Documente Academic
Documente Profesional
Documente Cultură
New TX of DM Neuropathy Pathogen Oriented Treatment PDF
Încărcat de
Chikezie OnwukweTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
New TX of DM Neuropathy Pathogen Oriented Treatment PDF
Încărcat de
Chikezie OnwukweDrepturi de autor:
Formate disponibile
New Treatments for Diabetic Neuropathy: Pathogenetically Oriented Treatment
Angelika Bierhaus, PhD, Per M. Humpert, MD, Gottfried Rudofsky, MD, Thoralf Wendt, MD, Michael Morcos, MD, Andreas Hamann, MD, and Peter P. Nawroth, MD
Address Department of Medicine I, University of Heidelberg, Bergheimer Str. 58, Heidelberg 69115, Germany. E-mail: Peter.Nawroth@med.uni-heidelberg.de Current Diabetes Reports 2003, 3:452458 Current Science Inc. ISSN 1534-4827 Copyright 2003 by Current Science Inc.
Oxidative Stress in Diabetic Neuropathy
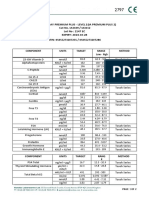
Animal models have demonstrated an improvement of experimental diabetic neuropathy (EDN) through lowering oxidative stress by supplementation of antioxidative substances (Fig. 1). Subcutaneous injections of M40403, a functional mimetic of superoxide dismutase, reduced the appearance of superoxide in epineurial vessels and significantly improved the diabetes-induced decrease in endoneurial blood flow, acetylcholine-mediated vascular relaxation, and motor nerve conduction velocity (NCV) [5]. Dietary supplementation with antioxidative scavengers such as butylated hydroxytoluene, probucol, dehydroepiandrosterone, taurine, vitamin E, transition metal chelators and thiol agents such as acetyl cysteine, glutathione, and -lipoic acid prevented loss of motor and sensory conduction velocity and latency in pain perception of diabetic animals [6]. It is noteworthy that lipoic acid not only acts as radical scavenger and metal chelator, but also regenerates thioredoxin, vitamin C, and glutathione (recycling vitamin E), and induces cyclooxygenase (having anti-inflammatory properties) [7]. However, the optimal dose of antioxidants is not yet known. Extremely large doses of potentially radical scavenging concentrations are often used to achieve protective effects, whereas low concentrations, which regulate the cycle-dependent ROS metabolism and may have beneficial effects apart from radical scavenging, have not yet been studied. A pilot study testing the effect of vitamin E on electrophysiologic parameters in patients with symptomatic diabetic sensory polyneuropathy (DSPN) resulted in improvement of motor NCV, but not sensory NCV [8]. A small study in 14 type 2 diabetic patients demonstrated that a 6-week treatment with the thiamine derivate benfothiamine improved vibratory sensitivity and parasympathetic control of heart rhythm [9]. Large randomized, placebo-controlled clinical trials in patients with symptomatic DSPN using -lipoic acid demonstrated a reduction of major neuropathic symptoms such as pain, paresthesia, and numbness in short-term application [10], and a reduction in neuropathic deficits and improvement of cardiac autonomic neuropathy and motor and sen-
Although there is clear evidence from experimental diabetic neuropathy (DN) models that the multiple pathways involved in neuronal degeneration cause overproduction of reactive oxygen species, oxidative stress, and cellular dysfunction, therapeutic approaches addressing these mechanisms have not yet provided a basis for a successful treatment of patients with DN. This review discusses the current knowledge on the pathomechanisms of unchecked reactive oxygen species accumulation, implications for specific treatment, and the need for carefully designed experimental studies and clinical trials closing the gap between promising results in experimental DN and its implementation into a pathogenetically oriented treatment.
Introduction
Accumulating data indicate that diabetes is a state of increased production of reactive oxygen species (ROS) with parallel depletion of antioxidant defense mechanisms [1,2]. Polyunsaturated fatty acids in neuronal tissues are vulnerable targets of ROS-dependent peroxidation, which in turn initiate autocatalytic chain reactions to form peroxide and other fatty acids [3]. Although a large number of studies demonstrated alterations in the antioxidative defense of diabetic non-neuronal tissues, little is known about changes in peripheral nerves. Even though these have cytosolic and lipophilic antioxidant defense mechanisms, their radical defense is reduced in comparison to central nervous tissue [4]. In addition, ROS induces the dysfunction of microvessels supplying peripheral nerves and ganglia, and promotes ischemic damage of the tissue.
New Treatments for Diabetic Neuropathy: Pathogenetically Oriented Treatment Bierhaus et al.
453
Figure 1. Pathways involved in the pathogenesis of diabetic neuropathies and sides for possible intervention. AGEsadvanced glycation end products; ARaldose reductase; ARIsaldose reductase inhibitors; NF-kBnuclear factor-kB; NGFnerve growth factor; O2-superoxide; ONOO-peroxynitrite; PARPpoly(ADP-ribose) polymerase; PKCprotein kinase C; RAGEreceptor for advanced glycation end products.
sory NCV upon long-term treatment [11,12]. The SYDNEY trial confirmed that metabolically stable patients with symptomatic DSPN benefit from long-term intravenous treatment with -lipoic acid therapy by a significant improvement of the total symptom score, summing up the presence, severity, and duration of lancinating pain, burning pain, prickling, and numbness while asleep [12]. Despite beneficial effects, the clinical trials so far did not live up to the expectations originally provided by EDN studies implicating oxidative stress as a central mediator in diabetic neuropathy (DN). This may be due to the fact that oxidative stressdependent activation of the transcription factor nuclear factor-B (NF-B) may be deleterious to microvessels of the vasa nervorum, while it is supposed to have neuroprotective effects in neuronal cells. Thus, the role of oxidative stress for the development of DN is still not clear due to lack of experimental studies comparing the effects of antioxidant therapies on different cellular compartments at different time points of the disease. In addition, the time course of EDN and clinical trials is different. The development of diabetes in experimental settings is a well-controlled event, generally targeted by the respective treatments right after the onset of hyperglycemia. In
EDN, antioxidants are, therefore, given much earlier than in patients with DN.
The Consequences of Oxidative Stress
Neuroprotective and neurodegenerative NF-B activation One major target of oxidative stress is the transcription factor NF-B, which is rapidly activated by a variety of stimuli such as ROS, high glucose, proinflammatory cytokines, and growth factors [13]. NF-B activates the transcription of target genes, such as cytokines, adhesion molecules, the procoagulant tissue factor, endothelin-1 (ET-1), inducible nitric oxide (NO) synthase, inducible cyclooxygenase, heme oxygenase type 1, 5-lipoxygenase, receptor for advanced glycation end products (RAGE), and I kBa . Remarkably, all antiapoptotic genes known thus far, including BcL-XL, Bcl-2, and the Bcl-2 homologue A1, are also controlled by NF-B. Therefore, NF-B activation provides a rapid and sensitive cellular response and ensures cellular survival [13]. A number of studies provide evidence for NF-B having a protective role in sensory neurons, although only
454
Microvascular ComplicationsNeuropathy
limited data are available with respect to DN. Purves and Tomlinson [14] have demonstrated a decrease in NF-B in dorsal root ganglia (DRG) obtained from 12-week-old streptozotocin (STZ)-induced diabetic rats. Conversely, two recent studies show that hyperglycemia and diabetes result in upregulation of NF-B in epineural and endoneural vessels and the perineurium in both STZ-induced diabetic rats [15] and in patients with long-standing diabetes [16]. A combined treatment with two NF-Bspecific inhibitors, PDTC and TLCK, did not only reduce NF B activation in sciatic nerves of diabetic rats, but also improved NCVs in these animals [15]. Experimental models have provided ample evidence that neuronal dysfunction and neuropathic pain are induced and increased through NF-Bcontrolled proinflammatory cytokines, such as interleukin-6 and tumor necrosis factor- [17]. NF-Bregulated adhesion molecules are also induced during pain and initiate the migration of opioid-containing immune cells into inflamed sites [18]. Further evidence for an involvement of NF-B in the pathology of neuronal dysfunction comes from studies in which NF-B decoys injected into the endoneurium at sites of nerve lesions suppress cytokine and adhesion molecule expression, and subsequently thermal hyperalgesia in a rat neuropathic pain model [19]. This observation implies that increased NF-B activation may also contribute to pain in DN. Immunohistochemical analysis of sural nerve biopsies from patients with DN, however, demonstrated increased NF-B activation, particularly in the vasa nervorum of all diabetic patients with long-standing diabetes and painful as well as painless neuropathy [16]. Therefore, studies are required to address the time course of NF-B activation from the early stages of diabetes (often associated with pain) to long-standing diabetes. Thus, it is not yet clear whether the increased NF-B activation observed in the peripheral nerves and ganglia of diabetic animals and patients has neuroprotective or neurodegenerative effects. Evidence for a dual role of NF-B in neuronal function comes from studies in chick embryos either unlesioned, or after a unilateral tectal lesion, which axotomizes ganglion cells. Although the number of dying cells in the retina contralateral to the lesion were reduced in embryos receiving NF-B inhibitors, the same NF-B inhibitors administered as pretreatment before intraocular injection of toxic substances drastically raised neuronal death and induced degenerative changes in the retina [20]. A comparable stimulus-dependent activation of NF-B, resulting in either apoptosis or neuroprotection, has recently been observed in cultured cerebellar granule cells [21] and suggests that activation of NFB is a double-edged sword. This strongly demands reconsideration of the use of high doses of antioxidants. Furthermore, it will be necessary to carefully investigate defined models of EDN and to validate the effects of antioxidants on both neuroprotective and neurodestructive properties of NF-B in different cellular compartments.
Apoptosis Studies in both experimental models and human sural nerve biopsies indicate an association of oxidative stress, mitochondrial membrane depolarization, and induction of programmed cell death. DRG isolated from STZ-induced rats with decreased peripheral NCVs demonstrate increased apoptosis associated with an elevated mitochondrial membrane potential [22,23]. The antiapoptotic genes Bcl-2, Bax, and Bcl-XL are primarily expressed in the inner mitochondrial membrane stabilizing the mitochondrial membrane by inhibiting the opening of the mitochondrial permeability transition pore [23]. Opening the permeability transition pore results in loss of the mitochondrial membrane potential and expansion of the intermembranous space, leading to outer membrane rupture and subsequent release of caspase-activating enzymes [23]. Diabetic sensory polyneuropathy is associated with a selective decrease in the levels of Bcl-2 and increased apoptosis in diabetic neurons [23]. Thus, the pathophysiology of early DSPN could involve activation of the apoptosis cascade. Besides excessive ROS production, downstream effectors such as caspases may represent potential targets for diagnosis and therapeutic intervention in DN. Remarkably, acute lowering of glucose levels under hypoxic conditions can also lead to apoptosis of DRG neurons [23], suggesting that there is an optimal glucose concentration for neuronal survival. This may be relevant for the acute painful neuropathy occurring in patients rapidly correcting their blood glucose levels after a period of hyperglycemia [22,24]. Consistent with the hypothesis of apoptosis playing a role in the development of DN, circulating soluble Fas and Fas ligand, two transmembrane glycoproteins involved in apoptosis, are significantly elevated in patients with DN. In addition, sera from patients with type 1 diabetes and DN contain an activator of Fas-regulated apoptosis that may also contribute to the pathogenesis of DN. Vascular dysfunction Increased ROS are known to promote endothelial dysfunction. Because vasoregulation of nerve microvessels is regulated at the arteriolar, venular, and endothelial cell level, the etiology of DN is considered to have a large vascular component. Therefore, the pathophysiology of nerve dysfunction in diabetes can also be explained by reduced endoneurial microcirculation, impaired blood flow due to a perturbed NO, prostanoid metabolism, and alterations in endoneurial metabolism. A number of experimental models have demonstrated that infusion of glucose or induction of diabetes results in abnormalities of vasodilatation by NO and prostacyclin. Reduced NO release can be improved in the presence of antioxidants; however, it is not yet known whether antioxidants primarily improve nerve blood flow or normalize systemic or endoneurial oxidative metabolism. An overactive polyol
New Treatments for Diabetic Neuropathy: Pathogenetically Oriented Treatment Bierhaus et al.
455
pathway that competes with the endothelial NO synthase for NADPH, thereby resulting in pseudohypoxia and NO deficiency and the presence of advanced glycation end products (AGEs) able to quench NO, may further promote the depletion of NO [25]. A recent study demonstrated that elevated plasma homocysteine, a strong predictor for DN in patients with type 2 diabetes, increases asymmetrical dimethylarginine, an endogenous inhibitor of NO synthase, leading to a decreased NO generation by endothelial cells [26]. Recent studies have demonstrated that proinsulin Cpeptide stimulates the activity of Na+,K+-ATPase and endothelial NO synthase via a G-proteincoupled membrane receptor. Consistently, C-peptide replacement ameliorates nerve dysfunction in EDN [27]. This suggests that besides hyperglycemia, impaired insulin secretion could significantly contribute to defective nerve fiber regeneration in type 1 (but not type 2) DN [28]. In addition to impaired NO-mediated vasodilation, upregulation of NF- B is likely to support endoneural ischemia by inducing NF-Bregulated proinflammatory and procoagulant gene products including tissue factor and ET-1. Because the vasa nervorum expresses ET-1 receptors, it is susceptible to ET-1dependent vasoconstriction. Microvascular ischemia may be further promoted by a substantial reduction in vascular endothelial thrombomodulin expression recently reported in the human diabetic nerve microvasculature [29]. Recent observations that restoring vascularization of the vasa nervorum through vascular endothelial growth factor induced angiogenesis in mice results in reversal of EDN [30] support the notion that microvascular ischemia involving the vasa nervorum contributes to EDN. Initial studies using microlightguide spectrophotometry to measure intravascular oxygen saturation and blood flow in human sural nerve confirmed a reduced nerve oxygenation and impaired blood flow in patients with mild-moderate sensory motor DN. Intravascular oxygen saturation was higher in patients with painful neuropathy compared to those without pain [31]. This implies that hemodynamic factors could play an important role in the pathogenesis of neuropathic pain or, alternatively, that arterial O2-exchange is impaired [31]. Despite the solid theoretic background for a treatment with vasodilating drugs and a large number of experimental models, very few clinical studies have been performed so far. One reason for the lack of clinical trials may be that the role of peripheral nerve ischemia is still discussed antithetically. Some authors postulate that early reduction in nerve blood flow accounts for DN [32,33]. Other experimental studies do not support a role of early ischemia for DN, but demonstrate that vasodilatation after guanethidine sympathectomy actually worsened indices of neuropathy, although it increased nerve blood flow [34]. This suggests that vasodilators may exacerbate postural hypotension, particularly in diabetic patients with autonomic dysfunction [34]. Despite these considerations, the clinical studies performed so far demonstrate an effective reduction in some
(but not all) neuropathic symptoms. A placebo-controlled 1-year study with 41 normotensive type 1 or type 2 diabetic patients with mild neuropathy receiving the angiotensinconverting enzyme inhibitor trandolapril resulted in an improvement of NCV, whereas vibration-perception threshold, autonomic function, and the neuropathy symptom and deficit score did not change compared to control subjects [35]. Treatment of 364 diabetic patients with neuropathy or leg ulcers with prostaglandin E1 (PGE1) incorporated in lipid microspheres (lipo-PGE1) for 4 weeks improved motor conduction velocity [36]. Furthermore, lipo-PGE administration reduced elevated circulating plasma ET-1 levels. Interestingly, local administration of isosorbide dinitrate, an NO donor with local vasodilating properties, reduced overall neuropathic pain and burning sensations in a pilot study with 22 patients [37]. In accordance with the experimental data mentioned above, recent studies have demonstrated that administration of proinsulin C-peptide for 3 months ameliorates nerve dysfunction in patients with type 1 diabetes [38]. Thus, impaired insulin action may explain the differences in nerve fiber regeneration between type 1 and type 2 diabetes [28]. However, C-peptide deficiency may also play a role in DN in patients with type 2 diabetes, because patients with good residual C-peptide secretion seem to be better protected from endothelial dysfunction than patients with poor Cpeptide secretion.
Lipolysis and depletion of -linolenic acid Endoneurial ischemia promotes increased lipolysis, resulting in disturbances of the n-6 essential fatty acid metabolism. Peroxidation of arachidonic acids leads to formation of 4hydroxynonenal, which impairs glutamate transport and mitochondrial function in neurons and mediates oxidative stressinduced neuronal apoptosis. Essential fatty acid desaturation contributes to reductions in peripheral NCV and blood flow [39]. The fatty acid imbalance can be corrected by dietary supplementation with -linolenic acid (GLA)rich oils such as evening primrose oil [39]. In clinical studies, substitution with GLA had beneficial effects on NCV, paresthesias, and numbness, but not on neuropathic pain. Synergistic effects between GLA and aldose reductase inhibitors or GLA and antioxidants have been described [40]. Metabolic changes Brownlee [41] has demonstrated hyperglycemia-induced superoxide overproduction by the mitochondrial electron transport chain as an integrator of various metabolic changes contributing to the development of DN. Intracellular glucose oxidation during glycolysis results in NADH production, which donates reduction equivalents to the mitochondrial respiratory chain. The electron flow through the mitochondrial respiratory chain is triggered by four inner membraneassociated multi-enzyme complexes (complex IIV), cytochrome C, and the mobile electron carrier ubiquinone, and results in a potential difference at the inner mitochondrial
456
Microvascular ComplicationsNeuropathy
membrane that provides energy for adenosine triphosphate production. A high mitochondrial membrane potential results in increased half-life of the superoxide (O2-)-producing electron transport systems and promotes the production of ROS. One mechanism by which the mitochondrial-derived superoxides induce metabolic changes is by inhibition of glyceraldehyde-3-phosphate dehydrogenase (GAPDH) [41]. During glycolysis glucose is converted via glucose-6phosphate, fructose-6-phosphate, and fructose-1,6-biphosphate to form the triose glyceraldehyde-3-phosphate. The latter is oxidized by GAPDH to form 1,3-diphosphoglycerate using NAD + as substrate. An excess of superoxide and consumption of NAD+ due to an excess of NADH reduces GAPDH activity [41]. Inhibition of GAPDH results in accumulation of upstream metabolites, which are metabolized in pathways of glucose overutilization. These are 1) extrahepatic conversion of glucose to fructose by the polyolpathway, 2) increased flux of fructose-6-phosphate through the hexosamine pathway, 3) increased de novo synthesis of diacylglycerol, a cofactor of protein kinase C (PKC) from dihydroxyacetonphosphate, and 4) increased formation of reactive intracellular AGEs from accumulating trioses. Because an excessive activation of the polyol pathway increased PKC activation and increased AGE formation is supposed to contribute to the development of DN, this model implicates that controlling excessive oxidative stress may, at least in part, restore the metabolic and vascular imbalance observed in DN.
tion, mice with no or low polyol pathway activity still develop functional and structural DN [43]. Although no in vivo studies have demonstrated a direct inhibition of the polyol pathway by antioxidants, there is increasing evidence that excessive activation of AR may promote cellular oxidative stress. Transgenic mice overexpressing AR in Schwann cells show a significant reduction of glutathione in the sciatic nerves of AR transgenic mice [44]. Thus, excessive AR activation may deplete the antioxidant defense most probably through competing for NADPH, which is needed to recycle reduced glutathione from its oxidized form and to produce NO from arginine and oxygen. Consistently, the AR inhibitor sorbinil has been shown to restore reduced glutathione and ascorbate levels and arrest the diabetes-induced lipid peroxidation in early EDN [45]. Remarkably, this report postulates that only high concentrations of AR inhibitors able to completely inhibit increased sorbitol pathway activity are effective to reverse functional and metabolic deficits in DN; this suggests that problems with efficacy and toxicity of AR inhibitors in most of the clinical trials resulted from either inadequate doses and insufficient inhibition of the sorbitol pathway activity or unacceptably high systemic toxicity [45].
Oxidative Stress As an Integrator of Metabolic Changes
Increased polyol pathway activity Hyperglycemia increases the glucose flux through the polyol pathway, particularly in neuronal tissues, characterized by an insulin-independent glucose uptake. Neuronal tissues highly express the enzymes aldose reductase (AR) and sorbitol dehydrogenase catalyzing the conversion from glucose to fructose. It is thought that an increased flux through the polyol pathway promotes a cellular redox imbalance. Depletion of myo-inositol, reduced Na+,K+ ATPase activity, reduced glutathione and NO synthesis, and increased PKC activity have been identified as critical changes secondary to enhanced AR activity. The exact role of AR activation and sorbitol accumulation in DN, however, is still not clear. Sorbitol-dehydrogenase inhibitors do not show any beneficial effect on nerve function, whereas animal models demonstrate correction of decreased conduction velocity by AR inhibitors [42]. However, the efficacy and specificity of AR inhibitors in both experimental and clinical trials is still discussed controversially, particularly because studies in giant cell arteritis imply that AR may represent an oxidative defense mechanism able to neutralize the toxic effects of lipid peroxidation. In addi-
PKC activation In cells and tissues that take up glucose independently of insulin, PKC is activated by a hyperglycemia-dependent increase in diacylglycerol. In contrast to other tissues, however, diacylglycerol levels are reduced in diabetic nerves and a consistent pattern of change in PKC activity has not been observed [46]. However, PKC activation results in multiple changes in the vasculature, such as increased vascular permeability, altered vascular blood flow, modulation of NO, and activation of NF-B and NF-Bdependent gene expression, resulting in increased leukocyte adhesion. Consistently, inhibition of PKC with LY333531 (ruboxistaurin) corrected the reduced nerve blood flow and improved NCV in rat models of EDN [6]. Ongoing first clinical trials indicate that PKC inhibitors could form a basis for therapeutic intervention in DN [47]. Advanced glycation end products Advanced glycation end products are the result of nonenzymatic glycation and glycoxidation processes, which are enhanced with concomitant hyperglycemia, oxidant stress, carbonyl stress, and delayed macromolecular turnovers. Extensive intra- and extracellular accumulation of AGEs, in particular carboxymethyllysine, has been described in perineural basal laminae, axons, Schwann cells, endoneurial and epineurial microvessels, and the perineurium of human diabetic subjects [48]. An association between diabetes and AGE accumulation in peripheral nerves is also provided by the observation that AGEs in the sciatic nerve of diabetic rats were decreased by pancreatic islet cell transplantation [48]. Furthermore, AGE immunoreactivity
New Treatments for Diabetic Neuropathy: Pathogenetically Oriented Treatment Bierhaus et al.
457
increased with diabetes and correlated with a reduction in myelinated fiber density in EDN [48]. The functional consequences of AGEs deposition, however, are still poorly understood. AGE formation preferentially occurs on long-lived proteins such as myelin, where it promotes the myelin uptake by macrophages and subsequent demyelinization, and extracellular matrix proteins, thereby altering permeability, cell interaction, and cell adhesion. Intracellular-formed AGEs influence the assembly of the cytoskeleton, promote protein aggregation, and modify nuclear proteins and nucleic acids. Several inhibitors of AGE formation such as aminoguanidine, OPB-9195, and pyridoxamine have been demonstrated to reduce AGE accumulation in diabetic rats and to improve NCV and morphometric parameters in EDN [48]. In contrast, in a type 1 baboon model aminoguanidine did not restore conduction velocity or autonomic dysfunction [48]. Recent studies demonstrate that ligation of AGEs to their surface receptor RAGE perpetuates activation of the redox-sensitive transcription factor NF- B in cultured endothelial and neuronal cells [49]. Because RAGE is expressed in both vascular and neuronal tissue, it is likely that RAGE-dependent NF-B activation may promote neuronal dysfunction [50]. However, direct proof for AGE- or RAGE-mediated impairment of neuronal function is missing. Ongoing experiments with recently developed RAGE-/mice may provide data leading to inhibition of the AGE/ RAGE/NF-B axis as a new therapeutic option [16].
diabetes [43]. Only a minority of studies in EDN focused on autonomic neuropathy. In addition, mice models which are often favored due to the availability of knock-out, knock-in, and transgene manipulations, are difficult to interpret with respect to determination of NCV and blood flow due to the relatively short distances between measure points. Experimental studies normally focus on isolated nerves and compartments rather than on the multiple changes occurring in clinical DN. Thus, adverse effects in different cell types and in different compartments are often not noticed, resulting in a too optimistic view that cannot be confirmed by clinical trials. This may be one reason for the many unexpected side effects observed when initially promising experimental approaches enter clinical trials. Besides these considerations, it is important to better understand the time course of metabolic changes in DN to ensure that a pathogenetically oriented treatment targets certain metabolic pathways at time points where they are most vulnerable, thereby maximizing the therapeutic benefit. Ad hoc panels on end points for DN and defined criteria for assessing the neuropathy symptom score in both EDN and clinical trials are required to close the gap between promising results in EDN and its implementation into a pathogenetically oriented treatment, which will most probably consist of a combination of inhibitors targeting different pathways at different time points.
Acknowledgment Conclusions
Although a large number of studies strongly suggest overproduction of ROS as a major cause for neuronal damage and degeneration in DN, therapeutic approaches addressing these mechanisms are thus far rather disappointing. Identification of multiple pathways causing or promoting oxidative stress has not yet provided the basis for a successful pathogenetically oriented treatment of DN. One reason may be that there is still no clear definition of animal models suitable to investigate defined subgroups of DN. The majority of investigations are still using STZinduced diabetic mice and rats, which resemble type 1 diabetes. The results obtained, however, are often uncritically universalized, implicating general rather than specific mechanisms for the pathology of a specific subgroup of DN. Because at least short-term STZ models do not require insulin, they are often strikingly different from the clinical situation. Although a number of type 2 models are available, only a limited number of studies have focused on EDN in type 2 diabetes. Besides differences in the pathomechanisms of type 1 and 2 diabetes, the characteristic structural changes in DN are different and less severe in type 2 diabetes [43]. Models describing primary axonal disorders resemble the changes in type 1 diabetes, whereas those describing Schwann cell disorders are closer to type 2 This work was in part supported by grants from the Deutsche Forschungsgemeinschaft (Na 138/5-3, DFG/SFB 405 to PPN).
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: Of importance Of major importance
Vinik AI: Diabetic neuropathy: pathogenesis and therapy. Am J Med 1999, 107(2B):17S26S. 2. Feldman E: Oxidative stress and diabetic neuropathy: a new understanding of an old problem. J Clin Invest 2003, 111:431433. Discusses the need of a combination therapy for DN. 3. Cameron NE, Cotter MA: Oxidative stress and abnormal lipid metabolism in diabetic complications. In Frontiers in Animal Diabetes Research. Chronic Complications in Diabetes. Edited by Sima AAF. Amsterdam: Harwood Academic; 2000:93130. 4. Romero FJ, Monsalve E, Hermenegildo C, et al.: Oxygen toxicity in the nervous tissue: comparison of the antioxidant defense of rat brain and sciatic nerve. Neurochem Res 1991, 16:157161. 5. Coppey LJ, Gellett JS, Davidson EP, et al.: Effect of M40403 treatment of diabetic rats on endoneurial blood flow, motor nerve conduction velocity and vascular function of epineurial arterioles of the sciatic nerve. Br J Pharmacol 2001, 134:2129. 6. Cameron NE, Eaton SE, Cotter MA, Tesfaye S: Vascular factors and metabolic interactions in the pathogenesis of diabetic neuropathy. Diabetologia 2001, 44:19731988. 1.
458
Microvascular ComplicationsNeuropathy
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18. 19.
20.
21.
22.
23.
24.
25.
26. 27.
Packer L, Tritschler HJ, Wessel K: Neuroprotection by the metabolic antioxidant alpha-lipoic acid. Free Radic Biol Med 1997, 22:359378. Tutuncu NB, Bayraktar M, Varli K: Reversal of defective nerve conduction with vitamin E supplementation in type 2 diabetes: a preliminary study. Diabetes Care 1998, 21:19151918. Sadekov RA, Danilov AB, Vein AM: Diabetic polyneuropathy treatment by benfotiamine. Arzneimittelforschung 1999, 49:220224. Ziegler D, Hanefeld M, Ruhnau KJ, et al.: Treatment of symptomatic diabetic peripheral neuropathy with the anti-oxidant alpha-lipoic acid. A 3-week multicentre randomized controlled trial (ALADIN Study). Diabetologia 1995, 38:14251433. Ziegler D, Hanefeld M, Ruhnau KJ, et al.: Treatment of symptomatic diabetic polyneuropathy with the antioxidant alpha-lipoic acid: a 7-month multicenter randomized controlled trial (ALADIN III Study). ALADIN III Study Group. Alpha-Lipoic Acid in Diabetic Neuropathy. Diabetes Care 1999, 22:12961301. Ametov A, Barinov A, Dyck PJ, et al.: The sensory symptoms of diabetic polyneuropathy are improved with alpha-lipoic Acid: the SYDNEY trial. Diabetes Care 2003, 26:770776. Collins T, Cybulsky MI: NF-kappaB: pivotal mediator or innocent bystander in atherogenesis? J Clin Invest 2001, 107:255264. Purves TD, Tomlinson DR: Diminished transcription factor survival signals in dorsal root ganglia in rats with streptozotocin-induced diabetes. Ann N Y Acad Sci 2002, 973:472476. Cotter A, Cameron N: Effects of nuclear factor kappa B inhibition on neurovascular dysfunction. Diabetes 2003, 52(suppl 1):A192, P825. Bierhaus A, Haslbeck M, Humpert PM, et al.: The role of RAGE mediated NF-kB activation in diabetic neuropathy and its possible role in loss of pain perception. Diabetes 2003, 52(suppl 1): A4, OR18. Okamoto K, Martin DP, Schmelzer JD, et al.: Pro- and antiinflammatory cytokine gene expression in rat sciatic nerve chronic constriction injury model of neuropathic pain. Exp Neurol 2001, 169:386391. Machelska H, Cabot PJ, Mousa SA, et al.: Pain control in inflammation governed by selectins. Nat Med 1998, 4:14251428. Sakaue G, Shimaoka M, Fukuoka T, et al.: NF-kappa B decoy suppresses cytokine expression and thermal hyperalgesia in a rat neuropathic pain model. Neuroreport 2001, 12:20792084. Castagne V, Lefevre K, Clarke PG: Dual role of the NF-kappaB transcription factor in the death of immature neurons. Neuroscience 2001, 108:517526. Kaltschmidt B, Heinrich M, Kaltschmidt C: Stimulusdependent activation of NF-kappaB specifies apoptosis or neuroprotection in cerebellar granule cells. Neuromolecular Med 2002, 2:299309. Vincent AM, Brownlee M, Russell JW: Oxidative stress and programmed cell death in diabetic neuropathy. Ann N Y Acad Sci 2002, 959:368383. Srinivasan S, Stevens M, Wiley JW: Diabetic peripheral neuropathy: evidence for apoptosis and associated mitochondrial dysfunction. Diabetes 2000, 49:19321938. Honma H, Podratz JL, Windebank AJ: Acute glucose deprivation leads to apoptosis in a cell model of acute diabetic neuropathy. J Peripher Nerv Syst 2003, 8:6574. Bucala R, Tracey KJ, Cerami A: Advanced glycosylation products quench nitric oxide and mediate defective endothelium-dependent vasodilatation in experimental diabetes. J Clin Invest 1991, 87:432438. Chan NN, Vallance P: Hyperhomocysteinaemia and neuropathy in type 2 diabetes. Diabet Med 2001, 18:10081009. Cotter MA, Ekberg K, Wahren J, Cameron NE: Effects of proinsulin C-peptide in experimental diabetic neuropathy: vascular actions and modulation by nitric oxide synthase inhibition. Diabetes 2003, 52:18121817.
Pierson CR, Zhang W, Sima AA: Proinsulin C-peptide replacement in type 1 diabetic BB/Wor-rats prevents deficits in nerve fiber regeneration. J Neuropathol Exp Neurol 2003, 62:765779. 29. Hafer-Macko CE, Ivey FM, Gyure KA, et al.: Thrombomodulin deficiency in human diabetic nerve microvasculature. Diabetes 2002, 51:19571963. 30. Schratzberger P, Schratzberger G, Silver M, et al.: Favorable effect of VEGF gene transfer on ischemic peripheral neuropathy. Nat Med 2000, 6:405413. 31. Eaton SE, Harris ND, Ibrahim S, et al.: Increased sural nerve epineurial blood flow in human subjects with painful diabetic neuropathy. Diabetologia 2003, 46:934939. 32. Cameron NE, Cotter MA, Low PA: Nerve blood flow in early experimental diabetes in rats: relation to conduction deficits. Am J Physiol 1991, 261:E1E8. 33. Stevens EJ, Carrington AL, Tomlinson DR: Nerve ischaemia in diabetic rats: time-course of development, effect of insulin treatment plus comparison of streptozotocin and BB models. Diabetologia 1994, 37:4348. 34. Zochodne DW: Diabetic neuropathies: features and mechanisms. Brain Pathol 1999, 9:369391. 35. Malik RA, Williamson S, Abbott C, et al.: Effect of angiotensinconverting-enzyme (ACE) inhibitor trandolapril on human diabetic neuropathy: randomised double-blind controlled trial. Lancet 1998, 352:19781981. 36. Toyota T, Hirata Y, Ikeda Y, et al.: Lipo-PGE1, a new lipidencapsulated preparation of prostaglandin E1: placebo-and prostaglandin E1-controlled multicenter trials in patients with diabetic neuropathy and leg ulcers. Prostaglandins 1993, 46:453468. 37. Yuen KC, Baker NR, Rayman G: Treatment of chronic painful diabetic neuropathy with isosorbide dinitrate spray: a double-blind placebo-controlled cross-over study. Diabetes Care 2002, 25:16991703. 38. Ekberg K, Brismar T, Johansson BL, et al.: Amelioration of sensory nerve dysfunction by C-peptide in patients with type 1 diabetes. Diabetes 2003, 52:536541. 39. Cotter MA, Cameron NE: Effects of dietary supplementation with arachidonic acid rich oils on nerve conduction and blood flow in streptozotocin-diabetic rats. Prostaglandins Leukot Essent Fatty Acids 1997, 56:337343. 40. Hounsom L, Horrobin DF, Tritschler H, et al.: A lipoic acidgamma linolenic acid conjugate is effective against multiple indices of experimental diabetic neuropathy. Diabetologia 1998, 41:839843. 41. Brownlee M: Biochemistry and molecular cell biology of diabetic complications. Nature 2001, 414:813820. Describes mitochondria-derived oxidative stress as one major cause underlying late diabetic complications including DN. 42. Oates PJ: Polyol pathway and diabetic peripheral neuropathy. Int Rev Neurobiol 2002, 50:325392. 43. Sima AAF, Pierson CR: Metabolic alterations in experimental models. In Textbook of Diabetic Neuropathy. Edited by Gries FA, et al. Stuttgart, Germany: Georg Thieme-Verlag; 2003:96105. 44. Song Z, Fu DT, Chan YS, et al.: Transgenic mice overexpressing aldose reductase in Schwann cells show more severe nerve conduction velocity deficit and oxidative stress under hyperglycemic stress. Mol Cell Neurosci 2003, 23:638647. 45. Obrosova IG: How does glucose generate oxidative stress in peripheral nerve? Int Rev Neurobiol 2002, 50:335. 46. Eichberg J: Protein kinase C changes in diabetes: is the concept relevant to neuropathy? Int Rev Neurobiol 2002, 50:6182. 47. Wheeler GD: Ruboxistaurin (Eli Lilly). IDrugs 2003, 6:159163. 48. King RH: The role of glycation in the pathogenesis of diabetic polyneuropathy. Mol Pathol 2001, 54:400408. 49. Bierhaus A, Schiekofer S, Schwaninger M, et al.: Diabetesassociated sustained activation of the transcription factor nuclear factor-kappaB. Diabetes 2001, 50:27922808. 50. Schmidt AM, Stern DM: RAGE: a new target for the prevention and treatment of the vascular and inflammatory complications of diabetes. Trends Endocrinol Metab 2000, 11:368375.
28.
S-ar putea să vă placă și
- CDC Document Ebola Nigeria PDFDocument32 paginiCDC Document Ebola Nigeria PDFChikezie OnwukweÎncă nu există evaluări
- MRCP EcgDocument52 paginiMRCP EcgHasan Mahmud100% (1)
- Viral Haem Fevers Nigeria PDFDocument60 paginiViral Haem Fevers Nigeria PDFChikezie OnwukweÎncă nu există evaluări
- MDGs-SDGs2015 Toc PDFDocument10 paginiMDGs-SDGs2015 Toc PDFChikezie OnwukweÎncă nu există evaluări
- Guidelines For Dissertation FormatsDocument4 paginiGuidelines For Dissertation FormatsChikezie OnwukweÎncă nu există evaluări
- Medicine As A BusinessDocument33 paginiMedicine As A BusinessChikezie OnwukweÎncă nu există evaluări
- WHO-SEARO Snakebite Guidelines 2010Document162 paginiWHO-SEARO Snakebite Guidelines 2010Galantry Ahmad AzhariÎncă nu există evaluări
- Guidelines For Dissertation FormatsDocument4 paginiGuidelines For Dissertation FormatsChikezie OnwukweÎncă nu există evaluări
- HI76933 - Daily Meal Planning Guide - EnglishDocument5 paginiHI76933 - Daily Meal Planning Guide - EnglishChikezie OnwukweÎncă nu există evaluări
- Arafah ReviewDocument21 paginiArafah ReviewChikezie OnwukweÎncă nu există evaluări
- Tiozzo HDL Subfractions and Carotid PlaqueDocument7 paginiTiozzo HDL Subfractions and Carotid PlaqueChikezie OnwukweÎncă nu există evaluări
- Mittendorf Giant InsulinomaDocument6 paginiMittendorf Giant InsulinomaChikezie OnwukweÎncă nu există evaluări
- Adrenal Gland Disorders PDFDocument12 paginiAdrenal Gland Disorders PDFChikezie OnwukweÎncă nu există evaluări
- PSRDocument169 paginiPSRvitogbadosÎncă nu există evaluări
- Civil Service ServicomDocument71 paginiCivil Service ServicomChikezie OnwukweÎncă nu există evaluări
- Tests in EndocrinologyDocument1 paginăTests in EndocrinologyChikezie OnwukweÎncă nu există evaluări
- Guias para El Diagnostico y Tratamiento de Acromegalia AACE 2011Document44 paginiGuias para El Diagnostico y Tratamiento de Acromegalia AACE 2011Ricardo HemurÎncă nu există evaluări
- Bariatric GuidelinesDocument83 paginiBariatric Guidelinessavvy_as_98100% (1)
- Nigeria PHC TextDocument86 paginiNigeria PHC TextChikezie OnwukweÎncă nu există evaluări
- Stephens Performance of Two New AlgorithmsDocument7 paginiStephens Performance of Two New AlgorithmsChikezie OnwukweÎncă nu există evaluări
- Gender Nigeria2012Document99 paginiGender Nigeria2012Chikezie OnwukweÎncă nu există evaluări
- Abdulraheem Et Al PHC in NigeriaDocument9 paginiAbdulraheem Et Al PHC in NigeriaChikezie OnwukweÎncă nu există evaluări
- Hassan Doing A Pilot StudyDocument4 paginiHassan Doing A Pilot StudyChikezie OnwukweÎncă nu există evaluări
- Association Between Glycaemic Control and Erectile Dysfunction PDFDocument2 paginiAssociation Between Glycaemic Control and Erectile Dysfunction PDFAlmira Shabrina SaraswatiÎncă nu există evaluări
- Kahaly Polyglandular Autoimmune SyndromesDocument10 paginiKahaly Polyglandular Autoimmune SyndromesChikezie OnwukweÎncă nu există evaluări
- Clinical Guideines For The MGT of DsdsDocument73 paginiClinical Guideines For The MGT of DsdsChikezie OnwukweÎncă nu există evaluări
- Canadian Lipid Guidelines Update: FacultyDocument4 paginiCanadian Lipid Guidelines Update: FacultyChikezie OnwukweÎncă nu există evaluări
- Maurice Nicoll The Mark PDFDocument4 paginiMaurice Nicoll The Mark PDFErwin KroonÎncă nu există evaluări
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Francisco GS Conference March 2022Document69 paginiFrancisco GS Conference March 2022SamuelÎncă nu există evaluări
- TetanusDocument7 paginiTetanusallah akbarÎncă nu există evaluări
- Full Download Book Medical Epigenetics PDFDocument41 paginiFull Download Book Medical Epigenetics PDFandrew.lindsey981100% (14)
- Safety Seal Certification ChecklistDocument2 paginiSafety Seal Certification ChecklistKathlynn Joy de GuiaÎncă nu există evaluări
- 2 AleDocument10 pagini2 AleAna María ReyesÎncă nu există evaluări
- LeptospirosisDocument35 paginiLeptospirosisJep ValentinÎncă nu există evaluări
- M1 All ProgramsDocument26 paginiM1 All ProgramsDaisy Joy MBardz100% (1)
- EUOGS OSCE Booklet 2020Document26 paginiEUOGS OSCE Booklet 2020Amanda Leow100% (1)
- 701 1941 1 SMDocument6 pagini701 1941 1 SMANNISA DAMAYANTIÎncă nu există evaluări
- Flagile X SyndromeDocument2 paginiFlagile X Syndromeapi-314093325Încă nu există evaluări
- 2023 Projects Microbiology-Hons-BookletDocument56 pagini2023 Projects Microbiology-Hons-Bookletchand198Încă nu există evaluări
- The Significance of Immunization in The Prevention of Childhood Killer DiseasesDocument69 paginiThe Significance of Immunization in The Prevention of Childhood Killer DiseasesUsman Ahmad Tijjani100% (1)
- Local AnestheticDocument4 paginiLocal AnestheticAndrea TrescotÎncă nu există evaluări
- Olive, D. L., & Pritts, E. A. (2001) - Treatment of Endometriosis. The New England Journal of Medicine, 345 (4), 266-275.Document11 paginiOlive, D. L., & Pritts, E. A. (2001) - Treatment of Endometriosis. The New England Journal of Medicine, 345 (4), 266-275.Hernando Rivera-DuqueÎncă nu există evaluări
- Ma. Lammatao: Trion AKG Marble LLCDocument11 paginiMa. Lammatao: Trion AKG Marble LLCNasir AhmedÎncă nu există evaluări
- Fauci Dossier Valentine S Day Document 2022 (1) SummaryDocument5 paginiFauci Dossier Valentine S Day Document 2022 (1) SummarySherri StreightÎncă nu există evaluări
- Leung 2019Document10 paginiLeung 2019Ari KurniawanÎncă nu există evaluări
- Granulomatous Mastitis: The Histological Differentials: Click To Edit Master Subtitle StyleDocument13 paginiGranulomatous Mastitis: The Histological Differentials: Click To Edit Master Subtitle StyleAsmara SyedÎncă nu există evaluări
- Tosoh Series 2147Document3 paginiTosoh Series 2147ShahinÎncă nu există evaluări
- Script Roleplay KonselingDocument4 paginiScript Roleplay KonselingVella MerytaÎncă nu există evaluări
- Instrument Cleaning ProgramDocument6 paginiInstrument Cleaning ProgramGood M ArifinÎncă nu există evaluări
- T2 Sains KSSM (Section B &C)Document15 paginiT2 Sains KSSM (Section B &C)Azreen Syazwani Azmi100% (1)
- Module 6 Gram Staining PreLabDocument24 paginiModule 6 Gram Staining PreLabcloudÎncă nu există evaluări
- Literature Review Low Birth WeightDocument4 paginiLiterature Review Low Birth Weightc5qx9hq5100% (1)
- Self Care Management and Puberty Health IssuesDocument10 paginiSelf Care Management and Puberty Health IssuesIan Atienza0% (1)
- General Population (No Diabetes or CKD) Diabetes or CKD PresentDocument2 paginiGeneral Population (No Diabetes or CKD) Diabetes or CKD PresentLalu Ranova100% (1)
- Mean Alt Üst SD Range Mean Alt Üst SD Range Mean Alt Üst SD Mean Alt Üst SD FaktörDocument5 paginiMean Alt Üst SD Range Mean Alt Üst SD Range Mean Alt Üst SD Mean Alt Üst SD FaktörZeynep DenizÎncă nu există evaluări
- HLTENN045 - HO - Physiological Changes and Affect Nursing CareDocument3 paginiHLTENN045 - HO - Physiological Changes and Affect Nursing CareChepwogen TowettÎncă nu există evaluări
- Absite January2014 ReviewDocument1.226 paginiAbsite January2014 ReviewAnnTran100% (12)
- MS2 - Neurologic Disorder My ReportDocument30 paginiMS2 - Neurologic Disorder My ReportNeil Lansang BallobanÎncă nu există evaluări