Documente Academic
Documente Profesional
Documente Cultură
A. Collecting Data:: Foundations of Nursing
Încărcat de
shenric16Descriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
A. Collecting Data:: Foundations of Nursing
Încărcat de
shenric16Drepturi de autor:
Formate disponibile
Foundations of Nursing Nursing Process Prepared by: Mark Fredderick R. Abejo R.N, M.A.
A. Collecting Data: Data collection is the process of gathering information about a clients health status. It must be both systematic and continuous to prevent the omission of significant data and reflect a clients changing health status. FOUNDATIONS OF NURSING Nursing Process Lecturer: Mark Fredderick R. Abejo R.N, M.A.N NURSING PROCESS A systematic, rational method of planning providing nursing care. Goal: 1. 2. 3. To identify a clients healthcare status, and actual or potential health problems To establish plans to meet the identified needs To deliver specific nursing interventions to address those needs Subjective Data also referred to as symptoms or covert data are apparent only to the person affected and can be described or verified only by that person. Itching, pain, and feelings of worry are examples of subjective data. It all includes the clients sensations, feelings, values, beliefs, attitudes, and perception of personal health status and life situation
I. ASSESSMENT PHASE
Objective Data also referred to as signs or overt data, are detectable by an observer or can be measured or tested against an accepted standard. They can be seen, heard, felt, or smelled, and they are obtained by observation or physical examination. Primary source is the client Secondary source is family or anyone else that is not the client Methods of Data Collection Observing To observe is to gather data by using the sense. Observation is a conscious, deliberate skill that is developed through effort and with an organized approach. It has to aspects: (a) noticing the data and (b) selecting, organizing, and interpreting the data. Interviewing An interview is a planned communication or a conversation with purpose, for example, to get or give information, identify problems of mutual concern, evaluate change, teach, provide support, or provide counseling or therapy. There are two approaches to interviewing: o Directive interview - Nurse directs interview, client responds to questions and has limited chances to discuss concerns. o Nondirective interview rapport-building where the client is in control of the purpose, subject, and pace. Questions : Open-ended invites client to discover and explore, elaborate, clarify, or illustrate their thoughts or feelings. How have you been feeling lately? Closed-ended used in directive interviewing, and are questions that require a yes or no answer.
The nurse carry out a complete & holistic nursing assessment of every patient's needs Utilizes an assessment framework, based on a nursing model or Waterlow scoring wherein problems are expressed as either actual or potential. Assessing is a systematic and continuous collection, organization, validation, and documentation of data (information) Assessing is a continuous process carried out during all phases of the nursing process Nursing assessments focus on a clients responses to a health problem Should include the clients perceived needs, health problems, related experience, health practices, values, and lifestyles
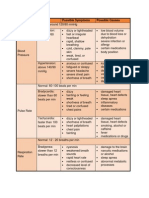
Types of Assessment Initial Assessment Problem-focused Assessment Emergency Assessment Time-lapsed Reassessment The assessment process involves four closely related activities: collecting data, organizing data, validating data, and documenting data.
Foundations of Nursing
Abejo
Foundations of Nursing Nursing Process Prepared by: Mark Fredderick R. Abejo R.N, M.A.N
Neutral question a question that the client can answer without direction. Why do you think you had the operation? Leading question directs the clients answer. Youre stressed about surgery tomorrow, arent you?
Examining The physical examination or physical assessment is a systematic data-collection method that uses observation (i.e., the senses of sight, hearing, smell, and touch) to detect health problems. To conduct the examination the nurses uses techniques of inspection, auscultation, palpation, and percussion.
D. Documenting Data: To complete the assessment phase, the nurse records client data. Accurate documentation is essential and should include all data collected about the clients health status. Data are recorded in a factual manner and not interpreted by the nurse o The nurse records the clients breakfast intake (objective) as coffee 240 mL, 1 egg, and 1 slice of toast II. DIAGNOSIS PHASE
B. Organizing Data: Using a written or computerized format that organizes the assessment data. Most schools of nursing and health cause agencies have developed their own structured assessment format. Frameworks: o Gordon 11 functional health patterns o Orem 8 universal self-care requisites of humans o Roys adaptation model o Maslows hierarchy of needs C. Validating Data: The information gathered during the assessment phase must be complete, factual, and accurate because the nursing diagnoses and interventions are based on this information. Validation is the act of double-checking or verifying data to confirm that it is accurate and factual. Cues vs. Inferences: o Cues subjective or objective data that can be directly observed by the nurse, either what the client says or what the nurse can see. o Inferences nurses interpretations or conclusions based on the cues. (A nurse observes the cues that an incision is red, hot, and swollen; the nurse makes the inference that the incision is infected.) You dont have to check all data (like birth dates, height, weight and most lab studies) Validating data helps the nurse complete these tasks: Ensure that assessment information is complete. Ensure that objective and related subjective data agree. Obtain additional information that may have been overlooked. Differentiate between cues and inferences. Avoid jumping to conclusions and focusing in the wrong direction to identify problems. The term diagnosing refers to the reasoning process, whereas the term diagnosis is a statement or conclusion regarding the nature of a phenomenon. The standardized North American Nursing Diagnosis Association (NANDA) names for the diagnoses are called diagnostic labels; and the clients problem statement, consisting of the diagnostic label plus etiology (causal relationship between a problem and its related Types of Nursing Diagnoses The five types of nursing diagnoses are actual, risk, wellness, possible, and syndrome. An actual diagnosis is a client problem that is present at the time of the nursing assessment. Examples are Ineffective Breathing Pattern and Anxiety. An actual nursing diagnosis is based on the presence of associated signs and symptoms. A risk nursing diagnosis is a clinical judgment that a problem does not exist, but the presence of risk factors indicates that a problem is likely to develop unless nurses intervene. A wellness diagnosis describes human responses to levels of wellness in an individual, family or community that have a readiness for enhancement A possible nursing diagnosis is one in which evidence about a health problem is incomplete or unclear. A possible diagnosis requires more data either to support or to refute it. Syndrome diagnosis is a diagnosis that is associated with a cluster of other diagnoses.
Foundations of Nursing
Abejo
Foundations of Nursing Nursing Process Prepared by: Mark Fredderick R. Abejo R.N, M.A.N
The Diagnostic Process The diagnostic process uses the critical-thinking skills of analysis and synthesis. Critical thinking is a cognitive process during which a person reviews data and considers explanations before forming an opinion. Analysis is the separation into components, that is, the breaking down of the whole into its parts . Synthesis is the opposite, that is, the putting together of parts into the whole. T he diagnostic has three steps: analyzing data, identifying health problems, risks, and strengths, and formulating diagnostic statements. A. Analyzing Data In the diagnostic process, analyzing involves the following steps: o Compare data against standards (identify significant cues). o Cluster cues (generate tentative hypotheses). Identify gaps and inconsistencies. B. Identifying Health Problems, Risks, and Strengths. After data are analyzed, the nurse and client can together identify strengths and problems. This is primarily a decision-making process. Determining problems and risk After grouping and clustering the data, the nurse and client together identify problems that support tentative actual, risk, and possible diagnoses. In addition, the nurse must determine whether the clients problem is a nursing diagnosis, medical diagnosis, or collaborative problem. Determining strengths At this stage, the nurse and client also establish the clients strengths, resources, and abilities to cope. Most people have a clearer perception of their problems or weakness than of their strengths and assets, which they often take for granted. A clients strengths can be found in the nursing assessment record (health, home life, education, recreation, exercise, work, family and friends, religious beliefs, and sense of humor). C. Formulating Diagnostic Statements Most nursing diagnoses are written as two-part or three-part statements, but there are variations of these. Basic two-part statements The basic two-part statement includes the following: Problem (P): statement of the clients response. Etiology (E): factors contributing to or probable cause of the responses.
Basic three-part statements The basic three-part nursing diagnosis statement is called the PES format and includes the following: Problem (P): statement of the clients response. Etiology (E): factors contributing to or probable cause of the responses. Signs and Symptoms (S): defining characteristics manifested by the client.
Problem Statement describes the clients health problem or response for which nursing therapy is given Qualifiers added words to give additional meaning to the diagnostic statement Altered change from baseline Impaired made worse, weakened, damaged Decreased smaller in size, amount or degree Ineffective not producing the desired effect Acute severe or of short duration. Chronic lasting a long time Diagnostic Labels o Describes the clients health problem or response for which nursing therapy is given. o Independent function areas of health care that are unique to nursing and separate and distinct from medical management. o Dependent function- Nurses are obligated to carry out physician-prescribed therapies and treatments.
Foundations of Nursing
Abejo
Foundations of Nursing Nursing Process Prepared by: Mark Fredderick R. Abejo R.N, M.A.N
Differentiating Nursing Diagnoses from Collaborative Problems o Collaborative monitoring the clients condition and preventing development of the potential complication and using physician-prescribed interventions. o Nursing Diagnoses involve the human response, which vary from one person to the next. COMMON ERRORS IN FORMULATING NURSING DIAGNOSES 1. Using medical diagnosis INCORRECT: Self-care deficit related to stroke CORRECT: Self-care deficit related to neuromuscular impairment 2. Relating the problem to an unchangeable situation 3. Confusing the etiology or signs/symptoms for the problem INCORRECT: Post-operative lung congestion related to bed rest CORRECT: Ineffective airway clearance related to general weakness and immobility 4. Use of a procedure instead of a human response INCORRECT: Catheterization related to urinary retention CORRECT: Urinary retention related to perineal swelling 5. Lack of specificity INCORRECT: Constipation related to nutritional intake CORRECT: Constipation related to inadequate dietary bulk and fluid intake 6. Combining two nursing diagnosis INCORRECT: Anxiety and fear related to separation from parents CORRECT: Anxiety related to change in environment and unmet needs 7. Relating one nursing diagnosis to another INCORRECT: Coping, individual ineffective related to anxiety CORRECT: Anxiety, severe related to change in role functioning and socio-economic status 8. Use of judgmental/value-laden language Ineffective airway clearance related to bad habit 9. Making assumptions INCORRECT: Risk for altered parenting related to inexperience CORRECT: Deficient knowledge regarding child care issues related to lack of previous experience, unfamiliarity with resources 10. Writing a Legally Inadvisable Statement INCORRECT: Skin integrity related to not being turned every 2 hours CORRECT: Impaired skin integrity related to pressure and altered circulation
A Nursing Diagnosis Is A statement of a patient problem Actual or potential Within the scope of nursing practice Directive of nursing intervention
Is not
A medical diagnosis A nursing action A physician order A therapeutic treatment
III. PLANNING PHASE
The third phase of the nursing process, in which the nurse and client develop client goals/desired outcomes and nursing interventions to prevent, reduce, or alleviate the clients health problems. Planning is a deliberative, systematic phase of the nursing process that involves decision making and problem solving. In planning, the nurse refers to the clients assessment data and diagnostic statements for direction in formulating clients goals and designing the nursing interventions required to prevent, reduce, or eliminate the clients health problems. A nursing intervention is any treatment, based upon clinical judgment and knowledge that a nurse performs to enhance patient/client outcomes
Types of Planning Planning begins with the first client contact and continues until the nurse-client relationship ends, usually when the client is discharges from the health care agency. Initial Planning The nurse perform the admission assessment usually develops the initial comprehensive plan of care. This nurse has the benefit of the clients body language as well as some intuitive kinds of information that are not available solely from the written database. Planning should be initiated as soon as possible after the initial assessment, especially because of the trend toward shorter hospital stays.
Foundations of Nursing
Abejo
Foundations of Nursing Nursing Process Prepared by: Mark Fredderick R. Abejo R.N, M.A.N
Ongoing Planning Is done by all nurses who work with the client. As nurses obtain new information evaluate the clients responses to care, they can individualize the initial care plan further. Ongoing planning also occurs at the beginning of a shift as the nurse plans the care to be given that day. Discharge Planning The process of anticipating and planning for needs after discharge, is a crucial part of comprehensive health care and should be addressed in each clients care plan. NURSING CARE PLAN Types of NCP Informal Nursing Care Plan o Strategy for action that exists in the nurses mind. Formal Nursing Care Plan o Written or computerized guide for organizing information Standardized Nursing Care Plan o Formal plan that specifies the nursing care for groups of clients with common needs. o Not for individuals o Preprinted guides for the nursing care of a client who has a need that arises frequently in the agency. o Problem -> Goals/desired outcomes -> Nursing interventions -> Evaluation Individualized Nursing Care Plan o Is tailored to meet the unique needs of a specific client. - When nurses use the clients nursing diagnoses to develop goals and nursing interventions, the result is a holistic, individualized plan of case that will meet the clients unique needs. - During planning phase, the nurse must decide which of the clients problems need individualized plans and which problems can be addressed by standardized plans and routine care, and write unique desired outcomes and nursing interventions for client problems that require nursing attention beyond preplanned, routine care. Guidelines for writing a Nursing Care Plan Date and sign the plan Use category headings Nursing Diagnoses Goals/Desired Outcomes Use standardized medical or English symbols and key words rather that complete sentences to communicate your ideas. Be specific Refer to procedure books or other sources of info rather than including all steps on something
Foundations of Nursing
Tailor plan to the client: Ask when the best time is for the client to do interventions Ensure that the plan incorporates preventive and health maintenance aspects as well as restorative ones. Ensure that the plan contains interventions for ongoing assessment of the client. Include collaborative and coordination activities in the plan Include plans for the clients discharge and home care need
The Planning Process In the process of developing client care, the nurse engages in the following activities: Priority Setting Is the process of establishing a preferential sequence for addressing nursing diagnoses and interventions. The nurse and client begin planning by deciding which nursing diagnosis requires attention first, which second, and so on. Instead of rankordering diagnoses, nurses can group them as having high, medium, or low priority. Life-threatening problems such as loss of respiratory or cardiac function are designated as high priority. The nurse must consider a variety of factors when assigning priorities, including the following: Clients health values and beliefs Clients priorities Resources available to the nurse and client Urgency of the health problem Medical treatment plan Establishing Client Goals/Desired Outcomes After establishing priorities, the nurse and client set goals for each nursing diagnosis. On a care plan the goals/desired outcome describe, in terms of observable client responses, what the nurse hopes to achieve by implementing the nursing interventions. The term goal and desired outcome are used interchangeably in this text, except when discussing and using standardized language. Selecting Nursing Interventions and Activities Nursing interventions and activities are the actions that a nurse performs to achieve client goals. The specific interventions chosen should focus on eliminating or reducing the etiology of the nursing diagnosis, which is the second clause of the diagnostic statement. Types of Nursing Interventions Independent interventions Are those activities that nurses are licensed to initiate on the basis of their knowledge and skills. They include physical care, ongoing assessment, emotional support and comfort, teaching, counseling, environmental management, and making referrals to other health care professionals.
Abejo
Foundations of Nursing Nursing Process Prepared by: Mark Fredderick R. Abejo R.N, M.A.N
Dependent interventions Are activities carried out under the physicians orders or supervision, or according to specified routines. Collaborative interventions Are actions the nurse carries out in collaboration with other health team members, such as physical therapist, social workers, dietitians, and physicians. Criteria for Choosing Nursing Interventions The following criteria can help the nurse to choose the best nursing interventions. The plan must be: Safe and appropriate for the individuals age, health, and condition. Achievable with the resources available. Congruent with the clients values, beliefs, and culture. Congruent with other therapies. Based on nursing knowledge and experience or knowledge from relevant sciences. Within established standards of care as determined by state laws, professional associations, and the policies of the institution. Writing Nursing Order After choosing the appropriate nursing interventions, the nurse writes them on the care plan as nursing orders. Nursing orders are instructions for the specific individualized activities the nurse performs to help the client meet established health care goals. The term order connotes a sense of accountability for the nurse who gives the order and for the nurse who carries it out. IV. IMPLEMENTATION / INTERVENTION PHASE
interventions that were developed in the planning step and then concludes the implementing step by recording nursing activities and the resulting client responses. Implementing Skills To implement the care plan successfully, nurses need cognitive, interpersonal, and technical skills. These skills are distinct from one another; in practice, however, nurses use them in various combinations and with different emphasis, depending on the activity. Having these skills contributes to the greater improvement of the nurse's delivery of health care to the patient, including the patient's level of health, or health status. Cognitive or Intellectual Skills Such as analyzing the problem, problem solving, critical thinking and making judgments regarding the patient's needs. Included in these skills are the ability to identify, differentiate actual and potential health problems through observation and decision making by synthesizing nursing knowledge previously acquired. Interpersonal Skills Which includes therapeutic communication, active listening, conveying knowledge and information, developing trust or rapport-building with the patient, and ethically obtaining needed and relevant information from the patient which is then to be utilized in health problem formulation and analysis. Technical Skills Which includes knowledge and skills needed to properly and safely manipulate and handle appropriate equipment needed by the patient in performing medical or diagnostic procedures, such as vital signs, and medication administrations. Process of Implementing The process of implementing normally includes: Reassessing the Client Just before implementing an intervention, the nurse must reassess the client to make sure the intervention is still needed. Even though an order is written on the care plan, the clients condition may have changed. Determining the Nurses Need for Assistance When implementing some nursing interventions, the nurse may require assistance for one of the following reasons: The nurse is unable to implement the nursing activity safely alone (e.g., ambulating an unsteady obese client). Assistance would reduce stress on the client (e.g., turning a person who experiences acute pain when moved). The nurse lacks the knowledge skills to implement a particular nursing activity (e.g., a nurse who is not familiar with a particular model of traction equipment needs assistance the first time it is applied).
Abejo
The methods by which the goal will be achieved are also recorded at this stage. The methods of implementation must be recorded in an explicit and tangible format in a way that the patient can understand should he wish to read it. Clarity is essential as it will aid communication between those tasked with carrying out patient care. Implementing consists of doing and documenting the activities that are specific nursing actions needed to carry out the
Foundations of Nursing
Foundations of Nursing Nursing Process Prepared by: Mark Fredderick R. Abejo R.N, M.A.N
Implementing the Nursing Interventions It is important to explain to the client what interventions will be done, what sensations to expect, what the client is expected to do, and what the expected outcome is. For many nursing activities it is important to ensure the clients privacy, for example by closing doors, pulling curtains, or draping the client. When implementing interventions, nurses should follow these guidelines: Base nursing interventions on scientific knowledge, nursing research, and professional standards of care whenever possible. Clearly understand the orders to be implemented and question any that are not understood. Adapt activities to the individual client. Implement safe care. Provide teaching, support, and comfort. Be holistic. Respect dignity of the client and enhance the clients self-esteem. Encourage clients to participate actively in implementing the nursing interventions. Supervising Delegated Care If care has been delegated to other health care personnel, the nurse responsible for the clients overall care must ensure that the activities have been implemented according to the care plan. Other caregivers may be required to communicate their activities to the nurse by documenting them on the client record, reporting verbally, or filling out a written form. The nurse validates and responds to any adverse findings or client responses. Documenting Nursing Activities After carrying out the nursing activities, the nurse completes the implementing phase by recording the interventions and client responses in the nursing progress notes. These are a part of the agencys permanent record for the client. Nursing care must not be recorded in advance because the nurse may determine on reassessment of the client that the intervention should not or cannot be implemented. V. EVALUATION PHASE
To evaluate is to judge or to appraise. Evaluating is a planned, ongoing, purposely activity in which clients and health care professionals determine (a) the clients progress toward achievement of goals/outcomes (b) the effectiveness of the nursing care plan. The purpose of this stage is to evaluate progress toward the goals identified in the previous stages. If progress towards the goal is slow, or if regression has occurred, the nurse must change the plan of care accordingly
Process of Evaluating Client Responses Before evaluation, the nurse identifies the desired outcomes (indicators) that will be used to measure client goal achievement Desired outcomes serve two purposes: they establish the kind of evaluative data that needed to be collected and provide a standard against which the data are judged. The evaluation process has five components:
Collecting Data Using the clearly stated, precise, and measurable desired outcomes as a guide, the nurse collects data so that conclusions can be drawn about whether the goals have been met. It is usually necessary to collect both objective and subjective data. Comparing Data with Outcomes If the first two parts of the evaluation process have been carried out effectively, it is relatively simple to determine whether a desired outcome has been met. Both the nurse and the client play an active role in comparing clients actual responses with the desired outcomes. After determining whether a goal has been met, the nurse writes an evaluative statement (either on the care plan or in the nurses notes). An evaluation statement consists of two parts: a conclusion (is a statement that the goal/desired outcomes was met, partially met, or not met), and supporting data (are the list of client responses that support the conclusion). Relating Nursing Activities to Outcomes The third aspect of the evaluating process is determining whether the nursing activities had any relation to the outcomes. It should never be assumed that a nursing activity was the cause of or the only factor in meeting, partially meeting, or not meeting a goal. Drawing Conclusions about Problem Status The nurse uses the judgments about goal achievement to determine whether the care plan was effective in resolving, reducing, or preventing client problems. When goals have been met, the nurse can draw one of the following conclusions about the status of the clients problem: The actual problem stated in the nursing diagnosis has been resolved; or potential problem is being prevented and the risk factors no longer exist.
Foundations of Nursing
Abejo
Foundations of Nursing Nursing Process Prepared by: Mark Fredderick R. Abejo R.N, M.A.N
In these instances, the nurse documents that the goals have been met and discontinues the care for the problem. The potential problem stated in the nursing diagnosis is being prevented, but the risk factors are still present. In this case, the nurse keeps the problem on the care plan. The actual problem still exists even though some goals are being met. The nursing interventions must be continued.
Quality Improvement Quality improvement (QI) is also known as continuous quality improvement (CQI), total quality management (TQM), performance improvement (PI), or persistent quality improvement (PQI) Nursing Audit An audit means the examination or review of records. A retrospective audit is the evaluation of a clients record after discharge from an agency. Retrospective means relating to past events. These evaluations use interviewing, direct observation of nursing care, and review of clinical records to determine whether specific evaluative criteria have been met.
Continuing, Modifying, and Terminating the Nursing Care Plan After drawing conclusions about the status of the clients problems, the nurse modifies the care plan as indicated. Depending on the agency, modifications may be made by drawing a line through proportions of the care plan, or marking portions using a highlighting pen, or writing Discontinued (dcd) and the date. Whether or not goals were met, a number of decisions need to be made about continuing, modifying, or terminating nursing care for each problem. Before making individual modifications, the nurse must first determine why the plan as a whole was not completely effective. This requires a review of the entire care plan and a critique of the nursing process steps involved in its development for a checklist to use when reviewing a care plan. Evaluating the Quality of Nursing Care In addition to evaluating goal achievement for individual clients, nurses are also involved in evaluating and modifying the overall quality of care given to groups of clients. This is an essential part of professional accountability. Quality Assurance A quality-assurance (QA) program is an ongoing, systematic process designed to evaluate and promote excellence in the health care provided to clients. Quality assurance frequently refers to evaluation of the level of care provided in a health care agency, but it may be limited to the evaluation of the performance of one nurse or more broadly involve the evaluation of the quality of the care in an agency, or even in a country. It consists of three components of care: The structure evaluation (focuses on the setting in which care is given. It answers this question: what effect does the setting have on the quality of care?), The process evaluation (focuses on how the care was given. It answers question such as these: Is the care relevant to the clients needs? Is the care appropriate, complete and timely?), Outcome evaluation (focuses on demonstrable changes in the clients health status as a result of nursing care. Outcome criteria are written in terms of client responses or health status.
Foundations of Nursing
Abejo
S-ar putea să vă placă și
- Care of The Newborn PDFDocument5 paginiCare of The Newborn PDFzhai bambalan100% (2)
- Fertilization To Conception: Maternal and Child Health Nursing PregnancyDocument8 paginiFertilization To Conception: Maternal and Child Health Nursing PregnancyNikki M. Arapol100% (1)
- Nursing ProcessDocument43 paginiNursing ProcessFitz Jaminit100% (1)
- Florence Nightingale'S Environmental TheoryDocument16 paginiFlorence Nightingale'S Environmental TheoryZAY EMÎncă nu există evaluări
- Funda Lab - Prelim ReviewerDocument16 paginiFunda Lab - Prelim ReviewerNikoruÎncă nu există evaluări
- N1R01A - Transes in Introduction To NursingDocument8 paginiN1R01A - Transes in Introduction To NursingMikhaella GwenckyÎncă nu există evaluări
- Banagen, Philip B. BSN1 - S6: Abraham MaslowDocument5 paginiBanagen, Philip B. BSN1 - S6: Abraham MaslowLegendXÎncă nu există evaluări
- Health Assessment LectureDocument115 paginiHealth Assessment Lectureteuuuu100% (1)
- History of NursingDocument4 paginiHistory of NursingMichelleneChenTadle100% (1)
- Heat and Cold ApplicationDocument21 paginiHeat and Cold Applicationbemina jaÎncă nu există evaluări
- Nursing Process: CYCLIC-regularly Repeated Events DYNAMIC - Continuously ChangingDocument16 paginiNursing Process: CYCLIC-regularly Repeated Events DYNAMIC - Continuously ChangingHeide Basing-aÎncă nu există evaluări
- Finals TFN ReviewerDocument5 paginiFinals TFN ReviewerNicole Faith L. NacarioÎncă nu există evaluări
- Iv FluidsDocument11 paginiIv FluidsDianna Rose BelenÎncă nu există evaluări
- Dorothea Elizabeth Orem: Self-Care TheoryDocument3 paginiDorothea Elizabeth Orem: Self-Care TheoryE.R.OÎncă nu există evaluări
- New PRC Exhibit FormDocument6 paginiNew PRC Exhibit FormPixel DinibitÎncă nu există evaluări
- Vital SignsDocument85 paginiVital SignsSara SabraÎncă nu există evaluări
- Male Reproductive System and DiseasesDocument10 paginiMale Reproductive System and DiseasesMadan Kumar100% (2)
- Fundamentals of Nursing Transes 3Document4 paginiFundamentals of Nursing Transes 3Louise TorresÎncă nu există evaluări
- NCM 112 - Rle Skills Lab Performance Checklist Obtaining An ElectrocardiogramDocument3 paginiNCM 112 - Rle Skills Lab Performance Checklist Obtaining An ElectrocardiogramDominicManlutacÎncă nu există evaluări
- ISUI-NUR-Syl-Effectivity: September 7, 2020 Revision: 2Document6 paginiISUI-NUR-Syl-Effectivity: September 7, 2020 Revision: 2cara100% (1)
- Basic Concepts in Nursing (TFN & Fundamentals) - Heart of Nursing PHDocument17 paginiBasic Concepts in Nursing (TFN & Fundamentals) - Heart of Nursing PHDalene Evangelio100% (1)
- Assessment of Skin, Hair and Nails FinaleDocument7 paginiAssessment of Skin, Hair and Nails FinaleCristine SyÎncă nu există evaluări
- TFN MidtermDocument16 paginiTFN MidtermEhm Margreth CabiscuelasÎncă nu există evaluări
- Fundamentals of Nursing Practice Lecture Session 1: Concept of NursingDocument4 paginiFundamentals of Nursing Practice Lecture Session 1: Concept of NursingViea Pacaco SivaÎncă nu există evaluări
- 220 Nursing Bullets Fundamentals of Nursing Reviewer 1 - NurseslabsDocument35 pagini220 Nursing Bullets Fundamentals of Nursing Reviewer 1 - NurseslabsjackyÎncă nu există evaluări
- Fundamentals of NursingDocument5 paginiFundamentals of NursingKaren Mae Santiago AlcantaraÎncă nu există evaluări
- Nursing Student Manual: Iloilo Doctors' College College of Nursing West Avenue, Molo, Iloilo CityDocument94 paginiNursing Student Manual: Iloilo Doctors' College College of Nursing West Avenue, Molo, Iloilo Citysha uyÎncă nu există evaluări
- Physical Assessment by KozierDocument58 paginiPhysical Assessment by KozierDennis Nabor Muñoz, RN,RM100% (8)
- M1: CDU-CN BSN Program Outcomes of The BSN CurriculumDocument8 paginiM1: CDU-CN BSN Program Outcomes of The BSN CurriculumMeteor 858Încă nu există evaluări
- Fundamentals-Of-Nursing-Module-PrelimDocument18 paginiFundamentals-Of-Nursing-Module-PrelimLalajim100% (1)
- Communicable Disease Nursing Study BulletsDocument12 paginiCommunicable Disease Nursing Study Bulletsoh_chamieÎncă nu există evaluări
- MCN Book ProjectDocument74 paginiMCN Book ProjectRonnie De Vera IIÎncă nu există evaluări
- Slu Bedbath NursingDocument13 paginiSlu Bedbath NursingGabeÎncă nu există evaluări
- The Nursing Health History (NHH) : NCM 101-A: Health AssessmentDocument7 paginiThe Nursing Health History (NHH) : NCM 101-A: Health Assessmentthe someoneÎncă nu există evaluări
- Sample NCLEX Questions With RationaleDocument26 paginiSample NCLEX Questions With RationaleSalanio JinalineÎncă nu există evaluări
- NCM 103 WK3 Communication Quiz ReviewerDocument5 paginiNCM 103 WK3 Communication Quiz ReviewerCarolyn Moquerio-serniculaÎncă nu există evaluări
- Health Assessment Reviewer (Prelims)Document9 paginiHealth Assessment Reviewer (Prelims)Frances Nicole Flores100% (1)
- NCM 104 - RleDocument25 paginiNCM 104 - RleAbigael Patricia GutierrezÎncă nu există evaluări
- 2 Nursing Foundation II Including Health Assessment Module-Converted - 020222Document17 pagini2 Nursing Foundation II Including Health Assessment Module-Converted - 020222Akshata BansodeÎncă nu există evaluări
- Funda NotesDocument55 paginiFunda NotesKristine CastilloÎncă nu există evaluări
- Vital SignsDocument94 paginiVital Signsglennm68100% (5)
- Assessment of Immune FunctionDocument3 paginiAssessment of Immune Functionhalloween candyÎncă nu există evaluări
- Host Response To InfectionDocument36 paginiHost Response To InfectionFrancia Toledano100% (1)
- Administering Oral Medication ScriptDocument4 paginiAdministering Oral Medication ScriptJoanna MontebonÎncă nu există evaluări
- En Notes EscDocument7 paginiEn Notes EscCG Patron BamboÎncă nu există evaluări
- Medicationpart1 110202192115 Phpapp02Document10 paginiMedicationpart1 110202192115 Phpapp02Jessamine Rochelle Reyes Esberto100% (1)
- Physical AssessmentDocument55 paginiPhysical AssessmentDidik Atmojo100% (1)
- Fundamentals of Nursing HistoryDocument6 paginiFundamentals of Nursing HistoryFrancis ObmergaÎncă nu există evaluări
- PDF NCM 103 Lecture NotesDocument5 paginiPDF NCM 103 Lecture Notesyoshi kento100% (2)
- 1 Institutional Nursing - Field in NursingDocument18 pagini1 Institutional Nursing - Field in NursingsannsannÎncă nu există evaluări
- Nurses NotesDocument4 paginiNurses NotesMay Ann Ann ButaranÎncă nu există evaluări
- Health Assessment NotesDocument40 paginiHealth Assessment NotesShane Tamil100% (7)
- NCM 112 Lecture Notes (Respiratory System and Its Diseases)Document9 paginiNCM 112 Lecture Notes (Respiratory System and Its Diseases)Kyle FernandezÎncă nu există evaluări
- Healthcare Delivery System and Administration - QUIZ 1Document4 paginiHealthcare Delivery System and Administration - QUIZ 1Creature of LightÎncă nu există evaluări
- Asepsis and Infection ControlDocument120 paginiAsepsis and Infection Controlnagarjungali100% (1)
- Critical Thinking and Nursing ProcessDocument49 paginiCritical Thinking and Nursing ProcessjeorjÎncă nu există evaluări
- The Nursing ProcessDocument17 paginiThe Nursing ProcessElla Lobenaria100% (1)
- Week 1Document73 paginiWeek 1Kimberly Jane TogñoÎncă nu există evaluări
- Nursing Process-Part 1Document31 paginiNursing Process-Part 1abigael cheptanuiÎncă nu există evaluări
- Evidence Based Nursing PracticeDocument21 paginiEvidence Based Nursing Practiceshenric16Încă nu există evaluări
- Maternity Nursing ReviewDocument37 paginiMaternity Nursing Reviewshenric16Încă nu există evaluări
- Uhc Irr DraftDocument107 paginiUhc Irr Draftshenric16Încă nu există evaluări
- Evidence Based Nursing PracticeDocument21 paginiEvidence Based Nursing Practiceshenric16Încă nu există evaluări
- Fhsis Annual 2018Document496 paginiFhsis Annual 2018shenric16Încă nu există evaluări
- Anti Psychotic DrugsDocument2 paginiAnti Psychotic DrugsJohn Corpuz100% (1)
- Patient Positioning in The Operating RoomDocument33 paginiPatient Positioning in The Operating Roomshenric16Încă nu există evaluări
- Professional Adjustment Leadership Management and ResearchDocument10 paginiProfessional Adjustment Leadership Management and Researchshenric16100% (1)
- Health Teaching PDFDocument1 paginăHealth Teaching PDFshenric16Încă nu există evaluări
- Nursing Board Exam Test Drill 3Document2 paginiNursing Board Exam Test Drill 3Kira100% (15)
- Community Health Nursing Practice Questions With RationalesDocument15 paginiCommunity Health Nursing Practice Questions With RationalesFelice Lamzon Labrador100% (2)
- Course Audit Professional AdjustmentDocument9 paginiCourse Audit Professional Adjustmentshenric16Încă nu există evaluări
- Fundamentals of NursingDocument31 paginiFundamentals of NursingAngelica Soriano93% (14)
- Palmer Complete Edited Royal PentagonDocument26 paginiPalmer Complete Edited Royal Pentagonshenric16100% (1)
- Reviewer For NleDocument14 paginiReviewer For Nleshenric16Încă nu există evaluări
- Cognitive DisordersDocument2 paginiCognitive DisordersSherrizah Alexis Naag NavaÎncă nu există evaluări
- 100 Item Comprehensive Exam With Answers and RationaleDocument21 pagini100 Item Comprehensive Exam With Answers and RationaleAijem Ryan93% (15)
- Maternal Ob NotesDocument37 paginiMaternal Ob Notesshenric16Încă nu există evaluări
- Community Health NursingDocument49 paginiCommunity Health Nursingshenric16Încă nu există evaluări
- Nle - July 2011Document12 paginiNle - July 2011shenric16100% (1)
- Community Health Nursing Practice Questions With RationalesDocument15 paginiCommunity Health Nursing Practice Questions With RationalesFelice Lamzon Labrador100% (2)
- Community Health NursingDocument49 paginiCommunity Health Nursingshenric16Încă nu există evaluări
- Pediatric Nursing Edison O Dangkeo RNDocument59 paginiPediatric Nursing Edison O Dangkeo RNshenric16100% (1)
- Final Outline Psychiatric NursingDocument52 paginiFinal Outline Psychiatric Nursingshenric16100% (1)
- Maternal and Child Health Nursing: KeepsDocument32 paginiMaternal and Child Health Nursing: Keepsshenric16Încă nu există evaluări
- Ms Penta NotesDocument84 paginiMs Penta Notesshenric16Încă nu există evaluări
- Medicationpart1 110202192115 Phpapp02Document10 paginiMedicationpart1 110202192115 Phpapp02Jessamine Rochelle Reyes Esberto100% (1)
- Maternal Ob NotesDocument37 paginiMaternal Ob Notesshenric16Încă nu există evaluări
- Erythroderma in Adults - UpToDateDocument39 paginiErythroderma in Adults - UpToDateGusti Ngurah PÎncă nu există evaluări
- Vital Signs Assessment TableDocument2 paginiVital Signs Assessment Tableapi-250869701Încă nu există evaluări
- Drug Name Drug Class Mechanism of Action Indications Contraindications Side Effects/ Adverse Effects Nursing ConsiderationDocument3 paginiDrug Name Drug Class Mechanism of Action Indications Contraindications Side Effects/ Adverse Effects Nursing ConsiderationKim SunooÎncă nu există evaluări
- Episiotomy DefinitionDocument4 paginiEpisiotomy Definitionnursing school0% (1)
- MCP NCP Benefits SlidesDocument13 paginiMCP NCP Benefits SlidesJonas Marvin AnaqueÎncă nu există evaluări
- Medical Aspects of Fitness For Offshore Work PDFDocument22 paginiMedical Aspects of Fitness For Offshore Work PDFParth DM100% (1)
- Bacterial Meningitis and Meningococcal Septicaemia: Implementing NICE GuidanceDocument18 paginiBacterial Meningitis and Meningococcal Septicaemia: Implementing NICE GuidanceZarwo Black UstadzÎncă nu există evaluări
- Sífilis Ocular 2021 Super CompletoDocument69 paginiSífilis Ocular 2021 Super CompletoouranpisÎncă nu există evaluări
- Third Year Bachelor of Pharmacy 2019 Pattern (1) TimetableDocument2 paginiThird Year Bachelor of Pharmacy 2019 Pattern (1) TimetablesaurabhpkotkarÎncă nu există evaluări
- Guidance Guide For Caregivers of Patients With DementiaDocument4 paginiGuidance Guide For Caregivers of Patients With DementiaSabrina JonesÎncă nu există evaluări
- The Diagnoses of Community NursingDocument8 paginiThe Diagnoses of Community NursingIOSRjournalÎncă nu există evaluări
- Assistant: SecretariesDocument15 paginiAssistant: Secretarieskima conÎncă nu există evaluări
- Group 7 - Subgroup 2 Chief ComplaintDocument5 paginiGroup 7 - Subgroup 2 Chief ComplaintKAYLLIEN DURANÎncă nu există evaluări
- The Effects of Pay-for-Performance Programs On Health, Health Care Use, and Processes of CareDocument14 paginiThe Effects of Pay-for-Performance Programs On Health, Health Care Use, and Processes of CareMasrun FatanahÎncă nu există evaluări
- Physiopedia DSDocument42 paginiPhysiopedia DSyenrilisnaÎncă nu există evaluări
- Responsible Parenthood and Reproductive Health Act of 2012Document22 paginiResponsible Parenthood and Reproductive Health Act of 2012Janette Anne Reyes MacaraigÎncă nu există evaluări
- List of Clinic Chains in UsDocument90 paginiList of Clinic Chains in Usarpit.mÎncă nu există evaluări
- ICDSDocument21 paginiICDSKrishnaveni MurugeshÎncă nu există evaluări
- Case Study:: CholelithiasisDocument19 paginiCase Study:: CholelithiasisGillarhymesÎncă nu există evaluări
- Staffing July 10 12 2022Document5 paginiStaffing July 10 12 2022Kasandra Dawn Moquia BerisoÎncă nu există evaluări
- SealBio: A Novel, Non-Obturation Endodontic Treatment Based On Concept of RegenerationDocument3 paginiSealBio: A Novel, Non-Obturation Endodontic Treatment Based On Concept of RegenerationPressInitiativeÎncă nu există evaluări
- The Problem: Best!'Document4 paginiThe Problem: Best!'HospitilioÎncă nu există evaluări
- Caregivers For Compromise PaperDocument2 paginiCaregivers For Compromise PaperChris VaughnÎncă nu există evaluări
- The Hospital AND The Department of Pharmaceutical ServicesDocument32 paginiThe Hospital AND The Department of Pharmaceutical Servicesdeep singhÎncă nu există evaluări
- Nursing Interventions For Identifying and Managing Acute Dysphagia Are Effective For Improving Patient OutcomesDocument9 paginiNursing Interventions For Identifying and Managing Acute Dysphagia Are Effective For Improving Patient OutcomesawinsyÎncă nu există evaluări
- 2021 Small For Gestational Age - StatPearls - NCBI BookshelfDocument12 pagini2021 Small For Gestational Age - StatPearls - NCBI BookshelfIlda IldaÎncă nu există evaluări
- Tugas Bahasa Inggris Nama: Yuniarti NPM: 6219111 Kelas: 3ADocument2 paginiTugas Bahasa Inggris Nama: Yuniarti NPM: 6219111 Kelas: 3AKiki Opo MeneÎncă nu există evaluări
- Zinc Deficiency and Clinical Practice PDFDocument6 paginiZinc Deficiency and Clinical Practice PDFBunga Erlita RosaliaÎncă nu există evaluări
- Cues/Data Family Nursing Diagnosis: B. First and Second Level AssessmentDocument6 paginiCues/Data Family Nursing Diagnosis: B. First and Second Level AssessmentMaranatha BuenaventuraÎncă nu există evaluări
- ConjunctivitisDocument16 paginiConjunctivitisClark LopezÎncă nu există evaluări