Documente Academic
Documente Profesional
Documente Cultură
Leptospirosis
Încărcat de
Vyramuthu AtputhanDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Leptospirosis
Încărcat de
Vyramuthu AtputhanDrepturi de autor:
Formate disponibile
Leptospirosis
Description
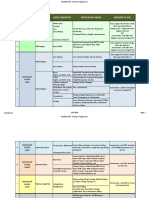
Leptospirosis is a disease that is caused by pathogenic spirochetes of the genus Leptospira Interrogans. It is a bacterial infection passed from animals to humans by way of contaminated urine. The bacteria penetrate mucous membranes or breaks in the skin,multiply in the bloodstream and carried to all parts of the body. Contents 1. 2. 3. 4. 5. 6. 7. 8. 1 Description 2 Causes of Leptospirosis 3 Outbreak of Leptospirosis 4 Signs and Symptoms 5 Incubation Period 6 Diagnosis 7 Treatment 8 Nursing Management 1. 8.1 Health teaching 2. 8.2 Management
Causes of Leptospirosis
Leptospirosis is not only acquired from absorbing contaminated flood waters through cuts in the skin but also by swallowing the bacteria directly from water or through food. Although the disease is commonly associated with rat urine, infection can also come from animals like cattle, pigs, horses, dogs, and wild animals.
Outbreak of Leptospirosis
The largest recorded U.S. outbreak occurred in 1998, when 775 people were exposed to the disease. Of these, 110 became infected. In the Philippines as of January 6 2012 the outbreak of leptospirosis was in northern Mindanao cities of Cagayan de Oro and Iligan that were devastated by flood and reported almost 300 cases and 15 deaths according to Cagayan de Oro City Health Office.
Signs and Symptoms
Leptospirosis can cause a wide range of symptoms, including:
High fever Headache Chills Muscle aches Vomiting Jaundice (yellow skin and eyes) Red eyes Abdominal Pain Diarrhea Rash
Many of these symptoms can be mistaken for other diseases. In addition, some infected persons may have no symptoms at all.The time between a persons exposure to a contaminated source and becoming sick is 2 days to 4 weeks. Illness usually begins abruptly with fever and other symptoms. Leptospirosis may occur in two phases: after the first phase (with fever, chills, headache, muscle aches, vomiting, or diarrhea) the patient may recover for a time but become ill again. if a second phase occurs, it is more severe; the person may have kidney or liver failure or meningitis. This phase is also called Weils disease.
The illness lasts from a few days to 3 weeks or longer. Without treatment, recovery may take several months..
Incubation Period
The incubation period usually 7 to 12 days, with a range of 2 to 29 days.
Diagnosis
Leptospirosis can be diagnosed by its clinical manifestation culture of the organism examination of blood and CSF during the first week of illness and urine after the 10 day. Generally, it is not necessary to confirm the diagnosis or wait for the result of the tests before starting treatment. The clinical assessment and epidemiologic history are more important. Early recognition and treatment is MORE important to prevent complications of the severe disease and mortality.
Treatment
Penecilins and other B- lactam antibiotics(PCN at 2M units q6H IM/IV) Teracycline(Doxycycline at 100mg q12H PO) Erythromycin (500mg q12H PO)- if allegic to Penicillin
Nursing Management
Health teaching
Provide education to clients telling them to avoid swimming or wading in potentially contaminated water or flood water. Use of proper protection like boots and gloves when work requires exposure to contaminated water. Drain potentially contaminated water when possible. Control rats in the household by using rat traps or rat poison, maintaining cleanliness in the house.
Management
Isolate the patient and concurrent disinfection of soiled articles. Stringent community-wide rat eradication program.Remove rubbish from work and domestic environment to reduce rodent population. Report all cases of leptospirosis. Investigation of contacts and source of infection Chemoprophylaxis can be done in a group of high risk infected hosts.
Nursing Lecture on Communicable Disease Presentation Transcript
1. Brought to you by : http://1nurses.com 2. Disclaimer All information and pictures presented in this slideshow were meant for EDUCATIONAL purposes only. 1Nurses.com does not claim any liability from the use of this slide and does not guarantee any action that might result from the use of this material. 1Nurses.com does not claim any ownership for the images and articles presented in this report. All articles and Images are the respective Copyright of the respective owners. 3. COMMUNICABLE DISEASE Is any disease that can be transmitted directly or indirectly from one person to another 4. INFECTION Is a condition caused by the entry and multiplication of pathogenic microorganisms within the host body. It is also an invasion of an organisms (bacteria, helminths, fungi, parasite, ricketsia and prion) 5. FACTORS AFFECTING RISK OF INFECTION AGE HEREDITY LEVEL OF STRESS NUTRITIONAL STATUS CURRENT MEDICAL THERAPY PRE-EXISTING DISEASE IMMUNIZATION STATUS 6. IMMUNITY THE QUALITY OF BEING INSUSCEPTIBLE TO OR UNAFFECTED BY A PARTICULAR DISEASE. 7. TYPES OF IMMUNITY INNATE = within the HOST Immune System ACQUIRED = inoculation and disease Active Passive 8. IMMUNE SYSTEM PROTECTION AGAINST ANTIGEN OR DISEASES BY A SYSTEM OF ANTIBODY PRODUCTION ANTIBODY PRODUCED BY LYMPHOCYTES IN RESPONSE TO ANTIGEN. ANTIGEN TRIGGERING AGENT OF THE IMMUNE SYSTEM 9. IMMUNOGLOBULINS IgG MOST PREVALENT ANTIBODY 80%, PRODUCE LATER IN THE IMMUNE RESPONSE, ONLY Ig THAT CAN CROSS THE PLACENTA IgA FOUND IN COLOSTRUM , TEARS, SALIVA, SWEAT IgM PRINCIPAL ANTIBODY OF BLOOD, QUICKLY PRODUCED IN RESPONSE TO AN ANTIGEN, RESPONDS TO ARTIFICIAL IMMUNIZATION IgE ALLERGIC REACTION IgD UNKNOWN, ANTIGEN RECEPTOR, FOUND IN THE SURFACE OF B CELLS
10. IMMUNIZATION A PROCESS BY WHICH RESISTANCE TO AN INFECTIOUS DISEASE IS INDUCED OR AUGMENTED. ACTIVE AND PASSIVE IMMUNIZATION 11. EPI Hepa b 3 shots, 0-1-6 mo, im, 0.5 ml, vas. lateralis Bcg 1 at birth, id, 0.05 ml, right arm Bcg 2 at 6 y/o, id, 0.1 ml, left arm Dpt 3 shots, 6 weeks old, 4 weeks interval im, 0.5 ml, vas. lateralis Opv 3x, same with dpt, oral gtts, 2-3 months Measles 1x, 9 mo, sq, 0.5 ml, right arm 12. Active Immunity ANTIBODIES ARE PRODUCED BY THE BODY IN RESPONSE TO INFECTION. ANTIGEN IS INTRODUCED, LONG DURATION EXAMPLE: NATURAL ACTIVE = DISEASE ARTIFICIAL ACTIVE = VACCINES 13. ARTIFICIAL ACTIVE ANTIGENS (VACCINES OR TOXOIDS) ARE ADMINISTERED TO STIMULATE ANTIBODY PRODUCTION. REINFORCED BY BOOSTER DOSE TO INCREASE IMMUNITY. KILLED VACCINES PERTUSSIS VACCINE, TYPHOID VACCINE LIVE VACCINES ATTENUATED, WEAKENED SABIN, MEASLES TOXOID INACTIVATED BACTERIAL TOXIN-TETANUS, DIPHTHERIA 14. Artificial Active 15. Artificial Active 16. Artificial Active 17. PASSIVE IMMUNITY ANTIBODIES ARE PRODUCED BY ANOTHER SOURCE. ANTIBODIES ARE INTRODUCED, SHORT DURATION Example: NATURAL PASSIVE = MOTHER ARTIFICIAL PASSIVE = GLOBULINS 18. ARTIFICIAL PASSIVE IMMUNE SERUM (ANTIBODY) FROM ANIMAL OR HUMAN IS INJECTED. PROVIDE IMMEDIATE PROTECTION (DIPHTHERIA ANTITOXIN, TETANUS ANTITOXIN) SKIN-TESTING IS A MUST. 19. CONDITIONS BEFORE AN INFECTION DEVELOPS Sufficient number of microorganisms Virulence of microorganisms Resistance of the of the host Immunity of the host Cycle of infection must be completed 20. THE INFECTION PROCESS CYCLE Agent (bacteria or virus) Reservoir (fomites or living things) Portal of Exit Mode of Transmission (direct or indirect) Portal of Entry The Host 21. STAGES OF AN INFECTIOUS PROCESS INCUBATION PERIOD PRODROMAL PERIOD ILLNESS PERIOD (PATHOGNOMONIC SIGN) CONVALESCENT PERIOD 22. Terminologies ETIOLOGY EPIDEMIOLOGY INCIDENCE PREVALENCE ENDEMIC EPIDEMIC PANDEMIC SPORADIC 23. FUNDAMENTALS OF STANDARD PRECAUTION HANDWASHING GLOVES MASKS, GOGGLES, FACE SHIELDS AIR FILTERS GOWNNS ISOLATION STRICT ISOLATION CONTACT ISOLATION RESPIRATORY ISOLATION TUBERCULOSIS ISOLATION ENTERIC PRECAUTION DRAINAGE/SECRETION PRECAUTION BLOOD/BODY FLUIDS PRECAUTION 24. ISOLATION It is necessary when a person is known or suspected to be infected with pathogens that can be transmitted by direct or indirect contact. The
principle behind isolation technique is to create a physical barrier that prevents the transfer of infectious agents. To do this you have to know how the organisms are transmitted. 25. Transmission-Based Precautions Airborne Droplets Contact 26. AIRBORNE PRIVATE ROOM NEGATIVE AIR PRESSURE VENTILATION SAFEGUARDS air from room is not recirculated to other areas DOOR SHOULD BE KEPT CLOSED BARRIER TO SMALL PARTICLES masks HEPA high efficiency particulate air COVER MOUTH OF PATIENT WITH MASK DURING TRANSPORT 27. 28. DROPLET PRIVATE ROOM WEAR MASK IF WORKING WITHIN 3 FEET WEAR MASKS UPON ENTRY INTO THE ROOM COVER MOUTH OF PATIENT WITH MASK DURING TRANSPORT 29. CONTACT PRIVATE ROOM WEAR GLOVES GLOVES ARE REMOVED BEFORE EXITING FROM THE ROOM HANDS ARE WASHED THOROUGHLY NOTHING IS TOUCHED BEFORE EXITING THE ROOM GOWN IS WORN WHEN ENTERING THE ROOM REMOVE GOWN CAUTIOUSLY BEFORE LEAVING THE ROOM PATIENT CARE ITEMS SHOULD BE RESTRICTED TO SINGLE PATIENT 30. OTHER TYPE OF ISOLATION AFB ISOLATION STRICT ISOLATION RESPIRATORY ISOLATION WOUND AND SKIN ISOLATION ENTERIC ISOLATION PROTECTIVE OR REVERSE ISOLATION 31. AFB ISOLATION VISITORS REPORT TO NURSES STATION BEFORE ENTERING ROOM MASKS ARE TO BE WORN IN THE PATIENTS ROOM GOWNS ARE INDICATED TO PREVENT CLOTHING CONTAMINATION GLOVES ARE INDICATED FOR BODY FLUIDS AND NON-INTACTSKIN HANDWASHING-after touching the patient or potentially contaminated articles and after removing gloves articles should be discarded, cleaned or sent for decontamination and reprocessing room is to remain closed patient is to wear mask during transport 32. STRICT ISOLATION VISITORS-REPORT TO NURSES STATION BEFORE ENTERING ROOM PRIVATE ROOM-necessary, door must be kept closed GOWNS-must be worn by all persons entering the room MASKS- must be worn by all persons entering the room HANDS-must be washed on entering and leaving room GLOVES-must be worn by all persons entering the room ARTICLES-must be discarded, or wrapped before being sent to CENTRAL SUPPLY for disinfection or sterilization 33. RESPIRATORY ISOLATION VISITORS-REPORT TO NURSES STATION BEFORE ENTERING ROOM PRIVATE ROOM-necessary, door must be kept closed GOWNS-gowns not necessary MASKS- must be worn by all persons entering the room if susceptible disease HANDS-must be washed on entering and leaving room GLOVES-not necessary ARTICLES-those contaminated with secretions must be disinfected CAUTION-all persons susceptible to the specific disease should be excluded from the area, susceptibles must wear masks
34. WOUND AND SKIN PRECAUTIONS VISITORS-REPORT TO NURSES STATION BEFORE ENTERING ROOM PRIVATE ROOM-desirable GOWNSmust be worn by all persons having direct contact with the patient MASKSduring dressing changes HANDS-must be washed on entering and leaving room GLOVES-must be worn by all persons having direct contact with infected area ARTICLES-instruments, dressing, linens 35. ENTERIC PRECAUTIONS VISITORS-REPORT TO NURSES STATION BEFORE ENTERING ROOM PRIVATE ROOM-necessary FOR CHILDREN ONLY GOWNS- must be worn by all persons having direct contact with the patient MASKS- not necessary HANDS-must be washed on entering and leaving room GLOVES-must be worn by all persons having direct contact with patient or articles contaminated with fecal material ARTICLES-special precautions necessary for articles contaminated with urine and feces, must be disinfected or discarded 36. PROTECTIVE ISOLATION VISITORS-REPORT TO NURSES STATION BEFORE ENTERING ROOM PRIVATE ROOM-necessary, door must be kept closed GOWNS- must be worn by all persons entering room MASKS- - must be worn by all persons entering room HANDS-must be washed on entering and leaving room GLOVES-must be worn by all persons having direct contact with patient 37. DIAGNOSTIC TOOLS COLLECTION OF SPECIMEN PRINCIPLES TYPES OF SPECIMEN COLLECTION BLOOD URINE STOOL SPUTUM WOUNDS THROAT 38. LABORATORY TESTS MICROSCOPY CULTURE ANTIBIOTIC SUSCEPTIBILITY TESTING WHITE BLOOD CELL COUNT IMMUNOLOGIC TEST 39. DISORDERS CNS DISEASES GIT DISEASES RESPIRATORY DISEASE BLOOD BORNE DISEASES ERUPTIVE FEVER DISEASES CONTACT DISEASE SEXUALLY TRANSMITTED DISEASES TORCHS HIV AND AIDS HEPATITIS 40. CNS 41. Tetanus Clostridium tetani MOT = wound setting IP = 3 -21 days IMMUNITY Active = TT Passive = TAT and TIG Natural = active none, passive (+) 42. Tetanus Wound Infection FATAL INFECTION OF THE CNS TOXINNEUROTOXIN 43. PATHOPHYSIOLOGY: SETTING OF WOUND ---- ENTRANCE OF C.T. ---- RELEASES TETANUS TOXIN ---- TETANOSPASMIN (CNS), TETANOLYSIN (BLOOD) ---- ABSORBED BY MOTOR NERVE ENDINGS ---- SYNAPSE (CONNECTION BETWEEN NEURONS) ---- MYONEURAL JUNCTION ---- ACETYLCHOLINE DISTURBANCE IN THE TRANSMISSION OF NERVE IMPULSE 44. Trismus lock jaw Risus sardonicus - maskface Risorius - grinsmile Dx wound and blood extraction (non specific) 45.
46. Immunization DPT (0.5 ml IM) 1 1 months old 2 - after 4 weeks 3 after 4 weeks 1 st booster 18 mos 2 nd booster 4-6 yo subsequent booster every 10 yrs thereafter TT (0.5 ml IM) TT1 - 6 months within preg TT2 - one month after TT1 TT3 to TT5 - every succeeding preg or every year TAT (horse) and TIG (human) 47. 3 types of patients w/ skin wounds post exposure prophylaxis (+) immunization as a child w/ boosters but last shot > 10 yrs give TT 2. (-) immunization - TT + TIG/TAT 3. (+) tetanus TIG/TAT + TT + Abx + wound cleansing + supportive therapy 48. Management 1. Anticonvulsant, muscle relaxants, antibiotics, wound cleansing and debridement, hyperbaric chamber 2. Active-DPT and tetanus toxoid 3. Passive-TIG and TAT, placental immunity 49. Rabies/Lyssa (Zoonotic) Rhabdovirus/filterable virus MOT = Bite from warm blooded animals Canine (human) and sylvatic (animals) IP = 10 days to several years IMMUNITY Active = rabies vaccine Passive = HRIG, ERIG Natural = active none, passive none 50. Rabies/Lyssa (Zoonotic) Hydrophobia (fear of choking) Aerophobia (laryngospasm) Bite from warm blooded animals Encephalitis/meningitis/respiratory paralysis 51. 52. Category of bites I intact skin (lick) II mucosal, non bleeding wounds, abrasions III bleeding bites and above neck, stray dogs, laceration, multiple bites 53. Rabies/Lyssa (Zoonotic) Observe dog for maniachal s/sx Active-rabies vaccine Passive-rabies immunoglobulin Dx History taking Quarantine the dog Staining of brain tissue (dog) (+) Negri bodies 54. AFTER THE BITE WASH WITH SOAP AND WATER GIVE ANTIBIOTICS AND ANTITETANUS OBSERVE DOG FOR 14 DAYS, IF IT DIES CONSULT DOCTOR IF DOG SHOWS SUGGESTIVE OF RABIES, KILL THE DOG IMMEDIATELY AND BRING HEAD FOR LAB EXAM (+) NEGRI BODIES SUBMIT FOR IMMUNIZATION WHILE WAITING FOR RESULTS IF DOG IS NOT AVAILABLE FOR OBSERVATION SUBMIT FOR IMMUNIZATION 55. Immunization Rabies vaccine (5 shots) IM (2 ml deltoid) 0, 3, 7, 14, 28 days ID (0.1 ml deltoid) 0, 3, 7 days (0.1 ml deltoid 2 shots) 30, 90 days (0.1 ml deltoid single shot) Rabies immunoglobulin (HRIG and ERIG) IM (0.2 x kg) single shot wound 40% deltoid 60% 56. 4 STAGES 1. prodrome - fever, headache, paresthesia, 2. encephalitic excessive motor activity, hypersensitivity to bright light, loud noise, hypersalivation, dilated pupils 3. brainstem dysfunction dysphagia, hydrophobia, apnea 4. death/recovery 57. RESPONSIBLE PET OWNERSHIP HAVE PET IMMUNIZED AT 3 MONTHS AND EVERY YEAR AFTER NEVER ALLOW PETS TO ROAM IN THE STREET LEASHED YOUR DOG YOUR PET ACTION IS YOUR RESPONSIBILITY
58. Poliomyelitis Infantile Paralysis Polio virus, Legio debilitans Legio brunhilde (fatal) Legio lansing Legio leon MOT = Fecal oral route (common) and droplets IP = 7-12 days IMMUNITY Active = OPV Passive = none Natural = active (+), passive none 59. Poliomyelitis Infantile Paralysis Assymetrical paralysis Haynes sign - head drop Pokers sign - opisthotonus Landrys sign - ascending paralysis Pandys Test increased in CSF CHON 60. Poliomyelitis Infantile Paralysis I abortive or inapparent II meningitis (non-paralytic) III paralytic (anterior horn of spinal cord) IV bulbar (encephalitis) 61. 62. 63. Meningitis Menigococcemia Neisseria meningitides (bacteria) MOT = droplets IP = 1-2 days IMMUNITY = xxx 64. Meningitis Menigococcemia Immunocompetent are susceptible Petechiae (volar/palm of hands) EARLY Opisthotonus MENIGEAL IRRITATION Brudzinski MENINGEAL IRRITATION Kernigs MENINGEAL IRRITATION Increased ICP BRAIN Seizure BRAIN 65. Menigococcemia S/sx: Meningococcemia spiking fever, chills, arthralgia, petechial rash Fulminant Meningococcemia (Waterhouse Friderichsen) septic shock; hypotension, tachycardia, enlarging petecchial rash, adrenal insufficiency Meningitis most common; nuchal rigidity, brudzinski, kernigs, Photophobia, confusion 66. Menigococcemia Dx: CT/ MRI, CSF analysis, CSF gram stain, CSF and blood culture Mgmt: antibiotics (Pen G, ceftriaxone), steroids, anticonvulsants, Rifampin for close contacts of meningococcemia 67. Encephalitis Arbo virus (arthropod borne virus) MOT = bite from mosquito (St. Louise) IP = xxx IMMUNITY = xxx 68. Encephalitis S/sx: fever, abdominal pain, sore throat, respiratory symptoms, headache, meningeal signs, photophobia, Seizure (lacrosse), SIADH w/ hypoNa (St Louis) Dx: CSF analysis r/o other CNS disease, CT scan, MRI Mgmt: nonspecific; control seizures 69. Leprosy Mycobacterium Leprae, Hansens Bacillus MOT = (unknown) may be due to prolonged skin-skin contact (common) or droplets IP = years to decades IMMUNITY Active = BCG Passive = none Natural = none 70. Leprosy EARLY Skin lesion and paresthesia LATE Lagopthalmos Madarosis Gynecomastia Saddle Nose Contractures 71. Leprosy 72. Leprosy Dx: Lepromin Test ID injection Slit Skin Smear DapsoneLamprene-Rifampicin Dapsone-dont give to anemic Lamprene-dry skin, hyperpigmentation (lasting) Rifampicin-renal and liver toxicity 73. Leprosy MDT-RA 4073 (home meds) Paucibacillary - 6-9 months 1. Dapsone 2. Rifampicin Multibacillary- 12-24 months 1. Dapsone mainstay; hemolysis, agranulocytosis 2. Clofazimine reddish skin pimentation, intestinal toxicity 3. Rifampicin bactericidal; renal and liver toxicity
74. Leprosy MDT- two or more drugs RA 4073 (home meds) Paucibacillary.- 6-9 months Multibacillary.- 12-24 months Tuberculoid high resistant, less severe (+LT) Lepromatous most severe, low resistant (-LT) 75. Leprosy Non - communicable After 1 week of medication Considered cured After completing the course of treatment 76. Red Tide Poisoning Pyromidium Bahamense Exotoxin Dinoflagellates Plankton Algae MOT = Ingestion of contaminated bi-valve shellfish IP = within 30 minutes IMMUNITY = xxx 77. Red Tide Poisoning Dx gastric siphoning EARLY Circumoral numbness nausea and vomiting LATE Bulbar paralysis and metabolic acidosis Mgmt: emesis/gastric lavage + activated charcoal, supportive 78. CLINICAL MANIFESTATIONS: NUMBNESS OF THE FACE ESPECIALLY AROUND THE MOUTH VOMITING, DIZZINESS, HEADACHE TINGLING SENSATION, WEAKNESS RAPID PULSE, DIFFICULTY OF SPEECH (ATAXIA), DYSPHAGIA, RESPI PARALYSIS, DEATH. 79. MANAGEMENT AND CONTROL MEASURES: NO DEFINITE MEDICATIONS INDUCE VOMITING (EARLY INTERVENTION) DRINKING PURE COCONUT MILK (WEAKENS TOXIC EFFECT) DONT GIVE DURING LATE STAGE IT MAY WORSEN THE CONDITION. NaHCO3 SOLUTION (25 GRAMS IN GLASS OF WATER) RESPIRATORY SUPPORT AVOID USING VINEGAR IN COOKING SHELLFISH AFFECTED BY RED TIDE (15X virulence) TOXIN OF RED TIDE IS NOT TOTALLY DESTROYED IN COOKING. AVOID TAHONG, TALABA, HALAAN, KABIYA, ABANIKO. WHEN RED TIDE IS ON THE RISE. 80. Botulism Clostridium Botulinum (bacteria) Endotoxin MOT canned foods Ingestion of contaminated foods) IP = 12-36H canned food, 4-14 days wound IMMUNITY Active = xxx Paiive = botulinum antitoxin Natural = xxx 81. Botulism Dx = gastric siphoning EARLY VISUAL DIFFICULTY, DYSPHAGIA, DRY MOUTH LATE VOMITING, CONSTIPATION/DIARRHEA DESCENDING SYMMETRICAL FLACCID BULBAR PARALYSIS 82. GIT 83. 84. Amoebiasis Entamoeba Hystolitica protozoan (parasite) MOT = 5 Fs, fecal oral route IP = 2-4 weeks IMMUNITY = xxx 85. Amoebiasis Dx microscopic stool exam or rectal secretions (tetra nucleated cyst and trophozoites) Diarrhea and constipation (non dysenteric) Blood streaked, diarrhea and watery mucoid, abdl cramps (dysenteric) Extra amoebiasis-penile, vagina, spleen, liver, anal, lungs and meninges Metronidazole (Flagyl) 86. Bacillary Dysentery Shigellosis Shiga bacillus (bacteria) s. dysenterae (fatal) s. flexneri (common in the Philippines) s. boydii s. sonnei MOT = same with amoebiasis IP = 1-7 days IMMUNITY = xxx 87. Bacillary Dysentery Shigellosis Dx stool exam Watery mucoid, bloody with pus feces Tenesmus = rectal prolapse Chloramphenicol, Tetracycline
88. Cholera, El Tor Vibrio Coma (inaba, ogawa, hikojima) Vibrio Cholerae Vibrio El Tor (bacteria) MOT = same with amoebiasis IP = few hours to 5 days IMMUNITY Active = cholera vaccine Passive = none Natural = none 89. Cholera, El Tor Dx stool exam Rice watery stool with fishy odor Washerwomans appearance Severe dehydration Chloramphenicol 90. Typhoid Fever Salmonella typhosa (bacteria) MOT = same with amoebiasis (5 Fs) IP = 1-3 weeks IMMUNITY Active = vaccine Passive = xxx Natural = lifetime immunity 91. Pathophysiology Oral ingestion Bloodstream Reticuloendothelial system (lymph node, spleen, liver) Bloodstream Gallbladder Peyers patches of SI necrosis and ulceration 92. Typhoid Fever 1st week step ladder (BLOOD) 2nd week rose spot and fastidial typhoid pyschosis (URINE & STOOL) 3rd week (complications) intestinal bleeding, perforation, peritonitis, encephalitis, 4th week (lysis) decreasing S?SX 5th week (convalescent) 93. Typhoid Fever Blood (typhi dot) 1st week after Stool and urine 2nd week after Chloramphenicol 94. Typhoid Fever Rose spot (abdominal rashes) Step ladder fever to fastidial (peak of fever) typhoid psychosis Peyers patches of small intestine May stay in the gallbladder (hiding area) 95. Hookworm (Roundworm) Necator Americanus, Ancylostoma Duodenale Skin entry (sole of the feet to blood steam then into the lungs then ascends to the pharynx where it is swallowed and attached into the intestinal mucosa and subsists on the blood of the host) Anemia, abdl cramps, abdl distention, perforation to peritinotis to septicemia 96. Hookworm (Roundworm) IP few weeks to months Dx microscopic exam (stool exam) Pyrantel Pamoate and Mebendazole Note: dont give drug without (+) stool exam members of the family must be examined and treated also. 97. Hookworm (Roundworm) Nursing Consideration FOLLOW-UP EXAMINATION OF THE STOOL 2 WEEKS AFTER THERAPY NUTRITION COUNSELING AND IRON SUPPLEMENTS FAMILY MEMBERS AND CLOSE CONTACTS SHOULD BE EXAMINED AND TREATED FOR PARASITES EDUCATE PUBLIC ABOUT DANGERS OF CONTAMINATED SOIL IMPORTANCE OF WEARING SHOES DEWORMING 98. Ascariasis (Roundworm) Ascaris Lumbricoides MOT ingestion of food contaminated by ascaris lumbricoides GIT to LUNGS and other ORGANS 99. MOT: ingestion of food contaminated by ascaris eggs larvae in large intestine penetrate wall towards lung where larvae grow and coughed up intestine larvae mature and passed out in feces 100. Ascariasis (Roundworm) Coughing, wheezing and hemoptysis IP same with hookworm Drug: same with hookworm Dx same with hookworm 101. Tapeworm Taenia Saginata (cattle) Taenia Solium (pigs) MOT fecal oral route (ingestion of food contaminated by the agent) Dx: Stool Exam S/Sx diarrhea, abdominal discomfort, anemia
102. Pinworm Enterobiasis (nocturnal animation/alive) Vermicularis Enterobius MOT fecal oral route S/sx Itchiness at the anal area (eggs of the agent causes the itchiness) Dx tape test at night time (agents release their eggs during night time) 103. Thread worm storgyloidiasis Whip worm trichoniasis voracious eating abdominal pain weight loss Flat worm - paragonimiasis 104. QUIZ 1. hookworm a. taenia s. 2. ascariasis b. vermicularis enterobius 3. pinworm c. ascaris lumbricoides 4. tapeworm d. necator americanus 105. 5. Common s/sx of worm infestation? 6. single most important nursing consideration prior to DEWORMING? 7. MOT of hookworm infestation? 8. distinct s/sx of PINWORM infestation? 9. WHIPWORM infestation s/sx? 10. LUNG FLUKE infestation? 106. Schistosomias, Snail Fever, Takayama Blood fluke Schistosoma japonicum S. hematobium S. mansoni MOT skin entry (cercaria) travel in to the blood stream where they will infiltrate the liver, from liver to intestines 107. Schistosomias, Snail Fever, Takayama Cycle: Egg-larvae (miracidium)intermediary host (oncomelania quadrasi-tiny snail)-cercaria Itchiness at the site RUQ pain (hepatomegaly) Intestine infiltration-abdl cramps, diarrhea with blood Praziquantel Dx COPT (stool exam) 108. Schistosomiasis KEY POINTS! Egg miracidium snail cercaria- human Itchiness liver intestines Praziquantel COPT PREVENTION Samar and Leyte 109. Mumps Mumps virus/filtrable virus MOT = droplets and airborne HIGHLY CONTAGIOUS IP 12-16 days IMMUNITY Active = MMR Passive = mumps Ig Natural = active =lifetime 110. Mumps Unilateral or bilateral parotitis Ice collar Stimulating foods cause severe pain Bilateral orchitis and oophoritis Active spermatogenesis Sterility Steroids Supporter 111. Respiratory System 112. Diphtheria Corynebacterium diphtheriae Klebsloefflers bacillus (bacteria) MOT = droplets and airborne HIGHLY CONTAGIOUS IP 2-5 days IMMUNITY Active = DPT Passive = DAT Natural = xxx 113. Diphtheria Dx = throat swab, MOLONEY, SCHICK Pseudomembrane, Bullneck Penicillin or erythromycin Resp Acidosis with hypoxemia Cx: myocarditis, septicemia 114. Diphtheria Nursing Considerations: OBSERVE CNS, CARDIAC AND KIDNEY COMPLICATIONS PSEUDOMEMBRANOUS MAY LEAD TO RESP. OBSTRUCTION ISOLATION UNTIL 2 NEGATIVE CULTURE AT 24 HOUR INTERVAL F&E RESUSCITATION PARENTS OR SIBLINGS WHO HAVE NEVER IMMUNIZED SHOULD RECEIVE A DOSE OF DIPH. ANTITOXIN ATTENTION TO NASOPHARYNGEAL DISCHARGE ANTIBIOTICS-PENICILLIN, ERYTHROMYCIN IF ALLERGIC TO PENICILLIN 115. S/sx: sore throat, fever, Bull-neck (Pseudomembrane- gray exudate, foul breath, massive swelling of tonsils and uvula, thick speech, cervical lymphadenopathy, swelling of submandibular and anterior neck), obstruction of respiratory tract Dx: Schick test - susceptibility to diphtheria toxin Moloney sensitivity to diphtheria toxoid Throat swab (K tellurite and Loefflers coagulated
blood serum) Mgmt: Diphtheria antitoxin (Skin test), Penicillin,erythromycin, rifampicin, clindamycin 116. Diphtheria KEY POINTS! Highly contagious Pseudomembrane and bullneck Immunization best intervention PREVENTION Obstruction and myocarditis Isolation technique 117. Whooping Cough, Pertussis Bordetella pertussis (bacteria) B. parapertussis B. bronchiseptica Hemophilus bacillus MOT = droplets and airborne HIGHLY CONTAGIOUS IP 3-21 days IMMUNITY Active = DPT Passive = xxx Natural = xxx 118. Whooping Cough, Pertussis Manifestations: CATARRHAL (HIGHLY CONTAGIOUS) 1-2 WEEKS, CORYZA, SNEEZING, DRY COUGH, FEVER, ANOREXIA PAROXYSMAL 4-6 WEEKS, SEVERE VIOLENT COUGHING ATTACKS IN CLUSTERS, THAT ENDS IN WHOOP (NOISY SPASM OF INSPIRATION) RESULTING TO CYANOSIS, VOMITING, EXHAUSTION. 119. Whooping Cough, Pertussis Ferrous iodide to liquefy thicky secretions Erythromycin or Ampicillin Bordet gengao (agar for culture) Catarrhal stage (highly contagious) Clusters of cough that ends with a whoop Prostration 120. PERTUSSIS key points! Highly contagious Thick secretions Cluster of cough Extreme exhaustion HYPOXIA PREVENTION is still the BEST intervention IMMUNIZATION 121. PTB, Kochs Pulmonary Mycobacterium tubercle Tubercle bacillus (bacteria) MOT: Airborne/droplets INCUBATION-DEPENDS ON HOST RESISTANCE RISK FACTORS: DECREASED BODY RESISTANCE MALNUTRITION, POVERTY, OVERCROWDING, STEROID THERAPY, CHEMOTHERAPY 122. PTB Pathogenesis: Transmission into the lungs Immune response macrophage (bacilli) creating a lesion Tubercle formation scar or spot Dissemination EPTB 123. 124. 125. 126. PTB, Kochs Pulmonary Manifestation: EARLY WEIGHT LOSS, LISTLESSNESS, VAGUE CHEST PAIN, PLEURISY, ANOREXIA, FEVER, NIGHT SWEATS LATE PULMONARY HEMORRHAGE, EXPECTORATION OF PURULENT SPUTUM, DYSPNEA, HEMOPTYSIS (CAVITARY SPREAD) 127. PTB Dx: PPD-exposure 0-4 mm (negative) 5 mm variable > 10 mm (positive) Chest xray-cavitary lesion Sputum-confirmatory 128. PTB MDT r-orange urine i-neuritis and hepatitis p-hyperuricemia eimpairment of vision s-8th cranial nerve damage 129. PTB CGFNS and NCLEX Usual Dose RIE 9 months to 12 months 2-4 weeks non infectious Drug Resistant Tuberculosis RIE+ (2 nd line drug) STREPTOMYCIN PYRAZINAMIDE CAPREOMYCIN PARAAMINOSALICYLIC ACID CYCLOSERINE 130. PTB 2 weeks after medications non communicable 3 successive negative sputum-non communicable rifampicin-prophylactic
131. PTB category I (new PTB (+) sputum) category II (relapsed) category III (PTB case (-) sputum) short course 6-9 months long course 9-12 months DOTS- direct observe treatment short course Case finding Home meds (members of the family) Referrals Follow-up 132. TREATMENT: CATEGORY 1 NEW PTB, (+) SPUTUM GIVE RIPE 2 MONTHS, MAINTENANCE OF RI 4 MONTHS CATEGORY 2 PREVIOUSLY TREATED WITH RELAPSES GIVE RIPES 1ST 2 MONTHS, REPS 1 MONTH, MAINTENANCE RIE 5 MONTHS CATEGORY 3 NEW PTB (-) SPUTUM FOR 3X GIVE RIP 2 MONTHS, MAINTENACE RI 2 MONTHS 133. Pneumonia Typical Community Acquired Streptococcus pneumoniae Hospital Acquired Staphylococcus aureus, Pseudomonas aeruginosa Elderly Hemophilus influenzae type B 134. Pneumonia Atypical Pneumocystis carinii (fungal) Aspergillosis (fungal) Azole, SARS 135. Pneumonia s/sx chest pain, fever with chills, Dx: C&S and XRAY Productive cough pneumococcal purulent, rusty sputum staphylococcal yellow, blood streaked klebsiella species red, gelatinous sputum mycoplasmal non productive, mucoid sputum ABG Pulse Oximetry 136. Pneumonia CARI-health teachings Watchout for complications Respiratory distress In 24 hours death will occur RESPIRATORY SUPPORT! 137. Pneumonia Cx: pleural effusion Empyema consolidation Diminished Lung Sound: egophony CHANGE IN VOICE bronchophony CLARITY OF VOICE whispered pectoriloquy AUSCULTATE 138. Severe Acute Respiratory Syndrome Coronavirus Severe acute respiratory syndrome IP: 2-7 days MOT: respiratory droplet/person to person contact Risk Factors: History of recent travel to China Hong Kong Taiwan Close contact w/ ill persons with a hx of recent travel to such areas Health workers 139. SARS Dx: sputum C&S CLINICAL MANIFESTATIONS: FEVER-38 C AND ABOVE CONTINUOUS FOR 7-10 DAYS CHILLS HEADACHE, GENERAL FEELING OF DISCOMFORT, BODY ACHES, DRY PRODUCTIVE COUGH WITH HYPOXEMIA (RESP. ACIDOSIS) DYSPNEA RELATED TO LOSS OF AERATING SURFACE 140. SARS NURSING CONSIDERATIONS: NO SPECIFIC TREATMENT ANTIVIRAL AGENT-OSELTAMIVIR OR RIBAVIRIN CLOSE SUPERVISION/OBSERVATION PROPHYLACTIC ANTIBIOTIC AVOID INFECTED AREAS IDENTIFIED BY WHO (HONGKONG, GUANDONG, SHANXI, CHINA, HANOI, VIETNAM, TORONTO, CANADA, SINGAPORE) 141. SARS NURSING CONSIDERATIONS: SEEK IMMEDIATE MEDICAL ATTENTION IF YOU SUSPECT SARS WEAR FACE MASK N95, BRA MASK (HONGKONG), DONT GO TO WORK OR SCHOOL OBSERVE PERSONAL HYGIENE HANDWASHING (5 MINUTES) BUILD UP BODY RESISTANCE (PROPER DIET) DIET (HIGH IN CHON, CHO, VIT C, D , E , A, MINERAL ZINC (INCREASE BODY RESISTANCE) 142. BLOOD BORNE DISEASES 143. Dengue Fever, H-Fever, Dandy Fever, Breakbone Disease Acute Febrile Disease CAUSATIVE AGENT-FILTRABLE VIRUS DENGUE VIRUS TYPE
1,2,3,4, CHIKUNGUNYA VIRUS MOT (Mode of Transmission) bite from: Aedes aegypti Aedes albopictus Culex fatigans IP (Incubation Period) 1 week 144. Dengue Fever, H-Fever, Dandy Fever, Breakbone Disease Hyperpyrexia without focal of infection TRIAD: fever, rashes and muscle pain Bleeding to hypovolemic shock ASA (Aspirin) is contraindicated Watchout for bleeding PLATELET is being attack 145. Dengue Fever, H-Fever, Dandy Fever, Breakbone Disease Dx: ACUTE FEBRILE ILLNESS WITH NO IDENTIFIABLE FOCUS OF INFECTION Internal and external sign of bleeding Torniquet Test or Rumpel Lead Test Platelet count PT (Prothrombin Time) APTT (Activated Partial Thromboplastin Time) Bleeding time Coagulation time 146. TRIAD (FEVER, RASH, SEVERE HEADACHE/BACKACHE/MYALGIA) 1ST STAGE, FIRST 4 DAYS HIGH FEVER, ABDOMINAL PAIN, HEADACHE, FLUSHING, VOMITING, EPISTAXIS 2ND STAGE, 4-7 DAYS TOXIC OR HEMORRHAGIC STAGE LOWERING OF BODY TEMP., SEVERE ABDOMINAL PAIN, VOMITING, GIT BLEEDING-HEMATEMESIS, MELENA, NARROW BP, SHOCK 3RD STAGE, 7-10 DAYS CONVALESCENT OR RECOVERY STAGE SIGN OF PLASMA LEAKAGE PLEURAL EFFUSION, ASCITES, HYPOPROTEINEMIA HERMANS SIGN 147. GRADE 1 (+) TORNIQUET TEST, NO BLEEDING GRADE 2 SPONTANEOUS BLEEDING, (+) GRADE 1 GRADE 3 CIRCULATORY FAILURE,,DECREASED BP, RAPID WEAK PULSE, NARROWING OF PULSE PRESSURE, COLD CLAMMY SKIN, RESTLESSNESS GRADE 4 PROFOUND SHOCK, UNDETECTABLE BP AND PULSE 148. Dengue Fever, H-Fever, Dandy Fever, Breakbone Disease Nursing Considerations ANY CONDITION ASSOCIATED WITH BLEEDING IS ENOUGH CAUSE FOR ALARM FOR FEVER DONT GIVE ASA RAPID REPLACEMENTS OF FLUIDS IS THE MOST IMPORTANT TREATMENT GIVE ORESOL/HYDRITE VIT C TO PROMOTE CAPILLARY INTEGRITY 149. Dengue Fever, H-Fever, Dandy Fever, Breakbone Disease Nursing Considerations BLOOD TRANSFUSION IV CRYSTALLOIDS (PLAIN LRS, PLAIN 0.9 NSS) DEXTRAN (COLLOIDS) PLATELETS FRESH FROZEN PLASMA CRYOPRECIPITATE WHOLE BLOOD NO KNOWN IMMUNIZATION (VACCINE CURRENTLY UNDERWAY) 150. Dengue KEY POINTS Day biting aedes aegypti, stagnant Fever with no focal of infection Bleeding is imminent when fever subsides Fluid replacement BT platelets 151. Malaria, King of Tropical Disease Protozoan plasmodium plasmodium ovale - dormant (liver) plasmodium vivax - benign plasmodium malariae - mild but resistant plasmodium falciparum - malignant (cerebral malaria) P. VIVAX AND OVALE MAY HAVE RECCURENCE OF SYMPTOMS tertian-febrile paroxysm q24H-48H quartan-febrile paroxysm q48H-72H 152. Malaria, King of Tropical Disease MOT Bite from infected anopheles mosquito or minimus flavire (night biting) Blood Transfusion Sexual cycle
sporogony (mosquito) gametes is the infective stage Asexual cycle schizogony (human) IP (Incubation Period) 5-6 days 153. 154. 155. Malaria, King of Tropical Disease Nursing Considerations Dx: blood extraction (extract blood at the height of fever) Fever, chills, profuse sweatingconvulsion Anemia and fluid and electrolytes imbalance, hepatomegaly, splenomegaly, rigor, headache and diarrhea. Chloroquine and Primaquine drug of choice Chloroquine for pregnant women For resistant plasmodium-use chemo drug RBC is being attack 156. Malaria, King of Tropical Disease Nursing Considerations IV FLUIDS AND ELECTROLYTES Blackwater Fever hemolysis and hemoglobinuria Sickle Cell Trait provides natural resistance DECREASE FLUIDS IN CEREBRAL EDEMA ASSISTED VENTILATION IN PULMONARY EDEMA DIALYSIS IN RENAL FAILURE BT IN ANEMIA 157. Malaria, King of Tropical Disease TRAVELERS TO MALARIA ENDEMIC area SHOULD FOLLOW PREVENTIVE MEASURES(CHEMOPROPHYLAXIS CHLOROQUINE MAY BE TAKEN 1 WEEK BEFORE ENTERING ENDEMIC AREA) SOAKING OF MOSQUITO NET IN AN INSECTICIDE SOLUTION BIO PONDS FOR FISH ON STREAM CLEARING (TO EXPOSE THE BREEDING STREAM TO SUNLIGHT) VECTORS PEAK BITING AT NIGHT 9PM-3AM PLANTING OF NEEM TREE (REPELLENT EFFECT) ZOOPROPHYLAXIS (DEVIATE MOSQUITO BITES FROM MAN TO ANIMALS) INFECTED MOTHER CAN STILL CONTINUE BREAST FEEDING 158. MALARIA key points Night biting anopheles, running water Falciparum fatal Ovale and vivax exacerbate Sporogony sexual mosquito Schizogony asexual human Chloroquine Seizure, fluid and elec loss Rbc and liver 159. Filariasis, Elephantiasis, Human Lymphatic Filariasis CAUSATIVE AGENT-NEMATODE PARASITE MICROFILARIAE OR FILARIAL WORMS WUCHERERIA BRONCOFTI BRUGIA MALAYI BRUGIA TIMORI MOT Bite from aedes poecilius (night biting) Invade the lymph vessel, obstructing the lymphatic channel-leads to edema and may infiltrate the reproductive organs. IP 8-16 months 160. CLINICAL MANIFESTATIONS: ASYMPTOMATIC STAGE (+) MICROFILARIAE IN THE BLOOD NO CLINICAL S/SX ACUTE STAGE LYMPHADENITIS (LYMPH NODES) LYMPHANGITIS (LYMPH VESSELS) GENETALIA-FUNICULITIS, EPIDYDIMITIS, ORCHITIS CHRONIC STAGE HYDROCOELE LYMPHEDEMA (UPPER AND LOWER EXTREMITIES) ELEPHANTIASIS 161. Filariasis, Elephantiasis, Human Lymphatic Filariasis 162. Filariasis, Elephantiasis, Human Lymphatic Filariasis INCIDENCEREGION 5,8,11 AND CARAGA, MARINDUQUE, SARANGGANI Drug: Diethyl Carbamazine Citrate or Hetrazan 6mg/KgBW one dose every year Dx: NBE nocturnal blood exam (night) ICT immunochromatographic test (day)
163. Nursing Considerations MASS TREATMENT-DOSE IS 6mg/KBW, SINGLE DOSE PER YEAR. ENVIRONMENTAL SANITATION PERSONAL HYGIENE MOSQUITO NETS LONG SLEEVES, LONG PANTS AND SOCKS INSECT REPELLENT SCREENING OF HOUSES HEALTH EDUCATION 164. Filariasis KEY POINTS Night biting aedes poecilius, plants Chronic, lymphedema HETRAZAN ICT and NBE Lymphatic vessel obstruction 165. Leptospirosis, Weils Disease (Zoonotic) Spirochete-leptospira interrogans IP 5-6 days MOT (Mode of Transmission) Skin penetration = flood INGESTION OF CONTAMINATED FOOD SKIN, MUCUS MEMBRANE, ABRADED SKIN, CONJUNCTIVA INHALATION AFTER PENETRATION LEPTOSPIRES ENTER THE BLOOD STREAM AND ARE CARRIED TO ALL PARTS OF THE BODY INCLUDING Liver, kidneys and CSF 166. Leptospirosis, Weils Disease (Zoonotic) Dx: CULTURE OF MICROORGANISMS BLOOD AND CSF EXAMINATION (FIRST WEEK) URINE EXAM- AFTER 10 DAYS MICROSCOPIC AGGLUTINATION TEST (MAT) A RISE IN ANTIBODY TITER 167. CLINICAL MANIFESTATIONS EARLY = fever and headache LEPTOSPIREMIC PHASE = vasculitis HEPATITIS, JAUNDICE, SKIN HEMORRHAGE, FEVER, CHILLS, RENAL FAILURE, MENINGITIS WITH MENTAL STATUS CHANGE, MUSCULAR PAIN, NAUSEA AND VOMITING, COUGH AND CHEST PAIN IMMUNE PHASE APPEARANCE OF CIRCULATING IgM 168. NURSING CONSIDERATIONS PENICILLIN OR DOXYCYCLINE (IMMEDIATELY) ERYTHROMYCIN IF ALLERGIC TO PENICILLIN FLUID AND ELECTROLYTE BALANCE ENSURE ADEQUATE RENAL PERFUSION TO PREVENT ARF IF AZOTEMIA IS SEVERE OR PROLONGED (CONSIDER DIALYSIS) DISEASE IS USUALLY SHORT LIVED AND MILD BUT SEVERE INFECTION CAN DAMAGE KIDNEYS, LIVER, CNS AND RESPIRATORY SYSTEM MOST SERIOUS FORM IS CALLED WEILS DISEASE PRIMARILY A DISEASE OF DOMESTICATED AND WILD ANIMALS 169. PREVENTION AND CONTROL AVOIDANCE OF EXPOSURE TO URINE AND TISSUES FROM INFECTED ANIMALS (FLOOD) RODENT CONTROL VACCINATION OF ANIMALS HYGIENIC CONDITIONS IN SLAUGHTERHOUSES, FARM YARD BUILDINGS AND BATHING POOLS USE OF PROTECTIVE CLOTHING AND BOOTS CHEMOPROPHYLAXIS (DOXYCYCLINE 200 mg PO ONCE A WEEK SUPPORTIVE MANAGEMENT ALL PATIENT SUSPECTED TO HAVE LEPTO, MILD OR SEVERE SHOULD BE ADMITTED 170. LEPTOSPIROSIS key points Spirochette, rat, urine and feces Skin penetration, ingestion Fever and headache Liver, kidneys and CSF Doxycycline 171. ERUPTIVE FEVER 172. Measles, Rubeola, 7 Day Fever, Hard Red Measle Paramyxo virus MOT = droplets and airborne PC 4 days before and 5 days after rash HIGHLY CONTAGIOUS IP 7-14 days IMMUNITY Active = measles vaccine, MMR Passive = measles Ig Natural = lifetime
173. Measles, Rubeola, 7 Day Fever, Hard Red Measle Rashes: Maculopapular Cephalocaudal With desquamation Pruritus 174. Measles, Rubeola, 7 Day Fever, Hard Red Measle Rashes: maculopapaular, cephalocaudal (hairline and behind the ears to trunk and limbs), confluent, desquamation, pruritus 175. PS kopliks spot Characteristic: stimsons, photophobia (typical complaint) Fever: high fever CX pneumonia, meningitis 176. German Measles, Rubella, Rotheln Disease, 3 Day Measles RNA rubella virus MOT = droplets and airborne PC 5 days before and 5 days after rash HIGHLY CONTAGIOUS IP = 10-21 days IMMUNITY Active = MMR Passive = rubella Ig Natural = lifetime 177. German Measles, Rubella, Rotheln Disease, 3 Day Measles Rashes: Maculopapular Diffuse No desquamation 178. German Measles, Rubella, Rotheln Disease, 3 Day Measles Rashes: Maculopapular, Diffuse/not confluent, No desquamation, spreads from the face downwards 179. PS forschheimers Characteristic: cervical lymphadenopathy Fever: low grade fever CX rare CX to pregnant women: 1st tri-congenital anomalies 2nd triabortion 3rd tri-pre mature delivery 180. Chicken Pox, Varicella Herpes Zoster Virus Varicella Zoster Virus MOT = droplets and airborne PC one day before rash and 6 days after first crop of vesicles HIGHLY CONTAGIOUS IP 14-21 days IMMUNITY Active = varicella vaccine Passive = xxx Natural = lifetime 181. 182. Chicken Pox, Varicella Rashes: Maculopapulovesicular (covered areas), Centrifugal, starts on face and trunk and spreads to entire body Leaves a pitted scar (pockmark) 183. Chicken Pox, Varicella Dx = Tzanck smear (scraping of ulcer for staining) Rashes: Maculopapulovesicular (covered areas) Centrifugal Leaves a pitted scar (pockmark) CX furunculosis, erysipelas, meningoencephalitis Dormant: remain at the dorsal root ganglion and may recur as shingles 184. Small Pox, Variola Pox virus MOT = droplets and airborne PC until all crust disappear HIGHLY CONTAGIOUS IP 1-3 weeks ERADICATED BIOLOGIC WEAPON 185. 186. Small Pox, Variola Rashes Maculopapulovesiculopustular Centripetal CX same with chicken pox Differential Dx Pauls test - instilling of vesicular fluid of small pox into the cornea if keratitis develops its small pox 187. CONTACT 188. Pediculosis Blood sucking lice Pediculus humanus p. capitis-scalp p. palpebrarum-eyelids and eyelashes p. pubis-pubic hair p. corporis-body Drugs: Lindane (Kwell) topical Permethrin (Nix) topical CX impetigo to AGN, RHD, SLE MOT skin contact 189. 190.
191. Scabies Sarcoptes scabie Pruritus (excreta of mites) Mites come-out from burrows to mate at night Drugs: Permethrin (Nix) cream Sulfur soap Linens: wash with hot water MOT skin contact 192. 193. Conjunctivitis Children Viral-hygiene and rest Bacterial-yellow, green or white pus, photophobia-antibiotic eyedrops or ointment Chlamydial cough, history of maternal infection-antibiotic Herpetic-pain, photophobia, skin lesionsantiviral agents Allergic-itching, watery discharge-antihistamine S/Sx From mild pruritus to severe drainage, burning, hyperemia and chemosis (edema) Pink eyeinfectious conjunctivitis MOT direct contact with eye secretions 194. STD 195. Gonorrhea (bacteria) Neisseria gonorrheae (gram positive) IP 3 -7 days Asymptomatic in women Mucopurulent discharge Painful urination DX: gram stain of cervical secretions Drugs: single dose only Ceftriaxone (Rocephin) 125 mg IM Ofloxacin (Floxin) 400 mg orally CX: PID, ectopic pregnancy and infertility Ophthalmia neonatorum and sepsis (infant) vaginal birth 196. 197. Syphilis (bacteria) Treponema pallidum (spirochete) IP 10-90 days Painless, clean chancre DX: Non specific VDRL Confirmed by-antitreponemal antibody tests Dark-field examination of lesion 198. Primary painless chancre Secondary generalized rash Tertiary - gumma 199. Syphilis (bacteria) Primary-chancre-most infectious Secondary-generalized macular papular rash including palms and soles (condylomata lata) Tertiaryneurosyphilis-permanent damage (insanity) (gumma) Drugs: Primary and secondary Pen G Tertiary IV Pen G 200. Chlamydia (bacteria) Chlamydia trachomatis IP 2-10 days Maybe asymptomatic Gray white discharge Burning and itchiness at the urethral opening DX: Antigen detection test on cervical smear Urinalysis 201. Chlamydia (bacteria) 202. Chlamydia (bacteria) Drugs: Azithromycin (Zithromax) 1 g orally one dose Erythromycin and Ofloxacin CX: PID Ectopic pregnancy Fetus transmittal (vaginal birth) 203. Herpes Genitalis (virus) HSV 2 Painful sexual intercourse Painful lesion (cervix, vagina, perineum, glans penis) DX: Viral culture Pap smear (shows cellular changes) Tzanck smear (scraping of ulcer for staining) Drugs: Anti viralacyclovir (zovirax) CX: Meningitis Neonatal infection (vaginal birth) 204. Genital Warts, Condyloma Acuminatum (virus) HPV type 6 & 11, papilloma virus Single or multiple soft, fleshy painless growth of the vulva, vagina, cervix, urethra, or anal area Vaginal bleeding, discharge, odor and dyspareunia DX: Pap smear-shows cellular changes (koilocytosis) Acetic acid swabbing (will whiten lesion) Management: Laser treatment is more effective CX: Neoplasia Neonatal laryngeal papillomatosis (vaginal birth) 205. Genital Warts, Condyloma Acuminatum (virus) Mgmt: Laser treatment is more effective CX: Neoplasia Neonatal laryngeal papillomatosis (vaginal birth)
206. Candidiasis, Moniliasis Yeast or fungus Cheesy white discharge Extreme itchiness DX: KOH (wet smear indicate positive result) Drugs: Monistat Diflucan CX: Oral thrush to baby (vaginal birth) 207. Trichomoniasis Parasite Trichomona vaginalis Yellow gray frothy vaginal discharge Foul smelling Drugs: Metronidazole (Flagyl) CX: PROM 208. Prevention A abstinence B be faithful C condom D do it yourself One stick one hole Both partners must be treated 209. TORCHS T toxoplasmosis O others Papilloma virus - STD Gonorrhea - STD Varicella zoster chicken pox Hepa B HIV Measles Mumps R rubella C cytomegalovirus hemolytic anemia, hydro/microcephalus H herpes genitalis STD S syphilis - STD 210. HIV 211. HIV and AIDS Retrovirus (HIV1 & HIV2) Attacks and kills CD4+ lymphocytes (T-helper) Capable of replicating the lymphocytes undetected by the immune system Immunity declines and opportunistic microbes sets in 212. 213. 214. HIGH RISK GROUP Homosexual or bisexual Intravenous drug users BT recipients before 1985 Sexual contact with HIV+ Babies of mothers who are HIV+ 215. MOT Sexual intercourse (oral, vaginal and anal) Exposure to contaminated blood, semen, breast milk and other body fluids placenta 216. 217. HIV TEST Elisa Western Blot Rapid hiv test Suds hiv-1 Results are obtained in less than 10 minutes Color indicator similar to pregnancy test Positive result needs a confirmatory test 218. How to Diagnose HIV+ 2 consecutive positive ELISA and 1 positive Western Blot Test AIDS+ HIV+ CD4+ count below 500/ml Exhibits one or more of the ff: (next slide) Full blown AIDS CD4 is less than 200/ml 219. Exhibits one or more of the ff: Extreme fatigue Intermittent fever Night sweats Chills Lymphadenopathy Enlarged spleen Anorexia Weight loss Severe diarrhea Apathy and depression PTB Kaposis sarcoma Pneumocystis carinii AIDS dementia 220. 221. HIV CLASSIFICATION CATEGORY 1 CD4+ 500 OR MORE CATEGORY 2 CD4+ 200-499 CATEGORY 3 CD4+ LESS THAN 200 222. Management Prevention of spread (safe sex) Universal precautions Health Education Symptomatic intervention No known cure Prevent CD4 reduction 223. DRUGS 1. Nucleoside Reverse Transcriptase Inhibitors NRTIs INTERFERES WITH DNA CHAIN Zidovudine (AZT) SE NEUROPATHY AND RASH 224. DRUGS 2. Non-nucleoside Reverse Transcriptase Inhibitors NNRTIs BINDS TO REVERSE TRANSCRIPTASE AND BLOCKS RNA AND DNA REPLICATION Ritonavir (Norvir) SE RASH, HEPATOTOXICITY, BONE MARROW DEPRESSION
225. DRUGS 3. Protease Inhibitors PI BLOCK VIRUS ABILITY TO BREAK DOWN LARGER PROTEIN MOLECULES Indinavir (Crixivan) SE HEPATOTOXICITY, NV, ABDOMINAL PAIN, RENAL CALCULI 226. Hepatitis 227. 228. Types of Hepatitis Hepa A fecal oral route Hepa B body fluids Hepa C non A non B, BT, body fluids Hepa D hypodermic, body fluids Hepa E fecal oral route, fatal and common among pregnant women Hepa G body fluids (HIV) 229. Hepatitis A Hepa A virus Infectious hepa Fecal oral route Short incubation (3-5 weeks) Poor sanitation Worldwide distribution Spread from person-person Food handlers, contaminated water Mortality 1%, with full recovery Enteric precautions Active Immunity (Havrix) Passive Immunity (HAIg) (+) ANTI HAV INFECTED (+) Igm ANTI HAV RECENT INFECTION (ANTIBODY) 230. Hepatitis B Hepa B virus Serum hepa Blood recipients, hemodialysis, IV drug users, sexually active homosexual, tattoing and health care workers (high risk) Blood and other body fluids route Long incubation (2-5 months) Worldwide distribution Main cause of liver cirrhosis and liver cancer (+) HBsAg indicates acute, chronic and carrier Active Immunity (hevac-B) Passive Immunity (HBIg) 85% full recovery, 15% lifetime carrier 231. DX Elevated AST or SGPT (specific) and ALT or SGOT Increased IgM during acute phase HBsAg (+) or REACTIVE = INFECTED maybe acute, chronic or carrier HBeAg (+) = highly infectious HBcAg found only in the liver cells Anti-HBc (+) = acute infection Anti-HBe (+) = reduced infectiousness AntiHBs (+) = with antibodies (FROM vaccine or disease) Blood Chem. Analysis (to monitor progression) Liver biopsy (to detect progression to CA) 232. Manifestations: Stage I pre-icteric for 1-21 days Anorexia, nausea and vomiting, LBM, weight loss RUQ pain, fatty food intolerance, fever, chills and headache Satge II icteric for 2-6 weeks Jaundice, pruritus, weight gain, ascites, dark-tea colored urine (urobilirubin) ADEK deficiency Stage III pre coma NH3 level increases with decreasing LOC Flapping tremors or asterixis Stage IV recovery 233. jaundice 234. Manifestations CHO fatigue CHON toxicity (latent phase) Fats bile, fat intolerance, ADEK Bilirubin jaundice, kernicterus (children) Deamination NH3 increases Synthesis CHON immunocompetent Cirrhosis and Cancer complications 235. Management: Rest Diet: - high CHON 75-100 g/day - high CHO energy low fat - high calorie 2,500-3,000 cal/day - increase vit A, E if there is steatorrhea Bile sequestrants to reduce pruritus Cholestryamine (Questran) Avoid hepatotoxic drugs Acetaminophen, Sedatives, ASA Give Antiviral and Interferon 236. Other diseases 237. Lyme disease Named for the Connecticut town, 1975 Appears in summer or early fall Spirochete, Borrelia burgdorferi Carried by deer ticks Pahogenesis: Tick injects spirochete-laden saliva into the blood stream or deposits fecal matter
on the skin disseminate to other skin sites or travel into the blood stream and lymphatic system 238. s/sx: may take years to fully develop *Skin lesion erythema chronicum migrans Early localized (Stage 1) = lesion with bright red outer rim with white center, itchy, may sting or burn; fatigue, headache, chills, fever, sore throat and muscle joint pain Early disseminated (Stage 2) = meningitis, extreme neck flexion and cranial nerve palsy, cardiac symptoms, brief attacks of arthritis Late (Stage 3) = Chronic arthritis, Behavioral changes, depression and psychosis Cardiac, neurologic, arthritis (complications) 239. Lyme disease Dx: biopsy, antibody titer, ELISA, Western Blot Mgmt: symptomatic 14-28 day oral tetracycline or doxycycline Children oral Penicillin Late stage: IV or IM antibiotics Vaccine Immulyme, Lymerix 240. Toxoplasmosis ZOONOTIC Toxoplasma gondii, parasite Affects birds, mammals ie cats Infected person may carry the organism for life (reactivation is possible) Pathogenesis: ingestion of cyst from uncooked meat / fecal oral route from infected cats (feces) Quickly multiply in the GIT Distributed to CNS, lymphatic tissue, skeletal muscle, myocardium, retina and placenta 241. S/sx: Toxoplasmosis Malaise, fever, myalgia, headache, fatigue, sore throat, lymphadenopathy Fulminant = vomiting, cough and dyspnea, hyperpyrexia, delirium and seizures, encephalopathy, meningitis Infants = hydrocephalus and microcephalus, seizure, jaundice later strabismus, blindness, epilepsy, mental retardation 242. Toxoplasmosis Dx: serology, CT scan Mgmt: 4-6 weeks of sulfonamide and pyrimethamine (take folic acid to counteract drugs adverse effects) 243. TORCHS T toxoplasmosis O others Papilloma virus - STD Gonorrhea - STD Varicella zoster chicken pox Hepa B HIV Measles Mumps R rubella C cytomegalovirus hemolytic anemia, hydro/microcephalus H herpes genitalis STD S syphilis - STD 244. Ebola ZOONOTIC Filoviruses, 1960 Unknown reservoir Viral replication takes place in almost all organs 90% mortality, recovery is often prolonged BIOLOGICAL WEAPON IP: 3-9 days MOT: direct contact w/ blood, vomitus, urine, stool, semen probably aerosol transfer during later stages 245. Ebola S/sx: frontal and temporal headache, malaise, myalgia, nausea, vomiting, fever, conjunctivitis, watery diarrhea (3 rd day), lethargy, nonpruritic maculpapular rash, desaquammation, hemorrhagic manifestations (5 th day) Dx: history Symptomatic intervention Report suspected EBOLA case Health workers = advised to wear cap, goggles, mask, gown, gloves and shoe covers 246. Bird Flu ZOONOTIC Avian influenza, virus Occur naturally among birds (intestines) but some types very contagious among birds Influenza A (H5N1) virus deadly to birds and has caused human illness and death in Asia Person to person transmission rare 247. Bird Flu MOT: saliva, nasal secretions, and feces direct contact with infected waterfowl or other infected poultry contact with surfaces (such as dirt or cages) or materials (such as water or feed) contaminated with virus
248. Bird Flu S/sx: Influenza-like symptoms Fever, Cough, sore throat, muscle aches, eye infections, Pneumonia Mgmt: * resistant to amantadine and rimantadine comon influenza drugs * oseltamavir and zanamavir - under study 249. Foot and Mouth Disease ZOONOTIC Aphthovirus Hosts - cattle, buffaloes, sheep, goats, swine IP: 2-4 days MOT: contact w/ infected animals Ingestion of unprocessed milk or dairy products from infected animals Humans act as transmitter to animals Harbor virus in respiratory tract for 1-2 days Contaminated boots, clothing, vehicles Spread to susceptible animals 250. Foot and Mouth Disease s/sx: Very rarely develop mild clinical signs malaise, fever, vomiting, red ulcerative lesions of oral tissues, vesicular lesions skin Dx: Virus isolation or antibody identification required for diagnosis Mgmt: supportive care 251. Infectious Mononucleosis 3 hallmarks fever sore throat swollen cervical lymph nodes (+) heterophil antibodies No major complications Self limiting Kissing Disease Incubation period is 10-50 days 252. EBV Caused by EBV epstein-barr virus Or cytomegalovirus Lodges in the salivary glands Spread via oropharyngeal route Kissing (intimate) Contagious before symptoms start until fever subsides 253. EBV Virus invades the B cells of lymphoid tissue As the B cells die virus is released in the blood Causing fever and other symptoms Antiviral antibodies in the blood fights the virus They disappear in the blood and lodges in to the salivary glands 254. EBV Diagnostic WBC count abnormally high (+) heterophil antibodies Indirect immunoflourescent (+) EBV (specific) 255. EBV Management Symptomatic ASA Steroids 256. Gas Gangrene Clostridium perfringens welchii novyi Deep wound (bronzed or blackened wound) Necrosis of muscle tissue Pain and Anemia 257. Gas Gangrene CS Incision and Drainage Debridement Hyperbaric oxygenation Amputation SEPSIS 258. Anthrax (Zoonotic) Bacillus anthracis (gram negative) Cattle, sheep, goat and pig Biological weapons 259. Anthrax Inhalation- URTI-fever-3-5 days-lower infection (alveoli)-metabolic acidosis-hypoxia GIT- ingestion of contaminated carcasses-severe gastroenteritisbloody stools-perforation-peritoniitis-septicemia Skin- most commondirect/indirect-itchiness-papule-vesicle-depressed black eschars-painlesssepticemia-death 260. Lyme Disease Named for the Connecticut town, 1975 Appears in summer or early fall Skin lesion erythema chronicum migrans Cardiac, neurologic, arthritis (complications) 261. Lyme Disease Caused by spirochete borrelia burgdorferi Carried by deer ticks Tick injects spirochete-laden saliva into the blood stream or deposits fecal matter on the skin Spirochetes disseminate to other skin sites or travel into the blood stream and lymphatic system 262. Lyme Disease Signs and symptoms may take years to fully develop Stage 1 = site, red lesion, it may itch, sting or burn lesion has white center, bright red
outer rim rash is accompanied with fatigue, headache, chills, fever, sore throat and muscle joint pain severe headache may suugest meningeal irritation 263. Lyme Disease Stage 2 = meningitis and cranial nerve palsy also cardiac symptoms may appear extreme neck flexion Stage 3 = Chronic arthritis Note: may change the behavior, depression and psychosis 264. Lyme Disease Diagnostic antibody titer ELISA Western Blot IgM AST WBC ESR 265. Lyme Disease Management 14-28 day oral tetracycline or doxycycline Children oral Penicillin Late stage: IV or IM antibiotics symptomatic 266. Toxoplasmosis (Zoonotic) Toxoplasma gondii Affecting birds and mammals Transmitted to humans by ingestion of uncooked meat and fecal oral route from infected cats (feces) Quickly multiply in the GIT Disseminate to the CNS, lymphatic tissue, skeletal muscle, myocardium, retina and placenta 267. Toxoplasmosis Malaise, fever, myalgia, headache, fatigue and sore throat Fulminant = vomiting, cough and dyspnea, hyperpyrexia, delirium and seizures Infants = hydrocephalus and microcephalus, seizure, jaundice later strabismus, blindness, epilepsy, mental retardation Infected person may carry the organism for life (reactivation is possible) 268. Toxoplasmosis Management 4-6 weeks of sulfonamide and pyrimethamine (take folic acid to counteract drugs adverse effects) 269. Ebola and Marburg Viruses (Zoonotic) Filoviruses, 1960 Biological weapons Extreme virulence Reservoir not yet confirmed Exposure to unrecognized host Insect bites Asia and Africa (animals) 270. Ebola MOT not known Diagnosis = febrile and hemorrhagic fever from Asia and Africa (travellers) Health workers = advised to wear cap, goggles, mask, gown, gloves and shoe covers 271. 272. Ebola Rapid onset of symptoms profound hemorrhage organ failure and shock 90% mortality, recovery is often prolonged No known antiviral drugs Symptomatic intervention Report suspected EBOLA case 273. Bird Flu (Zoonotic) Avian influenza Infection caused by avian (bird) influenza (flu) viruses. Occur naturally among birds Wild birds worldwide carry the viruses in their intestines, but usually do not get sick from them However, avian influenza is very contagious among birds and can make some domesticated birds, including chickens, ducks, and turkeys, very sick and kill them. 274. Bird Flu MOT = saliva, nasal secretions, and feces direct contact with infected waterfowl or other infected poultry, or through contact with surfaces (such as dirt or cages) or materials (such as water or feed) that have been contaminated with the virus. 275. Bird Flu Low and high extremes of virulence The low pathogenic form may go undetected and usually causes only mild symptoms (such as ruffled feathers and a drop in egg production) The highly pathogenic form spreads more rapidly through flocks of poultry. This form may cause disease that affects multiple internal organs and has a mortality rate that can reach 90-100% often within 48 hours.
276. Bird Flu Human infection with avian influenza viruses There are many different subtypes of type A influenza viruses. These subtypes differ because of changes in certain proteins on the surface of the influenza A virus (hemagglutinin [HA] and neuraminidase [NA] proteins). There are 16 known HA subtypes and 9 known NA subtypes of influenza A viruses. Many different combinations of HA and NA proteins are possible. Each combination represents a different subtype. All known subtypes of influenza A viruses can be found in birds. 277. Bird Flu Usually, avian influenza virus refers to influenza A viruses found chiefly in birds Infections with these viruses can occur in humans The risk from avian influenza is generally low to most people, because the viruses do not usually infect humans However, confirmed cases of human infection from several subtypes of avian influenza infection have been reported since 1997 Most cases of avian influenza infection in humans have resulted from contact with infected poultry (e.g., domesticated chicken, ducks, and turkeys) or surfaces contaminated with secretion/excretions from infected birds The spread of avian influenza viruses from one ill person to another has been reported very rarely, and transmission has not been observed to continue beyond one person. 278. Bird Flu Human influenza virus usually refers to those subtypes that spread widely among humans. There are only three known A subtypes of influenza viruses (H1N1, H1N2, and H3N2) currently circulating among humans. It is likely that some genetic parts of current human influenza A viruses came from birds originally. Influenza A viruses are constantly changing, and they might adapt over time to infect and spread among humans. 279. Bird Flu During an outbreak of avian influenza among poultry, there is a possible risk to people who have contact with infected birds or surfaces that have been contaminated with secretions or excretions from infected birds. 280. Bird Flu Influenza-like symptoms Fever Cough sore throat muscle aches eye infections Pneumonia severe respiratory diseases 281. Bird Flu Avian Influenza A (H5N1) Avian influenza A (H5N1) in Asia and Europe Influenza A (H5N1) virus also called H5N1 virus is an influenza A virus subtype that occurs mainly in birds, is highly contagious among birds, and can be deadly to them. 282. Bird Flu Outbreaks of avian influenza H5N1 occurred among poultry in eight countries in Asia (Cambodia, China, Indonesia, Japan, Laos, South Korea, Thailand, and Vietnam) during late 2003 and early 2004. At that time, more than 100 million birds in the affected countries either died from the disease or were killed in order to try to control the outbreaks. By March 2004, the outbreak was reported to be under control. Since late June 2004, however, new outbreaks of influenza H5N1 among poultry were reported by several countries in Asia (Cambodia, China [Tibet], Indonesia, Kazakhstan, Malaysia, Mongolia, Russia [Siberia], Thailand, and Vietnam). It is believed that these outbreaks are ongoing. Influenza H5N1 infection also has been reported among poultry in Turkey and Romania and among wild migratory birds in Croatia. 283. Bird Flu Human cases of influenza A (H5N1) infection have been reported in Cambodia, China, Indonesia, Thailand, and Vietnam. For the most current information about avian influenza and cumulative case numbers
284. Bird Flu Human health risks during the H5N1 outbreak H5N1 virus does not usually infect people, but more than 130 human cases have been reported by the World Health Organization since January 2004. Most of these cases have occurred as a result of people having direct or close contact with infected poultry or contaminated surfaces; however, a few cases of human-to-human spread of H5N1 have occurred. 285. Bird Flu No one can predict when a pandemic might occur. However, experts from around the world are watching the H5N1 situation in Asia and Europe very closely and are preparing for the possibility that the virus may begin to spread more easily and widely from person to person. 286. Bird Flu Treatment and vaccination for H5N1 virus in humans The H5N1 virus that has caused human illness and death in Asia is resistant to amantadine and rimantadine, two antiviral medications commonly used for influenza. Two other antiviral medications, oseltamavir and zanamavir, would probably work to treat influenza caused by H5N1 virus, but additional studies still need to be done to demonstrate their effectiveness. 287. Bird Flu Treatment and vaccination for H5N1 virus in humans There currently is no commercially available vaccine to protect humans against H5N1 virus that is being seen in Asia and Europe. However, vaccine development efforts are taking place. Research studies to test a vaccine to protect humans against H5N1 virus began in April 2005, and a series of clinical trials is under way. 288. Foot and Mouth Disease (Zoonotic) Picornaviridae, genus Aphthovirus One of the most contagious animal diseases, with important economic losses Low mortality rate in adult animals, but often high mortality in young due to myocarditis 289. Foot and Mouth Disease Hosts Bovidae (cattle, zebus, domestic buffaloes, yaks), sheep, goats, swine, all wild ruminants and suidae. Camelidae (camels, dromedaries, llamas, vicunas) have low susceptibility 290. Foot and Mouth Disease Transmission Direct or indirect contact (droplets) Animate vectors (humans, etc.) Inanimate vectors (vehicles, implements) Airborne, especially temperate zones (up to 60 km overland and 300 km by sea) 291. Foot and Mouth Disease Sources of virus Incubating and clinically affected animals Breath, saliva, faeces, and urine; milk and semen (up to 4 days before clinical signs) Meat and by-products in which pH has remained above 6.0 Carriers: particularly cattle and water buffalo; convalescent animals and exposed vaccinates (virus persists in the oropharynx for up to 30 months in cattle or longer in buffalo, 9 months in sheep). African Cape buffalo are the major maintenance host of SAT serotypes 292. Foot and Mouth Disease Occurrence FMD is endemic in parts of Asia, Africa, the Middle East and South America (sporadic outbreaks in free areas) Incubation Period 2-14 days 293. Foot and Mouth Disease PREVENTION AND CONTROL Sanitary prophylaxis Protection of free zones by border animal movement control and surveillance Slaughter of infected, recovered, and FMD-susceptible contact animals Disinfection of premises and all infected material (implements, cars,
clothes, etc.) Destruction of cadavers, litter, and susceptible animal products in the infected area Quarantine measures ( Code Chapter 2.1.1.) 294. Foot and Mouth Disease PREVENTION AND CONTROL Medical prophylaxis Inactivated virus vaccine containing an adjuvant. Immunity: 6 months after two initial vaccinations, 1-month apart, depending on the antigenic relationship between vaccine and outbreak strains 295. Your #1 NursesPortal http://1nurses.com
WHAT IS LEPTOSPIROSIS? - Leptospirosis is a disease caused by leptospira bacteria that can be transmitted to humans by contact with the urine of rats, cattle, foxes, rodents, and other wild animals.
- Leptospirosis is common in tropical regions but is also found in temperate areas, including the UK.
- There are two main types of leptospirosis in the UK:
- Weils disease - a serious and sometimes fatal infection that is transmitted by contact with the urine of infected rats;
- The Hardjo form of leptospirosis that is transmitted by cattle.
- Infection with leptospirosis is usually through contact with water, food, or soil that contains urine from infected animals. This contact can either be through ingestion or contact with the skin, especially the mucosal surfaces.
WHO IS AT RISK? - People exposed to rats, rat or cattle urine, or to foetal fluids from cattle.
- Farmers are a major risk group.
- Other at-risk groups include vets, meat inspectors, butchers, abattoir and sewer workers.
- People in contact with canals, lakes, and rivers through work or leisure activities are also at risk.
SYMPTOMS AND DIAGNOSIS - The incubation period is between two days and four weeks, and illness can last from a few days to three weeks or longer.
- Without treatment, recovery may take several months.
- Leptospirosis causes a wide range of symptoms, although some patients may be asymptomatic.
- Symptoms include:
- High fever;
- Arthralgia;
- Splenomegaly;
- Severe headache;
- Sore throat;
- Chills;
- Muscle aches;
- Vomiting;
- Jaundice;
- Red eyes;
- Abdominal pain;
- Diarrhoea;
- Mental disturbance;
- Rash.
- If untreated, it can lead to kidney damage, meningitis, liver failure, and respiratory distress. In rare cases the disease is fatal.
- Diagnosis is made by clinical suspicion and history of exposure, and is confirmed by laboratory testing of a blood or urine sample.
- Leptospirosis is a notifiable disease.
PREVENTION AND TREATMENT - Leptospirosis is treated with antibiotics, such as doxycycline or penicillin, which should be given early in the course of the disease.
- People with severe symptoms may need IV antibiotics.
- No effective human vaccine is available in the UK.
- The risk of infection can be reduced by avoiding swimming or wading in water that may be contaminated with animal urine.
- Protective clothing or footwear should be worn by those exposed to contaminated water or soil because of their job or recreational activities.
- Hands should be washed after handling animals or contaminated clothing or other materials, and always before eating, drinking or smoking.
- Doxycycline (200mg weekly) can be effective for people who may be at high risk for short periods, especially through their occupation.
- General preventative advice includes taking measures to reduce rodent populations, such as clearing rubbish and preventing rodent access into buildings.
- Existing cuts or abrasions should be covered with waterproof dressings before possible exposure.
- Any cuts or abrasions received during activities should be thoroughly cleaned.
- Showering as soon as possible after immersion in surface waters is recommended.
S-ar putea să vă placă și
- Communicable Disease Nursing2Document43 paginiCommunicable Disease Nursing2CAÑADA, JOHANNELYN M.Încă nu există evaluări
- RabiesDocument50 paginiRabiesMichael John TahadlangitÎncă nu există evaluări
- Source of Infections 1. Endogenous SourceDocument6 paginiSource of Infections 1. Endogenous SourceDeepu VijayaBhanuÎncă nu există evaluări
- Mumps - DishaDocument18 paginiMumps - DishaDr Bharat ZinjurkeÎncă nu există evaluări
- Historical Background and Trends in The Treatment of Infectious DiseasesDocument50 paginiHistorical Background and Trends in The Treatment of Infectious DiseasesJoeven HilarioÎncă nu există evaluări
- RabiesDocument28 paginiRabiesrouhanbinrashidÎncă nu există evaluări
- Introduction of MicroparasitoryDocument36 paginiIntroduction of MicroparasitoryEben Alameda-PalapuzÎncă nu există evaluări
- Chain of InfectionDocument69 paginiChain of Infectiondarkdark38Încă nu există evaluări
- NoteesDocument177 paginiNoteespearlanne1292100% (1)
- Human Health & DiseasesDocument62 paginiHuman Health & DiseasesSumiÎncă nu există evaluări
- Introduction To Microbiology - CHDDocument52 paginiIntroduction To Microbiology - CHDFrancis muhia KaranjaÎncă nu există evaluări
- Communicable Disease ReviewerDocument18 paginiCommunicable Disease ReviewerMicah Jonah Elicaño100% (1)
- Linton Chapter 13 Immune, Infection, InflammationDocument7 paginiLinton Chapter 13 Immune, Infection, InflammationJose FloresÎncă nu există evaluări
- A. Infectious ProcessDocument22 paginiA. Infectious ProcessKyla Malapit GarvidaÎncă nu există evaluări
- Immunitization and VaccinationDocument46 paginiImmunitization and VaccinationMazhar RehmanÎncă nu există evaluări
- Normal Body Defences - Basic NursingDocument28 paginiNormal Body Defences - Basic NursingAmfo Baffoe FrederickÎncă nu există evaluări
- Asepsis 1Document52 paginiAsepsis 1严子明 Renz Ryan SevillenoÎncă nu există evaluări
- Occupational Biohazards: Dr. Tajuddin Bantacut Department of Agroindustrial Technology Bogor Agricultural UniversityDocument29 paginiOccupational Biohazards: Dr. Tajuddin Bantacut Department of Agroindustrial Technology Bogor Agricultural UniversityAbdur RahmanÎncă nu există evaluări
- Infection Control and Prevention Protocols in Hotel Housekeeping (Final)Document44 paginiInfection Control and Prevention Protocols in Hotel Housekeeping (Final)Celso Jr FelipeÎncă nu există evaluări
- Production of Animal-Based Vaccines - Animal LeptospirosisDocument7 paginiProduction of Animal-Based Vaccines - Animal Leptospirosisjefina agnesÎncă nu există evaluări
- CHN Final TopicsDocument52 paginiCHN Final TopicsMary Ann SacramentoÎncă nu există evaluări
- Applied MicrobiologyDocument33 paginiApplied MicrobiologysanavoraÎncă nu există evaluări
- Lecture 7 - Communicable Disease ControlDocument26 paginiLecture 7 - Communicable Disease ControlBianca AnguloÎncă nu există evaluări
- Concept Communicable DiseasesDocument421 paginiConcept Communicable DiseasesJoric Magusara91% (11)
- Test Bank Current Medical Diagnosis and Treatment 2020 PapadakisDocument15 paginiTest Bank Current Medical Diagnosis and Treatment 2020 Papadakisguadaluperomerojz6s100% (13)
- Leptospirosis: Dr.T.V.Rao MDDocument40 paginiLeptospirosis: Dr.T.V.Rao MDMeitsu ChanÎncă nu există evaluări
- Immunology Notes WJEC 2022 SLJ 3Document37 paginiImmunology Notes WJEC 2022 SLJ 3zainpaÎncă nu există evaluări
- Funda NotesDocument4 paginiFunda Notesloviamae.belizarÎncă nu există evaluări
- Infection Control: IntroductionDocument17 paginiInfection Control: Introductionsuman gupta100% (1)
- Communicable DiseasesDocument164 paginiCommunicable DiseasesJasmin Jacob33% (3)
- AsepsisDocument14 paginiAsepsisKathleen MontañoÎncă nu există evaluări
- Asepsis and Infection ControlDocument10 paginiAsepsis and Infection ControlgilissaÎncă nu există evaluări
- MicrobesDocument6 paginiMicrobesemms meÎncă nu există evaluări
- Yellow FeverDocument31 paginiYellow FeverVibha AvasthiÎncă nu există evaluări
- Respiratory Infections ....Document195 paginiRespiratory Infections ....Poorny PurushothÎncă nu există evaluări
- Funda Lab Mod 1-4Document23 paginiFunda Lab Mod 1-4Liane BartolomeÎncă nu există evaluări
- Lab Technicians Job Interview Preparation GuideDocument9 paginiLab Technicians Job Interview Preparation Guidevishwanath cÎncă nu există evaluări
- Unit - Two - Infection Control - Universal PrecautionsDocument31 paginiUnit - Two - Infection Control - Universal Precautionsvirtus_kuwaitÎncă nu există evaluări
- I Infection ControlDocument11 paginiI Infection ControlTuTitÎncă nu există evaluări
- Chapter 18. Pinworm InfectionDocument12 paginiChapter 18. Pinworm InfectionMonica CiorneiÎncă nu există evaluări
- FUNDAMENTALS IN NURSING - Part 1Document5 paginiFUNDAMENTALS IN NURSING - Part 1arzooÎncă nu există evaluări
- Nature of InfectionDocument10 paginiNature of InfectionHussain FaqirjeeÎncă nu există evaluări
- Common Communicable DiseasesDocument213 paginiCommon Communicable Diseasesɹǝʍdןnos100% (24)
- 5.infection Control & Standard PrecautionsDocument33 pagini5.infection Control & Standard PrecautionsGilbert JohnÎncă nu există evaluări
- Mechanism of Infection and Transmission of Disease: PresentationDocument29 paginiMechanism of Infection and Transmission of Disease: PresentationSuryakant SonwaniÎncă nu există evaluări
- Cryptosporidium ParvumDocument7 paginiCryptosporidium ParvumKalebÎncă nu există evaluări
- UntitledDocument5 paginiUntitledKanike ChanÎncă nu există evaluări
- Communicable Nursing - LecturervDocument329 paginiCommunicable Nursing - LecturervCarl WaletÎncă nu există evaluări
- RabiesDocument43 paginiRabiesJerson PanopioÎncă nu există evaluări
- Biologics: by DR TanginaDocument41 paginiBiologics: by DR TanginaAnam AbidÎncă nu există evaluări
- Incidence:: Epidemiological DeterminantsDocument9 paginiIncidence:: Epidemiological DeterminantsGetom NgukirÎncă nu există evaluări
- Communicable Diseases HandoutsDocument15 paginiCommunicable Diseases HandoutsLloyd LozanoÎncă nu există evaluări
- COXIELLADocument6 paginiCOXIELLAFatima AbasovaÎncă nu există evaluări
- By-Dr. Samarjeet Kaur JR-II BRD Med. College GKPDocument17 paginiBy-Dr. Samarjeet Kaur JR-II BRD Med. College GKPSamarjeet Kaur100% (1)
- Bio ProjDocument12 paginiBio Projsb132086Încă nu există evaluări
- HHChapter 11 of Home Aid Care For Free (Education) YAAAYDocument85 paginiHHChapter 11 of Home Aid Care For Free (Education) YAAAYSamuel PerezÎncă nu există evaluări
- Leptospirosis: Cavite State University Indang, CaviteDocument9 paginiLeptospirosis: Cavite State University Indang, CavitePatricia Marie MojicaÎncă nu există evaluări
- Female Urinary Tract Infections in Clinical PracticeDe la EverandFemale Urinary Tract Infections in Clinical PracticeBob YangÎncă nu există evaluări
- Melidiosis FDocument24 paginiMelidiosis FVyramuthu AtputhanÎncă nu există evaluări
- PerceptionDocument11 paginiPerceptionVyramuthu Atputhan100% (1)
- Dis PreventionDocument38 paginiDis PreventionVyramuthu AtputhanÎncă nu există evaluări
- Who Mono 41 PDFDocument105 paginiWho Mono 41 PDFRyan Michael OducadoÎncă nu există evaluări
- Nursing Care Plan For Hypertension Nursing Assessment Nursing Care Plan For HypertensionDocument2 paginiNursing Care Plan For Hypertension Nursing Assessment Nursing Care Plan For HypertensionVyramuthu AtputhanÎncă nu există evaluări
- Communicable NursingDocument3 paginiCommunicable NursingVyramuthu AtputhanÎncă nu există evaluări
- 1stweek Intro Quanti Vs QualiDocument18 pagini1stweek Intro Quanti Vs QualiHael LeighÎncă nu există evaluări
- O o o O: (Approval and Adoption of BCPC AWFP) (Approval and Adoption of BCPC AWFP)Document2 paginiO o o O: (Approval and Adoption of BCPC AWFP) (Approval and Adoption of BCPC AWFP)Villanueva YuriÎncă nu există evaluări
- Pengaruh Skarifikasi Dan Hormon Giberelin (Ga) Terhadap Daya Kecambah Dan Pertumbuhan Bibit Palem Putri (Veitchia Merillii)Document8 paginiPengaruh Skarifikasi Dan Hormon Giberelin (Ga) Terhadap Daya Kecambah Dan Pertumbuhan Bibit Palem Putri (Veitchia Merillii)Adi IndraÎncă nu există evaluări
- Efficiency Improvement Oppertunities With BLDC Fan PDFDocument14 paginiEfficiency Improvement Oppertunities With BLDC Fan PDFjust_4_u_dear_in9549Încă nu există evaluări
- QuestionnaireDocument2 paginiQuestionnaireMili Gada100% (8)
- The 3 Basic Listening Models and How To Effectively Use ThemDocument6 paginiThe 3 Basic Listening Models and How To Effectively Use ThemTzuyu TchaikovskyÎncă nu există evaluări
- NG Uk RTR 0220 r15 PDFDocument9 paginiNG Uk RTR 0220 r15 PDFDuong Thai BinhÎncă nu există evaluări
- WAUZZZ8K0BA159120Document10 paginiWAUZZZ8K0BA159120Vedad VedaddÎncă nu există evaluări
- LFAMS Fee Structure OCT'2013Document7 paginiLFAMS Fee Structure OCT'2013Prince SharmaÎncă nu există evaluări
- NANOGUARD - Products and ApplicationsDocument2 paginiNANOGUARD - Products and ApplicationsSunrise VenturesÎncă nu există evaluări
- Soal Post TestDocument70 paginiSoal Post Testananda96% (25)
- OSCE Pediatric Dentistry Lecture-AnswersDocument40 paginiOSCE Pediatric Dentistry Lecture-AnswersR MÎncă nu există evaluări
- Hazard Risk Assessment of Roof of The Mazanine Floor..Document15 paginiHazard Risk Assessment of Roof of The Mazanine Floor..Akhtar BahramÎncă nu există evaluări
- Matriculation Chemistry Amino Acids-Part-1Document24 paginiMatriculation Chemistry Amino Acids-Part-1iki292Încă nu există evaluări
- Seed PrimingDocument4 paginiSeed PrimingbigbangÎncă nu există evaluări
- AdEasy Adenoviral Vector SystemDocument43 paginiAdEasy Adenoviral Vector SystemDaniel PintoÎncă nu există evaluări
- 2014 EN AdvancedBootkitTechniquesOnAndroid ChenZhangqiShendiDocument66 pagini2014 EN AdvancedBootkitTechniquesOnAndroid ChenZhangqiShendihombre pocilgaÎncă nu există evaluări
- Solved Rail Chapter 1Document7 paginiSolved Rail Chapter 1spectrum_48Încă nu există evaluări
- ComFlor 80 Load Span Tables PDFDocument4 paginiComFlor 80 Load Span Tables PDFAkhil VNÎncă nu există evaluări
- Allnex Powder BrochureDocument28 paginiAllnex Powder BrochureandreathomeÎncă nu există evaluări
- Clay Analysis - 1Document55 paginiClay Analysis - 1JCSÎncă nu există evaluări
- Shelf Life ControlDocument7 paginiShelf Life ControlRushikesh Deshpande100% (1)
- Channels of DistributionDocument101 paginiChannels of DistributionlakshmanlakhsÎncă nu există evaluări
- Impact of Odor From A Landfill Site On Surrounding Areas: A Case Study in Ho Chi Minh City, VietnamDocument11 paginiImpact of Odor From A Landfill Site On Surrounding Areas: A Case Study in Ho Chi Minh City, VietnamNgọc HảiÎncă nu există evaluări
- Dowry SystemDocument10 paginiDowry SystemBhoomejaa SKÎncă nu există evaluări
- Teri MicorisaDocument7 paginiTeri MicorisabiodieselnetÎncă nu există evaluări
- LR 1350 Operating InstructionsDocument1.495 paginiLR 1350 Operating InstructionsPatrick Polujan100% (12)
- Radfet DatasheetDocument6 paginiRadfet DatasheetNicholas EspinozaÎncă nu există evaluări
- MCQDocument5 paginiMCQJagdishVankar100% (1)
- Lesson Plan On Digestion in Stomach and Intestines Grade 4Document3 paginiLesson Plan On Digestion in Stomach and Intestines Grade 4jaydalene saga macay100% (5)