Documente Academic
Documente Profesional
Documente Cultură
Laproscopic Vagotony Paper
Încărcat de
peter_mrDescriere originală:
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Laproscopic Vagotony Paper
Încărcat de
peter_mrDrepturi de autor:
Formate disponibile
Bahrain Medical Bulletin, Vol. 29, No.
4, December 2007
Laparoscopic Vagotomy: Feasible Option for the Chronic Peptic Ulcer Patient Khalifa Bin Dayna, MD, German Board* Reem Al Bareeq, MRCSI, CAB(Urol)** Background: Highly selective vagotomy was developed to avoid dumping syndrome, diarrhea, bile reflux, and poor gastric emptying; the idea was to avoid vagal denervation of viscera other than the parietal cell mass. Objective: Preliminary review of the cases which underwent laparoscopic highly selective vagotomy. Design: Retrospective study. Setting: Surgical department, Salmaniya Medical Complex, Bahrain. Method: Cases of laparoscopic surgery for chronic peptic ulcer disease were retrospectively reviewed through their records from 1st January 1997 to 31st December 2003. Data were obtained about personal characteristics, operative time, complications and length of hospital stay. Result: The average age of these patients was 44.9 years, ranging from 33 to 64 years. Nine patients were males and two patients were females. Five patients had laparoscopic highly selective vagotomy. There were no immediate postoperative complications in this group. The average length of hospital stay was 7.8 days ranging from 3-17days. Five patients had laparoscopic truncal vagotomy with open pyloroplasty. The complications reported in this group were a case of intestinal obstruction and another case of persistent symptoms. The average length of hospital stay was 16 days, ranging from 6 to 46 days. One patient underwent laparoscopic truncal vagotomy with gastro-jejunostomy due to gastric outlet obstruction. The patient had intestinal obstruction postoperatively. Conclusion: Laparoscopic highly selective vagotomy has a significantly lower complication rate than other laparoscopic surgeries for chronic peptic ulcer disease, which makes it a feasible option. However, the hospital stay for these surgeries are higher than reported studies which hinders its cost-effectiveness. Bahrain Med Bull 2007; 29(4): Peptic ulcer disease has been managed well with the advent of H2-antagonist medical therapy. In addition, by eradicating Heliobacter Pylori with triple antibiotic therapy, many patients had their symptoms alleviated. However, there are more complicated cases that have a chronic course, where surgery plays an important role in the treatment, progression of the disease and its complications1. ___________________________________________________________________ * Consultant General Surgeon ** Chief Resident Salmaniya Medical Complex Kingdom of Bahrain
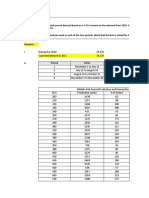
The indications for surgical intervention are intractable chronic peptic ulcer disease resistant to optimal medical therapy, duodenal ulcer bleeding and pyloric stenosis2. Highly selective vagotomy will decrease the sensitivity of the parietal cells to stimulation and the release of acid and avoids the undesired effect of delayed gastric emptying which necessitates a drainage procedure3. This procedure can be done laparoscopically which makes it minimally invasive. Although both vagotomy with antrectomy and vagotomy with pyloroplasty drainage can manage duodenal ulcers, they are associated with several complications, including dumping syndrome, diarrhea, bile reflux, and poor gastric emptying. Highly selective vagotomy was developed to avoid these complications; the idea was to avoid vagal denervation of viscera other than the parietal cell mass while keeping the pylorus mechanically and functionally intact. This procedure was found to reduce postvagotomy diarrhea and dumping dramatically4. This retrospective study reviews the cases of laparoscopic highly selective vagotomies and complications associated with this procedure. METHOD Cases of laparoscopic surgery for chronic peptic ulcer disease were retrospectively reviewed through their records from 1st January 1997 to 31st December 2003. Data were obtained about personal characteristics, operative time, complications and length of hospital stay. RESULT Eleven patients had laparoscopic surgery for chronic peptic ulcer disease during the study period. The types of surgery included laparoscopic highly selective vagotomy, laparoscopic truncal vagotomy with open pyloroplasty and laparoscopic truncal vagotomy with gastro-jejunostomy. The average age of these patients was 44.9 years, ranging from 33 to 64 years. Nine patients were males and two patients were females. The indications for surgery were: Four patients had chronic pain, one had pyloric stenosis, four had both chronic pain with pyloric stenosis and two had bleeding. Five patients had laparoscopic highly selective vagotomy. Four cases were suffering from persistent symptoms and one had bleeding. The mean operative time was 165 minutes, ranging from 115 to 240 minutes. There were no immediate postoperative complications in this group. The average length of hospital stay was 7.8 days ranging from 3-17days. Five patients had laparoscopic truncal vagotomy with open pyloroplasty. Four patients presented with pyloric stenosis and one had bleeding. The mean operative time was 149 minutes, ranging from 110 to 210 minutes. The complications reported in this group were a case of intestinal obstruction and another case of persistent symptoms. The average length of hospital stay was 16 days, ranging from 6 to 46 days.
One patient underwent laparoscopic truncal vagotomy with gastro-jejunostomy due to gastric outlet obstruction. The procedure took 180 minutes. The patient had intestinal obstruction post-operatively. His length of hospitalization was 42 days. None of the patients was converted to open method. DISCUSSION Surgical therapy is reserved for the chronic complicated peptic ulcer disease patient who persists to have symptoms regardless of the effective medical therapy. Laparoscopic surgery for chronic peptic ulcers can significantly reduce the hypersecretion of acid through a minimally invasive technique. With laparoscopic highly selective vagotomy, the complications attributed to vagotomy such as delayed gastric emptying and dumping syndrome can be avoided4. In the laparoscopic highly selective vagotomy group, there were no postoperative complications seen. This result was comparable with the result found in a small study from Univeriste Libre de Bruxelles, Belgium; thirty-three patients were operated through laparoscopic highly selective vagotomy and none had any morbidity or mortality5. Another larger study reported six complications: four perforations of gastric fundus and two bleeding episodes. Conversion to open surgery was done in four cases6. However, in this study, for the laparoscopic truncal vagotomy with open pyloroplasty group, two patients had complications (40%). One case of laparoscopic truncal vagotomy with gastro-jejunostomy had post-operative intestinal obstruction. The difference between the two groups was significant. There have been studies advocating laparoscopic truncal vagotomy with open pyloroplasty for bleeding ulcers; they had no postoperative complications7. The length of hospitalization was significantly longer in this study compared to the literature. The average length for laparoscopic highly selective vagotomy was 7.8 days and for laparoscopic truncal vagotomy with open pyloroplasty was 16 days. Most studies report 1-3 days for hospitalization of patients undergoing laparoscopic highly selective vagotomy5,6,8. This study consists of a small number of patients but gives a preliminary reflection on the effectiveness of laparoscopic surgery for chronic peptic ulcer disease. CONCLUSION Laparoscopic highly selective vagotomy has a significantly lower complication rate than other laparoscopic surgeries for chronic peptic ulcer disease, which makes it a feasible option. However, the hospital stay for these surgeries is longer than reported studies which compromises its cost-effectiveness. REFERENCES . Palanivelu C, Jani K, Rajan PS. Laparoscopic Management of Acid Peptic Disease. Surg Laparosc Endosc Percutan Tech. 2006; 16(5):312-6.
. Mouiel J, Kathouda N. Laparoscopic Vagotomy for Chronic Duodenal Ulcer Disease. World Journal of Surgery 1993; 17(1):34-9. . Gadacz TR. Laparoscopic Vagotomy. The SAGES Manual: Fundamentals of Laparoscopy and GI Endoscopy, Springer 1st edition, 1998. . Clancy TE, Ashley SW. 20 Procedures for Benign and Malignant Gastric and Duodenal Disease: Introduction. ACS Surgery, Principles & Practice 2006. . Cadiere GB, Bruyns J, Hippens J, et al. Laparoscopic Highly Selective Vagotomy. Hepatogastroenterology 1999; 46(27):1500-6. . Awad N, Csendes A, Bragnetto I, et al. Laparoscopic Highly Selective Vagotomy: Technical Considerations and Preliminary Results in 119 Patients with Duodenal Ulcers or Gastroesophageal Reflux Disease. World J Surg. 1997; 21(3):261-8. . Ng JW, Yeung GH. Laparoscopic Vagotomy and Open Pyloroplasty for Bleeding Duodenal Ulcer not Controlled Endoscopically. Surg Laparosc Endosc. 1998; 8(2):127-31. . Frantzides CT, Carlson MA. Laparoscopic Highly Selective Vagotomy. J Laparoendosc Adv Surg Tech A. 1997; 7(3):143-6.
S-ar putea să vă placă și
- Robber Bridegroom Script 1 PDFDocument110 paginiRobber Bridegroom Script 1 PDFRicardo GarciaÎncă nu există evaluări
- The Craving Mind From Cigarettes To Smartphones To Love - Why We Get Hooked and How We Can Break Bad Habits PDFDocument257 paginiThe Craving Mind From Cigarettes To Smartphones To Love - Why We Get Hooked and How We Can Break Bad Habits PDFJacques Savariau92% (13)
- Verb TensesDocument3 paginiVerb TensesVeronicaGelfgren92% (12)
- Body ImageDocument7 paginiBody ImageCristie MtzÎncă nu există evaluări
- Athletic KnitDocument31 paginiAthletic KnitNish A0% (1)
- Management of Benign Breast Conditions: Part 2 - Breast Lumps and LesionsDocument3 paginiManagement of Benign Breast Conditions: Part 2 - Breast Lumps and Lesionspeter_mrÎncă nu există evaluări
- 3 Pseudoscience and FinanceDocument11 pagini3 Pseudoscience and Financemacarthur1980Încă nu există evaluări
- Injection Pump Test SpecificationsDocument3 paginiInjection Pump Test Specificationsadmin tigasaudaraÎncă nu există evaluări
- Chapter 8: Organizational LeadershipDocument21 paginiChapter 8: Organizational LeadershipSaludez Rosiellie100% (6)
- Holistic Centre: Case Study 1 - Osho International Meditation Centre, Pune, IndiaDocument4 paginiHolistic Centre: Case Study 1 - Osho International Meditation Centre, Pune, IndiaPriyesh Dubey100% (2)
- Perbedaan Penanganan Antara Laparoskopi Vs Open Repair Pada Perforasi GasterDocument7 paginiPerbedaan Penanganan Antara Laparoskopi Vs Open Repair Pada Perforasi GasterAfiani JannahÎncă nu există evaluări
- Complicated AppendicitisDocument4 paginiComplicated AppendicitisMedardo ApoloÎncă nu există evaluări
- Art07 PDFDocument6 paginiArt07 PDFadan2010Încă nu există evaluări
- Main PDFDocument4 paginiMain PDFhhÎncă nu există evaluări
- Pattern of Acute Intestinal Obstruction: Is There A Change in The Underlying Etiology?Document4 paginiPattern of Acute Intestinal Obstruction: Is There A Change in The Underlying Etiology?neildamiÎncă nu există evaluări
- A Prospective Treatment Protocol For Outpatient Laparoscopic Appendectomy For Acute AppendicitisDocument5 paginiA Prospective Treatment Protocol For Outpatient Laparoscopic Appendectomy For Acute AppendicitisBenjamin PaulinÎncă nu există evaluări
- Management of Perforated Appendicitis in Children: A Decade of Aggressive TreatmentDocument5 paginiManagement of Perforated Appendicitis in Children: A Decade of Aggressive Treatmentapi-308365861Încă nu există evaluări
- Laparoscopic Vs Open Appendectomy: Which Way To Go?Document22 paginiLaparoscopic Vs Open Appendectomy: Which Way To Go?fahryzal_noteÎncă nu există evaluări
- Presentation Sheets Zhang Dong-Yang Feb.22nd的副本Document3 paginiPresentation Sheets Zhang Dong-Yang Feb.22nd的副本YangÎncă nu există evaluări
- 1 Bjs 10662Document8 pagini1 Bjs 10662Vu Duy KienÎncă nu există evaluări
- Pattern of Acute Intestinal Obstruction Is There A PDFDocument3 paginiPattern of Acute Intestinal Obstruction Is There A PDFMaría José Díaz RojasÎncă nu există evaluări
- 268 2011 Article 1088 PDFDocument6 pagini268 2011 Article 1088 PDFIoel Tovar TrovaÎncă nu există evaluări
- Bun V34N3p223Document6 paginiBun V34N3p223pingusÎncă nu există evaluări
- Corto y Largo PlazoDocument6 paginiCorto y Largo PlazoElard Paredes MacedoÎncă nu există evaluări
- Laparoscopic Appendectomy PostoperativeDocument6 paginiLaparoscopic Appendectomy PostoperativeDamal An NasherÎncă nu există evaluări
- Surgical Outcome of Genito Urinary Fistula - RayazDocument3 paginiSurgical Outcome of Genito Urinary Fistula - RayazRiaz Ahmed ChaudhryÎncă nu există evaluări
- Laparoscopic Cholecystectomy:An Experience of 200 Cases: Original ArticleDocument4 paginiLaparoscopic Cholecystectomy:An Experience of 200 Cases: Original ArticleAndrei GheorghitaÎncă nu există evaluări
- Jurnal DewiDocument8 paginiJurnal DewiAD MonikaÎncă nu există evaluări
- Risk of Failure in Pediatric Ventriculoperitoneal Shunts Placed After Abdominal SurgeryDocument31 paginiRisk of Failure in Pediatric Ventriculoperitoneal Shunts Placed After Abdominal SurgeryWielda VeramitaÎncă nu există evaluări
- Could Laparoscopic Colon and Rectal Surgery Become The Standard of Care? A Review and Experience With 750 ProceduresDocument9 paginiCould Laparoscopic Colon and Rectal Surgery Become The Standard of Care? A Review and Experience With 750 ProcedurespingusÎncă nu există evaluări
- World Journal of Emergency Surgery: Emergency Laparoscopy - Current Best PracticeDocument9 paginiWorld Journal of Emergency Surgery: Emergency Laparoscopy - Current Best PracticeHendra JojoÎncă nu există evaluări
- Versus: Laparoscopic Open Appendectomy: Which Way To Go?Document6 paginiVersus: Laparoscopic Open Appendectomy: Which Way To Go?Claudiu Ungureanu ClauÎncă nu există evaluări
- Stapled Rectal Mucosectomy vs. Close HemorrhoidectomyDocument9 paginiStapled Rectal Mucosectomy vs. Close HemorrhoidectomyNadllely Garcia ZapataÎncă nu există evaluări
- Usefulness of Gum Chewing To Decrease Postoperative Ileus in Colorectal Surgery With Primary Anastomosis: A Randomized Controlled TrialDocument5 paginiUsefulness of Gum Chewing To Decrease Postoperative Ileus in Colorectal Surgery With Primary Anastomosis: A Randomized Controlled TrialTay LiMinÎncă nu există evaluări
- IMU Learning Outcome: Psychomotor SkillsDocument11 paginiIMU Learning Outcome: Psychomotor SkillsRameshÎncă nu există evaluări
- General Surgery: Ruptured Liver Abscess: A Novel Surgical TechniqueDocument3 paginiGeneral Surgery: Ruptured Liver Abscess: A Novel Surgical TechniqueRahul SinghÎncă nu există evaluări
- Laparoscopic Appendectomy For Complicated Appendicitis - An Evaluation of Postoperative Factors.Document5 paginiLaparoscopic Appendectomy For Complicated Appendicitis - An Evaluation of Postoperative Factors.Juan Carlos SantamariaÎncă nu există evaluări
- Laparoscopic-Assisted Versus Open Surgery For Colorectal Cancer: Short-And Long-Term Outcomes ComparisonDocument7 paginiLaparoscopic-Assisted Versus Open Surgery For Colorectal Cancer: Short-And Long-Term Outcomes ComparisonRegina SeptianiÎncă nu există evaluări
- 014 - Primary-Colorectal-Cancer - 2023 - Surgical-Oncology-Clinics-of-North-AmericaDocument16 pagini014 - Primary-Colorectal-Cancer - 2023 - Surgical-Oncology-Clinics-of-North-AmericaDr-Mohammad Ali-Fayiz Al TamimiÎncă nu există evaluări
- Postoperative Management After Loop Ileostomy Closure: Are We Keeping Patients in Hospital Too Long?Document5 paginiPostoperative Management After Loop Ileostomy Closure: Are We Keeping Patients in Hospital Too Long?shah hassaanÎncă nu există evaluări
- Journal AppDocument3 paginiJournal AppliqqamuqitaÎncă nu există evaluări
- Study On Surgical Management of Acute Intestinal Obstruction in AdultsDocument5 paginiStudy On Surgical Management of Acute Intestinal Obstruction in AdultsIzz “MOCHI” FadhliÎncă nu există evaluări
- Evidencia 1Document6 paginiEvidencia 1Ricardo Uzcategui ArreguiÎncă nu există evaluări
- International Journal of Surgery ResearchDocument4 paginiInternational Journal of Surgery Researchali aydemirÎncă nu există evaluări
- Acute Intestinal ObstructionDocument9 paginiAcute Intestinal ObstructionRoxana ElenaÎncă nu există evaluări
- Short-Term Surgical and Long-Term Survival Outcomes After Laparoscopic Distal Gastrectomy With D Lymphadenectomy For Gastric CancerDocument7 paginiShort-Term Surgical and Long-Term Survival Outcomes After Laparoscopic Distal Gastrectomy With D Lymphadenectomy For Gastric CancerThế VũÎncă nu există evaluări
- Laparoscopic Appendectomy PDFDocument4 paginiLaparoscopic Appendectomy PDFdydydyÎncă nu există evaluări
- AfrJPaediatrSurg122119-3052943 082849 PDFDocument3 paginiAfrJPaediatrSurg122119-3052943 082849 PDFAndikaÎncă nu există evaluări
- Asghar Ali OADocument4 paginiAsghar Ali OAshah hassaanÎncă nu există evaluări
- Journal Medicine: The New EnglandDocument7 paginiJournal Medicine: The New England'Muhamad Rofiq Anwar'Încă nu există evaluări
- Kunio Et Al. - 2015 - Short EsophagusDocument12 paginiKunio Et Al. - 2015 - Short EsophagusDaniel PredaÎncă nu există evaluări
- Transanal Endorectal PullthroughDocument8 paginiTransanal Endorectal PullthroughMuhammad Harmen Reza SiregarÎncă nu există evaluări
- ERAS - SMALL Bowel RADocument6 paginiERAS - SMALL Bowel RASAURIN CHAUDHARYÎncă nu există evaluări
- Apendisitis MRM 3Document8 paginiApendisitis MRM 3siti solikhaÎncă nu există evaluări
- Jurnal 3Document3 paginiJurnal 3Ega Gumilang SugiartoÎncă nu există evaluări
- Tratamiento Laparoscópico de La Obstrucción Intestinal Por BridasDocument6 paginiTratamiento Laparoscópico de La Obstrucción Intestinal Por BridasRuthycita TafurÎncă nu există evaluări
- Jurnal Fistolotomi Vs FistulektomiDocument8 paginiJurnal Fistolotomi Vs FistulektomiAndriati Nadhila100% (1)
- Acute Appendicitis in AdultsDocument19 paginiAcute Appendicitis in Adultsdimi firmatoÎncă nu există evaluări
- Cytoreductive Surgery and IntraperitonealDocument11 paginiCytoreductive Surgery and IntraperitonealJorge FallasÎncă nu există evaluări
- Cutaneous Needle Aspirations in Liver DiseaseDocument6 paginiCutaneous Needle Aspirations in Liver DiseaseRhian BrimbleÎncă nu există evaluări
- 9 Management of Common Bile-Duct Stones and Associated Gallbladder Stones: Surgical AspectsDocument14 pagini9 Management of Common Bile-Duct Stones and Associated Gallbladder Stones: Surgical AspectsekoÎncă nu există evaluări
- Laparoscopy in The Acute AbdomenDocument15 paginiLaparoscopy in The Acute AbdomenDragoiu AlexandraÎncă nu există evaluări
- Ms AJCRS 99757Document6 paginiMs AJCRS 99757Cesar DominguezÎncă nu există evaluări
- 1 s2.0 S0022480423002895 MainDocument7 pagini1 s2.0 S0022480423002895 Mainlucabarbato23Încă nu există evaluări
- Togasj 6 25Document6 paginiTogasj 6 25Prabowo SuryaningtyasÎncă nu există evaluări
- Comparison of Laparoscopy and Laparotomy in The Surgical Management of Ectopic PregnancyDocument5 paginiComparison of Laparoscopy and Laparotomy in The Surgical Management of Ectopic PregnancyFitri Maya AnggrainiÎncă nu există evaluări
- Isj-5899 oDocument5 paginiIsj-5899 oAbhiram MundleÎncă nu există evaluări
- Bar Dram 2000Document6 paginiBar Dram 2000Prasetyö AgungÎncă nu există evaluări
- Typhoid Perforation NepalDocument3 paginiTyphoid Perforation NepalMagdalena PranataÎncă nu există evaluări
- Atlas of Laparoscopic Gastrectomy for Gastric Cancer: High Resolution Image for New Surgical TechniqueDe la EverandAtlas of Laparoscopic Gastrectomy for Gastric Cancer: High Resolution Image for New Surgical TechniqueÎncă nu există evaluări
- Sjams15493 495Document3 paginiSjams15493 495peter_mrÎncă nu există evaluări
- Folic Acid Supplementation and Risk For Imperforate Anus in ChinaDocument6 paginiFolic Acid Supplementation and Risk For Imperforate Anus in Chinapeter_mrÎncă nu există evaluări
- Anorectal Malformation PDFDocument13 paginiAnorectal Malformation PDFFrinciaÎncă nu există evaluări
- Application PDFDocument2 paginiApplication PDFpeter_mrÎncă nu există evaluări
- Superficial Skin Infections and The Use of Topical and Systemic Antibiotics in General PracticeDocument4 paginiSuperficial Skin Infections and The Use of Topical and Systemic Antibiotics in General Practicepeter_mrÎncă nu există evaluări
- Leprosy in The PhilippinesDocument9 paginiLeprosy in The Philippinespeter_mrÎncă nu există evaluări
- Superficial Skin Infections and The Use of Topical and Systemic Antibiotics in General PracticeDocument4 paginiSuperficial Skin Infections and The Use of Topical and Systemic Antibiotics in General Practicepeter_mrÎncă nu există evaluări
- 8 - Treating Skin Conditions With Antihomotoxic MedicinesDocument5 pagini8 - Treating Skin Conditions With Antihomotoxic Medicinespeter_mrÎncă nu există evaluări
- Peptic Ulcer DiseaseDocument17 paginiPeptic Ulcer DiseaseHazel Anne Ison DumayasÎncă nu există evaluări
- Issues in The Diagnosis and Management of Thombocytopenic DisordersDocument45 paginiIssues in The Diagnosis and Management of Thombocytopenic Disorderspeter_mrÎncă nu există evaluări
- Asthma in Infants and Young Children Tip SheetDocument6 paginiAsthma in Infants and Young Children Tip Sheetpeter_mrÎncă nu există evaluări
- Preventing Low Birth WeightDocument17 paginiPreventing Low Birth Weightpeter_mrÎncă nu există evaluări
- 2011 Pre-Reg Pharmacy AsthmaDocument22 pagini2011 Pre-Reg Pharmacy Asthmapeter_mrÎncă nu există evaluări
- Acute UrticariaDocument7 paginiAcute UrticariarofiqulalaÎncă nu există evaluări
- Nej Me 1303818Document2 paginiNej Me 1303818peter_mrÎncă nu există evaluări
- Pharmaceutical Journal Article SSTIDocument0 paginiPharmaceutical Journal Article SSTIpeter_mrÎncă nu există evaluări
- The Effect of Ringer's Acetate VersusDocument6 paginiThe Effect of Ringer's Acetate VersussmileyginaaÎncă nu există evaluări
- Laparoscopic Repair of Perforated Peptic Ulcers Versus Conventional Open SurgeryDocument5 paginiLaparoscopic Repair of Perforated Peptic Ulcers Versus Conventional Open Surgerypeter_mrÎncă nu există evaluări
- 8 - Treating Skin Conditions With Antihomotoxic MedicinesDocument5 pagini8 - Treating Skin Conditions With Antihomotoxic Medicinespeter_mrÎncă nu există evaluări
- Kanker PayudaraDocument8 paginiKanker PayudaraNopi DindaÎncă nu există evaluări
- Treatment of Osteoarthritis of The Knee GuidelineDocument1.229 paginiTreatment of Osteoarthritis of The Knee Guidelinepeter_mrÎncă nu există evaluări
- Urticaria and Angiodema (2007)Document8 paginiUrticaria and Angiodema (2007)peter_mrÎncă nu există evaluări
- Escholarship UC Item 4tv4m3tfDocument6 paginiEscholarship UC Item 4tv4m3tfpeter_mrÎncă nu există evaluări
- Evidence FGDocument14 paginiEvidence FGpeter_mrÎncă nu există evaluări
- Articles of Incorporation 2Document5 paginiArticles of Incorporation 2Marcos DmitriÎncă nu există evaluări
- Stance AdverbsDocument36 paginiStance Adverbsremovable100% (3)
- Aptitude For Civil ServicesDocument17 paginiAptitude For Civil Servicesnagarajuvcc123Încă nu există evaluări
- Banking - BPI V Sps Yu 2010Document8 paginiBanking - BPI V Sps Yu 2010roy dÎncă nu există evaluări
- Catibog Approval Sheet EditedDocument10 paginiCatibog Approval Sheet EditedCarla ZanteÎncă nu există evaluări
- Computer Awareness: Special Edition E-BookDocument54 paginiComputer Awareness: Special Edition E-BookTanujit SahaÎncă nu există evaluări
- Independent Distributor Price List: DXN Bolivia S.R.LDocument1 paginăIndependent Distributor Price List: DXN Bolivia S.R.LAdalid Llusco QuispeÎncă nu există evaluări
- Coffee in 2018 The New Era of Coffee EverywhereDocument55 paginiCoffee in 2018 The New Era of Coffee Everywherec3memoÎncă nu există evaluări
- Jsu Matematik SR Tahun 1Document24 paginiJsu Matematik SR Tahun 1Nurul NazierahÎncă nu există evaluări
- National Service Training Program 1Document13 paginiNational Service Training Program 1Charlene NaungayanÎncă nu există evaluări
- Family Decision MakingDocument23 paginiFamily Decision MakingNishant AnandÎncă nu există evaluări
- Fini Cat K-Max 45-90 enDocument16 paginiFini Cat K-Max 45-90 enbujin.gym.essenÎncă nu există evaluări
- The Old Rugged Cross - George Bennard: RefrainDocument5 paginiThe Old Rugged Cross - George Bennard: RefrainwilsonÎncă nu există evaluări
- News Item GamesDocument35 paginiNews Item GamesUmi KuswariÎncă nu există evaluări
- Poetry Analysis The HighwaymanDocument7 paginiPoetry Analysis The Highwaymanapi-257262131Încă nu există evaluări
- AquaSorb PlantDocument2 paginiAquaSorb Plantark6of7Încă nu există evaluări
- Practice Ch5Document10 paginiPractice Ch5Ali_Asad_1932Încă nu există evaluări
- Medical Secretary: A. Duties and TasksDocument3 paginiMedical Secretary: A. Duties and TasksNoona PlaysÎncă nu există evaluări
- The Library PK - Library of Urdu BooksDocument8 paginiThe Library PK - Library of Urdu Bookszamin4pakÎncă nu există evaluări
- Group Work, Vitruvius TriadDocument14 paginiGroup Work, Vitruvius TriadManil ShresthaÎncă nu există evaluări
- On Evil - Terry EagletonDocument44 paginiOn Evil - Terry EagletonconelcaballocansadoÎncă nu există evaluări