Documente Academic
Documente Profesional
Documente Cultură
Shock Exam
Încărcat de
Milagros Fuertes YosoresDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Shock Exam
Încărcat de
Milagros Fuertes YosoresDrepturi de autor:
Formate disponibile
1. A. B. C. D. 2.
A client is admitted to the ICU with a spinal cord injury from a motor vehicle accident. Which shock state is this client most at risk for developing? Obstructive Hypovolemic - neurogenic shock is a type of hypovolemic shock (analysis) Cardiogenic Transport A client has lost a considerable amount of blood and is demonstrating signs of pending shock. Which of the following shock states is this client most likely developing? Cardiogenic Obstructive
A. B.
C. Transport Hemorrhage is a transport shock state. A loss of blood is one example of a transport shock state. D.Hypovolemic 3. The nurse is trying to determine the client's current stage of shock. Which of the following body systems will begin the renin-angiotensin-aldosterone cycle? A. Cardiovascular B. C. Endocrine Pulmonary
D. Renal - As a result of decreased blood flow to the kidneys, the juxtaglomerular cells in the kidneys excrete renin. This begins the process. 4. A client is progressing into the third stage of shock. The nurse will expect this client to demonstrate: A. B. C. D. E. F. Profound hypotension. Buildup of metabolic wastes. Intractable circulatory failure. Neuroendocrine responses. Demonstrating MODS.
Increase in lactic acidosis. The third stage of shock, progressive, results in major dysfunction of many organs leading to multiple organ dysfunction syndrome or MODS. 5. Until the physician arrives to evaluate the status of a client in the ICU, the nurse is going to begin assessing a client for shock. Which of the following would be considered traditional methods to assess this client? A. Assess blood pressure. B. Have a serum lactate level drawn. C. Obtain the equipment for a sublingual capnography. D. Prepare the client for a gastric tonometry. E. Measure urine output. F. Analyze arterial blood gas sample. This is one of the traditional methods used to assess a client for shock. Traditional signs used to assess for shock include blood pressure, heart rate, mentation, and urine output.
6. The nurse is caring for a client who became ill after working on a car in his garage at home. Which of the following would help diagnose the cause for this client's illness? A. B. C. D. Presence of pulsus paradoxus Carboxyhemoglobin level Base deficit Presence of Beck's triad
An elevated carboxyhemoglobin level confirms carbon monoxide poisoning. 7. A client has been diagnosed with sepsis. The nurse will most likely find which of the following when assessing this client:
A. B. C. D. E.
Sepsis is manifested by two characteristics, such as temperature >38 degrees C, heart rate >90 bmp, respiratory rate >20 breaths/minute, WBC count >12,000 per liter.
8. A client in shock is prescribed an inotropic drug to act on alpha and beta receptors. The nurse will most likely be administering: A. B. C. D. Milrinone. Dopamine. Dobutamine. Pavulon.
Lactic acidosis. Severe hypotension. Oliguria. Elevated temperature. Rapid shallow respirations. F. Mental status changes.
Dopamine has both alpha- and betareceptor effects.
9. The nurse is caring for a client experiencing anaphylactic shock. Which of the following should be included in the plan of care for this client? A. Remove the mechanical barrier to blood flow. B. Restore body fluids. C. Maintain an adequate airway. D. Decrease myocardial oxygen demand E. Remove the source of infection. F. Support the blood pressure. Immediate goal in the treatment of anaphylactic shock is to maintain an adequate airway and to support the blood pressure.
10. A patient arrives in the emergency department with symptoms of myocardial infarction, progressing to cardiogenic shock. Which of the following symptoms should the nurse expect the patient to exhibit with cardiogenic shock? A. Hypertension. B. Bradycardia. C. Bounding pulse. D. Confusion.
Answer: Answer:
D - Cardiogenic shock severely impairs the pumping function of the heart muscle, causing diminished blood flow to the organs of the body. This results in diminished brain function and confusion, as well as hypotension, tachycardia, and weak pulse. Cardiogenic shock is a serious complication of myocardial infarction with a high mortality rate. 11. Tissue plasminogen activator (t-PA) is considered for treatment of a patient who arrives in the emergency department following onset of symptoms of myocardial infarction. Which of the following is a contraindication for treatment with t-PA? A. Worsening chest pain that began earlier in the evening. B. History of cerebral hemorrhage. C. History of prior myocardial infarction. D. Hypertension. Answer: B 12. A history of cerebral hemorrhage is a contraindication to tPA because it may increase the risk of bleeding. TPA acts by dissolving the clot blocking the coronary artery and works best when administered within 6 hours of onset of symptoms. Prior MI is not a contraindication to tPA. Patients receiving tPA should be observed for changes in blood pressure, as tPA may cause hypotension. 13. A patient is hemorrhaging from multiple trauma sites. The nurse expects that compensatory mechanisms associated with hypovolemia would cause all of the following symptoms EXCEPT
A. hypertension B. oliguria C. tachycardia D. tachypnea
14. Patrick who is hospitalized following a myocardial infarction asks the nurse why he is taking morphine. The nurse explains that morphine: a. Decrease anxiety and restlessness b. Prevents shock and relieves pain c. Dilates coronary blood vessels d. Helps prevent fibrillation of the heart answer: B. Morphine is a central nervous system depressant used to relieve the pain associated with myocardial infarction, it also decreases apprehension and prevents cardiogenic shock. 15. A 64 year old male client with a long history of cardiovascular problem including hypertension and angina is to be scheduled for cardiac catheterization. During pre cardiac catheterization teaching, Nurse Cherry should inform the client that the primary purpose of the procedure is.. a. To determine the existence of CHD b. To visualize the disease process in the coronary arteries c. To obtain the heart chambers pressure d. To measure oxygen content of different heart chambers
answer: B. The lumen of the arteries can be assessed by cardiac catheterization. Angina is
usually caused by narrowing of the coronary arteries.
16. During the first several hours after a cardiac catheterization, it would be most essential for nurse Cherry to a. Elevate clients bed at 45 b. Instruct the client to cough and deep breathe every 2 hours c. Frequently monitor clients apical pulse and blood pressure d. Monitor clients temperature every hour answer: C. Blood pressure is monitored to detect hypotension which may indicate shock or hemorrhage. Apical pulse is taken to detect dysrhythmias related to cardiac irritability. 17. A client has 15% blood loss. Which of the following nursing assessment findings indicates hypovolemic shock? a. Systolic blood pressure less than 90mm Hg b. Pupils unequally dilated c. Respiratory rate of 4 breath/min d. Pulse rate less than 60bpm
answer: A. Typical signs and symptoms of hypovolemic shock includes systolic blood
pressure of less than 90 mm Hg. 18. All of the following are primary patient management goals for hypovolemic shock except a. increasing urinary output. b. controlling hemorrhage. c. restoring adequate cardiac output. d. maximizing oxygen delivery
S-ar putea să vă placă și
- Shocks MCQDocument6 paginiShocks MCQJaya Krishna Naidu100% (1)
- MCQ Medical Surgical NursingDocument11 paginiMCQ Medical Surgical NursingHasan A AsFourÎncă nu există evaluări
- CPSP Demo Questions With Key - PDF Version 1Document23 paginiCPSP Demo Questions With Key - PDF Version 1Arshad AliÎncă nu există evaluări
- Medical MCQ PDFDocument3 paginiMedical MCQ PDFAslamCv50% (2)
- Acute Abdominal Pain MCQs and ManagementDocument4 paginiAcute Abdominal Pain MCQs and ManagementAsim NiazÎncă nu există evaluări
- Body Fluids Quiz: Extracellular vs Intracellular CompositionDocument7 paginiBody Fluids Quiz: Extracellular vs Intracellular CompositionNivya Mary100% (1)
- Sample MCQ Medical GIT DisordersDocument3 paginiSample MCQ Medical GIT DisordersJay Menon100% (2)
- MCQs TBIDocument9 paginiMCQs TBIAkbar Ali100% (3)
- Acid Base Multiple Choice QuestionsDocument6 paginiAcid Base Multiple Choice QuestionsAsgharÎncă nu există evaluări
- CIRCULATION PHYSIOLOGY MCQs Test PDFDocument6 paginiCIRCULATION PHYSIOLOGY MCQs Test PDFMiles Hui67% (3)
- Burn Mcqs With AnswersDocument20 paginiBurn Mcqs With AnswersMusa yohana80% (20)
- DD McqsDocument6 paginiDD McqsCHANGEZ KHAN SARDARÎncă nu există evaluări
- General AnestheticsDocument4 paginiGeneral AnestheticsMuhammad Sheraz100% (2)
- Exam 24 AnswersDocument4 paginiExam 24 AnswersJulyhathul KuraishiÎncă nu există evaluări
- Nursing Quiz Topic GlaucomaDocument3 paginiNursing Quiz Topic GlaucomaChieChay Dub100% (1)
- Anasthesia 2015 Eja MnuDocument41 paginiAnasthesia 2015 Eja MnuMysheb SS50% (4)
- MCQs in PharmacologyDocument7 paginiMCQs in Pharmacologysidharta_chatterjee100% (1)
- Midterm Exam 1Document6 paginiMidterm Exam 1Joanne Bernadette AguilarÎncă nu există evaluări
- Local Anesthetic Nerve Block ReviewDocument8 paginiLocal Anesthetic Nerve Block Reviewvelo100% (1)
- Asthma QUIZDocument4 paginiAsthma QUIZAjay Nainavat50% (2)
- NCLEX Test CVA, Neuro 24Document19 paginiNCLEX Test CVA, Neuro 24Ann Michelle TarrobagoÎncă nu există evaluări
- Burn Care NCLEX ReviewDocument5 paginiBurn Care NCLEX ReviewNicoh Avila100% (1)
- MCQ On Respiratory SystemDocument4 paginiMCQ On Respiratory SystemSucheta Ghosh ChowdhuriÎncă nu există evaluări
- T2 - QZ 3 - CardioDocument6 paginiT2 - QZ 3 - CardioenzoÎncă nu există evaluări
- Med Surg Questions Oct 25 Angela DeVarsoDocument38 paginiMed Surg Questions Oct 25 Angela DeVarsonochip10100% (1)
- Essential oral hygiene interventions for stroke clientsDocument42 paginiEssential oral hygiene interventions for stroke clientsPrince K. Tailey100% (2)
- Anesthesia MCQDocument13 paginiAnesthesia MCQbouchikhi100% (1)
- Compiled McqsDocument24 paginiCompiled Mcqsarbaz100% (1)
- Cardio Paper NewDocument24 paginiCardio Paper Newwarda abbasi100% (1)
- Water, ElectrolyteDocument15 paginiWater, Electrolytevicky_law_2Încă nu există evaluări
- Urinary System MCQDocument12 paginiUrinary System MCQshaiyrkul kasmambetova100% (2)
- 90 MCQsDocument18 pagini90 MCQsMarielou CoutinhoÎncă nu există evaluări
- Intensive Care Nursing OSCE Rxam Multiple Choice QuestionsDocument1 paginăIntensive Care Nursing OSCE Rxam Multiple Choice QuestionsMoh Yousif100% (2)
- Acute Renal Failure Questions With RationaleDocument2 paginiAcute Renal Failure Questions With RationaleAngelica Mae Adlawan Desalesa0% (2)
- Pharm Cns McqsDocument9 paginiPharm Cns McqsMohamed YousefÎncă nu există evaluări
- Trauma MCQ DiDocument13 paginiTrauma MCQ DiJohn M. HemsworthÎncă nu există evaluări
- Nursing Practice TestDocument19 paginiNursing Practice TestEdward Nicko GarciaÎncă nu există evaluări
- Medical Surgical NursingDocument6 paginiMedical Surgical NursingHCX dghhq100% (2)
- Neurology MCQDocument5 paginiNeurology MCQRaghu Nadh0% (1)
- Medical Surgical Nursing Questions and Answers With Rationale - Nurses ClassDocument5 paginiMedical Surgical Nursing Questions and Answers With Rationale - Nurses ClassKarren Fernandez100% (2)
- B.science McqsDocument13 paginiB.science McqsAamir100% (1)
- تجميعةDocument168 paginiتجميعةRn nadeenÎncă nu există evaluări
- 110 TOP SURGERY Multiple Choice Questions and Answers PDF - Medical Multiple Choice Questions PDFDocument11 pagini110 TOP SURGERY Multiple Choice Questions and Answers PDF - Medical Multiple Choice Questions PDFaziz0% (1)
- Respiratory Physiology AnswersDocument4 paginiRespiratory Physiology AnswersRamya100% (2)
- Anaesthesia MCQDocument10 paginiAnaesthesia MCQshbhumi576100% (1)
- MS1Document60 paginiMS1Jayson Britania MayugaÎncă nu există evaluări
- Ophthalmic ENT sLE MCQDocument10 paginiOphthalmic ENT sLE MCQAsif Newaz100% (4)
- General Paper September 2020Document26 paginiGeneral Paper September 2020Kumah Wisdom100% (1)
- 5 - Physiology MCQ Body Fluids & HormonesDocument5 pagini5 - Physiology MCQ Body Fluids & Hormonesaboody omerÎncă nu există evaluări
- Respiratory System Study Questions Directions: Each of The Numbered Items or Incompl Ete Statements in This Section Is Followed by AnswersDocument7 paginiRespiratory System Study Questions Directions: Each of The Numbered Items or Incompl Ete Statements in This Section Is Followed by AnswersKo Haku100% (1)
- Respiratory System Functions and ProcessesDocument9 paginiRespiratory System Functions and ProcessesIan MatatulaÎncă nu există evaluări
- Anaesthesia MCQ 2021Document18 paginiAnaesthesia MCQ 2021invisiblealchemist2007Încă nu există evaluări
- Chapter 20 - Postoperative Nursing ManagementDocument17 paginiChapter 20 - Postoperative Nursing ManagementTeemara KingÎncă nu există evaluări
- Practice Multiple Choice QuestionsDocument5 paginiPractice Multiple Choice QuestionsjunxicooperÎncă nu există evaluări
- MJCQDocument94 paginiMJCQElsayed Ahmed0% (1)
- Periop BDocument11 paginiPeriop BhopeyangÎncă nu există evaluări
- Local Media4482927318145976675Document9 paginiLocal Media4482927318145976675Shane Zia FabrosÎncă nu există evaluări
- RESPIRATORY AND CARDIOVASCULAR COMPETENCY APPRAISALDocument3 paginiRESPIRATORY AND CARDIOVASCULAR COMPETENCY APPRAISALaaron tabernaÎncă nu există evaluări
- MS Day 1 1Document13 paginiMS Day 1 1Hazel BandayÎncă nu există evaluări
- Icu Skills Assessment ExamDocument5 paginiIcu Skills Assessment ExamJona AureÎncă nu există evaluări
- 1psych Pre TestDocument2 pagini1psych Pre TestMilagros Fuertes YosoresÎncă nu există evaluări
- Special Problems in Marital RelationshipDocument43 paginiSpecial Problems in Marital RelationshipMilagros Fuertes YosoresÎncă nu există evaluări
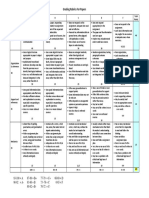
- Rubrics For EssayDocument1 paginăRubrics For EssayMilagros Fuertes YosoresÎncă nu există evaluări
- Grad Thesis ProposalDocument3 paginiGrad Thesis Proposalgio477Încă nu există evaluări
- The Concept of FamilyDocument22 paginiThe Concept of FamilyMilagros Fuertes YosoresÎncă nu există evaluări
- Perineal Care Checklist: Female Hygiene ProcedureDocument1 paginăPerineal Care Checklist: Female Hygiene ProcedureMilagros Fuertes YosoresÎncă nu există evaluări
- Rubrics For EssayDocument1 paginăRubrics For EssayMilagros Fuertes YosoresÎncă nu există evaluări
- Essential Developmental Tasks and Theories for New ParentsDocument3 paginiEssential Developmental Tasks and Theories for New ParentsMilagros Fuertes YosoresÎncă nu există evaluări
- Grading Rubrics For Papers PDFDocument1 paginăGrading Rubrics For Papers PDFMilagros Fuertes YosoresÎncă nu există evaluări
- PTSDDocument3 paginiPTSDMilagros Fuertes YosoresÎncă nu există evaluări
- Psychiatric NursingDocument46 paginiPsychiatric NursingMilagros Fuertes YosoresÎncă nu există evaluări
- Community Health NursingDocument11 paginiCommunity Health NursingMilagros Fuertes YosoresÎncă nu există evaluări
- Nursing Exam on Cellular Aberration and CancerDocument3 paginiNursing Exam on Cellular Aberration and CancerMilagros Fuertes YosoresÎncă nu există evaluări
- Legal and Ethical Issues in EMSDocument6 paginiLegal and Ethical Issues in EMSMilagros Fuertes YosoresÎncă nu există evaluări
- Triage Level 5Document78 paginiTriage Level 5DanielKnows100% (1)
- PTSDDocument3 paginiPTSDMilagros Fuertes YosoresÎncă nu există evaluări
- Revised Disaster NursingDocument25 paginiRevised Disaster NursingLlana Pauline JacintoÎncă nu există evaluări
- Care For The ElderlyDocument223 paginiCare For The ElderlyMilagros Fuertes Yosores100% (1)
- Perineal Care Checklist: Female Hygiene ProcedureDocument1 paginăPerineal Care Checklist: Female Hygiene ProcedureMilagros Fuertes YosoresÎncă nu există evaluări
- Psychiatric NursingDocument46 paginiPsychiatric NursingMilagros Fuertes YosoresÎncă nu există evaluări
- Care For The ElderlyDocument223 paginiCare For The ElderlyMilagros Fuertes Yosores100% (1)
- Comforting Infants and ToddlersDocument127 paginiComforting Infants and ToddlersTadeous Laurent100% (2)
- 8 PHYSIOLOGIC CHANGES IN AGING AFFECTING VARIOUS SYSTEMS 2nd PartDocument9 pagini8 PHYSIOLOGIC CHANGES IN AGING AFFECTING VARIOUS SYSTEMS 2nd Partgwen manalonÎncă nu există evaluări
- WSES Consensus Conference Guidelines - TCEDocument9 paginiWSES Consensus Conference Guidelines - TCEDr. Victor Alonso Hernández HernándezÎncă nu există evaluări
- Cas Medical 750 Service Manual PDFDocument145 paginiCas Medical 750 Service Manual PDFEdgar OsorioÎncă nu există evaluări
- General Survey, Mental Status Exam, andDocument25 paginiGeneral Survey, Mental Status Exam, andjazzreign50% (2)
- V100 User ManualDocument220 paginiV100 User Manualahmed Osama0% (1)
- DVD - Arachnophobia - Jeff Daniels y Sands - 1990 MP4 ENDocument74 paginiDVD - Arachnophobia - Jeff Daniels y Sands - 1990 MP4 ENTracy WynnÎncă nu există evaluări
- Prevention of Hypotension During Spinal AnesthesiaDocument4 paginiPrevention of Hypotension During Spinal AnesthesiaArdi FkuiÎncă nu există evaluări
- Mechanical Thrombectomy For Acute Ischemic Stroke - UpToDateDocument20 paginiMechanical Thrombectomy For Acute Ischemic Stroke - UpToDateisabel pangÎncă nu există evaluări
- 327-1659-1-PB YogaaDocument4 pagini327-1659-1-PB YogaaikaÎncă nu există evaluări
- Funda Lec ReviewerDocument13 paginiFunda Lec ReviewerDawn RallosÎncă nu există evaluări
- Hypertensive Disorders in Pregnancy: 2019 National GuidelineDocument14 paginiHypertensive Disorders in Pregnancy: 2019 National GuidelinerizkaÎncă nu există evaluări
- Converter ALL Purpose Worksheet (Conversions)Document28 paginiConverter ALL Purpose Worksheet (Conversions)CharyÎncă nu există evaluări
- Vital SignsDocument97 paginiVital SignsPrincess Mariscotes100% (1)
- Cilnidipine 1Document62 paginiCilnidipine 1dkhandke0% (1)
- What Is HypertensionDocument18 paginiWhat Is HypertensionShahzad ShameemÎncă nu există evaluări
- Sensors 20 00851 v2 PDFDocument12 paginiSensors 20 00851 v2 PDFsalemÎncă nu există evaluări
- Zoology Field ReportDocument11 paginiZoology Field ReportAnu Neth ThongonÎncă nu există evaluări
- Hemodynamics - New Diagnostic and The Rape Uric ApproachesDocument164 paginiHemodynamics - New Diagnostic and The Rape Uric Approachesa_artışÎncă nu există evaluări
- Vieillard-Baron2018 Article DiagnosticWorkupEtiologiesAndMDocument17 paginiVieillard-Baron2018 Article DiagnosticWorkupEtiologiesAndMFranciscoÎncă nu există evaluări
- Doppler Ultrasound of The KidneysDocument23 paginiDoppler Ultrasound of The KidneysivoklarinÎncă nu există evaluări
- Clinical Worksheet - PortfolioDocument3 paginiClinical Worksheet - Portfolioapi-691262000Încă nu există evaluări
- Natural Sea Salt Consumption Confers Protection Against Hypertension and Kidney Damage in Dahl Salt Sensitive RatsDocument11 paginiNatural Sea Salt Consumption Confers Protection Against Hypertension and Kidney Damage in Dahl Salt Sensitive RatsevitajulieÎncă nu există evaluări
- Pe ReviewerDocument11 paginiPe ReviewerJohn Arsen AsuncionÎncă nu există evaluări
- Exercise For Older Adults - ACE's Guide For Fitness Professionals (PDFDrive)Document577 paginiExercise For Older Adults - ACE's Guide For Fitness Professionals (PDFDrive)nitish sharmaÎncă nu există evaluări
- Drager Patient Monitor PM8060 User ManualDocument104 paginiDrager Patient Monitor PM8060 User ManualJOSE DE LA CRUZÎncă nu există evaluări
- Cardiovascular NotebookDocument140 paginiCardiovascular NotebookChantal CarnesÎncă nu există evaluări
- Clinical Nursing JudgmentDocument5 paginiClinical Nursing Judgmentapi-546730313Încă nu există evaluări
- NHS GuidelinesDocument339 paginiNHS GuidelinesAndri FerdianÎncă nu există evaluări
- Heartbeat Sensor Arduino Project Measures Heart RateDocument13 paginiHeartbeat Sensor Arduino Project Measures Heart Ratekrishna mohan pandeyÎncă nu există evaluări