Documente Academic
Documente Profesional
Documente Cultură
6 PDF
Încărcat de
Kerin ArdyTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
6 PDF
Încărcat de
Kerin ArdyDrepturi de autor:
Formate disponibile
Mycopathologia (2010) 170:143154 DOI 10.
1007/s11046-010-9312-7
Favus of the Scalp: An Overview and Update
Macit Ilkit
Received: 23 November 2009 / Accepted: 5 April 2010 / Published online: 22 April 2010 Springer Science+Business Media B.V. 2010
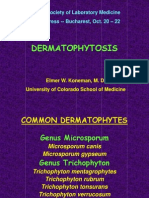
Abstract Tinea capitis favosa, a chronic inammatory dermatophyte infection of the scalp, affects over 90% of patients with anthropophilic Trichophyton schoenleinii. T. violaceum, T. verrucosum, zoophilic T. mentagrophytes (referred to as var. quinckeanum), Microsporum canis, and geophilic M. gypseum have also been recovered from favic lesions. Favus is typically a childhood disease, yet adult cases are not uncommon. Interestingly, favus is less contagious than other dermatophytoses, although intrafamilial infections are reported and have been widely discussed in the literature. Clinical presentation of T. schoenleinii infections is variable: this fungus can be isolated from tinea capitis lesions that appear as gray patches, but symptom-free colonization of the scalp also occurs. Although in the past T. schoenleinii was the dominant fungus recovered from dermatophytic scalp lesions, worldwide the incidence has decreased except in China, Nigeria, and Iran. Favus of the glabrous skin and nails are reported less frequently than favus of the scalp. This review discusses the clinical features of favus, as well as the etiological agents, global epidemiology, laboratory diagnosis, and a short history of medical mycology.
Keywords Anthropophilic Dermatophyte Favus Tinea capitis Trichophyton schoenleinii Abbreviation TCS Tinea capitis supercialis Introduction Scalp Ringworm: A Historical Perspective The earliest written records contain numerous descriptions of scalp ringworm. There is a reference in the Torah (in Leviticus 13) to Tzaraat, which may mean scalp disease, and De Medica, penned by Aulus Cornelius Celsus in the rst century AD, refers to porrigo, possibly meaning favus [1]. The ancient Greeks used the term achor-scap to describe favus lesions; the equivalent in Latin is Tinea, a term introduced by Cassius Felix [2]. In spite of the perceived mysterious nature of illnesses in the seventeenth to nineteenth centuries, several clear illustrations of ringworm or favus were produced. For example, in De vier Rengtenvan het leprozenhuis te Amsterdam by Ferdinand Bol in 1649, the artist depicts two young boys who probably have Trichophyton schoenleinii infections on their scalps. Both children are victims of the disgurement caused by their illness, which has been mistaken for leprosy since Biblical times [1]. At the beginning of the nineteenth century, Alibert [3] used the term favus to describe the honey-like exudate in some scalp infections.
M. Ilkit (&) Faculty of Medicine, Division of Mycology, Department of Microbiology, University of Cukurova, 01330 Adana, Turkey e-mail: milkit@cu.edu.tr
123
144
Mycopathologia (2010) 170:143154
Discovery of Achorion (Trichophyton) schoenleinii Medical mycology is the study of fungi related to human infections. Historically, this eld was launched by the discovery of the fungal etiology of favus (porrigo lupinosa). Three European physicians in the mid-nineteenth century, Johann Lucas Schoenlein (17901864), Robert Remak (18151865), and David Gruby (18101898), were prominent gures in the early years of medical mycology [4, 5]. In 1835, Remak rst observed peculiar microscopic structures that looked like rods and buds in crusts from favic lesions. He never published his observations, but permitted the observations to be cited in a doctoral dissertation by Xavier Hube in 1837 [4, 5]. Remak subsequently became an assistant to Schoenlein, and later claimed that he did not at rst recognize the structures he saw as fungal structures. Instead, he credited his recognition to his mentor Schoenlein, who described the fungal etiology in 1839. In 1842, Remak successfully infected his own arm with the fungus, establishing the causation between the fungal infection and the disease symptoms. Later, in 1945, Remak established denitively that the etiologic agent of favus was infectious, cultured the fungus on apple slices, and named the fungus as Achorion schoenleinii in honor of his mentors initial discovery [47]. Unaware of the observations of Remak and Schoenlein, Dr. David Gruby, who is considered the founder of medical mycology, published a series of papers that described the clinical and microscopic features of the causal agent of favus in accurate detail. Gruby is thus credited with establishing the contagious nature of the disease [4, 5, 7]. Signs and Symptoms Tinea Capitis Favosa Favus or tinea favosa is a chronic inammatory dermatophyte infection of the scalp and, less commonly, of the glabrous skin and nails [8]. It has an insidious course, usually lacking an acute phase, and often the patient does not feel any need to consult a physician [9]. The classic favus lesion is the scutulum, a concave, cup-shaped yellow crust on the scalp and glabrous skin that is associated with severe
alopecia [4, 10]. These keratotic crusts contain fungal hyphae and can be highly infectious [11]. The scutula form dense plaques, each composed of hyphae, neutrophils, and epidermis; secondary bacterial infections often occur in the plaques [10, 12]. The scutulum develops in a hair follicle, with the hair shaft in the center of the raised lesion [12]. The scutula gradually increase in size, and adjacent scutula tend to form conuent masses of crusts [11]. Hair is able to grow, and long hairs are observed frequently in the affected areas [8]. Of the infected individuals with favus, 95% have overt clinical symptoms, e.g., scutula, pale hairs, atrophy, and scarring [13]. Matted hair, tissue debris, and scutula (sometimes called godets) may be present, along with serous exudate, secondary bacterial involvement, pus, and general lth. The scalp is characterized by an unpleasant cheesy or mousy odor [10, 12]. Aksungur [9] reported the incidence of id reaction in 80 tinea capitis supercialis (TCS) cases, 130 kerion celsi cases, and 170 favus cases as 2 (2.5%), 18 (13.8%), and 3 (1.8%), respectively. In one study, the incidence of adenopathy in favus cases was reported to be much higher (43.2%) than the id reaction (5.8%) [14]. In another investigation, the mousy odor was reported in 11.9% of favus cases [13]. Antibodies to causative fungi have been observed in the sera of patients by charcoal agglutination and an immunodiffusion assay; however, the role of these antibodies is not clear [15]. In addition to the typical scutular form of favus, atypical tinea favosa makes up about 5% of the cases. Pityroides, psoriasiform, follicular, and impetiginous forms have been observed both on scalps and on glabrous skin [8, 13, 14]. Both kerion celsi and favus can cause permanent alopecia with scarring, a chronic disguring infection [7, 8]. When scarring is present, the differential diagnosis includes lupus erythematosus, lichen planoplaris, pseudopalade, and radiation dermatitis [12]. Clinical Stages Favus can be classied into three main stages according to infection severity. 1. First stage: There is only erythema of the scalp in this stage, primarily around follicles. The hairs are not loose or broken.
123
Mycopathologia (2010) 170:143154
145
2.
3.
Second stage: Scutula formation can be observed in this stage, along with the beginning of hair loss. Third stage: In the most severe stage, large areas of the scalp are involved, with at least one-third of the scalp affected; there is extensive hair loss, atrophy, and scarring. Formation of new scutula at the periphery of plaques is common [8].
Age and Sex Favus can be acquired during childhood or adolescence and typically persists into adulthood [7, 8, 16]. Unlike TCS, there is no tendency for the infection to resolve at puberty [12]. The incidence rate is higher in boys and in children 610 years of age [14]. However, infections have been detected in individuals as young as 6 weeks [17] and as old as 83 years [18]. Ural et al. [14] observed that 12 of 241 (5%) cases of favus were in postpubescent individuals; all infections had started before puberty. Two other studies reviewed adult cases of tinea capitis and reported that only 5.7% [19] and 8.9% [20] of the cases involved T. schoenleinii. Of all forms of tinea capitis, favus has the longest duration, with an average duration of about 5 years [9]. The reported duration is wide, ranging from 10 days to 59 years [9, 13, 14]. Thus, the infection can last the entire lifetime of the patient [12]. Aksungur [9] reported the male/female ratio to be 1.3/1. There is no evidence that the infection disproportionately affects any particular ethnic group [8]. Glabrous Skin Infections At most, 7% of tinea favosa cases are favus of the glabrous skin and nails [14]. On glabrous skin, favus is papulovesicular and there are papulosquamous eruptions in which typical scutula may be evident [12, 14]. The cup-shaped crusts may be very numerous and resemble a range of volcanoes. The skin may atrophy in affected areas, which is not observed for typical tinea corporis [12]. Krunic et al. [21] reviewed rare cases of favic invasion of the scalp and glabrous skin caused by M. audouinii and M. gypseum, with a focus on favus of the scrotum. One recent study reported scutular tinea of the scrotum due to M. gypseum [22]. Interestingly, T. schoenleinii was isolated in 0.4% [23]
Fig. 1 Tinea favosa of the scalp with yellowish-white scutula of 20-year-old patient (Courtesy of Prof Dr H. R. Memisoglu)
and 0.8% [24] cases of tinea pedis. In addition, Romano et al. [25] reviewed 207 cases of tinea incognito; no strains of T. schoenleinii were recovered (Fig. 1). Onychomycosis Favosa Like tinea unguium, tinea favosa resembles other forms of onychomycosis [12, 16]. Favus of the ngernails has been described in some individuals who accidentally infected themselves while epilating the infected scalp of patient [16]. Nail involvement was observed in 4 of 170 (2.4%) cases of favus; tinea corporis was observed in two of the four cases. This is very interesting considering that auto-inoculation is very rare in cases of T. schoenleinii infection [9]. In one study, 11 of the 13 subjects diagnosed with onychomycoses favosa had the infection only in their ngernails, whereas two had deformities and discoloration on their both ngernails and toenails [13]. In some other studies, it was reported that only 1.6% of dermatophytes isolated from nails were T. schoenleinii [23, 26]. Favus Generalisatus Generalized favus of the scalp and glabrous skin were quite common in European countries during the 19th and early twentieth centuries. With the vast improvements in hygienic standards and in health services, cases of favus were recorded mainly in communities in poor and developing areas [27]. Dostrovsky et al. [27] observed favus generalisatus in only 1 of 806 (0.1%) cases of tinea favosa.
123
146
Mycopathologia (2010) 170:143154
Systemic Infections While favus is a disease of the cutaneous tissues, in rare instances the mucous membranes may also become involved [28]. Kundrat [29] reported a case of generalized favus in a patient who subsequently died from a gastro-intestinal disease (gastro-enteritis favosa). At the autopsy, the favus fungus was present in the esophagus, stomach, and intestines. Rarely, T. schoenleinii can cause fungal keratitis, which may be associated with progressive keratolysis and perforation, scleral extension, and endophtalmitis [30]. Etiology Trichophyton schoenleinii is the most frequently identied causative organism in cases of favus [5, 9, 13, 14], although a few cases have been attributed to T. violaceum [9, 14, 3133], T. verrucosum [14, 31], zoophilic T. mentagrophytes (referred to as var. quinckeanum) [34, 35], M. canis [21, 31], and geophilic M. gypseum [12]. Simultaneous occurrence of T. schoenleinii and either T. violaceum [9, 36] or T. verrucosum [14] on the scalp has also been reported. T. schoenleinii has been recovered from a scalp carrier case [37]. Aksungur [9] reported that T. violaceum infections can last for long periods without any evidence of inammation, and that such infections can change to a kerion type of infection. The course probably depends on host resistance or on a change in fungal virulence, a hypothesis that has been conrmed by other studies [14, 32]. Zoophilic T. mentagrophytes (referred to as var. quinckeanum), the causative agent of mouse favus, also occurs as an infectious fungus in humans. This fungus produces acute, vesicular, and circinate lesions within a few days of infection [38]; it also mimics kerion celsi in that it causes inamed, scaly lesions [34, 35]. In humans, hair infections are rare, and the scutula observed in murine infections do not occur [38]. Source of Infection Transmission Patterns TCS is generally transmitted indirectly, i.e., via loose strands of hair and desquamated epithelial cells rather
than through direct contact. Shared barbershop instruments, hairbrushes, combs, and hats are common methods for disseminating TCS-associated dermatophytes [39]. In certain instances, the disease is transmitted from one child to another, but it is transmitted much less readily than more common varieties of fungi such as Trichophyton, Microsporum, and Epidermophyton [28, 40]. T. schoenleinii is an anthropophilic dermatophyte that has been cultured from the infected hairs, caps, and scarves of symptomatic patients, suggesting that human-to-human contact is the key route of transmission [9, 41]. Infections due to anthropophilic T. violaceum and T. schoenleinii can be perpetuated within families either through a low-grade infections of the scalp or by asymptomatic carriers [17]. Guirges [42] indicated that T. schoenleinii are viable in epilated favic hairs up to 54 months despite the extreme uctuations of temperature in the summer and winter months. Inman [43] described a case of scalp favus due to T. schoenleinii in an inmate at an institution for the mentally disabled that housed between 150 and 160 patients. For 17 years, there were no contact cases of favus in the other inmates, although there is strong evidence that the patient suffered from scalp favus during this period. Two outbreaks of contact cases (glabrous skin only) occurred in the 18th year: T. schoenleinii was isolated 1 of 6 patients and 2 of 12 patients. Family Patterns Transmission of favus probably requires long-term association and exposure: casual contacts are not usually infected [12]. Favus often persists in the same dwellings for generations [17, 40]. Hence, dwellings in which favus-infected individuals live should be thoroughly disinfected [40]. Gupta et al. [44] tested commercial chemical disinfectants including chlorine, phenol, sodium dodecyl sulfate, and several quaternary ammonium salts against T. mentagrophytes, T. raubitschekii, and T. tonsurans. The authors noted that chlorine (1%) exhibited the strongest fungicidal action against Trichophyton inoculum and can be classied as high level disinfectant for dermatophytes. In one study, 98 of 241 (40.7%) cases of favus had a history of intrafamilial infection [14]. Aksungur [9]
123
Mycopathologia (2010) 170:143154
147
observed family incidence in 42 of 170 (24.7%) cases in which the cause was T. schoenleinii: two infections were found in mothers and the other 40 in siblings. The reported family incidence for another anthropophilic T. violaceum was 12.5%, and for the zoophilic dermatophytes M. canis and T. verrucosum the family incidence was 7.4 and 4.3%, respectively. Carslaw [17] reported 39 cases of favus of the scalp among 13 families. It appeared that the infection was passed from the mother to the newborn child rather than from child to child. In addition, it seemed that when a child escapes infection in infancy, the risk of acquiring infection in later life was minimal. There were no cases in which the father of an infected family was infected. Endothrix Favosa When the hair is invaded by dermatophytes, the infections are classied as endothrix, ectothrix, or favus (endothrix favosa) [10]. The production of large numbers of arthroconidia, whether inside the hair shaft (endothrix) or outside it (ectothrix), contributes to the spread [7, 45, 46]. Endothrix infections (e.g., by T. tonsurans) are more likely to result in outbreaks among family members or intimate friends [17, 40, 45, 47, 48]. Small-spore ectothrix infections (e.g., by M. audouinii) have the potential to spread rapidly and often cause epidemics in schools and orphanages [7, 45, 46]. Notably, the specic type of hair invasion in favus contributes to the chronic course of favus. The favic infections resulting in long hyphae inside hair reduce contagiousness via direct contact among close family members [46]. Laboratory Diagnosis Direct Microscopic Examination (DME) DME of infected hairs in 10% potassium hydroxide (KOH) can be used to observe an endothrix infection [8]. Favus is characterized by the production of hyphae, which grow in parallel to the long axis of the hair shaft. When infected hairs are mounted on slides with KOH and subjected to DME, the hyphae can be seen lling with bubbles of air as a result of autolysis of the hyphae. This phenomenon is the basis of the term favus, which is derived from the Latin for
honeycomb [10]. In addition, one can observe septated hyphae with a bamboo appearance; arthrospores, which are very rare with an irregular size and shape; and fat droplets [10, 12]. Fungal Culture: Trichophyton schoenleinii (Lebert 1845, Langeron and Milochevitch 1930) T. schoenleinii can be cultured on Sabouraud glucose agar: the colonies are slow growing, dense and waxy or slightly downy, convoluted (often splitting the agar), white to creamy in color on surface, and white to pale yellow on the reverse. Microscopic examination of cultures reveals irregular septate hyphae that form characteristic chandelier (antler-like) structures, the tips of which are often swollen into a nail-head shape, as well as some chlamydoconidia [49]. Only rudimentary macroconidia have been described for T. schoenleinii. However, when cultures are prepared using inocula preincubated with the c globulin fraction of rabbit antiserum plus guinea-pig complement, T. schoenleinii produces young and fully developed macroconidia as well as many microconidia [50]. The fungus grows at 37C; when grown of BCP-milk solids-glucose agar at 25C, the agar changes color to purple within 710 days. The cultured fungus may be positive or negative for urease activity, and it does not perforate hair [49]. T. schoenleinii is most likely to be confused with T. verrucosum. However, the latter species grows poorly on vitamin-free casamino acids agar (Trichophyton agar #1), and growth is stimulated by thiamine (Trichophyton agar #2) and inositol (Trichophyton agar #3) or both (Trichophyton agar #4) [49]. The phenotype of T. schoenleinii is also close to M. ferrugineum when grown on routine media [41]. Woods Light Examination Under Woods light examination, T. schoenleinii uoresces a faint blue color. One study reported that in all 241 cases of favus, the infected hairs uoresced under Woods light [14]. In addition, at least 4 uorescent compounds have been extracted from human hair infected with T. schoenleinii. Two of these uorescent compounds have absorption spectra that are very similar to derivatives of xanthurenic acid. It is well established that xanthurenic acid and
123
148
Mycopathologia (2010) 170:143154
conjugates derived from it are excreted in increased amounts during pyridoxine deciency [51]. Taxonomy T. schoenleinii was classied in the Arthroderma simii group along with T. simii and zoophilic T. mentagrophytes (referred to as var. quinckeanum) [52]. It has been speculated that T. schoenleinii evolved from related species that infected camels, which live in desert-like environments [53]. However, T. schoenleinii has a very limited animal host range (i.e., only humans) and may have evolved recently by a genetic bottleneck; this would explain genetic homogeneity among T. schoenleinii isolates. Probst et al. [54] have shown that camel-associated isolates of T. mentagrophytes (neotype strain CBS 318.56), previously classied as T. langeronii (dromedaries in Saudi Arabia) and T. sarkisovii (Bactrian camels in Kazakhstan), form favic chandeliers and have a genetic makeup that is very similar to T. schoenleinii. This report conrmed the close relationship of these species. This hypothesis was also conrmed by Deng et al. [41] who recovered T. schoenleinii as a predominant pathogen in Xinjiang, a region of western China that borders Kazakhstan where Bactrian camels are widespread. This may explain the close phylogenetic relatedness of T. schoenleinii and T. mentagrophytes and suggests a host jump from camels to humans [52]. Histopathology In favus of the scalp, mycelium is present in the horny layer of the scalp, within and around the hairs, and in the scutulum. The periphery of infected lesions is composed of well-preserved hyphae, while dead and degenerating mycelium and granular debris are found in the center. The scutulum rests on atrophic epidermis. Inammation with round-cell inltrate is seen in the adjacent dermis. The horny layer of the skin often extends over the edge of the scutulum. T. schoenleinii; the secretion of proteolytic enzymes, including collagenase and elastase, may account for some of the bizarre pathology seen in favus [12]. Affected hair follicles tend to atrophy. In affected skin, scutula tend to form that have a raised periphery and a central depressed area [4].
Epidemiology An Overview The predominance of specic pathogens that cause TCS varies with geography, environment, climate, occupation, and host lifestyle [41]. Favus is seen often in geographic regions where there is a great poverty and thus poor hygiene, malnutrition, and little access to health care [8, 12, 55]. Notably, certain dermatophyte species such as M. audouinii and T. schoenleinii have declined drastically with the advent of drug therapies in the last half-century [4, 56, 57]. T. schoenleinii was formerly highly endemic in the Middle East, Iran, Kashmir, parts of Africa, and Greenland. In North America, there were a few small endemic foci, for example, in Kentucky (USA) and in Quebec and Montreal (Canada) [12]. Favus is extremely common among the Bantu in South Africa, where it is called witkop. There is also a focus in o Paulo in Brazil, and a few isolates the vicinity of Sa have been found in Chile and Argentina [12]. These foci have been largely eradicated, except in Iran [58], some parts of Africa [59], and China [41]. Europe Trichophyton schoenleinii was a predominant dermatophyte in Eastern Europe in the late 19th and early twentieth centuries [5, 60]. Improvements in living conditions and hygiene in developing countries after World War II have been associated with the almost complete disappearance of many anthropophilic species, including T. schoenleinii [10, 55]. In 1997, a survey of tinea capitis conducted by the European Confederation of Medical Mycology across 19 European countries showed that T. schoenleinii constituted 3 of 3,671 (0.08%) isolates [61]. In some other studies of tinea capitis cases, T. schoenleinii had varying low prevalence rates0% [6266], 0.4% [67], 0.5% [68, 69], and 1.5% [70]in different European countries in the last two decades. Currently, favus is uncommon in Europe and has nearly disappeared except in some small foci in geographic regions with a high level of poverty and malnutrition [71]. A study in Spain reported a decline in tinea capitis since 1951: M. canis was always the most common agent, and T. schoenleinii was found only between
123
Mycopathologia (2010) 170:143154
149
1951 and 1959, but not afterward [72]. In the Netherlands, Korstanje et al. [73] investigated 435 cases of tinea capitis for etiological agents over a period of 30 years (19631993). During this time, the dominant causative organism shifted from T. schoenleinii to T. violaceum, which may have been due in part to increased immigration from the Mediterranean countries where T. violaceum is more common. Borman et al. [56] found no cases of T. schoenleinii when they analyzed 15,333 isolates in the British Isles between 1980 and 2005. In Poland, T. schoenleinii was isolated in 2 of 1,045 (0.2%) samples collected from cases of tinea capitis over a 20-year period [74]. Africa and the Middle East
of the Americas conducted four detailed 3-year studies from 1979 to 1995. The authors recovered a total of 59,648 dermatophytes and reported that only 8 (0.01%) were T. schoenleinii. The anatomical sites of infection were not noted [8790]. T. schoenleinii was detected in 23 of 4,252 (0.5%) dermatophyte strains in Alberta, Canada over a 13-year period (19721984) [23]. Interestingly, the authors recovered T. schoenleinii in 2 of 355 (0.6%) tinea barbae cases. T. schoenleinii was introduced in Brazil by European immigrants, and this organism later became o Paulo among autochthonous very common in Sa patients [91]. In 1932, Magalhaes [92] reported that T. schoenleinii had caused favus epidemics in Minas Gerais, Brazil. China
In 1976, Malhotra et al. [75] detected 164 culturepositive cases of tinea capitis in Libya; T. schoenleinii (69.5%) was the most prevalent dermatophyte species. Two decades later, there had been a dramatic decrease in prevalence: of 584 scalp samples collected in Libya from 1997 to 1999, the fungus was recovered in only 10 (1.7%) [76]. In addition, one study noted a signicant drop in the incidence of favus in Libya, with the complete disappearance of T. schoenleinii as a causative agent of tinea capitis [32]. In Tunisia between 1998 and 2007, Neji et al. [77] observed 1,434 cases of tinea capitis, only 3 (0.2%) of which were due to T. schoenleinii. In 46 cases of tinea capitis in Jordan, T. schoenleinii was the third most prevalent fungus (17.4%) [78]. In the Nablus district in Palestine, Ali-Shtayeh et al. [79] reported 75 cases of tinea capitis in which T. violaceum was the most common causative agent (82.7%), followed by M. canis (16%) and T. schoenleinii (1.3%). In another Iranian study, 5.4% of the dermatophyte isolates from several anatomical sites were T. schoenleinii [80]. Interestingly, several studies from the Middle East [32, 76, 81], Africa [8284], and India [85, 86] reported no occurrence of favus. North and South America In 1896, according to Lane [40], Wende found that 22 of 29 (75.9%) cases of favus in Buffalo originated in the USA; 21 of the patients had been born in America. Almost a century later, the Dermatophyte Survey Committee of the Medical Mycology Society
In the 1950s and 1960s, T. schoenleinii and M. ferrugineum were the predominant pathogens in cases of tinea capitis in China. In the late 1960s, a concerted and successful treatment program was initiated in the Henan, Anhui, and Hubei provinces, which had a high incidence of favus. After treatment the incidence of favus decreased greatly to less than 1 per 100,000 [20]. More recently, however, Zhu et al. [93] presented a retrospective analysis of tinea capitis cases in southeastern China from 1993 to 2008. The authors observed only 1 case of favus due to T. schoenleinii among 866 patients. Turkey Dermatophytes and dermatophytoses have been reported in Turkey since the beginning of the twentieth century, despite research prior to 1950 that was unpublished or lost [94]. Talad [95] rst reported favus during the Ottoman Empire; and later, in the 1920s, Hulusi Behc et [96] reported favus cases in Turkey. Between 1938 and 1944, Marchionini [97] diagnosed mycosis in 5,820 of 106,956 (5.5%) cases referred to his clinic in Ankara; of these cases, 39% were diagnosed with favus. Working in Hamburg, tz [31] analyzed 96 Germany, Marchionini and Go clinical samples they obtained from patients with favus in Turkey. Dermatophytes isolated from these samples included T. schoenleinii (81.3%), M. canis (12.5%), T. verrucosum (3.1%), and T. violaceum (3.1%). Unat [98] isolated T. schoenleinii in 11 of
123
150
Mycopathologia (2010) 170:143154
107 (18%) cases with tinea capitis. Aksungur [9] recovered fungi in 162 cultures obtained from 170 favus cases; 95.7% were T. schoenleinii, 3.1% T. violaceum, and 1.2% T. violaceum ? T. schoenleinii. Taken together, these three studies revealed that tinea capitis was the most common dermatophytosis, with T. schoenleinii the most common agent for scalp ringworm in rural areas, and T. violaceum and M. canis the most common agents in urban areas [9, 31, 98]. The rst population-based investigation in Turkey to address this public health problem was performed by Erbakan and Ekmen [99] in three provinces, nine towns, and 49 villages. The study comprised 8,521 participants and found a prevalence of 0.22% for TCS in villages, towns, and provinces, and 2% for favus in villages and towns. Erbakan [100] reported yearly changes in dermatophytoses rates among patients applying to a dermatology clinic in Ankara, Turkey. From 1956 to 1975, TCS rates decreased from 24.6 to 1.8%; kerion celsi rates decreased from 7.0 to 3.8%; and favus rates decreased from 5.5 to 0.2%. In the following years, the decrease in cases of tinea capitis, including kerion celsi, continued, falling from rst place on the list of dermatophytoses in Turkey to the end of the list [94, 101]. The introduction of griseofulvin in 1958, together with vigilant surveillance in schools, has led to a marked decline in tinea capitis throughout Europe [61, 71, 94]. Erbakan et al. [13] reviewed 1,053 cases of tinea favosa from 1953 to 1985 in central Anatolia, Turkey. T. schoenleinii was the only fungus recovered in 642 (61.6%) of the patients. The authors noted the most common site(s) of infection were the scalp (93%), followed by glabrous skin (1.7%), nails (1.2%), scalp ? glabrous skin (2.1%), scalp ? nails (0.9%), and all of these sites at the same time (1.1%). In eastern Anatolia, Turkey, Ural et al. [14] recovered fungi in 186 of 241 (77.2%) cases of tinea capitis favosa from 1979 to 1982. The authors identied T. schoenleinii (93%), T. violaceum (3.2%), T. verrucosum (2.7%), and T. schoenleinii ? T. verrucosum (1.1%). In Turkey, favus is common among children in families living in east and mid-Anatolia and in families who emigrated from these regions [9, 13, 14, 31, 33, 9799]. Tumbay et al. [101] reported that most of the children with favus infections in the Aegean region had acquired the infection in their
hometowns in east Anatolia. In a survey of military recruits stationed in Izmir, tinea capitis favosa caused by T. schoenleinii was diagnosed in two soldiers whose hometowns were in east Anatolia. Both had been infected since childhood, and the study authors stated that these recruits could be a source for contagious infection among the privates [102]. For this reason, the authors suggested that candidates be examined regularly for favus and that their place of birth be recorded. Erbakan [13] reported that 95 private soldiers, aged 2034, were treated for favus in the period between 1975 and 1985 in the Dermatology Department of the Gulhane Military Medical Academy of Turkey. In the last decade, there have been several studies of tinea capitis in Turkey. Metin et al. [33] reported 1 case of favus (2.5%) due to T. violaceum among 40 cases of tinea capitis. In addition, Akpolat et al. [103] reported 2 isolates of T. schoenleinii (1.6%) among 124 culture-positive pediatric patients with tinea capitis. In contrast, two other reports detected no cases of tinea favosa in school children [104, 105]. In the examinations of over 110,000 school-aged children by our group from 1998 to 2009 in and around Adana, Turkey, there were no documented cases of favus or T. schoenleinii. Taking all of these studies into consideration, it seems that tinea favosa is still encountered sporadically in Turkey. Current Endemic Areas A worldwide survey in the 2000s, of the causative agents of tinea capitis revealed that T. schoenleinii was still the predominant species in China (31.5%), Nigeria (28.1%), and Iran (21.5%) [41, 58, 59]. Deng et al. [41] reported that T. violaceum (41.2%) and T. schoenleinii (35.1%) were the predominant etiologic agents of tinea capitis in Xinjiang school children in western China. Interestingly, clinical presentation was frequently different than expected: for example, of 31 cases caused by T. schoenleinii, only 9 were identied as favus and with the other 22 as identied as gray-patch type tinea capitis. In addition, T. schoenleinii was still the predominant dermatophyte (28.1%) in cases in school children in the Borno State of Nigeria, and this fungus was isolated from affected areas of the scalp, hand, trunk, ear, and face [59]. In Iran, Jahromi and Khaksar [58] reported 209 tinea capitis cases in which T. violaceum
123
Mycopathologia (2010) 170:143154
151
was the most common causative agent (37.3%), followed by T. schoenleinii (21.5%). Treatment The infection rarely resolves spontaneously, although the crusts, inammation, and debris may gradually subside over time [12]. With the introduction of griseofulvin in 1958, the anthropophilic agents of scalp ringworm, T. schoenleinii and M. audouinii, were almost eradicated in most parts of the world [56, 57]. This radical decrease is certainly one of the most important changes in the spectrum of dermatophytes isolated from scalp lesions [57]. There are number of options for treating tinea capitis, and it seems that these options are unchanged over years, in particular favus [10, 11, 16, 39, 61, 71]. Treatment protocols for TCS have been reviewed in detail [10, 16, 39, 61, 71, 106]. In favus, resolution of infection has been accomplished with the long-term use of some drugs. The drugs and the dosage schedules are the same as for TCS, e.g., terbinane or itraconazole [8, 12]. In vitro studies indicate that T. schoenleinii, like other dermatophytes, is sensitive to some of the newer antifungal drugs [8]. Clearing away the scalp debris, removing the crusts, and general improvement of scalp hygiene and aid in clinical management are essential in treating this infection. It is also important to treat all family members simultaneously [8, 12]. The treatment outcome depends to some extent on the stage at which the disease is arrested [8].
etiological agents of human favus are anthropophilic, zoophilic, and geophilic dermatophytes. Notably, favus of the scalp is the most common form of tinea favosa. In the past, favus was also the dominant form of tinea capitis in some parts of the world such as Eurasia and North Africa. Although the incidence of favus is declining in developing nations, it is still an unsolved epidemiological problem. In the future, favus is a good candidate for complete eradication worldwide via preventive medicine and the use of modern antifungals. Further elucidation of the molecular mechanisms of mycological infections and more epidemiological data may improve the management of this infection.
Acknowledgments This particular study is dedicated to an outstanding medical mycologist, emeritus Prof Dr Emel Tumbay, who spent a signicant part of her career researching into dermatophytic fungi and served as a master of science and education throughout her entire life in Turkey.
References
1. Marks AR. Dermatophytes in art. J Med Vet Mycol. 1991;29:18. 2. Kane J. A historical perspective. In: Kane J, Summerbell R, Sigler L, Krajden S, Land G, editors. Laboratory handbook of dermatophytes: a clinical guide and laboratory manual of dermatophytes and other lamentous fungi from skin, hair and nails. Belmont, CA: Star Publishing; 1997. p. xvxvi. es a ` 3. Alibert J. Description des malaides de la peau observe pital Saint-Louis et exposition des meilleures me thlho odes suivies pour leur traitement, Barrois, Paris; 1806. p. 129. 4. Weitzman I, Summerbell RC. The dermatophytes. Clin Microbiol Rev. 1995;8:24059. 5. Seeliger HP. The discovery of Achorion schoenleinii: facts and stories (Johann Lucas Schoenlein and Robert Remak). Mykosen. 1985;28:16182. 6. Seeliger HP. The beginnings of medical mycology. In: Tumbay E, editor. FEMS symposium on dermatophytoses and dermatophytoses in man and animals (May 2123, 1986, Izmir), proceedings. Izmir: Bilgehan Publishing House; 1988. p. 115. 7. Gupta AK, Summerbell RC. The dermatophytes. In: Hay RJ, Merz W, editors. Topley and Wilsons microbiology and microbial infections, medical mycology, vol. 5. 10th ed. London: Arnold Publishers; 2005. p. 22043. 8. Szepietowski J, Schwartz RA. Favus. eMedicine from WebMD. 2009. 9. Aksungur L. Dermatophyte ora of tinea capitis in eastern Anatolia. Turk J Pediatr. 1968;10:2331. 10. Elewski BE. Tinea capitis: a current perspective. J Am Acad Dermatol. 2000;42:120.
Conclusions This review is intended to summarize current knowledge about favus, increase awareness of studies that may not be well known, and highlight areas that merit further research. The discovery of T. schoenleinii by pioneering researchers launched the eld of medical mycology in the mid-nineteenth century, and their curiosity and spirits continue to motivate others to explore fungal diseases in greater depth. Over time, numerous studies revealed that T. schoenleinii is the most common causative agent of tinea favosa. However, infections due to T. schoenleinii may have different clinical presentations, as for TCS or the carrier state. It has been established that the
123
152 11. Schwartz RA, Janniger CK. Tinea capitis. Cutis. 1995;55:2933. 12. Rippon JW. Dermatophytosis and dermatomycosis. In: Medical mycologythe pathogenic fungi and the pathogenic actinomycetes. 3rd ed. Philadelphia: WB Saunders; 1988. p. 1979. 13. Erbakan AN, Erdem C, Gurler A, Peksar Y. The clinical and mycological characteristics of tinea favosa. In: Tumbay E, editor. FEMS symposium on dermatophytes and dermatophytoses in man and animals (May 2123, 1986, Izmir), proceedings. Izmir: Bilgehan Publishing House; 1988. p. 28592. 14. Ural A, Ergenekon G, Kot S. Tinea capitis favosa. A report on and analysis of 241 cases in Erzurum, Turkey. In: Tumbay E, editor. FEMS Symposium on dermatophytes and dermatophytoses in man and animals (May 2123, 1986, Izmir), proceedings. Izmir: Bilgehan Publishing House; 1988. p. 2936. 15. Grappel SF, Blank F, Bishop CT. Circulating antibodies in human favus. Dermatologica. 1971;143:2416. 16. Gupta AK, Summerbell RC. Tinea capitis. Med Mycol. 2000;38:25587. 17. Carslaw WR. Favus of the scalp: observation on the manner of spread. Br J Dermatol. 1955;67:3926. 18. Cecchi R, Paoli S, Giomi A, Rossetti R. Favus due to Trichophyton schoenleinii in a patient with metastatic bronchial carcinoma. Br J Dermatol. 2003;148:1057. 19. Devliotou-Panagliotidou D, Koussidou-Eremondi T, Chaidemenos GC, Theodoridou M, Minas A. Tinea capitis in adults during 19811995 in northern Greece. Mycoses. 2001;44:398400. 20. Yu J, Li R, Bulmer G. Current topics of tinea capitis in China. Jpn J Med Mycol. 2005;46:616. 21. Krunic AL, Cetner A, Tesic V, Janda WM, Worobec S. Atypical favic invasion of the scalp by Microsporum canis: report of a case and review of reported cases caused by a Microsporum species. Mycoses. 2007;50:1569. 22. Prochnau A, de Almeida HL, Souza PRM, et al. Scutular tinea of the scrotum: report of two cases. Mycoses. 2005;48:1624. 23. Sekhon AS, Garg AK. A 13-year (19721984) study of dermatophytic infections in Alberta, Canada. Mykosen. 1986;29:25562. 24. Sanic A, Gunaydn M, Durupnar B, et al. Samsun ve lt. 1996;30:57 c evresinde dermatotozlar. Mikrobiyol Bu 63. 25. Romano C, Maritati E, Gianni C. Tinea incognito in Italy: a 15-year survey. Mycoses. 2006;49:3837. 26. Kasmoglu O, Oke N. Tinea unguium vakalarndan izole edilen mantarlar. Istanbul Univ Tp Fak Mec. 1977;40:5248. 27. Dostrovsky A, Sagher F, Raubitschek F. Favus generalisatus. Br J Dermatol. 1957;69:35862. 28. Way SC, Weidman FD. Favus in California: report of case due to a strain pathogenic for mice. Cal West Med. 1932;36:3226. 29. Kundrat H. Wien Med Blatter; 1884. p. 1538. 30. Mohammad A, Al-Rajhi A, Wagoner D. Trichophyton fungal keratitis. Cornea. 2006;25:11822.
Mycopathologia (2010) 170:143154 ber Kopfpilzerkrankungen in tz H. U 31. Marchionini A, Go cksichtigung des Favus. Anatolien mit besonderer Beru Arch Dermatol Syph. 1950;100:7588. 32. Gargoom AM, Elyazachi MB, Al-Ani SM, Duweb GA. Tinea capitis in Benghazi, Libya. Int J Dermatol. 2000;39:2635. 33. Metin A, Subas S, Bozkurt H, C alka O. Tinea capitis in Van, Turkey. Mycoses. 2002;45:4925. 34. Besbes M, Cheikhrouhou F, Selami H, et al. Favus due to Trichophyton mentagrophytes var. quinckeanum. Mycoses. 2003;46:35860. 35. Garcia-Sanchez MS, Pereiro M, Pereiro MM, Toribio J. Favus due to Trichophyton mentagrophytes var. quinckeanum. Dermatology. 1997;194:1779. 36. Feurman EJ, Alteras I, Bashan D, Shohat B. Trichophytosis by double infection of Trichophyton schoenleinii and Trichophyton violaceum. Sabouradia. 1978;16:913. 37. Figueroa JI, Hawranek T, Abraha A, Hay RJ. Tinea capitis in south-western Ethiopia: a study of high risk factors for infection and carriage. Int J Dermatol. 1997;36:6616. 38. Hansell J, Partridge BM. Favus: a report of seven related cases. Br Med J. 1955;1:15101. 39. Aly R, Hay RJ, del Palacio A, Galimberti R. Epidemiology of tinea capitis. Med Mycol. 2000;38(suppl 1):1838. 40. Lane JE. The need of better control of some neglected contagious disease. Am J Public Health. 1916;6:24453. 41. Deng S, Bulmer GS, Summerbell RC, et al. Changes in frequency of agents of tinea capitis in school children from Western China suggest slow migration rates in dermatophytes. Med Mycol. 2008;46:4217. 42. Guirges SY. Viability of Trichophyton schoenleinii in epilated hairs. Sabouraudia. 1981;19:1556. 43. Inman P. Favus of the scalp with unusual epidemiological features. Br J Dermatol. 1954;66:40910. 44. Gupta AK, Ahmad I, Summerbell RC. Comparative efcacies of commonly used disinfectants and antifungal spray preparations against dermatophytic fungi. Med Mycol. 2001;39:3218. 45. Ilkit M, Demirhindi H. Asymptomatic scalp dermatophyte scalp carriage: laboratory diagnosis, epidemiology and management. Mycopathologia. 2008;165:6171. 46. Greer DL. Treatment of symptom-free carriers in management of tinea capitis. Lancet. 1996;348:3501. 47. Geerts CA, Uyttendaele-Geeraerts C, Uyttendaele K. A family with favus. Arch Belg Dermatol Syphiligr. 1967;23:99101. 48. Prochacki H. Familial favus. Mykosen. 1970;13:4515. 49. Summerbell RC, Kane J. The genera Trichophyton and Epidermophyton. In: Kane J, Summerbell R, Sigler L, Krajden S, Land G, editors. Laboratory handbook of dermatophytes: a clinical guide and laboratory manual of dermatophytes and other lamentous fungi from skin, hair and nails. Belmont, CA: Star Publishing; 1997. p. 13193. re A, Blank F. Macroconidia of 50. Grappel SF, Fethie Trichophyton schoenleinii. Sabouraudia. 1971;9:1445. 51. Chattaway FW, Barlew AJE. Further studies on the uorescent compounds produced in vivo by Trichophyton schoenleinii. Sabouraudia. 1966;4:26572.
123
Mycopathologia (2010) 170:143154 ser Y, Scott J, Summerbell RC. The new species 52. Gra concept in dermatophytesa polyphasic approach. Mycopathologia. 2008;166:23956. 53. Verankar MP, Pinto MJ, Rodrigues SJ, Singh I, Rege VL. Tinea capitis due to Trichophyton schoenleinii. Indian J Pathol Microbiol. 1991;34:299301. ser Y. Development of DNA 54. Probst S, de Hoog GS, Gra markers to explore host shifts in dermatophytes. Stud Mycol. 2003;47:5774. 55. Khaled A, Ben Mbarek L, Khar M, et al. Tinea capitis favosa due to Trichophyton schoenleinii. Acta Dermatoven Alp Panonica Adriat. 2007;16:346. 56. Borman AM, Campbell CK, Fraser M, Johnson EM. Analysis of the dermatophyte species isolated in the British Isles between 1980 and 2005 and review of worldwide dermatophyte trends over the last three decades. Med Mycol. 2007;45:13141. 57. Seebacher C, Bouchara JP, Mignon B. Updates on the epidemiology of dermatophyte infections. Mycopathologia. 2008;166:33552. 58. Jahromi SB, Khaksar AA. Aetiological agents of tinea capitis in Tehran (Iran). Mycoses. 2006;49:657. 59. Nweze EI. Etiology of dermatophytoses amongst children in northeastern Nigeria. Med Mycol. 2001;39:1814. 60. Ajello L. Natural history of the dermatophytes and related fungi. Mycopathol Mycol Appl. 1974;53:93110. 61. Hay RJ, Robles W, Midgley MK, Moore MK. Tinea capitis in Europe: new perspective on an old problem. J Eur Acad Dermatol Venereol. 2001;15:22933. 62. Nowicki R. Dermatophytoses in the Gdansk area, Poland. A 12-year survey. Mycoses. 1996;39:399402. I, Kucerova H. Dermatophytoses in Prague, 63. Kuklova Czech Republic, between 1987 and 1998. Mycoses. 2001;44:4936. llgren J, Petrini B, Wahlgren CF. Increasing tinea 64. Ha capitis prevalence in Stockholm reects immigration. Med Mycol. 2004;42:5059. 65. Koussidou-Eremondi T, Devliotou-Panaglitidou D, Mourellou-Tsatsou O, Minas A. Epidemiology of dermatomycoses in children living in Northern Greece 1996 2000. Mycoses. 2005;48:116. 66. Binder B, Lackner HK, Poessl BD, et al. Prevalence of tinea capitis in Southeastern Austria between 1985 and 2008: up-to-date picture of current situation. Mycoses. doi:10.1111/j.1439-0507.2009.01804. 67. Terragni L, Lasagni A, Oriani A. Dermatophytes and dermatophytoses in the Milan area between 1970 and 1989. Mycoses. 1993;36:3137. 68. Tietz HJ, Czaika V, Ulbricht HM, Sterry W. Tinea capitis in Germany. A survey in 1998. Mycoses. 1999;42(suppl 2):736. 69. Rubio-Calvo C, Gill-Thomas J, Rezusta-Lopez A, BenitoRuesca R. The aetiological agents of tinea capitis in Zaragoza, Spain. Mycoses. 2001;44:558. 70. Babic-Erceg A, Barisic Z, Erceg M, et al. Dermatophytoses in Split and Dalmatia, Croatia, 19962002. Mycoses. 2004;47:2979. 71. Ginter-Hanselmayer G, Weger W, Ilkit M, Smolle J. Epidemiology of tinea capitis in Europe: current state and changing patterns. Mycoses. 2007;50:613.
153 72. Pereiro-Miguens M, Pereiro M, Pereiro M. Review of dermatophytosis in Galicia from 1951 to 1987 and comparison with other areas of Spain. Mycopathologia. 1991;113:6578. 73. Korstanje MJ, Staats CCG. Tinea capitis in northwestern Europe 19631993: etiologic agents and their changing prevalence. Int J Dermatol. 1994;33:5489. 74. Niczyporuk W, Krajewska-Kulak E, Lukaszuk C. Tinea capitis favosa in Poland. Mycoses. 2004;47:25760. 75. Malhotra YK, Garg MP, Kanwar AJ, Nagrajan S. A study of tinea capitis in Libya (Benghazi). Sabouradia. 1979;17:1813. 76. Ellabib MS, Agaj M, Khalifa Z, Kavanagh K. Trichophyton violaceum is the dominant cause of tinea capitis in children in Tripoli, Libya: results of a two-year survey. Mycopathologia. 2002;153:1457. 77. Neji S, Makni F, Cheikhrouhou F, et al. Epidemiology of dermatophytoses in Sfax, Tunisia. Mycoses. 2009;52:5348. 78. Abu-Elteen KH, Abdul Malek M. Prevalence of dermatophytoses in the Zarga district of Jordan. Mycopathologia. 1999;145:13742. 79. Ali-Shtayeh MS, Arda HM, Abu-Ghdeib SI. Epidemiological study of tinea capitis in school children in the Nablus area (West Bank). Mycoses. 1998;41:2438. 80. Chadeganipour M, Shadzi S, Dehghan P, Movahed M. Prevalence and aetiology of dermatophytoses in Isfahan, Iran. Mycoses. 1997;40:3214. 81. Ali-Shtayeh MS, Salameh AAM, Abu-Ghdeib SI, Jamous RM, Khraim H. Prevalence of tinea capitis as well as of asymptomatic carriers in school children in Nablus area (Palestine). Mycoses. 2002;45:18894. 82. Menan EI, Zenga-Bonou O, Rouet F, et al. Tinea capitis in school children from Ivory Coast, western Africa. Int J Dermatol. 2002;41:2047. 83. Woldeamanuel Y, Leekassa R, Chryssanthou E, Menghistu Y, Petrini B. Prevalence of tinea capitis in Ethiopian schoolchildren. Mycoses. 2005;48:13741. 84. Sidat MM, Correia D, Buene TB. Tinea capitis among rural school children of the district Uaguda, in Maputo province, Mozambique. Mycoses. 2006;49:4803. 85. Johangir M, Hussain I, Khurshid K, Haroon TS. A clinico-etiologic correlation in tinea capitis. Int J Dermatol. 1999;38:2758. 86. Jha BN, Garg VK, Agrawal S, Khanal B, Agarwalla A. Tinea capitis in eastern Nepal. Int J Dermatol. 2006;45:1002. 87. Sinski JT, Flouras KA. A survey of dermatophytes isolated from human patients in the United States from 1979 to 1981. Mycopathologia. 1984;85:97120. 88. Sinski JT, Kelley LM. A survey of dermatophytes isolated from human patients in the United States from 1982 to 1984. Mycopathologia. 1987;98:3540. 89. Sinski JT, Kelley LM. A survey of dermatophytes isolated from human patients in the United States from 1985 to 1987. Mycopathologia. 1991;114:11726. 90. Weitzman I, Chin I-X, Kunjukunju N, Della-Latta P. A survey of dermatophytes isolated from human patients in the United States from 1993 to 1995. J Am Acad Dermatol. 1998;39:25561.
123
154 91. Londeros AT. The geographic distribution and prevalence of dermatophytes in Brasil. Sabouradia. 1963;2:10810. 92. Magalhaes O. Ensaios de Micologia. Mem Inst Oswaldo Cruz. 1935;30:155. 93. Zhu M, Li L, Wang J, Zhang C, Zhang Q. Tinea capitis in southeastern China: a 16-year survey. Mycopathologia. 2010;169:2359. ru rkiyede go len dermatotler ve mikolojik 94. Ilkit M. Tu zellikleri. In: Ozbal Y, Koc AN, editors. Dermatomikoz o etkenleri ve dermatomikozlar (34 Haziran 2004, Kayseri) rk Mikrobiyoloji Cemiyeti Yayn No: 48. Tutanaklar. Tu Kayseri: Erciyes Universitesi Basmevi; 2004. p. 2343. 95. Talad. Universeller Favus. Dtsch Med Wochenschr. 1908;34:13113. _ 96. Behc et H. Trichophytideler. Istanbul Seririyat. 1921 1922: No 7. rkiyede cilt mu tehassssn ilgilendi97. Marchionini A. Tu lk problemleri. Ankara ren epidemiyolojik ve sosyal sag Univ Tp Fak Mec. 1947;1:12742. _ 98. Unat EK. Istanbulda rastlanlan sac l deri dermatotleri _ hakknda. Istanbul Univ Tp Fak Mec. 1952;15:8906. 99. Erbakan N, Ekmen H. The ecology of dermatophytes in Central Anatolia. Acta Med Turcica. 1965;2:11825. 100. Erbakan AN. Dermatophytosis as seen in our clinic for the past nine years. In: Aksungur L, editor. 6. Ulusal
Mycopathologia (2010) 170:143154 l 1976, Mersin) kiDermatoloji Kongresi (2124 Eylu niversitesi Yaynlar No: 1. Adana: tabnda. C ukurova U niversitesi Basmevi; 1976. p. 1236. C ukurova U Tumbay E, Inci R, Gezen C. Pattern of dermatophytes in the Aegean Region of Turkey. In: Tumbay E, editor. FEMS symposium on dermatophytes and dermatophytoses in man and animals (May 2123, 1986, Izmir), proceedings. Izmir: Bilgehan Publishing House; 1988. p. 299304. Karaman A, Tumbay E, Demir O. Izmirde askerlerde ru len dermatotoz etkenleri. Lepra Mec. 1981;12: go 13643. Akpolat NO, Akdeniz S, Elci S, Atmaca S, Ozekinci T. Tinea capitis in Diyarbakr, Turkey. Mycoses. 2005;48: 810. Altndis M, Bilgili E, Kiraz N, Ceri A. Prevalence of tinea capitis in primary schools in Turkey. Mycoses. 2003;46:21821. Gumusay T, Ilkit M. Epidemiology of tinea capitis in Ceyhan district, Adana in Cukurova region, Turkey. Mycoses. 2006;49:3469. Fuller LC. Changing face of tinea capitis in Europe. Curr Opin Infect Dis. 2009;22:1158.
101.
102.
103.
104.
105.
106.
123
Reproduced with permission of the copyright owner. Further reproduction prohibited without permission.
S-ar putea să vă placă și
- Trombocytosis Essential PDFDocument5 paginiTrombocytosis Essential PDFKerin ArdyÎncă nu există evaluări
- Comparison of Angiotensin Converting Enzyme (Ace) Inhibitors Drug Approximate Dose Equivalence Maximum Daily Dose (Mg/day) Once Daily DosingDocument1 paginăComparison of Angiotensin Converting Enzyme (Ace) Inhibitors Drug Approximate Dose Equivalence Maximum Daily Dose (Mg/day) Once Daily DosingKerin ArdyÎncă nu există evaluări
- Ferritin TrendsDocument4 paginiFerritin TrendsKerin ArdyÎncă nu există evaluări
- Essential Trombocytosis EssentialDocument4 paginiEssential Trombocytosis EssentialKerin ArdyÎncă nu există evaluări
- Pregnancy ThalasemiaDocument3 paginiPregnancy ThalasemiaKerin ArdyÎncă nu există evaluări
- 10Document7 pagini10Kerin ArdyÎncă nu există evaluări
- Management and Outcomes For Patients With TTP: Analysis of 100 Cases at A Single InstitutionDocument6 paginiManagement and Outcomes For Patients With TTP: Analysis of 100 Cases at A Single InstitutionBilly Shan LastKagerooboroÎncă nu există evaluări
- A Practical Classification of Childhood Hypopigmentation DisordersDocument6 paginiA Practical Classification of Childhood Hypopigmentation DisordersKerin ArdyÎncă nu există evaluări
- 631927Document8 pagini631927Kerin ArdyÎncă nu există evaluări
- Pregnancy ThalasemiaDocument3 paginiPregnancy ThalasemiaKerin ArdyÎncă nu există evaluări
- Vitiligo in ChildrenDocument4 paginiVitiligo in ChildrenKerin ArdyÎncă nu există evaluări
- HLA-C Expression Pattern Is Spatially Different Between Psoriasis and Eczema Skin LesionsDocument7 paginiHLA-C Expression Pattern Is Spatially Different Between Psoriasis and Eczema Skin LesionsKerin ArdyÎncă nu există evaluări
- HB in Cardio PDFDocument5 paginiHB in Cardio PDFKerin ArdyÎncă nu există evaluări
- Trombocytosis Essential PDFDocument5 paginiTrombocytosis Essential PDFKerin ArdyÎncă nu există evaluări
- Ni Hms 600206Document13 paginiNi Hms 600206Kerin ArdyÎncă nu există evaluări
- Ferritin TrendsDocument4 paginiFerritin TrendsKerin ArdyÎncă nu există evaluări
- HB in Cardio PDFDocument5 paginiHB in Cardio PDFKerin ArdyÎncă nu există evaluări
- 10.1016@S0190 9622 (81) 80205 8Document6 pagini10.1016@S0190 9622 (81) 80205 8Kerin ArdyÎncă nu există evaluări
- 8261 23271 1 PBDocument8 pagini8261 23271 1 PBKerin ArdyÎncă nu există evaluări
- Superoxide Dismutase Activity Colorimetric Assay Kit Ab65354Document3 paginiSuperoxide Dismutase Activity Colorimetric Assay Kit Ab65354Kerin ArdyÎncă nu există evaluări
- Ni Hms 600206Document13 paginiNi Hms 600206Kerin ArdyÎncă nu există evaluări
- Human Papillomavirus-Associated Cancers in Patients With Human Immunodeficiency Virus Infection and Acquired Immunodeficiency SyndromeDocument11 paginiHuman Papillomavirus-Associated Cancers in Patients With Human Immunodeficiency Virus Infection and Acquired Immunodeficiency SyndromeKerin ArdyÎncă nu există evaluări
- The Epidemiology of HPVDocument9 paginiThe Epidemiology of HPVMG's Fhya Part IIÎncă nu există evaluări
- Essential Trombocytosis EssentialDocument4 paginiEssential Trombocytosis EssentialKerin ArdyÎncă nu există evaluări
- 28 14Document10 pagini28 14Kerin ArdyÎncă nu există evaluări
- HLA-Cw6 and The Genetic Predisposition To Psoriasis: A Meta-Analysis of Published Serologic StudiesDocument3 paginiHLA-Cw6 and The Genetic Predisposition To Psoriasis: A Meta-Analysis of Published Serologic StudiesKerin ArdyÎncă nu există evaluări
- Hum. Mol. Genet. 2000 Asumalahti 1533 42Document10 paginiHum. Mol. Genet. 2000 Asumalahti 1533 42Kerin ArdyÎncă nu există evaluări
- 1089 FullDocument2 pagini1089 FullKerin ArdyÎncă nu există evaluări
- Molecular Dissection of Psoriasis: Integrating Genetics and BiologyDocument14 paginiMolecular Dissection of Psoriasis: Integrating Genetics and BiologyKerin ArdyÎncă nu există evaluări
- EScholarship UC Item 8r48b2j2Document3 paginiEScholarship UC Item 8r48b2j2Kerin ArdyÎncă nu există evaluări
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (120)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Chapter 28Document14 paginiChapter 28ram sunderÎncă nu există evaluări
- Tinea - The DermatophytesDocument67 paginiTinea - The Dermatophytesmansoor aliÎncă nu există evaluări
- Resident's Page: Wood's Lamp Wood's Lamp Wood's Lamp Wood's Lamp Wood's LampDocument5 paginiResident's Page: Wood's Lamp Wood's Lamp Wood's Lamp Wood's Lamp Wood's LampMovaliya GhanshyamÎncă nu există evaluări
- Antifungal Agents: LipopeptidesDocument8 paginiAntifungal Agents: LipopeptidesCristian QuitoÎncă nu există evaluări
- Mycology McqsDocument6 paginiMycology McqsmryamÎncă nu există evaluări
- DERM Resource Common+Skin+Diseases+in+Africa-1Document94 paginiDERM Resource Common+Skin+Diseases+in+Africa-1OlaÎncă nu există evaluări
- Wood's Lamp in Dermatology: Applications in The Daily PracticeDocument3 paginiWood's Lamp in Dermatology: Applications in The Daily Practicethais ribeiroÎncă nu există evaluări
- Fungal InfectionsDocument42 paginiFungal InfectionsleenaloveuÎncă nu există evaluări
- Mycology Viva With AnswerDocument8 paginiMycology Viva With AnswerKumar KPÎncă nu există evaluări
- Classification of Fungal InfectionsDocument26 paginiClassification of Fungal Infectionstev26Încă nu există evaluări
- Dermatofitosis FitzpatrickDocument28 paginiDermatofitosis FitzpatrickFadli IlhamÎncă nu există evaluări
- Epidemiological Trends in Skin Mycoses Worldwide: Blanka Havlickova, Viktor A. Czaika and Markus FriedrichDocument14 paginiEpidemiological Trends in Skin Mycoses Worldwide: Blanka Havlickova, Viktor A. Czaika and Markus FriedrichRS Tk IV PekanbaruÎncă nu există evaluări
- ImpetigoDocument21 paginiImpetigoHanif GandohÎncă nu există evaluări
- DermatomycosesDocument34 paginiDermatomycosesRomMy WiEn MicKhoÎncă nu există evaluări
- An Asymptomatic Superficial Fungal Infection of The Hair ShaftDocument6 paginiAn Asymptomatic Superficial Fungal Infection of The Hair ShaftShaniaÎncă nu există evaluări
- Anki MycologyDocument23 paginiAnki MycologyMarietoni PicoÎncă nu există evaluări
- Updates On The Epidemiology of Dermatophyte InfectionsDocument19 paginiUpdates On The Epidemiology of Dermatophyte InfectionsAldo NovaÎncă nu există evaluări
- Dermatology Images (All in One Merged)Document692 paginiDermatology Images (All in One Merged)Woo Rin Park100% (2)
- Fungi Causing Superficial MycosesDocument41 paginiFungi Causing Superficial MycosesdiniÎncă nu există evaluări
- Dermatology OSPEDocument148 paginiDermatology OSPEAmira NabilÎncă nu există evaluări
- Telltale Signs of Skin Trespassers - Clues To Superficial MycosisDocument5 paginiTelltale Signs of Skin Trespassers - Clues To Superficial Mycosiskahkashanahmed065Încă nu există evaluări
- Management of Tinea Capitis in ChildhoodDocument26 paginiManagement of Tinea Capitis in ChildhoodSandra aneeÎncă nu există evaluări
- 4 DermatophytesDocument40 pagini4 DermatophytesGeoemilia1Încă nu există evaluări
- Superficial and Cutaneous Mycoses: 2. Disease CharacteristicsDocument4 paginiSuperficial and Cutaneous Mycoses: 2. Disease CharacteristicsMA. ANGELI DELA CRUZÎncă nu există evaluări
- Common Causes of Paediatric Alopecia: EpidemiologyDocument5 paginiCommon Causes of Paediatric Alopecia: EpidemiologyLiya SuwarniÎncă nu există evaluări
- Mycology 2019Document8 paginiMycology 2019Angellie100% (1)
- A Single Typical Trichoscopic Feature Is Predictive of Tinea Capitis: A Prospective Multicentre StudyDocument6 paginiA Single Typical Trichoscopic Feature Is Predictive of Tinea Capitis: A Prospective Multicentre StudyRose ParkÎncă nu există evaluări
- (FreeCourseWeb - Com) Dr. Sebi Hair Growth - Alk...Document42 pagini(FreeCourseWeb - Com) Dr. Sebi Hair Growth - Alk...Toni trejder100% (2)
- Dermatology Mini-OSCEDocument322 paginiDermatology Mini-OSCEMarrkÎncă nu există evaluări
- Derma EAMC ReviewerDocument25 paginiDerma EAMC ReviewerJanna Janoras ŰÎncă nu există evaluări