Documente Academic
Documente Profesional
Documente Cultură
Surgical Manag Exotropia
Încărcat de
jbahalkehDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Surgical Manag Exotropia
Încărcat de
jbahalkehDrepturi de autor:
Formate disponibile
Major Articles The Surgical Management of Consecutive Exotropia
Mark J. Donaldson, MBBS(Hons),a Michael P. Forrest, MBBS, BMedSci,b and Glen A. Gole, MD, FRANZCO, FRACSa,c Purpose: To review the results and techniques of surgical treatment of consecutive exotropia. Methods: We performed a retrospective chart review of all patients who underwent surgery for consecutive exotropia in a pediatric ophthalmology practice between 1992 and 2001. Patients were excluded if follow-up lasted 6 weeks or if exotropia was caused by other ocular disorders such as previous trauma or congenital cataracts. Results: Fifty-nine patients were identied. The procedure performed in the majority of cases was unilateral lateral rectus recession and medial rectus advancement to the original insertion. Seven patients underwent bilateral lateral rectus recession, and 6 underwent lateral rectus recession combined with medial rectus resection. The mean interval between original surgery and surgery for consecutive exotropia was 14.1 years (range 4 months to 47.5 years). The mean preoperative distance exodeviation was 31.7 prism diopters (PD). Satisfactory alignment (ie, within 10 PD of orthophoria) was achieved in 36 patients (61%) at week 1 and 42 patients (71%) at nal follow-up. Mean follow up was 16.0 months. Thirty-nine patients (66%) demonstrated an exodrift after surgery (mean 7.6 PD). Conclusion: Consecutive exotropia may occur many years, even decades, after esotropia surgery. Lateral rectus recession with advancement of the previously recessed medial rectus is an effective treatment. An exotropic drift occurs after consecutive exotropia surgery, usually within the rst 6 weeks. A suitable ocular alignment immediately after surgery for consecutive exotropia is a small-angle esotropia of 5 to 10 PD. (J AAPOS 2004;8: 230-236)
onsecutive exotropia is a manifest exotropia that develops spontaneously in a formerly esotropic patient or after optical or surgical treatment for esotropia. It has been reported in 3% to 29% of all patients after surgical treatment of esotropia1-6 with higher incidences reported in studies with longer follow-up.7,8 Most investigators have studied the results from series of patients who underwent surgery for esotropia and then attempted to identify causative factors among the patients ended up with an overcorrection. These factors include amblyopia,4,5,9 presence of A- or V-patterns,6 developmental delay,10 early-onset esotropia,7,11 esotropia surgery before 6 months of age,7 and multiple previous strabismus surgeries.12 When consecutive exotropia does occur, how should it be managed? Little is known about how patients with consecutive exotropia respond to surgery. We report the
results of a series of patients with consecutive exotropia managed surgically and make recommendations on the management of such patients.
SUBJECTS AND METHODS
We retrospectively reviewed the records of all patients who underwent surgery for consecutive exotropia between April 1, 1992 and March 31, 2001, in a single-surgeon pediatric ophthalmic practice. All patients had previously undergone at least 1 surgical procedure for infantile or acquired esotropia. Infantile esotropia had been diagnosed in 42 patients either by one of the investigators or the referring ophthalmologist. Eight patients had acquired esotropia, and in 9 patients the previous type of esotropia was unclear. Patients were excluded if follow-up lasted 6 weeks, if exotropia developed spontaneously, or if exotropia was caused by other ocular disorders such as previous ocular trauma or congenital cataracts. All patients were assessed at 2 or more separate examinations before surgery was performed. Assessments included visual acuity, cycloplegic refraction (using 1% cyclopentolate), ocular deviation, and dilated fundus examination. Preoperative deviations were measured using loose prisms at distance and near xation and left gaze, right gaze, upgaze, and downgaze gaze with corrective lenses when required. The Krimsky test was used for children too young for accurate alternate-prism cover tests at distance. The angle was measured for near at 33 cm and for distance
Journal of AAPOS
From the Department of Ophthalmology, Royal Childrens Hospital,a Brisbane, Australia; the Department of Ophthalmology, Mater Childrens Hospital,b Brisbane, Australia; and the Department of Pediatrics and Child Health, University of Queensland, Brisbane,c Brisbane, Australia. Submitted October 28, 2003. Revision accepted January 8, 2004. Reprint requests: Glen A. Gole MD, Department of Pediatrics and Child Health, Royal Childrens Hospital, Herston Rd, Brisbane, Queensland 4029, Australia. Copyright 2004 by the American Association for Pediatric Ophthalmology and Strabismus. 1091-8531/2004/$35.00 0 doi:10.1016/j.jaapos.2004.01.001
230
June 2004
Journal of AAPOS Volume 8 Number 3 June 2004
Donaldson, Forrest, and Gole
RESULTS
231
at a target at approximately 40 m through an open window. Amblyopia was dened as (1) a difference between the two eyes 2 lines of best-corrected visual acuity or (2) a lack of central, steady, maintained xation in infants. Amblyopia was treated with patching in all patients 8 years until no further improvement was observed after 3 consecutive months. The indication for surgery was most commonly a cosmetically obvious exotropia 15 prism diopters (PD). All surgery was performed with the patient under general anesthesia. Lateral rectus recession was performed using a standard technique by way of limbal incision.13 The muscle was reinserted at a xed point from the insertion for nonadjustable sutures or hung back from the insertion in the case of adjustable sutures. Adjustment, if required, was performed between 2 and 8 hours after surgery with the patient under topical anesthesia. For medial rectus advancement, 2 double-armed 6-0 Vicryl (Polyglactin 910; Ethicon, Somerville, NJ) sutures were inserted with locking bites, and the muscle was disinserted and advanced to the original insertion. Medial rectus resection was performed using a standard technique.13 Tenonectomy was not routinely performed. The conjunctiva was closed without recession using 8-0 Vicryl sutures. Conjunctival resection was not performed in case further muscle surgery would be necessary. Topical antibiotics and mild topical steroids were applied for 1 week after surgery. The specic surgical procedure was chosen to normalize any abnormal ductions. For example, where there was limitation of adduction or convergence insufciency, the affected medial rectus was strengthened. Consideration was given to the type and amount of previous surgery to avoid over-recession or resection of previously operated muscles. Unilateral surgery was performed preferably on the amblyopic eye. The extent of recession, advancement or resection was determined using a standard table developed by Parks.14 The general principle adopted was to advance the medial rectus back to the original insertion if the amount of advancement was equivalent within 1 mm to the amount of resection advised from Parks table for that angle of deviation. If the amount of possible advancement back to the original insertion was greater than the resection amount advised from the table, the muscle was positioned behind the original insertion by two double-armed hang-back sutures so that the muscle was advanced by the advised amount. If the amount of possible advancement to the original insertion was less than the resection amount advised, the muscle was advanced to the original insertion and the difference resected before reinsertion. The amount of lateral rectus recession was determined according to the same tables. In patients with large angles ( 50 PD), additional lateral rectus recession or medial rectus advancement was performed in the contralateral eye.
Sixty-four patients treated for consecutive exotropia were identied; 5 were excluded because of insufcient followup. Patient ages ranged from 11.5 months to 62.7 years; the mean was 21 years (95% condence interval [CI] 4.3), and the median was 15.1 years (SD 16.7). Twentyve patients were male (42%), and 34 (58%) were female. Forty-four of the 59 patients (74.6%) underwent their initial surgery elsewhere. Mean follow-up was 16.0 months (range 6 weeks to 7.5 years). Many of those with good results were discharged after 6 months to the care of the referring ophthalmologist for further follow up. For those patients whose original records were available, previous surgical procedures were as follows: 26 patients underwent bilateral medial rectus recession, 6 underwent bilateral medial rectus recession with unilateral lateral rectus resection, and 12 underwent unilateral medial rectus recession/lateral rectus resection. Seven patients had previously undergone inferior oblique surgery either as an independent procedure or in combination with horizontal rectus surgery. Details of the original esotropia surgery were not available for 15 patients. In these patients, either correspondence or discharge summaries recorded examination ndings but not the details of surgical procedures performed or the surgical notes gave only limited details (eg, esotropia2-muscle squint repair). The mean age at original surgery for esotropia was 37.7 months (n 54, data unavailable for 5 patients, CI 7.6, SD 29.9, median 26.). The study population comprised a mixture of patients with infantile and acquired esotropia, and many patients underwent their original esotropia surgery at a time before early surgery became standard management. Twenty-eight patients (47%) underwent 2 operations for esotropia before presenting with consecutive exotropia. There was no signicant difference in nal outcome or drift between patients with a history of infantile or acquired esotropia. The mean interval between the original surgery and the surgery for consecutive exotropia was 14.1 years (CI 3.7) and ranged from 4 months to 47.5 years. (n 54, data unavailable for 5 patients, SD 13.6 years, median 8.3 years). In 16 patients (27%), consecutive exotropia developed within 6 months of esotropia surgery. Seven of these patients had onset of consecutive exotropia within 1 month of the second or third operation. Amblyopia was present in 12 patients (20%). Eleven of these patients were 10 years old, and further amblyopia therapy was not attempted. Nine patients (15%) had hyperopia 2.50 D. These patients were operated on according to their angle when wearing glasses. Only 1 patient (1.7 %) had myopia 2.50 D. Four patients (6.7%) had anisometropia 1.0 D. Surgical procedures performed for the 59 patients were as follows: 42 patients (71%) underwent lateral rectus
232 Donaldson, Forrest, and Gole
Journal of AAPOS Volume 8 Number 3 June 2004
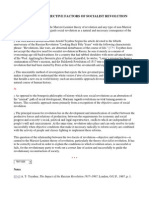
Fig 1. Mean preoperative and postoperative ocular alignments for each surgical procedure (horizontal bars). Vertical lines represent 1 SD on either side of the mean. Positive values represent esodeviations, and negative values represent exodeviations.
recession and medial rectus advancement (LRc/MR adv), 7 (12 %) underwent bilateral lateral rectus recession (BLRc), and 6 (10 %) underwent lateral rectus recession and medial rectus resection (LRc/MRs). Four patients with large deviations ( 50 PD) underwent three muscle surgeries: 1 patient each (1.7 %) underwent LRc/BMR adv (bilateral medial rectus advancement), BLRc/MR adv, BLRc/MRs, or BLRc/BMR adv. (These four patients are not depicted in Figure 1). The amount of lateral rectus recession performed before adjustment) averaged 6.5 mm and varied from 5 to 8 mm. Thirty-three patients underwent lateral rectus recession performed with hang-back adjustable sutures. Of these, 15 required adjustment after surgery, and in those patients the average adjustment was 3.5 mm of muscle advancement. The amount of medial rectus advancement averaged 5.5 mm and ranged from 3.5 to 8 mm. Seventeen patients (29%) underwent oblique surgery in combination with their consecutive exotropia surgery. No patients were found to have lost muscles requiring muscletransfer procedures. Of particular interest was 1 patient with 2 (of 4) defective adduction preoperatively who was found at surgery to have a medial rectus pseudotendon composed of scar tissue that measured 11 mm in length. Mean exodeviation before surgery was 31.7 PD for distance, (CI 3.3, SD 13.0, range 15 to 65) and 32.0 PD for near (CI 3.7, SD 14.4, range 10 to 75). Nine patients (15%) had convergence-insufciency pattern (exotropia 10 PD greater at near than distance), and 6 (10%) patients had divergence-excess pattern (exotropia 10 PD greater at distance than near). The remaining 44 patients (75%) had measurements within 10 PD of each other for distance and near. The mean preoperative and postoperative ocular alignments are depicted in Figure 1. Results of surgery at 1 week, 6 weeks, 6 months, and nal follow-up are detailed in Table 1. The number of patients who were orthotropic, esotropic, or exotropic at each time period are described. Figure 2 shows the distribution of overcorrections and undercorrections over time. Satisfactory alignment was dened as alignment within 10 PD of orthophoria for both distance and near. This was achieved in 36 patients (61%)
at 1 week1, in 40 patients (68%) at 6 weeks, and in 42 patients (71%) at nal follow-up. Five patients had satisfactory alignment at nal follow-up but required an additional procedure to accomplish this. Undercorrection was dened as exotropia of 10 PD for distance or near. Only ve patients (8%) had undercorrections in our series. Two of these were undercorrected at 1 week, whereas the other 3 patients showed satisfactory alignment at 1 week but were signicantly undercorrected at the second visit. One of these 5 patients drifted straight, and the other 4 remained signicantly undercorrected. One patient had satisfactory alignment after an additional procedure, and the other 3 patients are considering further surgery. Overcorrection was dened as esotropia 10 PD for distance or near. Twenty-one patients (36%) were overcorrected at 1 week, and 14 patients (24%) were overcorrected at 6 weeks. Of the 21 patients who were overcorrected at 1 week, 11 drifted straight spontaneously, 2 were straightened after a further surgical procedure, 1 was straightened with Botulinum toxin injections, and 7 remained overcorrected at nal analysis. Two patients who were straight at 1 week became overcorrected by nal follow-up. We also assessed the drift in the ocular alignment after surgery. Results are detailed in Table 2. Comparison between patients with satisfactory nal alignment and those with poor nal alignment showed no difference in the amount of correction (39.1 vs 38.6 PD) or the amount of postoperative drift. This suggests that patients who obtain a poor result demonstrate this soon after surgery and that the poor result is not related to postoperative drift. No patient developed slipped muscles or other serious complications. Four patients experienced intermittent diplopia after surgery. Four adult patients developed a temporary corneal dellen nasally. Two of these patients required resection of redundant nasal conjunctival folds at 2 and 4 months after surgery, respectively, before the dellen resolved. Five patients (8%) required additional procedures. Three patients underwent surgery for an overcorrection, 1 received Botulinum toxin injections for an overcorrection, and 1 underwent surgery for an undercorrection. All 5 patients had satisfactory nal alignments after the additional procedure. One patient is still awaiting surgery for an undercorrection. Amblyopia was present in 12 patients. These patients had signicantly larger preoperative exodeviations 43.1 PD for distance and 40.2 PD for near compared with 28.8 PD for distance and 30.0 PD for near for patients without amblyopia (P 0.002). Patients with amblyopia were no more likely to have a poor nal result. In fact, of the 12 patients with amblyopia, 10 had a satisfactory nal alignment compared with 36 of the 46 patients without amblyopia who had a nal satisfactory alignment. The amount of postoperative exodrift was similar in those with and without amblyopia.
Journal of AAPOS Volume 8 Number 3 June 2004
Donaldson, Forrest, and Gole
233
Fig 2. Distributions of overcorrections and undercorrections at 1 week, 6 weeks, and nal follow-up. *Five patients in the satisfactory alignment group at nal follow-up required an additional procedure to achieve this outcome (3 underwent surgery for an overcorrection, 1 underwent surgery for an undercorrection, and 1 received Botulinum toxin injections for an overcorrection). TABLE 1. Results of Surgery Results Mean deviation No. (%) orthophoria No. (%) Esotropia Mean esodeviation (PD) Range (PD) No. (%) Exotropia Mean exodeviation (PD) Range (PD)
1 Week 7.0 PD Esotropia (CI 2.4, SD 0.5) 5 (8) 49 (83) 9.9 4-25 5 (8) 12.2 4-35
6 Weeks* 2.7 PD Esotropia (n 56, CI 2.4, SD 9.2) 4 (7) 33 (56) 8.8 4-20 19 (32) 7.5 4-25
6 Months 3.1 PD Esotropia (n 44, CI 3.3, SD 11.2) 6 (10) 30 (51) 8.8 4-25 8 (14) 15.8 8-30
Final follow-up 1.5 PD Esotropia (CI 2.6, SD 9.6) 8 (14) 32 (54) 7.3 4-20 14 (24) 10.9 4-16
CI: condence interval; PD: prism diopters. *Two patients (3%) missed their 6-week visit but returned later, and 1 patient (1.7%) was treated with Botulinum toxin injections just before the 6-week appointment. Three patients (5%) required a second procedure by 6 months, and 12 patients (20%) did not return for their 6-month visit. Five patients (8%) were excluded from nal deviation calculations because their nal deviation was measured after a second operation.
DISCUSSION
This study highlights the long delay that may precede the development of consecutive exotropia. It was difcult to estimate the time of onset of consecutive exotropia after
the most recent procedure for esotropia because this information was not remembered accurately by patients and often not recorded in referral letters. For patients (n 38) with accurate information, the mean delay was 4.7 years.
234 Donaldson, Forrest, and Gole
TABLE 2. Postoperative Drift* Exodrift Time Period 1 to 6 weeks 1 week to nal result 6 weeks to 6 months Overall Drift (PD) 4.1 (CI 1.7, SD 6.8) 5.1 (CI 2.5, SD 9.4) 0.5 (CI 1.9, SD 6.2) No. (%) Patients 39 (66) 33 (56) 13 (22) Amount (PD) 7.6 (CI 1.5, SD 4.9) 10.5 (CI 2.8, SD 8.2) 5.5 (CI 4.1, SD 7.5) No. (%) Patients 10 (17) 12 (20) 19 (32)
Journal of AAPOS Volume 8 Number 3 June 2004
Esodrift Amount 6.0 (CI 1.7, SD 2.7) 5.8 (CI 3.3, SD 2.6) 5.1 (CI 1.0, SD 2.1)
No Drift No. (%) Patients 9 (15) 9 (15) 12 (20)
CI: condence interval; PD: prism diopters. *Negative values represent exodrift, and positive values represent esodrift. Patients who required a second operation or Botulinum toxin injections were excluded from drift calculations so that the effects of the second procedure were not attributed to drift. One patient (1.7%) was excluded from drift calculations from 1 to 6 weeks because of lack of data. Five patients (8.5%) were excluded from drift calculations from 1 week to nal result, and 16 patients (27%) were excluded from the 6 weeks-to-6 months calculations because of either a second procedure or a lack of follow-up to 6 months.
These gures reinforce the trend to increased prevalence of consecutive exotropia in studies of infantile esotropia with longer follow-up.8 It is therefore important to explain to parents of a child with infantile esotropia that a delayed exodeviation may occur even decades later. Amblyopia has been considered to be a contributing factor in the development of consecutive exotropia.4,5,9 Amblyopia was present in 12 patients (20.3%) in our series. This number is lower than that in several other series2,11,16 and lower than the reported incidence of amblyopia in infantile esotropia of 35% to 41%.17 Our amblyopic patients were no more likely to have a poor nal result than those without amblyopia. Similarly, the amount of postoperative exodrift was similar in those patients with and without amblyopia. The presence or absence of amblyopia therefore does not seem to inuence the nal result or the amount of postoperative exodrift after consecutive exotropia surgery. Twenty-eight patients (47%) underwent 1 operation before developing consecutive exotropia. This agrees with other series of consecutive exotropia in which a history of multiple surgeries was a frequent nding.8,12 It is not clear whether multiple surgeries lead to an increased risk of developing consecutive exotropia or whether a defect of binocular fusion leads to both failure of initial surgery and later development of consecutive exotropia. Risk factors for consecutive exotropia after surgery for undercorrected esotropia include medial rectus limitation6 and the presence of an exodeviation in the upgaze and downgaze positions.11 These ndings should serve as a caution to consider performing lesser degrees of surgery in these patients. Details of initial esotropia surgery were unavailable for 15 patients (25%) despite the fact that we wrote to the patients previous ophthalmologists and requested hospital charts. We believe the potential for delayed onset of consecutive exotropia means that hospitals and surgeons should preserve operative notes of all patients who underwent surgery for childhood strabismus, for several decades if not indenitely, so that details of the original surgery are available for planning subsequent procedures. Cooper1 proposed that surgeons should assess patients with consecutive exotropia as though there had been no previous
surgery (Coopers dictum) and argued eloquently against the notion that consecutive exotropia surgery should attempt to undo what was done at the rst operation. Knowing details of previous procedures, however, will help avoid attempts to operate on muscles that may have already undergone maximum amounts of surgery. Management options for consecutive exotropia include observation, optical therapy, Botulinum toxin injections, and surgical correction. Optical treatment may include decreasing the hyperopic correction or prescribing minus lenses for emmetropic patients. For large deviations, the results of optical treatment may be only temporary,18 and surgical correction is usually indicated.2 A number of different surgical optionsincluding medial rectus advancement,19,20 medial rectus advancement and resection,2 lateral rectus recession,1,2,21 or combinations of these techniques have been described as producing good results for patients with consecutive exotropia. The decision regarding which surgical procedure is appropriate should be made after a thorough examination, proper consideration of the type and amount of previous surgery, and the presence of limitation of adduction or convergence insufciency. Unilateral surgery should be performed, if possible, on the amblyopic eye to minimize the risk to the better eye. We recommend advancing the medial rectus back to the original insertion if the amount of advancement is equivalent within 1 mm to the amount of resection advised for that angle of deviation. If there is a large discrepancy, the muscle can be positioned behind the original insertion by two double-armed hang-back sutures. Medial rectus advancement combined with lateral rectus recession is indicated for those patients with consecutive exotropia with limited adduction after bilateral medial rectus recession. This technique achieved satisfactory nal alignment in 29 of 42 patients (69%) in our study. It should be performed on the eye with weaker adduction19,20 or on the amblyopic eye. Medial rectus advancement alone has been well described by Biedner et al,18 who suggested a grading system of advancement up to the original insertion for deviations 25 PD; to 2mm beyond the original insertion for deviations from 30 to 35 PD; and
Journal of AAPOS Volume 8 Number 3 June 2004
Donaldson, Forrest, and Gole
235
concomitant resection or additional muscle surgery for deviations 35 PD. Bilateral lateral rectus recessions achieved satisfactory nal results in 6 of 7 patients (86%) in our series. This procedure is indicated for those patients with divergence excess or basic exotropia with normal medial rectus function, but it should be avoided in patients with limitation of adduction. According to Kushner and Fisher,22 the presence of even mild convergence insufciency indicates medial rectus underaction, which warrants either advancing the medial recti or performing extra lateral rectus recession. Fifty-nine patients underwent surgery and had a mean correction of 34.3 PD for distance. This is similar to results obtained by Biedner et al18 (mean 24 to 36 PD) and slightly greater than that obtained by Ohtsuki et al19 (24.0 PD for distance and 32.1 PD for near). The denition of successful alignment is controversial. It is most commonly taken as being within 10 PD of orthophoria. Kushner and Fisher23 argued that alignment within 8 to 10 PD of orthotropia should not be the standard to evaluate the outcome of strabismus surgery. He demonstrated that after surgery for infantile esotropia, orthotropia is a better outcome than small-angle esotropia, and esotropia is better than small-angle exotropia. When anticipating the postoperative ocular deviation, surgeons must take into account the most likely postoperative drift pattern. Exodrift after consecutive exotropia surgery was rst noted in the literature by Kerkhof and Houtman,15 who described it after bilateral medial rectus resection. In their series, almost all of the 18 patients demonstrated exodrift, and in 9 patients it resulted in a recurrence of exotropia. A similar postoperative exodrift was shown in patients after surgery for intermittent exotropia24,25 and in patients overcorrected after surgery for infantile esotropia.8,26,27 Our results demonstrated a signicant exodrift in 66% of patients in the rst 6 weeks after surgery for consecutive exotropia. This exodrift averaged 7.6 PD. A smaller esodrift of 6.0 PD was found in 10 patients (15%), whereas no drift occurred in 9 patients (15%). The exodrift was more prominent in those patients who were overcorrected at 1 week. Although numbers were small (n 6), most of those patients who were undercorrected, with a small-angle exotropia (0 to 10 PD) at 1 week, showed either no drift or a slight esodrift in the rst 6 weeks after surgery. Almost all of the exodrift occurred within the rst 6 weeks after surgery with little drift occurring between 6 weeks and 6 months. As far as we know, this is the rst study to quantify exodrift after surgery for consecutive exotropia (as distinct from intermittent exotropia). This exodrift suggests that the ideal alignment within the rst week after surgery for consecutive exotropia should be a small-angle esotropia of 5 to 10 PD. However, an alignment 10 PD of esotropia at 1 week is undesirable and would result in a large increase in the number of
patients with long-standing overcorrection. The cause of the postoperative exodrift is not known. There was no evidence in this study that it is related to amblyopia. It is more prominent in those patients who are initially overcorrected to esotropia, therefore resulting in a drift toward orthotropia in these patients. This was a retrospective study and as such shares those limitations common to any such study. A number of investigators have argued that assessment of the sensory state is not important in the decision to operate, or in the planning of surgery, for manifest strabismus.28 Although we did not record data regarding the preoperative and postoperative sensory states, overcorrection of consecutive exotropia may only be appropriate for patients with adequate fusional potential. This was the case in the study by Dankner et al29 who showed that patients with acquired esotropia achieved better results with overcorrections, but this happened only in patients with adequate fusional potential. Consecutive exotropia is not an uncommon result of esotropia surgery and may not appear until many years after infantile esotropia surgery. Surgical correction of consecutive exotropia is successful in the majority of patients, so a fear of consecutive exotropia should not delay or discourage surgery for infantile esotropia.29 A number of surgical options are available for correction of consecutive exotropia. Based on our experience, we recommend lateral rectus recession ( adjustable sutures) and medial rectus advancement as a suitable procedure. There is an exotropic drift after consecutive exotropia surgery, most of which occurs within the rst 6 weeks after surgery. We conclude that a suitable ocular alignment immediately after surgery for consecutive exotropia is a small-angle esotropia of 5 to 10 PD.
References
1. Cooper EL. The surgical management of secondary exotropia. Trans Am Acad Ophthalmol Otolaryngol 1961;65:595-608. 2. Mittleman D, Folk ER. The surgical treatment of overcorrected esotropia. J Pediatr Ophthalmol Strabismus 1979;16:156-9. 3. Arruga A. Surgical overcorrections. J Pediatr Ophthalmol 1965;2:1522. 4. Bietti GB, Bagolini B. Problems related to surgical overcorrections in strabismus surgery. J Pediatr Ophthalmol 1965;2:11-4. 5. Windsor CE. Surgically overcorrected esotropia: a study of its causes, sensory anomalies, fusional results and management. Am Orthopt J 1966;16:8-15. 6. Bradbury JA, Doran RML. Secondary exotropia: a retrospective analysis of matched cases. J Pediatr Ophthalmol Strabismus 1993;30: 163-6. 7. Stager DR, Weakley DR, Everett M, Birch EE. Delayed consecutive exotropia following 7-millimeter bilateral medial rectus recession for congenital esotropia. J Pediatr Ophthalmol Strabismus 1994;31:14750. 8. Yazawa K. Postoperative exotropia. J Pediatr Ophthalmol Strabismus 1981;18:58-64. 9. Rosenbaum AL, Jampolsky A, Scott AB. Bimedial recession in high AC/A esotropia. Arch Ophthalmol 1974;91:251-3. 10. Pickering JD, Simon JW, Lininger LL, Melsopp KB, Pinto GL. Exaggerated effect of bilateral medial rectus recession in develop-
236 Donaldson, Forrest, and Gole
mentally delayed children. J Pediatr Ophthalmol Strabismus 1994; 31:374-7. Folk ER, Miller MT, Chapman L. Consecutive exotropia following surgery. Br J Ophthalmol 1983;67:546-8. Ing M, Costenbader FD, Parks MM. Early surgery for congenital esotropia. Am J Ophthalmol 1966;61:1419-27. Wright KW. Color atlas of ophthalmic surgery: strabismus. Philadelphia (PA): Lippincott; 1991. Parks MM. Concomitant exodeviations. In: Tasman W, Jaeger EA, editors. Duanes clinical ophthalmology. Vol 1. Philadelphia (PA): Lippincott; 2000. p. 12. Kerkhof TB, Houtman WA. Late consecutive exodeviations. Doc Ophthalmol 1992;82:65-71. Von Noorden GK. Binocular vision and ocular motility: theory and management of strabismus. 5th ed. St Louis (MO): Mosby; 1996. p. 311. Von Noorden GK. Binocular vision and ocular motility: theory and management of strabismus. 5th ed. St Louis (MO): Mosby; 1996. p. 334. Biedner B, Yassur Y, David R. Advancement and reinsertion of one medial rectus muscle as treatment for surgically overcorrected esotropia. Binocul Vis Strabismus Q 1991;6:197-200. Ohtsuki H, Hasebe S, Tadokoro Y, Kobashi R, Watanabe S, Okano M. Advancement of medial rectus muscle to the original insertion for consecutive exotropia. J Pediatr Ophthalmol Strabismus 1993;30: 301-5. Patel AS, Simon JW, Lininger LL. Bilateral lateral rectus recession for consecutive exotropia. J AAPOS 2000;4:291-4.
Journal of AAPOS Volume 8 Number 3 June 2004
21. Kushner BJ. Surgical pearls for the management of exotropia. Am Orthopt J 1992;42:65-71. 22. Kushner BJ, Fisher M. Is alignment within 8 prism diopters of orthotropia a successful outcome for infantile esotropia surgery? Arch Ophthalmol 1996;114:176-80. 23. Scott WE, Keech R, Mash AJ. The postoperative results and stability of exodeviations. Arch Ophthalmol 1981;99:1814-8. 24. Kushner BJ, Fisher MR, Lucchese NJ, Morton GV. Factors inuencing response to strabismus surgery. Arch Ophthalmol 1993;111: 75-9. 25. Arthur BW, Smith JT, Scott WE. Long-term stability of alignment in the monoxation syndrome. J Pediatr Ophthalmol Strabismus 1989;5:225-31. 26. Caputo AR, Guo S, Wagner RS, Picciano MV. Preferred postoperative alignment after congenital esotropia surgery. Ann Ophthalmol 1990;22:269-72. 27. Jampolsky A. A simplied approach to strabismus diagnosis. In: Burian HM, Dunlap EA, Dyer JA, Fletcher MC, Jampolsky A, Knapp P, Parks MM, editors. Symposium on strabismus: transactions of the New Orleans Academy of Ophthalmology. St Louis (MO): Mosby; 1971. p. 89-90. 28. Dankner SR, Mash AJ, Jampolsky A. Intentional surgical overcorrection of acquired esotropia. Arch Ophthalmol 1978;96:184852. 29. Parks MM. Concomitant esodeviations. In: Tasman W, Jaeger EA, editors. Duanes clinical ophthalmology. Vol 1. Philadelphia (PA): Lippincott; 2000. p. 13.
11. 12. 13. 14.
15. 16.
17.
18.
19.
20.
An Eye on the Arts The Arts on the Eye
The two stood before Akbar, who was resting on his bed with his eyes open. Murtaza Beg whispered his praise for the emperor, then started to narrate a storythe story of an unpardonable crime. He told Akbar of an unfortunate artist, born of a master and himself a genius, who had displeased his emperor. But his crime was a strange one . . . Akbar stopped him with a raised hand. He asked Bihzad to come forward. He approached with a few measured steps, and started to recite a prayer. Facing the bed, Bihzad prostrated himself with his forehead touching the ground. The emperor rose from his bed. Holding Bihzads shoulder, he brought his face close to his, staring at the patch over his eyes. In a swift move one with which hed sever a deers neck in a hunt he ung open the blindfold. Bihzad saw the green jade cup full of Akbars blood. He saw the mole on Akbars cheek, now a dried cherry. He started to cry. The emperor held his face, tears running down his hands. You are not an artist, Akbar told him. You are a saint, Bihzad. Only a saint is truly blind, seeing none but the God inside him. He raised him from the oor, drew him towards his bed, made him sit by his side. He kept on looking into his face for a long time. Then he spoke, still in the voice of the emperor. But I want you to turn into an artist for the last time. Kunal Basu (from The Miniaturist)
S-ar putea să vă placă și
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (120)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- Horkheimer - Traditional and Critical Theory (1937)Document28 paginiHorkheimer - Traditional and Critical Theory (1937)timsvh7059Încă nu există evaluări
- Digital Matte Painting: Our Experts This IssueDocument5 paginiDigital Matte Painting: Our Experts This IssueacsamsonÎncă nu există evaluări
- Sudoku ChallengeDocument3 paginiSudoku ChallengejbahalkehÎncă nu există evaluări
- Phrasal Verbs Cut Do GetDocument26 paginiPhrasal Verbs Cut Do Getjbahalkeh100% (1)
- Berlin - THE PURPOSE OF PHILOSOPHYDocument8 paginiBerlin - THE PURPOSE OF PHILOSOPHYjbahalkeh7570Încă nu există evaluări
- Structure of A PaperDocument6 paginiStructure of A PaperjbahalkehÎncă nu există evaluări
- IC RetinoblastomaDocument10 paginiIC RetinoblastomajbahalkehÎncă nu există evaluări
- Antimalarial DrugsDocument18 paginiAntimalarial DrugsjbahalkehÎncă nu există evaluări
- All Quiet On The Western FrontDocument73 paginiAll Quiet On The Western FrontjbahalkehÎncă nu există evaluări
- 5a. Marx - The Fetishism of CommoditiesDocument2 pagini5a. Marx - The Fetishism of Commoditiescs1702Încă nu există evaluări
- Research Method (DLM Slide)Document5 paginiResearch Method (DLM Slide)sahirbuleÎncă nu există evaluări
- Inverse Function: DefinitionsDocument11 paginiInverse Function: Definitionsjbahalkeh100% (1)
- International System of UnitsDocument11 paginiInternational System of UnitsjbahalkehÎncă nu există evaluări
- 400 Bad Request 400 Bad Request Nginx/1.2.9Document128 pagini400 Bad Request 400 Bad Request Nginx/1.2.9jbahalkehÎncă nu există evaluări
- Karl Marx Poverty of PhilosophyDocument84 paginiKarl Marx Poverty of PhilosophyjbahalkehÎncă nu există evaluări
- Objective Plus Subjective Factors of Socialist RevolutionDocument13 paginiObjective Plus Subjective Factors of Socialist RevolutionjbahalkehÎncă nu există evaluări
- 400 Bad Request 400 Bad Request Nginx/1.2.9Document17 pagini400 Bad Request 400 Bad Request Nginx/1.2.9jbahalkehÎncă nu există evaluări
- Koffi Annan Freedon From Fear Ch3Document12 paginiKoffi Annan Freedon From Fear Ch3jbahalkehÎncă nu există evaluări
- Zakaria Dont Rush To War With IranDocument1 paginăZakaria Dont Rush To War With Iranjbahalkeh7570Încă nu există evaluări
- Sanders DR Clinical Trial of The Implantable Contact Lens For Moderate To High MyopiaDocument25 paginiSanders DR Clinical Trial of The Implantable Contact Lens For Moderate To High MyopiajbahalkehÎncă nu există evaluări
- Maastricht Treaty: Navigation SearchDocument7 paginiMaastricht Treaty: Navigation SearchjbahalkehÎncă nu există evaluări
- Education: Early Years Arts and Sciences Bachelor in LebanonDocument6 paginiEducation: Early Years Arts and Sciences Bachelor in LebanonjbahalkehÎncă nu există evaluări
- 400 Bad Request 400 Bad Request Nginx/1.2.9Document33 pagini400 Bad Request 400 Bad Request Nginx/1.2.9jbahalkehÎncă nu există evaluări
- A Man For All SeasonsDocument75 paginiA Man For All SeasonsSamik DasguptaÎncă nu există evaluări
- 400 Bad Request 400 Bad Request Nginx/1.2.9Document48 pagini400 Bad Request 400 Bad Request Nginx/1.2.9jbahalkehÎncă nu există evaluări
- Impact Factor Ranking JournalDocument2 paginiImpact Factor Ranking JournaljbahalkehÎncă nu există evaluări
- Frederick Engels Socialism Utopian and ScientificDocument23 paginiFrederick Engels Socialism Utopian and ScientificjbahalkehÎncă nu există evaluări
- Khrushchev Secret Speech The Cult of The IndividualDocument27 paginiKhrushchev Secret Speech The Cult of The IndividualjbahalkehÎncă nu există evaluări
- Article Processing ChargesDocument4 paginiArticle Processing ChargesjbahalkehÎncă nu există evaluări
- Refractive Surgery Yanoff 2Document4 paginiRefractive Surgery Yanoff 2jbahalkehÎncă nu există evaluări
- Ludwig WittgensteinDocument22 paginiLudwig WittgensteinjbahalkehÎncă nu există evaluări
- Color Constancy at A Pixel PDFDocument2 paginiColor Constancy at A Pixel PDFStephanieÎncă nu există evaluări
- 1.ocular Biometry (Full) SEGi UDocument51 pagini1.ocular Biometry (Full) SEGi UDiana PhiriÎncă nu există evaluări
- Session 5Document16 paginiSession 5Noorullah ShariffÎncă nu există evaluări
- ASLAM A Dual Fisheye Stereo Edge SLAMDocument2 paginiASLAM A Dual Fisheye Stereo Edge SLAMDimas de la PeñaÎncă nu există evaluări
- Tonometry 1Document4 paginiTonometry 1Ashty RzgarÎncă nu există evaluări
- Computer Vision Syndrome: Dean J. Dotulong, Laya M. Rares, Imelda H.M. NajoanDocument6 paginiComputer Vision Syndrome: Dean J. Dotulong, Laya M. Rares, Imelda H.M. NajoanSteven Wisma KuncoroÎncă nu există evaluări
- White BalanceDocument4 paginiWhite Balancejeffreygovender5745Încă nu există evaluări
- Determination of Fruit Ripeness Degree of Carabao MangoDocument5 paginiDetermination of Fruit Ripeness Degree of Carabao MangoJamie VillaceranÎncă nu există evaluări
- Hasselblad Historical - Focal Length ComparisonsDocument3 paginiHasselblad Historical - Focal Length ComparisonsBrad BaoÎncă nu există evaluări
- TemplatesDocument1 paginăTemplatesSumaya SarhedÎncă nu există evaluări
- 18.IJAEST Vol No 6 Issue No 2 Development of Vision Based Iris Recognition System 277 281Document5 pagini18.IJAEST Vol No 6 Issue No 2 Development of Vision Based Iris Recognition System 277 281helpdesk9532Încă nu există evaluări
- KeratometryDocument3 paginiKeratometrycarol_marie_3Încă nu există evaluări
- Made By:-Shrish Ojha and Aryaman Singh MarjaraDocument34 paginiMade By:-Shrish Ojha and Aryaman Singh MarjaraSanskriti JoshiÎncă nu există evaluări
- Anamorphic ImageDocument7 paginiAnamorphic Imageapi-233934922Încă nu există evaluări
- How To Invert Colors in Photoshop 2021Document2 paginiHow To Invert Colors in Photoshop 2021designwÎncă nu există evaluări
- Color 1 Color 2 Color 3 Color 4 Color 5Document4 paginiColor 1 Color 2 Color 3 Color 4 Color 5Jo MaÎncă nu există evaluări
- AmericanCinematographer February2022Document79 paginiAmericanCinematographer February2022Fede GiardinaÎncă nu există evaluări
- Anaet 2Document3 paginiAnaet 2hidrisdmnk_747467972Încă nu există evaluări
- Underwater Image Enhancement For Improving The Visual Quality by CLAHE TechniqueDocument5 paginiUnderwater Image Enhancement For Improving The Visual Quality by CLAHE TechniqueijsretÎncă nu există evaluări
- Graphic Design VocabularyDocument10 paginiGraphic Design VocabularyCarlos ReyesÎncă nu există evaluări
- Submitted By: Ibno, Norhuda J. BN 322-A: Non-Infectious Dry WasteDocument3 paginiSubmitted By: Ibno, Norhuda J. BN 322-A: Non-Infectious Dry WasteMhay JimlanoÎncă nu există evaluări
- Versacol HP Brochure-Full RangeDocument4 paginiVersacol HP Brochure-Full RangeDuc NguyenÎncă nu există evaluări
- 05 - Stereoplotter ModuleDocument10 pagini05 - Stereoplotter ModuleAbay GenetÎncă nu există evaluări
- Inspiration FileDocument5 paginiInspiration Filejttizzle1995Încă nu există evaluări
- A Peninsula Ibérica 5º AnoDocument38 paginiA Peninsula Ibérica 5º AnoIsaura MiguelÎncă nu există evaluări
- 0416 801 Alcon SuppliedDocument8 pagini0416 801 Alcon SuppliedEnda TambajongÎncă nu există evaluări
- Asociación de Municipios: Escuela Superior de Administración Pública - ESAP BogotáDocument29 paginiAsociación de Municipios: Escuela Superior de Administración Pública - ESAP BogotáKaren RamirezÎncă nu există evaluări
- Marta BevacquaDocument13 paginiMarta Bevacquaapi-488655077Încă nu există evaluări
- Strategi Dan Praktik DIBSDocument39 paginiStrategi Dan Praktik DIBSDiaz ZulfaÎncă nu există evaluări