Documente Academic
Documente Profesional
Documente Cultură
Blood Brain Barrier PDF
Încărcat de
manoj_rkl_07Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Blood Brain Barrier PDF
Încărcat de
manoj_rkl_07Drepturi de autor:
Formate disponibile
Blood Brain Barrier
Darryl Ronnie Peterson, Chicago Medical School, Chicago, Illinois, USA
The blood brain barrier serves to restrict and control the movement of substances between the general circulation and brain extracellular fluid. It participates in regulating the volume and composition of fluid surrounding the brain through specific transport processes, and thus contributes to homeostasis of the central nervous system.
Introductory article
Article Contents
. Entry of Substances from Blood into Brain . Brain Capillaries are Impermeant Except in Specialized Areas . Tight Junctions and High Electrical Resistance Between Capillary Endothelial Cells . Contributions of Astrocytes to a Well-sealed Blood Brain Barrier . Getting Past the Barrier: Small Lipophilic Molecules and Molecules with Special Transport Systems . Delivering Drugs to the Brain . Summary
Entry of Substances from Blood into Brain
The bloodbrain barrier serves to restrict and control the movement of substances between the general circulation and brain extracellular uid. It participates in regulating the volume and composition of uid surrounding the brain through specic transport processes, and thus contributes to homeostasis of the central nervous system. Nutrients such as glucose and certain amino acids are allowed to enter the brain, but blood-to-brain passage of neuroexcitatory substances, which could otherwise alter brain function, is essentially prevented. Because of its restrictive properties, drugs intended to treat neurological disorders at the level of the brain must be designed to penetrate the barrier. The bloodbrain barrier consists of endothelial cells which line cerebral capillaries (Figure 1). Unlike endothelium elsewhere in the body, these cells possess tight junctions which separate the plasmalemma into luminal
Abluminal membrane Tight junction Astrocyte Luminal membrane Brain capillary Astrocyte Blood Endothelial cell
(blood facing) and abluminal (brain facing) membrane domains, each with a dierent set of properties. Thus, the endothelial cells forming the bloodbrain barrier are polarized, and function in many respects like an epithelium. This allows for net unidirectional movement of certain electrolytes and water across the barrier, and selective transport of other substances. Because the tight junctions greatly limit paracellular transport (i.e. between cells), substances must cross the bloodbrain barrier by penetrating two plasma membrane domains arranged in series. The organization of transport proteins in these two membrane domains determines the direction and extent of transport. The volume of extracellular uid surrounding the brain is quite small, averaging only about 250 mL in an average human adult. The total surface area of the bloodbrain barrier is approximately 12 m2 (100 ft2), however, suggesting a relationship sucient for adequate regulation. Because the size of the brain extracellular uid compartment is so small, it is implied that even modest changes in its volume or composition could impact signicantly on brain function. For instance, a pathological accumulation of brain extracellular uid could potentially increase damaging pressure to the brain in a compartment restricted by the skull.
Brain Capillaries are Impermeant Except in Specialized Areas
Basement membrane
Neuron Pericyte
Figure 1 The blood brain barrier consists of endothelial cells lining brain capillaries. These cells are connected by tight junctions, which separate the plasmalemma into luminal (blood facing) and abluminal (brain facing) plasma membrane domains. The capillaries are surrounded by a basement membrane, and are closely associated with astrocytes, neurons and pericytes.
Cerebral capillary endothelial cells provide a tight barrier between the blood and brain tissue in most regions of the brain, with a few exceptions. Relatively small regions associated with the brain ventricles are termed circumventricular organs (CVOs), which include the area postrema, median eminence, neurohypophysis, organum vasculosum lamina terminalis, pineal gland and subfornical organ. Capillaries perfusing these structures are highly porous, and allow substances in the blood to come in contact with
1
ENCYCLOPEDIA OF LIFE SCIENCES / & 2001 Nature Publishing Group / www.els.net
Blood Brain Barrier
neurons in the central nervous system. In some instances, this may provide a means for circulating hormones to inuence brain function, or for neurohormones to enter the blood. It has been estimated, however, that the surface area of the bloodbrain barrier is about 5000 times that of the CVOs, indicating that the barrier is essentially intact.
Tight Junctions and High Electrical Resistance Between Capillary Endothelial Cells
Closely associated with cerebral capillaries forming the bloodbrain barrier are pericytes, astrocytes and neurons (see Figure 1). These cells are present at the abluminal pole of the endothelial cells, separated by a basement membrane. Because of the intimate relationship of these cells with the capillaries, it was originally questioned whether they formed part of the barrier. To address this issue, early studies using horseradish peroxidase showed that this macromolecular marker could pass across the basement membrane and between the pericytes, astrocytes and neurons, but was stopped at the level of the endothelial tight junctions. This conrmed that the capillary endothelial cells represent the true bloodbrain barrier. The presence of tight junctions in the bloodbrain barrier greatly increases electrical resistance across the endothelium. This indicates that passage of electrolytes (i.e. Na 1 , Cl 2 ) between the cells is largely restricted, and that movement is dependent upon specic transport proteins present in the luminal and abluminal plasma membranes. Thus, as indicated above, a largely transcellular rather than a paracellular route of movement is implied. The specialized endothelial cells of the blood brain barrier develop a resistance as high as 8000Ocm 2 2, which is typical of some tight epithelia. The high electrical resistance also implies that solutes other than electrolytes must cross the bloodbrain barrier transcellularly.
cells are grown in tissue culture without astrocytes, they develop a typical nonpolar endothelium without tight junctions, and a low electrical resistance. If these same cells are grown in the presence of astrocytes, however, they become polarized and dierentiate into a high resistance bloodbrain barrier in vitro. Similar results can be achieved by culturing the cells in a medium that has been conditioned by previous exposure to astrocytes. In both cases, it is believed that a growth factor released by astrocytes stimulates dierentiation of growing endothelial cells destined to become the bloodbrain barrier. Specically, dierentiation includes the development of tight junctions and polarization of the cells. Furthermore, astrocytes appear to induce the expression of certain membrane-associated proteins, including the glucose transporter GLUT-1 (see below), potassium transporters, and the enzyme g-glutamyltranspeptidase. Upregulation of the glucose carrier is especially noteworthy, since transport of glucose from blood to brain is necessary for energy production in the central nervous system. Recently, this discussion has included the possibility that neurons and pericytes may also participate in the development of brain capillary endothelial cells.
Getting Past the Barrier: Small Lipophilic Molecules and Molecules with Special Transport Systems
Substances that are able to pass across the bloodbrain barrier include small lipophilic molecules. A small size and lipophilic disposition allow these molecules to penetrate the lipid components of the limiting plasma membranes. Lipid-soluble substances with a molecular weight of less than 600 Da readily permeate the bloodbrain barrier by simple diusion. Thus, alcohol, certain steroid hormones such as progesterone, as well as small lipophilic drugs such as codeine, can reach the brain. The lipophilic nature of a naturally occurring substance or drug may be determined by measuring its permeability coecient. This is done by quantifying its distribution between nonpolar and polar phases, such as 1-octanol and water. The permeability coecient varies directly with the ratio of distribution in the nonpolar over the polar solution. As mentioned above, nutrients such as glucose and certain amino acids are able to enter the brain by crossing the bloodbrain barrier. Entry of glucose is expected, since it is poorly stored by the brain, and is required for energy metabolism. Movement of glucose from blood to brain across the barrier is carrier mediated (Figure 2). The process is passive, with glucose moving down its concentration gradient from blood to brain. Carriers on both the luminal and abluminal plasma membranes facilitate its passage into the brain extracellular uid. Several isoforms of
Contributions of Astrocytes to a Well-sealed Blood Brain Barrier
The dierentiation of a specialized bloodbrain barrier is dependent upon the presence of astrocytes. Astrocytes are nonneuronal, multifunctional cells in the brain which apparently secrete a paracrine substance that stimulates the endothelial cells of the bloodbrain barrier to form tight junctions and develop a polar conguration. Normally astrocytes are closely aligned with the bloodbrain barrier, and project cellular extensions (end-feet) that terminate near the endothelium. Thus, they are in an ideal position to inuence its dierentiation. If the endothelial
2
ENCYCLOPEDIA OF LIFE SCIENCES / & 2001 Nature Publishing Group / www.els.net
Blood Brain Barrier
Blood G AA AA Luminal membrane L y+ Gln AA Glu AA G Na+ Glu H+ Tight junction Brain capillary endothelial cell Abluminal AA membrane L Na+ AA y+ A Na+ AA Bo,+ N Glu Na+ AA G G Glu K+ Na+
Na+ AA Na+ AA Brain
Figure 2 Brain capillary endothelial cells forming the blood brain barrier are polarized and possess distinct transport proteins in the luminal and abluminal plasma membranes. This illustration depicts a current model describing some of these transporters. Organic nutrients such as amino acids (AA) and glucose (G) move passively from blood to brain extracellular fluid, with the assistance of carrier systems (i.e. L, y 1 , G) in both plasma membranes. Sodium-dependent amino acid cotransporters positioned at the abluminal membrane (i.e. A, Bo, 1 ) apparently serve to limit the influx of certain amino acids. Transporters for glutamate (Glu) are arranged to remove this neuroexcitatory amino acid from the brain. Together, the transport systems for glutamate and glutamine (Gln, N) in the blood brain barrier may contribute to regulating the presence of these nitrogen-containing amino acids in the brain, and thus participate in balancing brain nitrogen. Finally, the arrangement of sodium transporters (Na 1 /H 1 antiporter, Na channel, Na 1 /K 1 adenosine triphosphatase) in the luminal and abluminal plasma membranes favours net unidirectional blood to brain movement of fluid.
glucose transporters have been identied in a variety of tissues. As indicated above, the facilitative glucose carrier of the bloodbrain barrier is called GLUT-1. Several amino acid transport systems have been identied in the bloodbrain barrier (Figure 2). These are carrier-mediated pathways, and may be classied generally into sodium-independent and sodium-dependent processes. Large neutral amino acids, such as leucine and phenylalanine, are transported from blood to brain by system L (leucine preferring), which is typical of the sodium-independent category. Movement across the barrier is passive, with the amino acids moving down their concentration gradients, and transport is facilitated by L carriers on both plasma membrane domains. Although these carrier proteins have a greater anity for large neutral amino acids, other amino acids may also be transported to varying degrees. Basic amino acids such as arginine, lysine and ornithine are passively transported across the bloodbrain barrier by system y 1 , with these sodium-independent carriers presumably on both the luminal and abluminal membranes. Various sodium-dependent amino acid transporters have been described in the bloodbrain barrier, including systems A, ASC, Bo, 1 , N, and a glutamate carrier. System A has a high anity for small neutral amino acids such as alanine, and preferentially transports N-(methylamino)isobutyric acid (MeAIB), which has become its dening substrate. This carrier protein is characterized by secondary active transport of amino acids from the brain
extracellular uid into the endothelial cells forming the bloodbrain barrier, driven by cotransport of sodium down its electrochemical gradient. For this reason, the transporter functions to reduce entry of amino acids into the brain. Recently it has been shown that the system A transport protein is upregulated by oxoproline, an intracellular metabolite that is probably formed during enhanced blood to brain transport of amino acids. Thus it appears that a negative feedback mechanism is in place that serves to limit brain uptake of certain amino acids, when the blood to brain gradient would otherwise enhance their passive movement across the bloodbrain barrier. Sodium-dependent transport of neutral amino acids by the bloodbrain barrier can be accounted for by other carriers, in addition to system A. A component of sodiumdependent neutral amino acid transport has been observed in isolated rat cerebral capillaries that is not inhibited by MeAIB, presumably occurring at the abluminal membrane of the endothelial cells. This transport has been attributed to system ASC, because of its preference for small neutral amino acids. However, recent studies have challenged the presence of system ASC in the bloodbrain barrier, and have suggested that a carrier typical of system Bo, 1 is present. This is a sodium-dependent transporter positioned at the abluminal membrane, which is characterized by a high anity for neutral amino acids. Furthermore, there is recent evidence for the presence of system N at the abluminal membrane, which has a high anity for the nitrogen-containing amino acid glutamine. Since a facil3
ENCYCLOPEDIA OF LIFE SCIENCES / & 2001 Nature Publishing Group / www.els.net
Blood Brain Barrier
itative carrier for glutamine is also present at the luminal membrane, it appears that the bloodbrain barrier has the capability to transport glutamine from brain to blood, and thus may serve as a means of removing nitrogen from the brain. Conceivably, this could be important in certain pathological disorders (e.g. liver disease) associated with increased levels of nitrogen-containing compounds, including ammonia, in brain extracellular uid. Finally, there appears to be a sodium-dependent amino acid carrier in the abluminal membrane that is capable of transporting glutamate from brain extracellular uid into the endothelium of the bloodbrain barrier. Under normal circumstances, the barrier is largely impermeable to glutamate entering the brain from the blood. This is expected, since glutamate is a common neurotransmitter in the central nervous system, and its inux could alter nerve impulses and brain function. Like glutamine, glutamate may passively cross the luminal membrane of the barrier by a facilitative carrier. However, a facilitative transporter does not appear to be present at the abluminal membrane. This arrangement of carriers is consistent with blood to brain movement of glutamate, and suggests that the bloodbrain barrier may serve to remove glutamate from the brain extracellular uid. In addition to the amino acid transporters mentioned above, there is evidence for systems T, b and X 2 in the bloodbrain barrier. These are low-capacity carriermediated systems that transport thyroid hormones (T3, T4), b amino acids (e.g. taurine) and anionic amino acids (e.g. aspartate) respectively. Furthermore, there are reports describing transport of monocarboxylic acids, amines, purine bases and nucleosides. The bloodbrain barrier appears to be generally impermeable to peptides and proteins, although some exceptions have been described. There are reports that the following peptides may enter the brain by crossing the barrier: enkephalin, thyroid-releasing hormone, d sleepinducing peptide, vasopressin and glutathione. The apparent uptake of several peptides is characterized by saturation kinetics, suggesting the presence of carrier-mediated transport systems. There is evidence that insulin may be transcytosed across the bloodbrain barrier. In addition, much attention has been given recently to the circulating protein transferrin, which appears to cross the blood brain barrier transcytotically. Both insulin and transferrin bind to specic receptor sites located on the luminal plasma membrane. After binding, endocytosis of the substrate occurs, after which the endocytic vesicle moves across the endothelial cell and exocytically releases the substrate at the abluminal membrane. It is currently believed that the bloodbrain barrier serves to regulate extracellular uid homeostasis in the brain. The emerging picture is that the barrier drives net unidirectional movement of electrolytes and water from blood to brain. Thus, uid is secreted into the brain. This is thought to be accomplished by a polar arrangement of
4
transport proteins in the luminal and abluminal plasma membrane domains of the endothelial cells that form the barrier. Furthermore, the processes responsible for uid and electrolyte transport appear to be under the control of peptide hormones released within the brain. Studies suggest that a Na 1 /H 1 antiporter is present in the luminal membrane, along with a nonspecic cationic channel, and a Na 1 /K 1 adenosine triphosphatase is located at the abluminal membrane (Figure 2). Such an arrangement of sodium transporters would allow for net unidirectional transport of uid from blood to brain. Thus, sodium would enter the endothelial cells from the blood, utilizing the transport proteins in the luminal membrane. It would then be actively extruded into the brain extracellular uid by the sodium pump positioned at the abluminal membrane. As net unidirectional sodium transport occurs from blood to brain, water follows passively. It appears that alterations in brain extracellular uid homeostasis may bring about the release of peptide hormones within the brain, which can modulate the rate of net uid transport across the blood brain barrier. Centrally released peptides that have been implicated in this process include atrial natriuretic factor, angiotensin II and vasopressin. Normally, uid secretion and drainage are balanced in the central nervous system, preventing uid accumulation.
Delivering Drugs to the Brain
Drugs may potentially cross the bloodbrain barrier by a variety of mechanisms. These include: simple diusion, carrier-mediated transport and transcytosis. Simple diusion occurs by unassisted movement of solute down its electrochemical gradient, from blood to brain. For a drug to diuse across the bloodbrain barrier, it must either pass between the endothelial cells via a paracellular pathway, or traverse the endothelium by penetrating the respective luminal and abluminal plasma membranes. As discussed above, since the endothelial cells are joined by tight junctions, relatively little paracellular transport occurs, and solutes enter the brain primarily by crossing the limiting plasma membranes. Thus, a hydrophilic drug must be small enough to enter water-lled channels in the membranes to get across by simple diusion. A lipophilic drug, however, could penetrate the lipid components of the membranes and traverse the cell. For this reason, a common strategy for designing drugs to cross the blood brain barrier is to make them more lipophilic. The disadvantages of this approach, however, are that: (1) the specicity of drug delivery may be compromised, since these drugs would likely enter cells throughout the body, and (2) the action of the drug may be aected by altering its chemical composition to make it more lipophilic. An additional strategy that has been used is to perfuse the brain with a hyperosmotic solution, temporarily disrupt-
ENCYCLOPEDIA OF LIFE SCIENCES / & 2001 Nature Publishing Group / www.els.net
Blood Brain Barrier
ing the tight junctions of endothelial cells forming the bloodbrain barrier, and thus allowing for simple diusion of administered drugs through a paracellular pathway into the brain. A second mode of transport across the bloodbrain barrier involves membrane carriers. If a drug is recognized by carrier proteins in both membranes, and the conditions favour blood to brain movement, then passage of this drug across the bloodbrain barrier is carrier mediated. Carriermediated transport is either active or passive, depending on whether transfer occurs against an electrochemical gradient, or not. Theoretically, primary active transport would involve the direct application of energy in the form of adenosine triphosphate to one of the carriers. Secondary active transport would require co- or counter-transport of a solute passing down its electrochemical gradient, which in turn drives movement of the drug against its electrochemical gradient. Passive carrier-mediated transport would involve passage of drugs across the bloodbrain barrier in the direction of an electrochemical gradient, but movement is facilitated by the presence of carriers. Since substances such as glucose and amino acids normally enter the brain by utilizing carriers in the bloodbrain barrier, a possible strategy for drug delivery is to fashion therapeutics that are recognized by these or other transporters. Transcytosis represents a third mechanism by which drugs may be delivered to the brain. For this process, a solute binds to the luminal plasma membrane of the bloodbrain barrier, and is carried across the endothelial cell in an endocytic vesicle. Exocytosis occurs at the abluminal membrane, releasing the solute into the brain extracellular uid. A current strategy utilizing this mechanism is to conjugate a drug to a vehicle solute which is transcytosed by the bloodbrain barrier. Transferrin, which is recognized by a specic receptor on the luminal membrane, has been used in this way. Cationic albumin has also been suggested as a possible vehicle for transcytosis of drugs across the bloodbrain barrier.
allowing certain ones to pass and preventing the passage of others. Small lipophilic molecules (Mr 5 600 Da) such as alcohol or progesterone are able to penetrate the blood brain barrier by permeating the lipid components of the limiting plasma membranes, and diusing across the endothelium. Glucose and certain amino acids are transported by specic carrier proteins present in the membranes. These organic nutrients move passively from blood to brain extracellular uid down their electrochemical gradients, utilizing their respective carriers to facilitate transport. In addition, there is evidence describing transport of monocarboxylic acids, amines, purine bases and nucleosides by the bloodbrain barrier. Fluid and electrolyte transport is mediated by channels and carriers. It is currently believed that net unidirectional uid movement occurs from blood to brain across the bloodbrain barrier. This is accomplished by a polar arrangement of sodium transporters in the respective luminal and abluminal plasma membranes, with water passively following transport of sodium. The process appears to be regulated by hormones produced in the brain. With few exceptions, circulating peptides and proteins generally do not cross the bloodbrain barrier. There is evidence for carrier-mediated transport of enkephalin, thyroid-releasing hormone, d sleep-inducing peptide, vasopressin and glutathione. Furthermore, insulin and transferrin are able to cross by the process of receptormediated transcytosis. When designing systemically administered drugs for the treatment of central nervous system disorders, the molecules must be fashioned to cross the bloodbrain barrier in order to reach their site of action in the brain. This may involve making the molecules lipophilic, or designing them to interact with known transport mechanisms.
Further Reading
Betz AL and Goldstein GW (1986) Specialized properties and solute transport in brain capillaries. Annual Reviews of Physiology 48: 241 250. Davson H, Zlokovic B, Rakic L and Segal MB (1993) An Introduction to the Blood Brain Barrier. Boca Raton, FL: CRC Press. Doczi T (1993) Volume regulation of the brain tissue a survey. Acta Neurochirurgica 121: 18. Drewes LR (1998) Biology of the bloodbrain glucose transporter. In: Pardridge WM (ed.) Introduction to the Blood Brain Barrier, pp. 165 174. Cambridge: Cambridge University Press. Frelin C and Vigne P (1998) Ion channels in endothelial cells. In: Pardridge WM (ed.) Introduction to the Blood Brain Barrier, pp. 214 220. Cambridge: Cambridge University Press. Pardridge WM (1991) Peptide Drug Delivery to the Brain. New York: Raven Press. Peterson DR and Hawkins RA (1998) Isolation and behavior of plasma membrane vesicles made from cerebral capillary endothelial cells. In: Pardridge WM (ed.) Introduction to the Blood Brain Barrier, pp. 62 70. Cambridge: Cambridge University Press.
Summary
The bloodbrain barrier is formed by endothelial cells which line capillaries in the brain. Unlike endothelium elsewhere in the body, these cells possess tight junctions which form cell-to-cell attachments and separate the limiting plasmalemma into luminal (blood facing) and abluminal (brain facing) plasma membrane domains. The junctional complexes display a high electrical resistance, indicating that solute transport across the bloodbrain barrier is predominantly transcellular, rather than paracellular. Thus, for substances to pass from the blood to brain extracellular uid, they must cross both the luminal and abluminal plasma membranes. These membranes are selectively permeable to solutes carried in the blood,
ENCYCLOPEDIA OF LIFE SCIENCES / & 2001 Nature Publishing Group / www.els.net
Blood Brain Barrier
Smith QR and Stoll J (1998) Bloodbrain barrier amino acid transport. In: Pardridge WM (ed.) Introduction to the Blood Brain Barrier, pp. 188197. Cambridge: Cambridge University Press. Strange K (1992) Regulation of solute and water balance and cell volume in the central nervous system. Journal of the American Society of Nephrology 3: 1227.
Tsuji A and Tamai I (1998) Bloodbrain barrier transport of drugs. In: Pardridge WM (ed.) Introduction to the Blood Brain Barrier, pp. 238 247. Cambridge: Cambridge University Press.
ENCYCLOPEDIA OF LIFE SCIENCES / & 2001 Nature Publishing Group / www.els.net
S-ar putea să vă placă și
- Principles of Stem Cell Biology and Cancer: Future Applications and TherapeuticsDe la EverandPrinciples of Stem Cell Biology and Cancer: Future Applications and TherapeuticsÎncă nu există evaluări
- Preclinical PDFDocument36 paginiPreclinical PDFxyzÎncă nu există evaluări
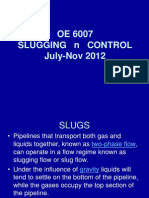
- LectureslugsDocument83 paginiLectureslugsKrishnan ChockalingamÎncă nu există evaluări
- Renal SystemDocument85 paginiRenal SystemFerasKarajehÎncă nu există evaluări
- Animal ModelsDocument21 paginiAnimal ModelsSudarshan UpadhyayÎncă nu există evaluări
- Animal Models in Disease Research: Honours Department of Pathology University of Melbourne Theo MantamadiotisDocument35 paginiAnimal Models in Disease Research: Honours Department of Pathology University of Melbourne Theo MantamadiotisRiv sashÎncă nu există evaluări
- Experiment 4 Blood CultureDocument14 paginiExperiment 4 Blood CulturesarahinaÎncă nu există evaluări
- Hemodynamic Disorders ThrombosisDocument106 paginiHemodynamic Disorders ThrombosisRamez AnaniÎncă nu există evaluări
- Cerebrospinal FluidDocument13 paginiCerebrospinal Fluidsakshi panwarÎncă nu există evaluări
- Basic Immunology 2017 - AmaDocument122 paginiBasic Immunology 2017 - AmaEka RizkyanaÎncă nu există evaluări
- Postgraduate Manual of Pathology 4th Ed. 2021Document87 paginiPostgraduate Manual of Pathology 4th Ed. 2021sindhuja polareddyÎncă nu există evaluări
- Endocrine System Pathology 2009Document195 paginiEndocrine System Pathology 2009SofiaemanginteÎncă nu există evaluări
- Apoptosis and Necrosis: Yodit Getahun, MDDocument37 paginiApoptosis and Necrosis: Yodit Getahun, MDWolderufaelÎncă nu există evaluări
- 3.4 Homeostasis in HumanDocument35 pagini3.4 Homeostasis in HumanIMELDAÎncă nu există evaluări
- DR - Shamim Rima Mbbs - Dmu.Fcgp M.Phil BsmmuDocument46 paginiDR - Shamim Rima Mbbs - Dmu.Fcgp M.Phil Bsmmudr_shamimrÎncă nu există evaluări
- Carbohydrate Storage and Synthesis in Liver and Muscle: GlycogenDocument40 paginiCarbohydrate Storage and Synthesis in Liver and Muscle: GlycogenJay R PlogioÎncă nu există evaluări
- Complement SystemDocument13 paginiComplement SystemKush Shrivastava100% (3)
- Erythropoiesis Lect 3Document18 paginiErythropoiesis Lect 3Pramesh PaudelÎncă nu există evaluări
- Cagayan State University College of Medicine and Surgery SY: 2009-2010Document41 paginiCagayan State University College of Medicine and Surgery SY: 2009-2010ahmad usmanÎncă nu există evaluări
- Saquinavir Sodgganga PDFDocument104 paginiSaquinavir Sodgganga PDFSiva PrasadÎncă nu există evaluări
- Histopathologist and InternetDocument2 paginiHistopathologist and InternetNischita JayarajÎncă nu există evaluări
- Intergration of MetabolismDocument112 paginiIntergration of MetabolismSantino MajokÎncă nu există evaluări
- Pathology of Adrenal Glands.Document41 paginiPathology of Adrenal Glands.Sukma Eka PratiwiÎncă nu există evaluări
- In The Name of GodDocument54 paginiIn The Name of GodrostaminasabÎncă nu există evaluări
- Immunology of Transplant RejectionDocument8 paginiImmunology of Transplant Rejectionxplaind100% (1)
- Cell Communication and Signal TransductionDocument34 paginiCell Communication and Signal TransductionArina SafiraÎncă nu există evaluări
- Second Year: 2.1 Pathophysiolog Y (Theory)Document15 paginiSecond Year: 2.1 Pathophysiolog Y (Theory)Prashanth RajuÎncă nu există evaluări
- Principles of Fluid Management 2015 PDFDocument17 paginiPrinciples of Fluid Management 2015 PDFJorge DíazÎncă nu există evaluări
- Pharmacokinetics of IV InfusionDocument49 paginiPharmacokinetics of IV InfusionsamanÎncă nu există evaluări
- MicropropagationDocument30 paginiMicropropagationBrigitte ReyesÎncă nu există evaluări
- Wound Healing and Factors Affecting Wound Healing: Principles of SurgeryDocument57 paginiWound Healing and Factors Affecting Wound Healing: Principles of SurgeryAmit RamdinÎncă nu există evaluări
- Drug Delivery Through NanohydrogelsDocument11 paginiDrug Delivery Through NanohydrogelsPrabhat BistÎncă nu există evaluări
- Biosensors PowerpointDocument26 paginiBiosensors PowerpointDevansh DurgarajuÎncă nu există evaluări
- II. Subdivisions of PathologyDocument2 paginiII. Subdivisions of PathologySiegÎncă nu există evaluări
- Chapter Two Tissue InjuryDocument38 paginiChapter Two Tissue Injuryapi-19916399Încă nu există evaluări
- Serotonin (5-HT)Document35 paginiSerotonin (5-HT)adeesasaadÎncă nu există evaluări
- Blood ProductDocument89 paginiBlood ProductSam0% (1)
- Plasma EnzymesDocument4 paginiPlasma EnzymesIbrahim ZorobÎncă nu există evaluări
- Corticosteroid PDFDocument21 paginiCorticosteroid PDFAida YuliaÎncă nu există evaluări
- Autocoid PharmacologyDocument29 paginiAutocoid PharmacologyLyadelou Fortu100% (1)
- National Drug Policy 2003Document18 paginiNational Drug Policy 2003Danish SarwarÎncă nu există evaluări
- Euthanasia in Experimental AnimalsDocument22 paginiEuthanasia in Experimental AnimalsParmanand AtalÎncă nu există evaluări
- Upper Gastrointestinal Bleeding (Ugib) : Muhammad Izzat Bin FatasDocument47 paginiUpper Gastrointestinal Bleeding (Ugib) : Muhammad Izzat Bin FatascopperÎncă nu există evaluări
- Physiology of Skin ReceptorsDocument16 paginiPhysiology of Skin ReceptorsJaynier Jayson JayaÎncă nu există evaluări
- Cell SignalingDocument118 paginiCell SignalingHimakiran BabuÎncă nu există evaluări
- ANNEX VII ASEAN GL Claims and Claims Substantiation TMHS V14 13nov14 PDFDocument19 paginiANNEX VII ASEAN GL Claims and Claims Substantiation TMHS V14 13nov14 PDFaquarianchemÎncă nu există evaluări
- Erythropoietin PDFDocument13 paginiErythropoietin PDFZeynep SemenÎncă nu există evaluări
- Cancer of Reproductive SystemDocument42 paginiCancer of Reproductive Systemmaria erika100% (6)
- Acute Coronary Syndrome: Aminah DalimuntheDocument48 paginiAcute Coronary Syndrome: Aminah Dalimunthesintesis obatÎncă nu există evaluări
- Laboratory Medicine Practice Guidelines: Laboratory Analysis and Application of Pharmacogenetics To Clinical PracticeDocument54 paginiLaboratory Medicine Practice Guidelines: Laboratory Analysis and Application of Pharmacogenetics To Clinical PracticeAde NasutionÎncă nu există evaluări
- Hormonal Control of Calcium and Phosphate MetabolismDocument50 paginiHormonal Control of Calcium and Phosphate MetabolismhamidÎncă nu există evaluări
- Stem Cells, Cell Lineages and SourcesDocument48 paginiStem Cells, Cell Lineages and SourcesChris PenielÎncă nu există evaluări
- Lecture - 1 Hematological StainingDocument20 paginiLecture - 1 Hematological StainingOjambo FlaviaÎncă nu există evaluări
- Molecular Carcinogenesis Endometrium PDFDocument7 paginiMolecular Carcinogenesis Endometrium PDFMelati HasnailÎncă nu există evaluări
- Format of Animal Development Practical Report:: Text Book Berbahasa Indonesia Atau Bahasa InggrisDocument14 paginiFormat of Animal Development Practical Report:: Text Book Berbahasa Indonesia Atau Bahasa InggrisSafira Dwi OktavianiÎncă nu există evaluări
- BMJ - GerdDocument43 paginiBMJ - Gerdwalit ukhri mukrinin0% (1)
- Lagendroff'sDocument1 paginăLagendroff'sArun DavesarÎncă nu există evaluări
- Imuune Thrombocytopenia (Itp)Document34 paginiImuune Thrombocytopenia (Itp)Roshandiep GillÎncă nu există evaluări
- Plasma Exchange Vs IVIGDocument2 paginiPlasma Exchange Vs IVIGclaudiaÎncă nu există evaluări
- Surface Tension Impact On Pharma ProductsDocument4 paginiSurface Tension Impact On Pharma ProductsOmar Alta'amerehÎncă nu există evaluări
- Evolution of Ecosystems - Terrestrial PDFDocument4 paginiEvolution of Ecosystems - Terrestrial PDFmanoj_rkl_07Încă nu există evaluări
- Ca Binding Proteins A0001347-001-000 PDFDocument8 paginiCa Binding Proteins A0001347-001-000 PDFmanoj_rkl_07Încă nu există evaluări
- 2,4-Thiazolidinedione As Antimicrobial and Cytotoxic AgentsDocument10 pagini2,4-Thiazolidinedione As Antimicrobial and Cytotoxic Agentsmanoj_rkl_07Încă nu există evaluări
- Evolution of Genome Organizn1699-001-000 PDFDocument5 paginiEvolution of Genome Organizn1699-001-000 PDFmanoj_rkl_07Încă nu există evaluări
- Ephrins: Ru Diger KleinDocument6 paginiEphrins: Ru Diger Kleinmanoj_rkl_07Încă nu există evaluări
- BMP Antags &nural Inducna0000805-001-000 PDFDocument5 paginiBMP Antags &nural Inducna0000805-001-000 PDFmanoj_rkl_07Încă nu există evaluări
- Evolution of Development A0001661-001-000 PDFDocument4 paginiEvolution of Development A0001661-001-000 PDFmanoj_rkl_07Încă nu există evaluări
- Calibration of A Transillumanator For UV Fixation of DNA To PDFDocument2 paginiCalibration of A Transillumanator For UV Fixation of DNA To PDFmanoj_rkl_07Încă nu există evaluări
- Heavy Metal Adaptation PDFDocument4 paginiHeavy Metal Adaptation PDFmanoj_rkl_07Încă nu există evaluări
- Electron Carriers PDFDocument8 paginiElectron Carriers PDFmanoj_rkl_07100% (1)
- Cyanogenesis in Higher Plant and InsectsDocument3 paginiCyanogenesis in Higher Plant and Insectsmanoj_rkl_07Încă nu există evaluări
- Plant Macro-And Micronutrient MineralsDocument5 paginiPlant Macro-And Micronutrient Mineralsmanoj_rkl_07Încă nu există evaluări
- Electroporation: Jac A NickoloffDocument3 paginiElectroporation: Jac A Nickoloffmanoj_rkl_07Încă nu există evaluări
- DNA Damage: Paul W DoetschDocument7 paginiDNA Damage: Paul W Doetschmanoj_rkl_07Încă nu există evaluări
- DNA Repair by Reversal of Damage PDFDocument8 paginiDNA Repair by Reversal of Damage PDFmanoj_rkl_07100% (1)
- Flocyt Anal Nstem Cel in DevDocument11 paginiFlocyt Anal Nstem Cel in Devmanoj_rkl_07Încă nu există evaluări
- Forward-Cristopher Reeve PDFDocument1 paginăForward-Cristopher Reeve PDFmanoj_rkl_07Încă nu există evaluări
- Genetic Code Introduction PDFDocument10 paginiGenetic Code Introduction PDFmanoj_rkl_07Încă nu există evaluări
- FGF1Document9 paginiFGF1manoj_rkl_07Încă nu există evaluări
- Closteroviridae: Historical PerspectiveDocument6 paginiClosteroviridae: Historical Perspectivemanoj_rkl_07Încă nu există evaluări
- Immunologival Tolerance Therpeutic Induction PDFDocument6 paginiImmunologival Tolerance Therpeutic Induction PDFmanoj_rkl_07Încă nu există evaluări
- Phyllosphere PDFDocument8 paginiPhyllosphere PDFmanoj_rkl_07Încă nu există evaluări
- Dideoxy Sequencing of DNA PDFDocument16 paginiDideoxy Sequencing of DNA PDFmanoj_rkl_07Încă nu există evaluări
- Dideoxy Sequencing of DNA PDFDocument16 paginiDideoxy Sequencing of DNA PDFmanoj_rkl_07Încă nu există evaluări
- Root Nodules (Rhizobium Legumes) PDFDocument2 paginiRoot Nodules (Rhizobium Legumes) PDFmanoj_rkl_07Încă nu există evaluări
- Calibration of A Transillumanator For UV Fixation of DNA To PDFDocument2 paginiCalibration of A Transillumanator For UV Fixation of DNA To PDFmanoj_rkl_07Încă nu există evaluări
- Capillary Blotting of RNA and DNA Gels PDFDocument3 paginiCapillary Blotting of RNA and DNA Gels PDFmanoj_rkl_07Încă nu există evaluări
- Heavy Metal Adaptation PDFDocument4 paginiHeavy Metal Adaptation PDFmanoj_rkl_07Încă nu există evaluări
- Gertrude Belle Elion PDFDocument1 paginăGertrude Belle Elion PDFmanoj_rkl_07Încă nu există evaluări
- Terpenoids Lower PDFDocument7 paginiTerpenoids Lower PDFmanoj_rkl_07Încă nu există evaluări
- Chloride (CL) : Share ThisDocument5 paginiChloride (CL) : Share ThisAnonymous Z7adG1yHÎncă nu există evaluări
- Lesson 9: Endocrine System: Prepared by Arianne V. JulianDocument34 paginiLesson 9: Endocrine System: Prepared by Arianne V. JulianGisselleÎncă nu există evaluări
- Documentation ExamplesDocument5 paginiDocumentation ExamplesErika HarveryÎncă nu există evaluări
- Meat Processing TechnologyDocument52 paginiMeat Processing TechnologyAnna FloraÎncă nu există evaluări
- Advanced Trauma Life SupportDocument8 paginiAdvanced Trauma Life SupportAbouzr Mohammed ElsaidÎncă nu există evaluări
- "The Black Cat" by Edgar Allan Poe Vocabulary & QuestionsDocument5 pagini"The Black Cat" by Edgar Allan Poe Vocabulary & Questionsapi-329592091Încă nu există evaluări
- Amniocentesis HindiDocument6 paginiAmniocentesis HindiRohit KumarÎncă nu există evaluări
- Diagnostic Exam Nepbe All GradesDocument24 paginiDiagnostic Exam Nepbe All GradeselprofeleoÎncă nu există evaluări
- Pest Control Services DelhiDocument3 paginiPest Control Services DelhiShikha ChoutalaÎncă nu există evaluări
- Structural Organisation in Animals - IIDocument70 paginiStructural Organisation in Animals - IIMay HarukaÎncă nu există evaluări
- Resume 6 2015Document2 paginiResume 6 2015api-290445636Încă nu există evaluări
- Grammar Workbook Gr. 4 - HomeschoolDocument195 paginiGrammar Workbook Gr. 4 - HomeschoolJessica Pollard Adams100% (2)
- Pertanyaan Yang Harus DijawabDocument6 paginiPertanyaan Yang Harus DijawabMuhammad RhezaÎncă nu există evaluări
- Bioquell - BDS-3-bioefficacy-v5.0 PDFDocument12 paginiBioquell - BDS-3-bioefficacy-v5.0 PDFAdamÎncă nu există evaluări
- Allergy BDS Seminar ReportDocument21 paginiAllergy BDS Seminar ReportErSandeepVermaÎncă nu există evaluări
- Why No Garlic and OnionDocument2 paginiWhy No Garlic and Onionapi-3716330100% (1)
- V. Diagnostic ExaminationDocument3 paginiV. Diagnostic ExaminationArlene MacatangayÎncă nu există evaluări
- Root Word Meanings Origin: For More Examples, VisitDocument34 paginiRoot Word Meanings Origin: For More Examples, VisitEsteban Marcelo Totoy BarreraÎncă nu există evaluări
- 0 Bxzs HMZydz R5 C Ed OSl B2 TK 9 LWUkDocument10 pagini0 Bxzs HMZydz R5 C Ed OSl B2 TK 9 LWUkTricia LlorinÎncă nu există evaluări
- OB Evals 1Document28 paginiOB Evals 1Zelle Pamplona RamosÎncă nu există evaluări
- Mengenal Aspergillosis, Infeksi Jamur Genus Aspergillus Uswatun HasanahDocument10 paginiMengenal Aspergillosis, Infeksi Jamur Genus Aspergillus Uswatun HasanahTiza JulyanÎncă nu există evaluări
- BronopolDocument3 paginiBronopolImut MainahÎncă nu există evaluări
- Dengue 1Document6 paginiDengue 1Johannah Ruth BacolodÎncă nu există evaluări
- Palikaras2015 PDFDocument17 paginiPalikaras2015 PDFDanilo RosaÎncă nu există evaluări
- Periodontology Question BankDocument44 paginiPeriodontology Question BankVanshika Jain100% (6)
- DR Fares ElKhayat - Avian BiologyDocument16 paginiDR Fares ElKhayat - Avian BiologyfareselkhayatÎncă nu există evaluări
- Cat DiseasesDocument1 paginăCat DiseasesEsen KayaÎncă nu există evaluări
- The Cubonomicon v1Document43 paginiThe Cubonomicon v1javandarÎncă nu există evaluări
- Bsc2086 Ass. 1 SummerDocument51 paginiBsc2086 Ass. 1 SummerGeico88Încă nu există evaluări
- Hematology 1 Laboratory SheetDocument3 paginiHematology 1 Laboratory SheetNatsuki MiyajiÎncă nu există evaluări
- The Molecule of More: How a Single Chemical in Your Brain Drives Love, Sex, and Creativity--and Will Determine the Fate of the Human RaceDe la EverandThe Molecule of More: How a Single Chemical in Your Brain Drives Love, Sex, and Creativity--and Will Determine the Fate of the Human RaceEvaluare: 4.5 din 5 stele4.5/5 (517)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisDe la EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisEvaluare: 3.5 din 5 stele3.5/5 (2)
- Why We Die: The New Science of Aging and the Quest for ImmortalityDe la EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityEvaluare: 4 din 5 stele4/5 (5)
- A Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsDe la EverandA Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsEvaluare: 4.5 din 5 stele4.5/5 (6)
- 10% Human: How Your Body's Microbes Hold the Key to Health and HappinessDe la Everand10% Human: How Your Body's Microbes Hold the Key to Health and HappinessEvaluare: 4 din 5 stele4/5 (33)
- Gut: the new and revised Sunday Times bestsellerDe la EverandGut: the new and revised Sunday Times bestsellerEvaluare: 4 din 5 stele4/5 (393)
- Undeniable: How Biology Confirms Our Intuition That Life Is DesignedDe la EverandUndeniable: How Biology Confirms Our Intuition That Life Is DesignedEvaluare: 4 din 5 stele4/5 (11)
- Masterminds: Genius, DNA, and the Quest to Rewrite LifeDe la EverandMasterminds: Genius, DNA, and the Quest to Rewrite LifeÎncă nu există evaluări
- Gut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)De la EverandGut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)Evaluare: 4 din 5 stele4/5 (411)
- Tales from Both Sides of the Brain: A Life in NeuroscienceDe la EverandTales from Both Sides of the Brain: A Life in NeuroscienceEvaluare: 3 din 5 stele3/5 (18)
- The Ancestor's Tale: A Pilgrimage to the Dawn of EvolutionDe la EverandThe Ancestor's Tale: A Pilgrimage to the Dawn of EvolutionEvaluare: 4 din 5 stele4/5 (812)
- All That Remains: A Renowned Forensic Scientist on Death, Mortality, and Solving CrimesDe la EverandAll That Remains: A Renowned Forensic Scientist on Death, Mortality, and Solving CrimesEvaluare: 4.5 din 5 stele4.5/5 (397)
- Buddha's Brain: The Practical Neuroscience of Happiness, Love & WisdomDe la EverandBuddha's Brain: The Practical Neuroscience of Happiness, Love & WisdomEvaluare: 4 din 5 stele4/5 (216)
- Return of the God Hypothesis: Three Scientific Discoveries That Reveal the Mind Behind the UniverseDe la EverandReturn of the God Hypothesis: Three Scientific Discoveries That Reveal the Mind Behind the UniverseEvaluare: 4.5 din 5 stele4.5/5 (52)
- The Other Side of Normal: How Biology Is Providing the Clues to Unlock the Secrets of Normal and Abnormal BehaviorDe la EverandThe Other Side of Normal: How Biology Is Providing the Clues to Unlock the Secrets of Normal and Abnormal BehaviorÎncă nu există evaluări
- Who's in Charge?: Free Will and the Science of the BrainDe la EverandWho's in Charge?: Free Will and the Science of the BrainEvaluare: 4 din 5 stele4/5 (65)
- A Series of Fortunate Events: Chance and the Making of the Planet, Life, and YouDe la EverandA Series of Fortunate Events: Chance and the Making of the Planet, Life, and YouEvaluare: 4.5 din 5 stele4.5/5 (62)
- Fast Asleep: Improve Brain Function, Lose Weight, Boost Your Mood, Reduce Stress, and Become a Better SleeperDe la EverandFast Asleep: Improve Brain Function, Lose Weight, Boost Your Mood, Reduce Stress, and Become a Better SleeperEvaluare: 4.5 din 5 stele4.5/5 (15)
- Seven and a Half Lessons About the BrainDe la EverandSeven and a Half Lessons About the BrainEvaluare: 4 din 5 stele4/5 (110)
- Why We Sleep: Unlocking the Power of Sleep and DreamsDe la EverandWhy We Sleep: Unlocking the Power of Sleep and DreamsEvaluare: 4.5 din 5 stele4.5/5 (2083)
- Lymph & Longevity: The Untapped Secret to HealthDe la EverandLymph & Longevity: The Untapped Secret to HealthEvaluare: 4.5 din 5 stele4.5/5 (13)
- Human: The Science Behind What Makes Your Brain UniqueDe la EverandHuman: The Science Behind What Makes Your Brain UniqueEvaluare: 3.5 din 5 stele3.5/5 (38)
- Good Without God: What a Billion Nonreligious People Do BelieveDe la EverandGood Without God: What a Billion Nonreligious People Do BelieveEvaluare: 4 din 5 stele4/5 (66)
- The Rise and Fall of the Dinosaurs: A New History of a Lost WorldDe la EverandThe Rise and Fall of the Dinosaurs: A New History of a Lost WorldEvaluare: 4 din 5 stele4/5 (595)
- Moral Tribes: Emotion, Reason, and the Gap Between Us and ThemDe la EverandMoral Tribes: Emotion, Reason, and the Gap Between Us and ThemEvaluare: 4.5 din 5 stele4.5/5 (115)
- The Consciousness Instinct: Unraveling the Mystery of How the Brain Makes the MindDe la EverandThe Consciousness Instinct: Unraveling the Mystery of How the Brain Makes the MindEvaluare: 4.5 din 5 stele4.5/5 (93)