Documente Academic
Documente Profesional
Documente Cultură
A Study On Stress, Stressors and Coping Strategies Among Malaysian Medical Students
Încărcat de
NurhafizahImfistaDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
A Study On Stress, Stressors and Coping Strategies Among Malaysian Medical Students
Încărcat de
NurhafizahImfistaDrepturi de autor:
Formate disponibile
InternatIonal Journal of StudentS reSearch
Volume 1, Issue 2, Year 2011 www.ijsronline.com
RESEARCH
A study on stress, stressors and coping strategies among Malaysian medical students
Muhamad Saiful Bahri Yusoff1, Liew Yen Yee2, Ling Heng Wei2, Tan Chin Siong2, Loke Hon Meng2, Lim Xue Bin2, Ahmad Fuad Abdul Rahim1
ABSTRACT Introduction: The milieu of tertiary education has always been regarded as a highly stressful environment for students especially for medical students. The study aims to explore the stress level, stressors, and coping strategies among first year medical students in Malaysian public universities and factors contributed to the stress at the end of year. Methodology: A multicenter cross-sectional study involving four Malaysian public universities. The 12-item General Health Questionnaire (GHQ-12), Medical Student Stressor Questionnaire (MSSQ) and Brief COPE inventory were self-administered to measure stress level, sources of stress and coping strategies respectively among the participants. Calculated sample size was 387. Results: Out of 387 selected participants, 359 (92.7%) responded to this survey. This study found that the prevalence (at the end of the year) of distressed first year medical students was 50%. The major stressors across the universities were academic-related issues. The top five coping strategies were religion, active coping, positive reinterpretation, acceptance and planning. University, parent income, academic activities, group activities, and desire related stressors were significant factors contributing to the students stress (p-value < 0.05). Conclusion: This study found that there was a high prevalence of distressed among first year medical students at the end of year, the major stressors were related to academic and contributing factors of stress were related to university, coping strategy, types of stressor and parent income status. Training first year medical students on adaptive coping strategies, managing stressors, and improving peer-group supports to the students will help to improve this condition. Key Words: Medical students, stressors, stress, coping, GHQ, MSSQ. Brief COPE Introduction The milieu of tertiary education has always been regarded as a highly stressful environment for students and especially for medical students. Studies have quoted high prevalence of stress in medical students, ranging from 21% to 56%, particularly in the first year as they face difficult moments in adjustment to new environment of medical training [1-10]. Studies have highlighted that depression in medical students becomes twice as prevalent between the beginning and end of the first year [1, 11]. In addition, numerous studies have revealed high rates of psychological morbidity in medical students at various stages of their training [1, 3-5, 12]. In Malaysia, two studies that were done at Government universities reported that 29.1 % to 41.9% of the medical students surveyed had distress [8, 10]; while a study that was done in a private medical school reported that 46.2% had distress [9]. These facts suggested that Malaysian medical students were not immune from the problem confronting the other medical students. Distress has been found to be associated with anxiety and depression [13, 14], interpersonal conflict [15], sleep problems [16], lower academic and clinical performance [17]. It was also found to decrease attention, reduce concentration, hamper decision-making, and reduce students abilities to establish good relationships with patients resulting in feeling of inadequacy and dissatisfaction with
1Medical
clinical practice in the future [15]. Furthermore, it was linked to medical student suicide [18], drug abuse [19, 20], and use of alcohol [21]. These alarming facts confirmed the negative association of distress with mental, emotional and physical morbidity. These invariably affect patients lives and communitys health. Therefore, early detection and intervention may prevent and minimize the exert effects of distress on the students in the future [1, 3, 4, 8]. It is noteworthy that stress on medical students need to be recognized, and strategies developed to improve it should be focused on both individual and situational factors [22]. Park and Adler [23] reported that effective and appropriate coping strategies may buffer the impact of newly encountered stressful situations on physical health. Therefore, using coping strategies effectively and as appropriate will undoubtedly help medical students in reducing their stress level. According to Folkman and Lazarus [24, 25], coping strategies can be grouped into two general types; problemfocused and emotion-focused. Problem-focused coping is aimed at problem solving or doing something to alter the source of stress. Emotion-focused coping is aimed at reducing or managing the emotional distress that is associated with the situation. Although most stressors elicit both types of coping, problem-focused coping tends to predominate when people feel that something constructive can be done, whereas emotion-focused coping tends to predominate when people feel that the stressor is something that must be endured [24, 25]. Carver et al. [25] and Carver [26] have proposed 16 dimensions of coping: five dimensions assess conceptually distinct aspects of problemfocused coping (active coping, planning, suppression of
Education Department, School of Medical Sciences, Universiti Sains, Kelantan, Malaysia; 2Medical Student, School of Medical Sciences, Universiti Sains Malaysia, Kelantan, Malaysia Corresponding author: Muhamad Saiful Bahri Yusoff, Email: msaiful@kb.usm.my
Yusoff et al. Int J Stud Res 2011;1(2):45-50
45
InternatIonal Journal of StudentS reSearch
Volume 1, Issue 2, Year 2011 www.ijsronline.com
RESEARCH
competing activities, restraint coping, seeking of instrumental social support); five dimensions assess aspects of what might be viewed as emotion-focused coping (seeking of emotional social support, positive reinterpretation, acceptance, denial, turning to religion); and six dimensions assess coping responses that are less useful (focus on and venting of emotions (venting), behavioral disengagement, mental disengagement (self-distraction), humor, substance use, self-blame). These coping strategies if used effectively may buffer the unwanted impacts of stressful situation on physical, emotional and mental wellbeing [23]. The purpose of this study was to explore the nature of stress, stressors, and coping strategies among first year medical students in Malaysian public universities by determining the stress level, stressors, coping strategies and factors contributing to the distress. This information is very useful for establishing a database on the extent of the problem in Malaysian public universities. It also provides valuable information for medical teachers and students regarding this common problem; and will particularly be of aid in planning interventional measures in the future. Methodology This was a multicenter cross-sectional study involving first year medical students from four Malaysian public universities in academic session 2008/2009; Universiti Sains Malaysia (USM), Universiti Putra Malaysia (UPM), Universiti Malaysia Sabah (UMS) and Universiti Malaysia Sarawak (UNIMAS). The total number of first year medical students for the four universities was approximately 800. Sample size calculated using SPPC software [27] based on Z-value of 1.98, significance level of 0.05 and prevalence of 30% was 322 students. Modified sample size after 20% dropout rate was 387 students (97 medical students from each university). Simple random sampling was done in one university and for the other three universities, convenient sampling method was applied due to logistic and timing constraints where the researchers had difficulties in obtaining student list before hand and examination periods were close to each other. A questionnaire was used for data collection. There were two parts; the first part collected the socio-demographic data and the second consisted of questions from the 12-item General Health Questionnaire (GHQ-12), Medical Student Stressor Questionnaire (MSSQ), and Brief Coping Orientation of Problem Experienced (COPE). In the first part, variables pertaining to demographic profile of the subjects were collected including information on gender, race, entry qualification, religion, parent income, parent s relationship status, university, and parents education level. One of the most widely used measurement tool to measure stress levels is the GHQ-12 [28]. Reliability coefficients of the questionnaire have ranged from 0.78 to 0.95 in various studies. The items of GHQ-12 represent 12 manifestations of stress and respondents were asked to rate the presence of each of the manifestations in themselves during recent weeks. This is done by choosing from four responses, typically being not at all, no more than usual, rather more than usual and much more than usual. The scoring
method is a binary scoring method where the two least symptomatic answers score 0 and the two most symptomatic answers score 1 i.e. 0-0-1-1. The sensitivity and specificity of the GHQ-12 score at cut-off point of 4 were 81.3% and 75.3% respectively with positive predictive value of 62.9% and therefore, caseness was considered as a score of 4 or more [29-31]. The MSSQ is a validated instrument used to identify sources of stress [32]. The items in MSSQ represent 40 possible sources of stress in medical students identified from the literature grouped into six main domains; Academic Related Stressor (ARS), Intrapersonal and Interpersonal Related Stressor (IRS), Teaching and Learning Related Stressor (TLRS), Social Related Stressor (SRS), Drive and Desire Related Stressor (DRS), and Group Activities Related Stressor (GARS). Respondents were asked to rate each source by choosing from five responses, causing no stress at all, causing mild stress, causing moderate stress, causing high stress and causing severe stress. The scoring method assigns marks from 0 to 4 to each of the responses respectively. The reliability coefficients of the stressor groups have ranged from 0.64 to 0.92 [32]. The Brief COPE is a validated inventory and is used to identify ways in managing stress [26, 33]. This inventory consists of 30 items describing coping methods and they are rated under 4 categories of responses (I havent been doing this at all, Ive been doing this a little bit, Ive been doing this a medium amount, Ive been doing this a lot) to indicate how frequent they have been doing what the items describe. There are 15 domains: behavioral and mental disengagement, active coping, seeking of instrumental support, seeking of mental support, focus, positive interpretations, planning, humor, acceptance, turning to religion, restraint coping, denial, substance abuse, suppression of competing activities and self blame. The reliability coefficients of the coping strategies have ranged from 0.50 to 0.82 [33]. Data collection was done just after examinations to measure the stress level of medical students, a period considered to be most stressful for students. Guided self-administered questionnaires were distributed to the medical students during face-to-face sessions in a lecture hall. The students were told to follow the instructions. Filling in the questionnaire took about 15 to 25 minutes and they were returned on the same day. Written consent was obtained from the participants. Completion of the questionnaires was voluntary. Permission was obtained from the medical schools and Human Ethical Committee of Universiti Sains Malaysia prior to the start of the study. Data were analyzed using Statistical Package for Social Sciences (SPSS) version 12. All data collection forms were given serial numbers. The researcher used alpha () at 0.05 and confidence interval of 95%. Descriptive statistics was applied for analysis of the demographic data, the students stress prevalence based on GHQ-12 score, the stressors, and the coping strategies. Assumptions were made before running statistical tests. Binary Logistic Regression was
Yusoff et al. Int J Stud Res 2011;1(2):45-50
46
InternatIonal Journal of StudentS reSearch
Volume 1, Issue 2, Year 2011 www.ijsronline.com
RESEARCH
applied to determine the factors contributed to stress level and its odds ratio. Results A total of 359 (92.7%) medical students responded to the survey. In general, the demographic profile reflected the Malaysian population distribution in term of gender, race and religion (Table 1).
Table 1 Socio-demographic profile of participants Variable Frequency (%)(N=359) Gender Male 133 (37.0) Female 226 (63.0) Race Malay 188 (52.4) Chinese 126 (35.1) Indian 26 (7.2) Others 19 (5.3) Entry Matriculation 278 (77.4) qualification STPM 69 (19.2) Others 12 (3.3) Religion Muslim 198 (55.2) Buddhist 83 (23.1) Christian 54 (15.0) Hindu 17 (4.7) Others 7 (1.9) University USM 98 (27.6) UPM 103 (28.9) UMS 71 (19.9) UNIMAS 84 (23.6) Father Primary 45 (12.5) education Secondary 162 (45.1) level Tertiary 140 (39.0) Others 7 (1.9) Never underwent 5 (1.4) formal education Mother Primary 59 (16.4) education Secondary 193 (53.8) level Tertiary 97 (27.0) Others 4 (1.1) Never underwent 6 (1.7) formal education Parent Less than RM 700 31 (8.6) total RM 701 RM 1500 101 (28.1) income RM 1501 RM 5000 140 (39.0) RM 5001 RM 10000 55 (15.3) RM 10001 RM 20000 20 (5.6) More than RM 20000 12 (3.3) Parent Living together 325 (90.5) relationship Divorced 13 (3.6) Mother stays alone 14 (3.9) (father passed away) Father stays alone 5 (1.4) (mother passed away) Others 2 (0.6)
Table 2 Top 10 stressors ranked by mean degree of stress as perceived by medical students (identified by the MSSQ) Rank Items *Degree of stress Mean (SD) Causing moderate to high stress 1 Tests/examinations 2.74 (0.96) 2 Large amount of contents to 2.69 (0.97) be learnt 3 Getting poor marks 2.68 (1.10) 4 Lack of time to review what 2.65 (1.06) have been learnt 5 Need to do well (self2.50 (1.18) expectation) 6 Falling behind in reading 2.34 (1.01) schedule 7 Not enough medical skill 2.30 (1.13) practice 8 Heavy workload 2.27 (0.99) 9 Having difficulty 2.29 (1.04) understanding the content 10 Unable to answer the 2.25 (1.04) questions from the teachers * Degree of stress classification: 0 - 1.00 is causing nil to mild stress, 1.01 2.00 is causing mild to moderate stress, 2.01 3.00 is causing moderate to high stress 3.01 4.00 is causing high to severe stress
The rank of coping strategies based on the mean score as rated by the medical students is depicted in table 3. The top five coping strategies practiced were turning to religion, active coping, positive reinterpretation, acceptance, and planning. Two out of the top three coping strategies were emotion-focused coping (turning to religion and positive reinterpretation).
Table 3 Rank of coping strategies according to mean score as rated by medical students Rank Coping Strategy N *Mean Std. Deviation 1 Religion 359 6.28 1.790 2 3 4 5 6 7 8 9 10 11 12 13 14 15 Active coping Positive reinterpretation Acceptance Planning Use of instrument support Self-distraction Use of emotional support Restraint coping Humor Venting of emotion Self-blame Behavioral disengagement Denial Substance abuse 359 359 359 359 359 359 359 359 359 359 359 359 359 359 6.12 6.05 5.97 5.90 5.50 5.48 5.38 5.03 4.64 4.55 4.51 3.66 3.54 2.33 1.274 1.389 1.463 1.393 1.608 1.483 1.645 1.563 1.767 1.507 1.749 1.725 1.452 0.994
The overall prevalence of distress (GHQ score of 4 as cut-off point) was 50%. Prevalence of stress for USM, UPM, UMS, and UNIMAS were 59.2%, 45.6 %, 57.7%, and 38.1% respectively. The highest prevalence of stress was in USM students, followed closely by UMS students. The top ten stressors ranked based on the degree of stress they caused as perceived by the students is shown in table 2. All the stressors were related to academic matters.
* Minimum score was 2 and maximum score was 8. Mean score interpretations were as below: 2.00 = havent been doing this at all, 2.01 to 4.00 = have been doing this a little bit, 4.01 to 6.00 = have been doing this a medium amount, 6.01 to 8.00 = have been doing this a lot
Yusoff et al. Int J Stud Res 2011;1(2):45-50
47
InternatIonal Journal of StudentS reSearch
Volume 1, Issue 2, Year 2011 www.ijsronline.com
RESEARCH
Table 4: Factors that contributed to stress level of the medical students. Variables B coefficient Wald-X2 statistics (df) Universiti UPM -0.921 6.97 (1) UMS -0.311 0.68 (1) UNIMAS -1.000 6.97 (1) USM (reference group) 10.38 (3) Parent income RM 701 RM 1500 RM 1501 RM 5000 RM 5001 RM 10000 RM 10001 RM 20000 More than RM 20000 Less than RM 700 (reference group) ARS group Causing mild to moderate stress Causing moderate to high stress Causing high to sever stress Causing nil to mild stress (reference group) DRS group Causing mild to moderate stress Causing moderate to high stress Causing high to sever stress Causing nil to mild stress (reference group) GARS group Causing mild to moderate stress Causing moderate to high stress Causing high to sever stress Causing nil to mild stress (reference group) 1.085 0.571 1.640 2.615 0.078 4.03 (1) 1.17 (1) 7.71 (1) 11.73 (1) 0.01 (1) 19.68 (5) 0.79 (1) 3.15 (1) 5.70 (1) 16.75 (3) 0.18 (1) 8.16 (1) 4.06 (1) 11.42 (3) 5.54 (1) 9.78 (1) 3.15 (1) 10.30 (3)
P-value* 0.009 0.409 0.008 0.016 0.045 0.280 0.005 0.001 0.932 0.001 0.373 0.076 0.017 0.001 0.670 0.004 0.044 0.010 0.019 0.002 0.076 0.016
Odd Ratio (95% CI) 0.398 (0.20, 0.70) 0.773 (0.35, 1.53) 0.368 (0.17, 0.77)
2.96 (1.03, 8.54) 1.77 (0.63, 4.99) 5.16 (1.62, 16.42) 13.67 (3.06, 61.10) 1.08 (0.18, 6.40)
0.991 1.978 2.789
2.69 (0.30, 23.86) 7.23 (0.81, 64.19) 16.27 (1.65, 160.48)
0.126 1.290 2.219
1.13 (0.64, 2.02) 3.63 (1.50, 8.81) 9.2 (1.06, 79.66)
0.870 1.349 1.495
2.39 (1.16, 4.93) 3.85 (1.65, 8.97) 4.46 (0.85, 23.27) 0.04
Constant -3.266 7.77 (1) 0.005 *Binary Logistic Regression test, p-value less than 0.05 was considered as significance at 95% Confident Inter val.
Binary Logistic regression (Forward Stepwise Method) was applied to determine factors which contributed to the medical students stress level. Logistic regression model indicated that there were five factors which significantly contributed toward the stress condition (Table 4): university of study, parent income, ARS score, DRS score and GARS score (X2 = 126.37, p-value < 0.001). About 40.1% of the distress condition among medical students was influenced by the five factors (Nagelkerke R2 = 0.401). Stress level among medical students were not affected by gender, race, religion, father and mother education level, parent relationship status, IRS score, SRS score, and TLRS score. Discussion This present study found that prevalence of distress among Malaysian first year medical students was high, approximately 50%. The prevalence was higher compared to the normal population [4] and findings of other local studies [8, 10, 34]. However, this finding was consistent with the findings of previous studies which showed that the prevalence of distress among medical students ranged from 21% to 56% [1-6, 8, 9, 12]. It is interesting to highlight that the baseline prevalence of distress in USM eight months prior to this study was 26.3% [10], while this study found that the prevalence was 50%; data in this study was collected during examination period.
Therefore the finding suggested that examination period is one of the reasons for the high prevalence of distress found in this study. Two studies have highlighted that depression in medical students became twice as prevalent between the beginning and end of the first year [1, 11]; perhaps, the increased risk to develop depression was due to examination pressure as found in this study. It also interesting to highlight that there was a significant difference in the stress prevalence between universities. Students in UPM and UNIMAS were at lesser risk to develop distress compare to USM. One possible reason for this was the different examination systems practiced in the universities especially the differences in the requirements as well as the importance of their end of year examination in determining their advance to the second year. This highlights an interesting and important area: the impact of particular examination designs on students mental health and behavior. Research in this aspect would certainly worth to be explored through proper study designs in the future [35]. As expected, the top ten stressors (based on ratings by the medical students) were related to academic matters. The top ten stressors were tests and examinations, large amount of contents to be learnt, lack of time to review what has been learnt, obtaining poor marks, need to do well (selfexpectation), not enough skills in medical practice, falling behind in reading schedule, heavy workload, having
Yusoff et al. Int J Stud Res 2011;1(2):45-50
48
InternatIonal Journal of StudentS reSearch
Volume 1, Issue 2, Year 2011 www.ijsronline.com
RESEARCH
difficulty understanding the content, and unable to answer questions from the teachers; all of the stressors were rated as causing moderate to high stress. The findings were in keeping with findings from other studies, although the rank of the stressors within this category may be significantly different from studies done elsewhere [36, 3, 4, 7, 10, 37]. One important lesson learnt from this finding was regardless types of curriculum implemented in medical schools, the stressors were almost similar. It is interesting to highlight those students who perceived academic stressors as causing high to severe stress are 16 times more risk to develop distress compare to those who perceived it as causing nil to mild stress as shown in table 4. This highlights the link of developing stress to a persons perception of the stressor. This fact suggests two more areas for further study: firstly the design of a curriculum which optimizes the balance between the push factors (bringing out the best in students, maintaining standards, etc.) and inducing unacceptable and unproductive stress. The second area is the focus of intervention programs. The facts suggest that training students to have a healthy mindset with positive coping strategies will be beneficial [13, 38, 39]. It is also interesting to highlight that DRS (Drive) and GARS (Group activity) scores significantly contributed to the stress condition of medical students. The higher the rating by the students on those stressor groups the higher their risk of developing distress. These facts highlighted two more areas for further scrutiny: student motivation and group skills, which are linked to student selection. Most of medical schools in Malaysia select students solely by academic merit; and it is presumed that a certain percentage of students selected will have low motivation to do medicine [40]. Professional skills, including teamwork and group skills, are also not used as selection criteria. It will be interesting to look at students in schools which do pay attention to those areas in student selection and measure their stress levels. Our study found that psychological distress among first year medical students were significantly influenced by parent income groups where to our knowledge this is the first study to report as such finding. Those medical students who their parents earned income between RM 5001 to RM 20000 were significantly at 5 to 13 times higher risk to develop psychological distress compared to those medical students who their parents earned income less than RM 700. While those medical students whose parents earned income less than RM 700, RM 701 to RM 5000 and more than RM 20000 were equally at risk to develop psychological distress. We postulated that the different of vulnerability in developing psychological distress is due to different socioeconomic status where lower socio-economic status (less than RM 5000) are used to difficulties of life while the highest socioeconomic status (income more than RM 20000) are able to fulfill their life needs, however, those in the middle income group (RM 5001 to RM 20000) are struggling to fulfill their own and other expectations. Coping strategies is defined as how a person react or response toward a stressor [41-44]. Effective and appropriate coping strategies may minimize the impact of encountered stressful situations on ones wellbeing [23]. This study found
that the major coping strategies practiced by the medical students were turning to religion, active coping and positive reinterpretation. These strategies are positive coping strategies which have been reported in studies as very adaptive and hasten the recovery from distress [43, 26, 33]. Even though positive coping strategies were adopted by the students as main coping strategies, but yet the prevalence of distress was very high. Since this was a cross-sectional study, the recovery period from distress, of those who cope with this positive coping, could not be measured. It will be interesting to explore this matter further. These facts also suggested that medical schools should conduct an intervention programs to induce awareness among the students regarding the issues. It may help the medical students to cope with the stressors especially related to academic. One of the programs that can be considered is the medical students well-being workshop as it has been reported as an effective way in inducing awareness regarding the issues to the students [38, 39]. This study has several limitations which need to be considered in the future. The first limitation was related to the study design which may not reflect the real pattern of stress in the study population. The second limitation was the sampling method of this study which may lead to sample bias that compromised accuracy of the results. The last limitation was the study population involved first year medical students only, which the results may not be generalized to other years of study. Considering all these limitations the results of this study should be interpreted cautiously. Conclusion The prevalence of stress among first year medical students in Malaysian public universities is high. Academic related problems were the major stressor among the students. The main coping strategies were religion, active coping, and positive reinterpretation. The factors most significantly contributed to the students stress level were university, parent income, and ARS, DRS and GARS scores. In conclusion, we believe that these findings prompt the requirement for higher attention to medical students during the examination period. References
1. Aktekin M, Karaman T, Senol YY, Erdem S, Erengin H, Akaydin M. Anxiety, depression and stressful life events among medical students: a prospective study in Antalya, Turkey. Med Educ, 2001;35(1):12-7. Dahlin M, Joneborg N, Runeson B. Stress and depression among medical students: a cross sectional study, Med Educ 2005;39:594-604. Firth J. Levels and sources of stress in medical students. Br Med J (Clin Res Ed) 1986;292(6529):1177-80. Guthrie E, Black D, Bagalkote H, Shaw C, Campbell M, Creed F. Psychological stress and burnout in medical students: a five-year prospective longitudinal study. J R Soc Med 1998;91(5):237-43. Guthrie EA, Black D, Shaw CM, Hamilton J, Creed FH, Tomenson B. Embarking upon a medical career: psychological morbidity in first year medical students. Med Educ 1995;29(5):337-41. Ko SM, Kua EH, Fones CSL. Stress and the undergraduate, Singapore Med. J 1999;40:627-30. Saipanish R. Stress among medical students in a Thai medical school. Med Teach 2003;25(5):502-6. Sherina MS, Lekhraj R, Nadarajan K. Prevalence of emotional disorder among medical students in a Malaysian university. Asia Pac Family Med 2003;2:213-217.
2. 3. 4.
5.
6. 7. 8.
Yusoff et al. Int J Stud Res 2011;1(2):45-50
49
InternatIonal Journal of StudentS reSearch
Volume 1, Issue 2, Year 2011 www.ijsronline.com
RESEARCH 9. Zaid ZA, Chan SC, Ho JJ. Emotional disorders among medical students in a Malaysian private medical school. Singapore Med J 2007;48(10):895-9. Yusoff MSB, Rahim AFA, Yaacob MJ. Prevalence and sources of stress among Universiti Sains Malaysia medical students. Malays J Med Sci 2010;17(1). Vitaliano PP, Maiuro RD, Russo J, Mitchell ES. Medical student distress: A longitudinal study. J Nerv Ment Dis, 1989;177(2):70-6. Miller PM, Surtees PG. Psychological symptoms and their course in first-year medical students as assessed by the Interval General Health Questionnaire (I-GHQ). Br J Psychiatry 1991;159:199-207. Shapiro SL, Shapiro DE, Schwartz GE. Stress management in medical education: a review of the literature. Acad Med 2000;75(7):748-59. Rosal MC, Ockene IS, Ockene JK, Barrett SV, Ma Y, Hebert JR. A longitudinal study of students' depression at one medical school. Acad Med 1997;72(6):542-6. Clark EJ, Rieker PP. Gender differences in relationships and stress of medical and law students. J Med Educ, 1986;61(1):32-40. Niemi PM, Vainiomaki PT. Medical students' distress - quality, continuity and gender differences during a six-year medical programme. Med Teach 2006;28(2):136-41. Linn BS, Zeppa R. Stress in junior medical students: relationship to personality and performance. J Med Educ 1984;59(1):7-12. Hays LR, Cheever T, Patel P. Medical student suicide, 1989-1994. Am J Psychiatry 1996;153(4):553-5. Newbury-Birch D, White M, Kamali F. Factors influencing alcohol and illicit drug use amongst medical students. Drug Alcohol Depend 2000;59(2):125-130. Pickard M, Bates L, Dorian M, Greig H, Saint D. Alcohol and drug use in second-year medical students at the University of Leeds. Med Educ 2000;34(2):148-150. Flaherty JA, Richman JA. Substance use and addiction among medical students, residents, and physicians. Psychiatric Clin North Am 1993;16(1):189-97. Brissie JS, Hoover-Demprey KV, Bassler OC. Individual, situational contributors to teacher burnout. J Educ Res 1988;82(2):106-12. Park CL, Adler NE. Coping styles as a predictor of health and wellbeing across the first year of medical school. Health Psychol 2003;22(6): 627-31. Folkman S, Lazarus RS. An analysis of coping in a middleaged community sample. J Health Soc Behav 1980;21:219-39. Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer; 1984;12-3. Carver CS, Scheier MF, Weintraub, JK. Assessing coping strategies: A theoretically based approach, J Pers Soc Psychol 1989; 56: 257-283. Barman A. Sample size, Precision, and Power Calculator (SPPC). Malaysia: Arunodaya Barman; 2009. McDowell I. Measuring health: A guide to rating scales and questionnaires. 3rd ed. New York; Oxford University Press; 2006; 259270. Goldberg D. Manual of the General Health Questionnaire. NFER Publishing Company; 1978. Goldberg D, Gater R, Sartorius N, Ustun TB, Piccinelli M, Gureje O, Rutter C. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol Med 1997;27(1):1917. Yusoff MSB, Rahim AFA, Yaacob MJ. The Sensitivity, Specificity and Reliability of the Malay version 12-items General Health Questionnaire (GHQ-12) in Detecting Distressed Medical Students, ASEAN J Psychiatry 2010;11(1). Yusoff MSB, Rahim AFA, Yaacob MJ. The Development and Validity of the Medical Student Stressor Questionnaire (MSSQ), ASEAN J Psychiatry 2010;11(1). Carver CS. You want to measure coping but your protocol too long: Consider the Brief COPE. Int J Behav Med 1997; 4 (1): 92-100. Zabidi-Hussin AM, Embong M. Attitude formation and ethics among medical students strategies adopted by the School of Medical Sciences Universiti Sains Malaysia. Malays J Med Sci 1997;4(1):8791. Van Der Vleutten CPM, Schuwirth LWT. Assessing professional competence: from methods to programmes, Med Educ 2005;39:30917. Kaufman DM, Day V, Mensink D. Stressors in Medical School: Relation to curriculum format and year of study. Teach Learn Medic 1998;10(3):188-94. Kaufman DM, Day V, Mensink D. Stressors in 1 st -year medical school: comparison of a conventional and problem-based curriculum. Teach Learn Med 1996;8(4):188-94. 38. Yusoff MSB, Rahim AFA. Impact of the medical students well -being in reducing medical students stress level, ASEAN J Psychiatry 2010;11(1). 39. Yusoff MSB, Rahim AFA. Experiences from a medical students' wellbeing workshop, Med Educ J 2009;43(11):1108-9. 40. Silver HK, Glicken AD. Medical student abuse. Incidence, severity, and significance. JAMA 1990;263(4):527-32. 41. Rosenham DL, Seligman MEP. Abnormal psychology. 2nd ed. New York: Norton; 1989;463-4. 42. Selye H. Stress without distress. New York: Harper & Row; 1974;1213. 43. Myers DG. Stress and Health, in: Exploring Psychology. 6th edn. New York: Worth Publishers, 2005; 402 44. Lazarus RS. Theory-Based Stress Measurement. Psychol Inq 1990;1(1):3-13.
10.
11. 12.
13. 14.
15. 16.
17. 18. 19.
Authors Contributions All authors contributed in research design, data collection, drafting article and analysis of data. Acknowledgements Our special thanks to Universiti Sains Malaysia for funding this study through short-term grant 304/PPSP/6139070. Our deepest appreciation to the medical schools of USM, UPM, UMS, and UNIMAS for allowing us to involve their medical students in this study. Our special thanks to Dr Mohamad Najib Mat Pa from Medical Education Department USM, Prof Madya Dr Narasappa Kumaraswamy from UMS Medical School, Pn Rasidah Abdul Wahad from UNIMAS Medical School, and Prof Madya Dr Latiffah Abdul Latiff from UPM Medical School for their help in our study. Last but not least, our deepest thanks to the first year medical students at USM, UPM, UNIMAS, and UMS for their participation in this study. Competing Interest This study was funded by Universiti Sains Malaysia and done by researchers from its medical school. Funding Universiti Sains 304/PPSP/6139070.
20.
21.
22. 23.
24. 25. 26. 27. 28.
29. 30.
Malaysia
Short-term
Grant
31.
32.
Please cite this paper as: Yusoff MSB, Yen Yee L, Heng Wei L, Hon Meng L, Xue Bin L, Chin Siong C, Abdul Rahmin AF. A study on stress, stressors and coping strategies among Malaysian medical students. Int J Stud Res 2011;1(2):45-50. doi: 10.5549/IJSR.1.2.45-50 This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
33. 34.
35.
36.
37.
Yusoff et al. Int J Stud Res 2011;1(2):45-50
50
S-ar putea să vă placă și
- Comprehensive Healthcare Simulation: Mastery Learning in Health Professions EducationDe la EverandComprehensive Healthcare Simulation: Mastery Learning in Health Professions EducationÎncă nu există evaluări
- Perceived Stress Among Medical Students To IdentifDocument7 paginiPerceived Stress Among Medical Students To IdentifClarisseÎncă nu există evaluări
- Academic Advising Program: A Perception From Emotions, Stress and Well-Being in University ContextDocument6 paginiAcademic Advising Program: A Perception From Emotions, Stress and Well-Being in University ContextmarluciotmÎncă nu există evaluări
- Academic StressDocument6 paginiAcademic StressagnesnovaraniÎncă nu există evaluări
- Research Article: Medical Students' Experience of and Reaction To Stress: The Role of Depression and AnxietyDocument8 paginiResearch Article: Medical Students' Experience of and Reaction To Stress: The Role of Depression and AnxietyRiama Sagita GutawaÎncă nu există evaluări
- Stres Med StudDocument4 paginiStres Med StudFaruqi FarisÎncă nu există evaluări
- Dukungan DokterDocument9 paginiDukungan DokterYosi GafriandaÎncă nu există evaluări
- Effects of COVIDDocument24 paginiEffects of COVIDMika ReyesÎncă nu există evaluări
- tmpB71A TMPDocument5 paginitmpB71A TMPFrontiersÎncă nu există evaluări
- GROUP 1 - Chapter 2 (Revised)Document9 paginiGROUP 1 - Chapter 2 (Revised)itsgumbololÎncă nu există evaluări
- The in Uence of Emotional Intelligence On Academic Stress. A Study With University of Medical Sciences StudentsDocument18 paginiThe in Uence of Emotional Intelligence On Academic Stress. A Study With University of Medical Sciences StudentsHamda EjazÎncă nu există evaluări
- Stress Coping Style 2Document20 paginiStress Coping Style 2Stephanie Bragat0% (1)
- Anxiety Among Medical StudentsDocument4 paginiAnxiety Among Medical Studentsvihaan chaudharyÎncă nu există evaluări
- Recognition of Stressors in Postgraduate PDFDocument8 paginiRecognition of Stressors in Postgraduate PDFAmalul Fadly HasibuanÎncă nu există evaluări
- A Mindfulness-Based Stress Prevention Training For Medical Students (Medimind) : Study Protocol For A Randomized Controlled TrialDocument11 paginiA Mindfulness-Based Stress Prevention Training For Medical Students (Medimind) : Study Protocol For A Randomized Controlled TrialSaur Maria Fitri SinambelaÎncă nu există evaluări
- Ayala2018 Article USMedicalStudentsWhoEngageInSe PDFDocument9 paginiAyala2018 Article USMedicalStudentsWhoEngageInSe PDFKaiken DukeÎncă nu există evaluări
- 8 03 Lin Y.MDocument6 pagini8 03 Lin Y.MAnda SmarandaÎncă nu există evaluări
- Medical Student Mental Health 3.0 ImprovingDocument5 paginiMedical Student Mental Health 3.0 Improvingmemmuse95Încă nu există evaluări
- Evaluation of Undergraduate Students' Responsiveness To A 4-Week University-Based Animal-Assisted Stress Prevention ProgramDocument16 paginiEvaluation of Undergraduate Students' Responsiveness To A 4-Week University-Based Animal-Assisted Stress Prevention ProgramFelipe FookÎncă nu există evaluări
- Personality Trait Relationship With Depression and Sucidal IdeationsDocument11 paginiPersonality Trait Relationship With Depression and Sucidal Ideationsaiza jameelÎncă nu există evaluări
- Stress and Resilience and Associated Factors Among Nursing Undergraduates in The Early Stages of The COVID-19 PandemicDocument10 paginiStress and Resilience and Associated Factors Among Nursing Undergraduates in The Early Stages of The COVID-19 PandemicIJPHSÎncă nu există evaluări
- Stress Management in Medical Education A Review.23Document12 paginiStress Management in Medical Education A Review.23Kaycee100% (1)
- Barikani, A., 2007. Stress in Medical Students. Journal of Medical Education, pp.41-44 PDFDocument4 paginiBarikani, A., 2007. Stress in Medical Students. Journal of Medical Education, pp.41-44 PDFJeane SuyantoÎncă nu există evaluări
- A Systematic Review of Depression and Anxiety in Medical Students in ChinaDocument13 paginiA Systematic Review of Depression and Anxiety in Medical Students in ChinaSteven FongÎncă nu există evaluări
- Stress Intensity of A Nursing Students Regarding ToDocument10 paginiStress Intensity of A Nursing Students Regarding ToRajaAnantaÎncă nu există evaluări
- Dr. Abraham ResearchDocument19 paginiDr. Abraham ResearchAbraham GebeyehuÎncă nu există evaluări
- The Learning Environment and Medical Student Burnout, A Multicentre Study PDFDocument9 paginiThe Learning Environment and Medical Student Burnout, A Multicentre Study PDFTalika Rifen HanifiaÎncă nu există evaluări
- Abdulghani PDFDocument6 paginiAbdulghani PDFsjhfksglakdjalfsfÎncă nu există evaluări
- DepressionDocument10 paginiDepressionKate Lucernas MayugaÎncă nu există evaluări
- Perceived Medical School Stress of Undergraduate Medical Students Predicts Academic Performance: An Observational StudyDocument6 paginiPerceived Medical School Stress of Undergraduate Medical Students Predicts Academic Performance: An Observational StudyAngelica DecalÎncă nu există evaluări
- New RLDocument7 paginiNew RLjeanelle velascoÎncă nu există evaluări
- Identifying The Sources of Academic Stress and Coping Strategies in New Nursing StudentsDocument9 paginiIdentifying The Sources of Academic Stress and Coping Strategies in New Nursing StudentsRemar Jhon PaineÎncă nu există evaluări
- Effectiveness of Aerobic Exercises On StressDocument20 paginiEffectiveness of Aerobic Exercises On StressRegina EstherÎncă nu există evaluări
- 795-Article Text-3604-4037-10-20221205Document9 pagini795-Article Text-3604-4037-10-20221205RS Research SolutionsÎncă nu există evaluări
- Predictors of Prevention Failure in College Students Participating in Two Indicated Depression Prevention ProgramsDocument19 paginiPredictors of Prevention Failure in College Students Participating in Two Indicated Depression Prevention Programs95kodok85Încă nu există evaluări
- Cfa Usmeq PDFDocument19 paginiCfa Usmeq PDFAthirah Mustaffar KamarÎncă nu există evaluări
- Bista2018 PDFDocument8 paginiBista2018 PDFYuvenn YV Cajilig CanutoÎncă nu există evaluări
- Rs SourceDocument11 paginiRs SourceAmber Jan TorresÎncă nu există evaluări
- Estressores PBLDocument8 paginiEstressores PBLFabricio BarbosaÎncă nu există evaluări
- Designing and Evaluation of E-Health Educational Intervention On Students' Physical Activity: An Application of Pender's Health Promotion ModelDocument19 paginiDesigning and Evaluation of E-Health Educational Intervention On Students' Physical Activity: An Application of Pender's Health Promotion Modelmitha letoÎncă nu există evaluări
- Stress Indicators Among 21st Century University StudentsDocument7 paginiStress Indicators Among 21st Century University Studentsbaldonidochristian03Încă nu există evaluări
- Social Sciences & Humanities: Lee, M. F. and Syaid, SDocument8 paginiSocial Sciences & Humanities: Lee, M. F. and Syaid, SHadi IdaÎncă nu există evaluări
- Aet2 10354Document8 paginiAet2 10354Edris ZamroniÎncă nu există evaluări
- A Comparison Study of Perceived Stress and Quality of Life Among Master of Pharmacy and Non-Pharmacy Master's StudentsDocument8 paginiA Comparison Study of Perceived Stress and Quality of Life Among Master of Pharmacy and Non-Pharmacy Master's StudentsHuang Zheng XianÎncă nu există evaluări
- Review of Related Literature CHRISTY FANIEDocument6 paginiReview of Related Literature CHRISTY FANIEphoenixgirl1980zÎncă nu există evaluări
- Nursing Students' Perceived Stress and Influences in Clinical PerformanceDocument5 paginiNursing Students' Perceived Stress and Influences in Clinical PerformanceAndersonTPÎncă nu există evaluări
- Journal Club Presentation IrfanaDocument16 paginiJournal Club Presentation IrfanaIrfana ThasniÎncă nu există evaluări
- Prevalence of Stress Among Medical Students in Jizan University Kingdom of Saudi ArabiaDocument7 paginiPrevalence of Stress Among Medical Students in Jizan University Kingdom of Saudi ArabiaDeby Tri Widia LestariÎncă nu există evaluări
- tmp847B TMPDocument7 paginitmp847B TMPFrontiersÎncă nu există evaluări
- The Effect of Stress Management Training Through PRECEDE-PROCEED Model On Occupational Stress Among Nurses and Midwives at Iran Hospital, IranshahrDocument5 paginiThe Effect of Stress Management Training Through PRECEDE-PROCEED Model On Occupational Stress Among Nurses and Midwives at Iran Hospital, IranshahrsatmayaniÎncă nu există evaluări
- Understanding Stress and Coping Mechanisms in Indian Student NursesDocument5 paginiUnderstanding Stress and Coping Mechanisms in Indian Student NursesJefford TorresÎncă nu există evaluări
- Temporal Trends in Medical Student Burnout: OriginalDocument6 paginiTemporal Trends in Medical Student Burnout: OriginalHendryjatiÎncă nu există evaluări
- Nursing ResearchDocument14 paginiNursing Researchzyyw.abello.uiÎncă nu există evaluări
- A Mixed Methods Study of Student Stress in PTADocument9 paginiA Mixed Methods Study of Student Stress in PTATâm TịnhÎncă nu există evaluări
- Depression, Anxiety and Symptoms of Stress Among Baccalaureate Nursing Students in Hong Kong: A Cross-Sectional StudyDocument26 paginiDepression, Anxiety and Symptoms of Stress Among Baccalaureate Nursing Students in Hong Kong: A Cross-Sectional StudyRiama Sagita GutawaÎncă nu există evaluări
- Depression, Anxiety and Symptoms of Stress Among Baccalaureate Nursing Students in Hong Kong: A Cross-Sectional StudyDocument26 paginiDepression, Anxiety and Symptoms of Stress Among Baccalaureate Nursing Students in Hong Kong: A Cross-Sectional StudyRiama Sagita GutawaÎncă nu există evaluări
- Depression, Anxiety and Symptoms of Stress Among Baccalaureate Nursing Students in Hong Kong: A Cross-Sectional StudyDocument25 paginiDepression, Anxiety and Symptoms of Stress Among Baccalaureate Nursing Students in Hong Kong: A Cross-Sectional StudyMaysoun AtoumÎncă nu există evaluări
- Romantic Relationships Mental Health and Academic Performance in Medical School A Pilot StudyDocument6 paginiRomantic Relationships Mental Health and Academic Performance in Medical School A Pilot StudyBaki HanmaÎncă nu există evaluări
- English Week 5 Task 3 Students Mental HealthDocument9 paginiEnglish Week 5 Task 3 Students Mental HealthAtyylliaaÎncă nu există evaluări
- Davies Et Al., 2014Document22 paginiDavies Et Al., 2014Bruno PereiraÎncă nu există evaluări
- Pyogenic GranulomaDocument6 paginiPyogenic GranulomaNurhafizahImfistaÎncă nu există evaluări
- Treatment of Acute Low Back PainDocument17 paginiTreatment of Acute Low Back PainNurhafizahImfistaÎncă nu există evaluări
- DafDocument1 paginăDafNurhafizahImfistaÎncă nu există evaluări
- DAPUSDocument2 paginiDAPUSsyukrinaalviÎncă nu există evaluări
- Hospital in India. Journal of Gynecologic Surgery. Vol 22/no.4. 2006Document3 paginiHospital in India. Journal of Gynecologic Surgery. Vol 22/no.4. 2006NurhafizahImfistaÎncă nu există evaluări
- 4Document6 pagini4NurhafizahImfistaÎncă nu există evaluări
- Ac PolypDocument8 paginiAc PolypDr. T. BalasubramanianÎncă nu există evaluări
- TreatmentDocument1 paginăTreatmentNurhafizahImfistaÎncă nu există evaluări
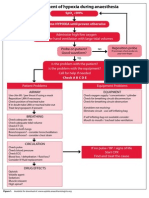
- Management of Hypoxia During AnaesthesiaDocument5 paginiManagement of Hypoxia During AnaesthesiaNurhafizahImfista100% (1)
- Management of Hypoxia During AnaesthesiaDocument5 paginiManagement of Hypoxia During AnaesthesiaNurhafizahImfista100% (1)
- Daftar PustakaDocument1 paginăDaftar PustakaNurhafizahImfistaÎncă nu există evaluări
- A Study On Stress, Stressors and Coping Strategies Among Malaysian Medical StudentsDocument6 paginiA Study On Stress, Stressors and Coping Strategies Among Malaysian Medical StudentsNurhafizahImfistaÎncă nu există evaluări
- Antrochoanal Polyp: Seung Kyu Chung, M.DDocument4 paginiAntrochoanal Polyp: Seung Kyu Chung, M.DNurhafizahImfistaÎncă nu există evaluări
- AntroChoanal Polyp SurgeryDocument14 paginiAntroChoanal Polyp SurgeryNurhafizahImfistaÎncă nu există evaluări
- OR1 Somchai TanawattanacharoenDocument6 paginiOR1 Somchai TanawattanacharoenNurhafizahImfistaÎncă nu există evaluări
- Jurnal AnastesiDocument20 paginiJurnal AnastesiNurhafizahImfistaÎncă nu există evaluări
- Vesicolithiasis With BPHDocument17 paginiVesicolithiasis With BPHNurhafizahImfistaÎncă nu există evaluări
- Gagal GinjalDocument1 paginăGagal GinjalNurhafizahImfistaÎncă nu există evaluări
- Ciarrochi Deane PID Emotional Intelligence Moderates The Relationship Between Stress and Mental Health 2002Document13 paginiCiarrochi Deane PID Emotional Intelligence Moderates The Relationship Between Stress and Mental Health 2002NurhafizahImfistaÎncă nu există evaluări
- HyperhidrosisDocument7 paginiHyperhidrosisNurhafizahImfistaÎncă nu există evaluări
- Education in Medicine Journal: Curricular Mapping: An Anti-Stress Tool For New Medical StudentsDocument7 paginiEducation in Medicine Journal: Curricular Mapping: An Anti-Stress Tool For New Medical StudentsNurhafizahImfistaÎncă nu există evaluări
- Stres Dan KognitifDocument121 paginiStres Dan KognitifNurhafizahImfistaÎncă nu există evaluări
- Gujarat Urja Vikas Nigam LTD., Vadodara: Request For ProposalDocument18 paginiGujarat Urja Vikas Nigam LTD., Vadodara: Request For ProposalABCDÎncă nu există evaluări
- Low Speed Aerators PDFDocument13 paginiLow Speed Aerators PDFDgk RajuÎncă nu există evaluări
- Maha Vedha DikshaDocument1 paginăMaha Vedha DikshaBallakrishnen SubramaniamÎncă nu există evaluări
- Analytics Designer - Comment Deletion - SAP CommunityDocument6 paginiAnalytics Designer - Comment Deletion - SAP CommunityARPITA BISWASÎncă nu există evaluări
- Fire Prevention Plan Template - FINAL 5-30-08Document5 paginiFire Prevention Plan Template - FINAL 5-30-08Peter GeorgeÎncă nu există evaluări
- International Freight 01Document5 paginiInternational Freight 01mature.ones1043Încă nu există evaluări
- 21 Tara Mantra-Wps OfficeDocument25 pagini21 Tara Mantra-Wps OfficeAlteo FallaÎncă nu există evaluări
- Functional Programming in Swift by Eidhof Chris, Kugler Florian, Swierstra Wouter.Document212 paginiFunctional Programming in Swift by Eidhof Chris, Kugler Florian, Swierstra Wouter.angloesamÎncă nu există evaluări
- Outline Calculus3Document20 paginiOutline Calculus3Joel CurtisÎncă nu există evaluări
- Clint Freeman ResumeDocument2 paginiClint Freeman ResumeClint Tiberius FreemanÎncă nu există evaluări
- Possessive Determiners: A. 1. A) B) C) 2. A) B) C) 3. A) B) C) 4. A) B) C) 5. A) B) C) 6. A) B) C) 7. A) B) C)Document1 paginăPossessive Determiners: A. 1. A) B) C) 2. A) B) C) 3. A) B) C) 4. A) B) C) 5. A) B) C) 6. A) B) C) 7. A) B) C)Manuela Marques100% (1)
- SAFE RC Design ForDocument425 paginiSAFE RC Design ForMarlon Braggian Burgos FloresÎncă nu există evaluări
- CUBE Dealer Book 2009Document280 paginiCUBE Dealer Book 2009maikruetzÎncă nu există evaluări
- L5V 00004Document2 paginiL5V 00004Jhon LinkÎncă nu există evaluări
- Changed Report 2015 PDFDocument298 paginiChanged Report 2015 PDFAnonymous FKjeRG6AFnÎncă nu există evaluări
- 2022 Tony Elumelu EntrepreneursDocument10 pagini2022 Tony Elumelu EntrepreneursOladosu EmmanuelÎncă nu există evaluări
- Camless EnginesDocument4 paginiCamless EnginesKavya M BhatÎncă nu există evaluări
- 32 Hyderabad HITEC City BisleriDocument23 pagini32 Hyderabad HITEC City BisleriSridhar ViswanathanÎncă nu există evaluări
- EZ Water Calculator 3.0.2Document4 paginiEZ Water Calculator 3.0.2adriano70Încă nu există evaluări
- 4B - Urp - Shavya's FarmDocument22 pagini4B - Urp - Shavya's FarmSnehansh KishoreÎncă nu există evaluări
- Nescom Test For AM (Electrical) ImpDocument5 paginiNescom Test For AM (Electrical) Impشاہد یونسÎncă nu există evaluări
- Paper 1 AnalysisDocument2 paginiPaper 1 AnalysisNamanÎncă nu există evaluări
- PetrifiedDocument13 paginiPetrifiedMarta GortÎncă nu există evaluări
- IMDSI22Document82 paginiIMDSI22Dang JinlongÎncă nu există evaluări
- Boarding House Preferences by Middle Up Class Students in SurabayaDocument8 paginiBoarding House Preferences by Middle Up Class Students in Surabayaeditor ijeratÎncă nu există evaluări
- Mathematics - Mathematics of Magic - A Study in Probability, Statistics, Strategy and Game Theory XDocument32 paginiMathematics - Mathematics of Magic - A Study in Probability, Statistics, Strategy and Game Theory XHarish HandÎncă nu există evaluări
- IQAc 04-05Document10 paginiIQAc 04-05ymcacollegewebsiteÎncă nu există evaluări
- Fortigate Firewall Version 4 OSDocument122 paginiFortigate Firewall Version 4 OSSam Mani Jacob DÎncă nu există evaluări
- X - WORMWOOD EVENT IMMEDIATE - Paranormal - 4chanDocument7 paginiX - WORMWOOD EVENT IMMEDIATE - Paranormal - 4chanAnonymous dIjB7XD8ZÎncă nu există evaluări
- Project Chalk CorrectionDocument85 paginiProject Chalk CorrectionEmeka Nicholas Ibekwe100% (6)
- The Stoic Mindset: Living the Ten Principles of StoicismDe la EverandThe Stoic Mindset: Living the Ten Principles of StoicismEvaluare: 5 din 5 stele5/5 (5)
- Summary: Atomic Habits by James Clear: An Easy & Proven Way to Build Good Habits & Break Bad OnesDe la EverandSummary: Atomic Habits by James Clear: An Easy & Proven Way to Build Good Habits & Break Bad OnesEvaluare: 5 din 5 stele5/5 (1635)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDe la EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeEvaluare: 2 din 5 stele2/5 (1)
- The 7 Habits of Highly Effective People: The Infographics EditionDe la EverandThe 7 Habits of Highly Effective People: The Infographics EditionEvaluare: 4 din 5 stele4/5 (2475)
- Master Your Emotions: Develop Emotional Intelligence and Discover the Essential Rules of When and How to Control Your FeelingsDe la EverandMaster Your Emotions: Develop Emotional Intelligence and Discover the Essential Rules of When and How to Control Your FeelingsEvaluare: 4.5 din 5 stele4.5/5 (321)
- Indistractable: How to Control Your Attention and Choose Your LifeDe la EverandIndistractable: How to Control Your Attention and Choose Your LifeEvaluare: 3 din 5 stele3/5 (5)
- The Power of Now: A Guide to Spiritual EnlightenmentDe la EverandThe Power of Now: A Guide to Spiritual EnlightenmentEvaluare: 4.5 din 5 stele4.5/5 (4125)
- The One Thing: The Surprisingly Simple Truth Behind Extraordinary ResultsDe la EverandThe One Thing: The Surprisingly Simple Truth Behind Extraordinary ResultsEvaluare: 4.5 din 5 stele4.5/5 (709)
- Summary: The Laws of Human Nature: by Robert Greene: Key Takeaways, Summary & AnalysisDe la EverandSummary: The Laws of Human Nature: by Robert Greene: Key Takeaways, Summary & AnalysisEvaluare: 4.5 din 5 stele4.5/5 (30)
- Summary: The Gap and the Gain: The High Achievers' Guide to Happiness, Confidence, and Success by Dan Sullivan and Dr. Benjamin Hardy: Key Takeaways, Summary & AnalysisDe la EverandSummary: The Gap and the Gain: The High Achievers' Guide to Happiness, Confidence, and Success by Dan Sullivan and Dr. Benjamin Hardy: Key Takeaways, Summary & AnalysisEvaluare: 5 din 5 stele5/5 (4)
- Becoming Supernatural: How Common People Are Doing The UncommonDe la EverandBecoming Supernatural: How Common People Are Doing The UncommonEvaluare: 5 din 5 stele5/5 (1478)
- The War of Art by Steven Pressfield - Book Summary: Break Through The Blocks And Win Your Inner Creative BattlesDe la EverandThe War of Art by Steven Pressfield - Book Summary: Break Through The Blocks And Win Your Inner Creative BattlesEvaluare: 4.5 din 5 stele4.5/5 (273)
- The 16 Undeniable Laws of Communication: Apply Them and Make the Most of Your MessageDe la EverandThe 16 Undeniable Laws of Communication: Apply Them and Make the Most of Your MessageEvaluare: 5 din 5 stele5/5 (73)
- The 5 Second Rule: Transform your Life, Work, and Confidence with Everyday CourageDe la EverandThe 5 Second Rule: Transform your Life, Work, and Confidence with Everyday CourageEvaluare: 5 din 5 stele5/5 (9)
- The Silva Mind Method: for Getting Help from the Other SideDe la EverandThe Silva Mind Method: for Getting Help from the Other SideEvaluare: 5 din 5 stele5/5 (51)
- Uptime: A Practical Guide to Personal Productivity and WellbeingDe la EverandUptime: A Practical Guide to Personal Productivity and WellbeingÎncă nu există evaluări
- Own Your Past Change Your Future: A Not-So-Complicated Approach to Relationships, Mental Health & WellnessDe la EverandOwn Your Past Change Your Future: A Not-So-Complicated Approach to Relationships, Mental Health & WellnessEvaluare: 5 din 5 stele5/5 (85)
- Mastering Productivity: Everything You Need to Know About Habit FormationDe la EverandMastering Productivity: Everything You Need to Know About Habit FormationEvaluare: 4.5 din 5 stele4.5/5 (23)
- Quantum Success: 7 Essential Laws for a Thriving, Joyful, and Prosperous Relationship with Work and MoneyDe la EverandQuantum Success: 7 Essential Laws for a Thriving, Joyful, and Prosperous Relationship with Work and MoneyEvaluare: 5 din 5 stele5/5 (38)
- Speaking Effective English!: Your Guide to Acquiring New Confidence In Personal and Professional CommunicationDe la EverandSpeaking Effective English!: Your Guide to Acquiring New Confidence In Personal and Professional CommunicationEvaluare: 4.5 din 5 stele4.5/5 (74)
- The Science of Self Discipline: How Daily Self-Discipline, Everyday Habits and an Optimised Belief System will Help You Beat Procrastination + Why Discipline Equals True FreedomDe la EverandThe Science of Self Discipline: How Daily Self-Discipline, Everyday Habits and an Optimised Belief System will Help You Beat Procrastination + Why Discipline Equals True FreedomEvaluare: 4.5 din 5 stele4.5/5 (866)
- The Motive: Why So Many Leaders Abdicate Their Most Important ResponsibilitiesDe la EverandThe Motive: Why So Many Leaders Abdicate Their Most Important ResponsibilitiesEvaluare: 5 din 5 stele5/5 (224)
- The Slight Edge: Turning Simple Disciplines into Massive Success and HappinessDe la EverandThe Slight Edge: Turning Simple Disciplines into Massive Success and HappinessEvaluare: 4.5 din 5 stele4.5/5 (117)
- Summary of The Art of Seduction by Robert GreeneDe la EverandSummary of The Art of Seduction by Robert GreeneEvaluare: 4 din 5 stele4/5 (46)
- How To Win Friends and Influence People by Dale Carnegie - Book SummaryDe la EverandHow To Win Friends and Influence People by Dale Carnegie - Book SummaryEvaluare: 5 din 5 stele5/5 (556)
- The Science of Deliberate Creation - A Quarterly Journal and Catalog Addendum - Jul, Aug, Sept, 2003 - Single Issue Pamphlet – 2003De la EverandThe Science of Deliberate Creation - A Quarterly Journal and Catalog Addendum - Jul, Aug, Sept, 2003 - Single Issue Pamphlet – 2003Evaluare: 5 din 5 stele5/5 (179)
- Leadership and Self-Deception: Getting out of the BoxDe la EverandLeadership and Self-Deception: Getting out of the BoxEvaluare: 5 din 5 stele5/5 (155)