Documente Academic
Documente Profesional
Documente Cultură
Sample Mental Health Progress Note
Încărcat de
warrenronaldDescriere originală:
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Sample Mental Health Progress Note
Încărcat de
warrenronaldDrepturi de autor:
Formate disponibile
OUTPATIENT PSYCHIATRIC CLINIC 2121 Main Street Raleigh, NSW 2644 02-9291-1343
TEMPLATE MENTAL HEALTH PROGRESS NOTE
How to fill in the Progress Notes form.
Progress Note Formats Clinicians may simply write a brief summary of the session and contain information pertaining to themes discussed during the session, the clients behavior, the process or interactions between clinicians and client, and plans or goals for future sessions. Another popular format is the SOAP outline. SOAP is an acronym for the sections of a clinical note: S = Subjective (The counselor describes his/her impressions of the client, and what the therapist understood the client to say) Mr. Apgar reported that he is sleeping 2-3 hours a night. He noted feeling sad, crying intermittently, and having suicidal ideation. O = Objective (A factual account of what was observed) Mr. Apgar appeared lethargic. He rarely made eye-contact. His affect was flat, and he spoke only when queried. A= Assessment (A synthesis of the Subjective and Objective portion of the note that includes diagnosis and clinical impressions) Mr. Apgar appears to be experiencing a major depressive episode. P = Plan (The counselor describes the treatment plan that follows from the Assessment) Mr. Apgar will be referred for a medication evaluation. He has been put on suicide watch. He will be seen again tomorrow for further assessment.
OUTPATIENT PSYCHIATRIC CLINIC 2121 Main Street Raleigh, NSW 2644 02-9291-1343
TEMPLATE MENTAL HEALTH PROGRESS NOTE
Date of Exam: Time of Exam: Patient Name: Patient Number: Subjective (The counselor describes his/her impressions of the client, and what the therapist understood the client to say)
Content of Therapy: Admissions by client about existing Therapy
Therapeutic Interventions: Therapeutic techniques used to help client.
MENTAL STATUS: Objective (A factual account of what was observed)
DIAGNOSES: Assessment (A synthesis of the Subjective and Objective portion of the note that includes diagnosis and clinical impressions) INSTRUCTIONS / RECOMMENDATIONS / PLAN: Plan (The counselor describes the treatment plan that follows from the Assessment) Link to Treatment Plan Problem: Short Term Goals: Target Date:
PROGRESS SUMMARY:
PLAN
Time spent counseling and coordinating care: Session start: Session end:
Liz Lobao, MD Electronically Signed By: Liz Lobao, RN On: 3/16/2012 3:22:34 PM
OUTPATIENT PSYCHIATRIC CLINIC 2121 Main Street Raleigh, NSW 2644 02-9291-1343
SAMPLE MENTAL HEALTH PROGRESS NOTE
Date of Exam: 3/16/2012 Time of Exam: 3:20:41 PM Patient Name: Smith, Anna Patient Number: 1000010544165 Anna shows minimal treatment response as of today. Anna continues to exhibit symptoms of a generalized anxiety disorder. Symptoms continue the same in frequency and intensity, and no significant improvement is noted. Symptoms of this disorder occur more days than not. Sleep difficulty continues unchanged. Feelings of increased muscular tension across neck and shoulders continue unchanged. Anna describes feeling irritable. Continuing difficulty concentrating is described. Feelings of fatigue are described as continuing unchanged. Medication has been taken regularly. She has to force herself to socialize with others. A fair night's sleep is described. Sleep was not continuous and not completely restful. Content of Therapy: Anna admitted to feeling overwhelmed and anxious even when completing the smallest project. Becoming easily frustrated was also discussed by the patient. "When will this jumpiness end?" Therapeutic Interventions: The main therapeutic techniques used this session involved helping to identify areas of difficulty and to develop coping skills and to manage stress. This session the therapeutic focus was on improving the patient's self-compassion. Patient will make positive statements regarding self and the ability to cope with the stresses of life. MENTAL STATUS: Anna is irritable, distracted, and fully communicative, casually groomed, and appears anxious. She exhibits speech that is normal in rate, volume, and articulation and is coherent and spontaneous. Language skills are intact. Mood is entirely normal with no signs of depression or mood elevation. Her affect is congruent with mood. There are no signs of hallucinations, delusions, bizarre behaviors, or other indicators of psychotic process. Associations are intact, thinking is logical, and thought content is appropriate. Homicidal ideas or intentions are convincingly denied. Cognitive functioning and fund of knowledge is intact and age appropriate. Short and long term memory is intact, as is ability to abstract and do arithmetic calculations. This patient is fully oriented. Clinically, IQ appears to be in the above average range. Insight into illness is fair. Social judgment is intact. There are signs of anxiety. Anna is fidgety. DIAGNOSES: The following Diagnoses are based on currently available information and may change as additional information becomes available. Axis I:
Generalized Anxiety Disorder, 300.02 (Active)
INSTRUCTIONS / RECOMMENDATIONS / PLAN: Link to Treatment Plan Problem: Anxiety Short Term Goals: Anna will have anxiety symptoms less than 50% of the time for one month. Target Date: 4/25/2012 In addition, Anna will exhibit increased self-confidence as reported by client on a self-report 0-10 scale weekly for two months. Target Date: 5/23/2012 ---------------------No progress in reaching these goals or resolving problems was apparent today. Recommend continuing the current intervention and short term goals. It is felt that more time is needed for the intervention to work. Return 1-2 weeks or earlier if needed. 90805 (psychotherapy w. E/M services) Time spent counseling and coordinating care: 45-50 min Session start: 2:00 PM Session end: 2:50 PM Liz Lobao, MD Electronically Signed By: Liz Lobao, RN On: 3/16/2012 3:22:34 PM
S-ar putea să vă placă și
- Sample Mental Health Treatment PlanDocument3 paginiSample Mental Health Treatment PlanCordelia Kpaduwa100% (4)
- Sample Treatment Plan With Goals For Anxiety and DepressionDocument3 paginiSample Treatment Plan With Goals For Anxiety and Depressionapi-310813184100% (1)
- Sample Treatment Plan With Goals For Anxiety and DepressionDocument3 paginiSample Treatment Plan With Goals For Anxiety and Depressionمودة عثمان100% (1)
- Psychotherapy Progress NoteDocument1 paginăPsychotherapy Progress NoteArmaan Malik100% (2)
- Psychotherapy: Pune Uni SybaDocument3 paginiPsychotherapy: Pune Uni SybaPrathamananta50% (4)
- Counseling SOAP Note Depression Anxiety SampleDocument2 paginiCounseling SOAP Note Depression Anxiety SampleCordelia KpaduwaÎncă nu există evaluări
- Psychotherapy DAP NoteDocument2 paginiPsychotherapy DAP NoteMistor Williams100% (1)
- Sample Discharge SummaryDocument4 paginiSample Discharge SummaryPatient Safety My100% (2)
- Sample Progress Note #1Document2 paginiSample Progress Note #1ccefsbc100% (1)
- ASWB EXAMINATION IN SOCIAL WORK – INTERMEDIATE/MASTERS (ASWB/II): Passbooks Study GuideDe la EverandASWB EXAMINATION IN SOCIAL WORK – INTERMEDIATE/MASTERS (ASWB/II): Passbooks Study GuideEvaluare: 2 din 5 stele2/5 (1)
- Pass the LMSW Exam: A Practice Test for the ASWB Master's Level Social Work Licensing ExaminationDe la EverandPass the LMSW Exam: A Practice Test for the ASWB Master's Level Social Work Licensing ExaminationEvaluare: 5 din 5 stele5/5 (2)
- Sample Progress Note #2Document2 paginiSample Progress Note #2ccefsbc100% (1)
- Progress NoteDocument2 paginiProgress Noteapi-317614978100% (2)
- Sample Psychotherapy NoteDocument2 paginiSample Psychotherapy NoteRafael Sanchez100% (3)
- Psychiatric Assessment Report Sample - Mental Health Evaluation ExampleDocument3 paginiPsychiatric Assessment Report Sample - Mental Health Evaluation ExampleLegoabe Isaac67% (3)
- Mental Health NotesDocument21 paginiMental Health Notesbazahoor97% (33)
- DocumentDocument219 paginiDocumentmelodyfathi100% (7)
- Treatment Plan Adolescent Self EsteemDocument2 paginiTreatment Plan Adolescent Self EsteemSophie25771% (7)
- Treatment PlanDocument4 paginiTreatment Planworship himÎncă nu există evaluări
- Sample SOAP Case 72 - SchizophreniaDocument20 paginiSample SOAP Case 72 - SchizophreniaNoreen Choudhri87% (15)
- HIP Sample Psychotherapy Progress NoteDocument23 paginiHIP Sample Psychotherapy Progress NoteALELE VINCENT100% (5)
- Mental Health Treatment Plans North Western Melbourne PHNDocument14 paginiMental Health Treatment Plans North Western Melbourne PHNMeryel de los Santos100% (2)
- Full Anxiety Treatment PlanDocument15 paginiFull Anxiety Treatment PlanDoneil Jones100% (2)
- n597 Psychiatric Soap Note 2Document7 paginin597 Psychiatric Soap Note 2api-532870494Încă nu există evaluări
- Adult Standard Biopsychosocial TemplateDocument11 paginiAdult Standard Biopsychosocial Templateapi-404660807Încă nu există evaluări
- Progress Notes and Psychotherapy NotesDocument4 paginiProgress Notes and Psychotherapy Notesnure8567% (3)
- Example Dap NoteDocument5 paginiExample Dap NoteLindsey Jo Townsend80% (5)
- Mental Status ExamDocument9 paginiMental Status Exammutant90100% (6)
- LCSW Master Study GuideDocument34 paginiLCSW Master Study GuideRYAN FONTANILLA100% (4)
- Mental Health Case StudyDocument10 paginiMental Health Case Studyapi-403506258100% (1)
- 1001 Biopsychosocial Assessment (PIHP) (Handwritten)Document26 pagini1001 Biopsychosocial Assessment (PIHP) (Handwritten)Sharon Price-James100% (3)
- Treatment Plan TemplatesDocument2 paginiTreatment Plan TemplatesShalini Dass100% (3)
- Theories SummaryDocument2 paginiTheories SummaryKalin Riu95% (40)
- Taking A History of DEPRESSIONDocument3 paginiTaking A History of DEPRESSIONPrarthana Thiagarajan100% (13)
- Psychiatry EvaluationDocument3 paginiPsychiatry Evaluatione-MedTools83% (24)
- Patient Progress Note ProtocolDocument8 paginiPatient Progress Note ProtocolVito Wilfredo100% (1)
- Treatment Plan Sample PDFDocument4 paginiTreatment Plan Sample PDFRM April AlonÎncă nu există evaluări
- TX Planning For SUD v3.0Document21 paginiTX Planning For SUD v3.0daniel100% (3)
- The Psychiatric Interview - Daniel CarlatDocument473 paginiThe Psychiatric Interview - Daniel CarlatAntonio L Yang96% (27)
- NCMHCE Study Supplement PDFDocument348 paginiNCMHCE Study Supplement PDFQuincy Bennett100% (14)
- Substance Abuse Prevention and Control: Progress Note (Soap Format)Document4 paginiSubstance Abuse Prevention and Control: Progress Note (Soap Format)Odaa Bultum100% (1)
- PMHNP Ancc ReviewDocument4 paginiPMHNP Ancc ReviewEllie Mehr75% (4)
- Sample Case Conceptualization & Treatment SummaryDocument7 paginiSample Case Conceptualization & Treatment SummaryJoshua Gonsher86% (7)
- LCSW Exam 1Document25 paginiLCSW Exam 1amdetriana3729100% (3)
- Family Therapy Treatment Plan PDFDocument2 paginiFamily Therapy Treatment Plan PDFSteve0% (4)
- Nce Study Guide Theories and Helping RelationshipsDocument50 paginiNce Study Guide Theories and Helping RelationshipsLuckyNB94% (17)
- Sample Treatment Plan Anxiety: DefinitionsDocument4 paginiSample Treatment Plan Anxiety: DefinitionsSheryl Diosto100% (1)
- Psychiatric Assessment ToolDocument53 paginiPsychiatric Assessment ToolLori100% (4)
- Depressive Disorders Social Isolation/Impaired Social InteractionDocument5 paginiDepressive Disorders Social Isolation/Impaired Social InteractionYannesa S. Bantilan - Balbin100% (2)
- Nce Study GuideDocument46 paginiNce Study Guidejacosta12100% (1)
- Adolescent Psychotherapy Homework Planner by Arthur E Jongsma JR L Mark Peterson William P McInnis Z-LiborgDocument570 paginiAdolescent Psychotherapy Homework Planner by Arthur E Jongsma JR L Mark Peterson William P McInnis Z-LiborgMar Diaz Ruiz93% (15)
- Treatment PlanningDocument6 paginiTreatment PlanningMarhamah RazakÎncă nu există evaluări
- Nce Practice TestDocument58 paginiNce Practice Testdakotalake80% (10)
- n597 Psychiatric EvalDocument11 paginin597 Psychiatric Evalapi-532870494100% (1)
- Treatment MoodDis Student OutlineDocument26 paginiTreatment MoodDis Student Outlinealex_gaston_20% (1)
- Children of Mothers With Borderline Personality Disorder (BPD)Document6 paginiChildren of Mothers With Borderline Personality Disorder (BPD)curiositykillcat100% (1)
- PTSD Clinical Case ExampleDocument10 paginiPTSD Clinical Case Exampleapi-552282470Încă nu există evaluări
- Anxiety,Worry and Panic in Children and Adolescents.Overcoming Anxiety using CBT informed ApproachesDe la EverandAnxiety,Worry and Panic in Children and Adolescents.Overcoming Anxiety using CBT informed ApproachesÎncă nu există evaluări
- NBNC 2407 CP 12 Mental Health Nursing Case StudyDocument14 paginiNBNC 2407 CP 12 Mental Health Nursing Case StudyMohamed Anwer NaleefÎncă nu există evaluări
- Nursing Process in PsychiatricDocument30 paginiNursing Process in PsychiatricEnfermería UPB Salud PúblicaÎncă nu există evaluări
- Resistor SheetDocument2 paginiResistor SheetwarrenronaldÎncă nu există evaluări
- Power Generation, Transmission & Distribution: ME 217: Energy, Environment & Society Fall 2015Document11 paginiPower Generation, Transmission & Distribution: ME 217: Energy, Environment & Society Fall 2015warrenronaldÎncă nu există evaluări
- The 4 Rs of SustainabilityDocument1 paginăThe 4 Rs of SustainabilitywarrenronaldÎncă nu există evaluări
- TL 401 UsbDocument3 paginiTL 401 UsbwarrenronaldÎncă nu există evaluări
- Microsoft Word - E003 Main QuizDocument6 paginiMicrosoft Word - E003 Main QuizwarrenronaldÎncă nu există evaluări
- Punch and Shears Machines14bDocument1 paginăPunch and Shears Machines14bwarrenronaldÎncă nu există evaluări
- Electricity Suppliers: These Exemptions Do Not Apply To The Installation of non-MEC Metering EquipmentDocument5 paginiElectricity Suppliers: These Exemptions Do Not Apply To The Installation of non-MEC Metering EquipmentwarrenronaldÎncă nu există evaluări
- TranspositionDocument9 paginiTranspositionspringpuaÎncă nu există evaluări
- ESCC Code of Conduct PolicyDocument4 paginiESCC Code of Conduct PolicywarrenronaldÎncă nu există evaluări
- Vet Electrotechnology Marking Guide 09Document12 paginiVet Electrotechnology Marking Guide 09warrenronaldÎncă nu există evaluări
- DC Drives Princ Iple of Ope Ration and C Onstruc Tion - A Re Vie WDocument5 paginiDC Drives Princ Iple of Ope Ration and C Onstruc Tion - A Re Vie WBalasubramaniÎncă nu există evaluări
- Audit Competency Grid PTDocument40 paginiAudit Competency Grid PTwarrenronaldÎncă nu există evaluări
- Brushed DC Motor FundamentalsDocument10 paginiBrushed DC Motor Fundamentalsgeorgescribd1103Încă nu există evaluări
- Weighted Average in ExcelDocument4 paginiWeighted Average in ExcelwarrenronaldÎncă nu există evaluări
- Your Personal NewspaperDocument7 paginiYour Personal NewspaperwarrenronaldÎncă nu există evaluări
- Understanding The P-N JunctionDocument21 paginiUnderstanding The P-N JunctionwarrenronaldÎncă nu există evaluări
- Understanding The P-N JunctionDocument21 paginiUnderstanding The P-N JunctionwarrenronaldÎncă nu există evaluări
- Solar CellDocument5 paginiSolar CellpurushothamkrÎncă nu există evaluări
- 1102108Document32 pagini1102108warrenronaldÎncă nu există evaluări
- TPT (Lehrman) WorkEnergyDocument4 paginiTPT (Lehrman) WorkEnergywarrenronaldÎncă nu există evaluări
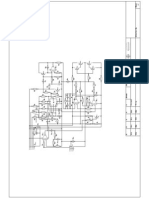
- Schematic Design - Analogue CircuitDocument1 paginăSchematic Design - Analogue CircuitwarrenronaldÎncă nu există evaluări
- How To Use Wordpress ThemesDocument9 paginiHow To Use Wordpress ThemeswarrenronaldÎncă nu există evaluări
- Heavy Vehicle Driver HandbookDocument136 paginiHeavy Vehicle Driver HandbookwarrenronaldÎncă nu există evaluări
- Management NotepadDocument1 paginăManagement NotepadwarrenronaldÎncă nu există evaluări
- Direct and Diffuse Components of Daylight: 800 To 900 600 To 800 300 To 700 250 To 400 200 To 300 100 To 200 20 To 100Document25 paginiDirect and Diffuse Components of Daylight: 800 To 900 600 To 800 300 To 700 250 To 400 200 To 300 100 To 200 20 To 100warrenronaldÎncă nu există evaluări
- Daylight Calculations Worked ExamplesDocument12 paginiDaylight Calculations Worked ExampleswarrenronaldÎncă nu există evaluări
- Product Specification Bulletin: Pulse Start 250 WattDocument1 paginăProduct Specification Bulletin: Pulse Start 250 WattwarrenronaldÎncă nu există evaluări
- Air Fin Cooler Discharge Temperature Control OptionsDocument13 paginiAir Fin Cooler Discharge Temperature Control OptionsMuhammad ImranÎncă nu există evaluări
- Waldram C - 4Document6 paginiWaldram C - 4warrenronald100% (1)
- Pharmacist-Question-paper-MPSC-Maharastra-MH-2023 (2) - Final - Google Docs 2Document26 paginiPharmacist-Question-paper-MPSC-Maharastra-MH-2023 (2) - Final - Google Docs 2Barkha MakhijaÎncă nu există evaluări
- Working With Physicians: A Massage Therapist'S GuideDocument13 paginiWorking With Physicians: A Massage Therapist'S GuideRumÎncă nu există evaluări
- History of PsychoAnalysisDocument32 paginiHistory of PsychoAnalysisMich RamÎncă nu există evaluări
- 6 DepressionDocument42 pagini6 DepressionEIorgaÎncă nu există evaluări
- Stephen Brooks and The Art of Compassionate Ericksonian Hypnotherapy: An Ericksonian Guide. Volume I: Phobias - Counselling & Advice ServicesDocument6 paginiStephen Brooks and The Art of Compassionate Ericksonian Hypnotherapy: An Ericksonian Guide. Volume I: Phobias - Counselling & Advice ServicesmedezyboÎncă nu există evaluări
- Prescription WritingDocument28 paginiPrescription WritingEshana AryaÎncă nu există evaluări
- Ge 110 Drug EducationDocument20 paginiGe 110 Drug EducationRojelu BurdeosÎncă nu există evaluări
- Isha Rejuvenation - Tamil Brochure - Siddha MedicinesDocument8 paginiIsha Rejuvenation - Tamil Brochure - Siddha MedicinesSuresh MuthusamyÎncă nu există evaluări
- CDER 2022 Guidance Agenda Half Year - July 2022Document6 paginiCDER 2022 Guidance Agenda Half Year - July 2022Aria SharifiÎncă nu există evaluări
- Health Approaches Mcqs PDFDocument10 paginiHealth Approaches Mcqs PDFTaonga Zulu100% (3)
- MDS3 Ch45 HospitalPharmacyMgmt Nov2011Document17 paginiMDS3 Ch45 HospitalPharmacyMgmt Nov2011Andre SamsungÎncă nu există evaluări
- Management of Paediatric Acute Mastoiditis: Systematic ReviewDocument9 paginiManagement of Paediatric Acute Mastoiditis: Systematic ReviewAldy GeriÎncă nu există evaluări
- Therapy QuestionsDocument23 paginiTherapy QuestionshellloooÎncă nu există evaluări
- Non-Pharmacological Methods of Pain ControlDocument12 paginiNon-Pharmacological Methods of Pain ControlCecilia Delos ReyesÎncă nu există evaluări
- Listado de Precios - 17/06/2020 02:20pm: Categoría Descripción P.V.M.PDocument19 paginiListado de Precios - 17/06/2020 02:20pm: Categoría Descripción P.V.M.PJhonathan YdrogoÎncă nu există evaluări
- Six Factors Necessary For Growth in Rogerian TheoryDocument1 paginăSix Factors Necessary For Growth in Rogerian TheoryCtmanis NyerÎncă nu există evaluări
- Rile - Therapy Techniques For DepressionDocument2 paginiRile - Therapy Techniques For DepressionIah RileÎncă nu există evaluări
- Medication Use Evaluation CurrentDocument18 paginiMedication Use Evaluation CurrentintanÎncă nu există evaluări
- Pain Community Centre - Who Analgesic Ladder - 2011-03-15Document3 paginiPain Community Centre - Who Analgesic Ladder - 2011-03-15Karina WibowoÎncă nu există evaluări
- Pharmaceutical Dosage Forms PresentationDocument17 paginiPharmaceutical Dosage Forms PresentationAliÎncă nu există evaluări
- Pe and Health 10 1st Quarter Hand OutDocument2 paginiPe and Health 10 1st Quarter Hand OutRenalyn SanchezÎncă nu există evaluări
- Essential Elements Ethics Addressing Relevant QuestionDocument4 paginiEssential Elements Ethics Addressing Relevant QuestionJulius Caesar ColladoÎncă nu există evaluări
- ResumeDocument2 paginiResumeSally BlechschmidtÎncă nu există evaluări
- Mat Presentation ProvidersDocument13 paginiMat Presentation Providersapi-649066372Încă nu există evaluări
- 5014-Prescription Regulation TableDocument3 pagini5014-Prescription Regulation Tableritchelle abigail mataÎncă nu există evaluări
- Cutaneous MelanomaDocument199 paginiCutaneous MelanomahapzanimÎncă nu există evaluări
- SAALT2W Protocol 2Document8 paginiSAALT2W Protocol 2Getwel Clinic And HospitalÎncă nu există evaluări
- Kim Ngoc Nguyen (21859825) - Reflective EssayDocument1 paginăKim Ngoc Nguyen (21859825) - Reflective EssaynkngocÎncă nu există evaluări
- Assessment and Management of Delirium in Pediatric PatientsDocument7 paginiAssessment and Management of Delirium in Pediatric PatientsEunike Karamoy100% (1)
- Kompilasi Resep (Updated)Document2 paginiKompilasi Resep (Updated)Ndok LhiaÎncă nu există evaluări