Documente Academic
Documente Profesional
Documente Cultură
Burns - Airway Clearance, Risk For Ineffective
Încărcat de
makyofrancis20Descriere originală:
Titlu original
Drepturi de autor
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Burns - Airway Clearance, Risk For Ineffective
Încărcat de
makyofrancis20Drepturi de autor:
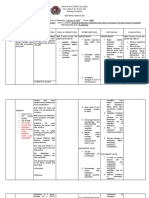
NURSING DIAGNOSIS: Airway Clearance, risk for ineffective Risk factors may include Tracheobronchial obstruction: mucosal edema
and loss of ciliary action (smoke inhalation); circumferential fullthickness burns of the neck, thorax, and chest, with compression of the airway or limited chest excursion Trauma: direct upper-airway injury by flame, steam, hot air, and chemicals/gases Fluid shifts, pulmonary edema, decreased lung compliance Possibly evidenced by [Not applicable; presence of signs and symptoms establishes an actual diagnosis.] DESIRED OUTCOMES/EVALUATION CRITERIAPATIENT WILL: Respiratory Status: Airway Patency (NOC) Demonstrate clear breath sounds, respiratory rate within normal range, be free of dyspnea/cyanosis.
ACTIONS/INTERVENTIONS
Respiratory Monitoring (NIC)
RATIONALE
Independent
Obtain history of injury. Note presence of preexisting respiratory conditions, history of smoking. Causative burning agent, duration of exposure, and occurrence in closed or open space predict probability of inhalation injury. Type of material burned (wood, plastic, wool, and so forth) suggests type of toxic gas exposure. Preexisting conditions increase the risk of respiratory complications. Suggestive of inhalation injury.
Assess gag/swallow reflexes; note drooling, inability to swallow, hoarseness, wheezy cough. Monitor respiratory rate, rhythm, depth; note presence of pallor/cyanosis and carbonaceous or pink-tinged sputum.
Tachypnea, use of accessory muscles, presence of cyanosis, and changes in sputum suggest developing respiratory distress/pulmonary edema and need for medical intervention. Airway obstruction/respiratory distress can occur very quickly or may be delayed, e.g., up to 48 hr after burn. Suggests presence of hypoxemia or carbon monoxide.
Auscultate lungs, noting stridor, wheezing/crackles, diminished breath sounds, brassy cough. Note presence of pallor or cherry-red color of unburned skin. Investigate changes in behavior/mentation, e.g., restlessness, agitation, confusion.
Although often related to pain, changes in consciousness may reflect developing/worsening hypoxia.
ACTIONS/INTERVENTIONS
Respiratory Monitoring (NIC)
RATIONALE
Independent
Monitor 24-hr fluid balance, noting variations/changes. Fluid shifts or excess fluid replacement increases risk of pulmonary edema. Note: Inhalation injury increases fluid demands as much as 35% or more because of obligatory edema.
Airway Management (NIC) Elevate head of bed. Avoid use of pillow under head, as indicated. Promotes optimal lung expansion/respiratory function. When head/neck burns are present, a pillow can inhibit respiration, cause necrosis of burned ear cartilage, and promote neck contractures. Promotes lung expansion, mobilization and drainage of secretions. Helps maintain clear airway, but should be done cautiously because of mucosal edema and inflammation. Sterile technique reduces risk of infection. Increasing hoarseness/decreased ability to swallow suggests increasing tracheal edema and may indicate need for prompt intubation.
Encourage coughing/deep-breathing exercises and frequent position changes. Suction (if necessary) with extreme care, maintaining sterile technique.
Promote voice rest, but assess ability to speak and/or swallow oral secretions periodically.
Collaborative
Administer humidified oxygen via appropriate mode, e.g., face mask. O2 corrects hypoxemia/acidosis. Humidity decreases drying of respiratory tract and reduces viscosity of sputum. Baseline is essential for further assessment of respiratory status and as a guide to treatment. Pao2 less than 50, Paco2 greater than 50, and decreasing pH reflect smoke inhalation and developing pneumonia/ARDS. Changes reflecting atelectasis/pulmonary edema may not occur for 23 days after burn. Chest physiotherapy drains dependent areas of the lung, and incentive spirometry may be done to improve lung expansion, thereby promoting respiratory function and reducing atelectasis. Intubation/mechanical support is required when airway edema or circumferential burn injury interferes with respiratory function/oxygenation.
Monitor/graph serial ABGs or pulse oximetry.
Review serial chest x-rays.
Provide/assist with chest physiotherapy and incentive spirometry.
Prepare for/assist with intubation or tracheostomy, as indicated.
S-ar putea să vă placă și
- NCP Ineffective Airway Clearance Related To Presence of Secretion in Trachea-Bronchial Tree Secondary To History of CAPDocument2 paginiNCP Ineffective Airway Clearance Related To Presence of Secretion in Trachea-Bronchial Tree Secondary To History of CAPpa3kmedina100% (1)
- NCP #2Document4 paginiNCP #2Nutz TolentinoÎncă nu există evaluări
- Burn NCPDocument4 paginiBurn NCPregÎncă nu există evaluări
- NCP - Ineffective Airway ClearanceDocument4 paginiNCP - Ineffective Airway ClearanceKim Gabrielle Exene LeeÎncă nu există evaluări
- NCP-Difficulty of Breathing Related To Presence of Phlegm and Always CoughingDocument3 paginiNCP-Difficulty of Breathing Related To Presence of Phlegm and Always CoughingCedie BarcaÎncă nu există evaluări
- Deficit)Document2 paginiDeficit)Lee DeeÎncă nu există evaluări
- Burns - Fluid Volume, Risk For DeficientDocument3 paginiBurns - Fluid Volume, Risk For Deficientmakyofrancis20Încă nu există evaluări
- NCP PainDocument2 paginiNCP PainApril_Ivy_Raga_3835Încă nu există evaluări
- HTP of AsthmaDocument1 paginăHTP of AsthmaMarland Faith Dela CruzÎncă nu există evaluări
- NCPDocument3 paginiNCPJezza RequilmeÎncă nu există evaluări
- NCP FVDDocument1 paginăNCP FVDsisjing88510Încă nu există evaluări
- Nursing Care PlanDocument11 paginiNursing Care Planaycee0316100% (1)
- Nueva Ecija University of Science and TechnologyDocument7 paginiNueva Ecija University of Science and TechnologyKym RonquilloÎncă nu există evaluări
- Risk For InfectionDocument1 paginăRisk For InfectionEuanne OrellanoÎncă nu există evaluări
- Stevens Johnson Syndrome CASEDocument53 paginiStevens Johnson Syndrome CASEKathrina CraveÎncă nu există evaluări
- Glaucoma NCPDocument4 paginiGlaucoma NCPChantal CaraganÎncă nu există evaluări
- Aubrey Rose A. Vidon BSN 3Y1 - 2Document2 paginiAubrey Rose A. Vidon BSN 3Y1 - 2Aria100% (1)
- 6639burn NCPDocument18 pagini6639burn NCPDivina Grace Renon Camba100% (1)
- Decrease Cardiac OutputDocument6 paginiDecrease Cardiac OutputGerardeanne ReposarÎncă nu există evaluări
- 10 CaritosDocument3 pagini10 CaritosDARREN EDMARK100% (4)
- Nursing Care PlanDocument4 paginiNursing Care Planapi-309251523Încă nu există evaluări
- Case Study ReportDocument23 paginiCase Study Reportapi-290866384Încă nu există evaluări
- NCP For CHF 3 Activity IntoleranceDocument2 paginiNCP For CHF 3 Activity IntoleranceAngelyn ArdinesÎncă nu există evaluări
- Ineffective Breathing PatternDocument3 paginiIneffective Breathing PatternErickson OcialÎncă nu există evaluări
- Concept Map - Abby !Document2 paginiConcept Map - Abby !Abegail Abaygar100% (3)
- Nursing Care PlanDocument5 paginiNursing Care Planruggero07100% (2)
- Scribd 020922 Case Study-Oncology A&kDocument2 paginiScribd 020922 Case Study-Oncology A&kKellie DÎncă nu există evaluări
- NCP AidsDocument16 paginiNCP AidstferdianingsihÎncă nu există evaluări
- COLCHICINE pptx1800128929Document15 paginiCOLCHICINE pptx1800128929April Mergelle LapuzÎncă nu există evaluări
- Nursing 215 Care Plan 2 FinalDocument7 paginiNursing 215 Care Plan 2 Finalapi-283303129Încă nu există evaluări
- NCPDocument3 paginiNCPArien CaleonÎncă nu există evaluări
- 14 Cerebrovascular Accident Nursing Care PlansDocument5 pagini14 Cerebrovascular Accident Nursing Care PlansNickesha Mckenzie75% (4)
- NCP Inffective Tissue PerfusionDocument3 paginiNCP Inffective Tissue PerfusionPaul Cubacub0% (1)
- NCPDocument3 paginiNCPErica Denice CastilloÎncă nu există evaluări
- Compartment Syndrome NCP (PAIN)Document2 paginiCompartment Syndrome NCP (PAIN)eunica16Încă nu există evaluări
- Assessment Diagnosis Planning Implementation Rationale EvaluationDocument14 paginiAssessment Diagnosis Planning Implementation Rationale EvaluationJennifer ArdeÎncă nu există evaluări
- As Needed.: Environmental Stimuli 6Document4 paginiAs Needed.: Environmental Stimuli 6Nicole GumolonÎncă nu există evaluări
- Hypokalemia NCP PDFDocument4 paginiHypokalemia NCP PDFMussaib MushtaqÎncă nu există evaluări
- NCM 118L/ 119L (Related Learning Experience) Day 3-ActivityDocument4 paginiNCM 118L/ 119L (Related Learning Experience) Day 3-ActivityNicole Villanueva, BSN - Level 3AÎncă nu există evaluări
- Case Scenario (Pedia)Document2 paginiCase Scenario (Pedia)Hamima Azis PandapatanÎncă nu există evaluări
- NCP - Ineffective Tissue PerfusionDocument2 paginiNCP - Ineffective Tissue PerfusionIan RamaÎncă nu există evaluări
- NCP CKDDocument3 paginiNCP CKDRiel TumandaÎncă nu există evaluări
- NCP MiDocument4 paginiNCP MiPitaca Madiam Annabehl PaulÎncă nu există evaluări
- Pain NCP BillrothDocument2 paginiPain NCP BillrotharjayÎncă nu există evaluări
- Subjective Cues: Independent: On The: "Nahihirapa N Ako Huminga" AsDocument5 paginiSubjective Cues: Independent: On The: "Nahihirapa N Ako Huminga" AsYessaminÎncă nu există evaluări
- SOMBILLO Scenario 1 ANGINADocument2 paginiSOMBILLO Scenario 1 ANGINAKarla SombilloÎncă nu există evaluări
- Cues Nursing Diagnosis Scientific Reason Objective Nursing Intervention Rationale EvaluationDocument4 paginiCues Nursing Diagnosis Scientific Reason Objective Nursing Intervention Rationale Evaluationjomsportg0% (1)
- NCP ModsDocument5 paginiNCP ModsKirstin del CarmenÎncă nu există evaluări
- Nursing Care Plan: Congestive Heart Failure-Deep Vein ThrombosisDocument19 paginiNursing Care Plan: Congestive Heart Failure-Deep Vein ThrombosisRiza Angela BarazanÎncă nu există evaluări
- Ineffective Airway ClearanceDocument6 paginiIneffective Airway Clearanceapi-252726911Încă nu există evaluări
- NCP For Rapid Shallow BreathingDocument1 paginăNCP For Rapid Shallow Breathingbamboo2dÎncă nu există evaluări
- Diarrhea Care PlanDocument2 paginiDiarrhea Care Planzepoli_zepoly6232100% (1)
- Cu 5Document2 paginiCu 5Clareze AbadÎncă nu există evaluări
- Drug Study GuideDocument2 paginiDrug Study GuideAubrey Sunga100% (1)
- Burns NCPDocument3 paginiBurns NCPKristian Jonas Lao0% (1)
- Burns - Tissue Perfusion, IneffectiveDocument3 paginiBurns - Tissue Perfusion, Ineffectivemakyofrancis20100% (1)
- 2nd Lecture Chest and LowerDocument18 pagini2nd Lecture Chest and LowerChucky VergaraÎncă nu există evaluări
- NCP 1 Ineffective Airway ClearanceDocument2 paginiNCP 1 Ineffective Airway ClearanceDivine Jane PurciaÎncă nu există evaluări
- CopdDocument4 paginiCopdapi-3739910100% (2)
- Scenario 5: Group 6Document51 paginiScenario 5: Group 6Gd SuarantaÎncă nu există evaluări
- Burns - Tissue Perfusion, IneffectiveDocument3 paginiBurns - Tissue Perfusion, Ineffectivemakyofrancis20100% (1)
- Peritoneal DialysisDocument23 paginiPeritoneal Dialysismakyofrancis20Încă nu există evaluări
- Burns - Skin Integrity, ImpairedDocument2 paginiBurns - Skin Integrity, Impairedmakyofrancis20Încă nu există evaluări
- Burns - Fluid Volume, Risk For DeficientDocument3 paginiBurns - Fluid Volume, Risk For Deficientmakyofrancis20Încă nu există evaluări
- Burns - Infection, Risk ForDocument4 paginiBurns - Infection, Risk Formakyofrancis20Încă nu există evaluări
- Burns - Knowledge, DeficientDocument2 paginiBurns - Knowledge, Deficientmakyofrancis20Încă nu există evaluări
- NURSING DIAGNOSIS: Fear/Anxiety May Be Related To: Actions/Interventions RationaleDocument2 paginiNURSING DIAGNOSIS: Fear/Anxiety May Be Related To: Actions/Interventions Rationalemakyofrancis20Încă nu există evaluări
- RENAL DIALYSIS - Self-Care Deficit (Specify)Document1 paginăRENAL DIALYSIS - Self-Care Deficit (Specify)makyofrancis20Încă nu există evaluări
- Burns: Thermal/Chemical/Electrical (Acute and Convalescent Phases)Document4 paginiBurns: Thermal/Chemical/Electrical (Acute and Convalescent Phases)makyofrancis20Încă nu există evaluări
- RENAL DIALYSIS - Thought Processes, Risk For DisturbedDocument2 paginiRENAL DIALYSIS - Thought Processes, Risk For Disturbedmakyofrancis20Încă nu există evaluări
- RENAL DIALYSIS - Nutrition, Imbalanced, Less Than Body RequirementsDocument3 paginiRENAL DIALYSIS - Nutrition, Imbalanced, Less Than Body Requirementsmakyofrancis20Încă nu există evaluări
- Renal Dialysis: Care SettingDocument1 paginăRenal Dialysis: Care Settingmakyofrancis20Încă nu există evaluări
- RENAL DIALYSIS - Mobility, Impaired PhysicalDocument2 paginiRENAL DIALYSIS - Mobility, Impaired Physicalmakyofrancis20Încă nu există evaluări
- SeizureDocument9 paginiSeizuremakyofrancis20Încă nu există evaluări
- 6th Central Pay Commission Salary CalculatorDocument15 pagini6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- Pathognomonic SignsDocument1 paginăPathognomonic Signsmakyofrancis20Încă nu există evaluări
- Atrial Arrhythmias Definition and Pathology Significance Etiology Clinical Manifestations InterventionDocument5 paginiAtrial Arrhythmias Definition and Pathology Significance Etiology Clinical Manifestations Interventionmakyofrancis20Încă nu există evaluări
- 40 Asthma DiaryDocument1 pagină40 Asthma DiaryMohammed MianÎncă nu există evaluări
- Spirometry (PPT & Words) 1Document5 paginiSpirometry (PPT & Words) 1Fluffyyy BabyyyÎncă nu există evaluări
- Patient-Ventilator AsynchronyDocument14 paginiPatient-Ventilator AsynchronyJavier Enrique Barrera PachecoÎncă nu există evaluări
- Respiratory Pastest NotesDocument10 paginiRespiratory Pastest NotesmuneebaÎncă nu există evaluări
- Kerry GomesDocument23 paginiKerry GomesAbegail IbañezÎncă nu există evaluări
- Meconium AspirationDocument7 paginiMeconium AspirationDelphy VargheseÎncă nu există evaluări
- Chest Physiotherapy or Techniques in Cardio Pulmonary Physiotherapy A Running CommentaryDocument5 paginiChest Physiotherapy or Techniques in Cardio Pulmonary Physiotherapy A Running CommentaryGopi KrishnanÎncă nu există evaluări
- Lung Parenchyma or Because of A Disease of The Pleura, Chest Wall, or Neuromuscular ApparatusDocument2 paginiLung Parenchyma or Because of A Disease of The Pleura, Chest Wall, or Neuromuscular ApparatusMarisha Christin TarihoranÎncă nu există evaluări
- Pneumothorax: ClinicalDocument5 paginiPneumothorax: ClinicalAlexander PazÎncă nu există evaluări
- NCP Rds 2Document1 paginăNCP Rds 2Angelokeizer Gavino0% (1)
- NCP - ANAPHYLACTIC SHOCK..2pdfDocument6 paginiNCP - ANAPHYLACTIC SHOCK..2pdfLycah RotoneÎncă nu există evaluări
- Bronchial AsthmaDocument46 paginiBronchial AsthmaKhor Kee GuanÎncă nu există evaluări
- Dyspnea and Pulmonary Edema: Harrison's 17 EditionDocument44 paginiDyspnea and Pulmonary Edema: Harrison's 17 EditionDizerine Mirafuentes RolidaÎncă nu există evaluări
- PPT HMDDocument60 paginiPPT HMDadityaÎncă nu există evaluări
- First Announcement Pdpi Update 1Document25 paginiFirst Announcement Pdpi Update 1sheeno2607Încă nu există evaluări
- NCP - Ineffective Breathing PatternDocument4 paginiNCP - Ineffective Breathing PatternPRINCESS KOBAYASHIÎncă nu există evaluări
- Critical Care Clinical Procedures 2023Document38 paginiCritical Care Clinical Procedures 2023nucahersheyskatÎncă nu există evaluări
- Principles of Chest Physiotherapy in ICUDocument42 paginiPrinciples of Chest Physiotherapy in ICUKapil Lakhwara100% (3)
- Journal Reading: Asma: Raden Muhamad HidayatDocument28 paginiJournal Reading: Asma: Raden Muhamad HidayatRaden Muhammad HidayatÎncă nu există evaluări
- Jadual Respiro 2021Document16 paginiJadual Respiro 2021yayayayayayayaÎncă nu există evaluări
- MCS 200 - 9 - Respiratory SystemDocument49 paginiMCS 200 - 9 - Respiratory SystemYotam MbaoÎncă nu există evaluări
- Trauma Thorax 2Document73 paginiTrauma Thorax 2----Încă nu există evaluări
- A Case Study On Malignant Pleural Effusion Secondary To Breast CancerDocument4 paginiA Case Study On Malignant Pleural Effusion Secondary To Breast Cancerpauline_almoÎncă nu există evaluări
- Pulmonary Function Test: By: Alfaro, Ruby Jane SDocument13 paginiPulmonary Function Test: By: Alfaro, Ruby Jane SgjevamÎncă nu există evaluări
- PneumothoraxDocument26 paginiPneumothoraxToni-Ann AllenÎncă nu există evaluări
- Capnography 1Document125 paginiCapnography 1tamikanjiÎncă nu există evaluări
- Presented by DR - Asha V Sasi 2 MD CR DeptDocument32 paginiPresented by DR - Asha V Sasi 2 MD CR DeptSariIdaMihartiÎncă nu există evaluări
- Vdocumentsmx - Pneumothorax-Referat-59217195d7a10 1Document7 paginiVdocumentsmx - Pneumothorax-Referat-59217195d7a10 1Vinna KusumawatiÎncă nu există evaluări
- Oxygen TherapyDocument8 paginiOxygen TherapyIndira MustafaÎncă nu există evaluări
- AssessmentDocument7 paginiAssessmentSheryhan Tahir BayleÎncă nu există evaluări