Documente Academic
Documente Profesional
Documente Cultură
Adrenaline PDF
Încărcat de
karpanaiTitlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Adrenaline PDF
Încărcat de
karpanaiDrepturi de autor:
Formate disponibile
Adrenaline and Noradrenaline: Introduction
S Clare Stanford, University College London, London, UK
Introductory article
Article Contents
. Introduction . Noradrenaline and Adrenaline in the Periphery . Noradrenaline and Adrenaline in Specific Brain Pathways . Noradrenaline and Adrenaline: Storage and Synthesis . Biosynthesis of Noradrenaline . Biosynthesis of Adrenaline . Influence of Noradrenaline on Behaviour . Regulation of Autonomic Function by Noradrenaline and Adrenaline . Summary
Online posting date: 15th April 2013
Adrenaline and noradrenaline belong to a family of molecules known as catecholamines. They are both released from the adrenal gland and neurons in the central nervous system. Noradrenaline is also released from the majority of postganglionic, sympathetic neurons in the peripheral (autonomic) nervous system. Conversion of the amino acid, tyrosine, to l-3,4-dihydroxyphenylalanine is the ratelimiting step in the pathway for synthesis of both of these catecholamines. This biosynthetic pathway is regulated by several hormones and neurotransmitters, which act through intracellular messengers and help to ensure that the rate of catecholamine synthesis matches the rate of their release. Adrenaline and noradrenaline have important roles in mediating peripheral autonomic function and the maintenance of a stable internal body state (homoeostasis). In the brain, their distribution and functional interactions underlie their strong inuence on arousal state (attention/vigilance/alarm) and its integration with the autonomic system.
This article rst outlines the distribution of adrenalineand noradrenaline-releasing neurons in the brain. The biosynthesis of these neurotransmitters is described next, including the regulation of this process, which enables neurons to adapt to continually changing demands on their neurotransmitter stores. Finally, recent ideas on the function(s) of these catecholamines in the brain and periphery will be discussed. Details of all the physiological responses in various peripheral organs that follow release of adrenaline and noradrenaline from the adrenal gland and postganglionic sympathetic neurons are beyond the scope of this article. These responses are described elsewhere. See also: Adrenaline and Noradrenaline; Autonomic Nervous System; Dopamine; Endocrine System in Vertebrates
Noradrenaline and Adrenaline in the Periphery
Noradrenaline is found in most, but not all, postganglionic neurons of the sympathetic nervous system. These neurons project from autonomic ganglia in the sympathetic chain, on either side of the spinal column, to their target organs (e.g. the heart, spleen, salivary glands and smooth muscle in the vasculature and gastrointestinal tract). Chroman cells in the core (medulla) of the adrenal gland also secrete noradrenaline and adrenaline into the circulation and so these two compounds have a hormonal function that complements their role as neurotransmitters. Both neuronal and hormonal release of these catecholamines are stimulated by preganglionic cholinergic neurons. A key feature of postganglionic sympathetic neurons is the absence of specialised synaptic contacts with their target cells. It is presumed that this indicates a lack of targeted release of noradrenaline in these tissues. Instead, noradrenaline is thought to diuse through the extracellular uid before it reaches its target receptors. This process is known as volume (or nonsynaptic or extrasynaptic)
1
Introduction
Adrenaline and noradrenaline (named epinephrine and norepinephrine in the USA) are members of a class of molecules known as catecholamines (Figure 1). They are both secreted from the core (medulla) of the adrenal gland and act as neurotransmitters in the brain. Noradrenaline is also released from the majority of postganglionic sympathetic neurons in the periphery.
eLS subject area: Neuroscience How to cite: Stanford, S Clare (April 2013) Adrenaline and Noradrenaline: Introduction. In: eLS. John Wiley & Sons, Ltd: Chichester. DOI: 10.1002/9780470015902.a0000271.pub3
eLS & 2013, John Wiley & Sons, Ltd. www.els.net
Adrenaline and Noradrenaline: Introduction
OH HO HO CH CH2 NH2
(a) Catechol nucleus OH HO HO CH CH2 NH CH2
(b)
Figure 1 The chemical structure of (a) noradrenaline and (b) adrenaline.
transmission. See also: Autonomic Nervous System; Dopamine; Endocrine System in Vertebrates
Noradrenaline and Adrenaline in Specific Brain Pathways
The distribution of neurons that release noradrenaline and adrenaline was rst mapped in the 1960s using uorescence microscopy of the rat brain. This technique involves incubating freeze-dried tissues with hot formaldehyde vapour, which reacts with catecholamines to produce compounds that uoresce in ultraviolet light (uorophores). A microscope, equipped with an ultraviolet light source, is used to visualise the uorophores which serve as markers for noradrenaline- and adrenaline-releasing neurons. The cell bodies of these neurons are all conned within the pons/medulla region in the brainstem (Figure 2), but their axons project to other regions throughout the brain and spinal cord. As far as it is known, the topographical distribution of these neurons in the brainstem and other brain regions is similar in all mammalian species, including humans, but many species (e.g. the mouse) have not yet been studied systematically.
ventral to A6. Of all noradrenergic nuclei, the A6 nucleus in the pons, has received the most attention because it is the source of more than 40% of all noradrenaline-releasing neurons in the brain. In fact, neurons from this nucleus innervate almost every region of the central nervous system. These neuronal projections are distributed to dierent forebrain regions via three major ascending pathways of which the most important is the noradrenergic dorsal bundle (Figure 2). Neuronal bres projecting to the cerebellum and the spinal cord form two further pathways. See also: Cerebellum: Anatomy and Organisation; Sensory System Organization The lateral tegmental system includes the A1, A3, A5 and A7 nuclei. Neurons project from these nuclei, via the central tegmental tract, and innervate the telencephalon (particularly the septum and amygdala), diencephalon (the thalamus and all areas of the hypothalamus) and brainstem, where they innervate primarily motor and visceral (i.e. nonsensory) nuclei. There are also descending (bulbospinal) neurons that pass down the spinal cord. Most of these noradrenaline-releasing neurons in the spinal cord derive from the A5 nucleus. The dorsomedial medullary noradrenaline-containing neurons in the A2 nucleus are sometimes included in the lateral tegmental group but are often regarded as a separate system within the nucleus tractus solitarius. See also: Motor System Organization There is extensive overlap in the innervation of dierent brain areas by neurons that project from the locus coeruleus complex and lateral tegmental nuclei, but there are a few exceptions (Figure 3). For instance, neurons projecting from the locus coeruleus are the sole source of noradrenaline that is released in the frontal cortex and hippocampus. Conversely, most subregions of the hypothalamus are innervated by neurons that derive from the lateral tegmental nuclei, but certain regions of the hypothalamus (e.g. the paraventricular nucleus and, possibly, the suprachiasmatic nucleus) are innervated by neurons from both the locus coeruleus and the lateral tegmental nuclei. See also: Hippocampus; Hypothalamus
Locus coeruleus: principal collection of noradrenaline-containing neurons in the brain
Despite being the source of the majority of noradrenalinereleasing nerve terminals in the brain, the locus coeruleus is remarkably small. Even in humans, there are only approximately 14 00020 000 cell bodies in this nucleus, on each side of the brain. In most species, it is a compact, distinct nucleus, but, in humans and cats, it is relatively diuse and the noradrenergic cell bodies are scattered amongst other types of neurons. The noradrenaline-containing neurons are multipolar and have dendrites that project into pericoerulear regions (the locus coeruleus shell). The axons of noradrenaline-releasing neurons that project from the locus coeruleus form an extensive, branching network that penetrates nearly every region of
Noradrenaline
The cell bodies of noradrenaline-releasing (noradrenergic) neurons in the brainstem are found within seven distinct, bilateral clusters (nuclei). These groups of cell bodies (known as nuclei A1A7) are subdivided into the locus coeruleus complex and the lateral tegmental system. See also: Brainstem The locus coeruleus complex comprises the A6 (the nucleus locus coeruleus, proper) and the A4 (locus subcoeruleus) nuclei. The latter is a group of cells that lies
2
eLS & 2013, John Wiley & Sons, Ltd. www.els.net
Adrenaline and Noradrenaline: Introduction
Neocortex
Hippocampus
Thalamus
Cerebellum
Septum Amygdala Median forebrain bundle Hypothalamus Dorsal longitudinal fasciculus Pituitary Ventral bundl A6 C3 A2 C2 A7A5 C1 Spinal cord A1 Central tegmental tract
Dorsal bundle
Figure 2 A schematic representation of the distribution of noradrenaline-releasing neurons in the rat brain. The brainstem nuclei that contain neurones the release for neurons that release noradrenaline or adrenaline (C1-C3) are indicated, also. The main projections from the locus coeruleus (A6) are the (noradrenergic) dorsal bundle, dorsal longitudinal fasciculus and central tegmental tract. Some fibres of the dorsal bundle innervate the thalamus directly, whereas others, together with the central tegmental tract, join the medial forebrain bundle at the level of the caudal hypothalamus. This pathway then projects to many brain areas, including the amygdala nuclei, anterior thalamus, septum, olfactory areas and the neocortex. Fibres from the dorsal longitudinal fasciculus innervate the paraventricular nucleus and, possibly, the supraoptic nucleus in the hypothalamus. The medullary bundle, in which neurons from the locus coeruleus branch from the central tegmental tract, projects to the caudal medulla (not illustrated). Fibres from the central tegmental tract also descend to the spinal cord.
Locus coeruleus A4, A6, subcoeruleus
Brainstem nuclei (sensory) Hippocampus Cerebral cortex Spinal cord Cerebellum Thalamus Hypothalamus (paraventricular nucleus) Amygdala Septum Brainstem nuclei (motor) Hypothalamus (all nuclei)
Ventral tegmental nuclei A1, A3, A5, A7 (A2)
Figure 3 The distribution of neuronal projections from the locus coeruleus and lateral tegmental (noradrenaline) systems in the brain.
the central nervous system. Each neuron is thought to yield approximately 100 000 terminals. Because of this diuse network of terminals, it is still widely believed that the brain noradrenergic system lacks either temporal or spatial specicity. This was apparently supported by early reports that these neurons did not make specialised synaptic contacts with their target cells. In fact, neither of these claims is correct (Foote et al., 1983). First, the majority (more than 90%) of neurons projecting from the locus coeruleus to the cerebral cortex form specialised synaptic contacts with somatodendritic regions of their target neurons, although this might not be the case throughout the brain. Second, there is topographical organisation of neuronal projection from the locus coeruleus. For example, most (if not all) noradrenaline-containing terminals in regions of
the cerebral cortex that are concerned with the special senses derive from cell bodies located in the dorsal rostrocaudal zone of the locus coeruleus. Neurons in the ventral zone of this nucleus project to the spinal cord. Cytochemical studies, using retrograde labelling techniques, have revealed that single neurons often project to more than one brain region, even those as remotely spaced as the neocortex and the spinal cord. In general, it is the neurons in the core of the locus coeruleus that branch the most. Further functional specicity could arise from the many dierent neuroactive molecules that have been identied within the locus coeruleus. These include b-endorphin, neurophysin, neurotensin, angiotensin II, acetylcholine (muscarinic), corticotropin-releasing factor (CRF) and substance P. Some of these agents are presumed to act as cotransmitters (i.e. to undergo impulse-evoked release from neurons that also release noradrenaline), but there is no rm evidence for this. Studies that have used retrograde labelling techniques have revealed many dierent sources of neuronal input to the locus coeruleus. These include: glutamatergic and GABAergic projections from the prefrontal cortex (Jodo et al., 1998) and a prominent input from areas of the brain that have an important role in arousal (Lee et al., 2005). Other neuronal inputs include: serotonergic neurons from nuclei; glycinergic inputs from the periaquethe raphe ductal grey; and hypocretin neurons from the lateral hypothalamus. See also: Neurotransmitters; Peptide Neurotransmitters and Hormones
Adrenaline
The most important source of adrenaline is the chroman tissue in the adrenal medulla. These chroman cells are innervated by preganglionic, cholinergic neurons and so
3
eLS & 2013, John Wiley & Sons, Ltd. www.els.net
Adrenaline and Noradrenaline: Introduction
they are functionally equivalent to postganglionic sympathetic neurons. In fact, mature adrenal medullary tissue and postganglionic sympathetic neurons derive from the same embryonic cells. This explains why most of the processes that govern the synthesis storage and release of noradrenaline were rst characterised in the adrenal medulla and later found in noradrenergic neurons in the peripheral and the central nervous systems as well. Any adrenaline found in other peripheral tissues probably derives from uptake from the circulation. See also: Endocrine System in Vertebrates There are also some adrenergic neurons in the brain (Ziegler et al., 2002). Many adrenergic neuron terminals in the brain are close to capillaries and glial cells, suggesting that they have a metabolic role, or possibly interact with neuroactive cytokines (e.g. interleukin-1b). Fluorescence microscopy and cytochemical studies, using labelled antibodies for the enzyme phenylethanolamine N-methyl transferase (PNMT), have identied three main clusters of these adrenergic neurons. These are known as nuclei C1C3 and are found in the rostral medulla of the brainstem, where they overlap with the A1A3 noradrenergic nuclei (Figure 2). It is striking that the brain areas in which these cell bodies are clustered are densely innervated by neurons projecting from the thorax and abdomen. The C1 group is found within the nucleus paragigantocellularis (PGi). These adrenergic neurons innervate brain areas that are strongly linked with anxiety and the response to stress (e.g. the periaqueductal grey and hypothalamus). The C1 group of neurons also provides the major adrenergic input to the locus coeruleus. C2 neurons are located in the nucleus tractus solitarius and dorsal motor nucleus of the vagus. They innervate neither the locus coeruleus nor the periaqueductal grey. However, C2 neurons are the source of most of the adrenaline-releasing neurons that innervate the amygdala, another brain area with a key role in anxiety. The C3 group of adrenergic neurons is located within the region of the nucleus prepositus hypoglossi. Like the C1 cell cluster, these neurons project rostrally to innervate the locus coeruleus. Neurons from these three nuclei project to other brainstem regions, including forebrain areas. They also pass down the spinal cord where they modulate the function of preganglionic sympathetic neurons. It is interesting that the innervation of the amygdala by the adrenergic neurons in the C1 and C3 nuclei is mirrored by neurons that project from the central nucleus of the amygdala, which innervate the C2 nucleus but not the C1 or C3 nucleus. The arrangement of these inputs and their connections with the spinal cord suggests that adrenaline-releasing neurons have a key role in the regulation of autonomic function, especially of blood pressure. Their connections nuclei, with brain areas, such as the serotonergic raphe locus coeruleus and limbic system, also point to their involvement in synchronising emotional and autonomic responses to external and internal (interoceptive) stimuli.
4
See also: Autonomic Control; Brainstem; Limbic System; Mood Disorders; Oculomotor System; Sensors of External Conditions in Vertebrates; Somatosensory Systems
Noradrenaline and Adrenaline: Storage and Synthesis
The concentration of noradrenaline is the greatest in the neuronal terminals, where it is stored in membrane-bound vesicles of approximately 5090 nm diameter. These vesicles are the site of the nal step in noradrenaline synthesis (see below). They are assembled in the neuronal cell body and transported down the axons to the terminals. The degree to which the terminal vesicles in postganglionic sympathetic neurons are lled with noradrenaline varies from organ to organ. In general, the vesicular store is less full in sympathetic neurons that are continually (tonically) active, such as those innervating the cardiovascular system, than in those which undergo short bursts of (phasic) activity, such as salivary glands and vas deferens. Nevertheless, the steady state concentration of noradrenaline in the neuronal storage vesicles is remarkably constant for each individual peripheral organ or brain region. This is possible because, under normal conditions, the rate of synthesis of noradrenaline balances the rate at which it is released and metabolised. The mechanisms that couple these two processes have been characterised and are described below.
Biosynthesis of Noradrenaline
The primary substrate for synthesis of noradrenaline is tyrosine. This amino acid is converted into l-3,4-dihydroxyphenylalanine (l-DOPA) by the enzyme tyrosine hydroxylase. This process is the rate-limiting step of the pathway. Synthesis of noradrenaline can be increased by giving l-DOPA, which bypasses this rate-limiting step (tyrosine hydroxylation). Because l-DOPA penetrates the bloodbrain barrier, this increase in synthesis even occurs in the brain and is exploited in treatment of Parkinsons disease. The amino acid, phenylalanine, can also be converted to tyrosine by the enzyme phenylalanine hydroxylase, but this is thought not to happen unless the dietary supply of tyrosine is compromised, which is exceptional. The activity of tyrosine hydroxylase is increased by phosphorylation of the enzyme by protein kinases, which are activated by intraneuronal second-messengers (e.g. cAMP) (Dunkley et al., 2004). This phosphorylation increases the anity (i.e., reduces the KD) of tyrosine hydroxylase for its substrate and/or increases its maximal activity (Vmax). The concentration of these intracellular messengers is increased by neuronal activation, which provides a mechanism that couples acceleration of the rate of synthesis of noradrenaline with an increase in its rate of release.
eLS & 2013, John Wiley & Sons, Ltd. www.els.net
Adrenaline and Noradrenaline: Introduction
The activity of tyrosine hydroxylase is inhibited by high concentrations of noradrenaline. This end-product inhibition was thought to operate a negative feedback pathway that regulated noradrenaline synthesis and stabilised the size of the transmitter store. It is now known that this happens only under exceptional circumstances: for example, when the metabolism of noradrenaline is prevented by drugs that block monoamine oxidase, which is one of the two enzymes that metabolise noradrenaline. It is this action which makes monoamine oxidase inhibitors eective in treatments for depression. l-DOPA is converted into dopamine by the enzyme, laromatic amino acid decarboxylase (also called DOPA decarboxylase, in this context). Dopamine is another catecholamine and neurotransmitter that is found in neurons in the brain with cell bodies clustered in nuclei (A8A12), within the midbrain and hypothalamus. All catecholaminergic neurons express tyrosine hydroxylase and DOPA decarboxylase and so the two-stage conversion of tyrosine to dopamine takes place in all catecholaminereleasing neurons. Because these are both soluble enzymes, synthesis of dopamine takes place only in the cell cytoplasm. See also: Amine Neurotransmitters; Dopamine; Enzyme Activity: Control The synthesis of noradrenaline from dopamine is the next step in the pathway and involves b-hydroxylation of dopamine by the enzyme dopamine-b-hydroxylase (DbH) (Figure 4). This is a Cu2+-containing glycoprotein, which needs O2 and ascorbic acid for its catalytic activity. DbH is found in vesicles (granules) within chroman cells of the
NA Dopamine DOPA decarboxylase DOPA Adrenaline Tyrosine hydroxylase DH PNMT
adrenal medulla and in the transmitter storage vesicles in the terminals of neurons that release noradrenaline or adrenaline. Most, but not all, of the enzymes are bound to the membranes of these vesicles. The remainder is soluble enzyme conned within these organelles. There is no DbH in the neuronal cytoplasm or chroman cells and so the synthesis of noradrenaline follows uptake of dopamine into the storage vesicles. Because only those neurons that express this enzyme are capable of synthesising noradrenaline and adrenaline, its expression is used to distinguish noradrenergic and adrenergic from dopaminergic neurones in immunocytochemical studies. See also: Amine Neurotransmitters; Enzymes: General Properties The high anity of DbH for dopamine and its high Vmax (maximum velocity of conversion of substrate into product) ensure that this step in the pathway is normally not rate-limiting in the biosynthesis of noradrenaline. However, like all proteins, DbH is assembled in the neuronal cell body and is delivered to the terminals by rapid axoplasmic transport. This can take several hours or days, depending on the length of the axon. If the supply of viable vesicles is compromised (such as after bursts of intense neuronal activity), their capacity to take up dopamine from the cytoplasm for conversion into noradrenaline is diminished. Under these conditions, DbH activity can become rate limiting and, as a consequence, dopamine accumulates in the neuronal cytosol. See also: Binding and Catalysis; Enzyme Activity: Control; Substrate Binding to Enzymes The activity of DbH is strongly dependent on pH (with a maximum at pH 6.0) and is increased by anions, such as Cl , which are present inside storage vesicles and chroman granules. However, stress, or drug treatments that stimulate noradrenaline release (e.g. d-amphetamine), triggers increased synthesis of DbH enzyme. Such stimuli could recruit any of a wide range of endogenous compounds that inuence DbH gene transcription. These include glucocorticoids, oestrogens, nerve growth factor, bradykinin, cyclic adenosine monophosphate (cAMP) and gene transcription factors such as activating protein-2 (AP-2) and cAMP response element-binding protein (CREB). See also: Axonal Transport and the Neuronal Cytoskeleton
Biosynthesis of Adrenaline
Adrenaline is the methylated derivative of noradrenaline. Conversion of noradrenaline into adrenaline depends on the enzyme PNMT and so the expression of PNMT is the criterion for distinguishing the adrenaline-releasing neuronal phenotype. The richest source of PNMT is the chroman tissue of the adrenal medulla, but it is also prominent in the brain, retina and heart. It is even found in astrocytes, which are one type of specialised non-neuronal cells in the brain, known as glia. Adrenaline can also be formed from noradrenaline by a less specic enzyme, N-methyltransferase. This enzyme is prevalent in the bronchi, liver and kidney, but whether neurons in these
5
Tyrosine
Figure 4 The synthetic pathway for noradrenaline (NA) and adrenaline in neuron terminals and chromaffin cells. Tyrosine, derived from the diet, is taken up into catecholamine-secreting neurons, where it is converted into l-DOPA in the neuronal cytoplasm. After conversion of l-DOPA into dopamine, the latter is taken up into the storage vesicles, where it is converted into NA by the enzyme DbH. NA that leaks out of the vesicles is converted into adrenaline in the cytoplasm of neurons that contain PNMT. Vesicle stores of NA and adrenaline are maintained by active uptake via a protein transporter in the vesicle membrane.
eLS & 2013, John Wiley & Sons, Ltd. www.els.net
Adrenaline and Noradrenaline: Introduction
tissues actually synthesise and release adrenaline under normal conditions is not known. PNMT is a cytoplasmic enzyme that requires the methyl donor, S-adenosylmethionine (SAM), as a cofactor. Noradrenaline is the preferred endogenous substrate for PNMT, but high concentrations of noradrenaline inhibit PNMT activity. The continuous leakage of noradrenaline from the storage vesicles into the cytoplasm, down its concentration gradient, gives PNMT access to its substrate and enables the synthesis of adrenaline. However, both adrenaline and noradrenaline are substrates for the vesicle membrane-associated transporters. These are proton antiporters that return these transmitters from the cytoplasm to the storage vesicles. See also: Binding Constants: Measurement and Biological Range; Neurotransmitter Transporters Experiments carried out by Julius Axelrod, in the 1960s, showed that removal of the pituitary gland (hypophysectomy) reduced the activity of PNMT in the adrenal medulla. This nding strongly suggested that PNMT activity in the adrenal gland was increased by glucocorticoid hormones (e.g. corticosterone or cortisol), which are secreted from the adrenal cortex (shell) in response to the pituitary hormone, adrenocorticotropin. The eciency of the stimulation of PNMT activity by glucocorticoids is optimised by an intra-adrenal portal vascular system which delivers hormones secreted from the adrenal cortex directly to the adrenal medulla. It is now known that PNMT gene transcription is augmented by a brief exposure to glucocorticoids, equivalent to a dose of hormone that would be experienced during a bout of stress. Under normal conditions, activation of PNMT synthesis by glucocorticoids is probably already maximal because it is not increased in patients suering from hypercortisolaemia (as in Cushing disease). However, glucocorticoids also prevent degradation of PNMT: this process depends on the methyl donor, SAM. It is thought that SAM induces a conformational change in the PNMT protein molecule that renders it less vulnerable to proteolysis. See also: Adrenal Disease; Axelrod, Julius Other processes that increase PNMT synthesis in the adrenal medulla include activation of nicotinic and muscarinic receptors. These cholinergic receptors recruit different second messenger systems and stimulate PNMT gene expression in dierent ways. The actions of muscarinic receptors involve an intermediate early gene product, Egr-1. The mechanism underlying the stimulation of PNMT gene expression by nicotinic receptors is not certain but could involve mobilisation of intracellular Ca2+ stores or activation of the PNMT gene promotor by a novel regulatory process (nicotine-responsive element) (Evinger et al., 2005). Several hormones, such as progesterone and oestradiol, also modify the expression of gene transcription factors (Egr-1, AP-2, Sp1 and MAZ0) that inuence the synthesis of PNMT. See also: Calcium Signalling and Regulation of Cell Function; Muscarinic Acetylcholine Receptors; Nicotinic Acetylcholine Receptors; Transcriptional Gene Regulation in Eukaryotes
6
Little is known about the regulation of PNMT activity/ gene expression in the brain. However, adrenalinereleasing neurons are richly endowed with glucocorticoid receptors and, drawing parallels with the noradrenaline system, the regulation of adrenaline synthesis in neurons is likely to resemble that in the adrenal medulla.
Influence of Noradrenaline on Behaviour
A good deal of research of the role of noradrenaline in the brain has concentrated on the locus coeruleus, which has an undisputed role in modulating arousal (Berridge et al., 2012). The spontaneous ring rate of noradrenergic neurons projecting from this nucleus increases with arousal state and is greater during quiet waking (12 spikes per second) than during slow-wave sleep (0.20.5 spikes per second) and is increased still further when animals change from vegetative or consummatory behaviours (e.g. grooming or feeding) to periods of vigilance. Because the increase in the ring rate anticipates changes in arousal, neurons in the locus coeruleus are thought to be responsible for thalamocortical desynchronisation and the ensuing behavioural changes. Destruction of the locus coeruleus increases slow-wave sleep and some cells (rapid eyemovement (REM)-o cells) stop ring altogether during REM (paradoxical) sleep. Yet, it is unlikely that noradrenaline release is needed for the waking state because animals with more than a 90% lesion of noradrenalinereleasing neurons in the brain are still capable of (quiet) waking periods. See also: Sleep There is less agreement about the role of central noradrenergic neurons during waking itself (Sara, 2009). Certainly, their activity is increased by sensory stimuli and shows a characteristic brief (phasic) burst of activity followed by a quiescent period of poststimulus inhibition. Stimuli that activate these neurons include not only noxious and internal (interoceptive) stimuli but also non-noxious environmental stimuli (e.g. tones and light ashes), especially those that provoke attention to specic stimuli (e.g. approach of the experimenter). However, not all arousing stimuli activate these neurons. For instance, the sight of rats, which have been conned within a distant cage, has no eect on ring rate of neurons in the cats locus coeruleus. Yet, this is evidently an arousing stimulus. Moreover, the neuronal response, along with behavioural arousal, declines on successive presentations of a stimulus, suggesting rapid habituation. On the basis of such ndings, it was proposed that noradrenergic neurons in the locus coeruleus serve as an alarm system that helps to integrate adaptive responses to environmental challenges. See also: Sensory Systems in Vertebrates: General Overview More recently, studies using the technique in vivo microdialysis, which enables the measurement of changes
eLS & 2013, John Wiley & Sons, Ltd. www.els.net
Adrenaline and Noradrenaline: Introduction
in the concentration of extracellular noradrenaline (an index of neurotransmission), have conrmed that this is increased by a wide range of noxious and non-noxious stimuli. In the frontal cortex, the concentration of extracellular noradrenaline is even increased when rats are exposed to a conditioned (formerly neutral) cue (a tone) that signals imminent exposure to a brightly lit novel environment, which rats nd mildly aversive (McQuade and Stanford, 2000). This response echoes early electrophysiological evidence for an increase in the ring rate of neurons in the locus coeruleus when rats are exposed to a conditioned cue for footshock. Such ndings have led to the suggestion that the salience of the stimulus is the key factor. Others have argued that noradrenergic neurons respond to a change in the salience of a stimulus. More recent research has led to the attentional shift hypothesis, whereby an increase in the ring rate of noradrenaline-releasing neurons is thought to inuence cognitive performance but does not aect the learning process directly. It is proposed that the tonic activity of these neurons determines arousal, whereas phasic responses determine attentiveness (Aston-Jones et al., 2000). Moreover, the phasic response seems to depend on the underlying tonic ring rate, and the relationship between the two is described by a bell-shaped curve. As a consequence, an optimal phasic response is evident only at intermediate levels of tonic arousal. This proposal is consistent with the relationship between noradrenergic transmission in the brain and behavioural resistance to stress (Stanford, 1993). This is also thought to be described by a bell-shaped curve, such that an increase in noradrenaline transmission would augment behavioural resistance to a mild stress but diminish behavioural resistance to a severe stress. See also: Learning and Memory; Neuronal Firing Pattern Modulation Few studies have investigated the role of neurons originating in the lateral tegmental area on behaviour. It is clear that these neurons respond to concurrent (unconditioned) environmental stimuli. They are also capable of adaptive changes on repeated exposure to the stimulus; these changes possibly contribute to behavioural habituation. However, unlike the cortex, they do not develop a response to conditioned (formerly neutral) environmental stimuli (McQuade and Stanford, 2000). These regional dierences in the noradrenergic response could reect the dierent sources of noradrenergic neurons that project to these two brain areas. Thus, it seems that neurons in the locus coeruleus that innervate the frontal cortex can respond to conditioned cues, whereas neurons in the lateral tegmental system, which innervate the hypothalamus, do not. Furthermore, it is likely that noradrenergic inputs to higher brain circuits encode contextual aspects of aversive stimuli, whereas those innervating lower brain circuits are more concerned with the ight/ght response to unconditioned aversive stimuli. This proposal resembles a scheme already proposed to explain the role of dierent groups of serotonergic neurons in the response to stress and anxiety.
Regulation of Autonomic Function by Noradrenaline and Adrenaline
Each of the catecholamine nuclei in the brainstem has numerous connections with, and receives reciprocal innervation from, other brainstem nuclei as well as higher brain centres. The overall inuence of noradrenaline and adrenaline on autonomic function will depend on the net eect of all these neuronal links. Although dierent clusters of catecholaminergic neurons in the brainstem probably have dierent roles in the regulation of autonomic function, there is still no clear picture of the eects of this complex network on neuronal circuits on higher brain centres or the periphery. Reasons for this include: . Experiments investigating the regulation of autonomic function usually require anaesthesia, which disrupts autonomic control. The development of in vivo telemetry is helping to resolve this problem. . Neuronal lesions or electrical stimulation can easily disrupt the function of other neurons whose axons pass through the brain region being tested. . The coexistence, and possible corelease, of neuropeptides (e.g. galanin, neuropeptide Y and substance P) makes it extremely dicult to tease out the specic roles of catecholamines. . Central actions of noradrenaline and adrenaline can be either excitatory or inhibitory, depending on which of the many receptors for these transmitters are activated. . Release of endogenous neurotransmitters and administration of exogenous drugs are likely to activate dierent populations of receptors (i.e. synaptic versus extrasynaptic transmission). Despite these diculties, there is strong evidence that noradrenaline-releasing neurons in the A1 and A2 nuclei innervate preganglionic sympathetic neurons in the spinal cord and modulate blood pressure. The A1-noradrenergicderived neurons are thought to operate indirectly by inhibiting C1 (adrenaline releasing) neurons. A2-derived neurons possibly act indirectly. Neurons in the A2 nucleus are thought to have an important role in autonomic regulation and project to several medullary centres including the cell bodies of neurons that slow down heart rate. Neurons in the A5 and A7 nuclei mainly innervate the spinal cord and they seem to regulate the activity of preganglionic, sympathetic neurons. Stimulation of the neurons in the A5 nucleus generally reduces blood pressure, but there are marked regional dierences in the response. The A6 nucleus has a pivotal role in regulating autonomic activity and synchronising peripheral autonomic function with arousal. The ring rate of neurons in this nucleus closely parallels the activation of sympathetic neurons and inhibition of parasympathetic neurons in the periphery. This is achieved through its projections to the spinal cord and also via brain regions that maintain homoeostasis (e.g. the hypothalamus).
7
eLS & 2013, John Wiley & Sons, Ltd. www.els.net
Adrenaline and Noradrenaline: Introduction
The integration of these responses could well be the role of the PGi, which is one of the major inputs to the locus coeruleus (see above). This nucleus is thought to act as a relay between environmental stimuli and autonomic activation. Such coordination of the activity of noradrenaline neurons in the locus coeruleus and peripheral sympathetic neurons could help to synchronise cognitive and autonomic responses (Samuels and Szabadi, 2008a, b). Even less is known about the role of central adrenalinereleasing neurons in regulation of the autonomic system. The C1 cell group of neurons is a major source of projections to the spinal cord, but it is not certain that they make direct connections with preganglionic sympathetic neurons. Nevertheless, the ring rate of neurons in the C1 area is synchronised with the cardiac rhythm and these neurons are thought to have a key role in autonomic control. Most ascending pathways, particularly those from the locus coeruleus, help to regulate complex behaviours and there are parallel, indirect changes in autonomic activity. Both noradrenaline- and adrenaline-releasing neurons in the brainstem innervate the hypothalamus. The hypothalamus, in turn, has reciprocal connections with catecholamine-releasing nuclei in the medulla and helps to coordinate autonomic function. Release of noradrenaline and adrenaline in the hypothalamus inuences hormone secretion and this will cause further, secondary, changes in autonomic activity. In these ways, medullary catecholaminergic nuclei could modulate activation of the locus coeruleus and higher centres, as well as inuence the activity of sympathetic neurons. Obviously, higher centres, such as the amygdala, will inuence this process and are doubtless involved in the modulation of autonomic function by emotionally arousing stimuli. See also: Adrenaline and Noradrenaline; Hypothalamus
Summary
The distribution of noradrenaline and adrenaline in the brain and periphery suggests that these catecholamines have pivotal roles in the regulation and synchronisation of arousal and the activity of the autonomic nervous system. The neurochemical plasticity of these neurons, evidenced by the adaptive changes in the enzymic machinery for manufacturing their neurotransmitters, conrms that these neurons are capable of responding to changing demands on their functional output. The extent to which noradrenalineand adrenaline-releasing neurons are capable of functional or temporal specicity, in terms of either the stimuli that activate them or the signals they transmit to higher centres, is as yet unclear but has probably been underestimated.
Berridge CW, Schmeichel BE and Espan a RA (2012) Noradrenergic modulation of wakefulness/arousal. Sleep Medicine Reviews 16: 187197. Dunkley PR, Bobrovskaya L, Graham ME et al. (2004) Tyrosine hydroxylase phosphorylation: regulation and consequences. Journal of Neurochemistry 91: 10251043. Evinger MJ, Mathew E, Cikos S et al. (2005) Nicotine stimulates expression of the PNMT gene through a novel promoter sequence. Journal of Molecular NeuroscienceVolume: 26(1): 3955. Foote SL, Bloom FE and Aston-Jones G (1983) Nucleus locus ceruleus: new evidence of anatomical and physiological specicity. Physiological Reviews 63: 844914. Jodo E, Chiang C and Aston-Jones G (1998) Potent excitatory inuence of prefrontal cortex activity on noradrenergic locus coeruleus neurons. Neuroscience 83(1): 6379. Lee HS, Kim MA and Waterhouse BD (2005) Retrograde doublelabeling study of common aerent projections to the dorsal raphe and the nuclear core of the locus coeruleus in the rat. Journal of Comparative Neurology 481: 179193. McQuade R and Stanford SC (2000) A microdialysis study of the noradrenergic response in rat frontal cortex and hypothalamus to a conditioned cue for aversive, naturalistic environmental stimuli. Psychopharmacology (Berl) 148: 201208. Samuels ER and Szabadi E (2008a) Functional neuroanatomy of the noradrenergic locus coeruleus: its roles in the regulation of arousal and autonomic function part I: principles of functional organisation. Current Neuropharmacology 6: 235253. Samuels ER and Szabadi E (2008b) Functional neuroanatomy of the noradrenergic locus coeruleus: its roles in the regulation of arousal and autonomic function part II: physiological and pharmacological manipulations and pathological alterations of locus coeruleus activity in humans. Current Neuropharmacology 6: 254285. Sara SJ (2009) The locus coeruleus and noradrenergic modulation of cognition. Nature Reviews Neuroscience 10: 211223. Stanford SC (1993) Monoamines in response and adaptation to stress. In: Stanford SC and Salmon P (eds) Stress from Synapse to Syndrome, pp. 283321. London: Academic Press. Ziegler MG, Bao X, Kennedy BP et al. (2002) Location, development, control, and function of extraadrenal phenylethanolamine N-methyltransferase. Annals of the New York Academy of Sciences 971: 7682.
Further Reading
Brading A (1999) The Autonomic Nervous System and its Eectors. Oxford: Blackwell Science. Fillenz M (1990) Noradrenergic Neurons. Cambridge, UK: Cambridge University Press. Iversen L, Iversen S, Bloom Fe et al. (2009) Introduction to Neuropsychopharmacology. Oxford: Oxford University Press. ISBN-10: 0195380533 | ISBN-13: 978-0195380538. Steckler T, Klain NH and Reul JMHM (2005) Handbook of Stress and the Brain. Amsterdam: Elsevier. ISBN: 0-444-51822-3. Trendlenburg U and Weiner N (eds) (2012) Catecholamines II (Handbook of Experimental Pharmacology) Vol. 90/II, ISBN10: 3642735533 | ISBN-13: 978-3642735530. Heidleberg: Springer.
References
Aston-Jones G, Rajkowski J and Cohen J (2000) Locus coeruleus and regulation of behavioral exibility and attention. Progress in Brain Research 126: 165182.
eLS & 2013, John Wiley & Sons, Ltd. www.els.net
S-ar putea să vă placă și
- Mind at Rest: How Neuron Structure Evolves in the Sleep Cycle.De la EverandMind at Rest: How Neuron Structure Evolves in the Sleep Cycle.Încă nu există evaluări
- Nervous System: Khaleel Alyahya, PHD, Med King Saud University School of Medicine @khaleelyaDocument31 paginiNervous System: Khaleel Alyahya, PHD, Med King Saud University School of Medicine @khaleelyaSalem AlshahraniÎncă nu există evaluări
- Second Quarter Grade 10 - Science HANDOUT No.2 On Neurons, Reflex, Reflex Arc & Brain General Information About The Nervous SystemDocument2 paginiSecond Quarter Grade 10 - Science HANDOUT No.2 On Neurons, Reflex, Reflex Arc & Brain General Information About The Nervous SystemMartin ReaporÎncă nu există evaluări
- 5 The Nervous SystemDocument72 pagini5 The Nervous SystemNardos TesfayeÎncă nu există evaluări
- Ilmiah Reticluar FormatioDocument29 paginiIlmiah Reticluar FormatioArdiya OktamaÎncă nu există evaluări
- Assigment About NeurologyDocument5 paginiAssigment About NeurologyYola NoviyanaÎncă nu există evaluări
- Nervous TissueDocument6 paginiNervous TissueAhmed JawdetÎncă nu există evaluări
- Psy 413 ProjectDocument38 paginiPsy 413 ProjectDumebi AneneÎncă nu există evaluări
- Hphy 228Document12 paginiHphy 228moses samuelÎncă nu există evaluări
- Nerve Muscle PhysioDocument30 paginiNerve Muscle Physiopatel_hanisha06Încă nu există evaluări
- 2 NSDocument65 pagini2 NSLilaÎncă nu există evaluări
- Lab8NervousSystemLabIII Sp22 CSDocument15 paginiLab8NervousSystemLabIII Sp22 CSAnwesha SharmaÎncă nu există evaluări
- The Nervous System RECORDINGSDocument52 paginiThe Nervous System RECORDINGSKathy Angeli Bel-idaÎncă nu există evaluări
- Human Physiology From Cells To Systems 9th Edition Sherwood Solutions ManualDocument12 paginiHuman Physiology From Cells To Systems 9th Edition Sherwood Solutions ManualSamanthaStuartijgt100% (40)
- Three Main Functions:: The Nervous System Is The Master Controlling System of The BodyDocument34 paginiThree Main Functions:: The Nervous System Is The Master Controlling System of The Bodyapi-19641337Încă nu există evaluări
- Trigeminal NerveDocument39 paginiTrigeminal NerveRanjana RavindranÎncă nu există evaluări
- Work Sheet 8 The Nervous System: Structure of A NerveDocument5 paginiWork Sheet 8 The Nervous System: Structure of A NerveJapet Floyd AlipioÎncă nu există evaluări
- Macroscopic Neuroanatomy: Neuroanatomy Deals With The Structure of TheDocument14 paginiMacroscopic Neuroanatomy: Neuroanatomy Deals With The Structure of TheRoziel Anne BasaÎncă nu există evaluări
- 5 BMCDocument18 pagini5 BMCRPh FarhatainÎncă nu există evaluări
- The Nervous System 001Document35 paginiThe Nervous System 001gelisar3sÎncă nu există evaluări
- Nervous SysDocument27 paginiNervous SysHakeemat AmusaÎncă nu există evaluări
- Module 2: Physiological Basis of BehaviorDocument23 paginiModule 2: Physiological Basis of BehaviorRoxie May Theresse AbagatnanÎncă nu există evaluări
- Form and FunctionDocument7 paginiForm and FunctionMaryam IshtiaqÎncă nu există evaluări
- CHAPTER 15: NERVOUS SYSTEM, Brain and Cranial Nerve: Embryology of The BrainDocument3 paginiCHAPTER 15: NERVOUS SYSTEM, Brain and Cranial Nerve: Embryology of The BrainDyah Ayu Pratama SariÎncă nu există evaluări
- The Nervous SystemDocument51 paginiThe Nervous SystemCho NaÎncă nu există evaluări
- The Brain Stem: Location and Basic PhysiologyDocument33 paginiThe Brain Stem: Location and Basic PhysiologyMohammad AliÎncă nu există evaluări
- Neural Control and Coordination Grade 11Document30 paginiNeural Control and Coordination Grade 11Dr. Remya RanjithÎncă nu există evaluări
- 09 Nerve TissueDocument13 pagini09 Nerve TissueGovind V PÎncă nu există evaluări
- CH 7 The Nervous SystemDocument4 paginiCH 7 The Nervous Systemapi-267543553Încă nu există evaluări
- Nervous System Lab ReportDocument10 paginiNervous System Lab Reportapi-269985211Încă nu există evaluări
- Glossary of Neuroanatomy TermsDocument10 paginiGlossary of Neuroanatomy Termsmohan730463Încă nu există evaluări
- About Neuron, Glia Cells & NeurotransmitterDocument15 paginiAbout Neuron, Glia Cells & NeurotransmitterSaba Parvin HaqueÎncă nu există evaluări
- Introduction and Overview of Neuroanatomy (Presentation) Author Al Muqsith, Ervi SuminarDocument55 paginiIntroduction and Overview of Neuroanatomy (Presentation) Author Al Muqsith, Ervi Suminarsari dianitaÎncă nu există evaluări
- Nervous Anatomy Updated (PC)Document94 paginiNervous Anatomy Updated (PC)Yahya JuneydiÎncă nu există evaluări
- Acknowledgments: Gray's Anatomy, The Remarkable Work From Which Gray's Clinical Neuroanatomy IsDocument7 paginiAcknowledgments: Gray's Anatomy, The Remarkable Work From Which Gray's Clinical Neuroanatomy IsAndreea LăzăroiuÎncă nu există evaluări
- Neural Control and Coordination Notes For NEET Download PDF - pdf-20Document7 paginiNeural Control and Coordination Notes For NEET Download PDF - pdf-20Legendary KingÎncă nu există evaluări
- Pharmacology of Autonomic Nervous System 2013Document166 paginiPharmacology of Autonomic Nervous System 2013Adimera TsehayeÎncă nu există evaluări
- Group 6 - Nervous Sytem PresentationDocument157 paginiGroup 6 - Nervous Sytem PresentationNgirlÎncă nu există evaluări
- General Appearance ThalamusDocument7 paginiGeneral Appearance ThalamusYubi KimÎncă nu există evaluări
- Hornung 2010Document14 paginiHornung 2010Leandy MartinezÎncă nu există evaluări
- Nervous SystemDocument46 paginiNervous SystemIponla KarlChristianÎncă nu există evaluări
- The Nervous System Is A Complex Network of Nerves and Cells That Carry Messages To and From TheDocument18 paginiThe Nervous System Is A Complex Network of Nerves and Cells That Carry Messages To and From TheJanineLingayoCasilenÎncă nu există evaluări
- Histology - Nerve Tissue and The Nervous SystemDocument21 paginiHistology - Nerve Tissue and The Nervous SystemDan UvarovÎncă nu există evaluări
- Neuro Anatomy and Physiological Work BookDocument36 paginiNeuro Anatomy and Physiological Work Bookshair e islamÎncă nu există evaluări
- The Nervous System 2Document84 paginiThe Nervous System 2Erika MatiasÎncă nu există evaluări
- Nervous SystemDocument212 paginiNervous SystemJimvel PelayoÎncă nu există evaluări
- Group 9 Neuron Structure & FunctionDocument14 paginiGroup 9 Neuron Structure & FunctionMosesÎncă nu există evaluări
- Introduction and Organization of Nervous System: Presented by Dr. Amen FatimaDocument37 paginiIntroduction and Organization of Nervous System: Presented by Dr. Amen FatimaShanailÎncă nu există evaluări
- Costa Et Al. - adrenalineNorAdrenalineDocument45 paginiCosta Et Al. - adrenalineNorAdrenalineVanessa BorgesÎncă nu există evaluări
- Human BrainDocument44 paginiHuman BrainSri vaishnava100% (1)
- Nervous System NotesDocument6 paginiNervous System NotesAlex Whitwam100% (3)
- Basic Basal Ganglia: The Basal Ganglia Consist of Several Interconnected NucleiDocument5 paginiBasic Basal Ganglia: The Basal Ganglia Consist of Several Interconnected NucleiFakhriÎncă nu există evaluări
- #1 CNS .... ScriptDocument15 pagini#1 CNS .... ScriptHashim GhazoÎncă nu există evaluări
- Nervous System (Student Version) PDFDocument65 paginiNervous System (Student Version) PDFAlex HigginsÎncă nu există evaluări
- Nervous System BSC 20161Document45 paginiNervous System BSC 20161Arohi ParlikarÎncă nu există evaluări
- Week 004 Animal-Nervous-SystemDocument8 paginiWeek 004 Animal-Nervous-SystemMark Lorens StaanaÎncă nu există evaluări
- Nervous SystemDocument48 paginiNervous SystemSuvalari Mimi JonathanÎncă nu există evaluări
- Structure of The NeuronDocument7 paginiStructure of The NeuronSmitaÎncă nu există evaluări
- Nervous SystemDocument70 paginiNervous SystemStephen MartinÎncă nu există evaluări
- Biology of MindOK1Document120 paginiBiology of MindOK16130019037 FATCHUR RIZQI HAMZAHÎncă nu există evaluări
- NFPA Codes & Standards - 3Document1 paginăNFPA Codes & Standards - 3karpanai100% (1)
- NFPA Codes & Standards - 1Document1 paginăNFPA Codes & Standards - 1karpanaiÎncă nu există evaluări
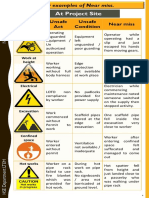
- Near Miss - Identification Made Simple en & HI - PDF-1 - 8Document1 paginăNear Miss - Identification Made Simple en & HI - PDF-1 - 8karpanaiÎncă nu există evaluări
- Near Miss - Identification Made Simple en & HI - PDF-1 - 4Document1 paginăNear Miss - Identification Made Simple en & HI - PDF-1 - 4karpanaiÎncă nu există evaluări
- Near Miss - Identification Made Simple en & HI - PDF-1 - 12Document1 paginăNear Miss - Identification Made Simple en & HI - PDF-1 - 12karpanaiÎncă nu există evaluări
- NFPA Codes & Standards - 2Document1 paginăNFPA Codes & Standards - 2karpanai100% (2)
- Fire Watcher Duties (7) - 6Document1 paginăFire Watcher Duties (7) - 6karpanaiÎncă nu există evaluări
- T1 Expose Limit PDFDocument1 paginăT1 Expose Limit PDFkarpanaiÎncă nu există evaluări
- SOP Fire Blankets PDFDocument4 paginiSOP Fire Blankets PDFkarpanaiÎncă nu există evaluări
- Chemical Engineering Science: Yanchang Wang, Fazhi Zhang, Sailong Xu, Lan Yang, Dianqing Li, David G. Evans, Xue DuanDocument7 paginiChemical Engineering Science: Yanchang Wang, Fazhi Zhang, Sailong Xu, Lan Yang, Dianqing Li, David G. Evans, Xue DuankarpanaiÎncă nu există evaluări
- Permits To Work - Scotland PDFDocument14 paginiPermits To Work - Scotland PDFFOZCANÎncă nu există evaluări
- Chemical Engineering Science: Saeikh Z. Hassan, Madhu VinjamurDocument11 paginiChemical Engineering Science: Saeikh Z. Hassan, Madhu VinjamurkarpanaiÎncă nu există evaluări
- Responsibilit Denfition PDFDocument1 paginăResponsibilit Denfition PDFkarpanaiÎncă nu există evaluări
- Form of Application For Approval of Safety Equipment For Use in MinesDocument5 paginiForm of Application For Approval of Safety Equipment For Use in MineskarpanaiÎncă nu există evaluări
- Tube Coating - ArticleDocument5 paginiTube Coating - ArticlekarpanaiÎncă nu există evaluări
- Form For Field Trial Report of Equipment-MaterialDocument22 paginiForm For Field Trial Report of Equipment-MaterialkarpanaiÎncă nu există evaluări
- No Injury-No Incident?: "Near Misses"Document15 paginiNo Injury-No Incident?: "Near Misses"Theresa West100% (1)
- Regulations & Syllabus 2016-2017Document98 paginiRegulations & Syllabus 2016-2017kannanÎncă nu există evaluări
- J Jclepro 2020 120777Document56 paginiJ Jclepro 2020 120777karpanaiÎncă nu există evaluări
- Forms For Permission Under OMR 1984Document5 paginiForms For Permission Under OMR 1984karpanaiÎncă nu există evaluări
- Application of CFD Technique To Simulate Enhanced Oil RecoveryDocument23 paginiApplication of CFD Technique To Simulate Enhanced Oil RecoverykarpanaiÎncă nu există evaluări
- A Novel Sophorolipid-Producing Candida Keroseneae GBME-IAUF-2 As A Potential Agent in Microbial Enhanced Oil Recovery (MEOR)Document8 paginiA Novel Sophorolipid-Producing Candida Keroseneae GBME-IAUF-2 As A Potential Agent in Microbial Enhanced Oil Recovery (MEOR)karpanaiÎncă nu există evaluări
- Fenton-Biostimulation Sequential Treatment of A Petroleum-Contaminated Soil Amended With Oil Palm Bagasse (Elaeis Guineensis)Document17 paginiFenton-Biostimulation Sequential Treatment of A Petroleum-Contaminated Soil Amended With Oil Palm Bagasse (Elaeis Guineensis)karpanaiÎncă nu există evaluări
- Fmicb 11 569019Document13 paginiFmicb 11 569019karpanaiÎncă nu există evaluări
- Discussion Points MAH Barriers: Date of Event: 6Document1 paginăDiscussion Points MAH Barriers: Date of Event: 6karpanaiÎncă nu există evaluări
- Adsorption Kinetics of Arsenic (V) On Nanoscale Zero-Valent Iron Supported by Activated CarbonDocument12 paginiAdsorption Kinetics of Arsenic (V) On Nanoscale Zero-Valent Iron Supported by Activated CarbonkarpanaiÎncă nu există evaluări
- Organises An: Intellectual Property Rights Awareness ProgrammeDocument1 paginăOrganises An: Intellectual Property Rights Awareness ProgrammekarpanaiÎncă nu există evaluări
- Isolation, Screening, and Crude Oil Degradation BacteriaDocument13 paginiIsolation, Screening, and Crude Oil Degradation BacteriakarpanaiÎncă nu există evaluări
- Discussion Points MAH Barriers: Date of Event: 23Document1 paginăDiscussion Points MAH Barriers: Date of Event: 23karpanaiÎncă nu există evaluări
- SFO A ParticipantsHandbookDocument336 paginiSFO A ParticipantsHandbookkarpanaiÎncă nu există evaluări
- (SUNY Series in Philosophy) William Maker-Philosophy Without Foundations - Rethinking Hegel-State University of New York Press (1994)Document329 pagini(SUNY Series in Philosophy) William Maker-Philosophy Without Foundations - Rethinking Hegel-State University of New York Press (1994)redolfiriva77Încă nu există evaluări
- HPI GuidelinesDocument5 paginiHPI GuidelinesHani NadiahÎncă nu există evaluări
- Captain Nobody CharactersDocument2 paginiCaptain Nobody CharactersAnita Shekeran AaksharanÎncă nu există evaluări
- Advantages of Living AloneDocument3 paginiAdvantages of Living AloneErika TorrenteraÎncă nu există evaluări
- Iep Case StudyDocument31 paginiIep Case Studyapi-273265436Încă nu există evaluări
- NEF Advanced SB Answer KeyDocument98 paginiNEF Advanced SB Answer KeyMaria Blasco86% (7)
- Planning A Sprint Training ProgrammeDocument5 paginiPlanning A Sprint Training ProgrammeShipra DawarÎncă nu există evaluări
- Edelman CardsDocument5 paginiEdelman CardsRussell KrizanÎncă nu există evaluări
- The SoulDocument16 paginiThe SoultaileshÎncă nu există evaluări
- Therapeutic Communication TechniquesDocument8 paginiTherapeutic Communication TechniquesPhilip Jay BragaÎncă nu există evaluări
- The ConceptDocument10 paginiThe ConceptJúlio C. Abdala FHÎncă nu există evaluări
- Lesson 5 UcspDocument15 paginiLesson 5 UcspElvie ColladoÎncă nu există evaluări
- Types of Speeches According To PurposeDocument9 paginiTypes of Speeches According To PurposeKamsa HamniÎncă nu există evaluări
- Audit Question List For ISO 9001Document21 paginiAudit Question List For ISO 9001David Phoa100% (2)
- Stages of The Listening Process ExplainedDocument3 paginiStages of The Listening Process ExplainedbmapiraÎncă nu există evaluări
- Lesson 2 Academic Writing StyleDocument23 paginiLesson 2 Academic Writing StyleDonnel AlexanderÎncă nu există evaluări
- StatisticsDocument193 paginiStatisticsSamson ScofieldÎncă nu există evaluări
- Assessment of Student Learning Basic ConceptsDocument5 paginiAssessment of Student Learning Basic Conceptsrujean romy p guisando67% (3)
- Nonmarket StrategyDocument27 paginiNonmarket StrategyMihaela GadircaÎncă nu există evaluări
- Chapter II Review of LiteratureDocument12 paginiChapter II Review of LiteratureShivank TripathiÎncă nu există evaluări
- Jealousy and The Threatened SelfDocument16 paginiJealousy and The Threatened Selfმარი ლელუაშვილიÎncă nu există evaluări
- TAT PicturesDocument83 paginiTAT PicturesAmna Shehzadi100% (7)
- Effective Early EducationDocument356 paginiEffective Early Educationekamaya28Încă nu există evaluări
- Matthew SteffensDocument2 paginiMatthew SteffensMatthew Brion SteffensÎncă nu există evaluări
- Part B: Session Plan 4 Completed With Details and AttachedDocument2 paginiPart B: Session Plan 4 Completed With Details and AttachedAAditya Shaujan PaudelÎncă nu există evaluări
- Chapter 13 Managing in A Unionized EnvironmentDocument10 paginiChapter 13 Managing in A Unionized EnvironmentLuke Thomas100% (1)
- SkilliZee Class 4 Journal Doodle Draft 3Document70 paginiSkilliZee Class 4 Journal Doodle Draft 3rashi sharmaÎncă nu există evaluări
- Performance AppraisalDocument17 paginiPerformance Appraisalemmanuel nyakiÎncă nu există evaluări
- Love and AffectionDocument1 paginăLove and AffectionStella AghenieÎncă nu există evaluări
- Likert ScaleDocument32 paginiLikert ScaleBErna Lou CezarÎncă nu există evaluări