Documente Academic
Documente Profesional
Documente Cultură
Transfusion Practices in Massive Haemorrhage in Pre-Intensive and Intensive Care
Încărcat de
Jose Miguel Arce RomoDescriere originală:
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Transfusion Practices in Massive Haemorrhage in Pre-Intensive and Intensive Care
Încărcat de
Jose Miguel Arce RomoDrepturi de autor:
Formate disponibile
Vox Sanguinis (2011) 101, 230236
ORIGINAL PAPER
2011 The Author(s) Vox Sanguinis 2011 International Society of Blood Transfusion DOI: 10.1111/j.1423-0410.2011.01482.x
Transfusion practices in massive haemorrhage in pre-intensive and intensive care
R. Sinha & D. Roxby
Transfusion Services, Flinders Medical Centre, Bedford Park, SA, USA
Background and Objectives Primary resuscitation for massive haemorrhage often occurs in emergency departments or operating theatres, with ongoing resuscitation in the intensive care unit (ICU). The aim of the study was to retrospectively review transfusion practice in the pre-ICU phase and ICU for patients with massive haemorrhage. Materials and Methods From 1998 to 2006, we developed an electronically linked database of blood and blood product usage and laboratory data with clinical outcome. All patients who received 10 or more units of red cells and required ICU admission were included. Results Of 238 patients who required massive transfusion, 40 died early (within 24 h of massive transfusion), out of which 16 died in pre-ICU and 24 died in ICU. Comparatively this group of patients presented in the pre-ICU phase and on ICU admission, respectively, with coagulopathy (median international normalized ratio 16 and 21) and acidosis (median base decit )115 and )14 mmol l). These patients had median ratios of fresh frozen plasma (FFP) to red blood cells of 1:33 and 1:13 in the pre-ICU and ICU phases, respectively. Severity of coagulopathy indicated by INR at ICU admission [P = 004; area under receiver operator curve (ROC) = 069] and RBC transfused (P = 001) in 24 h associated with mortality. Conclusions Patients who died early were coagulopathic before and on ICU admission and did not correct their coagulopathy. This study also shows that coagulopathy is associated with an increased risk of mortality. Early and aggressive correction of coagulopathy for patients presenting with coagulopathy may be effective in improving mortality. Key words: coagulopathy, intensive care, massive transfusion.
Received: 17 October 2010, revised 8 February 2011, accepted 10 February 2011, published online 25 April 2011
Introduction
Primary resuscitation for massive haemorrhage often occurs in emergency departments or operating theatres, with ongoing resuscitation in the intensive care unit (ICU). Because massive transfusion (MT) can occur in elective settings (both surgical and non-surgical in nature) and for trauma, the approach to the management may differ based
Correspondence: Romi Sinha, Transfusion Services, Flinders Medical Centre, Flinders Drive, Bedford Park, SA 5042, USA. Email: romi.sinha@ health.sa.gov.au
on where patients are treated (i.e., the emergency department, operating theatre, or ICU), with different protocols for these settings. During MT, the use of blood products is not indicated by laboratory tests but is generally based on clinical parameters. Such an approach [1] and the complexity of treating massive bleeding [2] may result in suboptimal transfusion therapy, further contributing to poor outcomes. Existing transfusion guidelines advocate early administration of crystalloids and colloids in conjunction with transfusion of red blood cells (RBCs). The use of fresh frozen plasma (FFP) and platelets is recommended only for patients with
230
Transfusion practices in massive haemorrhage 231
microvascular bleeding and if prothrombin time partial thromboplastin time (PT APTT) values exceed 15 times the mid-point of reference range and platelet counts are below 50 109 l. In recent years, there has been increasing evidence that early and more intensive replacement of coagulation factors and platelets may improve the outcome of massive haemorrhage associated with trauma [37], and in patients presenting with ruptured aortic aneurysms [8]. Recent retrospective studies also have indicated that RBCs, plasma, and platelets should be administered in a 1:1:1 ratio to patients with massive bleeding. Some institutions have adopted a proactive and structured approach with predened ratios of blood products for patients with massive bleeding; mainly in the trauma setting [911]. It is not known whether this approach is better than a specic transfusion practice based on clinical parameters and laboratory investigations. This study was undertaken to evaluate laboratory management and transfusion practices for patients with MT. In particular, we wanted to determine (1) transfusion practices both in the pre-ICU and ICU phases of patients receiving MT and (2) how coagulopathy was addressed in both phases.
Methods
We conducted a retrospective study of patients with MT from two teaching hospitals in South Australia: Flinders Medical Centre, a 560-bed tertiary care hospital and trauma centre, and Repatriation General Hospital, a 220-bed teaching hospital. The list of patients with MT was linked to an epidemiology database for patient demographics and outcomes, a pathology database to determine laboratory results, and a transfusion database to determine blood and blood product usage. The study population included patients who received MT as a consequence of trauma, liver transplantation, or abdominal aortic aneurysm (AAA), cardiothoracic, obstetrics, or major abdominal orthopaedic surgery. Patients with a clinical diagnosis of gastrointestinal bleeding were excluded because of the difculty in clearly identifying pre-ICU and ICU admission. Because patients who were directly admitted to the ICU could be analysed only for the ICU phase but not the pre-ICU phase, they also were excluded. MT was dened as transfusion of at least 10 units of RBCs in a 24-h period from the start of the initial transfusion. The transfusion laboratory dened one apheresis unit of platelets as equivalent to four or ve individual platelet donations and one pool of cryoprecipitate as equivalent to ve individual donations. Coagulopathy was dened by an international normalized ratio (INR) of 15 and or an activated thromboplastin time (APTT) of at least 15 (15 times the mid-point of the reference range). The following
variables were recorded: sex, age, diagnosis, overall in-hospital mortality, and laboratory results such as platelet count, INR, APTT, and base decit (BD). The study was conducted in two parts. The rst section evaluated the overall laboratory [INR, platelet count, and base decit (BD)] and transfusion (RBCs, FFP, platelet units, cryoprecipitate, and FFP RBC and platelet RBC ratios) management of patients in the pre-ICU and ICU. The 24-h period of the MT episode was divided into pre-ICU and ICU phases. Laboratory data were analysed at baseline and on admission to the ICU. Blood products were analysed until the patients arrival in the ICU and during ICU resuscitation. The second part of the study evaluated the pre-ICU and ICU laboratory and transfusion management of patients by outcome. Patients were stratied into three outcome groups: group 1 included patients who survived; group 2, patients who died within 24 h of MT; and group 3, and patients who died after 24 h. Laboratory data at baseline, on ICU admission, and within 24 h of ICU admission were compared among the three groups. Blood and blood products transfused in the pre-ICU phase and in the ICU were also compared among the groups. Continuous data were presented as medians and interquartile ranges (IQRs). Blood products used during the pre-ICU and ICU phases of MT were compared between the subgroups by use of the KruskalWallis test (Table 3). The laboratory parameters at three stages (baseline, ICU admission, and 24 h after ICU admission) for the three MT groups were compared by use of the Friedman test. A multivariate logistic regression analysis was used to identify the risk factors associated with mortality in ICU. The level of statistical signicance was taken to be P < 005. Analyses were performed by IBMSPSS, Chicago, IL.
Results
During the 9-year period from 1998 to 2006, 238 patients were identied with MT. Of these, 220 were treated both in pre-ICU and ICU settings, and 18 were treated only in preICU settings. Patient characteristics are detailed in Table 1. The most frequent cause of surgery was abdominal aortic aneurysm (AAA), followed by trauma and abdominal surgery not associated with preceding trauma. The patients were categorised into a major elective category, which included liver transplantation and cardiothoracic and abdominal surgery, and an emergency category, which included AAA, trauma, and obstetric patients. Overall, the patients received a median of 16 (IQR 1222) units of RBCs, 6 (IQR 411) units of FFP, and 2 (IQR 13) units of platelets. Twenty-four patients received cryoprecipitate, and ve patients received recombinant factor VIIa.
2011 The Author(s) Vox Sanguinis 2011 International Society of Blood Transfusion, Vox Sanguinis (2011) 101, 230236
232 R. Sinha & D. Roxby
Table 1 Demographic variables and diagnoses of all 238 patients requiring massive transfusion Age, years Male sex Diagnostic group Abdominal aortic aneurysm Trauma Cardiothoracic surgery Liver transplantation Abdominal orthopaedic surgery Obstetrics Type of surgery Major elective surgery Emergency surgery 63 (4076) 175 (735%) 70 (294%) 73 (307%) 18 (176%) 12 (50%) 49 (206%) 16 (67%) 79 (331%) 159 (669%)
platelets in the remaining 24-h period of MT. The median FFP:RBC ratio was 1:13 (IQR 1:21:38) and the platelet RBC ratio was 1:4 (IQR 1:21:8).
Comparison of MT groups
Among the three outcome groups, group 1 consisted of 174 patients; group 2, 40 patients; and group 3, 24 patients. Although the age ranges were similar among the groups, the distribution of diagnostic groups was different, with group 2 consisting predominantly of abdominal aortic aneurysm (AAA) and trauma patients (Table 2). Sixteen patients (eight trauma and eight AAA patients) in group 2 died in the emergency department or operating room. The median time to death was 4 h (IQR 1563), and the main cause of death was haemorrhage. The remaining 24 patients died in the ICU. At the start of the pre-ICU phase, patients in group 2 presented with signicantly worse BDs (P = 002) and a trend to higher INRs (P = 005) than patients in groups 1 and 3 (Fig. 1). During the pre-ICU phase, patients in all three outcome groups received high-volume RBC transfusions, with patients in group 2 receiving more RBCs (P < 0001). Patients in all three outcome groups received similar amounts of FFP and platelets, with similar FFP RBC and platelet RBC ratios (Table 3). Additionally, patients in group 2 who died in the emergency department or operating theatre had a median platelet count of 150 109 l (IQR 96 109 l230 109 l), INR of 17 (1623), and BD of -24 (-278 to -85) mmol l. These patients received a median of 18 units (133305) of RBCs and 45 units (078) of FFP. A total of 31% of the patients (5 of 16) did not receive any FFP, and 44% (7 of 16) did not receive any platelets. On arrival at the ICU, patients in group 2 had signicantly lower platelet counts (P = 004), higher INRs (P < 0001), and worse BDs (P < 0001) than did patients in
Pre-ICU setting
Notably, coagulopathy was present in some patients treated in the pre-ICU phase. The INR and or APTT were obtained for 176 patients; 76 (432%) of them were coagulopathic, and 30 of the 76 (395%) were trauma patients. Thrombocytopenia was not a common feature, with 168 of 215 (781%) patients having a platelet count greater than 150 109 l. Additionally, 583% of the patients were acidotic: 88 of 151 patients with available BDs had base BDs lower than 6 mmol l. Coagulopathy was common in the trauma, liver transplantation, and obstetrics groups, and moderate to severe acidosis was observed in all diagnostic groups except the cardiac and abdominal orthopaedic groups (data not shown). Patients received a median of 12 (IQR 817) units of RBCs, 4 (IQR 27) units of FFP, and 1 (IQR 02) unit of platelets. The median FFP:RBC ratio was 1:3 (IQR 1:2 1:38) and platelet:RBC ratio was 1:10 (IQR 1:81:13). Among the diagnostic groups, signicant differences were observed with regard to transfusion of blood products and blood products ratios. Cardiac patients received signicantly fewer RBCs, and liver transplantation patients received higher plasma and platelet ratios than patients in other groups (data not shown).
Table 2 Demographic variables and diagnoses of patients requiring massive transfusion in three outcome groups Group 1 (n = 174) Age, years 605 (3776) Male sex 130 (747%) Diagnostic group Abdominal aortic aneurysm 49 (282%) Trauma 51 (293%) Cardiothoracic surgery 12 (69%) Liver transplantation 11 (63%) Abdominal orthopaedic surgery 38 (218%) Obstetrics 13 (75%) Group 2 (n = 40) Group 3 (n = 24)
ICU phase
Of the 238 patients, 220 were admitted to the ICU. Sixtynine percent (146 212) of the patients were coagulopathic, 699% (142 203) were acidotic, and 736% (162 220) were thrombocytopenic on admission. On arrival to the ICU, the patients had median platelet counts of 113 109 l (IQR 79 109 l to 152 109 l); INR, 16 (IQR 1419); and BD, -8 mmol l (IQR -11 to -2). Patients received a median of 4 units (IQR 110) of RBCs, 3 units (IQR 06) units of FFP, and 1 unit (IQR 02) of
70 (3978) 67 (5376) 26 (65%) 19 (792%) 16 (40%) 16 (40%) 4 (10%) 0 (0%) 2 (5%) 2 (5%) 5 (208%) 6 (25%) 2 (83%) 1 (42%) 9 (375%) 1 (42%)
2011 The Author(s) Vox Sanguinis 2011 International Society of Blood Transfusion, Vox Sanguinis (2011) 101, 230236
Transfusion practices in massive haemorrhage 233
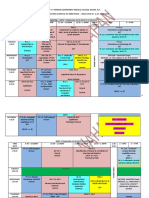
Fig. 1 The box plot indicates the interquartile range, median, and extreme values of international normalized ratio (INR) for baseline results , intensive care unit (ICU) admission results , and 24-h ICU admission results . The P values (KruskalWallis test) were 005 for comparing baseline results between groups and <0001 on ICU admission. The P values (Friedman test) for change in INR over the time points were <0001 for group 1, 030 for group 2, and <0001 for group 3. Table 3 Risk factors associated with mortality in ICU Variables Age, years Type of surgery (major elective surgery vs. emergency setting) ICUBD ICUPLT ICUINR RBC24 PLT24
Fig. 2 The box plot indicates the interquartile range, median, and extreme values of platelet count (109 l) for baseline results , ICU admission results , and 24-h ICU admission results . The P values (KruskalWallis test) were 003 for comparing baseline results between groups and 004 on ICU admission. The P values (Friedman test) for change in platelet count over the time points were for <0001 for group 1, 024 for group 2, and <0001 for group 3.
P
044 013
OR (95% CI) 1008 (09881027) 1909 (08184454)
severity of coagulopathy as indicated by the INR and measured at ICU admission (area under ROC, 069; Fig. 4) and RBCs transfused during the 24-h period were associated with mortality (Table 4).
Discussion
010 082 004 001 017 0929 (08501015) 1001 (09951007) 1827 (10343227) 1076 (10151141) 0800 (05811101)
This study highlights the laboratory and transfusion management of patients with massive haemorrhage. The study cohort comprised all patients receiving MT as a result of AAA, trauma, cardiac, liver transplantation, and abdominal orthopaedic or obstetrics surgery. Seventy percent of
OR, odds ratio; CI, condence interval; ICUBD, base decit on intensive care unit admission; ICUPLT, platelet count on ICU admission; ICUINR, international normalized ratio on ICU admission; RBC24, red blood cells transfused during the 24-h period of massive transfusion; PLT24, platelet units transfused during the 24-h period of massive transfusion.
the other two groups (Fig. 1). At 24-h ICU admission, group 2 remained coagulopathic, thrombocytopenic and, did not correct BD in comparison the other two outcome groups (INR, P = 030; platelet count, P = 026; and BD, P = 024) (Figs. 1, 2, 3). These patients received signicantly more red cells during resuscitation in the ICU than did patients in the other groups. Although patients in all three groups had similar FFP:RBC ratios, those in group 2 had higher ratios of platelets to RBCs (Table 3). Of the 220 patients treated both in the pre-ICU and ICU, 49 (22%) died. Forty of these deaths occurred in the ICU: 12 of the 40 patients had AAA (293%); 14, trauma (341%); 6, abdominal surgery (171%); 5, cardiac surgery (122%); 2, obstetric haemorrhage (49%); and 1, liver transplantation (24%). Multivariate logistic regression analysis found that
Fig. 3 The box plot indicates the interquartile range, median, and extreme values of the base decit (BD) (mmol l) for baseline results , ICU admission results , and 24-hour ICU admission results .The P values (Kruskal Wallis test) were 002 for comparing baseline results between groups and <0001 on ICU admission. The P values (Friedman test) for change in BD over the time points were <0001 for group 1, 026 for group 2, and <0001 for group 3.
2011 The Author(s) Vox Sanguinis 2011 International Society of Blood Transfusion, Vox Sanguinis (2011) 101, 230236
234 R. Sinha & D. Roxby
Fig. 4 Area under the receiving operator characteristic (ROC) curve. ICUINR, international normalized ratio on intensive care unit admission.
the RBC units, 60% of FFP, and 50% of the platelets transfused in rst 24 h of MT were transfused prior to admission to the ICU. Overall, there was a signicant difference in laboratory parameters and transfusion practice between the pre-ICU and ICU settings. Depending on the diagnosis, patients in the pre-ICU setting essentially are in a rapidly evolving acute clinical situation with uncontrolled bleeding. This was established by the presence of coagulopathy and acidosis at the very outset in patients in group 2 (with early deaths). Recent studies [1214] have identied the presence of acute coagulopathy of trauma in one-fourth of the trauma patients on admission. Moreover coagulopathy at the time of admission also predicts poor outcome in patients with ruptured AAA [15]. On admission to the ICU, 69% of the patients were coagulopathic. The patients were monitored with routine
laboratory tests at 2- to 4-h intervals and were resuscitated with FFP, platelets, and cryoprecipitate, with an FFP:RBC ratio of 1:1, which was consistent with recommended ratios published in recent studies [3, 5]. Importantly, the median platelet count on admission to the ICU was greater than 100 109 l, in all groups except group 2 indicating that patients received adequate platelets to maintain haemostasis. Platelet counts on ICU arrival in patients with surgically repaired ruptured AAA have been reported to be independently associated with outcome [16]. Notably, there was a failure to correct coagulopathy and acidosis in patients who died early (group 2) in ICU. In the pre-ICU phase, this group received similar amounts of FFP and platelets and had similar FFP:RBC ratios as compared with other groups. Patients in this group also received lower Platelet:RBC ratios both in the pre-ICU and ICU phase. It is not known if aggressive resuscitation in the preICU phase could have improved survival. In a study of 97 trauma patients, Gonzalez [3] reported that coagulopathy was not corrected during ICU resuscitation, perhaps due to inadequate pre-ICU monitoring. More aggressive pre-ICU intervention to correct coagulopathy may be effective in decreasing the RBC requirement during ICU resuscitation, leading to an improved outcome. Furthermore, group 2 had a subgroup of patients who died during resuscitation in the emergency department or operating theatre. They were mostly trauma and AAA patients and, although they were coagulopathic, 30% of them did not receive any FFP and 45% did not receive any platelets. Understandably, results from this subgroup could lead to bias in comparison with other elective surgery patients with bleeding because some of these patients were in extremis and died before receiving any blood products. In this study, coagulopathy was present in more than one third of the patients at the start of the pre-ICU phase, and nearly half of the patients with coagulopathy were
Table 4 Transfusion of blood products by three MT groups during the pre-ICU phase and ICU phase 24-h period Pre-ICU Group 1 RBC FFP Platelets FFP RBC PLT RBC 11 (817) 4 (26) 1 (02) 1:28 (238) 1:10 (813) Group 2 165 (113275) 6 (1388) 1 (02) 1:33 (2338) 1:12 (920) Group 3 85 (53148) 2 (055) 1 (018) 1:23 (1834) 1:78 (6890) ICU
P value
<0001 009 081 032 0004
Group 1 4 (18) 2 (06) 1 (02) 1:1 (0817) 1:33 (26)
Group 2 9 (1135) 4 (08) 1 (02) 1:13 (0722) 1:8 (312)
Group 3 65 (33143) 4 (2118) 1 (028) 1:14 (124) 1:5 (476)
P value
0007 003 012 024 0008
MT, massive transfusion; ICU, intensive care unit; RBC, red blood cells; FFP, fresh frozen plasma; PLT, platelets. Data are median and interquartile range. KruskalWallis test.
2011 The Author(s) Vox Sanguinis 2011 International Society of Blood Transfusion, Vox Sanguinis (2011) 101, 230236
Transfusion practices in massive haemorrhage 235
trauma patients. Coagulopathy is a signicant problem on ICU admission and a predictor of mortality in the ICU. Our results are comparable to the ndings of Gonzalez et al., where severity of coagulopathy was predictive of mortality. The main difference between Gonzelezs study and our study was the inclusion of all patients receiving MT. This study suggests the need for early recognition and correction of coagulopathy. Although a growing body of literature mostly in the trauma population shows that early use of plasma, platelets and RBCs in a 1:1:1 fashion during MT leads to decreased mortality [3, 5, 7, 17] and several centres have embraced early and higher ratios of FFP and platelets to RBCs in their MT protocols, these are retrospective studies with inherent bias and other confounding factors; it is not clear if the same benet can be extrapolated to non-trauma patients with MT. Goal-directed haemostatic therapy based on thromboelastography is the other option under scrutiny for managing these patients. Interestingly, even in the absence of an MT protocol, the FFP: RBC ratio was in the range of 1:1 in the ICU. However the FFP:RBC ratios in the pre-ICU phase were in the range of 1:21:3 and were similar between the groups. Based on the results of this study, a massive transfusion response (MTR) based on a proactive strategy and aimed at rapid and continuous delivery of blood-component therapy was implemented at our hospital in April 2007. Before MTR was implemented, transfusion triggers were based either on clinical judgment or laboratory results. From April 2007 to December 2009, 45 activations occurred, including 32 that were activated from the operating room, 6 from intensive care, and 7 from the emergency department. Thirty-three patients received MT, nine did not receive MT, and three did not use MTR. The median FFP:RBC ratios in the pre-ICU phase and overall were observed to be 1:18 and 1:19, respectively. Although we are limited by numbers, we are in the process of collecting data after the implementation
of MTR to demonstrate signicant change in transfusion practice and mortality. A signicant limitation in this study was the retrospective design. Through the limitations of the study, discrepancies could be identied in the management of the patients. Fibrinogen levels were not measured whenever coagulation screens were ordered, which may be a reason for the limited use of cryoprecipitate both in pre-ICU and ICU settings. Fibrinogen constitutes an important component of the haemostatic process, including its roles in the formation of platelet aggregates and the generation of a sufciently stable brin network. Often, the role of levels and function of brinogen as a haemostatic agent in the management of perioperative and traumatic haemorrhage are underestimated. There was a lack of analysis of clinical sequelae of potential transfusion-related complications, such as acute respiratory distress syndrome, multiple organ failure, abdominal compartment syndrome, and damage control surgery. Lastly, the three groups were not well matched. The authors are well aware of generating bias when comparing emergency surgery and elective surgery with bleeding. In conclusion, this study shows a representation of transfusion practices in patients with massive bleeding. Patients who died early were coagulopathic before and on ICU admission and did not correct their coagulopathy. This study also shows that coagulopathy is associated with an increased risk of mortality. Early and aggressive correction of coagulopathy for patients presenting with coagulopathy may be effective in improving mortality.
Acknowledgements
The authors gratefully acknowledge Zlatko Unterweger from ICT Services, SA Health for data provision; Dr. Ram Seshadri and Dr. Andrew Bersten for their input and guidance.
8 Johansson P, Stensballe J: Effect of haemostatic control resuscitation on mortality in massively bleeding patients: a before and after study. Vox Sang 2009; 96:111118 9 Cotton BA, Au BK, Nunez TC, et al.: Predened massive transfusion protocols are associated with a reduction in organ failure and postinjury complications. J Trauma 2009; 66:4148; discussion 4849 10 Gunter OLJ, Au BK, Isbell JM, et al.: Optimizing outcomes in damage control resuscitation: identifying blood product ratios associated with improved survival. J Trauma 2008; 65:527534 11 Daniel JR, Thomas CT, Loren R, et al.: Massive transfusion protocols: the role
References
1 Geeraedts JLMG, Demiral H, Schaap NP, et al.: Blind transfusion of blood products in exsanguinating trauma patients. Resuscitation 2007; 73:382 388 2 Johansson P, Hansen M, Sorensen H: Transfusion practice in massively bleeding patients: time for a change? Vox Sang 2005; 89:9296 3 Gonzalez E, Moore F, Holcomb J, et al.: Fresh frozen plasma should be given earlier to patients requiring massive transfusion. J Trauma 2007; 62:112119 4 Holcomb J, Jenkins D, Rhee P, et al.: Damage control resuscitation: directly
addressing the early coagulopathy of trauma. J Trauma 2007; 62:307310 5 Borgman M, Spinella P, Perkins J, et al.: The ratio of blood products transfused affects mortality in patients receiving massive transfusions at a combat support hospital. J Trauma 2007; 63:805813 6 Hoyt DB, Dutton RP, Hauser CJ, et al.: Management of coagulopathy in the patients with multiple injuries: results from an international survey of clinical practice. J Trauma 2008; 65:755765 7 Duchesne JC, Hunt JP, Wahl G, et al.: Review of current blood transfusions strategies in a mature level I trauma center: were we wrong for the last 60 years? J Trauma 2008; 65:272278
2011 The Author(s) Vox Sanguinis 2011 International Society of Blood Transfusion, Vox Sanguinis (2011) 101, 230236
236 R. Sinha & D. Roxby
of aggressive resuscitation versus product ratio in mortality reduction. J Am College Surg 2009; 209:198205 12 Brohi K, Singh J, Heron M, et al.: Acute traumatic coagulopathy. J Trauma 2003; 54:11271130 13 Niles SE, McLaughlin DF, Perkins JG, et al.: Increased mortality associated with the early coagulopathy of trauma in combat casualties. J Trauma 2008; 64: 14591465
14 MacLeod J, Lynn M, McKenney M, et al.: Early coagulopathy predicts mortality in trauma. J Trauma 2003; 55:39 44 15 Davies MJ, Murphy WG, Murie JA, et al.: Preoperative coagulopathy in ruptured abdominal aortic aneurysm predicts poor outcome. Br J Surg 1993; 80:974976 16 Johansson P, Stensballe J, Rosenberg I, et al.: Proactive administration of plate-
lets and plasma for patients with a ruptured abdominal aortic aneurysm: evaluating a change in transfusion practice. Transfusion 2007; 47:593598 17 Sperry JL, Ochoa JB, Gunn SR, et al.: An Ffp:Prbc transfusion ratio >=1:1.5 is associated with a lower risk of mortality after massive transfusion. J Trauma, 2008; 65:986993
2011 The Author(s) Vox Sanguinis 2011 International Society of Blood Transfusion, Vox Sanguinis (2011) 101, 230236
Copyright of Vox Sanguinis is the property of Wiley-Blackwell and its content may not be copied or emailed to multiple sites or posted to a listserv without the copyright holder's express written permission. However, users may print, download, or email articles for individual use.
S-ar putea să vă placă și
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Composition of Blood PlasmaDocument27 paginiComposition of Blood PlasmaSUNIL KUMAR100% (1)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- 209-Hematology Review - Case StudiesDocument129 pagini209-Hematology Review - Case StudiesKhalid Khalidi100% (2)
- Morphology OF Red Blood CellsDocument36 paginiMorphology OF Red Blood CellsFrancis ValdezÎncă nu există evaluări
- PMLS 2 LEC Module 3Document8 paginiPMLS 2 LEC Module 3Peach DaquiriÎncă nu există evaluări
- Chapter 30 Nursing Assessment Hematologic SystemDocument14 paginiChapter 30 Nursing Assessment Hematologic Systemmedic-24100% (1)
- 2.histologi DarahDocument38 pagini2.histologi DarahIrfanÎncă nu există evaluări
- Presentation On Blood DisordersDocument122 paginiPresentation On Blood Disordersvarshasharma05Încă nu există evaluări
- ''Sangrado Perioperatorio Severo GuiaDocument113 pagini''Sangrado Perioperatorio Severo GuiaHECTOR ESTRADAÎncă nu există evaluări
- A Guide To Diagnoses, Indications, and Contraindications For Interventions in Pediatric Chronic PainDocument11 paginiA Guide To Diagnoses, Indications, and Contraindications For Interventions in Pediatric Chronic PainJose Miguel Arce RomoÎncă nu există evaluări
- Airway and Ventilator Management in Trauma Patients PDFDocument6 paginiAirway and Ventilator Management in Trauma Patients PDFJose Miguel Arce RomoÎncă nu există evaluări
- A Comparison Between Volume-Controlled Ventilation and Pressure-Controlled Ventilation in Providing Better Oxygenation in Obese Patients Undergoing Laparoscopic CholecystectomyDocument7 paginiA Comparison Between Volume-Controlled Ventilation and Pressure-Controlled Ventilation in Providing Better Oxygenation in Obese Patients Undergoing Laparoscopic CholecystectomyJose Miguel Arce RomoÎncă nu există evaluări
- A Comparison of Intrathecal Dexmedetomidine, Clonidine, and Fentanyl As Adjuvants To Hyperbaric Bupivacaine For Lower Limb Surgery A Double Blind Controlled StudyDocument7 paginiA Comparison of Intrathecal Dexmedetomidine, Clonidine, and Fentanyl As Adjuvants To Hyperbaric Bupivacaine For Lower Limb Surgery A Double Blind Controlled StudyJose Miguel Arce RomoÎncă nu există evaluări
- A Comprehensive Review of Opioid-Induced HyperalgesiaDocument18 paginiA Comprehensive Review of Opioid-Induced HyperalgesiaJose Miguel Arce RomoÎncă nu există evaluări
- A Comparison Between Volume-Controlled Ventilation and Pressure-Controlled Ventilation in Providing Better Oxygenation in Obese Patients Undergoing Laparoscopic CholecystectomyDocument7 paginiA Comparison Between Volume-Controlled Ventilation and Pressure-Controlled Ventilation in Providing Better Oxygenation in Obese Patients Undergoing Laparoscopic CholecystectomyJose Miguel Arce RomoÎncă nu există evaluări
- A Comparative Study of Endotracheal Tube Positioning Methods in ChildrenDocument6 paginiA Comparative Study of Endotracheal Tube Positioning Methods in ChildrenJose Miguel Arce RomoÎncă nu există evaluări
- Pharmacological Treatment of Opioid-Induced Hyperalgesia A Review of The EvidenceDocument13 paginiPharmacological Treatment of Opioid-Induced Hyperalgesia A Review of The EvidenceJose Miguel Arce RomoÎncă nu există evaluări
- Molecular Insights Into μ Opioid Pharmacology From the Clinic to the BenchDocument7 paginiMolecular Insights Into μ Opioid Pharmacology From the Clinic to the BenchJose Miguel Arce RomoÎncă nu există evaluări
- Who Benefits From Red Blood Cell Salvage - Utility and Value of Intraoperative Autologous Transfusion.Document4 paginiWho Benefits From Red Blood Cell Salvage - Utility and Value of Intraoperative Autologous Transfusion.Jose Miguel Arce RomoÎncă nu există evaluări
- Alteration in OxygenationDocument8 paginiAlteration in Oxygenationraquel maniegoÎncă nu există evaluări
- Timetable DYSPGMC Nahan PDFDocument56 paginiTimetable DYSPGMC Nahan PDFkushalÎncă nu există evaluări
- Chapter 7 RH TypingDocument22 paginiChapter 7 RH TypingYo Issei Hyodono100% (1)
- Massive Transfusion in Trauma Guildelines PDFDocument18 paginiMassive Transfusion in Trauma Guildelines PDFChey Ochy Aprilia100% (2)
- Multiple Choice Questions: A. B. C. DDocument55 paginiMultiple Choice Questions: A. B. C. DwanderagroÎncă nu există evaluări
- Diagon Blood Controls PRESENTACION 2017Document47 paginiDiagon Blood Controls PRESENTACION 2017Leidy Tatiana RiveraÎncă nu există evaluări
- PRP Therapy Kit MainDocument1 paginăPRP Therapy Kit Maindrsuryakant9818Încă nu există evaluări
- RBSE Class 8 Science Notes Chapter 7 Blood Circulation - RBSE GuideDocument3 paginiRBSE Class 8 Science Notes Chapter 7 Blood Circulation - RBSE GuideAlpine AcademiaÎncă nu există evaluări
- BT Case Scenario 1 (Group 1)Document3 paginiBT Case Scenario 1 (Group 1)Rej GarbosaÎncă nu există evaluări
- Physiology Slide #1Document18 paginiPhysiology Slide #1anon_974423120Încă nu există evaluări
- Q and A in Antibody IdentificationDocument29 paginiQ and A in Antibody IdentificationMohamed ElmasryÎncă nu există evaluări
- Lesson 08Document9 paginiLesson 08asyafujisaki100% (2)
- Diagnosing Anemia Algorithm HandoutDocument2 paginiDiagnosing Anemia Algorithm HandoutValentino Farroñay TafurÎncă nu există evaluări
- Assays by Instruments IH-Com Version 4Document5 paginiAssays by Instruments IH-Com Version 4AceÎncă nu există evaluări
- Plasma ExpandersDocument21 paginiPlasma ExpandersvimalaÎncă nu există evaluări
- The Circulatory System:: BloodDocument101 paginiThe Circulatory System:: BloodAntonio MihaiÎncă nu există evaluări
- Exam 19 BloodDocument8 paginiExam 19 BloodPurwa RaneÎncă nu există evaluări
- Pediatric Hematology Oncology JournalDocument4 paginiPediatric Hematology Oncology JournalmitraÎncă nu există evaluări
- Blood and Its Components-NotesDocument10 paginiBlood and Its Components-NotesKelvin RequenaÎncă nu există evaluări
- Biology Module 2Document20 paginiBiology Module 2RieleoncioÎncă nu există evaluări
- Module 2 Blood and Bloostain Analysis Forensic 3Document29 paginiModule 2 Blood and Bloostain Analysis Forensic 3nikke requeÎncă nu există evaluări
- Week 12 - Muscles WorksheetDocument5 paginiWeek 12 - Muscles Worksheetxcupcakex122006Încă nu există evaluări
- PERIDA EMMALYN T. - BSci103-Lesson 4.2-Learning TaskDocument5 paginiPERIDA EMMALYN T. - BSci103-Lesson 4.2-Learning TaskEmmalyn PeridaÎncă nu există evaluări