Mount Bracket PART# 21946Document4 paginiInstallation Instructions: Harley-Davidson Softail Saddlebag Mount Bracket PART# 21946Justin StewartÎncă nu există evaluări
- MantrasDocument45 paginiMantrasharibhakta100% (1)
- A Better World - Volume 5Document146 paginiA Better World - Volume 5Zainuddin BusuÎncă nu există evaluări
- Esab Ok 55 (3.2 MM)Document1 paginăEsab Ok 55 (3.2 MM)DHANEESH VELLILAPULLIÎncă nu există evaluări
- DM HSD GU35 URAS2 Technical Guidelines For Usage of Rope Access System V2.1Document20 paginiDM HSD GU35 URAS2 Technical Guidelines For Usage of Rope Access System V2.1Natalie BlackmoreÎncă nu există evaluări
- SMAW Health Hazards of g12 Students During Laboratory ActivitiesDocument25 paginiSMAW Health Hazards of g12 Students During Laboratory ActivitiesPaul Patrick Guanzon100% (1)
- Method Statement For Boom Barrier Installation (Rev00) ELV2Document38 paginiMethod Statement For Boom Barrier Installation (Rev00) ELV2balajiÎncă nu există evaluări