Documente Academic
Documente Profesional
Documente Cultură
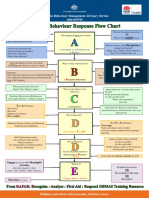
Dementia Care. Part 2 Understanding and Managing Behavioural Challenges
Încărcat de
dogstar23Descriere originală:
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Dementia Care. Part 2 Understanding and Managing Behavioural Challenges
Încărcat de
dogstar23Drepturi de autor:
Formate disponibile
Dementia care.
Part 2: understanding
and managing beiiaviourai chaiienges
Emma Ouldred, Catherine Bryant
including the course and prognosis of the condition, available
treatments, and support available from both voluntary and
Abstract statutory organizations. The provision of written information is
Management of dementia should focus on the maintenance of
recommended and the Alzheimer's Society provides a variety of
function and independence for the person with the disease. Non-
information sheets about all aspects of dementia and dementia
pharmacological interventions to manage dementia include
care (www.alzheimers.org.uk).
reality orientation, aromatherapy and validation therapy. Non-
pharmacological ways of managing challenging behaviour are
recommended in current guidance. Drug treatments, which may Coordination of care and care pianning
stahiUze the symptoms of Alzheimer's disease or slow down further Care for the person with dementia needs to be coordinated
progression for a time, have heen availahle in the United Kingdom across both health and social care agencies, and may involve
since 1997 and may help some people with dementia. There are high different specialists within the multidisciplinary team at
levels of stress, distress and psychological illness in family caregivers of certain time-points. Ideally care should be coordinated by
individuals with dementia, and practitioners are well placed to signpost a case manager. Care plans should address activities of daily
carers to appropriate support organizations. living (ADLs), which maximize independent activity, enhance
function, adapt and develop skills, and minimize the need for
Key words: Girers • Challenging behaviour • Dementia support (NICE, 2006). Care plans should consider:
Consistent and stable staffing
Retaining a familiar environment
P
art 1 of this series on dementia care provided an
outline of recent dementia care guidance and the Minimizing relocations
Mental Capacity Act 2005, in addition to giving Flexibihty to accommodate fluctuating abilities
practitioners a brief overview of the different forms Assessment and care planning advice regarding ADLs and
of dementia, the assessment process, and how to differentiate ADL skill training from an occupational therapist
between dementia, delirium and depression. Assessment and care planning advice about independent
This article explores the management of dementia (focusing toileting skills. If incontinence occurs all possible causes
on challenging behaviour), which includes use of psychosocial should be assessed and relevant treatments tried before
interventions and available drug treatments. Coping strategies concluding that it is permanent
and tips on effective communication are provided. It also Environmental modifications to aid independent functioning,
highlights the need for all practitioners to be aware of the including assistive technology, with advice from an
contribution informal carers make in caring for people with occupational therapist and/or clinical psychologist
dementia and also to be cognisant of what support is available Physical exercise, with assessment and advice from a
for carers to ensure timely referral to such services. physiotherapist when needed
Support for people to go at their own pace and participate
Person-centred care in activities they enjoy
One of the aims of management is to promote independence The needs of carers.
for the individual and maintenance of fiinction for as long as
Emma Ouldred
is Dementia
possible underpinned by the philosophy of person-centred Cognitive stimuiation
Nurse Specialist
care (National Institute for Health and Clinical Excellence Current guidelines recommend that all people with mild to
and Catherine [NICE], 2006), whereby the person with demetia is seen as an moderate dementia are offered cognitive stimulation, and the
Bryant is individual, rather than focusing on their illness and on abilities effects may add to the effects of drug treatment (NICE, 2006).
Consultant they may have lost. Instead of treating the person as a collection Cognitive stimulation can be defined as engagement in a range
Physician, King's of symptoms and behaviours to be controlled, person-centred of activities and discussions aimed at general enhancement of
College Hospital care takes into account each individual's unique qualities, cognitive and social flinctioning (Clare and Woods, 2004). It
NHS Trust, abilities, interests, preferences and needs (Kitwood, 1997) may occur informally through recreational activities, formally
London through group programmes that are designed to stimulate or
Accepted for Information engage people with dementia, or through training exercises
publication: Following a diagnosis of dementia both the patient and their designed to address specific cognitive fianctions. Cognitive
January 2008 carer are likely to need information and ongoing support rehabilitation programmes are usually individually tailored and
about the condition and the implications for the future. target specific goals (Clare and Woods, 2004).
242 British Journal of Nursing, 2008,Vol 17, No 4
NEUROSCIENCE NURSING
Pharmacological interventions Figure 1. The action of cholinesterase inhibitors on acetytcholine (a); and memantine effect on glutamine (b).
Drug treatments for Alzheimer's disease
There is currently no known cure for Alzheimer's, but Cholinergic Acetylcholine
Giutamate
nerve ending reduced to recognition site NMDA receptor in
there are drug treatments available (cholinesterase inhibitors inactive form by CNS neuron
choiinesterase Giutamate
[ChEIs]), which may stabilize or slow down the progression Acetylcholine
of the disease. They work by helping to stop the depletion Extracellular
of the chemical neurotransmitter, acetylcholine (deficiency
of acetylcholine occurs in Alzheimer's and is related to both Choiinesterase
Cytoplasm
cognitive and non-cognitive symptoms) (Figure 1) (Francis Postsynaptic neuron
et al, 1999). ChEIs may help cognitive symptoms, such as
memory loss, and patients and carers might report a positive
effect on activities of daily living, behaviour and mood. They Choiiinesterase
Biocked by
are effective in the mild to moderate stages of disease. There hibitor memantine
are three drugs currently available in the United Kingdom
(UK): Aricept®, Exelon® and Reminyl®. Common side-
effects include anorexia, diarrhoea and stomach cramps. Rare Choiinesterase
side-effects include nightmares and increased confusion. Not (b)
all individuals with Alzheimer's wOl respond to treatment - a
third will show improvement, a third will not deteriorate and • Smoking cessation: people with dementia should be
a third will have no response and continue to deteriorate encouraged to give up smoking. Appropriate guidance
(Overshott and Burns, 2005). ChEIs should only be prescribed regarding smoking cessation clinics and methods to give up
and monitored by specialists and the drug stopped if it is felt smoking should be given
not to be of benefit to the patient. • Physical exercise: people with dementia should be advised to
Memantine is licensed in the UK for moderate to severe exercise regularly, such as 30 minutes per day. This does not
dementia. Memantine blocks a neurotransmitter, glutamate, have to be intensive gym activity but could simply mean a
which is released in excessive amounts when brain cells are walk in a local park
damaged by Alzheimer's {Figure i) (Danysz et al, 2000). • Diet: advise to eat a varied low salt, low fat diet should be
NICE (2006) has recently issued guidance regarding the given. Referral to a dietician may be required.
availability of ChEIs on NHS prescriptions. It recommends
that these drugs should only be prescribed to people with Treatment for dementia with lewy bodies (DLB)
moderate Alzheimer's. NICE does not recommend the use of There is some evidence that rivastigmine may help both
memantine except as part of well-designed clinical trials. cognitive and non-cognitive symptoms in DLB (NICE, 2006).
Modification of vascular risk factors is also important in this
Treatment for vascular dementia (VaD) patient group.
Currently ChEIs are not licensed for the treatment of VaD
in the UK. However, if the clinical picture suggests a mixed Ciiallenging behaviour
form of dementia then they may be considered. Modification Challenging behaviour can be defined as any behaviour that is
of vascular vascular risk is widely recommended for the unpredictable, frequent and of long duration, and is distressing
management of vascular disease although long-term studies to the individual or a nuisance to others (Table 1) (Tarbuck and
directly addressing effect on cognition are lacking (NICE, Thompson, 1995). Adverse behavioural symptoms associated
2006). The main aim of treatment for people with VaD with the dementia need to be assessed thoroughly and a care
is to reduce their risk of further stroke damage through plan developed with the involvement ofthe individual and their
modification of cardiovascular risk factors as stated below. carer. Alleviation of carer burden should also be considered.
However, it is important to remember that modification of Neuropsychiatric and behavioural problems in older people
vascular risk also needs to be addressed in all people with can occur in a number of different conditions, including
dementia regardless ofthe dementia sub-type. dementia, delirium, depression, paranoid states, and drug and
Modification of vascular risk factors includes (Alzheimer's alcohol intoxication. More than 90% of people with dementia
Society, 2005a): develop neuropsychiatric symptoms at some stage during their
• Treatment of strokes and transient ischaemic attacks illness (BaUard and Howard, 2006) (Table 2). These symptoms
• Blood pressure control: people with dementia and carers can be distressing for people with dementia and their carers, and
should be encouraged to comply with anti-hypertensive contribute to caregiver burden. They are often the precipitant
medication and have their blood pressure checked regularly for admission to institutional care (Yaffe et al, 2002).
• Management and treatment of hypercholesterolaemia: this Neuropsychiatric symptoms (especially depression and apathy)
may be achieved through manipulation of diet alone or in are also common in VaD. In DLB, the presence of delusions,
combination with the prescription of a statin hallucinations and depression are a core part of the disease.
• Modification ofalcohol intake: people with dementia should Challenging behaviour is often attributed to the dementing
be advised to drink in moderation, i.e. no more than two units process. However, while changes in the brain can cause
ofalcohol per day (one unit is the equivalent of one shot of behavioural disturbance it is also important to consider other
spirit, a small glass of wine or half a pint of beer/lager) factors which may be contributing to distressing behaviour.
British Journal of Nursing, 2008, Vol 17, No 4 243
Possible causes of challenging behaviour Communication difficulties
Background factors People with dementia might not be able to communicate their!
Factors, such as personality, leisure and occupational activities, needs verbally due to word-finding difficulty or dysphasia. i
and a person's habitual way of responding to stress, are Behaviour, such as calling out, agitation or wandering, might
important to consider; for example, a person might wander be a way of communicating need.
because they were used to walking in a previous occupation
(Monsour and Robb, 1982). Sundowning |
In dementia the sleep-wake cycle is often disturbed with '
Current factors individuals becoming more agitated or active at night (in [
These include medical and physiological factors, such as pain, some cases the cycle is reversed with individuals sleeping j
hunger, need for the toilet, and need for exercise. during the day and awake all night). 'Sundowning' refers to j
behavioural difficulties that worsen towards the end of the
Emotional state day, with symptoms including: restlesness, agitation, suspicious j
Consider whether behaviour has been triggered by emotion, behaviour, disorientation, visual and auditory hallucinations, '
such as boredom (people with dementia have a short attention less cooperation and increased argumentative tendancies. It
span but still require stimulating activities), anger or anxiety. can often be worse after a move or change in routine. j
Although the cause of sundowning is unknown it seems to
Neuropsychological deficits result from changes within the brain and may be linked to a
Changes within the brain can cause functional deficits, such lack of sensory stimulation after dark (Alzheimer's Australia,
as an inability to carry out complex tasks, which can then 2005); there are fewer cues towards late evening and less
lead to frustration. routine at night which may exacerbate confusion. People with
dementia tire more easily and can become more difficult to
Inability to orientate spatially manage. This can often be very stressful for carers.
Changes within the brain can affect perception and spatial
awareness.This may result in a patient getting in the wrong bed Coping with sundowning
or not being able to put their clothes on in the right order. • Keep person with dementia active during the morning and
encourage an early afternoon nap
Environmental factors • Avoid physical restraint, allow person with dementia to pace
Environmental factors can contribute towards challenging if safe to do so; an evening walk is sometimes helpful
behaviour especially in the hospital setting. These include: • Avoid caffeine towards late evening, and promote sleep by
• Ward layout providing hot milky drinks and gentle music
• Proximity to other people • Some people find it reassuring to sleep with the radio on
• Lacking control over routine (e.g. bed time and meal times) or night-lights
• Being in a strange environment • Preparing the environment, such as closing curtains and
• Unfamiliar tasks, such as catheterization and blood pressure encouraging the person with dementia to assist in evening
measurement meal preparation, may promote routine and reduce anxiety
• Sensory stimulation overload: the general noise and • Consider whether loud noise from television might
atmosphere of a busy ward can be overwhelming to a person exacerbate confusion
with dementia who sometimes find it difficult to make sense • Encourage participation in activities familiar from earlier
of their usual home environment (Kerr, 1997). times such as card games
• Avoid invasive procedures towards evening if possible
Table 1. Examples of challenging behaviour in dementia • Make sure physical needs are met such as nutrition,
hydration, elimination, pain
Behaviour Example
• Exclude physical illness as a possible cause of sundowning.
Difficult behaviour Refusal to'cooperate with therapy Management of behavioural problems in dementia is often
Aggressive/ Verbai or physicai aggression, destroying objects around others
multifactorial and needs to be tailored for the individual
disruptive or self, e.g. trying to pull out catheters, rummaging through
patient. People with dementia should be managed by skilled
iockers, interfering with other people's belongings, wandering
Deficient behaviour Behaviour may be hypoactive, apathetic or withdrawn multidisciplinary teams, and psychiatric and/or psychology
expertise may be needed. Delirium and depression must
always be looked for and treated. Physical symptoms, such as
Tabie 2. Prevaience of neuropsychiatric symptoms pain or constipation, should be treated. Sensory deficits should
in Aizheimer's disease be corrected. Good dementia care practice means that non-
pharmacological interventions should always be tried first.
• Apathy (loss of drive and motivation or lack feeiing or emotion) (50-70%) Pharmacological interventions should only be considered if
• Agitation (excessive motor activity that may manifest as restlessness, wandering there is serious distress or risk to the patient. Case Studies 1
and agitation) (20-60%) and 2 describe unusual behaviour in dementia and encourage
• Depression and anxiety (40%) practitioners to consider various possible causes of challenging
• Psychotic symptoms such as hallucinations and delusions (25%)
behaviour in addition to providing advice on how to adopt
Source: Ballard and Howard (2006)
non-pharmacological ways of managing such behaviour.
244 British Journal of Nursing. 2008, Vol 17, No 4
NEUROSCIENCE NURSING
Case study 1. Unusual behaviour
Mr B suffers from moderate Alzheimer's disease. He also walks very slowly and wears glasses. He attends the local memory clinic and is wife is his
main carer. Mrs B reports to the dementia nurse specialist that over the past few weeks her husband has become much more agitated and has started
to become disoriented in his own home. She is particularly distressed cis he has started to pass urine in the waste paper basket, is getting up to use the
toilet frequently at night and is occcisionally incontinent of urine.
Possible causes of behaviour Possible solutions
Urinary tract infection Dipstick urine. Encourage 2 litres of fluids a day
Nocturnal polyuria might indicate prostatic hypertrophy Seek medical advice
Constipation Establish normal bowel pattern. Mr B may need a rectal examination. Encourage high fibre
diet, increase fluids, consider aperients
Mistaking waste paper bin for toilet due Consider use of a commode or urine bottle but advise Mrs B to gently show her husband
to perception problems where the toilet is
Mr B might not see the toilet due to visual impairment Ensure glasses are worn and regular eye checks are performed
Mr B might not remember where toilet is in home Ensure a large sign is placed on toilet door with a picture of toilet and also the written word.
Keep a light on in the corridor at night
Mr B sometimes does not get to the toilet in time and is Encourage Mr B to use the toilet on a regular basis. Try establishing a 2 hour toileting regime.
incontinent due to limited mobility, and messages from Consider placing urine bottle near Mr B. Encourage elasticated, easy wear trousers and
the brain are taking longer to get through due to the underwear. Refer to district nursesforcontinence assessment and provision of continence pads
dementing process
Communication and dementia Music therapy
As people with dementia lose the ability to use and As the name suggests music therapy is an innovative way of
understand language, communication difficulties result in using musical improvisation (by chent and practitioner) to
frustration for the patient and caregiver (Alzheimer's Society, create a healing environment. It has been shown to treat the
2005b). However, for staff managing a confused patient there symptoms of dementia and improve quality of life for people
are simple ways to improve communication {Table 3). with dementia and carers (Alzheimer's Society, 2003).
Psyciiosociai interventions in dementia Reminiscence therapy
Recent guidance suggests that non-pharmacological/ This involves the discussion of past activities, events and
psychosocial interventions for the management of non-cognitive experiences with another person or group of people, usually
symptoms (such as hallucinations, delusions and anxiety) and with the aid of prompts, such as photographs, household and
challenging behaviour should be considered in the first instance other familiar items from the past and music. Reminiscence
unless there is an immediate risk of harm to the person with groups typically involve group meetings in which participants
dementia or others, or if there is severe distress then medication are encouraged to talk about past events. Life review
might have to be used as a first line measure (NICE, 2006). usually involves individual sessions, in which the person is
A range of approaches have been used although good quality guided chronologically through life experiences and may
evidence of benefit for many is lacking (Livingston et al, 2005). produce a life storybook. Reminiscence is interactive and
Qualitative evidence suggests that it is important to avoid informative. Knowing a little about a person's past, hobbies
compounding feelings of failure and humiliation where people and experiences helps carers to understand an individual
with demenda have difficulty with interventions, activities and better (Livingstone et al, 2005). Although evidence is lacking
games (NICE, 2006). for this intervention, it is widely used and not harmful to the
person with dementia.
Complementary therapy
The benefits of aromatherapy and massage have been shown to
be an effective way of alleviating agitation in severe dementia Table 3. Communication advice
(Alzheimer's Society, 2003; Ballard and Holmes, 2004).
• Break down tcisks into manageable chunks
• Keep environmental noise to a minimum, e.g turn TV down
Multisensory stimulation • Avoid hostile body language
Multisensory therapy includes visual, auditory, tactile and • Remain pleasant, calm and supportive
olfactory stimulation offered to clients in a specially designed • Maintain eye contact with your patient
room. Stimulating music, lights, aromas, and objects are • Use short sentences
offered to people with dementia in a non-sequential and • Speak slowly and wait for response
unpatterned fashion, which does not place great intellectual • Ask only one question at a time
• Keep the pitch of your voice low but ensure patient can hear you
stress on the patient. Multisensory stimulation/snoezelen
• Point, touch, show, initiate a movement for the patient
therapy reduced apathy compared with activity therapy or no
• Talk to the main carer. How do they communicate with your patient? Do they
therapy in people with moderate to severe dementia (Verkaik have any special advice?
et al, 2005).
British Journal of Nursing, 2008,Vol 17, No 4 245
group format. The informal format depends on environmental
Case study 2. The wandering patient cues and memory aids, such as clocks, calendars, newspapers'
and incidental conversations that reinforce orientating content.
Mr N is a 73 year-old gentleman who has severe vascular dementia. He lives at The classroom format involves small groups with similar levels
home with his family and is admitted to the local hospital for an endoscopy to
of cognitive function meeting several times a week to focus
investigate anaemia. He has jDrofound word-finding difficulty.
on orientating tasks. The classic task is completing the reality
Diagnosis orientation board, which summarizes information such as
• Diverticular disease the day, date, place, weather, etc. In a systematic review RO
• Osteoarthritis was shown to improve cognitive function and behaviour in
• Hypertension dementia (Spector et al, 1998).
• Hypercholesterolaemia
• Previous exposure to asbestos
Cognidve behavioural therapy (CBT)
Has given up smoking but used to smoke a packet a week. He used to be a postman.
CBT works by changing people s attitudes behaviour. Therapies
Current medication focus on thoughts, images and beliefs, and how this relates to
Simvastatin 10 mg once daily (OD) behaviour. Examples include progressive relaxation techniques,
Aspirin 75 mg od which reduce agitation and anxiety (Prasher, 2005).
Bendrofiumethiazide 2.5 mg od
Quetiapine (atypical antipsychotic) 25 mg per night (nocte) Environmental modification
Lorazepam (benzodiazepine) 0.5 mg when required (prn) Kerr (1997) suggests that environments might require
Beiiaviourai probiems modification to make them calm, familiar and safe. Examples
• Mr N wanders around the ward during the day but especially at night of environmental modification include: wall colour, signage, the
• He is disinhibited and walks around with his trousers unbuttoned structure of a building and flooring.
• He interferes with other patients and their belongings
• He tries to pick up imaginary items from the fioor Psychological interventions with caregivers
This upsets other patients and staff, and increases his risk of falls. However, Research evidence suggests that specific techniques
this behaviour is not new and his fcimily admit they lock him in at home. (psychoeducation) to teach caregivers how to change their
Reasons for exiiibiting sucii beiiaviour interactions with people with dementia may alleviate the
' Change of environment: Mr N is used to his own home and may be frightened
neuropsychiatric symptoms of dementia (such as agitation).
by hospital admission. Ask his family to bring in fcimiliar items for him such as There is also some evidence to suggest that family counselling
photographs can be helpful in reducing institutionalization of people with
• Looking for somebody/something: Mr N feels insecure and needs reassurance dementia (Livingston et al, 2005).
' Lacking stimulation: Mr N may be bored. Ask his family what activities he enjoys
doing at home Carers
' Depressed: consider performing a Cornell Assessment of Depression in Dementia There are over 4 million carers in the UK. One million
Scale
people provide care for more than 50 hours per week (Audit
' Sleeping too much in the day: encourage participation in activities and avoid naps
' Over-sedated: ask the medical team to review his medication especially quetiapine
Commission, 2004). Carers provide the vast majority of health
and lorazepam and community care. Their works saves the nation an estimated
In pain: remember Mr N has other medical problems, such as osteoarthritis. and /;87 billion per year (Carers UK, 2007).
may not be able to conceptualize pain and may be unable to verbalize his feelings There are high levels of stress, distress and psychological
due to word-finding difficulty. Observe for non-verbal signs of pain such as posture illness in family caregivers of individuals with dementia
' Responding to hostility and negative body language: staff and other patients may (Mahoney et al, 2004). Many studies have shown that the
unwittingly exacerbate the situation by being aggressive towards Mr N. Remember incidence of depression in caregivers is high, ranging from
other patients need reassurance 18-47% (Rosenthal et al, 1993; Teri and Traux, 1994), and
' Continuing a habit: Mr N was a postman and was used to spending hours at a time
caregivers who are depressed experience higher degrees
on his fieet. His wandering might be a result of pre-learned behaviour
of burden (Lawton et al, 1991). The degree of behavioural
• Consider environment. Is it safe for him to wander around a certain area of the ward?
problems in people with dementia appears to contribute to
caregiver burden (Baunigarten et al, 1994).
Validation therapy
This is the process of communication with disorientated Support for carers
elderly people by acknowledging and supporting their feeUngs Over the past decade the needs of informal carers have been
in whatever time or location is real to them, even though this recognized through legislation and government guidance.
may not correspond to our'here and now' reality (Jones, 1985). NICE (2006) has recently set out comprehensive guidance
Rather than correcting factual errors in conversation, one seeks regarding the assessment, interventions and practical support
to find out the real meaning behind communication. that should be available for carers.
Reality orientation NICE guidance on carer support
Reality orientation (RO) is aimed at reducing confusion and Assessment
inappropriate behaviours in people with dementia. RO can be Health and social care managers should ensure that the rights
divided into a 24-hour or informal format and a classroom or of carers to an assessment of needs - as set out in the Carers and
246 British Journal of Nursing, 2008, Vol 17, No 4
NEUROSCIENCE NURSING
Disabled Children Act 2000 and Carers (Equal Opportunities) Alzheimer's Australia (2005) Sundowning Information Sheet. Alzheimer's
Atistralia, Hawker, Australia
Act 2004 — are upheld. Carers' assessments should seek to Alzheimer's Society (2003) Complementary and Alternative Medicine and Dementia.
identify any psychological distress and the psychosocial impact Alzheimer's Society, London
Alzheimer's Society (2005a) What is Vascular Dementia? Information Sheet 402.
on the carer, including after the person with dementia has Alzheimer's Society London
entered residential care. Alzheimer's Society (2005b) Communication. Carers Advice Sheet 500. Alzheimer's
Society, London
Audit Commission (2004) Support for Carers of Older People. AC, London
Interventions Ballard C, Holmes C (2004) Aromatherapy in dementia. Advances in Psychiatric
Treatment 10: 296-300
Care plans for carers should include tailored interventions, Ballard C, Howard R (2006) Neuroleptic drugs in dementia: benefits and harm.
such as: Nat Rev Neurosd 7(6): 492-500
Baumgarten M, Hanley JA, Infante-Rjvard C, Battista R N , Becker R, Cauthier
• Individual or group psychoeducation S (1994) Health of family members caring for elderly penons with dementia.
A longitudinal study. Ann Intern Med 120(2): 126-32
• Peer-support groups tailored to the needs ofthe individual, Carers UK (2007) Valuing Carers — Calculating the Value of Unpaid Care.
e.g. the stage of dementia of the person being cared for carers UK, London. Available at: http://tinyurl.com/2q46xl (last accessed 20
February 2008)
• Telephone and internet information and support Clare L, Woods R T (2004) Cognitive training and cognitive rehabilitation for
• Training courses about dementia, services and benefits, and people with early-stage Alzheimer's disease: a review. Netiropsychol Rehabil
14(4): 385-401
dementia care problem-solving DanyszW, Parsons CG, Mobius HJ, Stoffler A, Quack G (2000) Neuroprotective
• Consider involving the person with dementia and other and symptomatological action of memantine relevant for Alzheimer's disease
— a unified glutamatergic hypothesis on the mechanism of action. Netirotox
family members, as well as the primary carer Res 2(2-3): 85-97
• Ensure support, such as transport or short-break services, is Francis PT, Palmer AM, Snape M, Wilcock GK (1999) T h e cholinergic
hypothesis of Alzheimer's disease: a review of progress. J Neurol Neurosur^
provided to enable carer participation in interventions Psychiatry 66(2): 137-47
• Offer psychological therapy, including cognitive behavioural Jones G (1985) Validation therapy: a companion to reality orientation. Can Nurs
81(3): 20-3
therapy, with a speciahst practitioner to carers who Kerr D (1997) Dowtt's Syndrome and Dementia — Practitioners G»jV/e.Ventura Press,
experience psychological distress and negative psychological Birmingham
KitwoodT (1997) Dementia ReconsidcrediTlie Person Comes First. Open University
impact. Press, Buckingham
Lawton MP, Moss M, Kleban M H , Glicksman A, Rovine M (1991) A two-factor
model of caregiving appraisal and psychological well-being. J Gerontol 46(4):
Practical support 181-9
Livingston G, Johnston K, Katona C et al (2005) Systematic review of
• Health and social care managers should ensure that carers psychological approaches to the management of neuropsychiatric symptoms
of people with dementia have access to: of dementia. AmJ Psychiatry 162(11): 1996-2021
Mahoney R, Regan C, Katona C, Livingston G (2004) Anxiety and depression
- A range of respite or short-break services in family caregivers of people with Alzheimer's disease: the L A S E R - A D Study.
- Services should meet the needs of both the carer (in AmJ Ceriatr Psychiatry 13(9): 795-801
Monsour N, Robb SS (1982) Wandering behaviour in old age. A psychosocial
terms of location, flexibility, and timeliness) and the study. SocTOrfe27(5): 411-6
person with dementia National Institute for Health and Clinical Excellence (2006) Dementia. Supporting
People with Dementia and their Carers in Health and Social Care. NICE, London
- Services should include, for example, day care, day- and Overshott R, Burns A (2005) Treamient of dementia.J Neurol Neurosurg Psychiatry
night-sitting, adult placement and short-term and/or 76(Suppl 5): v53—9
Prasher VP (2005) Alzheimer's Disease and Dementia in Doum Syndrome and
overnight residential care Intellectual Disabilities. Oxford Radcliffe, Oxford
- Transport to these services should be offered Rosenthal CJ, Sulman J, Marshall V W (1993) Depressive symptoms in family
caregivers of long-stay patients. Cerontotogist 33(2): 249—56
• Respite/short-break care should include therapeutic Spector A, Orrell M, Davies S et a! (1998) Reality orientation for dementia: a
review of the evidence of effectiveness Review: reality orientation improves
activities tailored to the person with dementia provided in cognitive fijnctioning and behaviour in dementia Cochrane Review, latest
an environment that meets their needs (the person's own venion 23 April.
Tarbuck P, Thompson T (1995) Defining and treating challenging behaviour.
home wherever possible). Nurs Stand 9(42): 30-3
Teri L,Truax P (1994) Assessment of depression in dementia patients: association
of caregiver mood with depression rating. Gerontologist 34(2): 231—4
Conclusion Verkaik R, van Weert J C M , Francke AL (2005) The effects of psychosocial
This article highlights the importance of coordinated care methods on depressed, a^ressive and apathetic behaviours of people with
dementia: a systematic review. IntJ Ceriatr Psychiatry 20(4): 301—14
and a person-centred approach to dementia care. It outlines Yaffe K, Fox P, Newcomer R et al (2002) Patient and caregiver characteristics and
reasons why a person with dementia might exhibit behaviour nursing home placement in patients with dementia.JAMA 287(16): 2090-7
that challenges and provides useful coping strategies.
Non-pharmacological interventions in the management
of dementia can be therapeutic although more research is KEY POINTS
needed to provide a greater evidence base.
Informal carers have a difficult task to perform and are I Management of dementia should focus on the maintenance of function
often isolated. It is hoped that practitioners will understand and independence for the person with the disease.
the needs of carers better and also feel more confident in i Modification of vascuiar risk factors is important in aii forms of dementia.
directing carers to support organizations. i Choiinesterase inhibitors are avaiiabie for symptomatic reiief of cognitive
Part 3 moves onto the advanced stages of dementia. It symptoms in Aizheimer's disease.
highlights the need for dementia to be recognized as a
terminal condition, which deserves equal access to palliative i Neuropsychoiogicai and behavioural probiems are very common in people
care services as other more recognized conditions, such as with dementia and a variety of non-pharmacologicai interventions are available.
cancer. The article is a useful point of reference for nurses I Carer burden can be improved by a number of interventions, including
working in the acute hospital setting and the community provision of information, education and training.
environment. IBS
British Journal of Nursing, 2008, Vol 17, No 4 247
S-ar putea să vă placă și
- Care of The Older or Disabled AdultDocument63 paginiCare of The Older or Disabled Adultfairwoods100% (1)
- 14 Essentials To Assessment and Care PlanMT2013!08!018-BRODATY - 0Document9 pagini14 Essentials To Assessment and Care PlanMT2013!08!018-BRODATY - 0Danielcc Lee100% (1)
- Person-Directed Dementia Care Assessment ToolDocument54 paginiPerson-Directed Dementia Care Assessment Tooldogstar23Încă nu există evaluări
- Person-Directed Dementia Care Assessment ToolDocument54 paginiPerson-Directed Dementia Care Assessment Tooldogstar23Încă nu există evaluări
- Nursing Handover of Vital Signs at The Transition of Care Fromthe Emergency Department To The Inpatient Ward Anintegrative ReviewDocument12 paginiNursing Handover of Vital Signs at The Transition of Care Fromthe Emergency Department To The Inpatient Ward Anintegrative ReviewLilac SpaceÎncă nu există evaluări
- Mental Status Examination (Mse)Document28 paginiMental Status Examination (Mse)Rujha Haniena Ahmad RidzuanÎncă nu există evaluări
- Mental Health Capacity Assessment Toolkit OverviewDocument34 paginiMental Health Capacity Assessment Toolkit OverviewWilliam David Guse100% (1)
- DementiaDocument27 paginiDementiaJerryÎncă nu există evaluări
- Care For People With Chronic Conditions Guide For Community Health ProgramDocument42 paginiCare For People With Chronic Conditions Guide For Community Health ProgramAndrew Wong100% (1)
- HLTH 300 Reflection - ReflectionDocument5 paginiHLTH 300 Reflection - Reflectionapi-479186899Încă nu există evaluări
- Home Environmental AssessmentDocument2 paginiHome Environmental AssessmentSelvi Puspa SariÎncă nu există evaluări
- Dementia Case Study PDFDocument4 paginiDementia Case Study PDFTha Rahmye PupareTha100% (1)
- Multiple Sclerosis: Saadia Perwaiz, PT BSPT, M. Phil-MskDocument39 paginiMultiple Sclerosis: Saadia Perwaiz, PT BSPT, M. Phil-MskArslan Aslam100% (2)
- Psych Student NotesDocument23 paginiPsych Student NotesReymund Timog TalarocÎncă nu există evaluări
- Integrative Support and Interprofessional Collaboration in Palliative Care ServicesDocument56 paginiIntegrative Support and Interprofessional Collaboration in Palliative Care Servicesrose fania100% (1)
- Practical Neurology basics: syndromic approachDocument42 paginiPractical Neurology basics: syndromic approachm2rv110100% (2)
- Dementia Care 3 End of Life CareDocument7 paginiDementia Care 3 End of Life Caredogstar23100% (1)
- Nursing Diagnosis List for Basic Human NeedsDocument28 paginiNursing Diagnosis List for Basic Human NeedsAmit MartinÎncă nu există evaluări
- Eliopoulos, Charlotte - Gerontological Nursing (2018, Wolters Kluwer) PDFDocument1.376 paginiEliopoulos, Charlotte - Gerontological Nursing (2018, Wolters Kluwer) PDFMara Alanan94% (17)
- (Theory, Technology and Society) Michael Schillmeier-Eventful Bodies - The Cosmopolitics of Illness-Ashgate (2014)Document196 pagini(Theory, Technology and Society) Michael Schillmeier-Eventful Bodies - The Cosmopolitics of Illness-Ashgate (2014)Alex Javier Garzon OrduñaÎncă nu există evaluări
- Care Plan Number 2Document5 paginiCare Plan Number 2Teddy mc Bones100% (1)
- Cognitive Stimulation and Caregiver Support for Dementia PatientsDocument22 paginiCognitive Stimulation and Caregiver Support for Dementia PatientsAnonymous iG0DCOfÎncă nu există evaluări
- Delirium: AntipsychoticDocument2 paginiDelirium: Antipsychoticdcde2004100% (1)
- Dementia Symptoms Diagnosis ManagementDocument7 paginiDementia Symptoms Diagnosis Managementdogstar23Încă nu există evaluări
- Dementia Symptoms Diagnosis ManagementDocument7 paginiDementia Symptoms Diagnosis Managementdogstar23Încă nu există evaluări
- Collaborative Care Between Nurse Practitioners and Primary Care PhysiciansDocument11 paginiCollaborative Care Between Nurse Practitioners and Primary Care PhysiciansLeek AgoessÎncă nu există evaluări
- Assessment and Plan of Care: SOAP Notes Writing Patient Centered Functional GoalsDocument5 paginiAssessment and Plan of Care: SOAP Notes Writing Patient Centered Functional GoalsAaron James GrayÎncă nu există evaluări
- Forensic PsychiatryDocument108 paginiForensic Psychiatrydvsgh100% (2)
- "Geriatrics": in A NutshellDocument22 pagini"Geriatrics": in A Nutshellaustinhitz100% (1)
- OT7 - Outcome of Occupational Therapy GroupDocument17 paginiOT7 - Outcome of Occupational Therapy GroupAnnbe BarteÎncă nu există evaluări
- Behavioral Disturbances of DementiaDocument16 paginiBehavioral Disturbances of DementiaWorldEventsForumÎncă nu există evaluări
- Etiopathogenesis of DeliriumDocument36 paginiEtiopathogenesis of DeliriumAarti Gupta100% (1)
- Ethical Dilemmas in Nursing PDFDocument5 paginiEthical Dilemmas in Nursing PDFtitiÎncă nu există evaluări
- DeliriumDocument10 paginiDeliriumwordlife360100% (1)
- Dementia Dementia Diagnosis and Assessment PDFDocument10 paginiDementia Dementia Diagnosis and Assessment PDFAyudiah Uprianingsih0% (1)
- Psycho Education on Dementia: Signs, Symptoms and DiagnosisDocument23 paginiPsycho Education on Dementia: Signs, Symptoms and DiagnosisAntony Jen100% (1)
- Older Adult Health Promotion ProjectDocument6 paginiOlder Adult Health Promotion Projectapi-404271262Încă nu există evaluări
- Dementia Care 1 Guidance AssessmentDocument9 paginiDementia Care 1 Guidance Assessmentdogstar23Încă nu există evaluări
- Dementia AssignmentDocument19 paginiDementia AssignmentVandna Vikram Novlani50% (2)
- Behaviour Response Flow Chart 5 Nov 2012Document1 paginăBehaviour Response Flow Chart 5 Nov 2012jakilaÎncă nu există evaluări
- Liverpool Care Pathway PDFDocument63 paginiLiverpool Care Pathway PDFBryan DorosanÎncă nu există evaluări
- Occupational Therapy and Mental Health - Add Summary and Bullet PointsDocument11 paginiOccupational Therapy and Mental Health - Add Summary and Bullet Pointsapi-339190475100% (1)
- Unit 9-Personal Care and GroomingDocument110 paginiUnit 9-Personal Care and Groomingtau88Încă nu există evaluări
- Reflective Case StudyDocument33 paginiReflective Case StudyAmir MahmoudÎncă nu există evaluări
- Module Guide For Palliative Care AssessmentDocument83 paginiModule Guide For Palliative Care AssessmentAnd ReiÎncă nu există evaluări
- ECT Therapy for Severe DepressionDocument4 paginiECT Therapy for Severe DepressionSatya IndraÎncă nu există evaluări
- Dementia Assessment Management and Support For People Living With Dementia and Their Carers PDF 1837760199109Document42 paginiDementia Assessment Management and Support For People Living With Dementia and Their Carers PDF 1837760199109Jsohna BelinaÎncă nu există evaluări
- A close look at a rehabilitation center helping those struggling with substance abuseDocument12 paginiA close look at a rehabilitation center helping those struggling with substance abuseAyesha JunaidÎncă nu există evaluări
- Capstone Research PaperDocument22 paginiCapstone Research Paperapi-251333389Încă nu există evaluări
- Medical Emergencies in Rehabilitation MedicineDocument24 paginiMedical Emergencies in Rehabilitation MedicineAzza El Awar100% (1)
- Occupational JusticeDocument4 paginiOccupational JusticeHardeep Singh BaliÎncă nu există evaluări
- Pain Management in the Elderly: A ReviewDocument9 paginiPain Management in the Elderly: A ReviewDara Agusti MaulidyaÎncă nu există evaluări
- Resident e Progress NotesDocument2 paginiResident e Progress Notesapi-273537080Încă nu există evaluări
- Care of Pediatric Client With Dermatologic DisorderDocument3 paginiCare of Pediatric Client With Dermatologic DisorderAraw GabiÎncă nu există evaluări
- Ma Cristy L. Exconde, MD, FPOGSDocument62 paginiMa Cristy L. Exconde, MD, FPOGSCAROL ANN PATITICO100% (1)
- Running Head: CASE STUDY 1Document17 paginiRunning Head: CASE STUDY 1api-507206712Încă nu există evaluări
- Cognitive Decline And/orDocument17 paginiCognitive Decline And/orDinusha Saminda SirisenaÎncă nu există evaluări
- Medication Administration Error 3Document16 paginiMedication Administration Error 3Priya bhattiÎncă nu există evaluări
- Managing Type 2 Diabetes and Comorbidities with an Advanced Practice NurseDocument4 paginiManaging Type 2 Diabetes and Comorbidities with an Advanced Practice NurseChristine Guibao100% (1)
- Pocket Guide To 2015 Beers Criteria PDFDocument7 paginiPocket Guide To 2015 Beers Criteria PDFYuliEdySeringnyungsepÎncă nu există evaluări
- Evidence-Based Answers To Clinical Questions For Busy CliniciansDocument28 paginiEvidence-Based Answers To Clinical Questions For Busy CliniciansMohmmed Abu Mahady100% (1)
- Beyond Person Centred CareDocument11 paginiBeyond Person Centred CareJando Minggo SimonÎncă nu există evaluări
- Seizures in Children JULIO 2020Document29 paginiSeizures in Children JULIO 2020Elizabeth HendersonÎncă nu există evaluări
- HCA Job DescriptionDocument2 paginiHCA Job DescriptionAnonymous 8sBh71wrHÎncă nu există evaluări
- Ventricular Septal Defect, A Simple Guide To The Condition, Treatment And Related ConditionsDe la EverandVentricular Septal Defect, A Simple Guide To The Condition, Treatment And Related ConditionsÎncă nu există evaluări
- SECTION 5 - Diagnostic Criteria For DementiasDocument3 paginiSECTION 5 - Diagnostic Criteria For Dementiasdogstar23Încă nu există evaluări
- Neuro-Pathological Effects of Alcohol and SolventsDocument4 paginiNeuro-Pathological Effects of Alcohol and Solventsdogstar23Încă nu există evaluări
- Mild Cognitive Impairment in Older PeopleDocument8 paginiMild Cognitive Impairment in Older Peopledogstar23Încă nu există evaluări
- Management of Severe Alzheimer DiseaseDocument10 paginiManagement of Severe Alzheimer Diseasedogstar23Încă nu există evaluări
- Evaluation of The NINCDS-ADRDA CriteriaDocument6 paginiEvaluation of The NINCDS-ADRDA Criteriadogstar23Încă nu există evaluări
- Alcohol Intake and Risk of DementiaDocument8 paginiAlcohol Intake and Risk of Dementiadogstar23Încă nu există evaluări
- Clinical Diagnostic Criteria For AD and FTDDocument2 paginiClinical Diagnostic Criteria For AD and FTDdogstar23Încă nu există evaluări
- Subjective Memory Deterioration and Future DementiaDocument8 paginiSubjective Memory Deterioration and Future Dementiadogstar23Încă nu există evaluări
- Dementia - StatPearls - NCBI BookshelfDocument7 paginiDementia - StatPearls - NCBI BookshelfSMA N 1 TOROHÎncă nu există evaluări
- Geriatric Assessment: An Office-Based Approach: Older AdultsDocument13 paginiGeriatric Assessment: An Office-Based Approach: Older AdultsDonna DominnoÎncă nu există evaluări
- Caregiver Burden Among Caregivers of Patients With Mental Illness: A Systematic Review and Meta-AnalysisDocument16 paginiCaregiver Burden Among Caregivers of Patients With Mental Illness: A Systematic Review and Meta-AnalysisKatalin VikukÎncă nu există evaluări
- Psychosocial Interventions Improve Dementia Outcomes and Quality of LifeDocument11 paginiPsychosocial Interventions Improve Dementia Outcomes and Quality of Lifeariadna17Încă nu există evaluări
- Speech OutlineDocument3 paginiSpeech Outlinekarlymae33% (3)
- Autism, Impulsivity and Inhibition A Review of The LiteratureDocument13 paginiAutism, Impulsivity and Inhibition A Review of The Literaturecsepulveda10Încă nu există evaluări
- Psych Micro Teaching - AlzheimersDocument10 paginiPsych Micro Teaching - Alzheimersapi-269113291Încă nu există evaluări
- Understanding Dementia vs DeliriumDocument3 paginiUnderstanding Dementia vs DeliriumKirstin del CarmenÎncă nu există evaluări
- Nutrition and Dementia Care: Developing An Evidence-Based Model For Nutritional Care in Nursing HomesDocument14 paginiNutrition and Dementia Care: Developing An Evidence-Based Model For Nutritional Care in Nursing HomesJuan Olmo RomeroÎncă nu există evaluări
- Impacts of Applied Theatre on Ageing PopulationsDocument5 paginiImpacts of Applied Theatre on Ageing PopulationsThomas MooreÎncă nu există evaluări
- 1 4Document124 pagini1 4Angeline PatriciaÎncă nu există evaluări
- Evidences On Alzheimer S Disease Through The Analysis of Speech Pauses DistributionDocument10 paginiEvidences On Alzheimer S Disease Through The Analysis of Speech Pauses DistributionTherfer WarnÎncă nu există evaluări
- Dementia: Maartje I Kester, Philip ScheltensDocument11 paginiDementia: Maartje I Kester, Philip ScheltensStyliani KaramanouÎncă nu există evaluări
- Memantine 3Document15 paginiMemantine 3Marjan StosicÎncă nu există evaluări
- CNS DrugsDocument57 paginiCNS DrugsHussein Al-jmrawiÎncă nu există evaluări
- HCA 112 Capstone ProjectDocument16 paginiHCA 112 Capstone ProjectDr Nithya RajanÎncă nu există evaluări
- Frontal Assessment Battery SVUH MedEl ToolDocument2 paginiFrontal Assessment Battery SVUH MedEl ToolclauytomasÎncă nu există evaluări
- The Best Friends Approach To Dementia Care, Second Edition (Excerpt)Document13 paginiThe Best Friends Approach To Dementia Care, Second Edition (Excerpt)Health Professions Press, an imprint of Paul H. Brookes Publishing Co., Inc.Încă nu există evaluări
- The Relation Between Instrumental Music Activity and Cognitive AgingDocument23 paginiThe Relation Between Instrumental Music Activity and Cognitive AgingAsma AssidiÎncă nu există evaluări
- 16 June Dementia - Personal Experience Robin ThomsonDocument15 pagini16 June Dementia - Personal Experience Robin ThomsonKreshnik IdrizajÎncă nu există evaluări
- Clinical Questions PICO and Study Design EBM Part 1Document47 paginiClinical Questions PICO and Study Design EBM Part 1Yaser ZaherÎncă nu există evaluări
- Cognitive AgingDocument331 paginiCognitive AgingNiltom VieiraÎncă nu există evaluări
- Brain Breakthroughs MASTERCLASS Private WorkbookDocument15 paginiBrain Breakthroughs MASTERCLASS Private WorkbookRida ArifÎncă nu există evaluări
- 2015, Depression and Cognition in The Elderly, WangDocument30 pagini2015, Depression and Cognition in The Elderly, WangdiurrutiagÎncă nu există evaluări