Documente Academic
Documente Profesional
Documente Cultură
6 - Vesiculobullous Diseases
Încărcat de
Prince AhmedDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
6 - Vesiculobullous Diseases
Încărcat de
Prince AhmedDrepturi de autor:
Formate disponibile
Dr.
Tahani Abualteen
Vesiculobullous diseases
Vesiculobullous diseases: Diseases that result in collection of clear fluid (blisters) within or below the epithelium Blisters are classified into (vesicles and bullae) Vesicles: o Fluid filled lesion o Smaller in size o Mostly arise intra-epithelially Bullae: o Fluid filled lesion o Larger in size o Mostly arise sup- epithelially Vesiculobullous diseases are present as oral ulceration following rupture of the vesicles & bullae Classification of vesiculobullous diseases: o Vesiculobullous diseases are classified into 2 major groups depending on the histological location of the lesions: o Intraepithelial vesiculobullous diseases (lesions form within the epithelium): Intraepithelial vesiculobullous diseases are classified into 2 groups depending on the mechanism of formation of the lesion Acantholytic lesions: - Pemphigus vulgaris ** Lesions are produced by breakdown of intercellular attachments (desmosomes) between epithelial cells Non-acantholytic lesions: - Viral infections of the oral mucosa (e.g. ballooning degeneration in herpetic infections) ** Lesions are produced by death and rupture of groups of epithelial cells Pemphigoid Erythema multiforme Dermatitis herpetiformis Linear IgA disease Epidermolysis bullosa Angina bullosa hemorrhagica (oral blood blisters) Bullous lichen planus
o Subepithelial vesiculobullous diseases (lesions form between the epithelium & lamina propria):
History is important o Duration (ulceration lasts weeks to months) o Recurrence o Other lesions: skin, eye, genital lesions o Systemic manifestations o Certain types may be associated with medications
1/10
Dr. Tahani Abualteen
Pemphigus vulgaris: Pemphigus is a group of uncommon autoimmune blistering diseases of which Pemphigus vulgaris is the most common type Classified as intraepithelial acantholytic vesiculobullous disease Clinical features: o Present in middle age o More common in women than in men o More common in certain ethnic groups, particularly Ashkenazi Jews, where there may be a genetic link o Characterized by widespread bullous eruptions involving the skin and mucous membranes o Oral mucosa is involved in nearly all patients and in about 50% of cases is the site of initial lesions o Bullae are fragile (since they are intra-epithelial & not covered with a thick layer of tissue) and so, they readily rupture forming crusted areas on the skin and irregular, ragged mucosal ulcers o Any part of the oral mucosa may be involved, but the soft palate, buccal mucosa, and lips are most frequently affected o There may be also a desquamative gingivitis (a clinical term indicating sloughing and ulceration of attached gingiva that might be a manifestation of different diseases) o Bullae are produced as a result of acantholysis and this process extends laterally in the surrounding epithelium, often for a considerable distance o As a result, gentle lateral pressure to the mucosa in an involved area Nikolsky's sign can lead to the formation of a bulla (Nikolsky's sign) ** Rubbing the oral mucosa gently with a blunt instrument may result (within minutes) in vesicles or bullae formation; and this indicates the presence of immune mechanisms (like Ab attached to desmosomes) that are waiting for maybe a minor trauma to cause damage Histopathological features: o Intraepithelial separation o Cleft-like spaces produced by acantholysis in stratum spinosum cells just above basal cell layer o Basal cells forming the base of the lesion remain attached to the lamina propria o Little subepithelial inflammatory cell infiltration until the lesion ruptures o Acantholytic stratum spinosum cells are small and rounded and contain enlarged hyper-chromatic nuclei (the so called Tzanck cells)
2/10
Dr. Tahani Abualteen
Pathogenesis: o Autoimmune disease autoantibodies against desmosomes ** Desmosome is a junctional complex mediating cell-cell contact ** Desmosome = intercellular attachment plaque + intercellular adhesion protein Intercellular attachment s of epithelial cells are mediated ** Desmogleins are important by desmosomes comprising opposing attachment plaques intercellular adhesion proteins (P) and intercellular adhesion proteins ** Autoantibodies to desmoglein 3 are found in Pemphigus limited to mucosal sites ** Autoantibodies to desmoglein 1 and desmoglein 3 are found Pemphigus involving skin and mucosa o There's strong evidence that IgG autoantibodies against the intercellular proteins of the desmosomes (Ab-Ag complex) are responsible for the acantholysis but the mechanism by which this occurs is unclear! however, it is likely to involve the activity of proteineases Diagnosis: o Immunological studies are important in establishing the diagnosis and may be helpful in monitoring the progression of the disease o Indirect immunoflourescence: Circulating autoantibodies (IgG) to desmosomes can be demonstrated in the serum of patients Their titer is related to the severity of the disease and monitoring the titer over time may be helpful in disease monitoring and response to treatment Circulating autoantibodies may not be detected in all patients (especially in the early stages of the disease) o Direct immunoflourescence: Detection of antibodies while in their place using another florescent antibody Biopsy of peri-lesional mucosa to detect the binding of autoantibodies (IgG) to desmosomes ** IgG autoantibodies can be detected within the epithelial thickness producing a characteristic fish-net pattern Positive in all patients
Other forms of Pemphigus include: o P. vegetans o Drug induced o Paraneoplastic (associated with some malignancies, e.g. leukemia and lymphoma)
3/10
Dr. Tahani Abualteen
Pemphigoid: Pemphigoid is a group of autoimmune blistering diseases characterized by the production of autoantibodies against hemidesmosomes and basement membrane (which mediate attachment between epithelium and underlying connective tissue) Classified as subepithelial vesiculobullous disease The different subtypes and their clinical manifestations most likely reflect damage to different target antigens, however, they can be divided into 2 groups clinically:
Attachment op epithelium to connective tissue is mediated by hemidesmosomes (HD) and proteins of basement membrane zone (BMZ)
o Bullous Pemphigoid (involving skin mainly) o Mucous membrane Pemphigoid (involving mucosa mainly) ** Oral manifestations occur in almost all patients with mucous membrane Pemphigoid group, but they are very uncommon in bullous Pemphigoid Mucous membrane (cicatrical) Pemphigoid: o Etiology: the most common target antigen in mucous membrane Pemphigoid with oral manifestations is a Transmembrane protein bridging the hemidesmosomes and the basement membrane together known as BP antigen 2 o Clinical features: More common in women than in men Oral mucosa is almost always affected (either alone or in association with other mucosae) Bullae occur anywhere on the oral mucosa ** But over 90% of cases involve the gingiva where the condition presents as desquamative gingivitis ** In some patients, desquamative gingivitis is the only manifestation, and thus the condition is then called oral Pemphigoid Bullae are tense and tough (unlike those of Pemphigus vulgaris) since they consist of full thickness-epithelium and thus they remain intact for few days When bullae rupture, they give rise to erosions which heal slowly, sometimes with scarring (hence the other name cicatrical Pemphigoid) Bullae are produced as a result of acantholysis and this process extends laterally in the surrounding epithelium, often for a considerable distance As a result, gentle lateral pressure to the mucosa in an involved area can lead to the formation of a bulla (Nikolsky's sign)
4/10
Dr. Tahani Abualteen
Extraoral lesions: - Mucosa of nose, larynx, pharynx, esophageous, and genitalia - Skin - Conjunctiva: may cause blindness ** Ocular involvement is the most serious complication with scarring leading to opacity of the cornea and blindness Subepithelial separation (separation of the full thickness of the epithelium from the lamina propria) Initially, there's no evidence of an inflammatory reaction in the lamina propria Later on, as the bulla develops, there's infiltration by variable numbers of neutrophils & Eosinophils around and within the developing bulla Peri-vascular lymphocytic infiltrate in the lamina propria Release of proteases from neutrophils and Eosinophils enhances bulla formation in the basement membrane zone Immunological studies are important in establishing the diagnosis and may be helpful in monitoring the progression of the disease Indirect immunoflourescence: Circulating autoantibodies (IgG) to basement membrane antigens were seldom identified in the past by routine techniques, but using the modern techniques, they can now be detected in the serum of about 80% of patients - Their titer is related to the severity of the disease and monitoring the titer over time may be helpful in disease monitoring and response to treatment Direct immunoflourescence: Biopsy of peri-lesional mucosa to detect the binding of autoantibodies (IgG) to basement membrane zone Shows linear deposition of IgG and C3 in the basement membrane Positive in all patients -
o Histopathological features:
o Diagnosis:
o Treatment: topical and/or systemic corticosteroids o Prognosis: good, but monitor eye lesions
5/10
Dr. Tahani Abualteen
Erythema multiforme: A disease of sudden onset involving skin and mucous membranes and has a wide range of clinical presentations (hence the name multiforme) Clinical features: o Mainly in young adults o More common in males than in females o There may or may not be a Prodromal phase with upper respiratory infection, headache, malaise, nausea o Severity of the disease varies considerably In its severe form, the Stevens-Johnson syndrome, there's widespread involvement of the skin and oral, genital, and ocular mucosae ** Ocular involvement can lead to conjunctiva scarring and visual impairment Milder forms may involve the oral mucosa (with or without skin lesions) or the skin alone may be involved o Disease tends to subside after 10-14 days but recurrence may occur o Recurrent Erythema multiforme is associated in particular with recurrent attacks of herpes simplex virus infection o Skin lesions: Have variety of forms, including: erythematous maculopapular rashes and vesiculobullous eruptions in addition to the characteristic diagnostic target or iris lesions Target "iris" lesions consist of concentric rings of varying Erythema, in the center of which may be an intact or ruptured and crusted bulla Hands and feet are most commonly involved o Oral lesions: Involve any part of the mucosa Lips and anterior parts of the mouth are most commonly affected Appearance of lesions varies with time Erythematous patches are quickly followed by vesiculobullous eruptions which rapidly breakdown into erosions as the bullae disintegrate Erosions on the lips are associated with bleeding and crusting Circumoral crusting hemorrhagic lesions are an important sign to reach clinical diagnosis Pathogenesis: o Unknown (not fully understood)
6/10
Dr. Tahani Abualteen
o Has been suggested that the disease represents a type III hypersensitivity reaction and that the manifestations maybe related to deposition of immune complexes in which the antigen may be of drug, bacterial, or viral origin o Ag - Ab complexes have been detected in Erythema Multiforme and in some cases they have been associated with HSV infection ** Ag - Ab complexes deposition complement activation neutrophils chemotaxis Vasculitis epithelial damage o Many precipitating factors have been identified including drugs (especially sulphonamides & penicillin) and preceding infection (especially herpes simplex infection) o Many cases appear to arise spontaneously Diagnosis: o Diagnosis is primarily clinical o Microscopic features are not diagnostic May result in intraepithelial or subepithelial separation No autoantibodies, so negative direct & indirect immunoflourescence Treatment and prognosis: o o o o Remove causative drugs, if any Topical and systemic corticosteroids May be recurrent May benefit from prophylactic acyclovir
Dermatitis herpetiformis: A chronic, intensely pruritic autoimmune blistering disease of skin Classified as sub-epithelial vesiculobullous disease Primarily skin disease, but oral manifestations are variable and range from symptomless erythematous areas to extensive erosions About 90% of patients with dermatitis herpetiformis have gluten hypersensitivity Biopsy shows: subepithelial separation and granular accumulation of neutrophils Direct immunoflourescence studies show granular deposits of IgA in the tips of the connective tissue papillae together with some complement component, principally C3 Indirect immunoflourescence studies are negative Pathogenesis: activation of complement system and neutrophils chemotaxis
Linear IgA disease: Rare autoimmune blistering disease of skin Classified as subepithelial vesiculobullous disease Primarily skin disease, but oral involvement is occasional Clinically, this disease overlaps with dermatitis herpetiformis & bullous Pemphigoid (differential diagnoses) About 30% of patients with Linear IgA disease have gluten hypersensitivity
7/10
Dr. Tahani Abualteen
Biopsy shows: subepithelial separation Direct immunoflourescence studies show linear IgA along basement membrane Indirect immunoflourescence studies show the circulating autoantibodies (IgA) to basement membrane antigens in the serum of about 30% of patients
Epidermolysis Bullosa: The inherited forms of Epidermolysis bullosa form a complex group of syndromes They are due to mutation in the genes coding either for specific keratins in the basal epithelial layer (resulting in intraepithelial separation) or for various collagens and other attachment proteins in the basement membrane (resulting in subepithelial separation) Clinical features: o Skin lesions: Formation of skin bullae which may manifest at birth or shortly afterwards Extreme fragility of the skin Bullae usually develop in response to minimal trauma or pressure but they may arise spontaneously Hands, feet, knees, elbows are common sites Bullae tend to heal slowly with scarring which can result in claw-like deformity of the hands
o Oral lesions: Oral and other mucosae may be involved Bullae tend to heal slowly with scarring which can result in difficulty in eating, speaking, and swallowing as a result of involvement of the mouth, larynx and pharynx Oral lesions may appear in neonates in response to suckling, and later on minimal trauma from tooth brushing and routine dental treatment can cause serious consequences Bullae rupture to leave painful erosions and subsequent scarring can restrict the opening of the mouth, movement of lips and tongue, and cause obliteration of the sulci Effective oral hygiene may be impossible and rampant caries add to the dental complications
8/10
Dr. Tahani Abualteen
TYPES OF EPIDERMOLYSIS BULLOSA: o o o o Simplex localized skin lesions; oral lesions, good prognosis Dystrophic dominant nails; oral lesions; scarring; fair prognosis Dystrophic recessive severe skin and oral lesions, scarring, abnormal teeth, poor prognosis Junctional severe skin and oral lesions, abnormal teeth, fatal
Treatment: o Avoid trauma o Antibiotics, corticosteroids Prognosis: o Simplex: good o Recessive & Junctional: fatal
Epidermolysis bullosa acquisita: Uncommon autoimmune blistering disease Acquired in adult life Classified as subepithelial vesiculobullous disease Lesions arise mostly on the trauma-prone areas, such as: elbows and knees Oral lesions may occur Biopsy shows: subepithelial separation Direct immunoflourescence studies show linear deposition of IgG and C3 in the basement membrane Indirect immunoflourescence studies show the circulating autoantibodies (IgG) to basement membrane antigens in the serum of about 30-40% of patients
Angina Bullosa Hemorrhagica (oral blood blister): Spontaneous blood filled bullae Occasionally develop on the oral mucosa Usually solitary Middle aged or elderly Occur on any part of the oral mucosa Soft palate is the most commonly involved Cause is unknown, but bullae may be related to trauma Biopsy shows: subepithelial separation No autoantibodies, so negative direct & indirect immunoflourescence
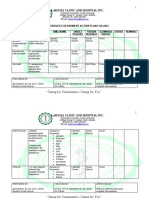
Treatment of non-microbial mucositis with corticosteroids: Mouth rinse o Triamcinolone acetonide Ointment o Triamcinolone acetonide o Fluocinonide (Lidex)
9/10
Dr. Tahani Abualteen
o Clobetasol Systemic Steroids o Prednisone o Contraindicated in certain systemic diseases Intralesional Steroids Triamcinolone acetonide, inject 10-40 mg Anesthetize area before injection of steroid
Differential diagnosis of subepithelial separation: 1234567Pemphigoid Bullous lichen planus Linear IgA disease Dermatitis herpetiformis Epidermolysis bullosa (both forms) Erythema multiforme Angina bullosa hemorrhagica
Differential diagnosis of desquamative gingivitis: 12345Mucous membrane Pemphigoid Pemphigus vulgaris Erosive lichen planus Allergic reaction Drug induced
11/10
S-ar putea să vă placă și
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (894)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- Checklist For Writing Audit Proof IepsDocument2 paginiChecklist For Writing Audit Proof Iepsapi-2307242610% (1)
- 1st Week ReflectionDocument2 pagini1st Week Reflectionacharyaamrit0780% (5)
- Salivary Gland Radiology PresentationDocument40 paginiSalivary Gland Radiology PresentationPrince AhmedÎncă nu există evaluări
- Salivary Gland - Part3Document27 paginiSalivary Gland - Part3Prince AhmedÎncă nu există evaluări
- Chapter 2Document1 paginăChapter 2Prince AhmedÎncă nu există evaluări
- Cons VII Script 1 Bleaching Discolored TeethDocument19 paginiCons VII Script 1 Bleaching Discolored TeethPrince AhmedÎncă nu există evaluări
- Abdomen LabDocument140 paginiAbdomen LabPrince AhmedÎncă nu există evaluări
- O.M II Script 1 PigmentationsDocument16 paginiO.M II Script 1 PigmentationsPrince AhmedÎncă nu există evaluări
- Thorax Lab... ZezoDocument104 paginiThorax Lab... ZezoPrince AhmedÎncă nu există evaluări
- Edition CH #23 Other Bone Diseases: Stuart C. White & Michael J. PharoahDocument21 paginiEdition CH #23 Other Bone Diseases: Stuart C. White & Michael J. PharoahPrince AhmedÎncă nu există evaluări
- Craniofacial Anomalies Part 3Document17 paginiCraniofacial Anomalies Part 3Prince AhmedÎncă nu există evaluări
- 6,8,9Document1 pagină6,8,9Prince AhmedÎncă nu există evaluări
- Oral Surgery Script 1 Facial TraumaDocument13 paginiOral Surgery Script 1 Facial TraumaPrince AhmedÎncă nu există evaluări
- Chapter 3,4Document1 paginăChapter 3,4Prince AhmedÎncă nu există evaluări
- Ortho 1Document9 paginiOrtho 1Prince AhmedÎncă nu există evaluări
- Implant Script 1implants History DefinitionDocument10 paginiImplant Script 1implants History DefinitionPrince AhmedÎncă nu există evaluări
- 1 Occlusal SplintsDocument17 pagini1 Occlusal SplintsPrince AhmedÎncă nu există evaluări
- 1 PrognosisDocument13 pagini1 PrognosisPrince AhmedÎncă nu există evaluări
- Developmental Disturbances of The Face and Jaws (Part 1) : By: Nasuha MaarifDocument33 paginiDevelopmental Disturbances of The Face and Jaws (Part 1) : By: Nasuha MaarifPrince AhmedÎncă nu există evaluări
- Pedo V Script 1management of Developing OcclusionDocument12 paginiPedo V Script 1management of Developing OcclusionPrince AhmedÎncă nu există evaluări
- Developmental Disturbances of The Face and Jaws (Part 1) : By: Nasuha MaarifDocument33 paginiDevelopmental Disturbances of The Face and Jaws (Part 1) : By: Nasuha MaarifPrince AhmedÎncă nu există evaluări
- 1 Occlusal SplintsDocument17 pagini1 Occlusal SplintsPrince AhmedÎncă nu există evaluări
- O.M II Script 1 PigmentationsDocument16 paginiO.M II Script 1 PigmentationsPrince AhmedÎncă nu există evaluări
- 1 PrognosisDocument13 pagini1 PrognosisPrince AhmedÎncă nu există evaluări
- Cons VII Script 1 Bleaching Discolored TeethDocument19 paginiCons VII Script 1 Bleaching Discolored TeethPrince AhmedÎncă nu există evaluări
- Pedo V Script 1management of Developing OcclusionDocument12 paginiPedo V Script 1management of Developing OcclusionPrince AhmedÎncă nu există evaluări
- Implant Script 1implants History DefinitionDocument10 paginiImplant Script 1implants History DefinitionPrince AhmedÎncă nu există evaluări
- Lab Prostho 10Document13 paginiLab Prostho 10Prince AhmedÎncă nu există evaluări
- Ortho 1Document9 paginiOrtho 1Prince AhmedÎncă nu există evaluări
- Oral Surgery Script 1 Facial TraumaDocument13 paginiOral Surgery Script 1 Facial TraumaPrince AhmedÎncă nu există evaluări
- Prosthodontics Laboratory 8 (Corrected)Document38 paginiProsthodontics Laboratory 8 (Corrected)Prince AhmedÎncă nu există evaluări
- Prostho II LAB 2Document27 paginiProstho II LAB 2Prince AhmedÎncă nu există evaluări
- Konsult Sip ReportDocument72 paginiKonsult Sip ReportMohit AgarwalÎncă nu există evaluări
- Causes and Treatment of Onychauxis or Nail HypertrophyDocument3 paginiCauses and Treatment of Onychauxis or Nail HypertrophyKathleen BazarÎncă nu există evaluări
- Jme by Country May2023Document347 paginiJme by Country May2023kaysbookishÎncă nu există evaluări
- Legacy of Tuskegee Syphilis StudyDocument2 paginiLegacy of Tuskegee Syphilis StudyLcgessamanÎncă nu există evaluări
- Iringan (1st Activity PHED 112)Document2 paginiIringan (1st Activity PHED 112)Juliezel IringanÎncă nu există evaluări
- Obstetrics 4Document9 paginiObstetrics 4Darrel Allan MandiasÎncă nu există evaluări
- Clinical Manifestation, DiagnosisDocument13 paginiClinical Manifestation, DiagnosisGeorgiana BlagociÎncă nu există evaluări
- Window of Tolerance GuideDocument19 paginiWindow of Tolerance GuideLê Trung DũngÎncă nu există evaluări
- Beat COVID-19 Situationer #004 (May 1)Document9 paginiBeat COVID-19 Situationer #004 (May 1)Glomarie Alyssa RacelisÎncă nu există evaluări
- A Materia Medica Comparison of Bowel Nosodes and Related Homoeopathic RemediesDocument211 paginiA Materia Medica Comparison of Bowel Nosodes and Related Homoeopathic RemediesjakÎncă nu există evaluări
- 243 471 1 SM PDFDocument6 pagini243 471 1 SM PDFFia lutfiahÎncă nu există evaluări
- 0 Notes 190815 204331 f4b PDFDocument4 pagini0 Notes 190815 204331 f4b PDFLovejeet KaurÎncă nu există evaluări
- Acute Care Surgery: Aryono D.Pusponegoro Warko KarnadihardjaDocument9 paginiAcute Care Surgery: Aryono D.Pusponegoro Warko KarnadihardjaDimas ErlanggaÎncă nu există evaluări
- NCM 105 SyllabusDocument5 paginiNCM 105 SyllabusHazel Rose0% (1)
- History and Mental Status Exam GuideDocument17 paginiHistory and Mental Status Exam Guideyeney armenterosÎncă nu există evaluări
- IBM India Benefits - Emergency Transport Assistance GuidelinesDocument6 paginiIBM India Benefits - Emergency Transport Assistance GuidelinesSushovan NandiÎncă nu există evaluări
- NURS FPX 6618 Assessment 1 Planning and Presenting A Care Coordination ProjectDocument5 paginiNURS FPX 6618 Assessment 1 Planning and Presenting A Care Coordination ProjectEmma WatsonÎncă nu există evaluări
- Specifications For Civic Education in Primary School PDFDocument44 paginiSpecifications For Civic Education in Primary School PDFNordiana Abd RahmanÎncă nu există evaluări
- Unit 1: Testing and Assessment: 1.0 Learning OutcomesDocument14 paginiUnit 1: Testing and Assessment: 1.0 Learning OutcomesJoshua Miguel L. BarrosÎncă nu există evaluări
- Medikolegal Swamedikasi PenyakitDocument8 paginiMedikolegal Swamedikasi PenyakitMiftahul JannahÎncă nu există evaluări
- Health Talk On ContraceptionDocument32 paginiHealth Talk On Contraceptionvaishali TMU studentÎncă nu există evaluări
- Press Release On Generic Medicine in English - 14-8-23Document2 paginiPress Release On Generic Medicine in English - 14-8-23dinesh saigalÎncă nu există evaluări
- ETHICSDocument18 paginiETHICSMichelle MunozÎncă nu există evaluări
- COVID-19 Vaccine Arrives in IndonesiaDocument3 paginiCOVID-19 Vaccine Arrives in Indonesiawawan budiantoÎncă nu există evaluări
- SOCIAL SERVICES aCTION PLAN FOR 2022Document6 paginiSOCIAL SERVICES aCTION PLAN FOR 2022Rocel Cañete Ordoyo-GabrielÎncă nu există evaluări
- Approaches To The Diagnosis of Portal HipertensionDocument12 paginiApproaches To The Diagnosis of Portal HipertensionValentina IorgaÎncă nu există evaluări
- PWC Case Study Tutorial 2021Document17 paginiPWC Case Study Tutorial 2021Anna PrasitdamrongÎncă nu există evaluări
- Dme Information Form Cms-10125 - External Infusion PumpsDocument2 paginiDme Information Form Cms-10125 - External Infusion PumpsSonof GoddÎncă nu există evaluări