Documente Academic
Documente Profesional
Documente Cultură
PLASMA LIPIDS 1 - in Mammals, Principal Lipids That Have Metabolic
Încărcat de
shafijan100%(2)100% au considerat acest document util (2 voturi)
42 vizualizări8 paginiPrincipal lipids that have metabolic significance are triacyl glycerol (TG) phospholipids and steroids, chief of which is cholesterol. TG derived from intestinal absorption of fats are transported in the blood as a lipoprotein complex called "chylomicrons" NEFA is now known to be metabolically most active of the PLASMA LIPIDS and 1 / 2 life being 2-3 minutes.
Descriere originală:
Titlu original
PLASMA LIPIDS 1- In Mammals, Principal Lipids That Have Metabolic
Drepturi de autor
© Attribution Non-Commercial (BY-NC)
Formate disponibile
DOC, PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentPrincipal lipids that have metabolic significance are triacyl glycerol (TG) phospholipids and steroids, chief of which is cholesterol. TG derived from intestinal absorption of fats are transported in the blood as a lipoprotein complex called "chylomicrons" NEFA is now known to be metabolically most active of the PLASMA LIPIDS and 1 / 2 life being 2-3 minutes.
Drepturi de autor:
Attribution Non-Commercial (BY-NC)
Formate disponibile
Descărcați ca DOC, PDF, TXT sau citiți online pe Scribd
100%(2)100% au considerat acest document util (2 voturi)
42 vizualizări8 paginiPLASMA LIPIDS 1 - in Mammals, Principal Lipids That Have Metabolic
Încărcat de
shafijanPrincipal lipids that have metabolic significance are triacyl glycerol (TG) phospholipids and steroids, chief of which is cholesterol. TG derived from intestinal absorption of fats are transported in the blood as a lipoprotein complex called "chylomicrons" NEFA is now known to be metabolically most active of the PLASMA LIPIDS and 1 / 2 life being 2-3 minutes.
Drepturi de autor:
Attribution Non-Commercial (BY-NC)
Formate disponibile
Descărcați ca DOC, PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 8
PLASMA LIPIDS
1- In mammals, principal Lipids that have metabolic significance are as follows:
• Triacyl glycerol (TG): also called Neutral fats (NF)
• Phospholipids and
• Steroids: chief of which is cholesterol.
Plasma lipids also constitute the products of the metabolism.
• Fatty acids: long-chain and short-chain (free FA) and
• Glycerol.
2-Extraction of plasma lipids with a suitable Lipid solvent and subsequent separation of the extract
into various classes of lipids shows the presence of:
• Triacyl glycerol (TG)
• Phospholipids (PL) Approximately in equal quantities
• Cholesterol and
• A much smaller fraction of non-esterified long-chain fatty acid (NEFA) or free-fatty acid (FFA),
which constitutes less than 5% of total FA present in plasma.
3-NEFA is now known to be metabolically most active of the plasma lipids and ½ life being 2-3
minutes.
4- Plasma lipids at any time may be considered to represent the net balance between production,
utilization and storage.
Table showing lipid fractions in plasma
Lipid fractions Plasma level in mg/100ml
Range Mean
Total lipids 360-820 560
Triacyl glycerol (TG) 80-180 150
Total Phospholipids (PL) 125-390 210
•Phosphatidyl choline 50-200
(lecithin)
•Phosphatidyl ethanolamine 50-130
(cephalin)
•Sphingomyelins 15-35
Total cholesterol 150-250 200
Free cholesterol (nonesterified) 25-105 55
Free fatty acids or nonesterified 6-16 10
FA(NEFA)
TRANSPORTATION OF PLASMA LIPIDS
Principal Lipid, triacyl glycerol (TG), is hydrophobic material. To transport them in blood in an
aqueous medium poses a problem, which is solved by associating more insoluble lipids with more
"Polar" ones, such as phospholipids, cholesterol and combining with a specific, protein molecule
(called as 'apo-proteins')- Thus, the hydrophobic and insoluble triacyl glycerol (TG) is converted by
above combination into a hydrophilic and "soluble" Lipoprotein "complex".
Thus:
• TG derived from intestinal absorption of fats are transported in the blood as a lipoprotein complex
called "chylomicrons". Chylomicrons are small microscopic particles of fats, about 1u in diameter and
are responsible for transport of exogenous (TG) in the blood.
• Similarly, TG that are synthesized in Liver cells are converted to lipoprotein particles, called "very
low density lipoproteins" (VLDL) and thrown into the circulation. VLDL is mainly concerned with
transport of endogenous TG.
In addition to above,
• Fatty acids released from adipose tissue by hydrolysis of TG are thrown in the circulation as free
fatty acid (FFA). They are carried in non-esterified state in plasma hence also called NEFA. In
circulation, FFA/ NEFA combines with albumin and are carried as "albumin-FFA complex". Some 25
to 30 mols of FFA are present in combination with one mol. of albumin.
SEPARATION OF PLASMA LIPIDS
(a) Ultracentrifugation: Pure fat is less dense than water. As the proportion of lipid to protein in
lipoprotein complex increases the density of the molecule decreases. This property has been utilized in
separation of plasma lipids, the various lipoprotein fractions, by ultracentrifugation.
Sf Unit: The rate at which each lipoprotein fraction floats up through a solution of NaCl (Sp. gr =
1.063) is expressed in "Svedberg units" (Sf units). One Sf unit is equal to 10r13 cm/sec/dyne/gm at
26°C.
Because of the low densities, the chylomicrons and VLDL rise to the surface most rapidly upon
ultracentrifugation and hence have relatively high Sf values. Composition of various Lipoprotein
fractions separated by ultracentrifugation is given in Table 21.2.
(b) Electrophoresis: Lipoproteins may be separated also according to their electrophoretic properties
and identified more accurately using immunoelectro-phoresis. Fredrickson and others (1967)
identified lipoproteins into 4 groups by electrophoresis as follows:
• HDL: moves fastest and occupies position of a globulin-called a lipoproteins
• LDL: β-lipoproteins
• VLDL: (Pre-β or α 2 lipoproteins) and
• Chylomicrons: slowest moving and remains near the origin.
Composition of lipoprotein complexes and apoproteins (Refer, Lipoproteins metabolism)
Table 21.3 shows the normal value of Lipoprotein fractions in health.
METABOLISM OF ADIPOSETISSUE
The lipids in the body physiologically exist in two forms:
• "Element constant" or structural lipids and
• "Element variable": stored lipids (Depot fats).
Although a sharpline of demarcation cannot be made between the two, it has been generally observed
that the value of the former remains constant even under extremes of starvation, whereas the latter
varies. Composition of Element Constant: Cytoplasm and cell membranes of all organs are
composed of "element constant", so that their fat content does not diminish in starvation. Element
constant is composed chiefly of Phospholipids (PL), along with smaller amounts of other lipids,
including cholesterol. It is independant of previous feeding. It remains an integral part of cell
protoplasm and is essential for its life.
Composition of Element Variable: The lipids which is stored in the body in excess of above. The
amount fluctuates and it is composed mainly of triacyl glycerol (TG), also called as neutral fats (NF).
Thus depot fat is chiefly composed of glycerides of various fatty acids and usually contains 75% of
oleic acid, 20% of palmitic acid and 5% of stearic acid. Traces of lecithin and cholesterol as well as a
little amount of Polyunsaturated FA are also present. The depot fat is called "adipose tissue", they are
intracelhilar fats which remain inside the cells of adipose tissue.
TABLE 21.3: NORMAL VALUES OF LIPOPROT (NORMAL LIPID PROFILE)
Lipid fraction
Normal value
Total cholesterol
Serum HDL—cholesterol
Serum TG (Triacyl glycerol) Serum chylomicrons
Serum pre-p lipoproteins (VLDL) Serum p-lipoproteins (LDL) "Serum LDL—cholesterol
150 to 240 mg/d males—35 to 60 female—40 to 7C males—60 to 16! females—40 to 1 up to 28 mg/dli post-absorptive males
—up to 24 females—up to', up to 550 mg/d
up to 190 mg/d
"Serum LDL—cholesterol can be calculated by the Friedeii • LDL—cholesterol in mg/dl =
T/"1
Total cholesterol—HDL cholesterol— -———
• LDL—cholesterol in m.mol/L =
TG
Total cholesterol—HDL cholesterol— —-
Note: The formula is not much reliable at TG co > 4.5 m. mol/L (> 400 mg/dl).
Dynamic State of Adipose Tissue: Adipose t just a static lump of fats; it is in "dynan breakdown of
fats and synthesis take place a
METABOLISM
TG stores in the body is continually und<
Esterification (synthesis) and (b) Lipolysis (bi
These two processes are not the forward,
processes of the same reaction. They are entinboys involving different reactants and enzymes. iyof
the nutritional, metabolic and hormonal factors ilate either of these two mechanisms, i.e., esterification
llipolysis. Resultant of these two processes determine '.magnitude of free fatty acid pool in adipose
tissue I this, in turn, will determine the level of free fatty i(FFA) circulating in the blood. Esterification
(Synthesis of TG): In adipose tissue, lor TG synthesis two substrates are required: v • AcylCoA ' a-
Glycero-P
Acyl-CoA a-Glycero-P
1
1 TG
For detailed steps see biosynthesis of TG.
, Sources ofAcyl Co A: Sources of FFA in blood are:
• Dietary,
• Synthesis of FA (palmitic acid) from acetyl CoA-'de novo' synthesis (extramitochondrial). Further
elongation to form other fatty acids in microsomes.
• Acyl CoA obtained from lipolysis taking place in
adipose tissue (FFA-Pool No. 1). ' FFA obtained from lipolysis of TG of circulating
chylomicrons and VLDL by lipoprotein lipase
enzyme present in capillary wall (FFA-Pool No.
2), which are taken up by adipose tissue. 1 Source ofa-Glycerol-P: Mainly two:
• Conversion of glycerol to a-Glycero-P by the enzyme Glycerokinase in presence of ATP.
• The other source is from glucose oxidation.
Dihydroxyacetone-P is converted to a-Glycero-P.
The enzyme glycerokinase is practically absent in
idipose tissue. If any glycerokinase is present, it has very
low activity. Hence glycerol produced by lipolysis in
idipose tissue cannot be utilized for provision of a-
Glycero-P and thus glycerol passes into the blood, from
where it is taken up by liver, kidney and other tissues
which possess glycerokinase and is utilized for
jluconeogenesis. Thus, for provision of a-glycero-P in
idipose tissue for TG. Synthesis, the tissue is dependant
wiasupply of glucose and glycolysis.
11, Lipolysis (Breakdown of TG): TG in adipose tissue
undergoes hydrolysis by a hormone-sensitive TG lipase
enzyme to form free fatty acids and glycerol.
h&polytic Upases are three:
\. "Hormone sensitive" triacyl glycerol lipase, key regulating enzyme.
2, Two others are not hormone-sensitive, > Diacyl glycerol lipase
• Monoacyl glycerol lipase.
These Upases are distinct from lipoprotein lipase that catalyzes lipoprotein TG (Present in
chylomicrons and VLDL) hydrolysis before it is taken up by extrahepatic tissues.
The free fatty acids formed by lipolysis can be reconverted in the tissue to acyl Co A by Acyl-
CoAsynthase and re-esterified with a-glycero-P to form TG. Thus, there is a continuous cycle of
lipolysis and reesterification within the tissue.
TG
Hormone sensitive TG Lipase 'a'
Diacyl glycerol + FFA
FFA
Monoacyl glycerol lipase
Diacyl glycerol lipase
Mono acyl glycerol + FFA
GLYCEROL
4 Diffuses out of plasma
Note: When the rate of re-esterification is less than rate of lipolysis, FFA accumulates and diffuses into
the plasma where it raises the level of FFA T in plasma.
Effect of Glucose: Under conditions of adequate nutritional intake or when utilization of glucose by
adipose tissue is increased, then more a-glycero-P will be available. Re-esterification will be greater
than lipolysis; as a result FFA outflow decreases and plasma FFA I level falls. In vitro studies have
shown that release of glycerol continues; that means lipolysis continues. Hence effect of glucose in
reducing plasma FFA level is not mediated by decreasing the rate of lipolysis. It proves that the effect
is due to provision of a-glycero-P from glycolysis, which enhances esterification.
Adipose tissue metabolism in Diabetes mellitus and in starvation: In diabetes mellitus and in
starvation, availability of glucose in adipose tissue is grossly reduced, resulting to lack of a-glycero-P.
Thus rate of re-esterification is decreasedl. Lipolysis is greater than re-esterification, resulting to
accumulation of FFA and increase in plasma FFA level.
INFLUENCE OF HORMONES ON ADIPOSETISSUE
Rate of release of FFA from adipose tissue, is affected by many hormones which influence either the
(a) rate of esterification or (b) the rate of lipolysis. I. List of hormones that increase the rate of esteri-
fication:
• Insulin is the principal hormone
• Prolactin effective in large doses. •.land is intact. Exact nature of the substance yet to be
kidated.
1SSIMILATION OF TGFA BY ADIPOSE TISSUE:
lajor chemical forms in which plasma lipids interact with ilipose tissue is TG.
1
As 'chylomicrons' derived from intestinal absorption of fats.
1
As "very low-density lipoprotein" complex (VLDL) by Liver.
TG of circulating chylomicrons and VLDL is acted iponby the enzyme Lipoprotein lipase to
hydrolyze TG to im FFA and glycerol. Significant correlation between ility of adipose tissue to
incorporate TG FA and the Etivity of the enzyme Lipoprotein lipase has been found IB! the activity
varies with the nutritional and hormonal •ate.Activity of lipoprotein lipase in adipose tissue is high j
the fed state and 'Low' in starvation and Diabetes idlitus.
laracteristics of Lipoprotein Lipase:
1
The enzyme lipoprotein lipase is located in, walls of blood capillaries. The enzyme remains bound to
wall byproteoglycan chains of Heparan-SO4Has been found in extracts of heart, adipose tissue,
spleen, lungs, renal medulla, aorta, diaphragm and
lactating mammary gland.
Normal blood does not contain appreciable quantities
of the enzyme.
However, following injection of Heparin lipoprotein
lipase is released from its binding with Heparan SO4
into the circulation and is accompanied by clearing of
lipaemia (hence called as "clearingfactor"). Another
lipase is also released from Liver, a hepatic lipase by
large quantities of heparin, but this enzyme has
properties different from those of lipoprotein lipase and
does not react readily with TG of chylomicrons and
VLDL.
Both phospholipids (PL) and apolipoprotein-CII are
required as cofactors for lipoprotein lipase activityApo-C-II contains a specific PL binding site
through which it is attached to the lipoprotein. Thus, the chylo-microns and VLDL provide the
enzyme for their metabolism with both its substrate and cof actors. Hydrolysis takes place while the
lipoproteins are attached to the enzyme on the endothelium. TG is progressively hydrolyzed to give
DG and then MG and finally glycerol and FFA (three molecules). Some of hydrolyzed FA return to
circulation being carried by albumin and bulk of FFA is taken up by tissues including adipose tissue
(FFA-Pool-2).
Role of Hormones: In adipose tissue, Insulin enhances the synthesis of lipoprotein lipase in adipose
tissue cells and its translocation to lumirial surface of capillary endothelium.
BROWN ADIPOSETISSUE
Types of Storage Fats: There are two types of storage fats:
• Storage "white" fat present in depot fats-predominant
• In addition to usual white storage fat, another type of "pigmented" brown fat is stored in some
species including humans.
Role in Thermogenesis:
1. Brown adipose tissue is involved in metabolism particularly at times when a heat generation is
necessary. Thus, the tissue is extremely active
• In arousal from hibernation,
• In animals exposed to cold, and
• In heat production in newborn animals. It is present in rats, throughout the life.
2. Though not a prominent tissue in humans, recently it has been shown to be active in normal
individuals, where it appears to be responsible for "diet-induced thermogenesis", which may account
for how some persons can "eat and do not get fat".
Note: It is to be noted that brown adipose tissue is reduced or may be absent in obese persons.
Location: It is located and present particulary in the thoracic region.
Characteristics of Brown Adipose Tissue: It is characterized by:
• A high content of mitochondria,
• A high content of cytochromes,
• A well-developed blood supply,
• Also relatively rich in carnitine, whid for FA oxidation,
• Unlike white adipose tissue, it ha; glycerokinase.
Note:
• The brown colour is related to a relatrv chrome content.
• There is lowATP-synthase activity.
• Oxygen consumption is high.
Metabolic Peculiarities:
1. Metabolic emphasis is on oxidativ oxidation of glucose and FA oxidatic oxidized to CO2 and H2O.
2. Nor-epinephrine liberated from symf endings is important in increasing lip tissue.
Mechanism of Heat Production:
• Oxidation and phosphorylation are n< mitochondria of this tissue. Dinitropl effect and there is no
respiratory contro
• The phosphorylation which occurs is at t level" in the glycolytic pathway and i thiokinase" step of
TCA cycle. Thus, o; duces much heat and very little free ener as ATP due to decreased coupling of o;
phosphorylation.
• In terms of chemi-osmotic theory, it app proton gradient, normally present aero mitochondrial
membrane of coupled m is continually dissipated in brown adipos thermogenic protein, called
"thermoge acts as a proton conductance pathway membrane. This explains the apparent la of
uncouplers.
Function: Brown storage fat has a somev temperature than other tissues. It plays a: production for vital
organs, serving as a sort pad" or "furnace" for the local application o the vital organs of the thorax, the
upper spin, the autonomic sympathetic chain. The amou fat increases in animals when subjected to "c
Direct measurements of heat production d stress in rats showed that brown adipose tissi for 82% of
total heat production. Study the metabolic fate of cholesterol in the body.
What are bile acids? Learn how they are formed in the body and their functions.
Study the role of cholesterol and TG in atherosclerosis and IHD.
OXIDATION OF FATTY ACIDS
Sources of Plasma FFA
Plasma free fatty acids are derived:
• Mainly from lipolysis in adipose tissue. (Pool-1)
• Portion of FFA is derived from degradation of circulating chylomicrons and VLDL by the action of the
enzyme lipoprotein lipase (Pool-2).
• A small portion of plasma FFA is derived from absorption of dietary source specially small chain and
medium chain fatty acids.
• Also FFA is obtained from synthesis from acetyl CoA in Liver cells, which are incorporated in TG.
In postabsorptive state, plasma contains 10 to 30 mg% of FFA, most of which is transported in plasma
as a loose complex with albumin, as "albumin-fFA complex" but in the cell they are attached to a fatty
acid binding protein or "Z-Protein". A small amount of FA is also associated with HDL. Shorter chain
FA are more water soluble and exist as the unionized acid or as a FA anion.
Fatty acids exhibit a very rapid turnover rate with a l/2 life of only 1 to 3 minutes, they are rapidly
taken up by tissues and metabolized. Plasma FFA is decreased by Insulin and Glucose administration.
Plasma FFA is increased by catecholamines, Growth hormone, Glucocorticoids and thyroid hormones.
Also increased in Diabetes mellitus, starvation and with high fat diets.
Methods by which fatty acids are oxidized in the body
are as follows:
A. beta-oxidation: Principal method of oxidation of FA.
Other methods are: B. alpha-oxidation, C. OMEGA-oxidation, and D. Peroxismal FA oxidation.
A. BETA-OXIDATION
Principal method by which FA are oxidized is called beta-oxidation. Several theories have been
proposed to explain the mechanism of the oxidation of FA chains. The classical theory of P-oxidation
was the outcome of the work of Knoop.
Knoop's Experiment: Tagged the -CH3 end of FA by substitution of a phenyl radical, this prevented
the complete oxidation. It resulted in urinary excretion of phenyl derivatives:
• On feeding dogs with FA with even carbon atoms,he observed that phenyl acetic acid is always is
conjugated with glycine and excreted as phenylaceturic acid.
• When FA with odd number of carbon at Benzoic acid was excreted as gly< "hippuric acid".
Conclusion: Knoop proposed the p-ox According to this mechanism FA chains. the removal of 2
carbon atoms at a time, in the p-position to COOH group is attacked with the formation of the corresf
acid; then the two terminal C-atoms are spliti CoA". A new -COOH group is formed at 1 keto (= CO)
grouping, so that a fatty acidi carbon atoms less than the original. Aga carbon atom is attacked and
two more ca split off as acetyl-CoA. In this way, the FA i the removal of 2 carbon atoms at a time, i
stage of acetoacetic acid is reached.
Tissues in which ^-Oxidation is Carried i
lating FA are taken up by various tissues, Tissues like liver, heart, kidney, muscle, bra and adipose
tissue have the ability to oxic FA. In cardiac muscle, fatty acids are an ir respiration (80% of energy
derived from F/
Enzymes Involved in ^-Oxidation: fl-oi place in mitochondrion. Several en2 collectively as EA-
oxidase system are fov chondrial matrix, adjacent to the respiratory! is found in the inner membrane.
These er the oxidation of FA to acetyl-CoA.
Activation of FA: Fatty acids are in cyt (extramitochondrial). Fatty acids must be i so that they
participate in metabolic activation requires energy which is provi presence of ATP, and coenzyme A,
the er synthetase (previously called as thiokin conversion of a free fatty acid to an 'active"!
The presence of inorganic pyrophosph activation goes to completion by facilit additional high energy
~ P bond of PPi. effect 2 - P bonds are expended during H of each FA molecule. Not only saturated
FA I FA and -OH fatty acids are also activated ZoA synthetases.
I types ofAcyl-CoASynthetases: The enzymes i the endoplasmic reticulum and inside (for and
outside (for long-chain FA) of the i. Several varieties of the enzyme have been |,each specific for
FA of different chain lengths. CoA synthetase —> acts on acetic acid and :acid
Iwifdium chain synthetase -» acts on FA with igth C4 to C12
JIM acyl-CoA synthetase ~^> Acts on FA with gth C8 to C22
a GTP-specific mitochondrial acyl-CoA ase described which forms GDP + Pi
! AND ITS ROLE IN FA METABOLISM
L (acyl-CoA) are formed in cytosol, whereas i of FA occurs in mitochondrial matrix. Acyl neable
to mitochondrial membrane. Long-ited FA penetrate the inner mitochondrial eonly in
combination with carnitine.
tChemistry and functions: s chemically "p-OH-y-trimethyl ammoniumHistorical background:
Fraenk^l's vitamin BT is same as carnitine. It was found to be required as a nutritional factor in
meal-worm (Tenebrio molitor). If the meal worms are fed on a synthetic diet, deficient in vitamin
BT they die in 4 to 5 weeks.
Distribution: Carnitine is widely distributed in yeast, milk, liver and particularly large quantities
in muscles and in meat extracts.
Concentration: Fraenkel used bio-assay technique based on the rate of growth of larvae of
Tenebrio molitor and found that in mammals, carnitine content of:
• Skeletal muscle: 1 mg/Gm dry weight
• Heart muscle: 560 mcg/Gm
• Kidneys: 412 mcg/Gm
• Liver: 280 mcg/Gm
Blood: Small amounts in blood 7-14 meg/ml. Excretion in 24 hrs urine: 50 to 100 meg/ml.
Biosynthesis of Carnitine: It is synthesized from lysine and methionine in liver principally, also in
kidneys. Synthesis of carnitine is shown below in the box.
Biosynthesis of CarnitineHistorical background: Fraenk^l's vitamin BT is same as carnitine. It
was found to be required as a nutritional factor in meal-worm (Tenebrio molitor). If the meal
worms are fed on a synthetic diet, deficient in vitamin BT they die in 4 to 5 weeks.
Distribution: Carnitine is widely distributed in yeast, milk, liver and particularly large quantities
in muscles and in meat extracts.
Concentration: Fraenkel used bio-assay technique based on the rate of growth of larvae of
Tenebrio molitor and found that in mammals, carnitine content of:
• Skeletal muscle: 1 mg/Gm dry weight
• Heart muscle: 560 mcg/Gm
• Kidneys: 412 mcg/Gm
• Liver: 280 mcg/Gm
Blood: Small amounts in blood 7-14 meg/ml. Excretion in 24 hrs urine: 50 to 100 meg/ml.
Biosynthesis of Carnitine: It is synthesized from lysine and methionine in liver principally, also in
kidneys. Synthesis of carnitine is shown below in the box.
Biosynthesis of CarnitineSuccinate
Functions: Carnitine is considered as a "carrier molecule"; it acts like a ferry-boat. It transports
long-chain acyl-CoA across mitochondrial membrane which is impermeable to acyl-CoA.
• Facilitates transport of long-chain acyl-CoA for oxidation in mitochondria.
• Facilitates exit of acetyl-CoA and acetoacetyl CoA from within mitochondria to cytosol, where
FA synthesis takes place
• Methionine-sparing action: Khairallah and Wolf (1965) found that in rats, carnitine has a
methionine-sparing action and may thus be considered a food factor required in marginal diets.
Mechanism of Transport of Long-Chain Acyl-CoA: Activation of lower FA and their oxidation
may occur within the mitochondria, independantly, of carnitine; but long-
S-ar putea să vă placă și
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Pashtun Tahafuz Movement 2019Document15 paginiPashtun Tahafuz Movement 2019shafijanÎncă nu există evaluări
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- Pakistan in 2018 Theft of An ElectionDocument10 paginiPakistan in 2018 Theft of An ElectionshafijanÎncă nu există evaluări
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- India Versus Pakistan in The Court of Global OpinionDocument6 paginiIndia Versus Pakistan in The Court of Global OpinionshafijanÎncă nu există evaluări
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- The Politics of Kartarpur Corridor and India-Pakistan RelationsDocument8 paginiThe Politics of Kartarpur Corridor and India-Pakistan RelationsshafijanÎncă nu există evaluări
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- Space Programs of India and Pakistan Military and Strategic Installations 2018Document12 paginiSpace Programs of India and Pakistan Military and Strategic Installations 2018shafijanÎncă nu există evaluări
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Pakistan Voting Under Military TutelageDocument17 paginiPakistan Voting Under Military TutelageshafijanÎncă nu există evaluări
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Pakistan's Economic Vulnerability and The US South Asia Strategy in Light of CPEC 2019Document22 paginiPakistan's Economic Vulnerability and The US South Asia Strategy in Light of CPEC 2019shafijanÎncă nu există evaluări
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Pashtun Tahafuz Movement 2019 Farooq YousafzaiDocument10 paginiPashtun Tahafuz Movement 2019 Farooq YousafzaishafijanÎncă nu există evaluări
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- Dynamics of Military Expenditure and Income Inequality in Pakistan 2017Document21 paginiDynamics of Military Expenditure and Income Inequality in Pakistan 2017shafijanÎncă nu există evaluări
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Master-s-Thesis - Muhammad-Ahsan-Jahangir Pakistan's National Identity 2010Document65 paginiMaster-s-Thesis - Muhammad-Ahsan-Jahangir Pakistan's National Identity 2010shafijanÎncă nu există evaluări
- Dependent State Security Relationship Between The Pakistani Terrorism Threat and Chinese State SecurityDocument28 paginiDependent State Security Relationship Between The Pakistani Terrorism Threat and Chinese State SecurityshafijanÎncă nu există evaluări
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- 14th TopicDocument16 pagini14th Topicusama_yasinÎncă nu există evaluări
- Occasional Paper#07: Shanghai Cooperation Organization and South Asia: Balancing ActDocument10 paginiOccasional Paper#07: Shanghai Cooperation Organization and South Asia: Balancing ActshafijanÎncă nu există evaluări
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- Mechanism of Brain Tumor HeadacheDocument5 paginiMechanism of Brain Tumor HeadacheshafijanÎncă nu există evaluări
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- Classification of Brain Tumor Types Using Multiclass Kernelbased Hellinger Decision Method For HD-Tree and HD-ForestDocument7 paginiClassification of Brain Tumor Types Using Multiclass Kernelbased Hellinger Decision Method For HD-Tree and HD-ForestshafijanÎncă nu există evaluări
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- 14th TopicDocument16 pagini14th Topicusama_yasinÎncă nu există evaluări
- Headaches in Brain Tumor Patients: Primary or Secondary?: Headache CurrentsDocument10 paginiHeadaches in Brain Tumor Patients: Primary or Secondary?: Headache CurrentsasfwegereÎncă nu există evaluări
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Hormonal Imbalance and Pituitary Adenoma During AntipsychoticDocument3 paginiHormonal Imbalance and Pituitary Adenoma During AntipsychoticshafijanÎncă nu există evaluări
- Brain Tumors Metastasis 2019Document16 paginiBrain Tumors Metastasis 2019shafijanÎncă nu există evaluări
- Hyperprolactinaemia A Guide For Psychiatrists 2017Document9 paginiHyperprolactinaemia A Guide For Psychiatrists 2017shafijanÎncă nu există evaluări
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- J.berghmans Proefschrift DigitaalDocument179 paginiJ.berghmans Proefschrift DigitaalshafijanÎncă nu există evaluări
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Chronic Atypical Depression As An Early Feature of Pituitary Adenoma 2019Document11 paginiChronic Atypical Depression As An Early Feature of Pituitary Adenoma 2019shafijanÎncă nu există evaluări
- Headaches in Brain TumorsDocument10 paginiHeadaches in Brain TumorsshafijanÎncă nu există evaluări
- Cerebral Syphilitic Gumma Mimicking A Brain TumorDocument4 paginiCerebral Syphilitic Gumma Mimicking A Brain TumorshafijanÎncă nu există evaluări
- Attitudes To Sexuality in Individuals With Mental Retardation From Perspectives of Their Parents and Teachers 2012Document13 paginiAttitudes To Sexuality in Individuals With Mental Retardation From Perspectives of Their Parents and Teachers 2012shafijanÎncă nu există evaluări
- Depression, Anxiety, and Suicidal Ideation Among Vietnamese Secondary School Students 2013Document10 paginiDepression, Anxiety, and Suicidal Ideation Among Vietnamese Secondary School Students 2013shafijanÎncă nu există evaluări
- Cyber Disorders PDFDocument6 paginiCyber Disorders PDFshafijanÎncă nu există evaluări
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Brain Tumor Location and Psychiatric SymptomsDocument9 paginiBrain Tumor Location and Psychiatric SymptomsshafijanÎncă nu există evaluări
- Nuevo Coronavirus NEJMDocument7 paginiNuevo Coronavirus NEJMSMIBA Medicina100% (1)
- Identifying Symptoms of Depression and Anxiety in Students in The School Setting 2013Document8 paginiIdentifying Symptoms of Depression and Anxiety in Students in The School Setting 2013shafijanÎncă nu există evaluări
- Current Concept of Obesity: January 2016Document17 paginiCurrent Concept of Obesity: January 2016Aria DomingoÎncă nu există evaluări
- Daftar Pustaka: 2018, Badan Penelitian Dan Pengembangan Kesehatan, KementrianDocument9 paginiDaftar Pustaka: 2018, Badan Penelitian Dan Pengembangan Kesehatan, KementrianRan NisÎncă nu există evaluări
- Body CompositionDocument110 paginiBody CompositionEvelyn PessanhaÎncă nu există evaluări
- Lesson Plan CaloriesDocument9 paginiLesson Plan Caloriesapi-353699297Încă nu există evaluări
- Obeppar Medical SlidesDocument52 paginiObeppar Medical SlidesNimesh ModiÎncă nu există evaluări
- Assessment of Obesity and Classification of Patients Historical Perspectives and Current PracticeDocument28 paginiAssessment of Obesity and Classification of Patients Historical Perspectives and Current PracticeRafi Akhtar SultanÎncă nu există evaluări
- Aqualyx Percentage - Google SearchDocument1 paginăAqualyx Percentage - Google SearchdrjoeÎncă nu există evaluări
- Bioscience Services Brochure SepDocument20 paginiBioscience Services Brochure SepsÎncă nu există evaluări
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- FN 121 SG 1Document11 paginiFN 121 SG 1BuiHopeÎncă nu există evaluări
- Belly Fat Burning PDFDocument3 paginiBelly Fat Burning PDFSunny BiswalÎncă nu există evaluări
- Dietary Balances, Regulation of Feeding, Obesity and Starvation, Vitamins & MineralsDocument62 paginiDietary Balances, Regulation of Feeding, Obesity and Starvation, Vitamins & MineralsPrixie AntonioÎncă nu există evaluări
- PosterDocument1 paginăPosterAyar HeinÎncă nu există evaluări
- Effects of A Meal Replacement On Body CompositionDocument10 paginiEffects of A Meal Replacement On Body CompositionGiffariÎncă nu există evaluări
- Genetics of Human ObesityDocument14 paginiGenetics of Human Obesitymuralidhar_mettaÎncă nu există evaluări
- Nutrition Interventions in Rheumatoid ArDocument11 paginiNutrition Interventions in Rheumatoid ArJULIETAÎncă nu există evaluări
- Neonatal ThermoregulationDocument4 paginiNeonatal Thermoregulationalicia618Încă nu există evaluări
- Mechanisms, Pathophysiology, and Management of ObesityDocument13 paginiMechanisms, Pathophysiology, and Management of ObesityJuanCarlosToledoGonzálezÎncă nu există evaluări
- Integration of MetabolismDocument51 paginiIntegration of MetabolismKaif AliÎncă nu există evaluări
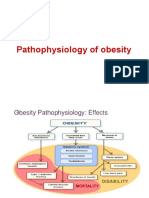
- Pathophysiology of ObesityDocument42 paginiPathophysiology of ObesityFitril WalidaÎncă nu există evaluări
- HKDSE BIOLOGY Topic 6 Food and HumansDocument13 paginiHKDSE BIOLOGY Topic 6 Food and Humans202011720Încă nu există evaluări
- DM Case StudyDocument21 paginiDM Case StudyBern TolentinoÎncă nu există evaluări
- May 2016 MS TZ0Document13 paginiMay 2016 MS TZ0Eda ŞafakÎncă nu există evaluări
- Marissiensis 2016 UmftgmDocument131 paginiMarissiensis 2016 UmftgmAdriana VillarrealÎncă nu există evaluări
- Jais e Bruning (2017) Hypothalamic Inflammation in Obesity and Metabolic DiseaseDocument10 paginiJais e Bruning (2017) Hypothalamic Inflammation in Obesity and Metabolic DiseaseAna Flávia SordiÎncă nu există evaluări
- Insulin and Its Metabolic Effects Ron RosedaleDocument2 paginiInsulin and Its Metabolic Effects Ron RosedaleBuzoianu MariaÎncă nu există evaluări
- Gastro Oesophageal RefluxDocument7 paginiGastro Oesophageal Refluxjustifieda13Încă nu există evaluări
- Coconut Research-Coconut Research CenterDocument38 paginiCoconut Research-Coconut Research CenterBlitzoneÎncă nu există evaluări
- The Polar Bear ParadoxDocument7 paginiThe Polar Bear ParadoxDouglas PageÎncă nu există evaluări
- SickKids Research ProgramsDocument44 paginiSickKids Research ProgramsKlutz4LifeÎncă nu există evaluări
- Effects of Sit Up Exercise Training On Adipose Cell SizeDocument7 paginiEffects of Sit Up Exercise Training On Adipose Cell SizeDeskaWijayantiÎncă nu există evaluări
- Is That a Fact?: Frauds, Quacks, and the Real Science of Everyday LifeDe la EverandIs That a Fact?: Frauds, Quacks, and the Real Science of Everyday LifeEvaluare: 5 din 5 stele5/5 (4)
- The Disappearing Spoon: And Other True Tales of Madness, Love, and the History of the World from the Periodic Table of the ElementsDe la EverandThe Disappearing Spoon: And Other True Tales of Madness, Love, and the History of the World from the Periodic Table of the ElementsEvaluare: 4 din 5 stele4/5 (146)
- The Elements We Live By: How Iron Helps Us Breathe, Potassium Lets Us See, and Other Surprising Superpowers of the Periodic TableDe la EverandThe Elements We Live By: How Iron Helps Us Breathe, Potassium Lets Us See, and Other Surprising Superpowers of the Periodic TableEvaluare: 3.5 din 5 stele3.5/5 (22)
- Monkeys, Myths, and Molecules: Separating Fact from Fiction, and the Science of Everyday LifeDe la EverandMonkeys, Myths, and Molecules: Separating Fact from Fiction, and the Science of Everyday LifeEvaluare: 4 din 5 stele4/5 (1)
- Chemistry for Breakfast: The Amazing Science of Everyday LifeDe la EverandChemistry for Breakfast: The Amazing Science of Everyday LifeEvaluare: 4.5 din 5 stele4.5/5 (90)
- Periodic Tales: A Cultural History of the Elements, from Arsenic to ZincDe la EverandPeriodic Tales: A Cultural History of the Elements, from Arsenic to ZincEvaluare: 3.5 din 5 stele3.5/5 (137)
- The Nature of Drugs Vol. 1: History, Pharmacology, and Social ImpactDe la EverandThe Nature of Drugs Vol. 1: History, Pharmacology, and Social ImpactEvaluare: 5 din 5 stele5/5 (5)