Documente Academic
Documente Profesional
Documente Cultură
Studying Diagnosis
Încărcat de
Camilo Parra CuadrosDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Studying Diagnosis
Încărcat de
Camilo Parra CuadrosDrepturi de autor:
Formate disponibile
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Module 2
Epidemiology and Evidence Based Practice: Designs Lecture 6
Probabilistic research II: Studying diagnosis
1
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Learning objectives Lecture 6
Student can describe and explain the analysis of research studying diagnosis, i.e. sensitivity/specificity, predictive values, likelihood ratios, ROC-curves Student can name methodological issues concerning internal and external validity in research studying diagnosis
2
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Agenda
1. Intro diagnostics 2. Studying Diagnosis: analysis (sensitivity/specificity, predictive values, likelihood ratios, ROC-curves) 3. Studying Diagnosis: methodology (cross-sectional design)
3
Universitaire Masterstudie Evidence Based Practice AMC-UvA
1. Intro diagnostics
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Probabilistic research
Predictive relation between one or more determinants and one (diagnosis) or more (prognosis) outcomes Descriptive No interest in confounding Data collection reflects practice Prognosis, Diagnosis
5
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Diagnosis
Predicting the presence, type, severity of disease based on patients profile
Individual prediction based on clinical profile Preferably multiple determinants (i.e. tests) Often one outcome Transversal
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Diagnostic reasoning
Descriptive - pattern recognition - hypothesis testing Probabilistic - rational and quantitative - from pre-test to post-test probabilities
7
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Thomas Bayes (1702-1761)
Estimating probabilities from new data using pre-existing knowledge Bayes theorem:
Post-test probability = Pre-test probability * X
8
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Clinical decision-making
Will the results of the test move a decision across the test (1) or treatment (2) threshold?
Do not test Do not treat Test and, depending on the results, treat (or not) Do not test, but treat now!
pre-test probability
Multistage, multidimensional diagnostic process
Therapy
Patient Outcomes
Presenting symptoms
History & Examination
Further Testing 1
Further Testing 2
No therapy
Patient Outcomes
Cave: focus on single disease
True positives [p*seA]
Treat
risk reduction as observed in trial + risk side effects risk side effects, no treatment effect
False positives [(1-p)*(1-specA)] Test A False negatives [p*(1-seA)] True negatives [(1-p)*spA]
Treat
No Treat risk untreated No Treat none
Test A or B?
True positives [p*seB] False positives [(1-p)*(1-specB)] Test B False negatives [p*(1-seB)] p = prevalence se = sensitivity sp = specificity
Treat
risk reduction as observed in trial + risk side effects risk side effects, no treatment effect
Treat
No Treat risk untreated
True negatives [(1-p)*spB]
No Treat none
Sutton et al. Integration of meta-analysis and economic decision modelling for evaluating tests. MDM 2008
Universitaire Masterstudie Evidence Based Practice AMC-UvA
1. Classical diagnostic thinking
Uni- or multivariable approach:
probability of disease being present given clinical profile one or multiple pieces of information estimate independent contribution (weight) uni- or multivariable analysis clinical decision rules Goal: better prediction/discrimination
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Tests can be
history physical examination blood tests imaging procedures questionnaires etcetera
Universitaire Masterstudie Evidence Based Practice AMC-UvA
2.
Studying Diagnosis: analysis
14
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Diagnostic accuracy
The extent to which the test results reflect the true state The ability of a test to discriminate among patients with and without the suspected disease
How accurate is the test?
Reference test
Patient t n ie t a P la m r o N
TP True Positive
Normal
FP False Positive Threshold
t s e t x e d n I
FN False Negative
TN True Negative
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Basic design
Patients with a suspected disease
Index test Reference test (gold standard) Compare test results
17
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Clinical problem
Patient with chest pain suggestive for acute myocardial infarction (AMI) Does this patient have an AMI?
18
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Clinical problem
Diagnostic value of creatine kinase (CK) measurement Does CK measurement distinguish between those with and without myocardial infarction?
19
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Anatomy of the study
Target population: patients with chest pain Index test: CK measurement Target condition: acute myocardial infarction Final diagnosis based on WHO criteria (reference standard):
clinical outcome ECG-changes enzym values autopsy
20
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Our example
Patients with chest pain CK measurement WHO criteria for AMI Cross-classification
21
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Results of CK study
AMI Present high (>80) low 215 ab cd 15 230 114 130 129 360
22
Absent 16 231
CK
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Measures of accuracy
sensitivity 215 / 230 = 93% < Pr(T+|D+) > specificity 114 / 130 = 88% < Pr(T-|D-) >
AMI Present high (>80) low 215 15 230 Absent 16 114 130 231 129 360
23
CK
Cut-off value
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Accuracy: Sens/Spec
dichotomous test outcomes depend on cut-off value (trade-off; FP/FN) independent of disease prevalence Se/Sp of a single test may vary widely across studies Se/Sp: from disease status to test result (testing the test)
25
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Measures of accuracy
PPV 215 / 231 = 93% < Pr(D+|T+) > NPV 114 / 129 = 88% < Pr(D-|T-) >
AMI Present high (>80) low 215 15 230 Absent 16 114 130 231 129 360
26
CK
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Prevalence
Prevalence: percentage of patients with the target disorder at a certain point in time
formula: (TP + FN) / N
reference positive index test positive negative TP FN TP+FN / standard negative FP TN FP+TN TP+FP FN+TN N
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Effect of prevalence on measures of outcome
D-dimer test in GP practice (low prevalence DVT) D-dimer test in academic hospital (high prevalence DVT)
Universitaire Masterstudie Evidence Based Practice AMC-UvA
High prevalence
DVT D-dimer positive negative 215 15 230 no DVT 16 114 130 231 129 360
prevalence = 230 / 360 = 64% Sens = 215 / 230 = 0.93 Spec = 114 / 130 = 0.88 PPV = 215 / 231 = 0.93 NPV = 114 / 129 = 0.88
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Low prevalence
DVT D-dimer positive negative 215 15 230 no DVT 248 1822 2070 463 1837 2300
prevalence = 230 / 2300 = 10% Sens = 215 / 230 = 0.93 Spec = 1822 / 2070 = 0.88 PPV = 215 / 463 = 0.46 NPV = 1822 / 1837 = 0.99
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Accuracy: PVs
post-test probabilities dichotomous test outcomes depend on Se/Sp dependent upon prevalence PVs: from test result to disease status (testing the patient)
31
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Estimating post-test probabilities
Unknown prevalence:
- SpPin/SnNout
Known prevalence:
- directly use PVs (similar prevalence) - calculate PVs using Se/Sp (prevalence not similar) - use likelihood ratios (LR +/-)
32
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Unknown prevalence: ruling out the target disorder
If a test has a sufficiently high Sensitivity, a Negative result rules out the target disorder the rule of SnNout low FN rate
e.g. breast cancer screening
TP FN
FP TN
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Unknown prevalence: ruling in the target disorder
If a test has a sufficiently high Specificity, a Positive result rules in the target disorder the rule of SpPin low FP rate
TP FN
FP TN
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Likelihood ratios
Direct link from pre-test probabilities to post-test probabilities Applicable in situations with more than two test outcomes
35
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Likelihood ratios
Summarize predictive power of a test result in a single measure Likelihood ratio of a positive and negative test result How more often a positive test result occurs in persons with compared to those without the target condition
36
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Positive likelihood ratio
Likelihood ratio of a positive test result
How more likely a positive test result is in persons with the target condition compared to those without the target condition
37
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Positive likelihood ratio
LR + = Pr(T + | D +) 215 / 230 = = 7.6 Pr(T + | D ) 16 / 130
AMI Present high (>80) low 215 15 230 Absent 16 114 130 231 129 360
38
CK
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Negative likelihood ratio
Likelihood ratio of a negative test result
How less likely a negative test result is in persons with the target condition compared to those without the target condition
39
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Negative likelihood ratio
LR = Pr(T | D +) 15 / 230 = = 0.07 Pr(T | D ) 114 / 130
AMI Present high (>80) low 215 15 230 Absent 16 114 130 231 129 360
40
CK
Universitaire Masterstudie Evidence Based Practice AMC-UvA
93% LR+ = 7.6
64%
41
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Advantages of likelihood ratios
Relatively stable (function of Se/Sp) Still useful when there are more than two test outcomes
42
Universitaire Masterstudie Evidence Based Practice AMC-UvA
CK is a continuous measurement
Dichotomisation of CK (high vs low) means loss of information Higher values of CK are more indicative of myocardial infarction
43
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Results of CK study
MI CK 280 80-279 40-79 1 - 39 Total Present 97 118 13 2 230 Absent 1 15 26 88 130 Total 98 133 39 90 360
44
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Likelihood ratios
Stratum-specific likelihood ratios in case of more than two test results
Pr(T = x | D +) Pr(T = x | D )
LR (T = x ) =
45
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Stratum-specific likelihood ratios
LR (CK 280) = Pr(CK 280 | D +) 97 / 230 = = 54.8 Pr(CK 280 | D ) 1 / 130
MI CK 280 80-279 40-79 1 - 39 Total Present 97 118 13 2 230 Absent 1 15 26 88 130
46
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Stratum-specific likelihood ratios
MI CK 280 80-279 40-79 1 - 39 Total Present 97 118 13 2 230 Absent 1 15 26 88 130 LR 54.83 4.45 0.28 0.01 360
47
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Bayes rule
Post-test odds for disease = Pre-test odds for disease * Likelihood ratio
48
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Bayes rule
odds = probability / (1 probability)
Odds( D + ) =
Pr( D + ) 1 Pr( D +)
probability = odds / (1 + odds)
Pr ( D +) =
Odds( D + ) 1 + Odds( D + )
49
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Bayes rule: patient with CK between 80-279
Pre-test probability = 0.5 Pre-test odds = 0.5 / (1-0.5) = 1 LR(CK 80-279) = 4.45 Post-test odds = 1 * 4.45 = 4.45 Post-test probability = 4.45 / (1+4.45) = 0.82
50
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Bayes rule: patient with CK lower than 40
Pre-test probability = 0.5 Pre-test odds = 0.5 / (1-0.5) = 1 LR(CK < 40) = 0.013 Post-test odds = 1 * 0.013 = 0.013 Post-test probability = 0.013 / (1+0.013) = 0.013
51
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Probability of MI after CK
Pre-test prob. CK 280 80 - 279 40-79 1-39 LR 50% Post test prob. 54.83 4.45 0.28 0.013 98% 82% 22% 1%
52
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Probability of MI after CK
Pre-test prob. CK LR 5% 50% Post test prob. 280 80 - 279 40-79 1-39 54.83 4.45 0.28 0.013 74% 19% 1% 0% 98% 82% 22% 1%
53
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Classification of LR values
>10 and <0.1: large and conclusive changes 5-10 and 0.1-0.2: moderate 2-5 and 0.5-0.2: small (but sometimes important) 1-2 and 0.5-1: small (and rarely important)
54
Universitaire Masterstudie Evidence Based Practice AMC-UvA
ROC-curve
ROC stands for Receiver Operating Characteristic ROC-curve shows the pairs of sensitivity and specificity that correspond to various cut-off points for the continuous test result
55
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Cut-off value
MI absent
MI-patients
TN
FP CK measurement
56
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Cut-off value
MI absent
MI-patients
FN
TP
CK measurement
57
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Change in cut-off value
MI absent
MI present
FP Spec
CK measurement
58
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Change in cut-off value
MI absent
MI present
FN Sens
CK measurement
59
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Change in cut-off value and effect on Se/Sp
Cut-off 9999 280 80 40 1 Sensitivity 0.0% 42.2% 93.5% 99.1% 100.0% Specificity 100.0% 99.2% 87.7% 67.7% 0.0%
60
Universitaire Masterstudie Evidence Based Practice AMC-UvA
ROC-curve CK
100% 80% Sensitivity 60% 40% 20% 0% 0% 20% 40% 60% 1-specificity 80% 100%
61
Cut-off: 80
Cut-off: 280
Universitaire Masterstudie Evidence Based Practice AMC-UvA
ROC-curve
AUC 0.91
62
Universitaire Masterstudie Evidence Based Practice AMC-UvA
ROC-curve
Shows the effect of different cut-off values on sensitivity and specificity Better tests have curves that lie closer to the upper left corner Area Under the ROC-Curve (AUC) is a single measure of test performance (0-1, higher is better)
63
Universitaire Masterstudie Evidence Based Practice AMC-UvA
So far,
Accuracy: how close to the true state? - measures of prediction (Se/Sp, PVs, LRs) Accuracy: distinguishing between patients - measures of discrimination (DOR, ROC with AUC)
64
Universitaire Masterstudie Evidence Based Practice AMC-UvA
3.
Studying Diagnosis: methodology
65
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Basic design
Patients with a suspected disease
Index test Reference test (gold standard) Compare test results
66
Universitaire Masterstudie Evidence Based Practice AMC-UvA
67
Whiting P et al. Ann Intern Med 2004;140:189-202
Universitaire Masterstudie Evidence Based Practice AMC-UvA
2. More modern diagnostic thinking
Determine the most likely role and position of a new test within the test-treatment pathway relative to current practice
- replacement, add-on, triage
Compare differences in:
- test safety etc. - Se/Sp - treated population - management following positive (TP/FP) and negative (TN/FN) test results - treatment effects - patient outcomes
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Roles of tests and positions in existing diagnostic pathways
Bossuyt et al. BMJ 2006;332:1089-92
Copyright 2006 BMJ Publishing Group Ltd.
69
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Test evaluation research
70
Van den Bruel et al. J Clin Epidemiol 2007;60:1116-22
Universitaire Masterstudie Evidence Based Practice AMC-UvA
Further reading
Knottnerus JA, Buntinx F (Ed.). The evidence base of clinical diagnosis. Theory and methods of diagnostic research, 2e edition. Blackwell Publishing, 2009
Newman TB, Kohn MA. Evidence-based diagnosis. Cambridge University Press, 2009
S-ar putea să vă placă și
- Epi & StatisticsDocument135 paginiEpi & StatisticsFatma AlSayeghÎncă nu există evaluări
- Diagnostic Test DesignDocument30 paginiDiagnostic Test DesignDika Gita PratamaÎncă nu există evaluări
- Screening of DiseasesDocument50 paginiScreening of Diseasesravi_rohilla100% (1)
- Evidence Based Medicine: Kiki Lukman, Bagian Bedah Fakultas Kedokteran UNPAD/ RS DR Hasan Sadikin BandungDocument70 paginiEvidence Based Medicine: Kiki Lukman, Bagian Bedah Fakultas Kedokteran UNPAD/ RS DR Hasan Sadikin BandungOby BedahÎncă nu există evaluări
- Diagnostic TestDocument26 paginiDiagnostic Testefmed2001Încă nu există evaluări
- Protokol Critical ApraisalDocument16 paginiProtokol Critical ApraisalMustika ayu lestariÎncă nu există evaluări
- Study of Diagnostic Test - Mirawati SudiroDocument32 paginiStudy of Diagnostic Test - Mirawati SudiroAVG2011Încă nu există evaluări
- Critical Appraisal: On Article of Diagnostic Test (EBM-Diagnostic)Document28 paginiCritical Appraisal: On Article of Diagnostic Test (EBM-Diagnostic)Giovan GaulÎncă nu există evaluări
- Lecture 8 and 9 Slides DiagnosisDocument35 paginiLecture 8 and 9 Slides DiagnosisJustDen09100% (1)
- Diagnosis: Research Methods Dent 313Document35 paginiDiagnosis: Research Methods Dent 313Rmz StudyÎncă nu există evaluări
- Screening: Department of Public Health Medical School, University of PécsDocument38 paginiScreening: Department of Public Health Medical School, University of PécsESSA GHAZWANI100% (1)
- QC Delta PV PPT Student 09Document8 paginiQC Delta PV PPT Student 09Susianna RismandaÎncă nu există evaluări
- Clinical Decision MakingDocument32 paginiClinical Decision MakingMUGISHA GratienÎncă nu există evaluări
- Screening TestDocument22 paginiScreening TestRabea DiaÎncă nu există evaluări
- Quality Control in Clinical Biochemistry BMLTDocument56 paginiQuality Control in Clinical Biochemistry BMLTSelim JaforÎncă nu există evaluări
- Probabilities in Clinical Medicine: Mohammad Saifur Rohman, Md. PHDDocument41 paginiProbabilities in Clinical Medicine: Mohammad Saifur Rohman, Md. PHDerlisaÎncă nu există evaluări
- Screening - DR Heba MahmoudDocument45 paginiScreening - DR Heba MahmoudMerna IbrahimÎncă nu există evaluări
- Lecture 2 Cpms16-ScreeningDocument40 paginiLecture 2 Cpms16-Screeningapi-263590842Încă nu există evaluări
- Practical Work CA On DX 2012Document26 paginiPractical Work CA On DX 2012Nurul Aulia AbdullahÎncă nu există evaluări
- Westgard1983 - Power CurvesDocument8 paginiWestgard1983 - Power CurvesAnderson CarvalhoÎncă nu există evaluări
- Decision Analysis: Matthew Scotch, PHD, MPHDocument29 paginiDecision Analysis: Matthew Scotch, PHD, MPHPedroMartinsÎncă nu există evaluări
- Quality ControlDocument65 paginiQuality ControlKirsten ValenzuelaÎncă nu există evaluări
- Epi Lec 5Document40 paginiEpi Lec 5Dr. Mahbub Alam MahfuzÎncă nu există evaluări
- Week 6-MCQ in EBP-1Document36 paginiWeek 6-MCQ in EBP-1Hasan KhawaldehÎncă nu există evaluări
- Week 6-MCQ in EBP-1Document36 paginiWeek 6-MCQ in EBP-1Geeta SureshÎncă nu există evaluări
- Conditional Probability and Medical TestsDocument20 paginiConditional Probability and Medical TestsRuslan MalovanyyÎncă nu există evaluări
- Diagnostic Studies PEBHC Workshop December 2015Document77 paginiDiagnostic Studies PEBHC Workshop December 2015Nursyamsi AhmadÎncă nu există evaluări
- 4 - Clinical EpidemiologyDocument8 pagini4 - Clinical EpidemiologyDiana Mitrea100% (1)
- Jarir Atthobari - Clinical TrialDocument38 paginiJarir Atthobari - Clinical TrialLilian KusumaÎncă nu există evaluări
- Introduction To Laboratory Medicine (Clinical Laboratory) : Dr. Dr. Tinny Rasjad SPPK (K)Document43 paginiIntroduction To Laboratory Medicine (Clinical Laboratory) : Dr. Dr. Tinny Rasjad SPPK (K)hendra2darmawanÎncă nu există evaluări
- Screening: To Sort Out Apparently Well Persons Who Probably Have A Disease From Those Who Probably Do Not."Document24 paginiScreening: To Sort Out Apparently Well Persons Who Probably Have A Disease From Those Who Probably Do Not."Munir AkhtarÎncă nu există evaluări
- 29 Sep 2023principles and Predictive Value of ScreeningDocument29 pagini29 Sep 2023principles and Predictive Value of Screening1.barron.whiteÎncă nu există evaluări
- Screening: Owais Raza - PHD Epidemiology - Tehran University of Medical SciencesDocument35 paginiScreening: Owais Raza - PHD Epidemiology - Tehran University of Medical Sciencespaperpin27100% (1)
- Summary of Diagnostic Test Accuracy For BR PDFDocument33 paginiSummary of Diagnostic Test Accuracy For BR PDFOlfat ashrafÎncă nu există evaluări
- Screening Test (Adv) : Rizwanul Karim NipsomDocument37 paginiScreening Test (Adv) : Rizwanul Karim NipsomRizwan ShameemÎncă nu există evaluări
- Evidence Based Medicine: Tugas MkduDocument6 paginiEvidence Based Medicine: Tugas MkduPutri Dwi KartiniÎncă nu există evaluări
- EBM TerapiDocument23 paginiEBM TerapiArum Ardisa RiniÎncă nu există evaluări
- Diagnostic and Prognostic Worksheet by DR Muhammad Febriandi Djunaidi Prodi Ilmu BedahDocument8 paginiDiagnostic and Prognostic Worksheet by DR Muhammad Febriandi Djunaidi Prodi Ilmu BedahMuhammad FebriandiÎncă nu există evaluări
- ENG - Epidemiology Biostatistics IMGDocument8 paginiENG - Epidemiology Biostatistics IMGManivanh AvalosÎncă nu există evaluări
- Quality Assurance in Hematology Group 11Document51 paginiQuality Assurance in Hematology Group 11Mandy A. DelfinÎncă nu există evaluări
- Quality Assurance in Hemat LabsDocument38 paginiQuality Assurance in Hemat LabsSmriti Dwivedi SharmaÎncă nu există evaluări
- MANI Quality Control in Hematology AnalysersDocument65 paginiMANI Quality Control in Hematology Analyserscandiddreams100% (1)
- Student Worksheet - CA DX - 221122Document5 paginiStudent Worksheet - CA DX - 221122MuhammadDzikriAuliaÎncă nu există evaluări
- Disease ScreeningDocument37 paginiDisease Screeningmwambungup100% (1)
- Lecture5 June15 05Document45 paginiLecture5 June15 05Wuri Kusuma AtmajaÎncă nu există evaluări
- Screening - Master - 2022Document57 paginiScreening - Master - 2022Kanwal KhanÎncă nu există evaluări
- Critical Appraisal of Articles About Diagnostic TestsDocument43 paginiCritical Appraisal of Articles About Diagnostic TestshardianÎncă nu există evaluări
- Screening TestsDocument35 paginiScreening Testsapi-3699330Încă nu există evaluări
- EBM, Design Study, Quantifying RiskDocument71 paginiEBM, Design Study, Quantifying Riskseptian kristyanaÎncă nu există evaluări
- Critical Appraisal Cross Sectional Case ControlDocument76 paginiCritical Appraisal Cross Sectional Case ControlAndita SyabanaÎncă nu există evaluări
- Update To The 2009 AMP Molecular Diagnostic Assay Validation White PaperDocument11 paginiUpdate To The 2009 AMP Molecular Diagnostic Assay Validation White PaperHuỳnh ChâuÎncă nu există evaluări
- Study Desien - by Tahani AlghamdiDocument41 paginiStudy Desien - by Tahani AlghamdiMian. Shoaib.Încă nu există evaluări
- Bio Statistics Hand OutDocument11 paginiBio Statistics Hand OutaymÎncă nu există evaluări
- Chapter 8Document26 paginiChapter 8Nathnael GebÎncă nu există evaluări
- Quality Control: Lucila B. Rabuco, PHDDocument47 paginiQuality Control: Lucila B. Rabuco, PHDChito PermejoÎncă nu există evaluări
- Journalclubjan 2015Document25 paginiJournalclubjan 2015api-277377339Încă nu există evaluări
- L 5 - Reference RangeDocument32 paginiL 5 - Reference RangehayatkuwaityÎncă nu există evaluări
- Interpretation of Diagnostic Screening TestsDocument33 paginiInterpretation of Diagnostic Screening TestsAMELIA CAROLINA HERRERA BRICEÑOÎncă nu există evaluări
- Nuclear Medicine Clinical Procedures for TechnologistsDe la EverandNuclear Medicine Clinical Procedures for TechnologistsÎncă nu există evaluări
- Elements Of Clinical Study Design, Biostatistics & ResearchDe la EverandElements Of Clinical Study Design, Biostatistics & ResearchÎncă nu există evaluări
- Iggy Med Surg Test Bank Chapter 007Document10 paginiIggy Med Surg Test Bank Chapter 007Tracy Bartell100% (5)
- Endometrial HyperplasiaDocument11 paginiEndometrial HyperplasiarinieeeÎncă nu există evaluări
- Gastroesophageal Reflux DiseaseDocument9 paginiGastroesophageal Reflux DiseaseNicole Tupayachi ArceÎncă nu există evaluări
- Dha 022019 PDFDocument20 paginiDha 022019 PDFDrNishchitha K100% (2)
- What Is ThalassemiaDocument2 paginiWhat Is ThalassemiaFatima Azzahra Khairul AnuarÎncă nu există evaluări
- NCP For Laryngeal CancerDocument5 paginiNCP For Laryngeal CancerMădălina PinciucÎncă nu există evaluări
- Department of Oral Periodontology: Topic: Free Gingival GraftDocument1 paginăDepartment of Oral Periodontology: Topic: Free Gingival GraftTenzin WangyalÎncă nu există evaluări
- Medical ReportDocument5 paginiMedical ReportRuthdel KazumiÎncă nu există evaluări
- A Case Presentation On:: Bipolar 1 Disorder, MRE With Psychotic FEARURESDocument57 paginiA Case Presentation On:: Bipolar 1 Disorder, MRE With Psychotic FEARURESLane Mae Magpatoc NoerrotÎncă nu există evaluări
- Medication, Toxic, and Vitamin-Related NeuropathiesDocument22 paginiMedication, Toxic, and Vitamin-Related Neuropathiessatyagraha84Încă nu există evaluări
- Total Patient Care Nursing or Case Method NursingDocument3 paginiTotal Patient Care Nursing or Case Method Nursingkint manlangitÎncă nu există evaluări
- For Website All Questions PDFDocument26 paginiFor Website All Questions PDFAyyaz HussainÎncă nu există evaluări
- OpicaponeDocument4 paginiOpicaponeAnonymous a6UCbaJÎncă nu există evaluări
- Director Emergency Medical Services in Nashville TN Resume Steve FustonDocument2 paginiDirector Emergency Medical Services in Nashville TN Resume Steve FustonSteveFustonÎncă nu există evaluări
- 129 Accommodative EsotropiaDocument6 pagini129 Accommodative EsotropiakarenafiafiÎncă nu există evaluări
- Annotated BibliographyDocument2 paginiAnnotated Bibliographyapi-237172063Încă nu există evaluări
- In-Patient Claim Form - ConventionalDocument2 paginiIn-Patient Claim Form - ConventionalAbdul Qayyum Sipra Madduki50% (2)
- ENT 2014 SovedDocument7 paginiENT 2014 SovedHasnat HussainÎncă nu există evaluări
- Baromtric (89 Pages)Document89 paginiBaromtric (89 Pages)jahangirealamÎncă nu există evaluări
- Improving Patient and Worker SafetyDocument171 paginiImproving Patient and Worker SafetylaggantigganÎncă nu există evaluări
- Bronchial Asthma SeminarDocument64 paginiBronchial Asthma SeminarShidevÎncă nu există evaluări
- As Far As Possible - en ISO 14971Document19 paginiAs Far As Possible - en ISO 14971Kanwal Jit Singh100% (1)
- Analyzing A Leader EssayDocument6 paginiAnalyzing A Leader Essayapi-253792021Încă nu există evaluări
- Granny Storm Crow's List Jan 2014 ConditionsDocument750 paginiGranny Storm Crow's List Jan 2014 ConditionsElectroPig Von FökkenGrüüvenÎncă nu există evaluări
- FullDocument59 paginiFullJyotiÎncă nu există evaluări
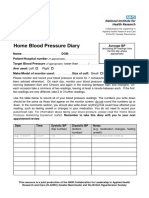
- Home Blood Pressure DiaryDocument2 paginiHome Blood Pressure DiaryCherieÎncă nu există evaluări
- USG Efusi Pleura PDFDocument7 paginiUSG Efusi Pleura PDFEnvhy AmaliaÎncă nu există evaluări
- SMA Advanced Sports Taping Presentation DSR Handouts PDFDocument4 paginiSMA Advanced Sports Taping Presentation DSR Handouts PDFHamada Said AliÎncă nu există evaluări
- Hospital Design GuidelinesDocument33 paginiHospital Design GuidelinesRohit Gupta100% (3)
- Thesis PoDocument5 paginiThesis PoJane SandovalÎncă nu există evaluări