Documente Academic
Documente Profesional
Documente Cultură
Clinical Differences Among Four Common Dementias
Încărcat de
Isaac EliasDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Clinical Differences Among Four Common Dementias
Încărcat de
Isaac EliasDrepturi de autor:
Formate disponibile
Clinical Differences Among Four Common Dementia Syndromes
Posted 10/25/2007
Weerasak Muangpaisan Author Information
Abstract
Cases of dementia are increasing due to longer life expectancy of the world population. Physicians should be able to recognize common dementia syndromes. After excluding reversible causes of dementia, there are four common dementia syndromes, which are Alzheimer's disease, vascular dementia, dementia with Lewy body, and frontotemporal dementia. The key points of clinical differences of these dementia syndromes are summarized in this article.
Introduction
There are four clinical dementia syndromes accounting for 90% of all cases after excluding other common reversible causes of cognitive impairment.[1] These four major diseases are Alzheimer's disease (AD) and vascular dementia (VaD), which together account for approximately 80% of dementias, dementia with Lewy body (DLB), and frontotemporal dementia (FTD). The four common diseases have different clinical characteristics, and there are diagnostic criteria for each of them. These criteria bear review as physicians who deal with dementia might not always recall them in detail. As AD is the most common cause of dementia, accounting for 50-60% of cases, physicians should be familiar with the clinical difference between AD and other diseases.[2,3] This article will focus on the clinical difference between AD and other common dementia syndromes Alzheimer's Disease A 70-year-old man presented with a 3-year history of progressive memory loss, which mainly affected his short term memory. He needed his daughter to remind him of his appointments and some day-to-day activities. He had problems with driving alone as he became confused with the routes, though he had used them for a long time. He could not manage his bills as usual. The physical examination was unremarkable. The Mini Mental State Examination (MMSE) was 20 out of 30. Alzheimer's disease is the most common cause of dementia among older adults. The major pathogenesis is the production and accumulation of beta-amyloid peptide, bringing about the formation of neurofibrillary tangles, oxidation and lipid peroxidation, glutaminergic excitotoxicity, inflammation, and activation of the cascade of apoptotic cell death. Furthermore, the other hypothesis regarding the pathophysiology of AD stresses tau-protein abnormalities, heavy metals, vascular factors, and viral infections. [4] The natural course of AD averages 10 years. The cardinal features are insidious onset, progressive course, and early memory loss; at least one other cognitive impairment such as language dysfunction, apraxia, agnosia, visuospatial disorder, as well as executive dysfunction, must be seen. These impairments should constitute a decline from the previous level of cognitive functioning, interfering with daily activities. Memory decline is the hallmark of cognitive change in AD. It is characterized as a storage deficit, meaning that material cannot be recalled with cue. In the early stage, memory impairment for recent events is common whereas long-term memory remains intact. As the disease progresses, individuals with AD are increasingly unable to recall more distant memories. Typically, the motor signs are absent early in the course. Likewise, sensory abnormalities, seizures, and gait difficulties are uncommon until the late phase of disease.[2,4] Behavioural changes, including depression, anxiety, apathy, aggression, agitation, wandering, vocalization, disinhibition, and abnormal eating, are common thereafter and cause caregiver stress as well as greater use of health care service.[5] Vascular Dementia A 65-year-old man with hypertension, diabetes mellitus, and coronary artery disease developed sudden left hemiparesis and dysarthria 6 months ago. Three months later, his wife noticed that he could not name the only two grandchildren he had and could not remember to take his medications. He could neither operate a remote control nor cook meals as usual. On examination, there was only slight pronator drift on his left arm and hyperreflexia of the left extremities. There are several clinical syndromes of vascular dementia (VaD), which are categorized into multi-infarct dementia, single strategic infarct (single brain infarct damaging functionally critical areas of the brain such as angular gyrus, thalamus, basal forebrain, posterior cerebral artery, and anterior cerebral artery territories), lacunar state, Binswanger's disease, genetic forms (e.g., cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy [CADASIL]), and hypoxic ischemic encephalopathy.[6-8] A number of mechanisms causing these clinical syndromes are hemorrhage, ischemia/thrombosis, vasospasm, low perfusion, hematologic and rheological problems. Since cases do not share common etiology and mechanism, patients may have different clinical presentations. For example, the onset may be abrupt or insidious. The progression may be stepwise, fluctuating, or marked by continuous worsening. [9-11] Frequently, individuals with VaD present with gradual and progressive cognitive decline without any stroke events. However, typical cases of VaD are usually seen with atherosclerotic comorbidities (diabetes mellitus, hypertension, coronary heart disease, and peripheral artery disease). The onset of cognitive decline is either subtle or abrupt, and there is psychomotor slowing, executive dysfunction, focal cognitive deficits and motor signs. The temporal association between the cerebrovascular event and the onset of dementia should be within 3 months. Nevertheless, as VaD is variable, sometimes the temporal association cannot be demonstrated easily due to an unclear onset of vascular event. Table 1 summarizes the clinical characteristics of AD and VaD. Dementia With Lewy Bodies A 72-year-old man with a 6-month history of cognitive impairment and visual hallucination presented to an emergency room after repeated falls a few days ago. His wife felt that he had been slow in thinking, speaking, and performing his routine activities for a few months. On examination, he had bilateral rigidity, parkinsonian gait, and masked face. No history of medication could be elicited. Dementia with Lewy bodies (DLB) is a clinically defined syndrome and is claimed to be the second most common type of degenerative dementia among older adults, accounting for 10-15% of cases at autopsy. The criteria for diagnosis of DLB are highly specific but not sensitive. Core clinical features are fluctuating cognitive impairment (50-75%), visual hallucinations, and parkinsonism (seen in 25-50% of patients at diagnosis). [12] Its supportive features are repeated falls, syncope, transient loss of consciousness, neuroleptic sensitivity, systematized delusion, hallucination of other modalities, REM sleep behaviour disorder, and depression. Physicians frequently encounter patients with dementia and parkinsonism, and a number of differential diagnoses should be raised such as multi-infarct dementia, normal pressure hydrocephalus, and Parkinson-plus syndrome.
In terms of making a diagnosis, the two most confusing diseases are DLB and Parkinson's disease with dementia (PDD) because the clinical features are similar. There are some clinical manifestations used to separate these two similar neuropathologic diseases. First, the temporal course of the disease is always used to distinguish these two overlapping syndromes. If the onset of dementia is within 12 months of parkinsonism's onset, it is likely to be DLB. By contrast, if the onset of parkinsonism is more than 12 months earlier than dementia onset, it should be PDD. Secondly, individuals with DLB usually have extrapyramidal signs in axial structures such as postural instability and masked face, whereas tremor is less prominent than among those with PDD. Finally, all individuals with PDD have parkinsonian features at the time of dementia diagnosis, whereas only 25-50% of those with DLB have parkinsonism at the time of diagnosis. However, 80-100% of individuals with DLB develop some parkinsonism during its natural course.[13] Potential predictors for the development of cognitive decline and dementia in PD include older age at the onset of motor symptoms, bradykinesis, akinetic-rigid parkinsonism, bilateral onset of parkinsonism, depression, early visual hallucinations, and declining response to levodopa. The clinical differences between DLB and AD are shown in Table 2 and the clinical differences of DLB and PDD are presented in Table 3. Frontotemporal Dementia A 50-year-old woman presented with behavioural change over the course of two years. She had less concentration to accomplish her assigned tasks and was less responsible to her job. She had begun eating more and had gained 20 pounds in 5 months. She told lies and dirty jokes, stole office stationary, and picked up objects within reach and sight. She had poor personal hygiene and refused to take a bath. Apart from grasp, and palmomental reflexes, the physical examination did not reveal any other abnormality. Her MMSE was 29/30, but her performance on the clock drawing test was poor. The clinical features of frontotemporal dementia (FTD) are described with the emphasis on prominent personality and behavioural changes with less prominent memory loss early in the course ( Table 4 ).[14-16] Frequently, FTD is misdiagnosed as personality disorders or late-onset psychiatric disorders. Common behaviour and conduct disturbances are loss of personal awareness, loss of social comportment, disinhibition, impulsivity, distractibility, hyperorality (e.g., excessive eating), social withdrawal, stereotyped or preservative behaviour, and speech output change (e.g., reduction of speech, stereotype of speech, and echolalia). The physical examination usually reveals early prominent primitive or frontal reflexes. One-half of patients have a family history of dementia in a first-degree relative. There are three principal varieties of FTD: frontal variant FTD, semantic dementia, and progressive nonfluent aphasia.[17] Physicians usually misdiagnose FTD if semantic dementia and progressive nonfluent aphasia are present because these two subtypes do not have prominent behavioural or personality disturbance like the frontal variant FTD. Conclusion Failure to recognize dementia syndromes remains common. Different types of dementia require different approaches and management. Among a long list of the differential diagnosis of dementia, four common diseases (Alzheimer's disease, vascular dementia, dementia with Lewy bodies, and frontotemporal dementia should come to mind just from the history, physical examination, and simple neuropsychological batteries. Further investigations may be needed to confirm the provisional diagnosis and rule out some mimics in complicated cases.
S-ar putea să vă placă și
- Neurocognitive DisordersDocument26 paginiNeurocognitive Disordershaidar aliÎncă nu există evaluări
- Dementia Tri Fold BrochureDocument2 paginiDementia Tri Fold BrochurePamela McCabeÎncă nu există evaluări
- Guidelines Dementia Age Related Cognitive ChangeDocument32 paginiGuidelines Dementia Age Related Cognitive ChangeFernanda Keren de PaulaÎncă nu există evaluări
- Abpsych ReviewerDocument17 paginiAbpsych ReviewerAGNER JASMIN ROSE L.Încă nu există evaluări
- Cognitive DisordersDocument3 paginiCognitive DisordersKayze UbaldoÎncă nu există evaluări
- Outline and evaluate the working memory model (40Document20 paginiOutline and evaluate the working memory model (40Srnt YyoÎncă nu există evaluări
- Dementia Symptoms ChecklistDocument16 paginiDementia Symptoms ChecklistAnand Prakash SinghÎncă nu există evaluări
- Neuro Behavior DisordersDocument80 paginiNeuro Behavior Disordersmohamadafif_drÎncă nu există evaluări
- MSE of Uncooperative PTDocument16 paginiMSE of Uncooperative PTGurvinder KalraÎncă nu există evaluări
- CH 4 Psychological DisordersDocument1 paginăCH 4 Psychological DisordersKshitij DasariÎncă nu există evaluări
- Lab TestsDocument1 paginăLab TestsnkivcÎncă nu există evaluări
- Geriatrics 2023 FinalDocument119 paginiGeriatrics 2023 FinalBelinda ELISHAÎncă nu există evaluări
- SUICIDEDocument29 paginiSUICIDERizwan ZafarÎncă nu există evaluări
- Understanding Depression: Helping Families & Friends Find Better WaysDocument4 paginiUnderstanding Depression: Helping Families & Friends Find Better WaysRajAnandÎncă nu există evaluări
- EmotionalDocument7 paginiEmotionalapi-367611011Încă nu există evaluări
- Neuro Notes UWDocument91 paginiNeuro Notes UWM.DalaniÎncă nu există evaluări
- What Is Mental Health?: Risk FactorsDocument2 paginiWhat Is Mental Health?: Risk FactorsElmaRabagoÎncă nu există evaluări
- GlossaryDocument8 paginiGlossarysnejinka1979Încă nu există evaluări
- Why Do Teens Consider Suicide (EAPP)Document5 paginiWhy Do Teens Consider Suicide (EAPP)michaellamigas04Încă nu există evaluări
- Mental Status Exam ERICDocument3 paginiMental Status Exam ERICDesiree AfagaÎncă nu există evaluări
- Common Uses For MBTI IncludeDocument8 paginiCommon Uses For MBTI IncludeRocker byÎncă nu există evaluări
- Acquired Brain Injury - The Facts - Forth Edition 2013Document45 paginiAcquired Brain Injury - The Facts - Forth Edition 2013rach2791100% (1)
- Mental Disorders: Key FactsDocument9 paginiMental Disorders: Key Factssoshi2691loveÎncă nu există evaluări
- General Definition, Causes, and Types of Mental IllnessDocument6 paginiGeneral Definition, Causes, and Types of Mental Illnesszahra03762Încă nu există evaluări
- Recovery Model HandoutDocument2 paginiRecovery Model HandoutRosalie Lotspeich100% (1)
- AP Psych Unit 4 VocabDocument3 paginiAP Psych Unit 4 Vocabdittman1430Încă nu există evaluări
- 312-Ops Asd Autism Parents Q and A BookletDocument16 pagini312-Ops Asd Autism Parents Q and A Bookletapi-233394844Încă nu există evaluări
- Fragmento Nonverbal-Stroop-Card-Sorting-Test-NSCST-Manual-SampleDocument7 paginiFragmento Nonverbal-Stroop-Card-Sorting-Test-NSCST-Manual-SampleTrinidad Farías PiñeiroÎncă nu există evaluări
- Suicide: Risk Factors, Assessment, Methodological Problems: Sweta Sheth Chair: Dr. Rajesh GopalakrishnanDocument59 paginiSuicide: Risk Factors, Assessment, Methodological Problems: Sweta Sheth Chair: Dr. Rajesh GopalakrishnanpriyagerardÎncă nu există evaluări
- Nervous System Disorders PPT 3 1Document9 paginiNervous System Disorders PPT 3 1Camille Joy BaliliÎncă nu există evaluări
- Summary of Terms - PsychDocument13 paginiSummary of Terms - Psychapi-642709499Încă nu există evaluări
- Neurocognitive Differential Diagnosis of Dementing Diseases - Alzheimer's Dementia, Vascular Dementia, Frontotemporal Dementia, and Major Depressive DisorderDocument23 paginiNeurocognitive Differential Diagnosis of Dementing Diseases - Alzheimer's Dementia, Vascular Dementia, Frontotemporal Dementia, and Major Depressive DisorderryrihelmiÎncă nu există evaluări
- CHAPTER 4 - NotesDocument5 paginiCHAPTER 4 - NotesAquamsha FahimÎncă nu există evaluări
- Free Trade, Protectionism, International Trade Theories, and Balance of PaymentsDocument25 paginiFree Trade, Protectionism, International Trade Theories, and Balance of PaymentsPravin AjaazÎncă nu există evaluări
- Neck Pain Headache: Brain Diseases: InfectionsDocument2 paginiNeck Pain Headache: Brain Diseases: Infectionsv@r0_5Încă nu există evaluări
- Rating Scales for Assessing Bipolar Disorder SymptomsDocument14 paginiRating Scales for Assessing Bipolar Disorder SymptomsDivia RainaÎncă nu există evaluări
- SchizophreniaDocument2 paginiSchizophreniaIT’S ME HAYLA100% (1)
- Models of Abnormality in PsychopathologyDocument18 paginiModels of Abnormality in PsychopathologyGift MwapeÎncă nu există evaluări
- Symptoms: Following SignsDocument3 paginiSymptoms: Following SignsAhmed FaidÎncă nu există evaluări
- Jose Gerardo Los Baños, M.D.: Topic OutlineDocument15 paginiJose Gerardo Los Baños, M.D.: Topic OutlineMaikka IlaganÎncă nu există evaluări
- Wikipedia: The Act or An Instance of Taking One's Own Life Voluntarily and IntentionallyDocument9 paginiWikipedia: The Act or An Instance of Taking One's Own Life Voluntarily and Intentionallysubham kumarÎncă nu există evaluări
- Psychiatric Charting EssentialsDocument7 paginiPsychiatric Charting EssentialsMeryville JacildoÎncă nu există evaluări
- Mental and Emotional HealthDocument2 paginiMental and Emotional HealthEden LacsonÎncă nu există evaluări
- V Adhd D T R S: Anderbilt Iagnostic Eacher Ating CaleDocument2 paginiV Adhd D T R S: Anderbilt Iagnostic Eacher Ating CaletraviscÎncă nu există evaluări
- What Exactly Is A Mental IllnessDocument2 paginiWhat Exactly Is A Mental IllnessEllee Hades100% (1)
- Outpatient Referral Guidelines: NeurosurgeryDocument11 paginiOutpatient Referral Guidelines: NeurosurgeryYuvraj Chauhan100% (1)
- Emotional Disorders and Physical IllnessDocument56 paginiEmotional Disorders and Physical IllnesssamuelÎncă nu există evaluări
- OpenDocument25 paginiOpenKatya KatyaÎncă nu există evaluări
- Feeding and Eating DisordersDocument73 paginiFeeding and Eating DisordersMAYLENE CUENCOÎncă nu există evaluări
- DFS Gender Dysphoria LetterDocument3 paginiDFS Gender Dysphoria LetterMatthew HamiltonÎncă nu există evaluări
- Developing Images: Mind Development, Hallucinations and All Mind Disorders Including AutismDe la EverandDeveloping Images: Mind Development, Hallucinations and All Mind Disorders Including AutismÎncă nu există evaluări
- Neuropsychology Bordeline Personality RDocument5 paginiNeuropsychology Bordeline Personality RJennie VargasÎncă nu există evaluări
- Schizo ToolDocument3 paginiSchizo Toolsherell220Încă nu există evaluări
- Myths and Facts About Mental Health 022007Document2 paginiMyths and Facts About Mental Health 022007Jemimah AlobaÎncă nu există evaluări
- Understanding Psychological DisordersDocument148 paginiUnderstanding Psychological Disordersmax lifeÎncă nu există evaluări
- Unit 5 Common Types of Mental IllnessDocument64 paginiUnit 5 Common Types of Mental IllnessNur Hazirah SadonÎncă nu există evaluări
- Mental Health Assessment Task - 2017Document14 paginiMental Health Assessment Task - 2017api-356887355Încă nu există evaluări
- Mental Health Check in Tip SheetDocument3 paginiMental Health Check in Tip SheetDiana SamÎncă nu există evaluări
- PSYCH 9 Reviewer - Chapter 7 Mood Disorders and SuicideDocument5 paginiPSYCH 9 Reviewer - Chapter 7 Mood Disorders and SuicideJoelle Marie GarciaÎncă nu există evaluări
- Diamond Kirkham AmsoDocument11 paginiDiamond Kirkham AmsoIsaac EliasÎncă nu există evaluări
- Artigo Com Tabelas HVLT e BVMTDocument4 paginiArtigo Com Tabelas HVLT e BVMTMaria CristinaÎncă nu există evaluări
- MBSR Vs Aerobic ExerciseDocument8 paginiMBSR Vs Aerobic ExerciseIsaac EliasÎncă nu există evaluări
- Effects of MindfulnessDocument21 paginiEffects of MindfulnessIsaac EliasÎncă nu există evaluări
- Why We Forget and How To RememberDocument6 paginiWhy We Forget and How To RememberTope Georges-Emmanuel100% (1)
- MascDocument14 paginiMascIsaac EliasÎncă nu există evaluări
- 10 Jeitos para Prevenir AlzheimerDocument6 pagini10 Jeitos para Prevenir AlzheimerIsaac EliasÎncă nu există evaluări
- Coloring Book For Web - 3.20.2020 - 1Document17 paginiColoring Book For Web - 3.20.2020 - 1Paulo Sergio SilvaÎncă nu există evaluări
- Cognitive Processes Mediate The Relation Betweein MindfulnessDocument10 paginiCognitive Processes Mediate The Relation Betweein MindfulnessIsaac EliasÎncă nu există evaluări
- Cap 18 Habilidades SociaisDocument22 paginiCap 18 Habilidades SociaisIsaac EliasÎncă nu există evaluări
- Development of Symbolic Play Trough The Use of VirtualDocument16 paginiDevelopment of Symbolic Play Trough The Use of VirtualIsaac EliasÎncă nu există evaluări
- Compulsão e ImpulsividadeDocument8 paginiCompulsão e ImpulsividadeIsaac EliasÎncă nu există evaluări
- We Are About To Cure MS in The Nest 10 Years Even Though We Do Not Know Its Cause NODocument4 paginiWe Are About To Cure MS in The Nest 10 Years Even Though We Do Not Know Its Cause NOIsaac EliasÎncă nu există evaluări
- Postgraduate Medicine Is It Alzheimer's Disease or Something ElseDocument7 paginiPostgraduate Medicine Is It Alzheimer's Disease or Something ElseIsaac EliasÎncă nu există evaluări
- Memory ImproverDocument1 paginăMemory ImproverIsaac EliasÎncă nu există evaluări
- Demencia FrontotemporalDocument10 paginiDemencia FrontotemporalIsaac EliasÎncă nu există evaluări
- Cognitive Function and Quality of Life in Ms Patients - A Cross - Sectional StudyDocument10 paginiCognitive Function and Quality of Life in Ms Patients - A Cross - Sectional StudyIsaac EliasÎncă nu există evaluări
- Increased Cerebral Activation After Behavioral Treatment For Memory Deficits in MsDocument10 paginiIncreased Cerebral Activation After Behavioral Treatment For Memory Deficits in MsIsaac EliasÎncă nu există evaluări
- Journal Pone 0020835Document10 paginiJournal Pone 0020835Christine BookmanÎncă nu există evaluări
- Converging Evidente For Triple Word Form Theory in Children With DyslexiaDocument43 paginiConverging Evidente For Triple Word Form Theory in Children With DyslexiaIsaac EliasÎncă nu există evaluări
- Transcendentalism EssayDocument4 paginiTranscendentalism Essayapi-248448724Încă nu există evaluări
- 2022-23 Registrar's Handbook FINALDocument77 pagini2022-23 Registrar's Handbook FINALicikapt registrarÎncă nu există evaluări
- Instrument Music Lesson Plan: KindergartenDocument4 paginiInstrument Music Lesson Plan: Kindergartenapi-510351548Încă nu există evaluări
- CSC 520 AI 2018 Spring SyllabusDocument7 paginiCSC 520 AI 2018 Spring SyllabusscribdfuckuÎncă nu există evaluări
- PHED 111 HealthDocument19 paginiPHED 111 HealthApril Ann HortilanoÎncă nu există evaluări
- BUS 102 Fundamentals of Buiness II 2022Document4 paginiBUS 102 Fundamentals of Buiness II 2022Hafsa YusifÎncă nu există evaluări
- Databaseplan 1Document3 paginiDatabaseplan 1api-689126137Încă nu există evaluări
- Demonstration FormDocument2 paginiDemonstration FormDomric Panunciar100% (1)
- Summary 6Document5 paginiSummary 6api-640314870Încă nu există evaluări
- Surgery Mind MapDocument4 paginiSurgery Mind MapioakasÎncă nu există evaluări
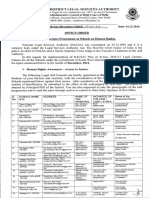
- Legal Awareness Programmes at Schools On Human RightsDocument2 paginiLegal Awareness Programmes at Schools On Human RightsSW-DLSAÎncă nu există evaluări
- Department of Education: Classroom Readiness ChecklistDocument3 paginiDepartment of Education: Classroom Readiness ChecklistL.V. BendañaÎncă nu există evaluări
- Lesson Plan SampleDocument7 paginiLesson Plan SampleSilvia RajeshÎncă nu există evaluări
- 2005 English Exam Assessment ReportDocument11 pagini2005 English Exam Assessment Reportpinkangel2868_142411Încă nu există evaluări
- Classroom Evaluation ChecklistDocument3 paginiClassroom Evaluation ChecklistAngelaLomagdong94% (18)
- ISAD - HW 2 Information Gathering Unobtrusive Methods Review QuestionsDocument3 paginiISAD - HW 2 Information Gathering Unobtrusive Methods Review QuestionsKathleen AgustinÎncă nu există evaluări
- Learning What is LearningDocument27 paginiLearning What is LearningShankerÎncă nu există evaluări
- 495 TextDocument315 pagini495 TextSaiful LahidjunÎncă nu există evaluări
- WARR The Measurement of Well-Being and Other Aspects of Mental HealthDocument19 paginiWARR The Measurement of Well-Being and Other Aspects of Mental HealthIqbal MehmoodÎncă nu există evaluări
- Modal verbs board gameDocument1 paginăModal verbs board gameEmmaBordetÎncă nu există evaluări
- 5E Lesson PlanDocument3 pagini5E Lesson PlanMarian Alvarado100% (1)
- Quantum Teaching For Educators (2 CR.)Document7 paginiQuantum Teaching For Educators (2 CR.)Cynthia IvanderÎncă nu există evaluări
- Materials Adaptation of Eap Materials - Part 2Document6 paginiMaterials Adaptation of Eap Materials - Part 2api-402780610Încă nu există evaluări
- Final Year Project Examination Time TableDocument7 paginiFinal Year Project Examination Time TableVid YashaÎncă nu există evaluări
- Erasmus Scholarship Guide-Ema NigeriaDocument31 paginiErasmus Scholarship Guide-Ema NigeriaMariana MolinaÎncă nu există evaluări
- 43 All India Conference of Dravidian LinguistsDocument6 pagini43 All India Conference of Dravidian LinguistsV N BHATTATHIRIÎncă nu există evaluări
- Part 6 Uasa Short Communicative Message - 1Document4 paginiPart 6 Uasa Short Communicative Message - 1Pearlyn LoÎncă nu există evaluări
- Biostats Exam Cheat SheetDocument2 paginiBiostats Exam Cheat SheetVauxswiftÎncă nu există evaluări
- Memory Engrams-Recalling The Past and Imagining The FutureDocument16 paginiMemory Engrams-Recalling The Past and Imagining The FutureluisÎncă nu există evaluări