Documente Academic
Documente Profesional
Documente Cultură
Niacin MOA
Încărcat de
Sri Nowo MinartiDescriere originală:
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Niacin MOA
Încărcat de
Sri Nowo MinartiDrepturi de autor:
Formate disponibile
Niacin Mechanism of Action Thomas Dayspring MD, FACP
It is only recently that we have begun to understand many of the complexities of niacins mechanism of action. Like most of lipid-modulating agents much of its action is mediated through nuclear transcription factors that regulate lipid homeostasis. Through some of its metabolites namely prostaglandins D2 and J2, niacin influences PPARs, especially the gamma isoforms. Since 1993 Cesare Sitori (of apoA-I Milano fame) has been calling niacin as well as fibrates, fraudulent fatty acids meaning they in essence trick PPARs into believing they are FA and PPAR agonism occurs (Eur J Clin Invest 1993;23:686-689). Only recently was the niacin receptor called HM74A, identified. By the way, no has discovered the natural ligand for HM74A. Lancet 2004; 363: 189294. 1) Classically it has been taught that niacins main action is to inhibit triacylglycerol or triglyceride (TG) hydrolysis (lipolysis) in adipose tissue. By attaching to the niacin receptor (HM74A) in adipocytes, hormone sensitive lipase (now being called triglyceride lipase) is inhibited. This reduces lipolysis (hydrolysis of TG) resulting in less fatty acids (FA) being secreted into plasma. This reduction of FA denies the liver its main substrate of TG production. However although there may be a transient reduction in FA release from adipocytes it is now known there is within a few hours a sudden surge in FA release, which likely plays a role in the insulin resistance associated with niacin use. 2) Within hepatocytes niacin both induces beta-oxidation of fatty acids (burns fat) and inhibits FA synthesis (lipogenesis). This reduction of hepatic FA reduces the main substrate for TG synthesis. Arterioscler Thromb Vasc Biol. 1999;19:1051-1059. 3) Niacin inhibits the enzyme diacyl-glycerol acyl transferase 2 (DGAT2) which esterifies monoglycerol and diglycerol, crucial enzymatic steps for TG production. J. Lipid Res. 45 (2004) 18351845, Arterioscler Thromb Vasc Biol. 1999;19:1051-1059. Steps 2 and 3 are extremely similar to those of fibrates and likely are mediated by PPAR agonism. Some experts are now classifying niacin as a fibrate. 4) Apolipoprotein B 100 is the main surface apoprotein of the betalipoproteins and is synthesized in hepatocytes and is either lipidated with sterols, phospholipids and TG or immediately degraded through a ubiquination process. The niacin-induced reduction in TG synthesis clearly reduces lipid substrate available for lipidation of apoB leading to increased post-translational degradation of apoB and ultimately less VLDL particles are produced. Ultimately this leads to less IDL and LDL and a reduction in apolipoprotein B (a very significant CV risk factor). Arterioscler Thromb Vasc Biol. 1999;19:1051-1059 5) The reduced numbers of VLDLs, produced in patients using niacin are also less likely to be TG-rich: this reduces cholesteryl ester transfer protein (CETP) activity reducing less swapping (transfer) of TG for cholesteryl ester (CE) between VLDL and LDL and HDLs. This will increase LDL and HDL size. Larger LDLs make the surface apoB assume a conformation more amenable to recognition and endocytosis by LDL-receptors: hepatic internalization of apoB particles of which LDLs are by far the most numerous, is now termed indirect reverse cholesterol transport and of course leads to reductions in LDL-C, non-HDL-C, VLDL-C, LDL-P and apoB. 6) Reduction of large, TG-rich VLDLs improves many rheologic factors like blood viscosity, and likely lessens FA induced endothelial dysfunction. 7) Niacin's main metabolite is prostaglandin D2. In turn its metabolite is prostaglandin J2 which is a potent PPAR-gamma agonist. Thus Niacin will have PPAR gamma activity. This likely is associated with many of the FA actions described above as well some cardioprotection actions as follows: In the liver PPAR gamma cross communicates with the Liver X receptor (LXR). LXRs main function is to prevent intracellular sterol toxicity. LXRs accomplish this through many functions including the increased esterification of free cholesterol to cholesteryl ester, via the enzyme
Niacin Mechanism of Action Thomas Dayspring MD, FACP
acylcholesterol acyl transferase (ACAT), and upregulation of several membrane sterol efflux transporters of the ATP Biding Cassette (ABC) Transporter family. Specifically, ABCA1 transporters efflux cholesterol from within cells into a cholesterol acceptor protein, namely apoA-I (the HDL precursor protein). Thus niacin induces the liver to rapidly lipidate the nascent HDL (prebeta) inducing its maturation into smaller and then large, more mature alpha- HDL particles (hepatic lipidation of HDLs will raise HDL-C, but is unlikely to be cardioprotective). Fortunately ABCA1 can also be expressed in arterial wall foam cells (sterol-laden macrophages). In the arterial wall, niacin through its metabolite induced PPAR gamma activity through cross-talk with the LXR would enhance macrophage RCT. Although macrophage RCT is cardioprotective, it does not affect the total HDL-C level. The PPAR gamma activity of niacin also causes an increase in expression of a scavenger receptor located in arterial wall macrophages called CD 36. This macrophage-receptor internalizes oxidized LDL particles leading to foam cell formation. However, the cholesterol within the macrophage can then be excreted into HDLs via the upregulated ABCA1. In review, niacin in effect makes the macrophages clear or internalize atherogenic LDLs, but immediately gets the cholesterol transferred to an HDL via induction of macrophage RCT. Biochemical Pharmacology 67 (2004) 411419 8) Niacin inhibits hepatic lipase (HL). This is a major enzyme in the LDL and HDL remodeling process. By removing (hydrolyzing) TG and surface phospholipids HL remodels large TG-rich LDLs and HDLs into small particles. Because the niacin effect on HL reduces HDL lipolysis patients on niacin will typically have increases in the number of larger HDL particles (which carry more cholesterol). This is certainly another way Niacin raises HDL-C. Circulation. 1999;99:19591964.) 9) The liver has three receptors which play a role in the direct RCT pathway (HDLs returning cholesterol to the liver for delipidation or internalization). The hepatic scavenger receptor B1 (SRB1) which attaches to and delipidates larger HDLs and then returns the empty smaller HDL to plasma is not affected by niacin. LDL receptors (LDLr) can internalize HDLs that are rich in apoE (usually large HDL species). Unlike statins or ezetimibe, niacin does not affect LDLr expression. There is also an HDL holoparticle or catabolism receptor (apoA-I beta chain synthase) which attaches to and internalizes (endocytoses) large HDL particles. This receptor is down-regulated by niacin enabling large HDLs to have a longer half life (clearly that would raise HDL-C and apoAI and HDL-P). If the HDLs are functional (capable of performing macrophage RCT), it is likely beneficial for HDLs to have increased half-lifes as they would have more time to perform their multiple cardioprotective actions. Nature Vol 421 p 75 January 2003 With respect to macrophage RCT, it is preferable to have it performed by smaller, unlipidated apoA-I or prebeta HDLs. Unlike fibrates niacin does not increase production of apoA-I but rather by delaying the catabolism of the large HDL, increases the number of larger, mature alpha HDLs (explaining the rise in HDL-C so characteristic of niacin use). Arterial wall foam cells are complex cells capable of synthesizing multiple proteins involved with HDL remodeling, such as lipoprotein, endothelial and hepatic lipase and phospholipid transfer protein. As the niacin-induced large mature HDLs (each usually carrying 3-4 apoA-I molecules approach the foam cells they are subject to lipolysis and as they reduce in size, apoA-I disassociate. The now unlipidated apoA-I is in a perfect position to induce efficient macrophage RCT. Although macrophage RCT would not change HDL-C it would increase plaque delipidation. 10) Because niacin like fibrates is so good at reducing TG (as explained above) there will be less CETP activity. That would keep cholesterol within LDLs, leading to larger LDLs which are more amenable to hepatic LDLr internalization Of course niacin (and fibrates) to not reduce CETP activity anywhere near the level that torcetrapib (a powerful CETP inhibitor), a drug associated with CV as adversity) did. If one maximally upregulates LDLr (statins, ezetimibe, bile acid sequestrants), the shifting of LDL size would help maximize hepatic LDL particle endocytosis (indirect RCT) leading to synergistic reductions in VLDL-C, LDL-C, non-HDL-C, apoB and LDL-P.
Niacin Mechanism of Action Thomas Dayspring MD, FACP
11) Niacin through mechanisms that are not well understood, but almost certainly related to its PPAR gamma agonism has multiple pleiotropic effects such as increasing adiponectin, reducing C-reactive protein (especially when combined with a statin) and lipoprotein associated phospholipase A2. It also seems to have antioxidant properties. So if we had to sum up: here is niacin's lipid MOA and how it may or may not relate to cardioprotection. 1) Lower apoB, LDL-C and Non HDL-C through its TG lowering abilities 2) Improves HDL functionality by increasing macrophage RCT (which does not raise HDL-C) 3) Lipidates HDLs by upregulating hepatic ABCA1 and then keeps them mature (larger) by inhibiting HL: this raises HDL-C considerably but this increase does not likely explain niacins cardioprotective actions. One might argue that it is better if the liver lipidates HDLs with cholesteryl ester rather than lapidating apoB particles (VLDLs). 4) Prevents hepatic delipidation of HDLs which increases the half life of circulating large HDL, increasing apoA-I and HDL-P: this of course also helps raise HDL-C and is likely cardioprotective if and only if those HDLs are functional and perform macrophage RCT (we have no way of assaying that). As speculated these larger HDLs may release unlipidated apoA-I upon exposure to foam cells. 5) Multiple pleiotropic effects Since we cannot measure HDL functionality, I believe the most important test to follow that should ensure cardioprotection is apoB or LDL-P. Since the niacin induced rise in HDL-C is expected (I'd be alarmed if there was no HDL-C increase) but has no correlation with HDL functionality, I am not sure that following HDL-C on niacin tells you anything and thus following Non HDL-C or the TC/HDL-C ratio would not be as good as following apoB or LDL-P which is now recommended by ADA/ACC. Although we still await serious, well empowered modern outcome data with niacin, we certainly have good data from very small trials that niacin added to a statin improves angiographic findings, lessens carotid intimal thickening and reduces clinical events and is well tolerated. We await confirmation of this in the much larger AIM HIGH trial which is underway. Clearly they are not seeing the 90% event reduction in AIM HIGH that occurred in HATS or the trial would have been stopped for ethical reasons.
S-ar putea să vă placă și
- Association Between Smoking Behavior and LDLDocument1 paginăAssociation Between Smoking Behavior and LDLSri Nowo MinartiÎncă nu există evaluări
- Afroz - Lipid ProfileDocument6 paginiAfroz - Lipid ProfileSri Nowo MinartiÎncă nu există evaluări
- Weight-For-Age GIRLS: 2 To 5 Years (Z-Scores)Document1 paginăWeight-For-Age GIRLS: 2 To 5 Years (Z-Scores)Gibson HorasÎncă nu există evaluări
- Daftar PustakaDocument1 paginăDaftar PustakaSri Nowo MinartiÎncă nu există evaluări
- Uroanalisis AnormalDocument13 paginiUroanalisis AnormalMyke EstradaÎncă nu există evaluări
- Nkcells Further ReadDocument1 paginăNkcells Further ReadSri Nowo MinartiÎncă nu există evaluări
- Abnormal Uterine Bleeding: Frequently Asked Questions FAQ095 Gynecologic ProblemsDocument3 paginiAbnormal Uterine Bleeding: Frequently Asked Questions FAQ095 Gynecologic ProblemsErwinÎncă nu există evaluări
- Cover Skripsi Bahasa InggrisDocument1 paginăCover Skripsi Bahasa InggrisSri Nowo MinartiÎncă nu există evaluări
- Nephrotic Syndrome in Adults 2009Document6 paginiNephrotic Syndrome in Adults 2009Mutiara RizkyÎncă nu există evaluări
- Management of Protozoal Diarrhoea in HIV DiseaseDocument6 paginiManagement of Protozoal Diarrhoea in HIV DiseaseSri Nowo MinartiÎncă nu există evaluări
- 0709Document4 pagini0709Sri Nowo MinartiÎncă nu există evaluări
- VancouverDocument11 paginiVancouverAndi Firman MubarakÎncă nu există evaluări
- Management of Protozoal Diarrhoea in HIV DiseaseDocument6 paginiManagement of Protozoal Diarrhoea in HIV DiseaseSri Nowo MinartiÎncă nu există evaluări
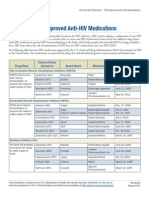
- ApprovedMedstoTreatHIV FS enDocument2 paginiApprovedMedstoTreatHIV FS enSri Nowo MinartiÎncă nu există evaluări
- Alcohol 10 QuestionnaireDocument1 paginăAlcohol 10 Questionnaireyash_magooÎncă nu există evaluări
- Eur Heart J 2003 Fröhlich 1365 72Document8 paginiEur Heart J 2003 Fröhlich 1365 72Sri Nowo MinartiÎncă nu există evaluări
- Dysuria in AdultsDocument8 paginiDysuria in AdultsSi vis pacem...Încă nu există evaluări
- Frequency of Renal Stone Disease in Patients With Urinary Tract InfectionDocument3 paginiFrequency of Renal Stone Disease in Patients With Urinary Tract InfectionSri Nowo MinartiÎncă nu există evaluări
- Frequency of Renal Stone Disease in Patients With Urinary Tract InfectionDocument3 paginiFrequency of Renal Stone Disease in Patients With Urinary Tract InfectionSri Nowo MinartiÎncă nu există evaluări
- The Effect of Human Recombinant Erythropoietin On Prevention of Anemia of PrematurityDocument6 paginiThe Effect of Human Recombinant Erythropoietin On Prevention of Anemia of PrematuritySri Nowo MinartiÎncă nu există evaluări
- 55 259Document6 pagini55 259Sri Nowo MinartiÎncă nu există evaluări
- Uroanalisis AnormalDocument13 paginiUroanalisis AnormalMyke EstradaÎncă nu există evaluări
- Difco BBL Mueller Hinton Agar BrothDocument5 paginiDifco BBL Mueller Hinton Agar BrothSri Nowo MinartiÎncă nu există evaluări
- ResourceDocument5 paginiResourceSri Nowo MinartiÎncă nu există evaluări
- Corrections: Theodore J. Cicero, Ph.D. Matthew S. Ellis, M.P.EDocument1 paginăCorrections: Theodore J. Cicero, Ph.D. Matthew S. Ellis, M.P.ESri Nowo MinartiÎncă nu există evaluări
- Corrections: Theodore J. Cicero, Ph.D. Matthew S. Ellis, M.P.EDocument1 paginăCorrections: Theodore J. Cicero, Ph.D. Matthew S. Ellis, M.P.ESri Nowo MinartiÎncă nu există evaluări
- EpoDocument15 paginiEpoSri Nowo MinartiÎncă nu există evaluări
- Etiology and Evaluation of Diarrhea in AIDS: A Global Perspective at The MillenniumDocument10 paginiEtiology and Evaluation of Diarrhea in AIDS: A Global Perspective at The MillenniumSri Nowo MinartiÎncă nu există evaluări
- Am J Clin Nutr 2008 Kupka 1802 8Document7 paginiAm J Clin Nutr 2008 Kupka 1802 8Sri Nowo MinartiÎncă nu există evaluări
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (119)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- VERMONT CHILD HEALTH IMPROVEMENT PROGRAM DEVELOPMENTAL SCREENING "PREFERRED TOOL LISTDocument27 paginiVERMONT CHILD HEALTH IMPROVEMENT PROGRAM DEVELOPMENTAL SCREENING "PREFERRED TOOL LISTsandeep gurjarÎncă nu există evaluări
- Administering Intramuscular Injections To Children - What Does The Evidence Say?Document8 paginiAdministering Intramuscular Injections To Children - What Does The Evidence Say?ZACHARIAH MANKIRÎncă nu există evaluări
- Manual Airway Opening TechniquesDocument3 paginiManual Airway Opening TechniquesnfacmaÎncă nu există evaluări
- Bleeding TimeDocument47 paginiBleeding Timechickenbacon34Încă nu există evaluări
- Treating Deep Overbite MalocclusionDocument1 paginăTreating Deep Overbite MalocclusionZhyema ZhyedeeÎncă nu există evaluări
- CPSP Basic Medical Sciences Course Dec 2011Document3 paginiCPSP Basic Medical Sciences Course Dec 2011asifcbmÎncă nu există evaluări
- Kamen Winner First 15 Tyler Marceca The Disciple ProgramDocument16 paginiKamen Winner First 15 Tyler Marceca The Disciple ProgramJohn GotesÎncă nu există evaluări
- NIDCD Noise Induced Hearing LossDocument4 paginiNIDCD Noise Induced Hearing LossquuyiixÎncă nu există evaluări
- The God Helmet PDFDocument5 paginiThe God Helmet PDFTiara Grhanesia DenashuryaÎncă nu există evaluări
- LDH and LeukemiaDocument4 paginiLDH and LeukemiaRicardo BallesterosÎncă nu există evaluări
- Soal Bahasa Inggris SMT 3 2017 2018Document7 paginiSoal Bahasa Inggris SMT 3 2017 2018Tuti Alawiyah100% (1)
- Maternal and Child Health NursingDocument78 paginiMaternal and Child Health NursingJerecho Ramon R. Arciaga100% (1)
- Standard Operating Procedure Manual For Obstetrics and Midwifery ServicesDocument64 paginiStandard Operating Procedure Manual For Obstetrics and Midwifery ServicesTmanoj Praveen75% (4)
- Fluid Resuscitation - Dita AditianingsihDocument48 paginiFluid Resuscitation - Dita AditianingsihGalih Wicaksono100% (1)
- Near Death ExperienceDocument18 paginiNear Death ExperienceVikas Saini100% (1)
- Kannur University (Examination Branch) 25 October 2011 (The Mark Is Provisional. Kindly Confirm The Same With The Mark List Issued by The University)Document16 paginiKannur University (Examination Branch) 25 October 2011 (The Mark Is Provisional. Kindly Confirm The Same With The Mark List Issued by The University)bobby_5300Încă nu există evaluări
- Efficient Antibiotic Bead Production TechniqueDocument5 paginiEfficient Antibiotic Bead Production Techniqueratnav_ratanÎncă nu există evaluări
- Quiz 2 - Healthcare Quality and Patient SafetyDocument3 paginiQuiz 2 - Healthcare Quality and Patient SafetyRaviraj Pishe100% (1)
- Reading ListDocument4 paginiReading Listmehmoodabid84Încă nu există evaluări
- Patient Health ProfileDocument4 paginiPatient Health ProfileChristopher WuÎncă nu există evaluări
- Position Paper Who ChinaDocument2 paginiPosition Paper Who Chinaapi-307248240Încă nu există evaluări
- 4 History of MassageDocument3 pagini4 History of MassageJoanna AaronÎncă nu există evaluări
- Complet Cardoio Pulmonary - Brochure NEW0.2 PDFDocument39 paginiComplet Cardoio Pulmonary - Brochure NEW0.2 PDFgladyannÎncă nu există evaluări
- Psychologist or School Psychologist or Therapist or CounselorDocument2 paginiPsychologist or School Psychologist or Therapist or Counselorapi-79222085Încă nu există evaluări
- Sepsis Power Point Slide Presentation - The Guidelines - Implementation For The FutureDocument25 paginiSepsis Power Point Slide Presentation - The Guidelines - Implementation For The Futuremontie13Încă nu există evaluări
- Contact DermatitisDocument11 paginiContact Dermatitismits98Încă nu există evaluări
- Pediatric NursingDocument29 paginiPediatric NursingjeshemaÎncă nu există evaluări
- Lingual Frenectomy With Electrocautery: Diagnostic Assessments For Case in PointDocument5 paginiLingual Frenectomy With Electrocautery: Diagnostic Assessments For Case in PointTasneem AbdÎncă nu există evaluări
- Upgrading a 63-Year-Old Philippine Public HospitalDocument77 paginiUpgrading a 63-Year-Old Philippine Public HospitalMark Ryan NagalesÎncă nu există evaluări
- Pediatric Drug DirectoryDocument404 paginiPediatric Drug DirectoryAlfitra Halil100% (1)