Documente Academic
Documente Profesional
Documente Cultură
Stuppy 2010 Blastocystis in Ibs Eradication With Nitazoxanide
Încărcat de
Nikola StojsicDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Stuppy 2010 Blastocystis in Ibs Eradication With Nitazoxanide
Încărcat de
Nikola StojsicDrepturi de autor:
Formate disponibile
disease with hepatocellular carcinoma (HCC). Microsporidial infection was positive on wet preparation in 8(2.7%), in 11(3.
7%) on Trichrome staining and in 13(4.3%) on PCR. Microsporidia was diagnosed with PCR in 8(61%) (p= 0.002) with IBS-D, 4(31%) with HCC and 1(8%) with functional dyspepsia. Conclusion: Microsporidial infection may be associated with IBS-D. PCR for microsporidia has a better yield than examination of a wet preparation or Trichrome staining
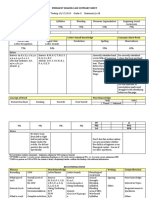
T1831 Do Caesarean Section and Birth Order in Twin Pairs Influence Development of IBS Later in Life May-Bente Bengtson, Jennifer R. Harris, Morten H. Vatn Background and aims: There is emerging evidence that previous gastrointestinal infection and persistent low-grade inflammation play an important role in the pathogenesis of at least a subset of patients with irritable bowel syndrome (IBS). We hypothesize that perinatal factors disturbing the gut colonization in newborn, might trigger an inflammatory response in the mucosa and thereby contribute to development of IBS later in life. Mode of delivery and birth order of twins within the pair might represent this group of perinatal factors. Earlier investigation of our population-based twin cohort has demonstrated that low birth weight increased the risk for development of IBS, with environmental factors in utero as the most relevant contributing factor. However, the analyses were not adjusted for possible perinatal confounders. Low birth weight is closely related to critical illness, perinatal infections and use of antibiotics, which all could influence the gut microflora of the newborn. In the present study we evaluated the association between IBS and perinatal factors including mode of delivery (caesarean versus vaginal) and birth order of twins within the pair. Methods: A postal questionnaire was sent in 1998 to 12700 Norwegian twins born between 1967 and 1979 who were identified from the Norwegian national birth registry, which was established in 1967. The questionnaire included a checklist of 31 illnesses and symptoms, including IBS. Results: In 321 twin pairs, at least one twin reported a positive history of IBS. Twenty four pairs were concordant, and 297 pairs were discordant for IBS. There was no link between caesarean section and IBS when tested by logistic regression in the full sample, adjusted for birth weight and gestational age (adjusted OR = 1.01, 95 % CI: 0.65, 1.55). The association between IBS and the first born (51.2 %) and the second born (48.8 %) twin in discordant twin pairs (285 pairs) was almost similar (OR = 0.91, 95 % CI: o.65, 1.26). Conclusion: The risk for development of IBS was not influenced by mode of delivery and birth order in twin pairs, suggesting that gut colonization is not important for IBS. T1832 Methanobrevibacter Smithii is Prominent in Stool of Subjects With Constipation Predominant IBS and Methane on Lactulose Breath Test Gene Kim, Stacy Weitsman, Jim Y. Chou, Janet Yang, Laura J. Hwang, Kimberly Low, Christopher Chang, Mark Pimentel Evidence supports the association between constipation and methane on breath testing. This association is more than casual since methane infusion in an animal model of transit results in a 70% slowing of intestinal transit. In a recent study of stool flora, Ruminococcus was noted to be prominent in C-IBS subjects (Kassinen, et al). Ruminococcus sp. are not methanogenic organisms but a known hydrogen donor to facilitate methane production by true methanogenic organisms. The most common methanogen in humans is Methanobrevibacter smithii. In this study, stool from subjects with C-IBS and methane on breath test are compared to hydrogen only IBS subjects for Ruminococcus and Methonobrevibacter. Methods: Consecutive Rome II IBS subjects presenting for lactulose breath testing were eligible for study. Using a questionnaire and breath test results, subjects with methane (>3ppm during 180 minutes of testing) and constipation predominant IBS were determined. The control group included subjects with IBS not positive for methane on breath testing. After completion of breath testing, subjects were asked to provide a fresh frozen stool sample. From each stool sample, bacterial DNA was extracted (Qiagen QIAamp). PCR with previously published primers specific for Methanobrevirbacter smithii, Ruminococcus albus and Ruminococcus flavifaciens 16S rRNA were used to detect their presence in stool Results: After exclusion criteria were applied 9 subjects (8 female) with and 10 subjects (8 female) without methane completed the study. The average age was no different between groups. In the methane group the validated symptom C-D score was 5.13.8 compared to -0.113.6 for non-methane subjects (P<0.01) indicating the balance towards significant constipation in methane subjects. Bloating and abdominal pain were not different between groups. The mean methane area-under-the-curve for the first 120 minutes of breath test was 15677ppm. On PCR only 1 patient (methane positive) had evidence of both R. albus and R. Flavifaciens. However, Methanobrevibacter smithii was strongly present in 5 of 9 (56%) methane producers and only weakly positive in 2 of 10 (20%) non-methane subjects. Among only methane producers, those positive for M. smithii had a greater area-under-the-curve for methane at 18785ppm compared to methane subjects without M. smithii (11853ppm) although not powered enough to be significant. Conclusions: Ruminococcus albus and flavifaciens appear to be uncommon in methane subjects with C-IBS. Methanobrevibacteri smithii appears important in these subjects although other methanogens must also be examined since 4 of 9 methane subjects had no detectable M. smithii. T1833 Blastocystis hominis in Patients With Irritable Bowel Syndrome and Eradication With Nitazoxanide William P. Stuppy Purpose: Blastocystis hominis (BH) is a protozoan commonly found in the human digestive tract. Surveillance studies from the United States and Europe indicate 11-38% of the population may be infected with this organism. However, the pathogenicity of BH is controversial despite increasing evidence supporting the role of this protozoan in digestive disorders.
While some patients with BH may be asymptomatic, recent studies indicate a strong association between irritable bowel syndrome (IBS) and BH infection. There is no drug indicated for the treatment of BH, metronidazole has traditionally been used for treatment. Unfortunately drug resistance has become problematic with metronidazole therapy. Currently, the 2009 Sanford Guide to Antimicrobial Therapy recommends nitazoxanide as the primary treatment option for BH. Nitazoxanide is indicated for the treatment of Cryptosporidium parvum and Giardia lamblia in adults and in children and has demonstrated activity against BH in both clinical and In Vitro studies. This abstract reports on the use of nitazoxanide for the eradication of BH in patients with IBS. Methods: Patients with a diagnosis of IBS by ROME II/III criteria had their stool examined via microscopy (Diagnos-Techs, Inc., Kent, WA) for the presence of BH as part of their serial workup. Those with positive stools were then treated with nitazoxanide 1 g twice daily for 14 days. Upon follow-up examination patients had their stools rechecked for the presence of BH and they were re-evaluated for their IBS symptoms. Microbiologic cure was defined as those with negative stools for BH after therapy. Clinical response was defined as resolution of IBS related symptoms. Results: Overall 22 patients (10 males and 12 females) with IBS had stool studies positive for BH. The mean age of the population was 53 years. A microbiologic cure was achieved in 82% (18/22) of the patients and a clinical cure in 86% (19/22) of the patients. There was an excellent correlation between the eradication of BH and the resolution of IBS symptoms, 94% (17/18). Nitazoxanide was well tolerated with most patients reporting yellowing of the urine, and a few complaining of gastrointestinal discomfort during therapy which had resolved at follow-up. Conclusion: In this study, nitazoxanide was effective for the treatment of Blastocystis hominis infection. The complete pathogenic role of BH remains unclear, however it should be considered a potential pathogen in symptomatic patients. Double-blind placebo controlled studies are warranted to determine the role of Blastocystis hominis in patients with IBS. T1834 The Expression of the Tight Junction Proteins, Claudin-1, Occludin and ZO-1 is Reduced in the Colonic Mucosa of Patients With Irritable Bowel Syndrome Nathalie Bertiaux-Vandale, Beutheu-Youmba Stphanie, Belmonte-Zalar Liliana, Stephane Lecleire, Michel Antonietti, Guillaume Gourcerol, Leroi Anne Marie, Pierre M. Dchelotte, Philippe R. Ducrott, Mose Coffier Introduction: Recent studies have suggested that an increased intestinal paracellular permeability is a key physiopathological factor in the irritable bowel syndrome (IBS). This increased permeability could be due to alterations of tight junction proteins. The aim of this prospective study was to compare in the colonic mucosa the expression of the tight junction proteins in patients between IBS patients and healthy controls. Materials and methods: 23 IBS patients (21 women, 2 men, mean age: 47,69 years) fulfilling the Rome III criteria and 20 controls (12 women, 8 men, mean age: 59,65years) were included. IBS patients were D-IBS in 9 cases, C-IBS in 7, and A-IBS in 7 cases. IBS was post-infectious in 3 patients. Controls underwent a colonoscopy within the framework of screening. IBS symptom intensity was quantified on 10-cm VAS. On the protein extracted from colonic biopsies, the expression of tight junction proteins (claudin-1, ZO-1, occludin) was analyzed by western - blot. The results, expressed as average mean deviation, were compared by Mann-Whitney and Kruskal-Wallis tests Results: The expression of the 3 proteins of the tight junctions was significantly lower in the patients with IBS than in the controls (Table). The comparison of the expression of proteins according to the subgroups of IBS revealed only a decrease expression of occluding in case of C-IBS vs controls (0,260,08; p < 0,05). The lowest expression of occludin was observed in patients with an abdominal pain intensity higher than 6 : 0,240,14 vs 0,550,16 for VAS between 3 and 6 (p < 0.05). There was also a trend for a more important decrease of occludin in case of new IBS (occurrence < 1year). Conclusion: This study shows that expression of tight junction proteins (claudin-1, occludin, ZO-1) is decreased in colonic biopsies of IBS patients. This factor could contribute to increase the intestinal permeability observed in IBS.
AGA Abstracts
T1835 Giardiasis and Chronic Dyspeptic Syndrome Michal Demeter, Peter Banovcin, Rudolf Hyrdel, Janka Bozikova INTRODUCTION: Giardia lamblia (GL) is the most prevalent human intestinal parasitic protist in the world. Clinical manifestations of GL infection vary from asymptomatic infection to chronic diarrhoea.Chronic GL infection prevalence and symptomatology is unclear. We studied the presence of GL in patients with chronic dyspeptic syndrome of unknown origin. AIMS & METHODS: We enrolled into study 116 patients (29 males/ 87 females) with chronic dyspeptic syndrome,normal laboratory tests, negative abdominal ultrasound and upper endoscopy findings. We studied presence of selected symptoms (heartburn, dull epigastric pain, epigastric cramps, epigastric fullness, flatulence, diarrhoea), weight loss and presence of GL infection (analysis of duodenal juice aspirate collected during upper endoscopy), Helicobacter pylori infection (HP), and coeliac disease (CD) in examined patients. We studied symptomatology of GL positive patients 2 months after metronidasol therapy. RESULTS: GL infection was diagnosed in 27% (9/22) patients. GL without CD or HP was present in 12% (4/10) patients, GL and HP in 12% (4/10), GL and CD in 2% (1/1), and GL,CD and HP in 1% (0/1) of patients. Average lenght of dyspeptic syndrome history was 23,3 months (22/24) with weight loss of 2,8kg (3,5/2,4). Most frequent symptoms in patients with isolated chronic GL infection were epigastric fullness (86%), dull epigastric pain (50%), heartburn (43%), flatulence (36%), abdominal cramps (29%) and diarrhoea (29%). We documented total remission of symptoms in 79%(7/17) examined patients with GL infection after 14-days course of therapy with metronidasol 250 mg tid. There were no statistically
AGA Abstracts
S-588
S-ar putea să vă placă și
- Srep39399 PDFDocument12 paginiSrep39399 PDFAlex DelgadoÎncă nu există evaluări
- A Candidate Probiotic With Unfavourable Effects in Subjects With Irritable Bowel Syndrome: A Randomised Controlled TrialDocument7 paginiA Candidate Probiotic With Unfavourable Effects in Subjects With Irritable Bowel Syndrome: A Randomised Controlled Trialdolo2000Încă nu există evaluări
- Van Nella 2010Document9 paginiVan Nella 2010Anonymous tSdibBveÎncă nu există evaluări
- H. pylori Eradication Improves Gastric Atrophy and MetaplasiaDocument8 paginiH. pylori Eradication Improves Gastric Atrophy and MetaplasiaadjinurÎncă nu există evaluări
- Abdominal Tuberculosis in Nepal Medical College Teaching Hospital, KathmanduDocument4 paginiAbdominal Tuberculosis in Nepal Medical College Teaching Hospital, KathmanduSavitri Maharani BudimanÎncă nu există evaluări
- A Vegan Diet Alters The Human Colonic Faecal MicrobiotaDocument8 paginiA Vegan Diet Alters The Human Colonic Faecal MicrobiotaWilver Edson Otalora AnturianoÎncă nu există evaluări
- Development of type I gastric carcinoid in chronic atrophic gastritis patientsDocument9 paginiDevelopment of type I gastric carcinoid in chronic atrophic gastritis patientsAbristaSeptikasariÎncă nu există evaluări
- Probiotics in Cystic Fibrosis Patients A Double Blind CrossoveDocument7 paginiProbiotics in Cystic Fibrosis Patients A Double Blind CrossoveDarwinÎncă nu există evaluări
- Corpus GastritisDocument5 paginiCorpus Gastritisameer143Încă nu există evaluări
- Digest: Predictors of Failure of Pneumatic Dilatation in AchalasiaDocument3 paginiDigest: Predictors of Failure of Pneumatic Dilatation in AchalasiaDian Eka PermataÎncă nu există evaluări
- Clinical Study Gene Expression of Leptin and Long Leptin Receptor Isoform in Endometriosis: A Case-Control StudyDocument38 paginiClinical Study Gene Expression of Leptin and Long Leptin Receptor Isoform in Endometriosis: A Case-Control StudyAnthony ChandraÎncă nu există evaluări
- Cancer Epidemiol Biomarkers Prev 2004 Ley 4 10Document8 paginiCancer Epidemiol Biomarkers Prev 2004 Ley 4 10Cristian BorrelliÎncă nu există evaluări
- 1 s2.0 S0140673684918166 MainDocument5 pagini1 s2.0 S0140673684918166 MainjimbojandersonÎncă nu există evaluări
- Fgene 12 631061Document7 paginiFgene 12 631061Elder Alonso Castro AliagaÎncă nu există evaluări
- 2 Bacteria UC ProbioticDocument22 pagini2 Bacteria UC Probioticu77Încă nu există evaluări
- Ajg 2009 524Document10 paginiAjg 2009 524Alex Cristian IonutÎncă nu există evaluări
- ESDID 2020 AbstractsDocument1.491 paginiESDID 2020 AbstractsAndreea PopicaÎncă nu există evaluări
- Jurnal 3 Fater 2Document8 paginiJurnal 3 Fater 2ANDIANY CAHYANTY TAHIRÎncă nu există evaluări
- Background: Ormdl3 and of GSDMB Were Significantly Increased in Hrv-Stimulated PBMCSDocument6 paginiBackground: Ormdl3 and of GSDMB Were Significantly Increased in Hrv-Stimulated PBMCSSav GaÎncă nu există evaluări
- Out 40Document9 paginiOut 40natanatalisÎncă nu există evaluări
- Srep 08508Document9 paginiSrep 08508thaisagoraer1Încă nu există evaluări
- Clinical Study: Chronic Gastritis in Dermatitis Herpetiformis: A Controlled StudyDocument5 paginiClinical Study: Chronic Gastritis in Dermatitis Herpetiformis: A Controlled Studyfirsa_artÎncă nu există evaluări
- Gut Microbiota May Not Be Fully Restored in Recovered COVID-19 Patients After 3-Month RecoveryDocument9 paginiGut Microbiota May Not Be Fully Restored in Recovered COVID-19 Patients After 3-Month RecoveryEdgar VázquezÎncă nu există evaluări
- Pancreas and Microbiome: C. Schulz, K. SchuetteDocument7 paginiPancreas and Microbiome: C. Schulz, K. Schuetteps piasÎncă nu există evaluări
- FK concetration is increase in children with celic d....Document6 paginiFK concetration is increase in children with celic d....Nejc KovačÎncă nu există evaluări
- Gerd in Subglottic StenosisDocument5 paginiGerd in Subglottic StenosisPantelis ChouridisÎncă nu există evaluări
- Paediatrica Indonesiana: Original ArticleDocument7 paginiPaediatrica Indonesiana: Original ArticleMyrtle SetiawanÎncă nu există evaluări
- US vs. Barium for Pediatric GERDDocument6 paginiUS vs. Barium for Pediatric GERDAndreea KÎncă nu există evaluări
- Systematic Review: Tuberculous Peritonitis - Presenting Features, Diagnostic Strategies and TreatmentDocument16 paginiSystematic Review: Tuberculous Peritonitis - Presenting Features, Diagnostic Strategies and TreatmenthendraÎncă nu există evaluări
- Clinical Guidelines Secondary Prevention of Gastric CancerDocument1 paginăClinical Guidelines Secondary Prevention of Gastric Cancerhenrique.uouÎncă nu există evaluări
- NIH Public Access: Gastrointestinal Microbiome Signatures of Pediatric Patients With Irritable Bowel SyndromeDocument19 paginiNIH Public Access: Gastrointestinal Microbiome Signatures of Pediatric Patients With Irritable Bowel SyndromesebaspezoaÎncă nu există evaluări
- Jurnal DigestifDocument19 paginiJurnal DigestifDianaarlyÎncă nu există evaluări
- Association Between Vegf 936cT Gene Polymorphism With Gastric Premalignant Lesions and Vegf Levels in Helicobacter Pylori PatientsDocument3 paginiAssociation Between Vegf 936cT Gene Polymorphism With Gastric Premalignant Lesions and Vegf Levels in Helicobacter Pylori PatientsDavid NicholasÎncă nu există evaluări
- Dr. Dhinesh Babu.K, Prof Dr. M .BhaskarDocument6 paginiDr. Dhinesh Babu.K, Prof Dr. M .BhaskarIOSRjournalÎncă nu există evaluări
- Egypt J Med Microbiol 2009 18 4 165 178Document14 paginiEgypt J Med Microbiol 2009 18 4 165 178Cristina RaduleaÎncă nu există evaluări
- Case-Finding in Primary Care For Coeliac Disease: Accuracy and Cost-Effectiveness of A Rapid Point-Of-Care TestDocument11 paginiCase-Finding in Primary Care For Coeliac Disease: Accuracy and Cost-Effectiveness of A Rapid Point-Of-Care TestmarcosÎncă nu există evaluări
- Acta PaediatricaDocument13 paginiActa PaediatricaDefranky TheodorusÎncă nu există evaluări
- Helicobacter Species in The Intestinal Mucosa of Patients With Ulcerative ColitiDocument3 paginiHelicobacter Species in The Intestinal Mucosa of Patients With Ulcerative ColitiAlexandru CozmaÎncă nu există evaluări
- Abdominal Tuberculosis in Children StudyDocument1 paginăAbdominal Tuberculosis in Children StudyDrMukesh BhaskarÎncă nu există evaluări
- WoMPBI9 Abstracts PDFDocument101 paginiWoMPBI9 Abstracts PDFMartha EndikaÎncă nu există evaluări
- A prospective pilot study of a gluten‐free diet for primary sclerosingDocument13 paginiA prospective pilot study of a gluten‐free diet for primary sclerosingNejc KovačÎncă nu există evaluări
- E 948Document13 paginiE 948ps piasÎncă nu există evaluări
- ICCH12 JohansenDocument2 paginiICCH12 Johansenevi_atunÎncă nu există evaluări
- Alterations of The Gut Microbiome in Chinese PatieDocument7 paginiAlterations of The Gut Microbiome in Chinese PatieMarcela Garzon O VelezÎncă nu există evaluări
- En V27n4a02Document6 paginiEn V27n4a02Humberto Liu BejaranoÎncă nu există evaluări
- Fecal Microbiota Transplantation - An Old Therapy Comes of AgeDocument2 paginiFecal Microbiota Transplantation - An Old Therapy Comes of AgeGonzalo Moyano BalbisÎncă nu există evaluări
- Development of A Novel Multiplexed QPCR and Pyrosequencing Method For The Detection of Human Pathogenic YersiniaeDocument7 paginiDevelopment of A Novel Multiplexed QPCR and Pyrosequencing Method For The Detection of Human Pathogenic YersiniaeMelisa NicevićÎncă nu există evaluări
- Ga TB Final ArticleDocument4 paginiGa TB Final Articleseema sharmaÎncă nu există evaluări
- Ceju 66 00246Document4 paginiCeju 66 00246Àlex MataÎncă nu există evaluări
- Small Intestinal Contrast UltrasonographDocument5 paginiSmall Intestinal Contrast UltrasonographСергей СадовниковÎncă nu există evaluări
- Podocyturia As A DiagnosticMarker For Preeclampsia 2012Document6 paginiPodocyturia As A DiagnosticMarker For Preeclampsia 2012Diapositivas08Încă nu există evaluări
- Fecal Calprotectin, Gut Inflammation and Spondyloarthritis: ClinicalDocument6 paginiFecal Calprotectin, Gut Inflammation and Spondyloarthritis: ClinicalPÎncă nu există evaluări
- PCR Detection of AIEC Using CRISPR Genes in IBDDocument2 paginiPCR Detection of AIEC Using CRISPR Genes in IBDNilo BarretoÎncă nu există evaluări
- Junal DispepsiaDocument6 paginiJunal DispepsiaJesryn Kaur DhillonÎncă nu există evaluări
- Review of Cap Polyposis in Children and Case ReportDocument6 paginiReview of Cap Polyposis in Children and Case ReportLuis ArrietaÎncă nu există evaluări
- Hepatitis in Children With Tuberculosis: A Case Report and Review of The LiteratureDocument4 paginiHepatitis in Children With Tuberculosis: A Case Report and Review of The LiteratureauliaÎncă nu există evaluări
- PraktLik 2013 4 8Document4 paginiPraktLik 2013 4 8mustafi28Încă nu există evaluări
- Thai Journal of Gastroenterology Vol 10 No 3 4729203Document6 paginiThai Journal of Gastroenterology Vol 10 No 3 4729203Humberto Liu BejaranoÎncă nu există evaluări
- Probiotik Clinical Applications in Gastrointestinal DiseaseDocument29 paginiProbiotik Clinical Applications in Gastrointestinal DiseaseDwi Feri HariyantoÎncă nu există evaluări
- Complementary and Alternative Medical Lab Testing Part 5: GastrointestinalDe la EverandComplementary and Alternative Medical Lab Testing Part 5: GastrointestinalÎncă nu există evaluări
- 3 HIPAA TrainingDocument2 pagini3 HIPAA TrainingNikola StojsicÎncă nu există evaluări
- Sayonved - Elisa Test Za BH Iz StoliceDocument4 paginiSayonved - Elisa Test Za BH Iz StoliceNikola StojsicÎncă nu există evaluări
- Male DomaciceDocument1 paginăMale DomaciceNikola StojsicÎncă nu există evaluări
- Cokoladni Cheesecake S Irish Cream BaileysDocument2 paginiCokoladni Cheesecake S Irish Cream BaileysNikola StojsicÎncă nu există evaluări
- Superior efficacy of pancreatin 25 000 MMS in PEI after pancreatic surgeryDocument12 paginiSuperior efficacy of pancreatin 25 000 MMS in PEI after pancreatic surgeryNikola StojsicÎncă nu există evaluări
- Prakash 2005Document9 paginiPrakash 2005Nikola StojsicÎncă nu există evaluări
- Pi Is 0016508510003136Document10 paginiPi Is 0016508510003136Nikola StojsicÎncă nu există evaluări
- Sedation and Analgesia in Pediatric Patients For ProceduresDocument13 paginiSedation and Analgesia in Pediatric Patients For ProceduresNikola StojsicÎncă nu există evaluări
- International Academy of Paediatric Endoscopy Training: Monthly Hands-On Ileo-Colonoscopy Courses 2013 ScheduleDocument3 paginiInternational Academy of Paediatric Endoscopy Training: Monthly Hands-On Ileo-Colonoscopy Courses 2013 ScheduleNikola StojsicÎncă nu există evaluări
- Male DomaciceDocument1 paginăMale DomaciceNikola StojsicÎncă nu există evaluări
- BH Human PatogenicDocument7 paginiBH Human PatogenicNikola StojsicÎncă nu există evaluări
- Sayonved - Elisa Test Za BH Iz StoliceDocument4 paginiSayonved - Elisa Test Za BH Iz StoliceNikola StojsicÎncă nu există evaluări
- Cancercare Booklet GISTDocument20 paginiCancercare Booklet GISTNikola StojsicÎncă nu există evaluări
- Arbaclofen GERDDocument11 paginiArbaclofen GERDNikola StojsicÎncă nu există evaluări
- EGDS LidokainDocument9 paginiEGDS LidokainNikola StojsicÎncă nu există evaluări
- Borody 2007 Drug CombinationDocument2 paginiBorody 2007 Drug CombinationNikola StojsicÎncă nu există evaluări
- Blastocystis InfectionDocument7 paginiBlastocystis InfectionNikola StojsicÎncă nu există evaluări
- Blastocyst IsDocument2 paginiBlastocyst IsNikola StojsicÎncă nu există evaluări
- Clin. Microbiol. Rev.-1996-Stenzel-563-84Document23 paginiClin. Microbiol. Rev.-1996-Stenzel-563-84Nikola StojsicÎncă nu există evaluări
- Sayonved - Elisa Test Za BH Iz StoliceDocument4 paginiSayonved - Elisa Test Za BH Iz StoliceNikola StojsicÎncă nu există evaluări
- B HomDocument1 paginăB HomNikola StojsicÎncă nu există evaluări
- Prevalence of Blastocystis hominis and other parasitesDocument5 paginiPrevalence of Blastocystis hominis and other parasitesNikola StojsicÎncă nu există evaluări
- Enteropatogeni VenecuelaDocument8 paginiEnteropatogeni VenecuelaNikola StojsicÎncă nu există evaluări
- Acute Supp App and BHDocument11 paginiAcute Supp App and BHNikola StojsicÎncă nu există evaluări
- Archdisch00570 0027Document3 paginiArchdisch00570 0027Nikola StojsicÎncă nu există evaluări
- Ni Hms 366279Document12 paginiNi Hms 366279Nikola StojsicÎncă nu există evaluări
- Minimal Ernteral Nutrition 150308Document8 paginiMinimal Ernteral Nutrition 150308Nikola StojsicÎncă nu există evaluări
- What Have We Learned About Acute Pancreatitis In.3Document9 paginiWhat Have We Learned About Acute Pancreatitis In.3Nikola StojsicÎncă nu există evaluări
- APACHE System Is Better Than Ranson System in The Prediction of Severity of Acute PancreatitisDocument6 paginiAPACHE System Is Better Than Ranson System in The Prediction of Severity of Acute PancreatitisNikola StojsicÎncă nu există evaluări
- Two Marks-8051.docx - 1570617188187Document4 paginiTwo Marks-8051.docx - 1570617188187PraveenÎncă nu există evaluări
- Neurology Shelf Exam Review - Part 2.newDocument14 paginiNeurology Shelf Exam Review - Part 2.newyogurtÎncă nu există evaluări
- 12 Years A Slave LitChartDocument52 pagini12 Years A Slave LitChartNobody Important100% (1)
- Learn Prepositions and ArticlesDocument12 paginiLearn Prepositions and ArticlesAl-Ami SarkerÎncă nu există evaluări
- Evaluate Narrativs Based On How The Author Developed The Element THEMEDocument30 paginiEvaluate Narrativs Based On How The Author Developed The Element THEMEDianArtemiz Mata Valcoba80% (25)
- Pharmacy Perspective on Improving Patient SafetyDocument44 paginiPharmacy Perspective on Improving Patient SafetydicodrÎncă nu există evaluări
- Report - Inclusive Education Experiences of Parents in MsiaDocument13 paginiReport - Inclusive Education Experiences of Parents in MsiaSuhana AhmadÎncă nu există evaluări
- Close Your MouthDocument144 paginiClose Your MouthSelvakumaran Dhandapani100% (13)
- Questions About ShoppingDocument4 paginiQuestions About ShoppingPutri Nur AzizahÎncă nu există evaluări
- TCMP Manual Provides Guidance for Inmate RehabilitationDocument159 paginiTCMP Manual Provides Guidance for Inmate RehabilitationDONALDO BRITAÑAÎncă nu există evaluări
- EEE 3101 Continuous Signals & Linear System: Convolution Integral Lecture-14Document13 paginiEEE 3101 Continuous Signals & Linear System: Convolution Integral Lecture-14Amanur AkashÎncă nu există evaluări
- The Province of North Cotabato, Et Al - V - The Government of The Republic of The Philippines, Et Al .Document11 paginiThe Province of North Cotabato, Et Al - V - The Government of The Republic of The Philippines, Et Al .Arbee ArquizaÎncă nu există evaluări
- Food ValuesDocument2 paginiFood ValuesMiss L. NelÎncă nu există evaluări
- AchievementsDocument4 paginiAchievementsapi-532080614Încă nu există evaluări
- Heirs of Jesus Fran v. Hon. Bernardo LL. SalasDocument3 paginiHeirs of Jesus Fran v. Hon. Bernardo LL. SalasMara Corteza San PedroÎncă nu există evaluări
- Full Download Ebook PDF Psychology 8e 8th Edition by Lester M Sdorow PDFDocument41 paginiFull Download Ebook PDF Psychology 8e 8th Edition by Lester M Sdorow PDFandrew.wilson391100% (28)
- Konark Sun Temple, a 13th century architectural marvelDocument18 paginiKonark Sun Temple, a 13th century architectural marvelSyed Ahmed KabeerÎncă nu există evaluări
- Stephen A. Douglas Homecoming'' Speech Summary: By: Miri Cooper, Rivky Schmidt, and Shiffy HeckmanDocument8 paginiStephen A. Douglas Homecoming'' Speech Summary: By: Miri Cooper, Rivky Schmidt, and Shiffy HeckmanChrisÎncă nu există evaluări
- Fantasy AGE - Spell SheetDocument2 paginiFantasy AGE - Spell SheetFran Bejarano100% (6)
- Thesis On Romantic RelationshipsDocument4 paginiThesis On Romantic RelationshipsSophia Diaz100% (1)
- Second Group Project - Risk and ReturnDocument3 paginiSecond Group Project - Risk and ReturnJeff RuncornÎncă nu există evaluări
- Emergent Reader Case Summary SheetDocument2 paginiEmergent Reader Case Summary Sheetapi-503192153Încă nu există evaluări
- Bilge System CalculationDocument12 paginiBilge System CalculationMuhammad Habib100% (1)
- Justice at Nuremberg FA 1946Document11 paginiJustice at Nuremberg FA 1946tcchildsÎncă nu există evaluări
- Shell Forces Stresses FormDocument4 paginiShell Forces Stresses FormYudikaWisnuPratomoÎncă nu există evaluări
- Zambian Languages Syllabus: Grades 5 - 7Document65 paginiZambian Languages Syllabus: Grades 5 - 7suwilanji siame100% (2)
- Birhau Ngan Identity Page4Document19 paginiBirhau Ngan Identity Page420 18Încă nu există evaluări
- Artica Web DocumentationDocument30 paginiArtica Web Documentationsnake972Încă nu există evaluări
- Tinkle July 2019Document176 paginiTinkle July 2019Ad85% (13)
- Staffing Report: New CLAIT Level 1 OCR Sample Assignment ADocument6 paginiStaffing Report: New CLAIT Level 1 OCR Sample Assignment AmpvukÎncă nu există evaluări