Documente Academic
Documente Profesional
Documente Cultură
Patient Profile Data Form: Advance Directives
Încărcat de
Ma Cecilia SorianoDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Patient Profile Data Form: Advance Directives
Încărcat de
Ma Cecilia SorianoDrepturi de autor:
Formate disponibile
PATIENT PROFILE DATA FORM
Student Name: Patient Identifier: Gender: Male Female Advance Directives Living Will: yes no Date of Care: Age: Admission Date: Do Not Resuscitate Order (DNR) yes no
Medical Durable Power of Attorney: yes no (If yes, relationship?) Reason for Hospitalization: Significant Medical Diagnoses: Relevant Surgical Procedure(s) and Date(s): Pathophysiology/Description of present illness/medical diagnoses or surgical procedures (Continue on back of this page, no less than 3-5 sentences per diagnosis/procedure, include how the present illness/condition relates to or is impacted by co-morbidities or previous illness, symptoms to watch for and any current treatments pertinent to the patient)
Laboratory Data Students MAY NOT use the term WNL or chart by exception on this form. Write normal value range, exact value for patient, and indicate if this is normal, high, or low. Sodium Positive Cultures Potassium Chloride Serum CO2 Glucose Insulin Therapy? Blood Urea Nitrogen Creatinine Calcium Magnesium Phosphorous Total Protein Albumin Pre-Albumin White Blood Cells Red Blood Cells Hemoglobin Hematocrit Platelets INR Coumadin Therapy? PTT Heparin Drip? Total Bilirubin AST ALT Alkaline Phosphatase
OTHER: (HGB A1c, amylase, lipase, ammonia, CPK, troponin, BNP, lactate, ABG pH, pO2, pCO2, HCO3)
What information can you obtain from these lab values? Why is this information important for this specific patient?
Diagnostic Tests Date completed and findings Chest X-Ray: EKG/Telemetry: Other:
CT/MRI:
**Write exactly what you see/hear/etc. and indicate if this is normal, abnormal, hyper, or hypo; if abnormal then state pathophysiology resulting in abnormal assessments students MAY NOT use the term WNL or chart by exception on this form. Physical Assessment Data T-P-R: Height: Pain rating on 0-10 scale: BP: Weight: Pain Assessment Details (OLD CART):
Last pain medication given (What was given and when):
Treatments (Eg: PT, OT, RT, etc) Treatment: Support Services: Other:
Treatment: Consultations:
Diet/fluids Type of diet: Fluid intake: Needs assistance with feeding Other:
Restrictions: Tube feedings (type and rate): Nausea or vomiting:
Appetite: Problems swallowing, chewing, dentures: Over-hydrated or dehydrated (how assessed):
Intravenous Fluids Type and rate: Condition of site and dressing:
Site(s) Other:
Elimination Last bowel movement (LBM): Circle problems that apply:
24 hour urine output: Bowel Constipation Diarrhea Flatus Hesitancy Incontinence
Catheter yes no Type: Urinary Pain/Burning Frequency Odor
Neurological/Mental Status LOC & Orientation: Speech: Memory (recent, remote):
Motor (ROM, gait, balance): Pupils (PERRLA): Sleep habits (meds, etc.)
Sensory Deficits (hearing, vision, taste, smell, sensation):
Musculoskeletal System Ability to walk/Gait: Transfers: ROM/Muscle Strength (weakness, paralysis): Bones, Joints, Muscles (fractures, contractures, arthritis, spinal curvatures, etc.) : Fall risk assessment (score and classification of risk):
Type of activity orders: Mobility aides: Restraints yes no Cast/Splint/Collar/Brace:
Side rails (number):
Cardiovascular system Extremity Circulation Checks (pulses, temperature, sensation, color): Neck Vein Distention: Sounds(S1, S2, regular/irregular): Respiratory System Airway (type, size): Cyanosis yes no Location: Breath Sounds (clear, crackles, wheezes, rhonchi, location): O2 humidification: Yes No Chest tube or other: Chest Pain:
Capillary Refill: Edema (degree, pitting, location): TED Hose, Compression Devices: Yes No Type: Use of accessory muscles: Cough (productive, nonproductive): Flow rate of O2: Smoking History Yes No
Depth, rate, rhythm: Sputum (color, amount): Use of O2 (nasal cannula, mask, trach collar): Pulse Oximetry: ____ % oxygen saturation
Gastrointestinal System Abdomen (pain, tenderness, guarding, distention, soft, firm): NG tube (describe drainage): Other: Skin and Wounds Color & Condition: (intact, rash, bruising, turgor) Edges approximated? Yes No Dressings (clean, dry, intact):
Bowel sounds:
Ostomy (describe stoma site & drainage):
Describe wound(s) location, size: Characteristics of drainage: Braden Risk Assessment (score and classification of risk):
Drains (type & location): Wound Closures (sutures, staples, steri-strips, other):
Other:
Head, Eyes, Ears, Nose, Throat (HEENT) Oral Mucous Membranes/Tongue (color, moisture, lesions): Eyes (redness, drainage, edema, ptosis): Nose (redness, drainage, edema): Reproductive System Female: LMP: # Pregnancies/# Live births: Vaginal discharge/bleeding: History of STIs: Last Mammogram: Last Pap Smear: Psychosocial and Cultural Assessment Religious preference: Primary Language: Emotional state:
Teeth (dentures, dental caries, edentulous): Ears (drainage, tinnitus): Throat (pain, redness, gag reflex):
Male: Any prostate problems: ED problems: Penile discharge/bleeding: Last Prostate Exam: History of STIs: Other:
Marital status: Occupation: Family interaction:
Patient/Family Education Education Materials Provided (Any available/utilized that apply to diagnosis):
S-ar putea să vă placă și
- ASSESSMENT FORM: Spring 2006 Client's Number: InstructionsDocument6 paginiASSESSMENT FORM: Spring 2006 Client's Number: Instructionsdenisemw88Încă nu există evaluări
- Wallace State Community College NURSING DATABASE: Nursing HomeDocument9 paginiWallace State Community College NURSING DATABASE: Nursing HomeEnger NushunÎncă nu există evaluări
- Care Plan Oct 23 380Document18 paginiCare Plan Oct 23 380api-256360167Încă nu există evaluări
- Nursing Assesment NewDocument14 paginiNursing Assesment NewsuhandinataÎncă nu există evaluări
- Internal MedicineDocument18 paginiInternal MedicineNashaat H. AlshawabkehÎncă nu există evaluări
- Introduction History and ExaminationDocument43 paginiIntroduction History and ExaminationDanyal Hassan100% (1)
- Gynecology and ObstetricsDocument125 paginiGynecology and Obstetricsapi-3712326100% (4)
- Hanh Nguyen1Document10 paginiHanh Nguyen1api-292717295Încă nu există evaluări
- (Current Clinica (Current - Clinical - Strategies) - Gynecology - and - Obstetrics - 2004l Strategies) - Gynecology and Obstetrics 2004Document125 pagini(Current Clinica (Current - Clinical - Strategies) - Gynecology - and - Obstetrics - 2004l Strategies) - Gynecology and Obstetrics 2004Eliza Stochita100% (1)
- Soap RoutineDocument3 paginiSoap RoutineRoberto Ramos100% (1)
- Chief Complaint: Samples of SOAP NotesDocument3 paginiChief Complaint: Samples of SOAP NotesWhit CarriganÎncă nu există evaluări
- 58 Cases History and Physical Exam BookDocument102 pagini58 Cases History and Physical Exam BookeleazarmdÎncă nu există evaluări
- Nursing Case Analysis FeliDocument20 paginiNursing Case Analysis FeliIanusGwapitusÎncă nu există evaluări
- Bedside Med HX Maker PDFDocument2 paginiBedside Med HX Maker PDFjustinryanÎncă nu există evaluări
- Health Assessment and Physical AssessmentDocument182 paginiHealth Assessment and Physical AssessmentAnonymous XunfAgd2BÎncă nu există evaluări
- Physical Assessment FormatDocument24 paginiPhysical Assessment FormatSruthi Krishna100% (1)
- Neuroscience Physical Therapy Evaluation FormDocument7 paginiNeuroscience Physical Therapy Evaluation FormTaral PatelÎncă nu există evaluări
- Gynecology and ObstetricsDocument190 paginiGynecology and Obstetricsbhesh_seanÎncă nu există evaluări
- Gynzmedicalzhistoryzquestionnaire PDFDocument2 paginiGynzmedicalzhistoryzquestionnaire PDFapi-267430063Încă nu există evaluări
- Obstetrics and Gynecology New Treatment Guidelines - 2008Document56 paginiObstetrics and Gynecology New Treatment Guidelines - 2008aminskiÎncă nu există evaluări
- New Patient History FormDocument6 paginiNew Patient History Formعبدالله الكافÎncă nu există evaluări
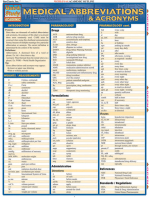
- Common Medical AbbreviationsDocument3 paginiCommon Medical AbbreviationsSwaleh YusufÎncă nu există evaluări
- Charting GuidelinesDocument4 paginiCharting Guidelinesgrad_nurse_2015Încă nu există evaluări
- Post OpDocument6 paginiPost OpFrinkaWijayaÎncă nu există evaluări
- Gynecology and ObstetricsvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvDocument133 paginiGynecology and ObstetricsvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvȚurcan IurieÎncă nu există evaluări
- 4 Examining Gastrointestinal SystemDocument75 pagini4 Examining Gastrointestinal SystemSafi MohammedÎncă nu există evaluări
- History and ExamDocument27 paginiHistory and ExamEmereole FrancesÎncă nu există evaluări
- History Taking and ExaminationDocument48 paginiHistory Taking and ExaminationNaomi Tolulope OlasehindeÎncă nu există evaluări
- Abdomen - Case Sheet - FinalDocument8 paginiAbdomen - Case Sheet - FinalHengkai NeoÎncă nu există evaluări
- Azusa Pacific University School of Nursing GNRS 588: Advanced Nursing Care For Adults Comprehensive Care Plan #: - 1Document18 paginiAzusa Pacific University School of Nursing GNRS 588: Advanced Nursing Care For Adults Comprehensive Care Plan #: - 1api-325691098Încă nu există evaluări
- Clinical Organization Sheet NursingDocument1 paginăClinical Organization Sheet NursingSarah S100% (1)
- Health Assessment FormDocument8 paginiHealth Assessment FormIrina Chpitalnik100% (1)
- Guide To The Comprehensive, Adult Write-UpDocument6 paginiGuide To The Comprehensive, Adult Write-UpKeaira Kc100% (1)
- Case Presenation Format: Bims College of Nursing Department: MSNDocument20 paginiCase Presenation Format: Bims College of Nursing Department: MSNJaanu JaanuÎncă nu există evaluări
- Gynecology and ObstetricsDocument125 paginiGynecology and ObstetricsIrma Sari MuliadiÎncă nu există evaluări
- HistoryandPhysicalExamDocument105 paginiHistoryandPhysicalExamsilentscream0618Încă nu există evaluări
- Medicine HandbookDocument43 paginiMedicine Handbookramavisalam100% (2)
- Abdominal Pain: Essential Diagnosis and Management in Acute MedicineDe la EverandAbdominal Pain: Essential Diagnosis and Management in Acute MedicineÎncă nu există evaluări
- Physician Assistant PANCE & PANRE: a QuickStudy Laminated Reference GuideDe la EverandPhysician Assistant PANCE & PANRE: a QuickStudy Laminated Reference GuideÎncă nu există evaluări
- Complementary and Alternative Medical Lab Testing Part 11: MenDe la EverandComplementary and Alternative Medical Lab Testing Part 11: MenÎncă nu există evaluări
- Top Trials in Gastroenterology & Hepatology, 2nd EditionDe la EverandTop Trials in Gastroenterology & Hepatology, 2nd EditionÎncă nu există evaluări
- One Step Med: General Medical Information Record Keeping ManualDe la EverandOne Step Med: General Medical Information Record Keeping ManualÎncă nu există evaluări
- Fast Facts for Patients and Supporters: Cholangiocarcinoma: A cancer of the bile duct and liver Information + Taking Control = Best OutcomeDe la EverandFast Facts for Patients and Supporters: Cholangiocarcinoma: A cancer of the bile duct and liver Information + Taking Control = Best OutcomeÎncă nu există evaluări
- Complementary and Alternative Medical Lab Testing Part 4: VascularDe la EverandComplementary and Alternative Medical Lab Testing Part 4: VascularÎncă nu există evaluări
- A Practical Guide to Common Presenting Complaints in Primary CareDe la EverandA Practical Guide to Common Presenting Complaints in Primary CareÎncă nu există evaluări
- Portal Vein Thrombosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDe la EverandPortal Vein Thrombosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsÎncă nu există evaluări
- Case Taking Proforma: Medicine, Paediatrics & ObgDe la EverandCase Taking Proforma: Medicine, Paediatrics & ObgÎncă nu există evaluări
- Physical Examination in Cardiovascular Chinese MedicineDe la EverandPhysical Examination in Cardiovascular Chinese MedicineÎncă nu există evaluări
- Complementary and Alternative Medical Lab Testing Part 8: UrologyDe la EverandComplementary and Alternative Medical Lab Testing Part 8: UrologyEvaluare: 3 din 5 stele3/5 (1)
- Practical Gastroenterology and Hepatology Board Review ToolkitDe la EverandPractical Gastroenterology and Hepatology Board Review ToolkitKenneth R. DeVaultÎncă nu există evaluări
- Checklists for Clinical Examinations in General SurgeryDe la EverandChecklists for Clinical Examinations in General SurgeryÎncă nu există evaluări
- The Ultimate Guide to Physician Associate OSCEs: Written by a Physician Associate for Physician AssociatesDe la EverandThe Ultimate Guide to Physician Associate OSCEs: Written by a Physician Associate for Physician AssociatesÎncă nu există evaluări
- Sarcoma SpecialistDocument5 paginiSarcoma SpecialistaminudinrahmanÎncă nu există evaluări
- Humoral Imune Respon: SuhermanDocument62 paginiHumoral Imune Respon: SuhermansuhermanÎncă nu există evaluări
- Auerbach's Wilderness Medicine PDFDocument1.672 paginiAuerbach's Wilderness Medicine PDFKieran D90% (10)
- ENT FinalDocument141 paginiENT FinalSujeet PatilÎncă nu există evaluări
- S94 - Harish Kumar Rao Manav Chowk Cc-Sahyogi Juneja Towers, 716, Rattangarh Road, Manav Chowk, Ambala CITY, PH-9996006678Document3 paginiS94 - Harish Kumar Rao Manav Chowk Cc-Sahyogi Juneja Towers, 716, Rattangarh Road, Manav Chowk, Ambala CITY, PH-9996006678EduÎncă nu există evaluări
- Role of MDCT in Coronary Artery Disease: Swachchhanda Songmen 2071Document63 paginiRole of MDCT in Coronary Artery Disease: Swachchhanda Songmen 2071Dr KhanÎncă nu există evaluări
- Catheter Ablation For AFDocument12 paginiCatheter Ablation For AFPeny Ruth Jessica DamanikÎncă nu există evaluări
- Notes in Human Anatomy and PhysiologyDocument9 paginiNotes in Human Anatomy and PhysiologyRikki Mae Bueno100% (3)
- Dialysis Center in BPDHDocument29 paginiDialysis Center in BPDHXien Cadiz100% (5)
- Orthodontic Pearls PDFDocument2 paginiOrthodontic Pearls PDFortho123Încă nu există evaluări
- Katzung QuestionsDocument29 paginiKatzung QuestionsToastie3100% (12)
- Asthma2 Case StudyDocument8 paginiAsthma2 Case StudyGlenn Asuncion PagaduanÎncă nu există evaluări
- ECF Onwards ReviewerDocument4 paginiECF Onwards ReviewerJury Andrew SeseÎncă nu există evaluări
- Cincinnati Physicians COVID Universal Mask Letter To Schools FinalDocument17 paginiCincinnati Physicians COVID Universal Mask Letter To Schools FinalWCPO 9 NewsÎncă nu există evaluări
- Positive and Negative Syndrome Scale (Panss)Document2 paginiPositive and Negative Syndrome Scale (Panss)Cruizer Davis100% (1)
- Muscular DystrophyDocument64 paginiMuscular DystrophysridharÎncă nu există evaluări
- Animal Caries ModelsDocument11 paginiAnimal Caries ModelscharitoupchÎncă nu există evaluări
- Essentials in Piezosurger Clinical Advantages in Dentistry VercellottiDocument136 paginiEssentials in Piezosurger Clinical Advantages in Dentistry VercellottiayudewintasariÎncă nu există evaluări
- Total Relaxation: The Complete Program For Overcoming Stress, Tension, Worry, and FatigueDocument0 paginiTotal Relaxation: The Complete Program For Overcoming Stress, Tension, Worry, and FatigueadtadÎncă nu există evaluări
- Revised Rate List of Hospital Charges, AIIMS, New Delhi, India PDFDocument30 paginiRevised Rate List of Hospital Charges, AIIMS, New Delhi, India PDFInder67% (3)
- Test Bank For Equipment Theory For Respiratory Care 5th Edition by WhiteDocument11 paginiTest Bank For Equipment Theory For Respiratory Care 5th Edition by Whiteharoldbrownorcnxeijgd100% (29)
- Assisting Arterial Blood Gas: Lesson PlanDocument2 paginiAssisting Arterial Blood Gas: Lesson PlanSwapnil MahapureÎncă nu există evaluări
- Gordon's Functional Health PatternDocument8 paginiGordon's Functional Health PatternDanica NuevaexcijaÎncă nu există evaluări
- Step by Step Root Canal TreatmentDocument157 paginiStep by Step Root Canal TreatmentKaaroma Tamoaieta100% (1)
- Activity On Lesson 2 Common Injuries in DanceDocument10 paginiActivity On Lesson 2 Common Injuries in DancePammy AlivenÎncă nu există evaluări
- Module 7 Anxiety Disorders PDFDocument12 paginiModule 7 Anxiety Disorders PDFprashansha kumudÎncă nu există evaluări
- Pharmacology McqNEW 2Document7 paginiPharmacology McqNEW 2Ayman Ragab100% (2)
- Care Plan TemplateDocument8 paginiCare Plan TemplateXosweetbebeÎncă nu există evaluări
- Right-Sided Heart Failure: College of NursingDocument30 paginiRight-Sided Heart Failure: College of NursingMatelyn OargaÎncă nu există evaluări
- FreeStyle Libre ManualDocument124 paginiFreeStyle Libre ManualPonz GibraltarÎncă nu există evaluări