Documente Academic
Documente Profesional
Documente Cultură
Studiu Brazilia
Încărcat de
Dragos GarofilDescriere originală:
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Studiu Brazilia
Încărcat de
Dragos GarofilDrepturi de autor:
Formate disponibile
origiNal article | artigo origiNal
Secondary hyperparathyroidism status in Brazil: Brazilian Census of Parathyroidectomy
Situao do hiperparatireoidismo secundrio autnomo no Brasil: dados do Censo Brasileiro de Paratireoidectomia
Authors Rodrigo Bueno de Oliveira 1,2 Eduardo Neves da Silva 2 Douglas Moraes Freire Charpinel 2 Jos Edevanilson Barros Gueiros 1 Carolina lara Neves 1 Elisa de Albuquerque Sampaio 1 Fellype de Carvalho Barreto 1 Cristina Karohl 1 Melani Custdio Ribeiro 1 Rosa Maria Affonso Moyss 1 Vanda Jorgetti 1 Aluizio Barbosa de Carvalho 1
Sociedade Brasileira de Nefrologia SBN: Comit de Distrbio Mineral e sseo na Doena Renal Crnica DMO-DRC So Paulo SP Brazil. 2 Universidade de Santo Amaro Unisa.
1
ABstrAct
Introduction: Secondary hyperparathyroidism (SHP) is a common and serious complication of chronic kidney disease (CKD), with a negative impact on morbidity and mortality. Despite advances in the clinical management of SHP, treatment failure still occurs in a significant number of patients. In such cases, parathyroidectomy (PTx) is indicated. Objective: To have an overview of the prevalence of severe SHP and of its surgical treatment in hemodialysis (HD) patients in Brazil. Methods: This was an observational and descriptive study. Data were obtained from questionnaires posted to 660 dialysis units (DU). Results: Results are expressed in absolute values and percentages, or means and standard deviation, as appropriate. 226 (34%) DU answered the questionnaire, providing data about 32,264 HD patients. The prevalence rate of severe SHP (PTH > 1,000 pg/mL) was 10.7% (n = 3,463). 68 hospitals countrywide perform PTX. Around 40% of them are university centers. 49 (21.7%) DU reported not to have a specialized medical center to refer their patients with severe SHP. 74 (33%) DU reported that the time interval between surgery indication and its performance was over 6 months. The main recognized obstacles to surgery performance were: difficulty to perform the preoperative exams, lack of head and neck surgeons and the long waiting time. Conclusions: Although severe SHP is highly prevalent in Brazil, a significant number of patients do not have access to PTx. Better public health policies and liaison between nephrologists and head and neck surgeons are urgently required to change this reality. Keywords: Renal Insufficiency Chronic. Hyperparathyroidism, Secondary. Parathyroidectomy.
resuMo
Introduo: O hiperparatireoidismo secundrio (HPS) uma complicao comum e grave no curso da doena renal crnica (DRC), com impacto direto sobre a morbidade e mortalidade desses pacientes. Apesar dos avanos no tratamento clnico do HPS a falncia teraputica ocorre em parcela significativa dos pacientes. Nesses casos, a paratireoidectomia (PTx) indicada. Objetivo: Este trabalho visa abordar a situao atual no Brasil de pacientes com HPS em hemodilise com indicao de PTx. Mtodos: Estudo observacional, descritivo, com dados obtidos de questionrio enviado a 660 centros de dilise (CD). Resultados: Os resultados esto expressos em valores absolutos, mdias e desvio padro; 226 (34%) CD responderam ao questionrio, representando 32.264 pacientes em hemodilise (HD). A prevalncia de pacientes com paratormnio (PTH) > 1.000 pg/mL foi de 3.463 (10,7%). Em 49 (21,7%) CD no possvel encaminhar os pacientes para PTx. Cerca de 40% dos servios que realizam PTx so ligados a centros universitrios. Em 74 (33%) CD o tempo de espera para que um paciente seja operado superior a 6 meses. Foram contabilizados 68 servios que realizam PTx. Os principais problemas relacionados para a realizao de PTx foram: dificuldades com a realizao dos exames properatrios, escassez de cirurgies de cabea e pescoo, e longa fila de espera. Concluses: a prevalncia de HPS grave elevada em nosso meio. Uma parcela significativa de pacientes no tem acesso ao tratamento cirrgico. Uma melhor organizao das polticas de sade pblica, alm de um maior entrosamento entre nefrologistas e cirurgies de cabea e pescoo, em torno dessa questo, so necessrios para a mudana dessa realidade. Palavras-chave: Insuficincia Renal Crnica. Hiperparatireoidismo Secundrio. Paratireoidectomia.
457
Submitted on: 10/07/2011 Approved on: 11/04/2011
Correspondence to: Rodrigo Bueno de Oliveira Avenida Doutor Arnaldo, 455, 3 andar, sala 3.342 Cerqueira Csar So Paulo SP Brazil Zip code 01246-903 E-mail: rodrigobueno.hc@ gmail.com This study was undertaken at the Brazilian Nephrology Society. The authors report no conflict of interest.
Brazilian Census of Parathyroidectomy
Introduction
Chronic kidney disease (CKD) affects millions of people worldwide, being now considered a public health problem. 1 CKD patients have a high mortality rate, 2 a significant proportion of which is attributed to mineral-bone disorder (MBD), a condition encompassing biochemical alterations, vascular calcification and bone disease.1,3 With CKD progression, there is reduced synthesis of calcitriol and reduced serum calcium (Ca) levels, with increased serum levels of phosphorus (P), FGF-23 and parathyroid hormone (PTH), characterizing secondary hyperparathyroidism (SHP). 4 These alterations may also be associated with vascular calcification and bone fractures.2 SHP treatment has traditionally been based on the control of hyperphosphatemia with dietary restriction and the use of P-chelating agents, of hypocalcemia with calcium salts and calcitriol, and of the PTH levels with calcitriol and, more recently, with selective vitamin D-receptor activators (VDRA) and calcium-mimetics.5,6 In spite of the advances in the treatment of SHP, therapeutic failure is frequent, with an estimated 5.5-30% of CKD patients on dialysis eventually undergoing parathyroidectomy (PTx) for inadequate response to medical therapy. These figures increase with dialysis time.7-9 Although another option to PTx is percutaneous ethanol or calcitriol injection, the only study undertaken in Brazil did not show satisfactory results. 8 According to the Brazilian Nerphrology Society`s guidelines, PTx is indicated when PTH serum levels remain persistently over 800 pg/mL, in the following settings: (a) hypercalcemia and/or hyperphosphatemia refractory to medical treatment; (b) extraosseous calcifications (soft and/or cardiovascular tissues) or calcific uremic arteriolopathy (calciphylaxis); (c) progressive, debilitating, advanced bone disease unresponsive to medical treatment and; (d) large-sized parathyroid glands (volume > 1.0 cm3) on ultrasonography. 10 The high prevalence of CKD patients with SHP and PTx indication has been recognized in several countries. In Japan, 10% of the patients on hemodialysis (HD) for over 10 years and 30% of those on HD for over 20 years, need PTx.7 In 1982, the European Dialysis and Transplantation Association Registry reported a 5/1,000 patients/year incidence of PTx during the second or third year on dialysis, but a rate of over 40/1,000 patients/year among those on dialysis
for more than 10 years.11 The Dialysis Outcomes and Practice Pattern Study (DOPPS), which assessed the HD status and quality from 1996 through 2001 in European countries, the United States and Japan, revealed that PTx is less frequent in Japan than in Europe (4.1% prevalence, with a 0.6/100 patients/year PTx incidence).12 In Brazil, the prevalence rate of SHP patients with PTx indication is unknown. It is thought that the access of SHP patients to medical and surgical treatment is limited and particularly restricted to university centers. It is noteworthy that CKD conservative treatment is offered by few centers, which hampers early control of MBD. Moreover, PTH measurement, both in patients on conservative treatment and in those on dialysis, is only allowed (RDC ordnance 154) at 6 month-intervals.13 There are also restrictions on the use of some medications, such as calcium mimetics and new vitamin D analogues. SHP is thus underdiagnosed and undertreated. The purpose of this study was to assess the prevalence of HD patients with SHP and PTx indication.in Brazil, as well as identify the factors that influence the availability of surgery for SHP.
Methods
This was an observational, descriptive, crosssectional study. During the August 2010-March 2011 period, the Brazilian Nephrology Society Committee of Mineral-Bone Disorder in Chronic Kidney Disease posted a questionnaire to the technical responsible staff of the 660 Brazilian dialysis units (DU). The questions concerned SHP, and clinical and biochemical data covering the second semester of 2010 were collected. The questionnaire enquired about: (1) The number of HD patients in the unit; (2) the number of patients with PTH levels over 1,000 pg/mL; (3) the biochemical method used for PTH measurement; (4) the referral procedure once SHP with PTx indication was diagnosed; (5) average time on the waiting-list for PTx; (6) source of medications to treat the bone hunger syndrome in the postoperative period of PTx and; (7) the main obstacles to the performance of PTx. Each question was followed by a blank space for information recording. A serum PTH level of 1,000 pg/mL was defined as the cut-off value above which there was a high likelihhod of PTx indication.
458
J Bras Nefrol 2011;33(4):457-462
Brazilian Census of Parathyroidectomy
The results were described as absolute values, percentages, means and standard deviations (SD).
Results
Of the 660 questionnaires posted 226 (34%) were answered, which corresponded to a sample of 32,264 patients, an estimated 35% of the whole dialysis population of Brazil, according to the 2010 dialysis census. 14 Table 1 shows the numbers of DU which responded, and of their patients with PTH > 1,000 pg/ml, according to the geographic region. So Paulo had the highest figures (60 DU and 9,240 patients) and Par the lowest ones (1 DU and 58 patients). 10.7% of the patients (3,463 out of the total 32,264) had PTH > 1,000 pg/ml, with the highest rate in Rio de Janeiro (22.9%; n = 689) and the lowest one in Par (1.7%, n = 1).
Chemoluminescence was the most frequent technique for PTH measurement, being used by 165 (73%) units. 43 (19%) units used another method and 17 (8%) did not inform the method used. Table 2 shows the referral procedure used for SHP patients with PTx indication. 49 (21.7%) units could not refer these patients, which corresponds to a total of 6,440 patients, 650 (10.1%) of whom had PTH levels > 1,000pg/ml, with surgical indication, although they will not be operated on. 28 (41.2%) of the services providing PTx belong to university hospitals. Table 3 shows the distribution of the services performing PTx, according to the geographical regions. The northern region has no such service, and the center-west has only 2. These two regions have 74 DU, with a total of 7,771 patients.14 So Paulo has the largest number of services, with 18 (26.4%). Waiting-time for
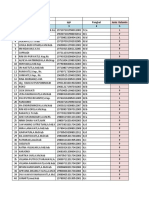
Table 1
Number of dialysis units number and percentage of the total of patients on dialysis and number and percentage of patients with pathyroid hormone levels > 1,000 pg/ml according to geographic region.
Number of dialysis units 122 55 32 14 3 226 Number of patients 18,592 (57 .6%) 6,039 (18.7%) 5,695 (17 .7%) 1,810 (5.6%) 128 (0.4%) 32,264 (100%) Number of patients with PTH > 1.000 pg/mL 2,279 (12.3%) 456 (7 .6%) 522 (9.2%) 201 (11.1%) 5 (3.9%) 3,463 (10.7%)
Region South-east South North-east Center-west North Total
PTH: parathyroid hormone.
Table 2
Referral of patients with secondary
hyperparathyroidism and indication of parathyroidectomy
Table 3
Services and university hospitals performing parathyroidectomy:
number and percentage of the total, according to geographical region in
Destination Services with CKD-MBD ambulatory facilities No referral arrangements The same unit where dialysis is performed Unified Health System hospitals Insurance-covered hospitals Total
Number of dialysis units 132 (58.4%) 49 (21.7%) 32 (14.2%) 10 (4.4%) 2 (0.9%) 226 (100%)* Region South-east South North-east Center-west North Total
Brazil
Number of services 36 (53%) 21 (31%) 9 (13%) 2 (3%) 0 (0%) 68 (100%) Number of university hospitals 17 (25%) 6 (8.8%) 5 (7 .3%) 0 (0%) 0 (0%) 28 (41.2%)
MBD: mineral-bone disease; CKD: chronic kidney disease *1 (0.4 %) dialysis unit informed that they rarely had patients with secondary hyperparathyroidism.
J Bras Nefrol 2011;33(4):457-462
459
Brazilian Census of Parathyroidectomy
PTx is described in Table 4. In 74 (32%) units the waiting time is longer thab 6 months. As for drug hunger syndrome medication (calcitriol and calcium salts) dispensation, 156 (69%) units request the drugs from the Special Medication Program of the Brazilian Unified Health System, 41 (18%) redirect the medications from patients who had the drugs withdrawn, because of hypercalcemia and hyperphosphatemia, to those in need, and 18 (8%) cover the cost of the drugs. 5% of the units did not inform about this issue. Table 5 describes the main obstacles to the performance of PTx. 136 (60%) units reported 2 difficulties and 75 (33%) reported 3 difficulties.
Discussion
This was the first study undertaken in Brazil about the status of SHP patients and their need of PTx. The response rate (34%) was low and unevenly distributed according to geographical region, with Par and Acre having the lowest figures. The prevalenced rate of SHP was 10,7%, taking into account PTH levels > 1,000pg/ml, a situation in which PTx indication is practically unequivocal. The prevalence rate would probably be higher if the 800pg/ml cut-off point recommended by the Clinical Practice Brazilian Guidelines were followed. It is noteworthy that a significant percentage of patients with PTH up to 500pg/ml do not respond to medical therapy either, which would further increase the number of patients requiring surgery. As for the services perfoprming PTx, 28 (41.1%) are linked to university hospitals. There are few such services belonging to the supplementary health network (n = 2; 0.9%). Because PTx is a middle-complexity surgical procedure, few patients requiring an intensive care environment for their recovery, secondary-care hospitals staffed with nephrologists and head and neck surgeons could implement the procedure, thus alleviating the load of university hospitals. According to the Brazilian Dialysis Census, 13.3% of the country`s dialysis patients have supplementary insurance coverage.14 However, few DU manage to refer their privately insured patients to PTx in the privately insured hospitals, thus further adding to the cost to be met by the Unified Health System. Most patients undergoing PTx develop the bone hunger syndrome during the postoperative period, thus requiring large amounts of calcium salts and calcitriol. Although most DU obtain calcitriol from the Special Medications Program of the Unified Health System, bureaucratic contraints lead to the delayed dispensation of insufficient amounts, as reported by 15 (6.6%) DU. This forces the units to redirect medication from those who had it withdrawn due to hypercalcemia and/or hyperphosphatemia, or pay with their own or the patients` resources. In Brazil, ,68 services perform PTx, of which 36 (53%) are in the south-east. If we take into account that Brazil has approximately 92,000 patients on dialysis, and that the estimated prevalence of SHP with indication of PTx is 10.7%, about 9,800 patients should be operated on. 350 to 500 PTx are estimated to be performed every year in Brazil, which allows a projection of 20 years before all present surgical indications are met.
Table 4
Waiting-time for parathyroidectomy
Number of dialysis units 26 (12%) 56 (25%) 46 (20%) 19 (8%) 9 (4%) 52 (23%) 18 (8%) 226 (100%)
Time (months) <1 > 1 and 6 > 6 and 12 > 12 and 24 > 24 No possibility of referral No information Total
Table 5
Main obstacles to the performance
of parathyroidectomy reported by the dialysis units
Obstacle reported Difficulty with preoperative examinations Lack of head and neck surgeons Long waiting time for PTx Few ambulatory services specialized in CKD-MBD Difficulty to get the unified health system authorization for PTx Lack of hospital beds Difficulty to get postoperative medications Patient`s refusal to undergo PTx Lack of intensive care beds
Number of dialysis units 88 (38.9%) 64 (28.3%) 60 (26.5%) 52 (23%) 31 (13.7%) 29 (12.8%) 15 (6.6%) 10 (4.4%) 7 (3%)
PTx: hyperparathyroidectomy; MBD: mineral-bone disorder; CKD: chronic kidney disease.
460
J Bras Nefrol 2011;33(4):457-462
Brazilian Census of Parathyroidectomy
A study undertaken at the CKD-MBD ambulatory service of the Hospital das Clnicas of the So Paulo University showed a 25%/year mortality rate among those waiting for a PTx, almost twice as high as that among the general population of patients on dialysis.15 According to the Brazilian Head and Neck Society, Brazil has 529 specialists in the field. The north and center-west have 48 specialists and 74 DU, with about 7,771 patients; yet, no PTx is performed in these regions. In So Paulo, although there are 18 services performing PTx and 241 specialists, the highest density in Brazil, in the two main CKD-MBD ambulatory reference centers (So Paulo University and Federal University of So Paulo) the waiting time is over 18 months. There are technical, political, economical and organizational reasons hampering liasion of public health managers, dialysis units, nephrologists, head and neck surgeons and centers performing PTx. One of the main obstacles to performing PTx concerns preoperative exams. Patients under 40 years of age, without diabetes mellitus, with no symptoms of coronary disease and who are no smokers are at low risk of cardiovascular complications, which obviates the need of invasive cardiovascular investigations. Specific PTx preoperative investigations include neck ultrasonography and parathyroid scintigraphy for gland localization. These exams can be omitted, however, with resource to intraoperative localization of the glands. Likewise, intensive care beds are seldom required after PTx. These considerations should reduce the waiting lists. At the same time, the health system must be organized with the creation of reference services for PTx, increased access to SHP diagnosis and treatment, greater degree of freedom for PTH determination, addition of calcium-mimetics and vitamin D receptor agonists to the list of medications dispensed by the Unified Health System and greater patients` access to nephrologists and head and neck surgeons. Simple actions, such as medication dispensation during the bone hunger postoperative period, authorization of PTx performance in secondary care hospitals and revision of the reimbursement of the professionals involved with the surgical procedure and postoperative care could solve many problems. Medical associations, such as the Brazilian Nephrology Society and the Brazilian Head and Neck Surgery Society should not only lead the continuing professional education and issue treatment protocols in this field, but also warn public health
managers about the situation of CKD patients with SHP in the country. The main limitations of our study were its crosssectional, observational design, along with the regional disparities and the 1,000 pg/ml as the cut-off point for PTx indication, which probably reduced the SHP prevalence. Furthermore, we did not obtain immediate morbidity and mortality data, such as the length of hospital admissions due to SHP complications or surgery-related complications.
Acknowledgements
The Brazilian Nephrology Society thanks the dialysis units which voluntarily responded the questionnaire, and Mrs Rosalina Soares and Mr Wellington Anselmo, from the executive secretariat, for their invaluable help with this study.
References
1. Eknoyan G, Lameire N, Barsoum R, et al. The burden of kidney disease: improving global outcomes. Kidney Int 2004;66:1310-4. 2. Block GA, Klassen PS, Lazarus JM, et al. Mineral metabolism, mortality, and morbidity in maintenance hemodialysis patients. J Am Soc Nephrol 2004; 15:2208-21. 3. Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Work Group. KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease-mineral and bone disorder (CKDMBD). Kidney Int 2009; 76(Suppl):S1-S130. 4. Gutierrez O, Isakowa T, Rhee E, et al. Fibroblast Growth Factor-23 mitigates hyperphosphatemia but accentuates calcitriol deficiency in chronic kidney disease. J Am Soc Nephrol 2005;16:2205:15. 5. Barreto FC, Oliveira RA, Oliveira RB, Jorgetti V. Pharmacotherapy of chronic kidney disease and mineral bone disorder. Expert Opin Pharmacother 2011; 12:2627-40. 6. Cunningham J, Locatelli F, Rodriguez M. Secondary hyperparathyroidism: pathogenesis, disease progression, and therapeutic options. Clin J Am Soc Nephrol 2011;6:913-21. 7. Tominaga Y. Current status of parathyroidectomy for secondary hyperparathyroidism in Japan. Nephrol Dial Tranplant plus 2008;1(Suppl):iii35:iii8. 8. Gueiros JEB, Chammas MC, Gerard R, et al. Percutaneous ethanol (PEIT) and calcitriol (PCIT) injection therapy are ineffective in treating severe secondary hyperparathyroidism. Nephrol Dial Transplant 2004;19:657-63. 9. Malberti F, Marcelli D, Conte F, et al. Parathyroidectomy in patients on renal replacement therapy: an epidemiologic study. J Am Soc Nephrol 2001;12:1242-8. 10. Sampaio EA, Moyss RMA. II Diretrizes Brasileiras de Prtica Clnica para o Distrbio Mineral e sseo na
J Bras Nefrol 2011;33(4):457-462
461
Brazilian Census of Parathyroidectomy
Doena Renal Crnica. Paratireoidectomia na DRC. J Bras Nefrol 2011;33(Suppl):31-4. 11. Young EW, Albert JM, Satayathum S, et al. Predictors and consequences of altered mineral metabolism: the dialysis outcomes and practice pattern study. Kidney Int 2005;67:1179-87. 12. Wing AJ, Broyer M, Brunner FP, et al. Combined report on regular dialysis and transplantation in Europe. XV, 1984. Proc Eur Dial Transplant Assoc 1985;22:5-54. 13. Brasil. Resoluo Anvisa-RDC N 154 de 15 de junho de 2004. Estabelece o Regulamento Tcnico para o
funcionamento dos Servios de Dilise. Dirio Oficial da Unio. 2004 Jun 17; Seo 1:65-69. [cited 2011 Sep 09]. Available from: http://www.sbn.org.br/pdf/ portarias/resolucao154. 14. Sesso RCC. Relatrio do Censo Brasileiro de Dilise, 2010. J Bras Nefrol 2011;33:442-7. 15. Goldenstein PT, Carmo LPF, Coelho FO, et al. Association of Secondary Hyperparathyroidism with High Mortality and Morbidity in Dialysis Patients. [abstract]. Renal Week 2010: SA-PO2905.
462
J Bras Nefrol 2011;33(4):457-462
S-ar putea să vă placă și
- Numărul Pensionarilor de Asigurări Sociale de Stat Şi Agricultori În Anul 2019Document1 paginăNumărul Pensionarilor de Asigurări Sociale de Stat Şi Agricultori În Anul 2019Dragos GarofilÎncă nu există evaluări
- Sh-36 Primary HPTDocument7 paginiSh-36 Primary HPTDragos GarofilÎncă nu există evaluări
- Pain Measurement PDFDocument13 paginiPain Measurement PDFDragos GarofilÎncă nu există evaluări
- PLAYLIST JumiJuma - Karaoke Promenada MallDocument2 paginiPLAYLIST JumiJuma - Karaoke Promenada MallDragos GarofilÎncă nu există evaluări
- Chestionarul SF 36Document2 paginiChestionarul SF 36Dragos GarofilÎncă nu există evaluări
- Failure of Central V.catheterisationDocument2 paginiFailure of Central V.catheterisationDragos GarofilÎncă nu există evaluări
- Rectal Cancer Checklist SmallDocument2 paginiRectal Cancer Checklist SmallDragos GarofilÎncă nu există evaluări
- NR CRT Simptom: Scorul PAS (Parathyroidectomy Alleviation of Symptoms)Document2 paginiNR CRT Simptom: Scorul PAS (Parathyroidectomy Alleviation of Symptoms)Dragos GarofilÎncă nu există evaluări
- Arteriovenous FistulasDocument21 paginiArteriovenous FistulasDragos GarofilÎncă nu există evaluări
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Perception and Awareness of Oral and Maxillofacial Surgery Speciality Among Medical Postgraduate TraineesDocument5 paginiPerception and Awareness of Oral and Maxillofacial Surgery Speciality Among Medical Postgraduate TraineesAmadea EmanuelaÎncă nu există evaluări
- PSM 2020-2008 Regular Question Papers WBUHS © Medical JunctionDocument15 paginiPSM 2020-2008 Regular Question Papers WBUHS © Medical JunctionJyotirmayeeÎncă nu există evaluări
- Health Care Delivery SystemDocument40 paginiHealth Care Delivery SystemArianne Kamille Andes100% (1)
- PCCM 2014Document703 paginiPCCM 2014PrastyaGalihÎncă nu există evaluări
- 396 1 MHSS Namibia MC Costing ReportDocument74 pagini396 1 MHSS Namibia MC Costing Reportckgeorge1303Încă nu există evaluări
- Letter of RecomendationDocument2 paginiLetter of RecomendationJorge Luis Sánchez Alarcón100% (1)
- NagpurDocument3 paginiNagpurVAIBHAV P ANPATÎncă nu există evaluări
- Laws That Maybe Related To Nursing PracticeDocument8 paginiLaws That Maybe Related To Nursing Practicealvin1317020009304100% (5)
- Posttest CHNDocument7 paginiPosttest CHNMeeKo VideñaÎncă nu există evaluări
- Prayer TherapyDocument7 paginiPrayer Therapymit-mit100% (1)
- NICE DRAFT - Drug Allergy Diagnosis and Management of Drug Allergy in Adults, Children and Young PeopleDocument29 paginiNICE DRAFT - Drug Allergy Diagnosis and Management of Drug Allergy in Adults, Children and Young Peopletian download doangÎncă nu există evaluări
- ��تجميعات الفارما�Document4 pagini��تجميعات الفارما�Turky TurkyÎncă nu există evaluări
- MAPEH 6 - Demo COTDocument36 paginiMAPEH 6 - Demo COTLucena GhieÎncă nu există evaluări
- MLGP MacArthur FinalDocument47 paginiMLGP MacArthur Finalcatherine joy macalosÎncă nu există evaluări
- Set 1 PDFDocument62 paginiSet 1 PDFAlyssa MontimorÎncă nu există evaluări
- Moderna CEO Stephane Bancel Says Coronavirus Vaccine Price Will Be LowDocument3 paginiModerna CEO Stephane Bancel Says Coronavirus Vaccine Price Will Be Lowtp4oyk fdtaz4100% (1)
- A. Factors in Mental Disorders: Name: SCORE: - /91 Intro To Psych Module 22-Assessment and Anxiety DisordersDocument4 paginiA. Factors in Mental Disorders: Name: SCORE: - /91 Intro To Psych Module 22-Assessment and Anxiety DisorderssusanwhittenÎncă nu există evaluări
- Epidemiology of Head Injury - A Level 1 Taei Centre StudyDocument2 paginiEpidemiology of Head Injury - A Level 1 Taei Centre StudyIJAR JOURNALÎncă nu există evaluări
- Form Pip - Dinkes (3) Puskesmas Purwodadi IIDocument9 paginiForm Pip - Dinkes (3) Puskesmas Purwodadi IIUptd Puskesmas Purwodadi IIÎncă nu există evaluări
- NCM 105 Nutrition and Diet Therapy:: Ferkiya A. Abduwa, R.NDocument29 paginiNCM 105 Nutrition and Diet Therapy:: Ferkiya A. Abduwa, R.NLouie Pangilinan LanajaÎncă nu există evaluări
- 88 Hospital Approved 02072021Document3 pagini88 Hospital Approved 02072021yogesh85kumawatÎncă nu există evaluări
- Indian Diagnostic Market AnalysisDocument2 paginiIndian Diagnostic Market Analysisradheshyam08Încă nu există evaluări
- The Advantages and Disadvantages of Being A DoctorDocument2 paginiThe Advantages and Disadvantages of Being A DoctorKarinaÎncă nu există evaluări
- Patients' Knowledge of Diabetes Complications and S Elf-Management Practices in GhanaDocument18 paginiPatients' Knowledge of Diabetes Complications and S Elf-Management Practices in GhanaNurul pattyÎncă nu există evaluări
- Physical Education and Health 12Document2 paginiPhysical Education and Health 12Jenia Alexis CapaÎncă nu există evaluări
- October 2019 PDFDocument71 paginiOctober 2019 PDFFehr GrahamÎncă nu există evaluări
- A History of Nurses Charged With Killing PatientsDocument2 paginiA History of Nurses Charged With Killing PatientsBrayen SabapatheeÎncă nu există evaluări
- Brazil's Unified Health System - The First 30 Years and Prospects For The FutureDocument12 paginiBrazil's Unified Health System - The First 30 Years and Prospects For The FutureRaisa Paredes PÎncă nu există evaluări
- Balance Method RevBalance Method Revolutionizes Acupunctureolutionizes AcupunctureDocument3 paginiBalance Method RevBalance Method Revolutionizes Acupunctureolutionizes Acupuncturedrtommy75Încă nu există evaluări